Abstract
Aims
The purpose of this study was to evaluate the accuracy of bone‐level assessments using either cone‐beam computed tomography (CBCT), intra‐oral peri‐apical (PA) radiographs or histology following reconstructive treatment of experimental peri‐implantitis.
Materials and Methods
Six Labrador dogs were used. Experimental peri‐implantitis was induced 3 months after implant placement. Surgical treatment of peri‐implantitis was performed and peri‐implant defects were allocated to one of four treatment categories; no augmentation, bone graft materials with or without a barrier membrane. Six months later, intra‐oral PA radiographs and block biopsies from all implants sites were obtained. Marginal bone levels (MBLs) were measured using PA radiographs, CBCT and histology.
Results
Significant correlations of MBL assessments were observed between the three methods. The measurements in PA radiographs consistently resulted in an overestimation of the bone level of about 0.3–0.4 mm. The agreement between the methods was not influenced by the use of bone substitute materials in the management of the osseous defects.
Conclusions
Although MBL assessments obtained from PA radiographs showed an overestimation compared to MBL assessments on corresponding CBCT images and histological sections, PA radiographs can be considered a reliable technique for peri‐implant bone‐level evaluations following reconstructive surgical therapy of experimental peri‐implantitis.
Keywords: cone‐beam computed tomography, experimental peri‐implantitis, histology, marginal bone level, radiography, reconstructive therapy
1. INTRODUCTION
Assessment of marginal bone‐level (MBL) changes is a key element in short‐ and long‐term evaluations of outcomes in implant dentistry. Although the information obtained from such procedures is confined to the mesio‐distal aspects of dental implants in intra‐oral radiographs, appraisals of interproximal bone‐level changes in epidemiological research and routine examinations in day‐to‐day clinical practice are nevertheless considered sufficient (Derks & Tomasi, 2015). The limitation of using intra‐oral radiographs should be viewed in the perspective of alternative techniques, such as cone‐beam computed tomography (CBCT), which may provide radiographic images from circumferential aspects of an implant (Raes et al., 2013; Veltri et al., 2016). While CBCT is often used in the examination of the bone structure in recipient sites for implants, its potential benefit in routine follow‐up procedures is unclear. The additional information obtained from assessments of MBL changes on buccal and lingual aspects of using CBCT should also be considered in the context of potential disadvantages and risks. Thus, the use of CBCT results in exposure of higher radiation levels to patients than that of intra‐oral radiographs (Kadesjö et al., 2018). In addition, analyses of data from pre‐clinical studies have revealed conflicting results on the accuracy of assessments of bone levels when comparing intra‐oral radiographs, CBCT and histology (Corpas et al., 2011; Ritter et al., 2014; Song et al., 2021; Stokholm et al., 2016).
Three‐dimensional radiographic assessments have also been used in the characterization of peri‐implant bony defects associated with peri‐implantitis, as their extension may encompass circumferential parts of the implant (Bender et al., 2017; Monje et al., 2018). Attempts were made to classify defect morphology and thereby facilitating the decision‐making process in treatment planning of surgical therapy of peri‐implantitis. In addition to classification of the morphology of the bone defects in peri‐implantitis sites, three‐dimensional evaluations may also be used in the evaluation of surgical treatment of such sites using reconstructive methods. The accuracy of the CBCT method as opposed to analysis of intra‐oral radiographs in this context, however, is unclear, because the detection of the ‘true’ marginal bone level may require histological techniques. In this study, data obtained from a pre‐clinical in‐vivo study on treatment of experimental peri‐implantitis (Almohandes et al., 2019) were used to evaluate the accuracy of bone‐level assessments using either CBCT, intra‐oral PA radiographs or histology.
