Abstract
Background:
Previous studies have demonstrated that Hospital at Home (HaH) care is associated with lower costs than traditional hospital care. Most prior studies were small, not U.S.-focused, or did not include post-acute costs in their analyses. Our objective was to determine if combined acute and 30-day post-acute costs of care were lower for HaH patients compared to inpatient comparisons in a Center for Medicare and Medicaid Innovation Center demonstration of HaH.
Methods:
A single-center New York City retrospective observational cohort study of patients admitted to either HaH or inpatient care from Sept 1, 2014 through Aug 31, 2017. Eligible patients were 18 years or older, required inpatient admission, lived in Manhattan, and met home safety requirements. Comparison individuals met the same criteria and were included if they refused HaH care or were admitted when HaH was not available. HaH care was substitutive hospital-level care and 30-days of post-acute transitional care. Main outcomes were costs of care of the acute and post-acute 30-day episodes. We matched subjects on age, sex, and insurance and conducted regression analyses using an unadjusted model followed by one adjusted for several patient characteristics.
Results:
Of 523 Medicare beneficiaries admitted, data were available for 201 patients in the HaH arm and 101 patients receiving usual care. HaH patients were older (81.6 [SD=12.3] yrs. vs 74.6 [SD=14.0], p<0.0001) and more likely to have activities of daily living (ADL) impairments (75.4% vs 46.5%, p<0.0001). Unadjusted mean costs were $5,054 lower for HaH episodes compared to inpatient episodes. Regression analysis with matching showed HaH costs were $5,116 (95% CI −$10,262 to $30, p = 0.05) lower, and when adjusted for age, sex, insurance, diagnosis, and ADL impairments, $5,977 (95% CI −$10,758 to −$1,196) lower.
Conclusions:
Hospital at home combined with 30-day post-acute transition care was less costly than inpatient care.
Keywords: hospital at home, costs of care, high value care
Introduction
Hospital at Home (HaH) provides hospital-level care at home as a substitute for traditional acute inpatient care. Multiple studies demonstrate that, compared with hospital care, HaH generates better or similar clinical outcomes1–10 and greater patient and caregiver satisfaction.3–7, 11–13 Most patients and their families surveyed on HaH have expressed willingness to receive acute care at home in place of the hospital.5, 7, 12, 14–16 Moreover, a growing body of literature suggests that HaH is cost-saving2, 5, 15, 17–27 owing to shorter lengths of stay5, 12, 22, 26 and less healthcare utilization.5, 23 HaH episodes may further lower spending by reducing discharges to skilled nursing facilities (SNFs)2, 12, 24 as well as hospital readmissions.3, 12, 23, 26
Despite these benefits, HaH has not yet been widely scaled in the US since first tested in the late 1990s28, in part due to a lack of sustainable reimbursement mechanisms. A paucity of relevant cost data on HaH may be contributing to policymakers’ hesitancy. Much of the literature on costs of HaH has come from international studies,2, 10, 13, 20–22, 24, 29, 30 whose findings may not be applicable to the US healthcare landscape. US studies have been limited by small sample sizes23 or restriction to treatment of a single or few diagnoses,15, 17 which may compromise generalizability to large scale HaH implementation. Moreover, few studies have examined costs inclusive of the post-acute period,23, 27, 30 in which health systems remain responsible for the care of patients with a variety of discharge diagnoses.
The COVID-19 pandemic has accelerated the demand for alternative care models that can provide acute, inpatient-level care while relieving the strain on traditional “brick and mortar” hospitals. That HaH may be cost-saving only further underscores the current opportunity. The aim of this study was to compare the costs of acute hospital-level care delivered in the home combined with a 30-day post-acute period of care transition services with the costs of inpatient care using data from a Center for Medicare and Medicaid Innovation Center and Hartford foundation demonstration.
Methods
Study Overview and Hospitalization at Home Program
In 2014, the Center for Medicare and Medicaid Innovation (CMMI) of the Centers for Medicare & Medicaid Services awarded a Health Care Innovation Award to the Icahn School of Medicine at Mount Sinai to implement a model of HaH bundled with a post-acute period of home-based transitional care. Upon completion of the CMMI award, the Mount Sinai IRB approved a retrospective analysis of these data with a waiver of informed consent. Primary outcomes of this study demonstrating clinical advantages associated with HaH care were published previously.12
The HaH model was a comprehensive, substitutive hospital service that included daily in-home nurse practitioner or physician visits, daily or twice-daily nursing visits, intravenous line insertion, intravenous infusions, supplemental oxygen, respiratory treatments, laboratory and imaging diagnostics, additional clinician and after-hours paramedic visits as needed, physical therapist evaluations, dedicated social work, and a 24/7 on-call physician. After HaH discharge, patients received post-acute transitional care for a 30-day period; symptoms were monitored via telephone check-ins, patients were scheduled for and reminded about follow-up visits, social work interventions continued, and additional urgent clinician visits were conducted if needed.
Patients and Setting
HaH clinicians engaged patients in the Mount Sinai Health System’s emergency departments (EDs) from September 1, 2014, through August 31, 2017. Recruiters identified patients being admitted and screened them for HaH eligibility. Additionally, patients were referred from outpatient clinics or from home after a clinical encounter during which it was determined that the patient required hospital admission. Patients were eligible for HaH admission if they were 18 years or older, had fee-for-service Medicare or coverage from a single private insurer that contracted with Mount Sinai for HaH services, and required inpatient or observation-level admission. Patients were excluded from HaH care if they were clinically unstable, required cardiac monitoring or intensive care, resided outside of Manhattan, or lived in an unsafe home environment, which included: inadequate home support (existing or new functional deficits without adequate caregiver support); illicit drug use or firearms in the home; lack of electricity, refrigeration, or running water; or active bedbug infestation. Brief interviews to assist with quality assurance and grant reporting requirements were conducted with 73% of subjects who agreed to participate in HaH; survey refusal did not affect participation.
