Abstract
Purpose
Electronic patient-reported outcomes (ePROs) are increasingly being used for symptom monitoring during routine cancer care, but have rarely been evaluated in diverse patient populations. We assessed ePRO user experiences and perceived value among Black and White cancer patients.
Methods
We recruited 30 Black and 49 White bladder and prostate cancer patients from a single institution. Participants reported symptoms using either a web-based or automated telephone interface over 3 months and completed satisfaction surveys and qualitative interviews focused on user experiences and value. Using a narrative mixed methods approach, we evaluated overall and race-specific differences in ePRO user experiences and perceived value.
Results
Most participants selected the web-based system, but Blacks were more likely to use the automated telephone-based system than Whites. In satisfaction surveys, Whites more commonly reported ease in understanding and reporting symptoms compared with Blacks. Blacks more often reported that the ePRO system was helpful in facilitating symptom-related discussions with clinicians. During interviews, Blacks described how the ePRO helped them recognize symptoms, while Whites found value in better understanding and tracking symptoms longitudinally. Blacks also expressed preferences for paper-based ePRO options due to perceived ease in better understanding of symptom items.
Conclusion
Electronic patient-reported outcomes are perceived as valuable for variable reasons by Black and White cancer populations, with greater perceived value for communicating with clinicians reported among Blacks. To optimize equitable uptake of ePROs, oncology practices should offer several ePRO options (e.g., web-based, phone-based), as well as paper-based options, and consider the e-health literacy needs of patients during implementation.
Keywords: Electronic patient-reported outcomes, Symptom monitoring, Cancer, Patient-provider communication
Background
Cancer patients experience a range of treatment-related symptoms, with Black patients reporting worse symptom burden than Whites [1–5]. Racial disparities in symptom burden have implications for inequities in health-related quality of life, treatment adherence, and survival. Symptom monitoring is a critical component of symptom management [6–8]; however, prior studies have documented bias in symptom assessment and monitoring, including providers underestimating and under-evaluating symptom burden in Black patients relative to Whites [9, 10]. Thus, strategies that routinize symptom monitoring may help mitigate inequities in symptom burden.
Existing research suggests that the integration of electronic patient-reported outcomes (ePROs) into routine oncology care is feasible and can help improve symptom management by facilitating symptom monitoring longitudinally, alerting clinicians to patients experiencing severe/worsening symptoms [6, 11, 12], engaging patients in symptom recognition [12, 13], and fostering patient-provider communication regarding symptoms [13, 14]. Yet, prior ePRO studies (have typically been carried out in homogenous populations of predominantly White, highly educated patients [6, 11, 14, 15], which limits generalizability to patients of color who, on average, report higher symptom burden [16], less education [17–19], and more barriers to care [20–23].
Past research suggests that adoption of health information technologies (e.g., mobile health applications, patient portals) varies along social gradients such as race, income, and education [24–27]. Thus, evaluating racial differences in cancer patient experiences with ePROs is critical for averting potential exacerbation of disparities in cancer-related symptom burden and outcomes. In this paper, we report on racial differences in user experiences and satisfaction with an ePRO tool among cancer patients. Specifically, we evaluated ePRO usability and perceived value among Black and White bladder and cancer patients and whether perceptions of usability and value differed by race.
Methods
Study overview
We implemented an ePRO system among a cohort of Black and White bladder and prostate cancer patients undergoing treatment (i.e., surgery or radiation) at the North Carolina (NC) Cancer Hospital, a large public academic facility located in the USA. We selected bladder and prostate patients as our study population due to the overlap in providers that treat these patients (urologists and radiation oncologists), as well as similarities in the side effects experienced by this patient population (e.g., urinary, bowel, and sexual dysfunction). The study was approved by the UNC Institutional Review Board, and all participants provided informed consent prior to study participation.
Participants completed ePRO symptom surveys capturing gastrointestinal function, sexual function, depression, anxiety, fatigue, sleep, and urinary function (approximately 45 symptom items total). All symptom domains were assessed with PROMIS short forms [28–36] except urinary function which was measured using the Bladder Cancer Index or Expanded Prostate Cancer Index Composite [37, 38].
ePRO symptom surveys were administered at baseline (pre-treatment) following an ePRO training with a clinical research assistant, one month and 3 months following treatment initiation. Participants were given the option of completing ePRO surveys at home or in clinic using either a web-based or automated telephone system. All ePRO surveys were administered using PRO Core, a PRO data collection system housed at the UNC Lineberger Comprehensive Cancer Center. During clinic visits, patients (and their clinicians) received a symptom summary report (Fig. 1) that summarized their symptom severity longitudinally.
Fig. 1.
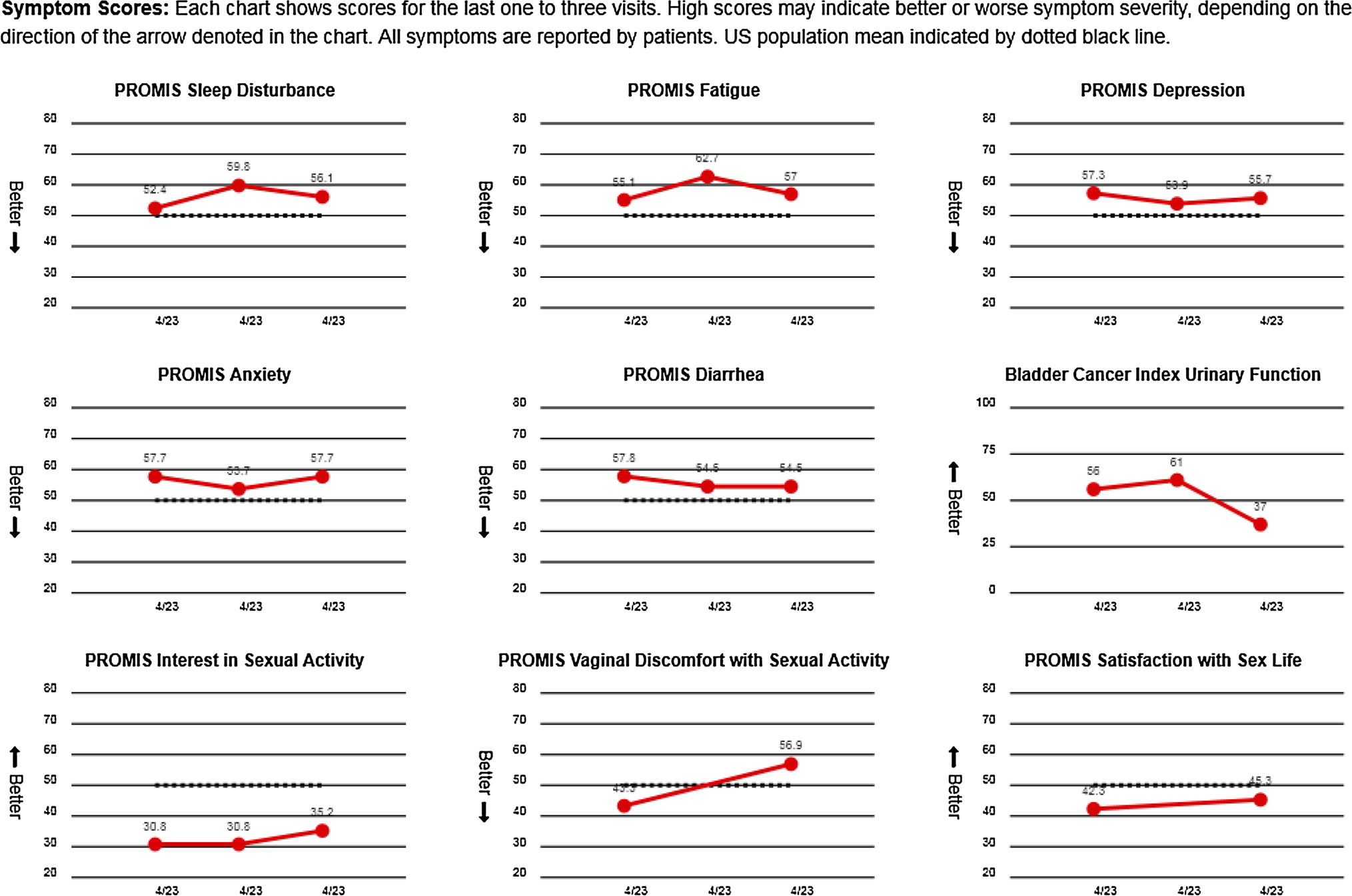
Symptom summary report
We employed a sequential explanatory mixed methods research design [39] to assess patient experiences with the ePRO system and symptom summary report using end-of-study patient satisfaction surveys (quantitative survey) and semi-structured qualitative interviews with participants.
