Abstract
Introduction
Occupational therapy practice within intensive care units (ICUs) is limited with respect to published research evidence and guidelines regarding scope of practice. An understanding of the current level of service provision, feasibility of services in ICUs and training and development needs of occupational therapists is required to enable consistent best practice and promote the occupational therapy profile. This study aimed to explore occupational therapy practice within ICUs in Australia including the barriers and enablers to practice perceived by occupational therapists.
Methods
In this cross‐sectional study, a national customised online survey was completed by registered occupational therapists who provide services in intensive care settings in Australia. Recruitment was from July to September 2019 through Occupational Therapy Australia and other professional networks and interest groups.
Results
The survey was completed by 43 respondents. The majority were experienced therapists from Queensland with greater than 10‐years post‐qualification and working in a tertiary hospital setting. The most common length of time spent working in the ICU was 0–2 h per week. Formal and informal self‐care measures, cognitive screens and physical outcome measures were commonly used. Bed‐based grooming retraining, pressure care management, functional upper limb retraining and passive ranging were the most frequent interventions provided on a daily basis. Perceived barriers to occupational therapy service provision in ICU included lack of funding for staffing, competing workload demands, lack of occupational therapy role delineation and scope of practice and lack of published evidence and training.
Conclusion
Occupational therapy services in intensive care settings in Australia are limited. Published practice guidelines, further research, applications for service funding and ongoing education of the ICU multidisciplinary team regarding the scope of occupational therapy practice are recommended to promote the development of occupational therapy services in ICU.
Keywords: cognition, critical care, delirium, intensive care unit, occupational therapy, rehabilitation
Key Points for Occupational Therapy.
Occupational therapy assessment and treatment within Australian ICUs is limited and variable.
Staffing allocation is perceived as the greatest barrier to occupational therapy practice in Australian ICUs.
Opportunities for training, education and guideline development are key to embed occupational therapy practice in ICU.
1. INTRODUCTION
Intensive care unit (ICU) clinical practice, or critical care, has come under close inspection following a global pandemic, yet the standard practice relating to usual care admissions continues to benefit from enhancements to optimise care delivery. An intensive care or critical care unit houses patients who require significant medical interventions such as breathing support through ventilators and/or require daily monitoring of sedation and medications to maintain critical organ functions (College of Intensive Care Medicine, 2016). They receive one‐to‐one nursing care and constant medical monitoring. ICUs range in complexity in terms of the medical interventions they can provide, and the level is designated according to services provided. Level III units are the highest level referral unit for intensive care patients, providing multisystem life support for an indefinite period. Level II units are capable of providing complex multisystem general intensive care life support. Level I units are capable of providing immediate resuscitation and short‐term cardiorespiratory support for critically ill patients (College of Intensive Care Medicine, 2016). Level III units are often found in tertiary hospitals, Level II in secondary and Level 1 in regional and rural hospitals. Specific terminology varies between states in Australia, for example, in Queensland, ICUs are graded using a 4–6 level whereby a Grade 6 unit is equivalent to a Level III tertiary unit (Queensland Health). Worldwide, intensive care complexity may be defined differently according to public or private services; however, systems remain similar with the expectations of life‐sustaining therapies.
While the chance of surviving an ICU stay is increasing (ANZICS, 2020), survival does not always equate to a return to premorbid level of ability (Cuthbertson et al., 2010) and negative economic impacts and quality of life consequences are noted (Elliott et al., 2014). Longitudinal studies on the outcomes of critical care survival show that 30%–80% of patients will acquire post‐intensive care syndrome (PICS), characterised as a collection of complications that includes persistent cognitive dysfunction, post‐traumatic stress disorder and acquired weakness (Harvey & Davidson, 2016; Myers et al., 2016).
During an ICU admission, patients are at risk of developing cognitive impairments. The most frequent presentation includes ICU delirium that has been implicated in the development of long‐term cognitive dysfunction and functional decline (Hopkins & Jackson, 2006) contributing to PICS. Patients are also at risk of developing physical weakness from prolonged best rest or sedation (Hermans & Van den Berghe, 2015) and mental health consequences arising from factors such as occupational and sensory deprivation (Howell, 1999), the trauma of the admission process or the lack of self‐efficacy when dependent on medical equipment (Harvey & Davidson, 2016). Recent research has focused on the implementation of early rehabilitation within critical care settings to minimise PICS sequelae, and rehabilitation is now considered effective and feasible when carried out within a multidisciplinary approach (Brummel et al., 2014; Schweickert et al., 2009; Sosnowski et al., 2015). Occupational therapy, as part of early mobility, cognitive stimulation programmes and delirium management, may be beneficial for minimising symptoms of PICS for patients (Harvey & Davidson, 2016).
Although there is a paucity of published evidence regarding role establishment and clinical effectiveness within ICUs (Costigan et al., 2019; Weinreich et al., 2017), occupational therapy is arguably a key profession for progressing the early rehabilitation philosophy by addressing basic self‐care and cognitive stimulation goals. Occupational therapists use the person–environment–occupation performance model (Baum et al., 2015) to deliver individualised therapy to meet the rehabilitation objectives within intensive care settings. The framework considers the interaction between the person (their abilities and goals) within the constraints of the environment (intensive care) to complete functional tasks (such as grooming or showering). These tasks are limited in the intensive care setting due to the nature of the admission and lead to sensory and functional deprivation (Howell, 1999). The recognition of long‐term consequences, PICS, is a relatively new area of practice with little known about the extent to which and how occupational therapy has been integrated into the ICU multidisciplinary approach. Foreman (2005) explored the evolving role of occupational therapists in ICUs in Canada using a survey capturing clinical service provision. Foreman identified that high‐frequency occupational therapy activities in Canadian ICUs included splinting and swallow assessments; however, this was impacted by limited staffing and the challenge of receiving timely and appropriate referrals (Foreman, 2005). Access to occupational therapy has traditionally been low, with a US survey revealing that only 35% of units had access to a dedicated therapy team including occupational therapy and physiotherapy (Bakhru et al., 2015). Encouragingly, a more recent UK study found earlier intervention policies and greater staffing numbers improved access to occupational therapy practice in ICUs (Algeo & Aitken, 2019). A single‐site qualitative study focusing on the perceptions of a Portuguese ICU multidisciplinary team towards occupational therapy were positive and supported the introduction of occupational therapy services (Bombarda et al., 2016). However, inherent to any exploration of effectiveness of service is the identification of therapy interventions. Published literature on therapy interventions have covered a wide range of mediums such as physical input (Connolly et al., 2016) early cognitive stimulation (Bos, 1997; Gorji et al., 2014) and cognitive therapy (Brummel et al., 2014), diary use (Jones et al., 2010; Laxton, 2017) and mindfulness practices (Shaffer et al., 2016).
In Australia, the lack of information regarding the current occupational therapy service provision, the feasibility of providing occupational therapy services and the training and development needs of occupational therapists to enable consistent best practice in ICU require exploration. Implementing a service change requires the use of a model to guide the transition and ensure that all aspects are addressed to maximise long‐term gains. A Sustainability Model (NHS Improvement, 2018) was adopted to explore factors that may contribute to occupational therapy delivery in intensive care and explored processes, staffing and organisational aspects that may lead to implementation success. Using the above model, this study aimed to profile occupational therapy practice in Australian intensive care units by identifying the staffing factors (training, leadership and experience), processes (referrals, workload, interventions) and organisational aspects (staffing levels, barriers and enablers to service provision) with the intention of providing a platform for improvement.