Comparison patients were recruited for purposes of program evaluation if they were offered but refused HaH admission (10%) or were admitted to the hospital at off-hours when a HaH clinician was unavailable (90%), and chart reviews were conducted to confirm that they met the same eligibility and inclusion criteria as HaH patients.
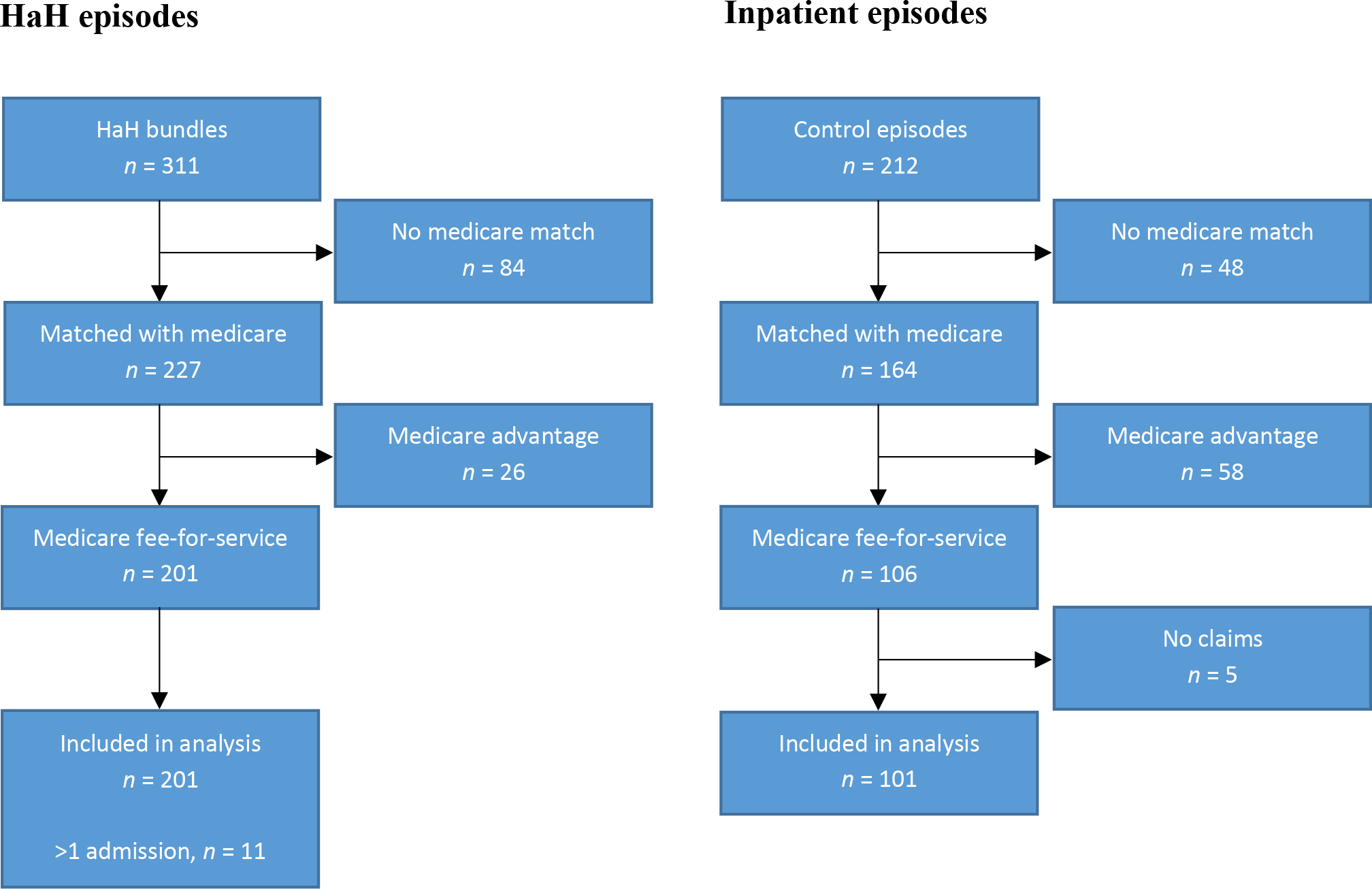
The study sample for this cost analysis was limited to fee-for-service Medicare patients with available claims data (Figure 1). The Icahn School of Medicine at Mount Sinai IRB approved all recruitment and prospective data collection procedures.
Figure 1. Selection of patient population under study.
Measures
HaH Costs
The primary outcome was total costs of care of the acute admission and the 30-day post-acute period. Costs for HaH patients were estimated by combining Medicare billing for the acute and post-acute episode with vendor costs covered by the CMMI award funds and documented in program ledgers. Costs from Medicare Part A and B claims data and vendor invoices were attributable to individual patients; these claims data were used to determine the costs of institutional and professional services during the index ED visit, as well as any home health, hospice, skilled nursing, durable medical equipment, professional services, and any additional inpatient or outpatient care. Vendors were engaged for services not billable to Medicare (see Supplemental Material). These included allied health services, laboratory tests, the transportation of patients, providers, and supplies, durable medical equipment, equipment and supply delivery, medications, and radiology services.