Study site
Participants were recruited from the NC Cancer Hospital’s Multidisciplinary Urology and Radiation Oncology clinics from May 2017 to January 2018.
Participant eligibility
We employed a purposive sampling approach (oversampling Blacks) to recruit 30 Black and 49 White participants for the ePRO study. Participants were eligible if they were 18 years or older, identified as Black or White, had a prostate or bladder cancer diagnosis, and intended to undergo treatment at the NC Cancer Hospital. Participants were ineligible if they already initiated cancer-directed treatment; identified as a race other than Black or White; were unable to read and speak English or unable to comply with the study for any reason apart from language; or had dementia, altered mental status, or any psychiatric condition that prohibited understanding and/or the ability to provide informed consent.
Data collection
End-of-study patient satisfaction survey
All study participants were invited to complete end-of-study patient satisfactions survey following the final ePRO survey. The satisfaction survey included items assessing patient perspectives on ePRO ease of use, understanding of the ePRO survey items and symptom summary report, helpfulness of the ePRO survey in facilitating conversations with clinicians, and overall satisfaction with the ePRO survey. All questions included either a yes/no or seven-point Likert scale response options (Supplemental Appendix A).
Semi-structured interviews
A random subset of study participants, racially proportional in number to the overall cohort (n = 15 Black; n = 25 White), were invited to participate in end-of-study semi-structured interviews to share their experiences with ePRO system. A semi-structured interview guide (Supplemental Appendix B) was developed to explore three general topics related to the ePRO survey: ease of use, perceived value, and impact on patient-provider communication regarding symptoms. Interviews were conducted by two clinical research assistants, audio recorded, and transcribed verbatim. Interview participants completed interviews in person or by telephone and received a $25 incentive.
Data analysis
Participant demographics and end-of-study patient satisfaction survey
We computed overall and unadjusted race-specific estimates for demographics and responses to satisfaction surveys.
Semi-structured interviews
With input from the larger research team, two graduate research assistants (GRAs) (i.e., doctoral students) with qualitative analysis experience developed a codebook (Appendix C). Topical codes were identified based on questions from the semi-structured interview guide. Next, the GRAs reviewed the interview transcripts to generate a set of emergent codes reflecting new topics that developed during the interviews. Each transcript was uploaded into NVivo version 12, a qualitative analysis software program. Both GRAs separately coded three transcripts and met to discuss coding agreement and resolve discrepancies. After establishing inter-coder reliability, GRAs coded each of the remaining transcripts separately. The GRAs then used the NVivo-generated code reports to identify overall patterns, main concepts, and themes. The NVivo query function was also used to generate race-specific code reports, which facilitated assessment of race-specific differences in codes and themes. Qualitative findings were integrated with satisfaction survey results using a mixed methods narrative approach [39, 40] where interview findings helped to expand upon and provide context for interpreting satisfaction survey results.
Results
Sample characteristics
Among the 79 ePRO study participants (overall cohort), 34 participants completed end-of study patient satisfaction surveys (n = 9 Black; n = 25 White) and 40 participants completed semi-structured interviews (n = 15 Black; n = 25 White). The majority of satisfaction survey and semi-structured interview participants were male, White, had a diagnosis of prostate cancer, had at least a high school diploma, and selected the web-based system, though Black participants were more likely to select the automated telephone system relative to Whites (Table 1). Compared with White participants who completed the satisfaction survey, Blacks participants were younger, had less education, and were less likely to be married. Black participants who completed semi-structured interviews were more likely to have prostate cancer than Whites. Additionally, compared with the overall cohort of ePRO study participants, those completing the satisfaction survey were more likely to be White, diagnosed with prostate cancer, and treated with radiation.
Table 1.