2. METHODS
2.1. Study design
In this cross‐sectional study, a customised online survey was used to collect data from Australian occupational therapists working in ICU settings. Ethical approval for the survey was obtained from the Metro South Hospital and Health Service Human Research Ethics Committee (EC00167) and the University of Queensland Human Research Ethics Committee.
2.2. Participants
Participants were registered Australian occupational therapists who either regularly worked, or were required on occasion to provide services, in an intensive care setting (across all levels). Participants were excluded if (a) they were not based in Australia, (b) they did not have access to an ICU, (c) they were occupational therapists who worked solely in paediatric or mental health forensic intensive care services (as approaches to assessment and treatment differ significantly to medical/surgical units) and (d) they were an occupational therapy student or other allied health/nursing/medical professional. Eligibility was determined by the initial survey questions. Staffing grades for occupational therapists were determined as entry‐level therapist (<5‐year post‐qualification), senior therapist (>5‐year post‐qualification) and team leader or clinical specialist (a role defined by the organisation with significant clinical experience, usually >10 years).
Participants were recruited via multiple methods through collaboration with Occupational Therapy Australia (OTA), the national professional body. The recruitment approach included special interest group email lists, an advertisement placed in the OTA Association newsletter, a survey link hosted on the OTA website, a membership newsletter email from OTA and advertising leaflets circulated at local allied health and occupational therapy conferences nationally. The survey was kept open from 3 July to 1 November 2019 with reminders being sent at the start of each month via the email lists. No incentives for completion of the survey were provided.
2.3. Data collection
Data were gathered using a 35‐item customised online survey that was hosted on the Survey Monkey™ platform. The survey incorporated components of a Sustainability Model Improvement design and explored concepts related to process, staffing and organisational factors. The survey link was located on the OTA national website. Informed consent was gained on page 1 of the survey, which included information on the purpose, number of questions and predicted time for completion. All responses were anonymous unless respondents chose to disclose their contact details at the end of the survey. The survey was developed by the research team and piloted for usability and technical functionality by two clinical occupational therapists prior to data collection. The time taken for survey completion was 13 min on average.
The survey was divided into two sections: Section 1 contained 20 items designed to collect data on the occupational therapy services and staffing in the ICU at the respondent's hospital (organisation). This included the number full time equivalent (FTE) positions and bed numbers; the level of ICU (complexity); the number of occupational therapy staff trained to work in ICU; and key clinical caseload diagnoses and workload practices. Section 2 contained 12 items designed to profile the activities and interventions of occupational therapists working in ICU (staffing and processes) including years of experience in ICU; the most commonly seen diagnoses; commonly used assessments and outcome measures; common clinical interventions; and barriers, challenges and enablers to occupational therapy practice in ICU. A combination of closed questions with check‐box responses and open‐ended questions was used. All intervention and assessment questions were developed through a comprehensive review of published literature and recommended outcome measures for measuring intensive care survival (Gosselink et al., 2012; Needham et al., 2017).
2.4. Data analysis
Both complete and incomplete surveys were included in the final analyses. Raw data were extracted from Survey Monkey™ to an Excel spreadsheet, and the IBM Statistical Package for the Social Sciences (Version 26) was used for additional analysis. Content analysis was used to analyse open‐ended questions. Hand coding was conducted by the principal investigator to create categories with similar content grouped together.
3. RESULTS
3.1. Work setting and experience
The survey was accessed by 43 occupational therapists across Australia, with full completion of questions by 27 respondents and partial completion by 16 respondents. Participant demographics are shown in Table 1. The participant sample was predominantly female therapists over the age of 31 years, who were trained in Australia. The majority of respondents worked in Queensland (48.8%) and had greater than 5‐year post‐qualification experience (or the equivalent of a mid‐level position/Health Practitioner Grade 4) (38.1%).
TABLE 1.
Participant demographics and work setting (N = 43)
| Variable | n (valid %) |
|---|---|
| Gender | |
| Male | 1 (2.3) |
| Female | 41 (95.3) |
| Not disclosed | 1 (2.3) |
| Age (years) (n = 42) | |
| 20–25 | 3 (7.1) |
| 26–30 | 13 (31.0) |
| 31–39 | 18 (42.9) |
| 40–49 | 5 (11.9) |
| 50+ | 3 (7.1) |
| Experience as an occupational therapist (years) (n = 42) | |
| <1 year | 0 |
| 1–3 years | 0 |
| 3–5 years | 7 (16.7) |
| 5–10 years | 12 (28.6) |
| 10–15 years | 8 (19.0) |
| 15–20 years | 9 (21.4) |
| >20 years | 6 (14.3) |
| Experience working in an ICU (years) (n = 42) | |
| <0.5 year | 8 (19.1) |
| 0.5–1 year | 3 (7.1) |
| 1–3 years | 10 (23.8) |
| 3–5 years | 10 (23.8) |
| 5–10 years | 8 (19.0) |
| 10–15 years | 1 (2.4) |
| 15–20 years | 2 (4.8) |
| >20 years | 0 |
| State | |
| Queensland | 21 (48.8) |
| Victoria | 12 (27.9) |
| New South Wales | 8 (18.6) |
| South Australia | 1 (2.3) |
| Western Australia | 1 (2.3) |
| Northern Territory, Australian Capital Territory, Tasmania | 0 |
| Hospital type | |
| Tertiary | 29 (67.4) |
| Secondary | 9 (20.9) |
| Regional | 5 (11.6) |
| Rural | 0 |
| Unit dependency level | |
| Level III (highest) | 25 (58.1) |
| Level II (moderate) | 12 (27.9) |
| Level I (lowest) | 5 (11.6) |
| High dependency unit (not ICU) | 0 |
| Staffing provision (full‐time equivalent/FTE) | |
| Ad hoc/no service provided | 24 (55.8) |
| Less than 0.5 FTE | 9 (18.6) |
| Greater than 0.5FTE | 10 (20.9) |
| Staff grade covering ICU (n = 42) | |
| Entry‐level therapist | 6 (14.3) |
| Senior therapist (>5 years) | 16 (38.1) |
| Team leader/clinical specialist | 2 (4.8) |
| Multiple grades covering service | 18 (42.9) |
| Clinical time spent on ICU (n = 41) | |
| 0–2 h per week | 25 (61.0) |
| 2–7.5 h/1 full day or less | 8 (19.5) |
| 8–15 h/1–2 full days | 3 (7.3) |
| 15.5–22.5 h/2–3 full days | 1 (2.4) |
| 23–30 h/3–4 full days | 4 (9.8) |
| 38 h/5 days full time | 0 |
Experience within the intensive care setting ranged substantially. The highest number of respondents had 1–3 (23.8%) or 3–5 years (23.8%) experience in ICU with a proportion of respondents having less than 6‐month experience in ICU settings (19.1%).