Several grant-funded activities, such as administrative operations, physician visits, care coordination, and provision of certain medical supplies, were paid in aggregate rather than on a per-patient basis. Staffing consisted of the following salaried positions: physicians, nurse practitioners, registered nurses, social workers, physical therapists, administrative assistants, practice manager, medical director, and clinical supervisors. Staffing costs were estimated from the final six months of the program, when the practice reached its highest patient volume; these costs accounted for the percent effort each staff member contributed to the HaH program, fringe benefits, and applicable malpractice insurance. The total cost of administrative staff was divided by the total number of HaH episodes, resulting in an average administrative staffing cost per patient episode. The clinical staff costs were divided by the total number of patient visits to arrive at a per-visit cost, and then multiplied by the visits attributable to an individual patient to arrive at the approximate cost of clinical staff attributable to each patient; the assumption that clinician time and effort – both in direct patient care, and also in travel, administrative tasks, and documentation – would be proportional to the amount of clinical care received.
Comparison Costs
The costs of care for comparison patients were calculated entirely from the Medicare Part A and B claims for the hospital admission (inclusive of the index ED encounter) and the 30 days following discharge from the hospital.
Patient Characteristics
Patient demographics and baseline characteristics including age, race and ethnicity, admission diagnosis, and insurance provider were abstracted from the electronic medical record or administrative records, while education, ADL impairment, and self-rated health were obtained from patient surveys. Diagnoses were determined by a trained medical coder who reviewed the electronic medical record.
Data Analysis
To account for observable differences among HaH patients and comparisons that could be associated with expenditures, we used coarsened exact matching (CEM).31 Matching was based on the following variables: age (dichotomized at 85+ to preserve sample), sex, and Medicaid status. Using CEM, we were able to match all observations in the sample using a one-to-many match. Regression analyses were conducted with both the matched and unmatched sample, and we also compared bivariate statistics using t-tests and chi-squared analyses on the unmatched sample and found results did not differ substantially. Because of skewed cost data, we used a generalized linear model (GLM) with log link and gamma distribution, a common approach for modelling health expenditures.32 All regressions used cluster robust standard errors to account for the 11 patients with more than one episode of care.
Within our matched sample, we first ran an unadjusted model followed by a model adjusted for age, sex, race/ethnicity, Medicaid status, diagnosis category, education, ADL impairment, and self-rated health. Data on education, self-rated health, and or ADL impairment were missing for 24% of episodes of care (6% of controls and 32% of HaH patients). We performed several sensitivity analyses to test the robustness of our primary modeling strategy. First, we added diagnosis category (exacerbation vs. infection, other diagnosis vs. infection) and ADL impairment to the CEM and then ran the adjusted GLM regression on the subset of our sample with non-missing diagnosis and ADL data (n = 219). Second, we imputed missing data using Multivariate Imputation using Chained Equations (MICE) and repeated the first sensitivity analysis (n= 286). Third, because Mount Sinai Hospital receives disproportionate share hospital (DSH) and indirect medical education (IME) payments from Medicare, we also performed sensitivity analyses that discounted the savings from our primary analyses by the combined DSH and IME rates (26.09% and 38.73%, respectively). Finally, we performed analyses on the data excluding control patients who refused the HaH intervention, as those patients may have had other, unobserved differences from the rest of the control group. All analyses were performed using SAS version 9.4 (Cary, NC) or Stata 16 (College Station, TX).
Results
There were 311 episodes of HaH and 212 comparison inpatient hospitalizations (Figure 1). Eighty-four (27%) HaH and 48 (23%) comparison episodes could not be matched with Medicare data because they had other insurance or their identifiers were not on file. Another twenty-six (8%) HaH episodes and 58 (27%) inpatient episodes were excluded from analysis because these patients did not have fee-for-service Medicare at the time of participation. An additional 5 (2%) comparison episodes were excluded because no Medicare claims could be identified. The final analysis included 201 HaH episodes and 101 inpatient episodes. Eleven patients were admitted to HaH more than once.
HaH episode patients were older (81.6 [12.3] years vs. 74.6 [14.0] years, p<0.0001) than patients in the comparison group (Table 1), but there were no significant differences in terms of sex, race or ethnicity, or education level. Patients dually eligible for Medicaid and Medicare comprised 96 (47.8%) of the HaH episodes and 43 (42.6%) of the comparison episodes. HaH patients were more likely to have ADL impairments (75.4% vs. 46.5%, p<0.0001). Patients in both groups were admitted with varied diagnoses, including infections, exacerbations of congestive heart failure (CHF), chronic obstruction pulmonary disease (COPD), and asthma, as well as deep vein thrombosis, pulmonary embolism, and hyperglycemia. HaH patients were more likely to have a diagnosis of dehydration than patients in the comparison group (14.9% vs 3.0%, p=0.001).
Table 1.