2. MATERIALS AND METHODS
Six female, 1‐year old destination‐bred Labrador dogs (mean weight 25 kg) were used. The study protocol was approved by the regional Ethics Committee for Animal Research in Gothenburg, Sweden (Dnr 5‐2014) and the experiment was performed during 2014–2015 at the Laboratory for Experimental BioMedicine at the Sahlgrenska Academy, University of Gothenburg. The manuscript was written in accordance with ARRIVE guidelines (Kilkenny et al., 2011). At the start of the experiment, mandibular premolars and the 1st, 2nd and 3rd maxillary premolar were extracted bilaterally in each dog. After three months, four implants, 3.6 × 11 mm (EV Astra Tech Implant System™, Dentsply Implants IH AB) were installed using a non‐submerged technique on each side of the mandible. Three months later, experimental peri‐implantitis was induced using cotton ligatures and plaque formation was allowed. The ligatures were replaced every 3rd week until 40%–50% of the peri‐implant bone was lost. Four weeks after ligature removal, surgical treatment of peri‐implantitis was performed. During surgery, the implants were cleaned with curettes and cotton pellets soaked in saline and the implant sites were allocated to one of four treatment categories; (i) C; no augmentation, (ii) T1; bone defect filled with deproteinized bovine bone mineral (BioOss™) (iii) T2; bone defect filled with a biphasic bone graft material (Symbios™), (iv) T3; bone defect filled as T1 and covered with a collagen membrane (BioGide™). After suture removal, oral hygiene measures were reinstituted.
At the end of the experiment, that is six months after peri‐implantitis surgery, intra‐oral PA radiographs from all implant sites were obtained. The PA radiographs were obtained using a long‐cone paralleling technique and a digital radiography sensor (Kodak RVG 6,100 System; Carestream Health Inc.) in customized film holders (Kodak RVG RINN‐type bite blocks; Carestream Health Inc.) (Albouy, Abrahamsson, Persson, & Berglundh, 2008, 2011; Persson et al., 1999). The PA radiographs were analysed by the use of a software program (ImageJ64; National Institutes of Health). The known diameter and the inter‐thread distance of the implant were used to calibrate for the coronal–apical measurements. In the PA radiographs, the MBL was defined as the distance between the abutment‐fixture junction (A/F) and the most coronal position of bone judged to be in contact with the implant (B). MBLs were measured at the mesial and distal aspect of each implant at 10× magnification on a high‐definition monitor (Figure 1). One investigator (HL), blinded for treatment group, performed all radiographic measurements. Double measurements were made and revealed an intra‐examiner agreement (inter‐class correlation) of 0.98, with a mean (±SD) difference between the two observations of 0.20 and 0.26 mm.
FIGURE 1.

Implant site documented by a CBCT image (a), PA radiograph (b) and histological section (c). A/F, abutment /fixture (implant) border; B, the most coronal bone‐to‐implant contact
After the final examination, the dogs were euthanized with a lethal dose of Sodium‐Pentothal® (Hospira Enterprises B.V.) and perfused through the carotid arteries with a fixative (4% formaldehyde). The mandibles were retrieved and tissue blocks containing one implant and surrounding soft and hard tissues were prepared. Prior to the CBCT examination, a small mesio‐distal cut was made at the top of each implant abutment using a diamond saw (Exakt®, Kulzer). This cut indicated the position of the first intended histological section. Further, small metallic orientation markers were placed at the buccal and mesial aspects of each block (Figure 2). The specimens were then placed in a plexiglass bowl, embedded in a soft tissue equivalent material (Superflab, Eckert & Ziegler, BEBIG GmbH) and thereafter placed on a stand in the radiographic equipment. Using laser position lights, the specimen/dental implant was centred in the image volume. The radiographic examination was performed using Accuitomo 170 (J. Morita Mfg. Corp) utilizing an image volume of 40 × 40 mm, exposure parameters 80 kV, 5 mA and a 360‐degree rotation. The voxel size was set to 0.08 mm. Image data, comprising axial slices with slice thickness and interval of 0.08 mm, was exported using DICOM‐format (Digital Imaging and Communications in Medicine). Thereafter, the image data was imported into Osirix MD (Pixmeo SARL) for image processing. Reformatting was made in order to achieve optimal and standardized visualization of the dental implant and surrounding hard tissue in three to each other orthogonal planes; axial, sagittal and coronal. Reformatting was made according to the long axis of the implant and slice section according to the aforementioned mark at the top of the implant. In the CBCT images, MBL was defined as the distance between A/F and B. The MBL was assessed at four positions on each aspect around each implant (in all 16 positions/implant). Two central measurements (one corresponding to the intended histological section) and two other measurements were made 1 mm lateral to the central measurements (Figure 2). One investigator (HL) blinded for treatment group, performed all CBCT measurements. Double measurements revealed an intra‐examiner agreement (inter‐class correlation) of 0.98, with a mean (±SD) difference between the two observations of 0.04 and 0.32 mm.