Most respondents worked in a tertiary hospital within a Level III unit (58.1%). Bed numbers within each unit varied from 4 to 39 across states, with a variable service provision and mean of 0.009 FTE staffing per bed. Twenty‐four units (55.8%) were serviced on an ad hoc basis with no formal arrangement for occupational therapy services in ICU. The majority of respondents spend less than 2 h per week covering an ICU caseload (61%), with only four respondents (9.8%) covering up to 4 days in ICU. No respondents indicated they worked full time in the ICU.
The provision of orientation or training opportunities in ICU was reported as limited (19%) or absent (81%). Of the 14 respondents that provided a comment, seven described having access to a general clinical duties manual, and two indicated that the incumbent ICU therapist provided a generalised handover on rotation with the remaining five comments indicating that orientation was unsure or absent.
3.2. Patient pathways
Table 2 illustrates the patient pathways and common clinical diagnoses reported by respondents. Multiple methods were reported for referrals to occupational therapists in ICU with verbal referrals the most common method (65.1%). Blanket referrals (those not requiring a referral by virtue of diagnosis) were received in 23.3% with the blanket diagnoses listed as extracorporeal membrane oxygenation, multi‐trauma, spinal, burns, lung transplants, neurological (subarachnoid haemorrhages, Guillain–Barré syndrome), stroke or acquired brain injury diagnoses and patients who were sedated and ventilated for over 3 days. Access to goal setting meetings (in which a team collaborate on therapy progress and aims) were either absent (65%) or limited (25%) with comments on the process being ad hoc or with a focus on occupational therapy treatment only.
TABLE 2.
Patient pathways and clinical diagnoses (N = 43)
| Variable | n (valid %) |
|---|---|
| Method of referral | |
| Verbal referral | 28 (65.1) |
| Written referral | 10 (23.3) |
| Electronic notification | 25 (58.1) |
| At ward rounds | 10 (23.3) |
| At handover meetings with multidisciplinary team | 12 (27.9) |
| At clinical review/case conferences | 3 (7.0) |
| Proactive screening | 18 (41.9) |
| Blanket referral system | 10 (23.3) |
| Have access to ICU‐specific orientation package (n = 42) | 8 (19.0) |
| Access to goal setting meetings (n = 40) | |
| Yes | 10 (25.0) |
| No | 26 (65.0) |
| Other | 4 (10.0) |
| Provision of ICU step‐down service (n = 40) | |
| Yes | 20 (50.0) |
| No | 9 (22.5) |
| Other | 11 (27.5) |
| Participation in an ICU follow‐up clinic (n = 40) | |
| Yes | 0.0 |
| No | 40 (100.0) |
| Diagnoses seen | |
| Stroke | 21 (48.8) |
| Progressive neurological disease | 21 (48.8) |
| Hypoxic brain injury | 18 (41.9) |
| Sepsis/infectious disease | 18 (41.9) |
| Respiratory/pulmonary infections or conditions | 18 (41.9) |
| Cardiovascular disease | 18 (41.9) |
| Post‐surgical recovery | 18 (41.9) |
| Orthopaedic/multi‐trauma | 16 (37.2) |
| Traumatic brain injury | 16 (37.2) |
| Multi‐organ dysfunction | 14 (32.6) |
| Poisoning/drug overdose/toxic consumption | 11 (25.6) |
| Endocrine/metabolic dysfunction | 11 (25.6) |
| Spinal cord injury | 10 (23.3) |
| Gastrointestinal problems | 8 (18.6) |
| Burns/plastics | 7 (16.3) |
| Oncology/neuroplastic | 6 (14.0) |
| Mental health | 6 (14.0) |
| Maternity complications | 2 (4.7) |
| Other (not listed) | 9 (22.2) |
ICU step‐down or follow‐up processes, which enable treatment of a patient when transferred from the ICU to a general hospital ward, were varied, ranging from full handover (50%) to nil handover (25.5%). No respondents indicated that they participated in an ICU follow‐up clinic or service after discharge from hospital.
3.3. Client populations
As seen in Table 2, respondents reported providing services to a variety of client populations, with the most frequent diagnoses including stroke and other neurological conditions (48.8%), alongside respiratory conditions, cardiovascular conditions, sepsis, hypoxic brain injury and post‐surgical recovery. Twenty‐three therapists (69.7%) responded that they had no guidelines to follow, whereas the remaining respondents followed a combination of stroke guidelines, international general ICU rehabilitation guidelines, basic condition‐specific guidelines for rehabilitation and burns‐specific guidelines.
3.4. Assessments and outcome measures used in ICU
Table 3 lists cognitive, physical, psychosocial and functional assessments and outcome measures that could be used within the ICU setting, indicating the frequency of use (daily, monthly, infrequently or never used) as reported by respondents on the survey. The most commonly administered measures on a daily basis included the Glasgow Coma Scale (GCS) (37.5%), the Mental Status Questionnaire (8.3%), occupation‐based/functional activities (25.9%), manual muscle testing (20%) and range of movement using a goniometer or approximation (12.5%) Weekly administration of measures included informal or non‐standardised cognitive screens (21.7%), observation of occupation‐based or functional activities (20%), range of movement (12.5%), occupation‐based/functional activities (11.1%) and manual muscle testing (8%). All other assessments were either used monthly, infrequently or never used and often related to more specific or complex assessments such as the ASIA scoring (61.9%), the 4AT (18.2%) and the Montreal Cognitive Assessment (MoCA) (17.4%).
TABLE 3.