Episode patient characteristics
| All Episodes | Inpatient Episodes | Hospital at Home Episodes | P | |
|---|---|---|---|---|
| 302 | 101 | 201 | ||
| Age, years mean (sd) | 79.2 (13.3) | 74.6 (14.0) | 81.6 (12.3) | <0.0001 |
| Age, categorical | 0.005 | |||
| <65 years | 37 (12.3) | 18 (17.8) | 19 (9.5) | |
| 65–74 years | 59 (19.5) | 26 (25.7) | 33 (16.4) | |
| 75–84 years | 81 (26.8) | 28 (27.7) | 53 (26.4) | |
| ≥85 years | 125 (41.4) | 29 (28.7) | 96 (47.8) | |
| Female | 211 (69.9) | 66 (65.3) | 145 (72.1) | 0.23 |
| Race and ethnicity | 0.92 | |||
| Non-Hispanic White | 197 (65.2) | 66 (65.3) | 131 (65.2) | |
| Non-Hispanic Black | 54 (17.9) | 17 (16.8) | 37 (18.4) | |
| Hispanic | 51 (16.9) | 18 (17.8) | 33 (16.4) | |
| Highest education * | 0.75 | |||
| ≤8th grade | 42 (17.6) | 15 (15.8) | 27 (18.9) | |
| Any high school | 64 (26.9) | 26 (27.4) | 38 (26.6) | |
| Any college | 67 (28.2) | 30 (31.6) | 37 (25.9) | |
| More than four-year college degree | 65 (27.3) | 24 (25.3) | 41 (28.7) | |
| Dually eligible for Medicaid | 139 (46.0) | 43 (42.6) | 96 (47.8) | 0.39 |
| Any ADL impairment * | 153 (63.5) | 46 (46.5) | 107 (75.4) | <0.0001 |
| Poor self-rated health * | 159 (64.4) | 66 (66.7) | 93 (62.8) | 0.54 |
| Admitting diagnosis | 0.001 | |||
| Pneumonia | 64 (21.2) | 21 (20.8) | 43 (21.4) | |
| Urinary tract infection | 67 (22.2) | 17 (16.8) | 50 (24.9) | |
| Cellulitis | 50 (16.6) | 27 (26.7) | 23 (11.4) | |
| Diverticulitis | 5 (1.7) | 0 | 5 (2.5) | |
| COPD exacerbation | 15 (5.0) | 6 (5.9) | 9 (4.5) | |
| Asthma exacerbation | 14 (4.6) | 7 (6.9) | 7 (3.5) | |
| CHF exacerbation | 33 (10.9) | 12 (11.9) | 21 (10.4) | |
| Hyperglycemia | 3 (1.0) | 1 (1.0) | 2 (1.0) | |
| Hypertension | 1 (0.3) | 1 (1.0) | 0 | |
| Deep venous thrombosis | 5 (1.7) | 3(3.0) | 2 (1.0) | |
| Pulmonary embolism | 3 (1.0) | 2 (2.0) | 1 (0.5) | |
| Dehydration | 33 (10.9) | 3 (3.0) | 30 (14.9) | |
| Other | 9 (3.0) | 1 (1.0) | 8 (4.0) |
N=70, 24% of sample were missing ADL information (61), education (64), or self-rated health (55).
ADL, activities of daily living; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure.
Total and Per Service Costs
Mean unadjusted total costs of the acute hospitalization plus the 30-day post-acute period were $17,937 [$12,041] for HaH episodes vs. $22,991 [25,423] for inpatient episodes of care (Table 2). The bulk of the cost savings occurred during the acute phase, during which the mean cost of hospitalization for HaH patients was $9,843 [$5,057] vs. $14,323 [$6,572] for comparison patients. The most costly components of acute HaH, after charges related to ED visits, were personnel (clinical and administrative), transportation, and medications. In the post-acute phase, mean costs were slightly lower for HaH ($8,094 [$10,644]) than post-inpatient care ($8,668 [$23,939]). Sources of these post-acute costs differed; inpatient and SNF costs were higher for the comparison group than the HaH group ($3,681 [$21,293] vs. $2,694 [7,963] and $1,985 [$6,051] vs. $357 [$2,563], respectively), while skilled home health costs were lower in the comparison group ($982 [$1,691] vs. $1,217 [$1,873]).
Table 2.
Mean Cost (US$) per Patient Episode of Hospital at Home versus Inpatient Care
| Hospital at Home n=201 | Inpatient n=101 | |||
|---|---|---|---|---|
| Acute | Post-Acute | Acute | Post-Acute | |
| Costs from Medicare claims | ||||
| Index ED visit | 779 (984) | |||
| Inpatient | 318 (2,306) | 2,694 (7,963) | 13,235* (6,106) | 3,681 (21,293) |
| Outpatient | 113 (338) | 268 (851) | 58 (281) | 393 (1,211) |
| Home health | 14 (198) | 1,217 (1,873) | 30 (306) | 982 (1,691) |
| Hospice | 0 (0) | 357 (1,606) | 0 (0) | 275 (1,496) |
| Skilled nursing facility | 0 (0) | 357 (2,563) | 0 (0) | 1,985 (6,051) |
| Durable medical equipment | 16 (74) | 94 (605) | 2 (8) | 282 (2,218) |
| Professional services | 141 (190) | 838 (1,335) | 997 (760) | 1,070 (1,530) |
| Medicare claims subtotal | 1,380 (2619) | 5,825 (10,511) | 14,323 (6,572) | 8,668 (23,939) |
| HaH vendor-invoiced costs | ||||
| Transportation | 274 (160) | 24 (40) | ||
| Rehabilitative therapy | 18 (93) | 10 (145) | ||
| Infusion | 82 (255) | 13 (104) | ||
| Home health | 32 (184) | 31 (142) | ||
| Laboratory and diagnostics | 64 (103) | 37 (110) | ||
| Medications | 66 (168) | 3 (42) | ||
| Durable medical equipment | 37 (99) | 7 (64) | ||
| HaH operational costs | ||||
| Personnel | ||||
| Physician, nurse practitioner | 3,457 (2,091) | 937 (1,450) | ||
| Registered nurse | 2,694 (1,629) | 640 (990) | ||
| Social worker | 567 (343) | 207 (319) | ||
| Physical therapist | 63 (38) | 14 (22) | ||
| Administrative personnel | 802 (0) | 344 (0) | ||
| Non-Personnel | ||||
| Medical supplies | 86 (79) | |||
| Medications | 166 (168) | |||
| Administrative | 54 (16) | |||
| Subtotal | 9,843 (5,057) | 8,094 (10,644) | 14,323 (6,572) | 8,668 (23,939) |
| Total | 17,937 (12,041) Median (IQR): 14,221 (10,244 – 20,275) | 22,991 (25,423) Median (IQR): 16,996 (12,903 – 25,190) | ||
Mean costs are in US dollars from 2014 to 2017 not adjusted for inflation, and are per patient over the entire phase.
Inpatient costs for comparison patients include the index ED visit.