FIGURE 2.

Illustration (a) showing the orientation of the histological sections. CBCT section (b) illustrating the orientation of CBCT cuts that correspond to histological sections (white line) and other lateral cuts (dotted lines). Bucco‐lingual (c) and mesio‐distal (d) CBCT image. Metallic markers were placed at the buccal and mesial aspects of each block (b and c). A mesio‐distal cut was made at the top of implant abutment (d)
Following the CBCT examination, the tissue blocks were processed for ground sectioning according to methods described by Donath and Breuner (1982). The tissue samples were dehydrated in increasing grades of ethanol and embedded in Technovit 7200 VLC‐resin (Kulzer) and prepared as previously described (Albouy et al., 2012). From each block, two parallel sections were obtained in a mesio‐distal and in a bucco‐lingual plane, respectively. The sections were reduced in thickness by microgrinding (Exakt, Apparatebau) to 30 μm and the sections from each aspect were stained in toluidine blue and fibrin stain of Ladewig (Donath & Breuner, 1982). Histological analyses were performed using a Leica DM‐RBE microscope (Leica). One examiner (OC) blinded for treatment group, performed the histomorphometric analysis of the sections using a PC‐based image analysis system (Image‐Pro Premier 9.1; Media Cybernetics Inc.,). The following landmarks were identified and used for the evaluation: the abutment/fixture (implant) border (A/F) and the most coronal bone‐to‐implant contact (B). The linear distance between A/F and B was used to assess MBL. Double measurements revealed an intra‐examiner agreement (inter‐class correlation) of 0.98, with a mean (±SD) difference between the two observations of 0.11 and 0.30 mm.
2.1. Data analysis
Using MBL assessments as the target, bivariate correlation analyses were made between data obtained from (a) histological sections and corresponding CBCT images, (b) CBCT images and corresponding PA radiographs and (c) PA radiographs and corresponding histological sections. Pearson correlation coefficient (r) were calculated and Bland–Altman plots were applied to evaluate the agreement between MBL assessments obtained from (a) histological sections and corresponding CBCT images, (b) CBCT images and PA radiographs, (c) PA radiographs and histological sections and (d) histological sections and corresponding CBCT images according to treatment category. Moreover, simple linear regression results were added to the Bland–Altman plots in order to illustrate any tendencies in the MBL differences over different bone levels. Continuous variables were presented as mean (±SD). ANOVA and Student's t test for paired samples were used to test for differences. Results from the analyses were expressed as coefficients with 95% confidence intervals. The level of statistical significance was set to p < .05. The SPSS 24.0 software package (SPSS Inc.) and GraphPad Prism version 8.3.1 (GraphPad Software) were used.
3. RESULTS
3.1. Cone‐beam computed tomography versus histology
Correlations between MBL data obtained from measurements on histological sections and corresponding CBCT images are illustrated in Figure 3. Pearson correlation coefficients (r) for mesial, distal, buccal and lingual aspects were 0.93, 0.97, 0.92 and 0.91, respectively. All correlations were statistically significant (p < .05). Plot diagrams illustrating differences in data between histological sections and corresponding CBCT images are presented in Figure 4. The mean differences in MBL data between histological sections and corresponding CBCT images at mesial, distal, buccal and lingual aspects were 0.05 ± 0.5, −0.06 ± 0.33, 0.01 ± 0.59 and −0.45 ± 0.62 mm, respectively. A simple linear regression analysis did not reveal any significant trend for differences of MBL assessments over different bone levels (Figure 4).
FIGURE 3.

Plots illustrating correlations between MBL‐data obtained from histological sections (X axis) and corresponding CBCT images (Y axis) at mesial (a), distal (b), buccal (c) and lingual (d) aspects
FIGURE 4.