Assessment, outcome measures and interventions used in intensive care units by occupational therapists (N = 43)
| Valid % | |||||
|---|---|---|---|---|---|
| Daily | Weekly | Monthly | Infrequently | Never | |
| Cognitive assessments | |||||
| Glasgow Coma Scale | 37.5 | 8.3 | 8.3 | 29.2 | 16.7 |
| Mental Status Questionnaire | 8.3 | 16.7 | 4.2 | 20.8 | 50.0 |
| Montreal Cognitive Assessment | 0.0 | 13.0 | 17.4 | 39.1 | 30.4 |
| Short Form Informant Questionnaire on Cognitive Decline in the Elderly | 0.0 | 4.7 | 4.8 | 14.3 | 76.2 |
| Confusion Assessment Measure—ICU | 9.5 | 9.5 | 0.0 | 9.5 | 71.4 |
| The Long Confusion Assessment Measure | 0.0 | 4.8 | 0.0 | 9.5 | 85.7 |
| 4AT | 4.5 | 13.6 | 18.2 | 36.4 | 27.3 |
| Mini‐Mental Status Examination | 0.0 | 4.5 | 18.2 | 36.4 | 40.9 |
| Cognistat | 0.0 | 0.0 | 0.0 | 47.8 | 52.2 |
| Telephone Interview of Cognitive Status | 0.0 | 0.0 | 0.0 | 9.5 | 90.5 |
| Ranchos Los Amigo Scale | 4.5 | 9.1 | 4.5 | 22.7 | 59.1 |
| Sensory Modality and Rehabilitation Test | 0.0 | 0.0 | 0.0 | 5.0 | 95.0 |
| Western Sensory Neuro Profile | 0.0 | 0.0 | 0.0 | 5.0 | 95.0 |
| Wessex Head Injury Matrix | 0.0 | 0.0 | 5.0 | 5.0 | 90.0 |
| Coma Recovery Scale—Revised | 0.0 | 0.0 | 9.1 | 31.8 | 59.1 |
| Barry Rehabilitation Inpatient Screen of Cognition | 0.0 | 0.0 | 4.8 | 38.1 | 57.1 |
| Clock Drawing Test | 4.8 | 4.8 | 19.0 | 19.0 | 52.4 |
| Mini‐Cog | 5.0 | 0.0 | 0.0 | 5.0 | 90.0 |
| OT‐Assessment of Perceptual Skills Test | 0.0 | 0.0 | 0.0 | 5.0 | 95.0 |
| Westmead Post‐Traumatic Amnesia Test | 4.0 | 16.0 | 20.0 | 44.0 | 16.0 |
| PRPP | 0.0 | 4.8 | 4.8 | 0.0 | 90.5 |
| Informal/non‐standardised screens | 8.7 | 21.7 | 21.7 | 17.4 | 30.4 |
| Occupation‐based/functional observation | 8.0 | 20.0 | 24.0 | 24.0 | 24.0 |
| Other | 0.0 | 0.0 | 25.0 | 25.0 | 50.0 |
| Physical assessments | |||||
| Grip strength | 0.0 | 0.0 | 13.0 | 30.4 | 56.5 |
| Manual muscle testing | 20.0 | 8.0 | 32.0 | 36.0 | 4.0 |
| Range of movement | 12.5 | 12.5 | 20.8 | 29.2 | 25.0 |
| Tardieu Scale | 4.3 | 4.3 | 21.7 | 34.8 | 34.8 |
| Ashworth Scale | 4.5 | 4.5 | 18.2 | 36.4 | 36.4 |
| ASIA scoring | 0.0 | 0.0 | 9.5 | 28.6 | 61.9 |
| Oedema assessment | 10.7 | 7.1 | 21.4 | 35.7 | 25.0 |
| Occupation‐based/functional | 25.9 | 11.1 | 25.9 | 22.2 | 14.8 |
| Psychosocial assessments | |||||
| Interest Checklist Trauma Screening Questionnaire | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Initial interview with patient | 25.0 | 16.7 | 33.3 | 20.8 | 4.2 |
| Sleep/mood evaluation | 14.3 | 4.8 | 9.5 | 19.0 | 52.4 |
| Hospital Anxiety and Depression Scale | 0.0 | 0.0 | 5.0 | 5.0 | 90.0 |
| Beck Anxiety Inventory | 0.0 | 0.0 | 9.1 | 0.0 | 90.9 |
| Depression Anxiety Stress Scale | 0.0 | 0.0 | 0.0 | 15.0 | 85.0 |
| Impact of Events Scale—Revised | 0.0 | 0.0 | 0.0 | 5.0 | 95.0 |
| Post‐Traumatic Stress Syndrome | 0.0 | 0.0 | 0.0 | 9.1 | 90.9 |
| PTSD Checklist—Civilian Version | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| EQ‐5D | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Nottingham Health Profile | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Medical Outcomes Short Form 36‐V2 | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Sickness Impact Profile | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Other psychosocial measures | 9.1 | 0.0 | 0.0 | 9.1 | 81.8 |
| Functional outcomes measures | |||||
| Functional Independence Measure | 0.0 | 12.5 | 4.2 | 29.2 | 54.2 |
| Modified Barthel Index | 4.2 | 4.2 | 8.3 | 29.2 | 54.2 |
| Disability Rating Scale | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Early Rehabilitation Barthel Index | 0.0 | 0.0 | 0.0 | 5.0 | 95.0 |
| Functional Assessment Measure | 0.0 | 0.0 | 0.0 | 5.0 | 95.0 |
| Chelsea Critical Care Physical Assessment Tool | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Critical Care Functional Rehabilitation Outcome Measure | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Functional Status Score for the Intensive Care Unit | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| ICU Mobility Scale | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Perme Score | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Physical Function in Intensive Care Test Scored | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Short Physical Performance Battery | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| SICU Optimal Mobilisation Score | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 |
| Interventions | |||||
| Bed‐based ADL retraining (e.g. grooming) | 28.0 | 16.0 | 12.0 | 28.0 | 16.0 |
| ADL retraining in bathroom | 7.7 | 19.2 | 3.8 | 42.3 | 26.9 |
| Functional transfer training | 16.7 | 20.8 | 20.8 | 29.2 | 12.5 |
| Functional upper limb retraining | 26.9 | 19.2 | 23.1 | 23.1 | 7.7 |
| Upper limb exercise programmes | 15.4 | 19.2 | 30.8 | 23.1 | 11.5 |
| Pressure care management | 29.6 | 25.9 | 33.3 | 11.1 | 0.0 |
| Oedema management | 16.0 | 12.0 | 32.0 | 32.0 | 8.0 |
| Passive range of movement tasks | 30.4 | 13.0 | 17.4 | 34.8 | 4.3 |
| Upper limb splinting | 15.4 | 3.8 | 23.1 | 46.2 | 11.5 |
| Lower limb splinting | 13.6 | 0.0 | 18.2 | 13.6 | 54.5 |
| Orientation strategies | 24.0 | 24.0 | 20.0 | 20.0 | 12.0 |
| Cognitive strategy training | 18.2 | 4.5 | 27.3 | 13.6 | 36.4 |
| Delirium management (orientation boards, day plans, activity engagement) | 20.8 | 16.7 | 25.0 | 25.0 | 12.5 |
| Low arousal sensory stimulation | 4.8 | 4.8 | 19.0 | 23.8 | 47.6 |
| Stress management | 4.8 | 0.0 | 4.8 | 23.8 | 66.7 |
| Relaxation and meditation | 4.5 | 4.5 | 4.5 | 31.8 | 54.5 |
| Assistive device prescription | 13.6 | 13.6 | 13.6 | 27.3 | 31.8 |
| ICU diaries | 0.0 | 0.0 | 5.0 | 15.0 | 80.0 |
| Mindfulness activities (e.g. colouring in) | 0.0 | 10.0 | 0.0 | 20.0 | 70.0 |
| Technology applications (e.g. iPad use for leisure/cognition) | 4.8 | 0.0 | 14.3 | 28.6 | 52.4 |
| Communication strategies | 0.0 | 14.3 | 9.5 | 23.8 | 52.4 |
| Discharge planning | 13.0 | 21.7 | 34.8 | 8.7 | 21.7 |
| Education (patient and family) | 24.0 | 20.0 | 40.0 | 12.0 | 4.0 |
| Family meetings | 8.7 | 8.7 | 17.4 | 39.1 | 26.1 |
| MDT goal setting meetings | 9.1 | 4.5 | 18.2 | 31.8 | 36.4 |
Abbreviation: PRPP, Perceive Recall Plan Perform.
When surveyed regarding psychosocial outcome measures and assessments, only a subsample of respondents (n = 28) answered this question. Of those that completed assessments, initial assessments (25%) and sleep or mood evaluations (14.3%) were completed most often as a daily, weekly and monthly measure. Infrequent assessments completed by respondents included the Depression and Anxiety Scale (15%) and the Post‐Traumatic Stress Syndrome (9.09%).