Comparison of Overall Costs, HaH vs. Inpatient Care
In the matched unadjusted analysis, average costs for the acute episode of care plus 30-day post-acute period were lower for HaH vs. inpatient episodes of care, −$5,116 (95% confidence interval −$10,262 to $30, p=0.05) (Table 3). After adjusting for age, sex, race/ethnicity, insurance, diagnosis, education, ADL impairment, and self-rated health, HaH costs remained lower (−$5,977 [95% CI −$10,758 to −$1,196], p=0.01). These results were consistent in the sensitivity analyses. HaH episodes were lower cost than inpatient episodes when the matching included data on physical impairment and admission diagnosis (adjusted difference in costs, −$6,320 [95% CI −$11,881 to −$760], p=0.03) as well as when missing data were imputed (adjusted difference in costs, −$5,555 [95% CI −$11,039 to −$71], p=0.05). Results for each sensitivity analysis showed these differences in cost and the magnitudes were similar to the primary analysis. Cost savings remained substantial though expectedly reduced after discounting the Medicare DSH and IME payment rate for Mount Sinai Hospital (Table 3), and the differences remained statistically significant.
Discussion
In this multi-year demonstration of HaH, costs of acute care and the 30-day post-acute period were significantly and meaningfully lower than for a matched group of patients who received inpatient care, and were robust to several sensitivity analyses. While these findings are consistent with prior research,1, 2, 5, 10, 15, 17, 20–25, 30, 33 this study makes a unique contribution because the estimates included care-related costs during the 30-day post-acute period.
Costs during the acute period of care were markedly lower for HaH than the inpatient hospital episodes. This may be due to shorter length of stay of the HaH patients in this study, which is consistent with prior demonstrations.5, 9, 12, 22 While not tabulated here in a direct comparison, HaH care also tends to involve less use of healthcare services including laboratory tests and specialty consultations.5, 23 In the post-acute period, HaH realized savings through lower inpatient costs (i.e., a trend towards fewer readmissions)12 and fewer skilled nursing facility (SNF) admissions (see Supplemental Material). However, a trend towards greater use of skilled home health nursing by HaH patients somewhat offset these gains. It is noteworthy that HaH patients were more likely to have impairments of ADLs at the time of admission, yet were less likely to have a SNF admission. These findings and those of other studies suggest that HaH care enables patients to remain at home following an acute hospitalization.2, 12, 24, 25
Findings of our cost estimates for HaH point to potential targets for reducing costs of care in HaH delivery. Given that clinician time and travel were among the greater costs incurred for HaH in this study, replacement of some in-person visits with telemedicine encounters could substantially reduce per-patient costs and increase program capacity; the widespread and successful use of telemedicine during the COVID-19 pandemic34 strongly suggests the feasibility of such a strategy. Additionally, implementing flexible nursing protocols that allow for modulating the frequency of nurse visits based on patient stability, as well as employing advanced practice providers working at the top of their licenses as frontline providers, might also achieve greater efficiency in care delivery and reduce costs.
The safety, efficacy, and cost-savings of HaH are increasingly relevant in the setting of the COVID-19 pandemic given increasing patient preference for home-based treatment35 and limited bed availability in hospitals during surges in COVID-19 infection rates.36 Multiple institutions have demonstrated that some patients with COVID-19 who require hospitalization can be treated safely at home.37, 38 In response to the overcrowding of hospitals because of the COVID-19 pandemic, the Centers for Medicare & Medicaid Services announced a waiver in November 2020, which, for the duration of the ongoing public health emergency, allows eligible hospital systems to be reimbursed a full hospital diagnosis-related group (DRG) for HaH care.39 Before, there was a gulf between existing billing mechanism reimbursements for HaH under pre-waiver rules and the actual cost of delivering acute hospital-level care in the home.40 As of this writing, 90 healthcare systems in 34 states have been approved to implement HaH programs under this waiver,41 demonstrating that adequate reimbursement is a critical driver of HaH adoption.
There are important limitations to this study. We emphasize that this is an analysis of a single program, in its early phases of implementation, in which inefficiencies and steep learning curves were unavoidable, and may not be reflective of the costs of a more mature, stable operations phase. Medicare estimates in this analysis were significantly higher than in an actuarial analysis commissioned for a proposal recommending implementation of a payment mechanism for HaH that was submitted to the Physicians Technical Advisory Council of the Office of the Assistant Secretary for Planning and Evaluation of the Department of Health and Human Services in 2017.42 Differences in these estimates may be attributable to Mount Sinai Hospital’s Medicare Disproportionate Share Hospital (DSH) and Indirect Medical Education (IME) rates, which inflate Medicare payments by 68%. While we still observed statistically significant savings for HaH when discounting these rates, these results may not generalize to hospitals that do not receive DSH and IME-adjusted Medicare payments. Other elements of the 2017 analysis, for example staffing cost estimates that drew on national benchmarks from the U.S. Bureau of Labor Statistics, likely contributed to somewhat lower estimates of HaH program implementation costs, whereas actual costs were higher.
Our analyses have some limitations. Cost data were available for a subset of the original sample, which may have introduced bias in our results. We estimated HaH costs from per-person and practice-level expenditures, rather than entirely on Medicare billing since the program was mostly funded by a CMMI contract. This could reduce between-patient cost variation relative to that for HaH if it were supported entirely by insurance billing. We estimated cost during a period in time in which the program had achieved a steady patient census; per-person costs would be higher prior to this time. Our program had the ability to directly admit patients at home to HaH, bypassing the emergency department; costs of care would be higher for HaH programs that are not able to do so. Our analyses did not consider costs borne by patients and caregivers in HaH during the episode of care, such as food, labor, co-pays, and lost wages. Such costs could be substantial and are worthy of future evaluation.