Bland‐Altman plots representing the average of MBL data (X axis) and the difference in data (Y axis) between histological sections and corresponding CBCT images at (a) mesial, (b) distal, (c) buccal and (d) lingual aspects. Mean (black line), standard deviation (dotted lines) and simple linear regression (red line) of differences
3.2. Cone‐beam computed tomography versus peri‐apical radiographs
Correlations between MBL assessments on PA radiographs and maximum MBL in corresponding CBCT images are illustrated in Figure 5a,b. Pearson correlation coefficients (r) for mesial and distal aspects were 0.92 and 0.94, respectively. Both correlations were statistically significant (p < .05). The mean differences between MBL in PA radiographs and maximum MBL in corresponding CBCT images at mesial and distal aspects were 0.36 ± 0.54 and 0.47 ± 0.51 mm, respectively. A simple linear regression analysis did not reveal any significant trend for differences of MBL assessments over different bone levels (Figure 5c,d).
FIGURE 5.

(a and b) Plots illustrating correlations between maximum MBL from CBCT images (X axis) and MBL‐data obtained from PA radiographs (Y axis) on mesial (a), distal (b) aspects. (c and d) Bland‐Altman plots representing the average of MBL data (X axis) and the difference in data (Y axis) between PA radiographs and maximum MBL in CBCT images at (c) mesial, (d) distal aspects. Mean (black line), standard deviation (dotted lines) and simple linear regression (red line) of differences
3.3. Peri‐apical radiographs versus histology
Correlations between MBL data obtained from measurements on histological sections and corresponding PA radiographs are illustrated in Figure 6a,b. Pearson correlation coefficients (r) for mesial and distal aspects were 0.90 and 0.93, respectively. Both correlations were statistically significant (p < .05). The mean differences in MBL data between histological sections and corresponding PA radiographs at mesial and distal aspects were −0.13 ± 0.58 and −0.28 ± 0.56 mm, respectively. A simple linear regression analysis did not reveal any significant trend for differences of MBL assessments over different bone levels (Figure 6c,d).
FIGURE 6.
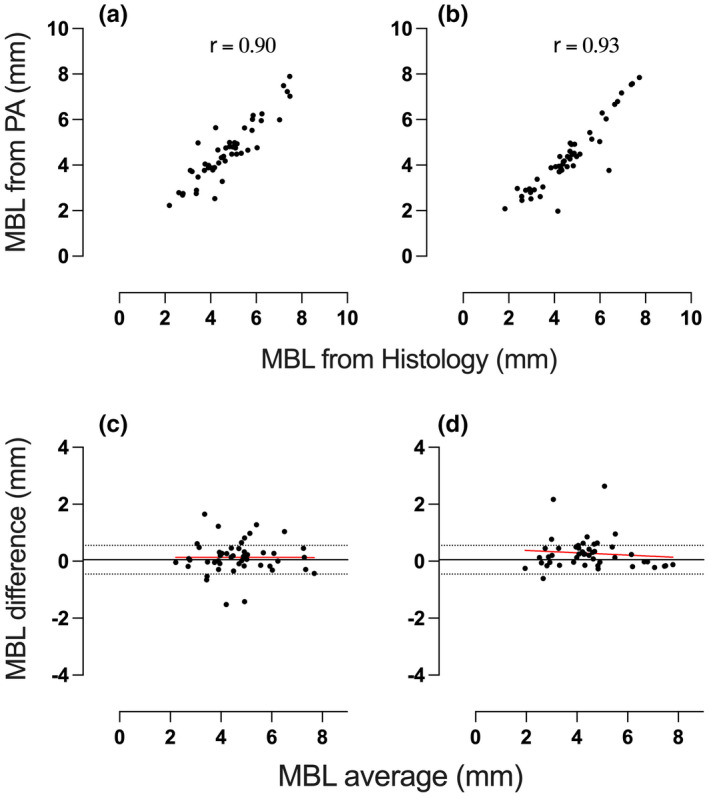
(a and b) Plots illustrating correlations between MBL‐data obtained from histological sections (X axis) and corresponding PA radiographs (Y axis) at mesial (a) and distal (b) aspects. (c and d) Bland‐Altman plots representing the average of MBL data (X axis) and the difference in data (Y axis) between histological sections and corresponding PA radiographs at mesial (c) and distal (d) aspects. Mean (black line), standard deviation (dotted lines) and simple linear regression (red line) of differences
3.4. Cone‐beam computed tomography versus histology according to treatment category
Plots representing the average of MBL data and the difference in data between histological sections and corresponding CBCT images for the different treatment categories are shown in Figure 7. The mean differences between histological data and corresponding CBCT data for treatment categories C, T1, T2 and T3 were −0.31 ± 0.56, −0.13 ± 0.74, −0.06 ± 0.48 and 0.02 ± 0.35), respectively. No statistically significant differences were detected between the two methods.