Respondents rarely reported completing outcome measures on a daily or weekly basis; rather, they reported a monthly administration of either the Functional Independence Measure (4.2%) or the Modified Barthel Index (8.3%). All other outcome measures were either never used or administered infrequently such as the Early Rehabilitation Barthel Index (5%) or the Functional Assessment Measure (5%).
3.5. Interventions performed in ICU
Table 3 also lists the most common interventions completed within ICU. Only 30 respondents answered questions regarding clinical interventions. Amongst these respondents, the most commonly completed interventions on a daily basis included passive range of movement tasks (30.4%), pressure care management (29.6%), bed‐based ADL retraining (28%), functional upper limb retraining (26.9%), orientation strategies (24%) and family and patient education (24%). All other interventions were reported as occurring less than 20% of the time. Interventions commonly completed on a weekly basis that differed to those completed daily included discharge planning (21.7%), functional transfer training (20.8%), ADL retraining in the bathroom (19.2%) and upper limb exercise programmes (using theraputty or home exercise plans) (19.2%).
Interventions never used by respondents in the ICU setting included ICU diaries (80%), mindfulness activities (70%), stress management (66.7%), relaxation and meditation (54.6%), technology applications (iPad usage for cognition/leisure) (52.4%) and communication strategies (52.4%).
3.6. Barriers and enablers for occupational therapy in ICU
When exploring the barriers, challenges and enablers of providing a service in ICU, respondents were asked to select all examples from a list of 15, relevant to their current service provision, and provide an explanation. Thirty‐two respondents completed this question. Figure 1 indicates the percentage of respondents who agreed with statements about barriers and challenges to the provision of occupational therapy in ICU.
FIGURE 1.
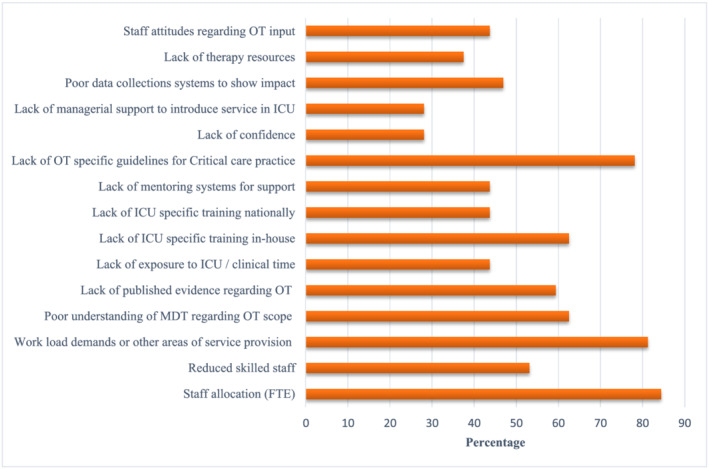
Perceived barriers and challenges for occupational therapy in intensive care
The largest barrier perceived by respondents in providing a comprehensive service in ICU related to the staffing allocation or FTE positions (84.4%). This was closely followed by the challenge of work demands or providing a service to other areas (81.3%), a lack of occupational therapy specific guidelines for critical care practice (78.1%), a poor understanding of the MDT regarding the occupational therapy scope of practice (62.5%), lack of ICU‐specific training in‐house (62.5%) and a lack of published evidence regarding occupational therapy specific interventions in the ICU setting (59.4%). The challenges identified less frequently included lack of confidence (28.1%) and lack of managerial support to introduce a service to ICU (28.1%).
Thirty‐two respondents completed an open‐ended question to detail and rank their greatest perceived barrier, which led to the identification and categorisation of three key barrier themes. The majority of respondents felt that the lack of specifically allocated staffing to cover and prioritise the ICU caseload was the main limitation in providing a service (59.3%). This was then closely influenced by a lack of guidelines or evidence to support the introduction and scope of occupational therapy in ICU settings (31.2%). The third highest ranked barrier related to a lack of training in completing specific occupational therapy interventions (12.5%).
When asked in an open‐ended question what strategies they used to promote occupational therapy within ICU, multiple strategies were cited across the sample of 24 respondents who completed the question. The key strategies were identified in relation to the ongoing lack of evidence and guidelines to support occupational therapy scope of practice (50%), the ongoing need for advocacy and promotion of the role of occupational therapy in ICU (41.7%), the importance of multidisciplinary communication and collaborative treatment opportunities (33.3%), the establishment and ongoing review of occupational therapy competencies for occupational therapy practice in ICU (16.7%) and the sustained staffing allocation to address workload management (12.5%).
Thirty‐one respondents completed the question regarding quality initiatives or current research activity. The majority of respondents (64.5%) reported that they were not completing any quality initiatives or research at this current time. Nine respondents (29%) were participating in quality initiatives on various aspects related to occupational therapy in ICU. Only 2 (6%) were currently completing or participating in research projects (both from the same hospital).
4. DISCUSSION
Occupational therapy practice within the ICU is a growing field of interest worldwide. This study is the first to describe occupational therapy practice within Australian ICUs, drawing upon a Sustainability Improvement Model (NHS Improvement, 2018), to identify key barriers and enablers that may inform a national approach towards scope and skill development. Results have shown similarities with other studies in relation to sample size limitations (Algeo & Aitken, 2019) and reduced clinical service delivery as barriers to consistent care (Foreman, 2005). Assessment and interventions delivered in Australia differ to international settings, with Australian therapists focusing more on bed‐based ADL retraining rather than seating and positioning (Algeo & Aitken, 2019) or dysphagia management (Foreman, 2005). Internationally, publications continue to highlight the benefit of adding occupational therapy to traditional rehabilitation models (Corcoran et al., 2017) through the positive perceptions of the multidisciplinary team regarding occupational therapy (Bombarda et al., 2016) and acknowledge the evolving role of occupational therapists in intensive care (Algeo & Aitken, 2019). With reference to the Sustainability Model, the areas for development and modification fall within staffing, process and organisational aspects and require varied approaches to ensure a consistent and feasible future delivery system.
4.1. Staff (experience, training, caseload)
The profile of participants in the survey indicates the sample may not be representative of all occupational therapists who provide services in Australian ICUs. There was a predominance of responses from several states that may suggest greater activity within special interest groups and the professional association through which the survey was distributed. No rural responses were submitted, which was anticipated due to the complexity of patients who would require an intensive care admission, where units are costly and only located in larger hospitals.
Similar to the survey conducted by Algeo and Aitken (2019), the majority of respondents were experienced occupational therapists; however, our cohort presented with a lower level of ICU experience. This is concerning in the light of the barriers identified by the survey in relation to training opportunities, guidelines and career development. The results suggest that occupational therapists inexperienced in ICU may be working in this complex and developing area of practice without access to sufficient training for the role. In addition, the absence of specific or targeted occupational therapy guidelines or recommendations for common diagnoses seen within intensive care, may have an overarching effect of reducing treatment consistency and ability to demonstrate the benefits of occupational therapy intervention in critical care settings.