In a single site study, HaH combined with 30-day post-acute, home-based transitional care achieved substantial savings compared to inpatient care. Pathways to cost savings may vary depending on where and how a given HaH program is implemented, but these findings add to the growing body of evidence that substituting inpatient care with HaH may reduce healthcare costs while producing good clinical outcomes and high patient satisfaction. The COVID-19 pandemic brings renewed urgency to moving HaH into the mainstream of acute healthcare delivery in the US.
Supplementary Material
Figure 2. Distribution of differences in costs (US$) of care between hospital at home and matched inpatient comparison group patients inclusive of the 30-day post-acute period.
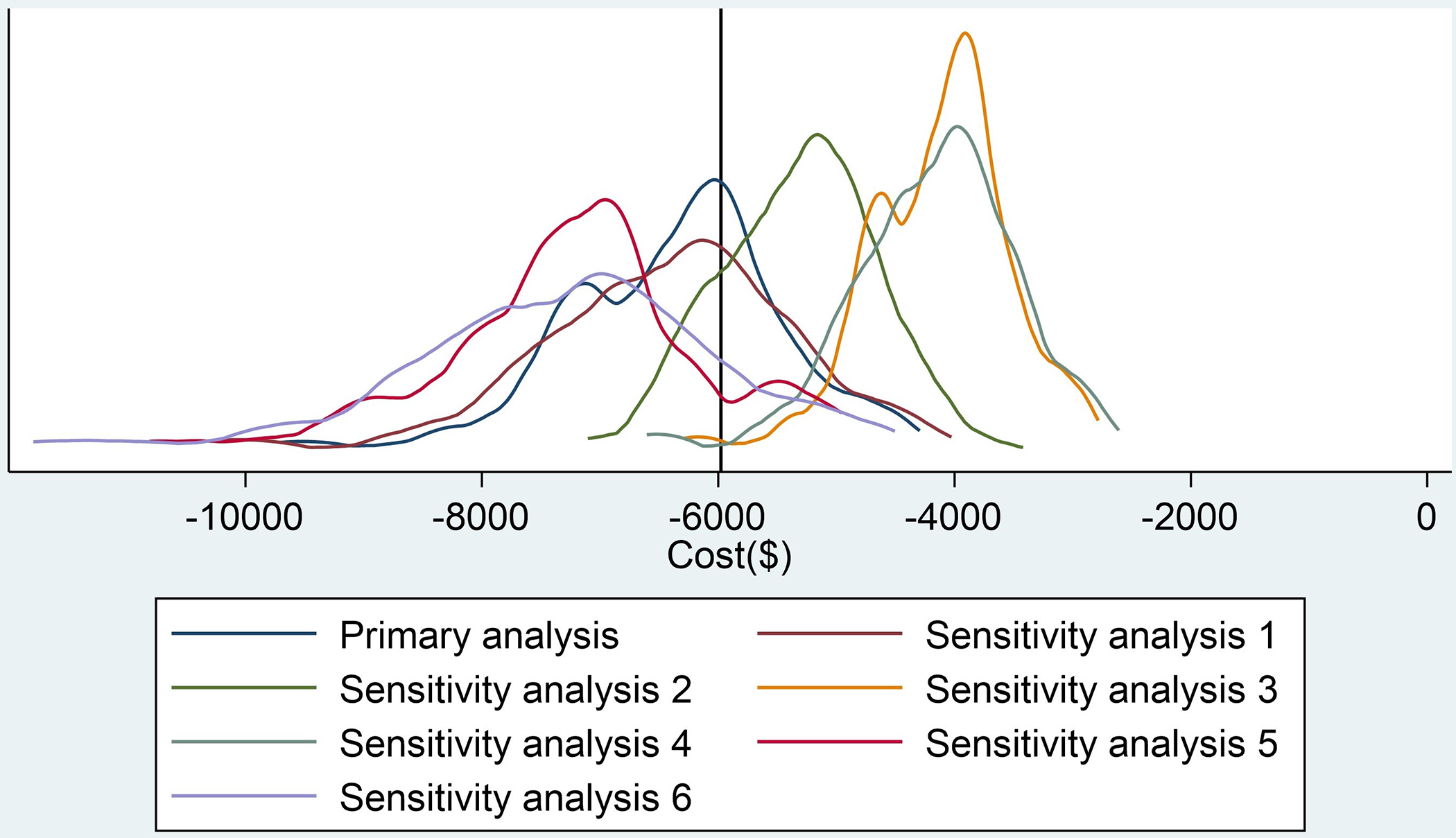
Primary Analysis: Coarsened Exact Matching (CEM) on age (dichotomized at ≥85 years), sex, and Medicaid status
Sensitivity Analysis 1: CEM on age, sex, Medicaid status, diagnosis, and ADL impairment
Sensitivity Analysis 2: CEM on age, sex, Medicaid status, diagnosis, and ADL impairment, with imputation of missing data
Sensitivity Analysis 3: CEM on age, sex, and Medicaid status, final costs discounted by Medicare disproportionate share hospital (DSH) and indirect medical education (IME) payment rates for Mount Sinai Hospital
Sensitivity Analysis 4: CEM on age, sex, Medicaid status, diagnosis, and ADL impairment, discounted for Medicare DSH and IME payment rates
Sensitivity Analysis 5: CEM on age, sex, and Medicaid status, excluding controls who refused HaH enrollment
Sensitivity Analysis 6: CEM on age, sex, Medicaid status, diagnosis, and ADL impairment, excluding controls who refused HaH enrollment
Key Points:
In a large-scale demonstration of Hospitalization at Home (HaH) inclusive of a 30-day post-acute period, HaH care cost several thousand dollars less compared to inpatient care.
Lower cost of HaH care persisted after adjusting for patient characteristics and across several sensitivity analyses.
Why does this matter?
HaH care may save costs as well as relieve strain on hospitals and healthcare systems.