FIGURE 7.

Bland‐Altman plots representing the average of MBL data (X axis) and the difference in data (Y axis) between histological sections and corresponding CBCT images for Group C (a), Group T1 (b), Group T2 (c), Group T3 (d) sites. Mean (black line), standard deviation (dotted lines) and simple linear regression (red line) of differences
3.5. MBL discrepancy between interproximal and bucco‐lingual sites
The mean MBL discrepancy between interproximal and bucco‐lingual sites assessed on CBCT images was 0.12 ± 0.26 mm. The corresponding discrepancy assessed on histological sections was 0.01 ± 0.01 mm.
4. DISCUSSION
This study evaluated the accuracy of MBL assessments using either CBCT, intra‐oral PA radiographs or histology on samples obtained from a pre‐clinical in‐vivo study on treatment of experimental peri‐implantitis. While significant correlations were observed between the three methods, measurements in PA radiographs consistently resulted in an overestimation of the bone level of about 0.3–0.4 mm. The agreement between methods was not influenced by the use of bone substitute materials in the management of the osseous defects.
Accuracy of bone‐level assessments has been evaluated in previous pre‐clinical in vivo experiments and comparisons between intra‐oral PA radiographs, CBCT and histology were made. The novelty of this study, however, is verified by its design and the target on the healing process following reconstructive surgical therapy of experimental peri‐implantitis. As previous data on comparisons between methods on bone‐level assessments were based on experiments on implants placed in normal bone with or without surrounding osseous defects, the validation of results from this study must be made with care. Nevertheless, the observed significant positive correlation between MBL assessments made on PA radiographs, CBCT images and histological sections in this study, is partly in agreement with data presented in other experimental studies. Corpas et al. (2011) in a study in minipigs reported on a significant correlation between data on MBL around implants obtained from measurements on CBCT, histology and PA radiographs. Similarly, Stokholm et al. (2016) in a study in monkeys found a significant correlation between bone‐level assessments made on radiographs and histological sections. On other hand, Ritter et al. (2014) in an experimental study in dogs on bone levels around implants placed in experimentally produced defects failed to demonstrate a significant correlation between MBL assessments of interproximal sites made on CBCT images, PA radiographs and histological sections. A significant correlation, however, was observed for buccal and lingual sites. In this context, it may be pointed out that the correlation between the different assessment methods in this study was higher than those reported in the studies by Corpas et al. (2011), Ritter et al. (2014) and Stokholm et al. (2016). One reason for the high level of correlation in this study may be the selection of corresponding sections in histology and CBCT as illustrated in Figure 3. It is not clear, however, if corresponding sections or pooled data on MBL were used in the aforementioned studies.
A high correlation between different methods, however, may not be sufficient to indicate the level of accuracy of techniques. Therefore, in this study, the level of agreement between different assessment methods was explored. Bone‐level assessments in PA radiographs consistently resulted in an overestimation of about 0.3–0.4 mm compared to corresponding bone levels on CBCT images. While this finding is in agreement with results presented by Corpas et al. (2011) and Stokholm et al. (2016), contrary data were presented in a clinical methodological study by Raes et al. (2013). They evaluated bone‐level measurements assessed at PA radiographs and CBCT images on 26 implants and reported that the bone levels were overestimated on CBCT images as opposed to those on PA radiographs. The analysis by Raes et al. (2013), however, was based on mean values of pooled MBL assessments from six CBCT images equally distributed around each implant. In this study, however, MBL assessments on PA radiographs were compared with the maximum MBL assessment on corresponding and matching CBCT images. Moreover, as the resolution of the CBCT scanner is important for the accuracy of the image, CBCT scanners with a small voxel size provide images with a higher resolution than scanners with a higher voxel size (Razavi et al., 2010). In this study, the voxel size was 0.08 mm, whereas in the study by Raes et al. (2013), the voxel size was 0.2 mm.