Whereas Australia may currently be limited in training opportunities in relation to the ICU caseload, in the United Kingdom, therapists can access greater professional development courses and support bodies (Algeo & Aitken, 2019). To proactively address this, in 2020, OTA convened a special interest group to provide support and training to occupational therapists in critical care, which mirrors the approach taken by the United Kingdom in 2015 (Algeo & Aitken, 2019). The results of this survey provide data that may be useful to inform future training activities for Australian occupational therapists working in ICU, which may be supported by internally published training approaches for occupational therapists (Woodard, 2020).
Staffing levels within ICUs were identified as a barrier that impacted on role scope and clinical service delivery similar to findings of the two previous surveys (Algeo & Aitken, 2019; Foreman, 2005). In Australia, there is a lack of clear guidelines about recommended staffing ratios and the recommended daily dose of occupational therapy. The survey results indicate they fall short of the recommended level of 0.22 FTE per bed, as proposed by the UK Faculty of Intensive Care Medicine and Intensive Care Society (2019) where patients are recommended to receive 45 min of daily therapy.
4.2. Process (referrals)
The results suggest that the provision of ad hoc services and a lack of clinical presence may impact on consistent delivery of practice as well as the ability to receive timely verbal referrals. Foreman (2005) similarly identified the challenge of receiving timely and appropriate referrals in the absence of exposure. Verbal referrals are key to enabling personalised feedback to referrers and growing the service through educating other professionals on the contribution of occupational therapy to patient care.
The common caseload reported by occupational therapists differed to that identified as primary admissions sources for adult ICUs based on the ANZICS Adult Database (ANZICS, 2020). Occupational therapists identified stroke and neurological disease or acquired brain injury as the main clinical cohort rather than orthopaedic, spinal or gastrointestinal diagnoses. This may be because the top five admission diagnoses to adult ICUs result in shorter length of stay with less complexity in terms of recovery; therefore, occupational therapists may not receive referrals. All stroke admissions are mandated to be seen within the first 24–48 h for assessment as per the stroke guidelines (Stroke Foundation, 2021), possibly further influencing the perception of patient caseload seen by occupational therapists in the ICU.
4.3. Process (assessment, intervention and clinical practice)
The most common assessments were those that are easily administered to a partially sedated population, had low demands with respect to patient participation and awareness, were universal for all conditions and do not require additional training. This is in accordance with agreed assessment literature (Needham et al., 2017). Yet, although delirium assessment in ICU is supported by the literature (Farina et al., 2015), its application may be perceived to be the responsibility of nursing staff and account for the low level of administration by occupational therapists, even when randomised controlled trials support occupational therapy delirium management within intensive care settings (Alvarez et al., 2017).
Few outcome measures were consistently administered by the survey respondents. The outcome measures that are supported by the rehabilitation literature for administration within ICU appear to be out of the scope of occupational therapists and more closely linked with other rehabilitation professions in ICU such as the ICU Mobility Scale (IMS) (Hodgson et al., 2014), the Functional Status Score for ICU (FSS‐ICU) (Thrush et al., 2012) and the Chelsea Critical Care Physical Assessment Tool (CPAx) (Corner et al., 2013). There may be a lack of outcome measures sensitive to occupational therapy interventions; generic outcome measures such as the Functional Independence Measure (FIM™) may not be sensitive enough to detect the small but functionally significant changes made through therapy with some ICU patients. However, the development of new assessments may be dependent on the scope of occupational therapy being more clearly defined within the ICU setting.
The survey results also indicate several interventions are never used by Australian occupational therapists in the ICU setting including ICU diaries, stress management, relaxation and technology applications, for example, iPad usage for cognition or leisure. These interventions are recommended in the literature (Jones et al., 2010; Laxton, 2017) to minimise the impact of an ICU admission on mental health (Myhren et al., 2010; Parker et al., 2015) and prevent cognitive deterioration associated with an inability to control one's environment and communicate. Sensory overload and deprivation continue to act as key influencers of recovery and rehabilitation (Affleck et al., 1986); therefore, techniques that address these components have long been seen as beneficial (Howell, 1999). Given occupational therapy staffing limitations, further research and guidelines are required to establish common interventions that can be safely and actively introduced into the ICU rehabilitation setting either through allied health assistant roles under the guidance of occupational therapists or through education of family members on the active role they can take in supporting the recovery process (Brown et al., 2015).
4.4. Organisation (enablers, barriers and future directions)
Occupational therapy managers are noted to be supportive in promoting the scope of occupational therapy in the critical care setting. However, a greater stakeholder support from executive and funding bodies is required in order to increase the occupational therapy staffing establishment and demonstrate the cost‐effective gains of acute care occupational therapists (Rogers et al., 2016). Managerial support will enable the promotion of best practice through provision of education resources and the development of ICU guidelines within the occupational therapy framework and caseload. Survey respondents identified the greatest barriers as staffing ratios. Additional funding and caseload reorganisation are required to optimise the presence of occupational therapists in ICUs. Respondents also identified limited opportunities for training and lack of orientation protocols. A lack of training in approaches to ICU practices can also lead inconsistent service delivery, which impacts on client outcomes and team perceptions. The lack of quality improvement initiatives and research activities may reflect time limitations and restrict access to exploring the scope of best practice.
4.5. Clinical implications
There is an ongoing requirement for well‐trained specialist staffing in occupational therapy to address the complexities of rehabilitation and treatment in severe medically dependent states. There is an acknowledged limitation in processes or guidelines to direct practice for occupational therapists in ICU, and this may impact heavily on a variety of decisions relating to the effectiveness of staffing units with occupational therapists to the approach and duration of treatment sessions.
4.6. Limitations of study
Multiple limitations exist within this study due to ethical approval and governance complications. We were unable to implement a more comprehensive survey of all ICUs due to a lack of funding for the study and the complexity of variable governance systems related to the 140 public hospital ICUs and 40 private hospital ICUs (ANZICS, 2020). The sampling therefore reflected a single governance site with recruitment through OTA and networking opportunities. Similar limitations in sample size were noted as to that found in Foreman (2005) and Algeo and Aitken (2019) where exposure and practice are reduced as few occupational therapists have the opportunity to carry out services in this complex clinical area.
The assessment and outcome measures section in the survey was limited due to a lower respondent number and partially completed answers. Respondents may not have been familiar with many of the outcome measures and assessments or reduced clarity over question phrasing, leading to an avoidance of the question. Further training and consolidation on the effectiveness and scope of practice may guide future occupational therapists in selecting the most appropriate assessments and outcome measures combined with optimised exposure to clinical scenarios and awareness of literature (Needham et al., 2017). A further limitation in the study was the lack of an occupational therapy framework within the design of the survey. Future development of occupational therapy services in ICU should be grounded in occupational therapy theoretical models.
This survey shows the enthusiasm of a relatively small number of Australian occupational therapists to enrich the client‐centred care within the critical care setting, despite the lack of time or guidelines to carry out consistent practice. The use of international publications on allied health critical care clinical skills core competencies (Intensive Care Society, 2018) and rehabilitation legislation documents (National Institute of Health and Care Excellence [NICE], 2009) can further assist in consolidating and embedding a practice of occupational therapy care within intensive care settings within Australia. This survey has identified a need for ongoing training and development, in addition to research and quality improvement, to further embed the beneficial contribution of occupational therapy to critical care rehabilitation philosophy.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest pertaining to the authorship, research and/or publication of this study.