Acknowledgements:
Sponsor’s Role: The HaH clinical project described was supported by grant No. 1C1CMS331334 from the US Department of Health and Human Services, Centers for Medicare & Medicaid Services. Research reported in this publication was supported by the US Department of Health and Human Services, Centers for Medicare & Medicaid Services (1C1CMS331334-01-00), the National Institute on Aging, Claude D. Pepper Older Americans Independence Center (TS, 3P30AG028741), and The John A. Hartford Foundation. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication
Footnotes
Conflicts of Interest: Dr. Leff serves as an advisor to Medically Home, Dispatch Health, and the Chartis Group. These arrangements are managed in accord with conflicts of interest requirements of the Johns Hopkins University School of Medicine.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- 1.Leff B, Burton L, Mader SL, et al. Comparison of functional outcomes associated with hospital at home care and traditional acute hospital care. Journal of the American Geriatrics Society. Feb 2009;57(2):273–8. doi: 10.1111/j.1532-5415.2008.02103.x [DOI] [PubMed] [Google Scholar]
- 2.Aimonino Ricauda N, Tibaldi V, Leff B, et al. Substitutive “hospital at home” versus inpatient care for elderly patients with exacerbations of chronic obstructive pulmonary disease: a prospective randomized, controlled trial. Journal of the American Geriatrics Society. Mar 2008;56(3):493–500. doi: 10.1111/j.1532-5415.2007.01562.x [DOI] [PubMed] [Google Scholar]
- 3.Summerfelt WT, Sulo S, Robinson A, Chess D, Catanzano K. Scalable hospital at home with virtual physician visits: pilot study. Am J Manag Care. Oct 2015;21(10):675–84. [PubMed] [Google Scholar]
- 4.Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative Strategies to Inpatient Hospitalization for Acute Medical Conditions: A Systematic Review. JAMA Intern Med. Nov 1 2016;176(11):1693–1702. doi: 10.1001/jamainternmed.2016.5974 [DOI] [PubMed] [Google Scholar]
- 5.Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood). Jun 2012;31(6):1237–43. doi: 10.1377/hlthaff.2011.1132 [DOI] [PubMed] [Google Scholar]
- 6.Corwin P, Toop L, McGeoch G, et al. Randomised controlled trial of intravenous antibiotic treatment for cellulitis at home compared with hospital. BMJ (Clinical research ed). 2005;330(7483):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris R, Ashton T, Broad J, Connolly G, Richmond D. The effectiveness, acceptability and costs of a hospital-at-home service compared with acute hospital care: a randomized controlled trial. Journal of health services research & policy. Jul 2005;10(3):158–66. doi: 10.1258/1355819054338988 [DOI] [PubMed] [Google Scholar]
- 8.Ricauda NA, Bo M, Molaschi M, et al. Home hospitalization service for acute uncomplicated first ischemic stroke in elderly patients: a randomized trial. Journal of the American Geriatrics Society. Feb 2004;52(2):278–83. doi: 10.1111/j.1532-5415.2004.52069.x [DOI] [PubMed] [Google Scholar]
- 9.Wilson A, Parker H, Wynn A, et al. Randomised controlled trial of effectiveness of Leicester hospital at home scheme compared with hospital care. BMJ (Clinical research ed). Dec 11 1999;319(7224):1542–6. doi: 10.1136/bmj.319.7224.1542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vianello A, Savoia F, Pipitone E, et al. “Hospital at home” for neuromuscular disease patients with respiratory tract infection: a pilot study. Respiratory care. Dec 2013;58(12):2061–8. doi: 10.4187/respcare.02501 [DOI] [PubMed] [Google Scholar]
- 11.Leff B, Burton L, Mader S, et al. Satisfaction with hospital at home care. Journal of the American Geriatrics Society. Sep 2006;54(9):1355–63. doi: 10.1111/j.1532-5415.2006.00855.x [DOI] [PubMed] [Google Scholar]
- 12.Federman AD, Soones T, DeCherrie LV, Leff B, Siu AL. Association of a Bundled Hospital-at-Home and 30-Day Postacute Transitional Care Program With Clinical Outcomes and Patient Experiences. JAMA Intern Med. Jun 25 2018;doi: 10.1001/jamainternmed.2018.2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caplan GA, Ward JA, Brennan NJ, Coconis J, Board N, Brown A. Hospital in the home: a randomised controlled trial. The Medical journal of Australia. Feb 15 1999;170(4):156–60. [PubMed] [Google Scholar]
- 14.Jimenez S, Aguilo S, Gil V, et al. [Psychosocial factors determine patients’ acceptance of emergency department discharge directly to hospital-at-home care]. Gac Sanit. Jul-Aug 2010;24(4):303–8. Los factores psicosociales determinan la aceptacion de la hospitalizacion a domicilio directamente desde el servicio de urgencias. doi: 10.1016/j.gaceta.2010.03.012 [DOI] [PubMed] [Google Scholar]
- 15.Leff B, Burton L, Mader SL, et al. Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Annals of internal medicine. Dec 6 2005;143(11):798–808. [DOI] [PubMed] [Google Scholar]
- 16.Saenger P, Federman AD, DeCherrie LV, et al. Choosing Inpatient vs Home Treatment: Why Patients Accept or Decline Hospital at Home. Journal of the American Geriatrics Society. Jul 2020;68(7):1579–1583. doi: 10.1111/jgs.16486 [DOI] [PubMed] [Google Scholar]
- 17.Frick KD, Burton LC, Clark R, et al. Substitutive Hospital at Home for older persons: effects on costs. Am J Manag Care. Jan 2009;15(1):49–56. [PubMed] [Google Scholar]