In this study, the agreement between different methods for MBL assessments (CBCT and histology) was explored for experimental peri‐implantitis sites exposed to different surgical reconstructive peri‐implantitis procedures. The analysis revealed that MBL assessments in CBCT or histological sections were not influenced by type of treatment. This finding is in agreement with previous data from an experimental study in dogs by Fienitz et al. (2012). They reported on similar MBL discrepancies between augmented and non‐augmented experimental defect sites in histological sections and corresponding CBCT images. The findings on consistencies of MBL assessments on treated bone defect sites, irrespective of method including bone graft materials or not, are important in the evaluation of clinical studies using radiographs to distinguish differences in outcomes using different augmentation protocols. Clinical studies using a randomized controlled clinical trial design to evaluate the potential benefit of applying a bone graft material in conjunction with reconstructive surgical therapy of peri‐implantitis sites are few and difficulties in distinguishing newly formed bone from graft material may hamper analysis (Heitz‐Mayfield et al., 2018; Tomasi et al., 2019).
A reason for using CBCT in clinical assessments of MBL is to obtain information about the buccal and lingual aspects of bone levels. This information is lacking when using PA radiographs. In this study, data from both CBCT and histological analyses revealed that the discrepancy of MBL between interproximal and bucco‐lingual sites was small (≈0.1 mm). It may therefore be suggested that, under the conditions of this study, bone‐level assessments of interproximal sites using PA radiographs may to a large extent provide a sufficient estimation of the entire circumferential bone level following reconstructive treatment of peri‐implantitis. It is also important to emphasize that different artefacts may influence the accuracy of detecting bone levels using CBCT (Schriber et al., 2020; Schulze et al., 2011). In this study, however, artefacts were few and of small magnitude.
In conclusion, this study demonstrated significant correlations between of MBL assessments obtained from CBCT images, histological sections and PA radiographs. Although MBL assessments obtained from PA radiographs showed an overestimation compared to maximum MBL assessments on corresponding CBCT images and histological sections, PA radiograph can be considered a reliable technique for peri‐implant bone‐level evaluations following reconstructive surgical therapy of experimental peri‐implantitis.
CONFLICT OF INTEREST
Dr. Berglundh reports grants from Swedish Research Council (VR), grants from TUA research funding, Gothenburg, Sweden, non‐financial support from Geistlich Biomaterials, Switzerland, non‐financial support from Dentsply Implants IH AB, Sweden, during the conduct of the study. Grants and Personal fees from Dentsply Implants IH AB, Mölndal, Sweden, outside the submitted work. Dr. Abrahamsson reports non‐financial support from Dentsply Sirona, non‐financial support from Geistlich Pharma AG, during the conduct of the study. Grants from Dentsply Sirona, outside the submitted work. Dr. Almohandes, Dr. Lund, Dr. Carcuac and Dr. Petzold have nothing to disclose.
AUTHOR CONTRIBUTIONS
Ahmed Almohandes: Data curation (equal); Formal analysis (equal); Investigation (equal); Writing – original draft (equal). Henrik Lund: Data curation (equal); Methodology (equal); Writing – original draft (supporting); Writing – review & editing (supporting). Olivier Carcuac: Data curation (equal); Investigation (equal); Methodology (equal); Writing – review & editing (equal). Max Petzold: Formal analysis (equal); Supervision (supporting); Writing – review & editing (supporting). Tord Berglundh: Conceptualization (equal); Methodology (equal); Supervision (equal); Writing – review & editing (equal). Ingemar Abrahamsson: Conceptualization (equal); Investigation (equal); Methodology (equal); Project administration (equal); Supervision (equal); Writing – original draft (equal); Writing – review & editing (equal).
Supporting information
Supplementary Material
Almohandes, A. , Lund, H. , Carcuac, O. , Petzold, M. , Berglundh, T. , & Abrahamsson, I. (2022). Accuracy of bone‐level assessments following reconstructive surgical treatment of experimental peri‐implantitis. Clinical Oral Implants Research, 33, 433–440. 10.1111/clr.13903
DATA AVAILABILITY STATEMENT
All date is available upon request.
REFERENCES
- Albouy, J.‐P. , Abrahamsson, I. , & Berglundh, T. (2012). Spontaneous progression of experimental peri‐implantitis at implants with different surface characteristics: An experimental study in dogs. Journal of Clinical Periodontology, 39(2), 182–187. 10.1111/j.1600-051X.2011.01820.x [DOI] [PubMed] [Google Scholar]
- Albouy, J.‐P. , Abrahamsson, I. , Persson, L. G. , & Berglundh, T. (2008). Spontaneous progression of peri‐implantitis at different types of implants. An experimental study in dogs. I: Clinical and radiographic observations. Clinical Oral Implants Research, 19(10), 997–1002. 10.1111/j.1600-0501.2008.01589.x [DOI] [PubMed] [Google Scholar]
- Albouy, J.‐P. , Abrahamsson, I. , Persson, L. G. , & Berglundh, T. (2011). Implant surface characteristics influence the outcome of treatment of peri‐implantitis: An experimental study in dogs. Journal of Clinical Periodontology, 38(1), 58–64. 10.1111/j.1600-051X.2010.01631.x [DOI] [PubMed] [Google Scholar]
- Almohandes, A. , Carcuac, O. , Abrahamsson, I. , Lund, H. , & Berglundh, T. (2019). Re‐osseointegration following reconstructive surgical therapy of experimental peri‐implantitis. A pre‐clinical in vivo study. Clinical Oral Implants Research, 30(5), 447–456. 10.1111/clr.13430 [DOI] [PubMed] [Google Scholar]
- Bender, P. , Salvi, G. E. , Buser, D. , Sculean, A. , & Bornstein, M. M. (2017). Correlation of three‐dimensional radiologic data with subsequent treatment approach in patients with peri‐implantitis: A retrospective analysis. The International Journal of Periodontics & Restorative Dentistry, 37(4), 481–489. 10.11607/prd.2844 [DOI] [PubMed] [Google Scholar]
- Corpas, L. D. S. , Jacobs, R. , Quirynen, M. , Huang, Y. , Naert, I. , & Duyck, J. (2011). Peri‐implant bone tissue assessment by comparing the outcome of intra‐oral radiograph and cone beam computed tomography analyses to the histological standard. Clinical Oral Implants Research, 22(5), 492–499. 10.1111/j.1600-0501.2010.02029.x [DOI] [PubMed] [Google Scholar]
- Derks, J. , & Tomasi, C. (2015). Peri‐implant health and disease. A systematic review of current epidemiology. Journal of Clinical Periodontology, 42(S16), S158–S171. 10.1111/jcpe.12334 [DOI] [PubMed] [Google Scholar]
- Donath, K. , & Breuner, G. (1982). A method for the study of undecalcified bones and teeth with attached soft tissues: The Säge‐Schliff (sawing and grinding) technique. Journal of Oral Pathology & Medicine, 11(4), 318–326. 10.1111/j.1600-0714.1982.tb00172.x [DOI] [PubMed] [Google Scholar]
- Fienitz, T. , Schwarz, F. , Ritter, L. , Dreiseidler, T. , Becker, J. , & Rothamel, D. (2012). Accuracy of cone beam computed tomography in assessing peri‐implant bone defect regeneration: a histologically controlled study in dogs. Clinical Oral Implants Research, 23(7), 882–887. 10.1111/j.1600-0501.2011.02232.x [DOI] [PubMed] [Google Scholar]
- Heitz‐Mayfield, L. J. , Aaboe, M. , Araujo, M. , Carrión, J. B. , Cavalcanti, R. , Cionca, N. , Cochran, D. , Darby, I. , Funakoshi, E. , Gierthmuehlen, P. C. , Hashim, D. , Jahangiri, L. , Kwon, Y. , Lambert, F. , Layton, D. M. , Lorenzana, E. R. , McKenna, G. , Mombelli, A. , Müller, F. , … Yeo, A. (2018). Group 4 ITI Consensus Report: Risks and biologic complications associated with implant dentistry. Clinical Oral Implants Research, 29, 351–358. 10.1111/clr.13307 [DOI] [PubMed] [Google Scholar]