AUTHOR CONTRIBUTIONS
ARB developed the survey, wrote the manuscript and coordinated the trial management and data analysis. JF and MT advised on and contributed to the survey development, data analysis and the manuscript. All authors reviewed and approved the final manuscript.
ACKNOWLEDGEMENT
Andrea Rapolthy‐Beck has been awarded a Metro South Health Research Support Scheme Postgraduate Scholarship to pursue doctoral studies for 2018–2020. Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians. [Correction added on 19 May 2022, after first online publication: CAUL funding statement has been added.].
Rapolthy‐Beck, A. , Fleming, J. , & Turpin, M. (2022). Occupational therapy service provision in adult intensive care units in Australia: A survey of workload practices, interventions and barriers. Australian Occupational Therapy Journal, 69(3), 316–330. 10.1111/1440-1630.12794
Funding information Metro South Health
DATA AVAILABILITY STATEMENT
Data available on request from the authors
REFERENCES
- Affleck, A. T. , Lieberman, S. , Polon, J. , & Rohrkemper, K. (1986). Providing occupational therapy in an intensive care unit. The American Journal of Occupational Therapy, 40(5), 323–332. 10.5014/ajot.40.5.323 [DOI] [PubMed] [Google Scholar]
- Algeo, N. , & Aitken, L. M. (2019). The evolving role of occupational therapists in adult critical care in England: A mixed methods design using role theory. Irish Journal of Occupational Therapy, 47(2), 74–94. 10.1108/IJOT-04-2019-0005 [DOI] [Google Scholar]
- Alvarez, E. A. , Garrido, M. A. , Tobar, E. A. , Prieto, S. A. , Vergara, S. O. , Briceno, C. D. , & Gonzalez, F. J. (2017). Occupational therapy for delirium management in elderly patients without mechanical ventilation in an intensive care unit: A pilot randomized clinical trial. Journal of Critical Care, 37, 85–90. 10.1016/j.jcrc.2016.09.002 [DOI] [PubMed] [Google Scholar]
- ANZICS Centre for Outcome and Resource Evaluation . (2020). 2019 report Melbourne, Australia. https://www.anzics.com.au/annual-reports/
- Bakhru, R. N. , Wiebe, D. J. , McWilliams, D. J. , Spuhler, V. J. , & Schweickert, W. D. (2015). An environmental scan for early mobilization practices in U.S. ICUs. Critical Care Medicine, 43(11), 2360–2369. 10.1097/CCM.0000000000001262 [DOI] [PubMed] [Google Scholar]
- Baum, C. , Christiansen, C. , & Bass, J. (2015). The person‐environment‐occupation‐performance (PEOP) model. In Christiansen C. H., Baum C. M., & Bass J. D. (Eds.), Occupational therapy: Performance, participation and well‐being (4th ed.) (pp. 49–56). SLACK Incorporated. [Google Scholar]
- Bombarda, T. B. , Lanza, A. L. , Santos, C. A. S. , & Joaquim, R. (2016). The occupational therapy in adult intensive care unit (ICU) and team perceptions. Cadernos de Terapia Ocupacional, 24(4), 827–835. 10.4322/0104-4931.ctoRE0861 [DOI] [Google Scholar]
- Bos, S. (1997). Coma stimulation. The Online Journal of Knowledge Synthesis for Nursing, 4, 1. 10.1111/j.1524-475X.1997.00001.x [DOI] [PubMed] [Google Scholar]
- Brown, S. M. , Rozenblum, R. , Aboumatar, H. , Fagan, M. B. , Milic, M. , Lee, B. S. , Turner, K. , & Frosch, D. L. (2015). Defining patient and family engagement in the intensive care unit. American Journal of Respiratory and Critical Care Medicine, 191(3), 358–360. 10.1164/rccm.201410-1936LE [DOI] [PubMed] [Google Scholar]
- Brummel, N. E. , Girard, T. D. , Ely, E. W. , Pandharipande, P. P. , Morandi, A. , Hughes, C. G. , Graves, A. J. , Shintani, A. , Murphy, E. , Work, B. , Pun, B. T. , Boehm, L. , Gill, T. M. , Dittus, R. S. , & Jackson, J. C. (2014). Feasibility and safety of early combined cognitive and physical therapy for critically ill medical and surgical patients: The activity and cognitive therapy in ICU (ACT‐ICU) trial. Intensive Care Medicine, 40(3), 370–379. 10.1007/s00134-013-3136-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- College of Intensive Care Medicine of Australia and Zealand . (2016). Minimum standards for intensive care units, IC‐1(2016).
- Connolly, B. , O'Neill, B. , Salisbury, L. , Blackwood, B. , & Enhanced Recovery After Critical Illness Programme Group . (2016). Physical rehabilitation interventions for adult patients during critical illness: An overview of systematic reviews. Thorax, 71(10), 881–890. 10.1136/thoraxjnl-2015-208273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcoran, J. R. , Herbsman, J. M. , Bushnik, T. , Van Lew, S. , Stolfi, A. , Parkin, K. , McKenzie, A. , Hall, G. W. , Joseph, W. , Whiteson, J. , & Flanagan, S. R. (2017). Early rehabilitation in the medical and surgical intensive care units for patients with and without mechanical ventilation: An interprofessional performance improvement project. Physical Medicine and Rehabilitation, 9(2), 113–119. 10.1016/j.pmrj.2016.06.015 [DOI] [PubMed] [Google Scholar]
- Corner, E. J. , Wood, H. , Englebretsen, C. , Thomas, A. , Grant, R. L. , Nikoletou, D. , & Soni, N. (2013). The Chelsea critical care physical assessment tool (CPAx): Validation of an innovative new tool to measure physical morbidity in the general adult critical care population; an observational proof‐of‐concept pilot study. Physiotherapy, 99(1), 33–41. 10.1016/j.physio.2012.01.003 [DOI] [PubMed] [Google Scholar]
- Costigan, A. F. , Duffett, M. , Harris, J. E. , Baptiste, S. , & Kho, M. E. (2019). Occupational therapy in the ICU: A scoping review of 221 documents. Critical Care Medicine, 47, e1014–e1021. 10.1097/CCM.0000000000003999 [DOI] [PubMed] [Google Scholar]
- Cuthbertson, B. H. , Roughton, S. , Jenkinson, D. , Maclennan, G. , & Vale, L. (2010). Quality of life in the five years after intensive care: A cohort study. Critical Care, 14(1), R6. 10.1186/cc8848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott, D. , Davidson, J. E. , Harvey, M. A. , Bemis‐Dougherty, A. , Hopkins, R. O. , Iwashyna, T. J. , Wagner, J. , Weinert, C. , Wunsch, H. , Bienvenu, O. J. , Black, G. , Brady, S. , Brodsky, M. B. , Deutschman, C. , Doepp, D. , Flatley, C. , Fosnight, S. , Gittler, M. , Gomez, B. T. , … Needham, D. M. (2014). Exploring the scope of post‐intensive care syndrome therapy and care: Engagement of non‐critical care providers and survivors in a second stakeholders meeting. Critical Care Medicine, 42(12), 2518–2526. 10.1097/CCM.0000000000000525 [DOI] [PubMed] [Google Scholar]