Demographics of overall ePRO study participants, satisfaction survey participants, and qualitative interview participants, by race
| Characteristics | Overall (n = 79) |
Participants that completed satisfaction survey (n = 34) |
Participants that Completed a qualitative interview (n = 40) |
|||
|---|---|---|---|---|---|---|
| Black (N = 30) | White (N = 49) | Black (N = 9) | White (N = 25) | Black (N = 15) | White (N = 25) | |
|
| ||||||
| Age | ||||||
| Mean, SD | 62.8 (8.1) | 66.8 (8.7) | 58.7 (7.2) | 66.1 (8.4) | 62.1 (8.0) | 66.9 (9.4) |
| Sex | ||||||
| Male | 25 (83.3%) | 44 (89.8%) | 9 (100.0%) | 23 (92.0%) | 12 (80.0%) | 22 (88.0%) |
| Female | 5 (16.7%) | 5 (10.2%) | 0 (0.0%) | 2 (8.0%) | 3 (20.0%) | 3 (12.0%) |
| Education | ||||||
| High school diploma or less | 10 (33.3%) | 9 (18.4%) | 4 (44.4%) | 3 (12.0%) | 4 (26.7%) | 3 (12.0%) |
| Some vocational, business, or technical college | 9 (30.0%) | 10 (20.4%) | 3 (33.3%) | 4 (16.0%) | 5 (33.3%) | 8 (32.0%) |
| Some college | 5 (16.7%) | 10 (20.4%) | 2 (22.2%) | 7 (28.0%) | 3 (20.0%) | 5 (20.0%) |
| Four-year college degree | 3 (10.0%) | 7 (14.3%) | 0 (0.0%) | 4 (16.0%) | 2 (13.3%) | 3 (12.0%) |
| Graduate School | 3 (10.0%) | 13 (26.5%) | 0 (0.0%) | 7 (28.0%) | 1 (6.7%) | 6 (24.0%) |
| Occupation status | ||||||
| Employed | 7 (23.3%) | 21 (42.9%) | 2 (22.2%) | 9 (36.0%) | 4 (26.7%) | 11 (44.0%) |
| Medical leave or disabled | 2 (6.7%) | 1 (2.0%) | 0 (0.0%) | 1 (4.0%) | 0 (0.0%) | 1 (4.0%) |
| Retired | 17 (56.7%) | 27 (55.1%) | 5 (55.6%) | 15 (60.0%) | 9 (60.0%) | 13 (52.0%) |
| Unemployed | 2 (6.7%) | 0 (0.0%) | 1 (11.1%) | 0 (0.0%) | 1 (6.7%) | 0 (0.0%) |
| Missing | 2 (6.7%) | 0 (0.0%) | 1 (11.1%) | 0 (0.0%) | 1 (6.7%) | 0 (0.0%) |
| Marital status | ||||||
| Married or living with a partner | 19 (63.3%) | 41 (83.7%) | 6 (66.7%) | 20 (80.0%) | 9 (60.0%) | 19 (76.0%) |
| Unmarried | 11 (36.7%) | 8 (16.3%) | 3 (33.3%) | 5 (20.0%) | 6 (40.0%) | 6 (24.0%) |
| Health insurance typea | ||||||
| Insured private | 8 (26.7%) | 30 (61.2%) | 2 (22.2%) | 12 (48.0%) | 5 (33.3%) | 12 (48.0%) |
| Insured public | 24 (80.0%) | 32 (65.3%) | 7 (77.7%) | 18 (72.0%) | 11 (73.3%) | 17 (68.0%) |
| Cancer type | ||||||
| Bladder | 9 (30.0%) | 19 (38.8%) | 0 (0.0%) | 7 (28.0%) | 3 (20.0%) | 13 (52.0%) |
| Prostate | 21 (70.0%) | 30 (61.2%) | 9 (100.0%) | 18 (72.0%) | 12 (80.0%) | 12 (48.0%) |
| Treatment type | ||||||
| Surgery | 20 (66.7%) | 35 (71.4%) | 3 (33.3%) | 13 (52.0%) | 9 (60.0%) | 20 (80.0%) |
| Radiation | 10 (33.3%) | 14 (28.6%) | 6 (66.7%) | 12 (48.0%) | 6 (40.0%) | 5 (20.0%) |
| Delivery methoda | ||||||
| Automated telephone system | 12 (40.0%) | 5 (10.2%) | 3 (33.3%) | 5 (20.0%) | 5 (33.3%) | 4 (16.0%) |
| Web-based system | 18 (60.0%) | 42 (85.7%) | 7 (77.8%) | 24 (96.0%) | 10 (66.7%) | 21 (84.0%) |
| Missing | 0 (0.0%) | 2 (4.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
Does not add up to 100 percent due to participants being able to select all that apply
Theme 1: ePRO system usability
Overall findings
End-of study patient satisfaction surveys
Most web-based ePRO users reported that the system was “very easy/easy” to use (87.1%) and were “very satisfied/satisfied” with the web-based system (88.2%; Fig. 2). Similarly, most automated telephone-based ePRO users reported that it was “very easy/easy” to use (75.0%) and were satisfied with the automated telephone interface (75.0%). The majority of participants reported that they understood all ePRO symptom questions (82.4%) and that it was “very easy/easy” to answer the questions (94.1%).
Fig. 2.
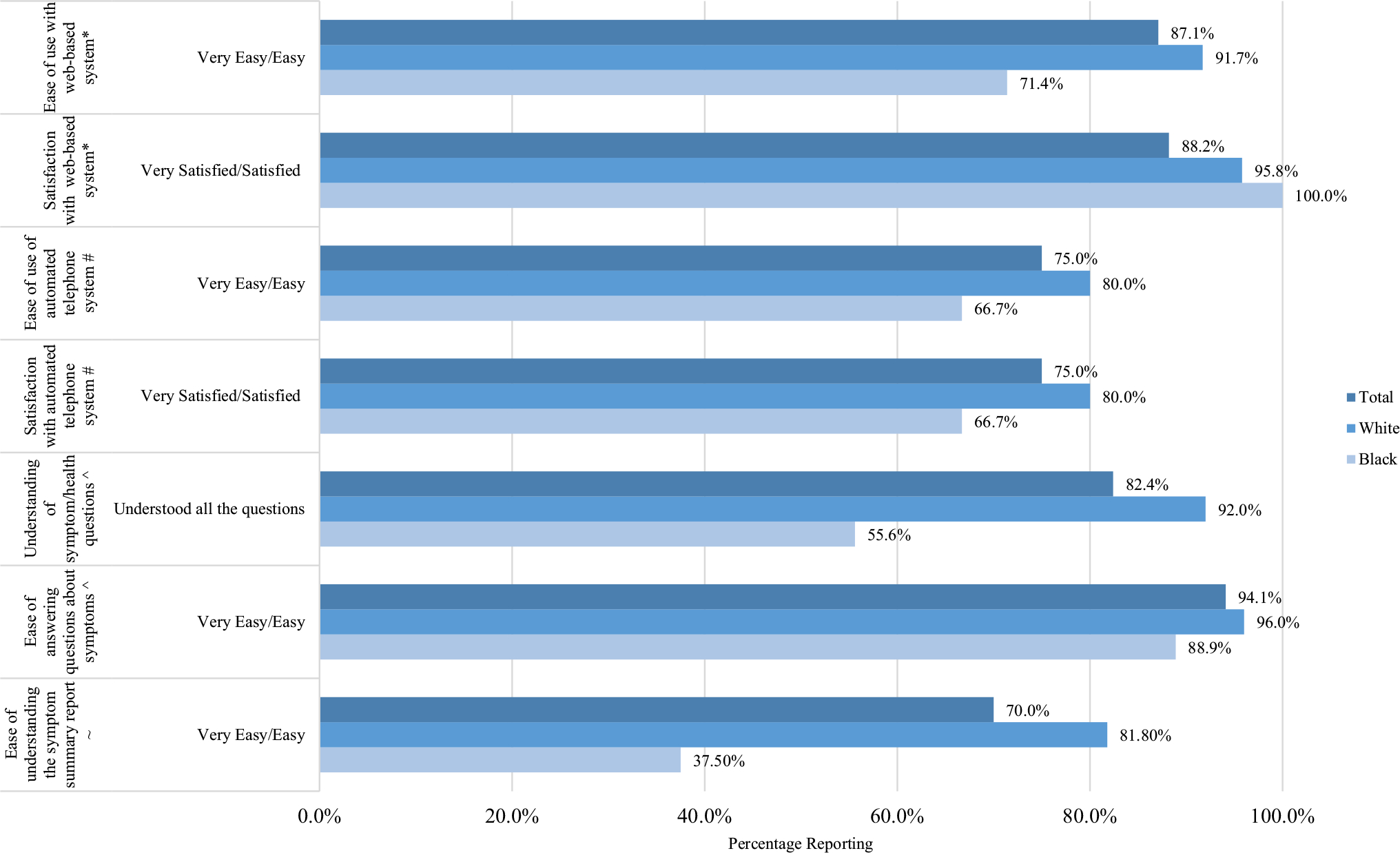
Satisfaction survey responses on usability of ePRO system, overall and by race. *Denominator is among those who completed online web-based ePRO (Total N = 31; Black N = 7; White N = 24); #Denominator is among those who completed automated telephone ePRO (Total N = 8, Black N = 3, White N = 5); ^Denominator is among all satisfaction survey participants (Total N = 34, Black N = 9, White N = 25); ~Denominator is among those who received a paper symptom summary report (Total N = 30, Black N = 8 White N = 22)
Semi-structured interviews
Participants described positive experiences using the ePRO survey, including satisfaction with the training processes and ease of use (Table 2). However, some described challenges in using the ePRO survey for the first time, such as difficulty understanding questions. As one participant explained, “When I first started out, I didn’t understand some of the questions. Then I asked the nurse and she told me what to do. Then I was good to go” (Black participant). Additionally, automated telephone ePRO users noted barriers to completing the survey, such as technical difficulties with their cell phone reception or the automated telephone system was offline when respondents tried to call.