- Kadesjö, N. , Lynds, R. , Nilsson, M. , & Shi, X.‐Q. (2018). Radiation dose from X‐ray examinations of impacted canines: Cone beam CT vs two‐dimensional imaging. Dentomaxillofacial Radiology, 47(3), 20170305. 10.1259/dmfr.20170305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilkenny, C. , Browne, W. , Cuthill, I. C. , Emerson, M. , & Altman, D. G. (2011). Editorial: Animal research: Reporting in vivo experiments‐The ARRIVE guidelines. Journal of Cerebral Blood Flow and Metabolism, 31(4), 991–993. 10.1038/jcbfm.2010.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monje, A. , Insua, A. , Rakic, M. , Nart, J. , Moyano‐Cuevas, J. L. , & Wang, H.‐L. (2018). Estimation of the diagnostic accuracy of clinical parameters for monitoring peri‐implantitis progression: An experimental canine study. Journal of Periodontology, 89(12), 1442–1451. 10.1002/JPER.18-0081 [DOI] [PubMed] [Google Scholar]
- Persson, L. G. , Araújo, M. G. , Berglundh, T. , Gröndahl, K. , & Lindhe, J. (1999). Resolution of peri‐implantitis following treatment. An experimental study in the dog. Clinical Oral Implants Research, 10(3), 195–203. 10.1034/j.1600-0501.1999.100302.x [DOI] [PubMed] [Google Scholar]
- Raes, F. , Renckens, L. , Aps, J. , Cosyn, J. , & De Bruyn, H. (2013). Reliability of circumferential bone level assessment around single implants in healed ridges and extraction sockets using cone beam CT. Clinical Implant Dentistry and Related Research, 15(5), 661–672. 10.1111/j.1708-8208.2011.00393.x [DOI] [PubMed] [Google Scholar]
- Razavi, T. , Palmer, R. M. , Davies, J. , Wilson, R. , & Palmer, P. J. (2010). Accuracy of measuring the cortical bone thickness adjacent to dental implants using cone beam computed tomography. Clinical Oral Implants Research, 21(7), 718–725. 10.1111/j.1600-0501.2009.01905.x [DOI] [PubMed] [Google Scholar]
- Ritter, L. , Elger, M. C. , Rothamel, D. , Fienitz, T. , Zinser, M. , Schwarz, F. , & Zöller, J. E. (2014). Accuracy of peri‐implant bone evaluation using cone beam CT, digital intra‐oral radiographs and histology. Dentomaxillofacial Radiology, 43(6), 20130088. 10.1259/dmfr.20130088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schriber, M. , Yeung, A. W. K. , Suter, V. G. A. , Buser, D. , Leung, Y. Y. , & Bornstein, M. M. (2020). Cone beam computed tomography artefacts around dental implants with different materials influencing the detection of peri‐implant bone defects. Clinical Oral Implants Research, 31(7), 595–606. 10.1111/clr.13596 [DOI] [PubMed] [Google Scholar]
- Schulze, R. , Heil, U. , Gross, D. , Bruellmann, D. D. , Dranischnikow, E. , Schwanecke, U. , & Schoemer, E. (2011). Artefacts in CBCT: a review. Dento Maxillo Facial Radiology, 40(5), 265–273. 10.1259/dmfr/30642039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, D. , Shujaat, S. , de Faria Vasconcelos, K. , Huang, Y. , Politis, C. , Lambrichts, I. , & Jacobs, R. (2021). Diagnostic accuracy of CBCT versus intraoral imaging for assessment of peri‐implant bone defects. BMC Medical Imaging, 21(1), 23–28. 10.1186/s12880-021-00557-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokholm, R. , Spin‐Neto, R. , Nyengaard, J. R. , & Isidor, F. (2016). Comparison of radiographic and histological assessment of peri‐implant bone around oral implants. Clinical Oral Implants Research, 27(7), 782–786. 10.1111/clr.12683 [DOI] [PubMed] [Google Scholar]
- Tomasi, C. , Regidor, E. , Ortiz‐Vigon, A. , & Derks, J. (2019). Efficacy of reconstructive surgical therapy at peri‐implantitis‐related bone defects. A systematic review and meta‐analysis. Journal of Clinical Periodontology, 46(S21), 340–356. 10.1111/jcpe.13070 [DOI] [PubMed] [Google Scholar]
- Veltri, M. , Ekestubbe, A. , Abrahamsson, I. , & Wennström, J. L. (2016). Three‐dimensional buccal bone anatomy and aesthetic outcome of single dental implants replacing maxillary incisors. Clinical Oral Implants Research, 27(8), 956–963. 10.1111/clr.12664 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
All date is available upon request.