- 18.Ram FS, Wedzicha JA, Wright J, Greenstone M. Hospital at home for patients with acute exacerbations of chronic obstructive pulmonary disease: systematic review of evidence. BMJ (Clinical research ed). 2004;329(7461):315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shepperd S, Doll H, Angus RM, et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. Cmaj. Jan 20 2009;180(2):175–82. doi: 10.1503/cmaj.081491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skwarska E, Cohen G, Skwarski KM, et al. Randomized controlled trial of supported discharge in patients with exacerbations of chronic obstructive pulmonary disease. Thorax. 2000/11// 2000;55(11):907–912. doi: 10.1136/thorax.55.11.907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Board N, Brennan N, Caplan GA. A randomised controlled trial of the costs of hospital as compared with hospital in the home for acute medical patients. Australian and New Zealand journal of public health. Jun 2000;24(3):305–11. doi: 10.1111/j.1467-842x.2000.tb01573.x [DOI] [PubMed] [Google Scholar]
- 22.Hernandez C, Casas A, Escarrabill J, et al. Home hospitalisation of exacerbated chronic obstructive pulmonary disease patients. The European respiratory journal. Jan 2003;21(1):58–67. doi: 10.1183/09031936.03.00015603 [DOI] [PubMed] [Google Scholar]
- 23.Levine DM, Ouchi K, Blanchfield B, et al. Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Annals of internal medicine. Jan 21 2020;172(2):77–85. doi: 10.7326/m19-0600 [DOI] [PubMed] [Google Scholar]
- 24.Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Archives of internal medicine. Sep 28 2009;169(17):1569–75. doi: 10.1001/archinternmed.2009.267 [DOI] [PubMed] [Google Scholar]
- 25.Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs Medical Center Hospital-in-Home Program. Journal of the American Geriatrics Society. Jul 2018;66(7):1392–1398. doi: 10.1111/jgs.15382 [DOI] [PubMed] [Google Scholar]
- 26.Mooney K, Titchener K, Haaland B, et al. Evaluation of Oncology Hospital at Home: Unplanned Health Care Utilization and Costs in the Huntsman at Home Real-World Trial. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. May 17 2021:Jco2003609. doi: 10.1200/jco.20.03609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cai S, Intrator O, Chan C, et al. Association of Costs and Days at Home With Transfer Hospital in Home. JAMA Network Open. 2021;4(6):e2114920–e2114920. doi: 10.1001/jamanetworkopen.2021.14920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leff B, Burton L, Guido S, Greenough WB, Steinwachs D, Burton JR. Home hospital program: a pilot study. Journal of the American Geriatrics Society. Jun 1999;47(6):697–702. [DOI] [PubMed] [Google Scholar]
- 29.Nicholson C, Bowler S, Jackson C, Schollay D, Tweeddale M, O’Rourke P. Cost comparison of hospital- and home-based treatment models for acute chronic obstructive pulmonary disease. Aust Health Rev. 2001 2001;24(4):181–187. doi: 10.1071/ah010181 [DOI] [PubMed] [Google Scholar]
- 30.Campbell H, Karnon J, Dowie R. Cost analysis of a hospital-at-home initiative using discrete event simulation. Journal of health services research & policy. Jan 2001;6(1):14–22. doi: 10.1258/1355819011927152 [DOI] [PubMed] [Google Scholar]
- 31.Iacus SM, King G, Porro G. Causal inference without balance checking: Coarsened exact matching. Political analysis. 2012:1–24. [Google Scholar]
- 32.Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health economics. Aug 2011;20(8):897–916. doi: 10.1002/hec.1653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of “hospital in the home”. The Medical journal of Australia. Nov 5 2012;197(9):512–9. [DOI] [PubMed] [Google Scholar]
- 34.Abelson R. Doctors and Patients Turn to Telemedicine in the Coronavirus Outbreak. New York Times. Accessed 10/21/2020. https://www.nytimes.com/2020/03/11/health/telemedicine-coronavirus.html
- 35.Johnson LA. Pandemic pushes expansion of ‘hospital-at-home’ treatment. News. AP. Updated 8/20/2020. Accessed 10/21/2020, 2020. https://apnews.com/article/37d72aeda92f3964f52c263eb8cd9fee
- 36.Hick JL, Biddinger PD. Novel Coronavirus and Old Lessons — Preparing the Health System for the Pandemic. New England Journal of Medicine. 2020;382(20):e55. doi: 10.1056/NEJMp2005118 [DOI] [PubMed] [Google Scholar]
- 37.Heller DJ, Ornstein KA, DeCherrie LV, et al. Adapting a Hospital-at-Home Care Model to Respond to New York City’s COVID-19 Crisis. Journal of the American Geriatrics Society. Jul 7 2020;doi: 10.1111/jgs.16725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sitammagari K, Murphy S, Kowalkowski M, et al. Insights From Rapid Deployment of a “Virtual Hospital” as Standard Care During the COVID-19 Pandemic. Annals of internal medicine. Nov 11 2020;doi: 10.7326/m20-4076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 11/25/2020, 2020. Accessed 12/4/2020. https://www.cms.gov/newsroom/press-releases/cms-announces-comprehensive-strategy-enhance-hospital-capacity-amid-covid-19-surge
- 40.DeCherrie LV, Wardlow L, Ornstein KA, et al. Hospital at Home services: An inventory of fee-for-service payments to inform Medicare reimbursement. Journal of the American Geriatrics Society. Apr 2 2021;doi: 10.1111/jgs.17140 [DOI] [PubMed] [Google Scholar]
- 41.Approved Facilities/Systems for Acute Hospital Care at Home. 9/7/2021, Accessed 9/7/2021, 2021. https://qualitynet.cms.gov/acute-hospital-care-at-home/resources
- 42.“HaH Plus” (Hospital at Home Plus) Provider-Focused Payment Model. 2017;
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