Table 2.
Key interview quotes on ePRO system ease of use, overall and by race
| Key qualitative interview findings: ease of use | Quotes reflecting patterns among overall participants | Quotes reflecting differences between Black and White participants (where applicable) |
|---|---|---|
|
| ||
| Participants generally reported positive experiences using the ePRO system, but noted a few key challenges (e.g., understanding some questions). Black participants noted that the ePRO system was initially challenging to use more often than White participants | “I don’t think any of it was hard. It was easier than any other type of thing like that than I’ve done.” (White participant) |
Black: “When I first started out, I didn’t understand some of the questions. Then I asked the nurse and she told me what to do. Then I was good to go.” (Black participant) White: “It was really not hard at all.” (White participant) |
| Generally, participants described preferences for completing the survey online for convenience, but Black participants described preferences for completing it by phone or paper (if given the option) | “I think it’s easier to use the online... ” (White participant) |
Black: “[I’d prefer the paper-based survey] because I’d have more time to sit and look at it and read it and think about it before I answered... ” (Black participant) White: “Because online is all right there. It’s easier. It transfers farter. It’s what I’m used to. I mean, paper is kind of not—it’s kinda going away.” (White participant) |
| Participants noted a few key barriers to completing the survey, such as technical difficulties with their cell phone reception or the integrated voice response system or being used for telephone survey completion | “...There was some sort of technical difficulty at... their end of it. Because it just went blank on me... where the phone call is made, and the beginning of the survey is just—it was like there was something wrong technically at the other end, because the phone just went dead (White participant).” | N/A (key barriers were consistent among Black and White participants) |
| Participants were divided about their preferences for completing the survey at home (so they would have more time) or in the clinic (so they could ask questions to the staff and/or complete it while waiting for their appointment) | “It was probably more convenient at home to do it on your time, plus you could stop, come bark, finish if somethin’ came up or somethin’ you had to do.” (White participant) “...I liked it better when I was in the clinic ’cause I already had that time to do it.” (Black participant) |
N/A |
| Overall, participants reported that the Symptom Summary was easy to understand. Among the participants who did report challenges in understanding the Symptom Summary, Black participants more often reported challenges related to their general understanding, whereas White participants reported more specific challenges (e.g., confusion about acronyms used and the numbers included) | “It [understanding the Symptom Summary] was pretty easy for me.” (White participant) |
Black: “I didn’t understand it. I remember seein’ that now.” (Black participant) White: “I mean, I’m totally at a loss. There’s another one about anxiety, and my answers are 51.2, 51.2 and 51.2. Now, I answered—I had probably six choices with anxiety, and I’ve got, somehow, an answer of 51.2. It’s just, like, it just doesn’t make any sense whatsoever.” (White participant) |
Participants who used the online web-based system and those using the automated telephone system indicated that they preferred their self-selected ePRO modality due to its convenience. When asked if they would prefer to use a paper survey if given the option, participants generally responded that they would not prefer this option because other methods (i.e., online or phone) are more convenient and because “…paper is… kinda going away” (White participant). However, a small subset of participants shared that they would prefer using a paper survey because they could more clearly see all the questions and take more time to answer.
Participants were divided about preferences for completing the ePRO at home versus in clinic. Some preferred completing ePRO surveys at home because there would be fewer interruptions and more time to focus on the because they could do so during their appointment wait time and/or ask staff questions in person.
Participants generally reported that the symptom summary report was easy to understand and helped them better understand their symptoms. However, some participants reported difficulty in interpreting the numbers in the symptom summary report. To address this challenge, one participant recommended: “I just think that y’all need to let people, whenever you give them the surveys, the scale, explain it to ‘em xactly what it’s supposed to show you” (Black participant). Participants also offered other suggestions for improving the symptom summary report display, such as clarifying what the numbers in the report mean, moving some of the lines in the graphs so they do not obscure the numbers, spelling out acronyms (e.g., PROMIS), and offering an executive summary of results.
Race-specific findings
End-of study patient satisfaction surveys
Web-based ePRO system use was more common among Whites relative to Blacks (77.7% Black; 96.0% White, Table 1). Black participants were also less likely than Whites to report that the web-based system was “very easy/easy” to use (71.4% Black; 91.7% White, Fig. 2); however, nearly all Black and White respondents reported being “very satisfied/satisfied” with the web-based system (100.0% Black; 95.8% White). Most White respondents reported that they understood all of the ePRO survey questions compared with roughly half of Black participants (55.6% Black; 92.0% White). Whites and Blacks similarly reported that that it was “very easy/easy” to answer the ePRO survey (88.9% Black; 96.0% White). Moreover, Whites more commonly reported that it was “very easy/easy” to understand the symptom summary report than Black participants (37.5% Black; 72.0% White).
Semi-structured interviews
Compared with White participants, Black participants more commonly reported that the ePRO survey was initially challenging to use. When elaborating on these challenges, Black participants focused on difficulty related to understanding the wording of some of the questions.
In terms of modality preferences, White participants commonly described a preference for completing the ePRO survey online because the process was quicker and easier. Some Black participants, on the other hand, commonly expressed a preference for paper-based reporting, if given the option, due to perceptions that paper-based surveys allow more time for processing symptom questions.
Among participants reporting challenges in understanding the symptom summary report, Black participants more often reported challenges in their general understanding of the report, whereas White participants reported more specific challenges (e.g., confusion about acronyms, inclusion of too much detail). Moreover, White participants commonly described being able to understand the symptom summary report with staff assistance.
Theme 2: perceived value of ePRO system
Overall findings
End-of study patient satisfaction surveys
Most participants reported that the ePRO survey was “very helpful/helpful” in reminding them of symptoms experienced in the last seven days (76.5%; Fig. 3). Similarly, 88.2% of participants reported they would use the ePRO survey during future clinic visits and 82.4% indicated that they would recommend other patients to use it. Additionally, most participants reported being “very satisfied/satisfied” with the ePRO survey (79.4%).
Fig. 3.