- Faculty of Intensive Care Medicine and Intensive Care Society . (2019). Guidelines for the provision of intensive care services. https://www.ficm.ac.uk/sites/default/files/gpics-v2.pdf
- Farina, N. , Smithburger, P. , & Kane‐Gill, S. (2015). Screening and management of delirium in critically ill patients. Hospital Pharmacy, 50(8), 667–671. 10.1310/hpj5008-667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foreman, J. (2005). Occupational therapists' roles in intensive care. OT Now, 7, 15–18. [Google Scholar]
- Gorji, M. A. , Araghiyansc, F. , Jafari, H. , Gorgi, A. M. , & Yazdani, J. (2014). Effect of auditory stimulation on traumatic coma duration in intensive care unit of Medical Sciences University of Mazandarn, Iran. Saudi Journal of Anaesthesia, 8(1), 69–72. 10.4103/1658-354X.125940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosselink, R. , Needham, D. , & Hermans, G. (2012). ICU‐based rehabilitation and its appropriate metrics. Current Opinion in Critical Care, 18(5), 533–539. 10.1097/MCC.0b013e328357f022 [DOI] [PubMed] [Google Scholar]
- Harvey, M. A. , & Davidson, J. E. (2016). Postintensive care syndrome: Right care, right now … and later. Critical Care Medicine, 44(2), 381–385. 10.1097/CCM.0000000000001531 [DOI] [PubMed] [Google Scholar]
- Hermans, G. , & Van den Berghe, G. (2015). Clinical review: Intensive care unit acquired weakness. Critical Care, 19, 274. 10.1186/s13054-015-0993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgson, C. , Needham, D. , Haines, K. , Bailey, M. , Ward, A. , Harrold, M. , Young, P. , Zanni, J. , Buhr, H. , Higgins, A. , Presneill, J. , & Berney, S. (2014). Feasibility and inter‐rater reliability of the ICU mobility scale. Heart & Lung, 43(1), 19–24. 10.1016/j.hrtlng.2013.11.003 [DOI] [PubMed] [Google Scholar]
- Hopkins, R. O. , & Jackson, J. C. (2006). Long‐term neurocognitive function after critical illness. Chest, 130(3), 869–878. 10.1378/chest.130.3.869 [DOI] [PubMed] [Google Scholar]
- Howell, D. (1999). Neuro‐occupation: Linking sensory deprivation and self‐care in the ICU patient. Occupational Therapy in Health Care, 11(4), 75–85. 10.1080/J003v11n04_07 [DOI] [PubMed] [Google Scholar]
- Intensive Care Society . (2018). Allied health professionals: Critical care professional development framework.
- Jones, C. , Backman, C. , Capuzzo, M. , Egerod, I. , Flaatten, H. , Granja, C. , Rylander, C. , Griffiths, R. D. , & RACHEL Group . (2010). Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: A randomised, controlled trial. Critical Care, 14(5), R168. 10.1186/cc9260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laxton, L. (2017). Implementing the ICU diary in the medical intensive care unit. OT Practice, 2(2), 19–20. [Google Scholar]
- Myers, E. A. , Smith, D. A. , Allen, S. R. , & Kaplan, L. J. (2016). Post‐ICU syndrome: Rescuing the undiagnosed. JAAPA, 29(4), 34–37. 10.1097/01.JAA.0000481401.21841.32 [DOI] [PubMed] [Google Scholar]
- Myhren, H. , Ekeberg, O. , Toien, K. , Karlsson, S. , & Stokland, O. (2010). Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Critical Care, 14(1), R14. 10.1186/cc8870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Health and Care Excellence . (2009). Rehabilitation after critical illness in adults: Clinical guideline CG83. https://www.nice.org.uk/guidance/cg83 [PubMed]
- Needham, D. M. , Sepulveda, K. A. , Dinglas, V. D. , Chessare, C. M. , Friedman, L. A. , Bingham, C. O. 3rd , & Turnbull, A. E. (2017). Core outcome measures for clinical research in acute respiratory failure survivors. An international modified Delphi consensus study. American Journal of Respiratory and Critical Care Medicine, 196(9), 1122–1130. 10.1164/rccm.201702-0372OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS Improvement . (2018). Sustainability model. https://webarchive.nationalarchives.gov.uk/ukgwa/20180501161051/https://improvement.nhs.uk/resources/sustainability-model/
- Parker, A. M. , Sricharoenchai, T. , Raparla, S. , Schneck, K. W. , Bienvenu, O. J. , & Needham, D. M. (2015). Posttraumatic stress disorder in critical illness survivors: A metaanalysis. Critical Care Medicine, 43, 1121–1129. 10.1097/CCM.0000000000000882 [DOI] [PubMed] [Google Scholar]
- Rogers, A. T. , Bai, G. , Lavin, R. A. , & Anderson, G. F. (2016). Higher hospital spending on occupational therapy is associated with lower readmission rates. Medical Care Research and Review, 74, 668–686. 10.1177/1077558716666981 [DOI] [PubMed] [Google Scholar]
- Schweickert, W. D. , Pohlman, M. C. , Pohlman, A. S. , Nigos, C. , Pawlik, A. J. , Esbrook, C. L. , Spears, L. , Miller, M. , Franczyk, M. , Deprizio, D. , Schmidt, G. A. , Bowman, A. , Barr, R. , McCallister, K. E. , Hall, J. B. , & Kress, J. P. (2009). Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. The Lancet, 373(9678), 1874–1882. 10.1016/S0140-6736(09)60658-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer, K. M. , Riklin, E. , Jacobs, J. M. , Rosand, J. , & Vranceanu, A. M. (2016). Mindfulness and coping are inversely related to psychiatric symptoms in patients and informal caregivers in the neuroscience ICU: Implications for clinical care. Critical Care Medicine, 44(11), 2028–2036. 10.1097/CCM.0000000000001855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosnowski, K. , Lin, F. , Mitchell, M. L. , & White, H. (2015). Early rehabilitation in the intensive care unit: An integrative literature review. Australian Critical Care, 28, 216–225. 10.1016/j.aucc.2015.05.002 [DOI] [PubMed] [Google Scholar]
- Stroke Foundation . (2021). Clinical guidelines for stroke management. [Google Scholar]
- Thrush, A. , Rozek, M. , & Dekerlegand, J. L. (2012). The clinical utility of the functional status score for the intensive care unit (FSS‐ICU) at a long‐term acute care hospital: A prospective cohort study. Physical Therapy, 92(12), 1536–1545. 10.2522/ptj.20110412 [DOI] [PubMed] [Google Scholar]
- Weinreich, M. , Herman, J. , Dickason, S. , & Mayo, H. (2017). Occupational therapy in the intensive care unit: A systematic review. Occupational Therapy in Health Care, 31, 205–213. 10.1080/07380577.2017.1340690 [DOI] [PubMed] [Google Scholar]
- Woodard, M. M. (2020). The occupational therapy intensive care unit guide: A practical guide for implementing occupational therapy services with people who are critically ill. ProQuest Dissertations & Theses Global (2374488935).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors