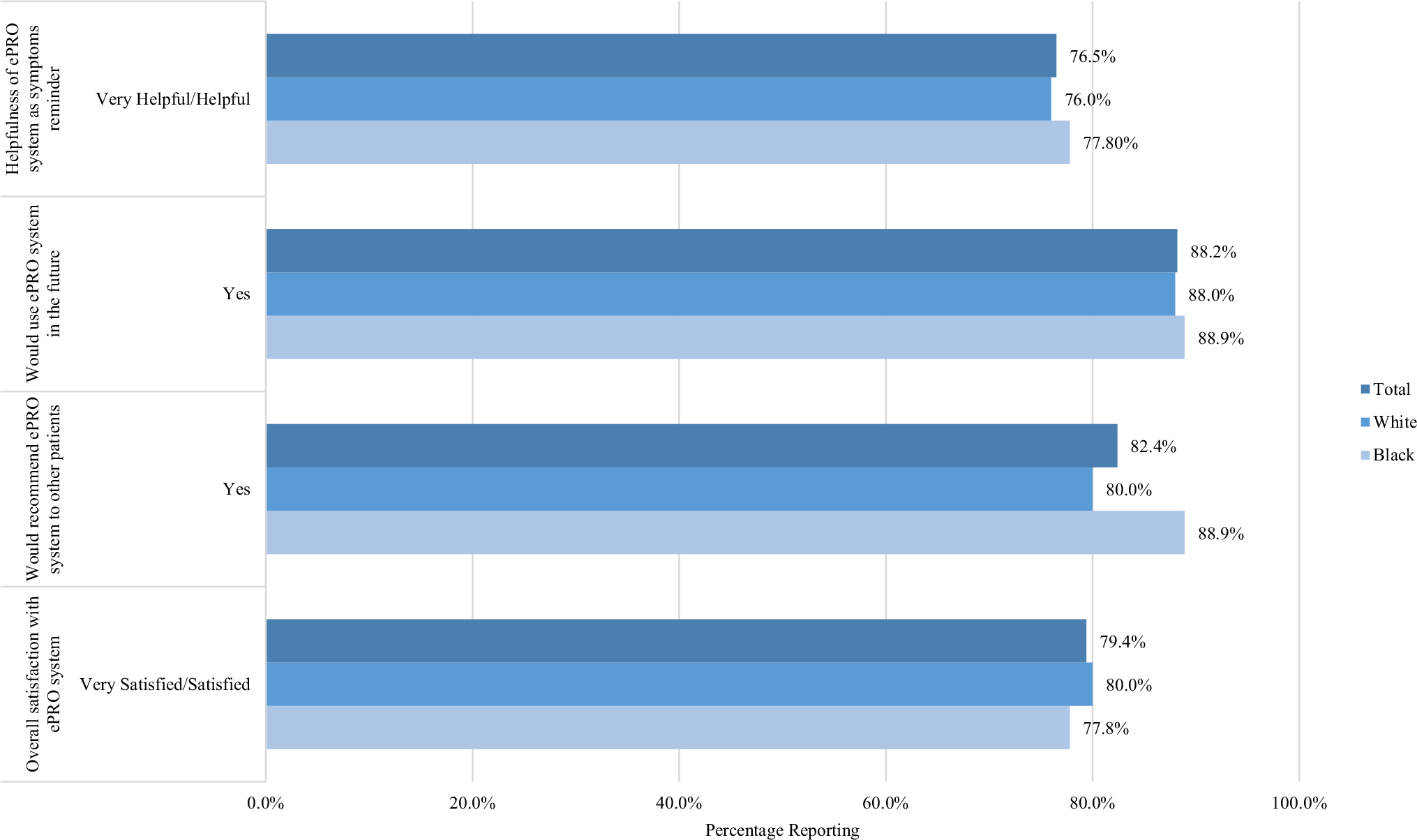
Satisfaction survey responses on perceived value of epro system, overall and by race. Denominator is among all satisfaction survey participants (Total N = 34, Black N = 9, White N = 25)
Semi-structured interviews
Participants described several benefits to completing the survey, including gaining knowledge about their disease, better awareness of their symptoms, identifying questions/topics to discuss with their doctor, tracking symptoms longitudinally, and being able to initially report on sensitive topics/symptoms electronically instead of face-to-face with a clinician (Table 3). Participants generally expressed a willingness to continue using the ePRO survey at future follow-up visits to help advance science or to help keep track of their symptoms: “I would choose to [continue completing it] because … It’s gonna help science” (Black participant).
Table 3.
Key interview quotes on perceived value of ePRO system, overall and by race
| Key qualitative interview findings: perceived value | Quotes reflecting patterns among overall participants | Quotes reflecting differences between Black and White participants (where applicable) |
|---|---|---|
|
| ||
| Participants described several benefits from the ePRO system (e.g., better understanding their symptoms). Black participants focused on how the ePRO system helped them better understand their disease/symptoms, whereas White participants noted additional specific benefits (e.g., tracking symptoms over time) | “I think it probably made me think mere concisely about symptoms. When I did talk to the doctor, I could express what was going on better.” (White participant) |
Black: “[It] just gives you more knowledge of your body, what to look for, so that you can conversate with your physician” (Black participant) White: “I see a self-awareness of where I was and where I am now. I think that was—looking at it in that form, I realized how much I have improved physically” (White participant) I would choose to [continue completing it] because it’s a survey that’s part [of a] study. It’s gonna help science” (Black participant) |
| Participants suggested additional health or symptom-related items to include in the ePRO system (e.g., about comorbid conditions). Suggestions generally came from White participants | “Well, the only other thing, you know, and I’m being treated for prostate cancer, but I also have diabetes. I’m being treated by that up here. The two—how do I say this—the two are really hard sometimes to take care of both at one time. Somebody in the survey needs to realize that people are being treated for multiple situations, what effect you have with one versus the other.” (White participant) | N/A (suggestions generally came from White participants) |
| Participants described key barriers that may be helpful to include in the ePRO system | “I live two hours’ drive. I can’t get no transportation.” (Black participant) “I think any of those things, especially barriers to getting symptoms diagnosed. Barriers to getting questions answered. Getting help from the provider. Those are probably the most important. Things like cost of medications. Transportation. Location. Timing of appointments. All of those things that are also barriers, I mean, you can also look at that. ” (White participant) |
N/A (suggestions were generally consistent among Black and White participants) |
| A small minority of participants (who were mostly White) said that the survey was not helpful because it made no difference in their treatment. When Black participants provided negative feedback about the ePRO system’s value, they often hedged their comments and/or paired them with positive observations, whereas White participants did not hedge negative feedback | “It just didn’t seem like it was an advantage or a disadvantage. Just another form to fill out but it didn’t have much impact on my life, to be honest” (White participant) |
Black: “...I’m not sure that the survey was a [benefit] to me at all... ‘Cause like I said, everybody at the clinic was pretty thorough when I was there. I don’t think they missed anything when it came to my prostatectomy” (Black participant) White: “I can’t say it made any difference.” (White participant) |
Participants also shared suggestions for enhancing the value of the ePRO survey, including adding questions about hot flashes, diet, physical activity, and symptoms related to comorbid conditions. As one participant explained, “…I’m being treated for prostate cancer, but I also have diabetes…. The two are really hard sometimes to take care of both at one time. Somebody [on] the survey [study team] needs to realize that people are being treated for multiple situations…” (White participant). Participants also recommended pairing the ePRO with more information about symptoms and side effects that they may experience during and after treatment, so that that they could be better prepared to recognize symptoms.
Finally, participants shared health care experiences/barriers that may be helpful to include in the survey, such as transportation challenges, coordinating care at multiple hospitals/clinics, paying for treatment/medications, convenience of medical appointments and parking, clinic wait times, long-term patient recovery and well-being, challenges communicating with providers, and friendliness of staff.
Race-specific findings
End-of study patient satisfaction surveys
The majority of Black and White reported that the ePRO survey was “very helpful/helpful” in reminding them of symptoms they experienced in the last seven days, (77.8% Black; 76.0% White), and that they would use the ePRO survey again if they returned to the clinic (88.9% Black; 88.0% White), and would recommend other patients to use it (88.9% Black; 88.0% White). Similarly, most Black and White reported feeling “very satisfied/satisfied” with the ePRO survey (77.8% Black; 80.0% White).
Semi-structured interviews
When discussing ePRO survey benefits, Black participants generally focused on how the survey helped them better understand their disease and symptoms: “[It] just gives you more knowledge of your body, what to look for, so that you can [converse] with your physician” (Black participant). White participants commonly described the benefits of better understanding their symptoms, but discussed several other benefits as well (e.g., tracking their symptoms over time). As one White participant explained, “I see a self-awareness of where I was and where I am now…. looking at it in that form, I realized how much I have improved physically” (White participant).
Additionally, in contrast with White participants, when Black participants provided negative feedback about the value of the ePRO tool, they generally hedged their comments and/or paired them with positive observations. For example, as one participant explained, “…I’m not sure that the survey was a [benefit] to me at all… ‘Cause like I said, everybody at the clinic was pretty thorough when I was there. I don’t think they missed anything when it came to my prostatectomy” (Black participant). Additionally, suggestions for symptoms to improve the ePRO survey generally came from White participants, despite more Blacks reporting difficulty using ePRO system.
A small minority of participants, most of whom were White, indicated that the ePRO was not helpful at any time because it did not make a difference in their treatment: “It just didn’t seem like it was an advantage or a disadvantage. Just another form to fill out but it didn’t have much impact on my life” (White participant). Similarly, a small subset of mostly White participants said that they would be unwilling to continue using the ePRO survey during follow-up appointments because it seemed unnecessary.
Theme 3: impact of ePRO system use on patient-provider communication
Overall findings
End-of study patient satisfaction surveys
Most participants reported that their doctor communicated with them about their ePRO-reported symptoms (85.3%; Fig. 4). About half of all participants reported that the ePRO survey helped them discuss medical issues with their doctor that they may not have otherwise discussed (52.9%). Over half of respondents reported that the ePRO survey was “very helpful/helpful” in talking with clinicians about symptom concerns (64.7%).
Fig. 4.
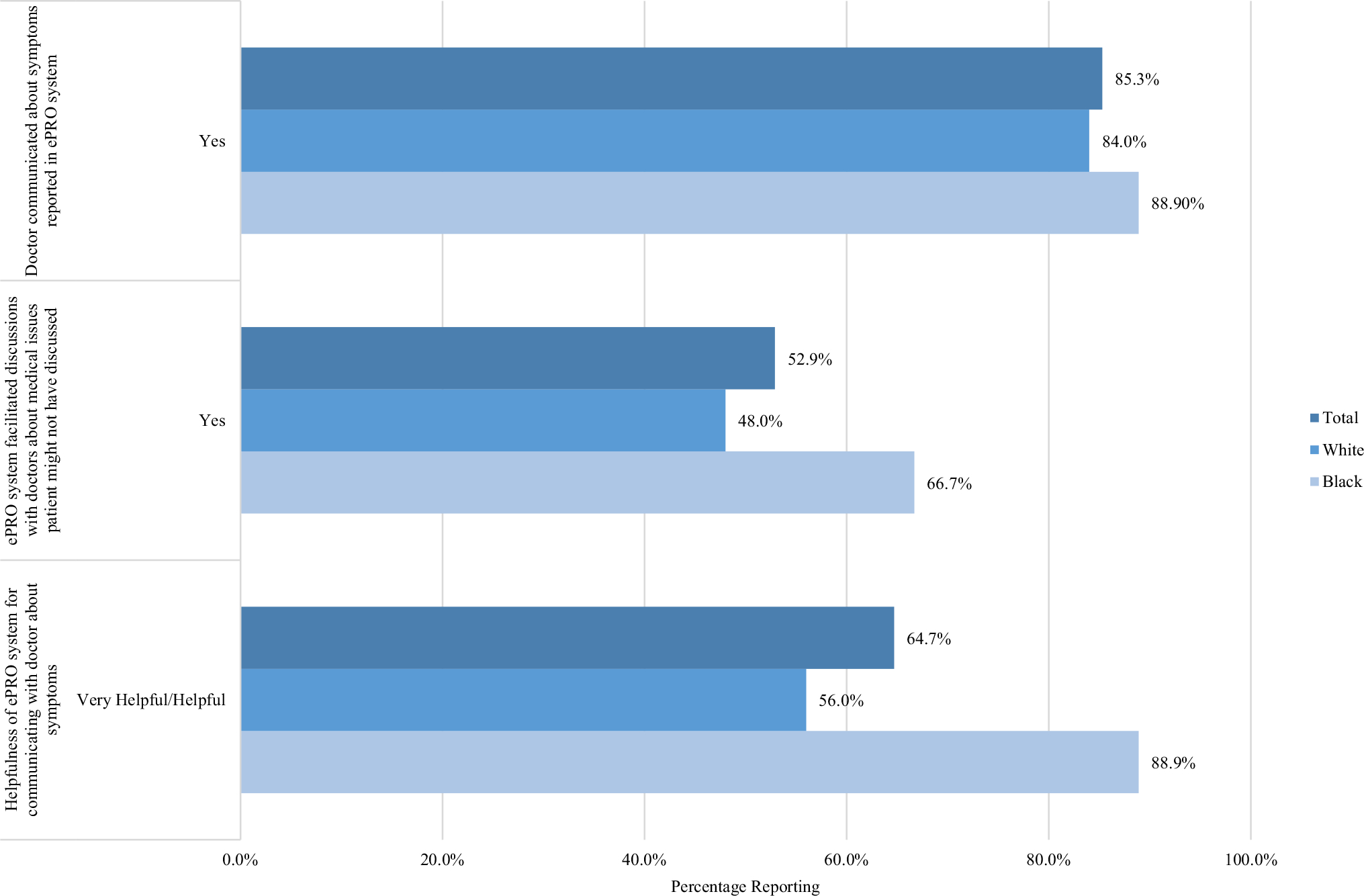
Satisfaction survey responses on the impact of ePRO system use on patient-provider communication, overall and by race. Denominator is among all satisfaction survey participants (Total N = 34, Black N = 9, White N = 25)
Semi-structured interviews
Participants commonly reported that the ePRO positively impacted communication with their provider by precipitating additional discussion about their symptoms/treatment and helping participants think of additional questions to ask clinicians (Table 4). One participant explained that, “It just brought up some talk points that maybe I wouldn’t have thought of in there—you’re emotional about having cancer and answering the questions, and I probably would have forgot some of those things, the talk topics” (White participant). Yet, a smaller subset of participants noted that the ePRO did not impact provider communication, as the ePRO survey results were not discussed during clinic visits. For example, one participant noted that, “We talked about what to do, given my symptoms and the problems I’m having, but we didn’t talk directly about the survey results itself” (White participant).
Table 4.
Key interview quotes on the impact of ePRO system use on patient-provider communication, overall and by race
| Key qualitative interview findings: impact on patient-provider communication | Quotes reflecting patterns among overall participants | Quotes reflecting differences between Black and White participants (where applicable) |
|---|---|---|
|
| ||
| Overall, participants described a positive impact of ePRO system on patient-provider communication (e.g., because it sparked additional discussion about symptoms and treatment) | “It just brought up some talk points that maybe I wouldn’t have thought of in the—you’re emotional about having cancer and answering the questions, and I probably would have forgot some of those things, the talk topics” (White participant) | N/A, both White and Black participants generally reported that the ePRO system positively impacted patient-provider communication |
| Some participants noted that the ePRO system did not impact patient-provider communication, with Black participants more often hedging comments and noting caveats | “We talked about everything that I would have talked about if there had been a survey or if there hadn’t been a survey” (White participant) |
Black: “No. I don’t think he did [discuss the survey]. Again, I probably had him thinking about somethin’ else ’cause I had other questions probably keeping him from even discussing that. I’m gonna say that’s my fault” (Black participant) White: “We talked about what to do, given my symptoms and the problems I’m having, but we didn’t talk directly about the survey results itself” (White participant) |
Race-specific findings
End-of-study patient satisfaction surveys
Most Black and White respondents reported that their doctor communicated with them about ePRO-reported symptoms (88.9% Black; 84.0% White). However, Black respondents more often reported that the ePRO was “very helpful/helpful” in facilitating discussions with their doctors about symptoms they experienced (88.9% Black; 56.0% White) as well as discussing medical issues that they may not have otherwise discussed with their doctor (66.7% Black; 48.0% White).
Semi-structured interviews
Findings were generally consistent between Black and White participants regarding the impact of the ePRO tool on patient-provider communication. However, unlike White participants, when Black participants reported that their provider did not discuss the ePRO survey results during their appointments, they often hedged their comments and noted caveats (e.g., by explaining that they may not remember or by blaming themselves). As one Black participant explained, “No. I don’t think he did [discuss the survey]. Again, I probably had him thinking about somethin’ else ‘cause I had other questions probably keeping him from even discussing that. I’m gonna say that’s my fault” (Black participant).
Discussion
In this study, we examined the usability and perceived value of ePRO use within routine oncology care among a cohort of Black and White bladder and prostate cancer patients undergoing treatment and whether user experiences and perceived value differed by race. Overall, the majority of Black and White patients reported high satisfaction and value from ePRO use and expressed a willingness to continue using ePROs as part of routine clinical care. Most patients indicated that the ePRO was beneficial in reminding them about symptom concerns and facilitating symptom discussions with doctors; however, this communication-related ePRO benefit was especially pronounced among Blacks. Whites, on the other hand, more commonly perceived value from gaining more awareness about their symptoms and the ability to monitor symptoms over time. Interestingly, despite reports of high perceived value among Black patients, Blacks were less likely than Whites to report ease in understanding ePRO symptom items. Additionally, although most patients selected the web-based ePRO modality option, use of the automated telephone interface was more common among Blacks relative to Whites.
Disparities in the diffusion of health informatics tools are well documented [41–43]. For example, past research has shown that compared with Whites, Black patients are less likely to use patient portals [44]. Additionally, higher levels of education and e-health literacy have been linked to greater adoption of mobile health applications [45]. Given the substantial symptom management benefits associated with ePRO use, and longstanding disparities in symptom burden, optimizing PRO survey adoption in diverse populations, whether electronically or through paper-based delivery, is critical to addressing cancer-related symptom inequities.
Although most Black patients reported high levels of perceived value in using the ePRO tool and supported continued ePRO use, Blacks were more inclined than Whites to report challenges in understanding ePRO survey questions and the symptom summary report. On average, our Black study participants reported lower levels of education relative to Whites, which is consistent with national data on educational attainment [46]. Past research has also reported racial inequities in health literacy and computer literacy; however, we did not collect these data in our study [47–49]. Thus, racial differences in education, computer literacy, and health/e-health literacy should be taken into account in the design and implementation of ePRO tools in clinical care. In particular, it may be beneficial to provide patients both with standardized baseline ePRO training (e.g., how to use the ePRO device and how to interpret the reports), as well as refresher ePRO trainings and/or technical assistance at follow-up time points. Additionally, providing patients with a reference sheet that explains, in plain language, the ePRO symptom items and summary report may help mitigate health literacy challenges. Moreover, some Black patients expressed a desire to have paper-based options available. A possible work-around might involve having designated clinic staff collect completed paper-based PRO surveys at clinic visits and enter those data into the ePRO system on behalf of patients. Such strategies can help ensure equitable uptake of ePROs and avert a potential “digital divide” in ePRO adoption and related benefits.
A key ePRO benefit includes its role in facilitating patient-provider communication regarding symptom concerns [13, 14]. For example, most study participants indicated that doctors discussed ePRO data with them and that the ePRO helped them identify and discuss health issues that they might have overlooked. Prior research suggests that racial disparities in symptom management may be partially due to racial differences in patient-provider communication [20, 50, 51]. Compared with White participants in our study, Black participants were more inclined to indicate that the ePRO was “very helpful/helpful” in facilitating communication with their doctors. Hence, if ePRO use disproportionately benefits Black patients, and potentially other patients of color, in communicating with clinicians regarding symptoms, it is possible that equitable implementation of ePROs in clinical care may help reduce racial gaps in symptom management. Thus, future research should explore the potential impact of equitable implementation of multi-modal PRO surveys (i.e., web-based, automated telephone-based, and paper-based delivery) on racial disparities in symptom management and symptom burden.
During interviews, study participants recommended additional items to include in the ePRO survey, such as symptoms associated with other conditions (e.g., diabetes) and symptom-relevant health care experiences/barriers. With respect to including additional symptoms, it may be helpful to include a free-text functionality that allows patients to share other symptoms they perceive as relevant to their cancer-related symptom management [28]. Moreover, past research has described the benefits of collecting PROs alongside patient-reported experience measures (PREMs), which capture patients’ clinical experiences (e.g., patient-provider communication, friendliness of clinical staff, medication affordability challenges), and have documented positive associations between PREMS and PROs [52, 53]. Thus, inclusion of PREMs in ePRO assessments may have implications for improving patient care and addressing symptom burden disparities that are partly driven by inequities in care experiences/barriers [20, 22, 23, 52]. Future research should explore the feasibility, usability, and perceived value of implementing ePREMs alongside ePROs in routine oncology care.
Limitations of this study include our focus on Black and White bladder and prostate cancer patients. Thus, our findings may not generalize to other racial/ethnic groups or other cancer types. Secondly, as this was a relatively small single-site study conducted at a large cancer hospital within an academic medical center, it remains unclear whether our findings will apply to other settings. Still, our hospital study site serves both rural and urban patients with variable levels of income and education, which reflects the broader US population. Moreover, to our knowledge, this is the first study to examine racial differences in user experiences and perceived value of ePRO use in oncology care and, therefore, is an important contribution to the PRO, oncology, and healthcare equity literature.
Conclusion
Despite racial differences in user experiences, implementation of ePROs in routine oncology care is perceived as valuable among Black and White cancer patients, with greater perceived value reported among Blacks. These findings may have implications for engaging patients and addressing disparities during cancer care. Nonetheless, when implementing ePRO systems, the health literacy needs and ePRO modality preferences of diverse populations must be considered in order to avoid exacerbation of existing disparities in care.
Supplementary Material
Acknowledgements
We would like to thank Dana Mueller for her efforts in implementing the ePRO study in the NC Cancer Hospital Urology Clinic.
Funding
This work was supported by a National Cancer Institute (NCI) Supplement to R01CA174453 (PI: Reeve and Chen). Dr. Cleo Samuel’s effort was also supported by the NCI Mentored Research Scientist Development Award 1 K01 CA218473–01A1. Jennifer Richmond’s effort was also supported by a Grant from the Robert Wood Johnson Foundation Health Policy Research Scholars program (Grant no. 73921). This project made use of systems and services provided by the Patient-Reported Outcomes Core (PRO Core; pro.unc.edu) at the Lineberger Comprehensive Cancer Center of the University of North Carolina. PRO Core is funded in part by a National Cancer Institute Cancer Center Core Support Grant (5-P30-CA016086) and the University Cancer Research Fund of North Carolina. LCCC Bioinformatics Core provided the computational infrastructure for the project.
Footnotes
Compliance with ethical standards
Conflicts of interest Dr. Cleo A. Samuel reports research funding from NCI and Pfizer for work unrelated to this study. Dr. Angela Smith reports funding from Patient-Centered Outcomes Research Institute and Agency for Healthcare Research and Quality and compensation as a consultant for Merck and scientific advisory board for Urogen and Photocure during the study time period, all of which were outside the relevant work. All other authors do not report any conflicts of interest.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (University of North Carolina Institutional Review Board IRB number: 16–2873) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s11136-020-02442-4) contains supplementary material, which is available to authorized users.
References
- 1.Alcalá HE (2014). Differential mental health impact of cancer across racial/ethnic groups: Findings from a population-based study in California. BMC Public Health, 14(1), 930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson KO, Green CR, & Payne R (2009). Racial and ethnic disparities in pain: Causes and consequences of unequal care. The Journal of Pain, 10(12), 1187–1204. [DOI] [PubMed] [Google Scholar]
- 3.Apenteng BA, Hansen AR, Opoku ST, & Mase WA (2017). Racial disparities in emotional distress among cancer survivors: Insights from the Health Information National Trends Survey (HINTS). Journal of Cancer Education, 32(3), 556–565. [DOI] [PubMed] [Google Scholar]
- 4.Chornokur G, Dalton K, Borysova ME, & Kumar NB (2011). Disparities at presentation, diagnosis, treatment, and survival in African American men, affected by prostate cancer. The Prostate, 71(9), 985–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reyes-Gibby CC, Anderson KO, Shete S, Bruera E, & Yennurajalingam S (2012). Early referral to supportive care specialists for symptom burden in lung cancer patients: A Comparison of Non-Hispanic Whites, Hispanics, and Non-Hispanic Blacks. Cancer, 118(3), 856–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, et al. (2016). Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. Journal of Clinical Oncology, 34(6), 557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Denis F, Basch E, Septans A-L, Bennouna J, Urban T, Dueck AC, et al. (2019). Two-year survival comparing web-based symptom monitoring vs routine surveillance following treatment for lung cancer. JAMA, 321(3), 306–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mooney K, Berry DL, Whisenant M, & Sjoberg D (2017). Improving cancer care through the patient experience: How to use patient-reported outcomes in clinical practice. American Society of Clinical Oncology Educational Book, 37, 695–704. [DOI] [PubMed] [Google Scholar]
- 9.Anderson KO, Mendoza TR, Valero V, Richman SP, Russell C, Hurley J, et al. (2000). Minority cancer patients and their providers: Pain management attitudes and practice. Cancer: Interdisciplinary International Journal of the American Cancer Society, 88(8), 1929–1938. [PubMed] [Google Scholar]
- 10.Yoon J, Malin JL, Tisnado DM, Tao ML, Adams JL, Timmer MJ, et al. (2008). Symptom management after breast cancer treatment: Is it influenced by patient characteristics? Breast Cancer Research and Treatment, 108(1), 69–77. [DOI] [PubMed] [Google Scholar]
- 11.Cleeland CS, Wang XS, Shi Q, Mendoza TR, Wright SL, Berry MD, et al. (2011). Automated symptom alerts reduce postoperative symptom severity after cancer surgery: A randomized controlled clinical trial. Journal of Clinical Oncology, 29(8), 994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stover A, Irwin DE, Chen RC, Chera BS, Mayer DK, Muss HB, et al. (2015). Integrating patient-reported outcome measures into routine cancer care: Cancer patients’ and clinicians’ perceptions of acceptability and value. Egems, 3(1), 1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, et al. (2004). Measuring quality of life in routine oncology practice improves communication and patient well-being: A randomized controlled trial. Journal of Clinical Oncology, 22(4), 714–724. [DOI] [PubMed] [Google Scholar]
- 14.Berry DL, Blumenstein BA, Halpenny B, Wolpin S, Fann JR, Austin-Seymour M, et al. (2011). Enhancing patient-provider communication with the electronic self-report assessment for cancer: A randomized trial. Journal of Clinical Oncology, 29(8), 1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Judson TJ, Bennett AV, Rogak LJ, Sit L, Barz A, Kris MG, et al. (2013). Feasibility of long-term patient self-reporting of toxicities from home via the Internet during routine chemotherapy. Journal of Clinical Oncology, 31(20), 2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwok W, & Bhuvanakrishna T (2014). The relationship between ethnicity and the pain experience of cancer patients: A systematic review. Indian journal of palliative care, 20(3), 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryan CL, & Bauman K Educational Attainment in the U.S Retrieved from https://www.census.gov/content/dam/Census/library/publications/2016/demo/p20-578.pdf.
- 18.Bennett IM, Chen J, Soroui JS, & White S (2009). The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. The Annals of Family Medicine, 7(3), 204–211. 10.1370/afm.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaudhry SI, Herrin J, Phillips C, Butler J, Mukerjhee S, Murillo J, et al. (2011). Racial disparities in health literacy and access to care among patients with heart failure. Journal of Cardiac Failure, 17(2), 122–127. 10.1016/j.cardfail.2010.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diette GB, & Rand C (2007). The contributing role of healthcare communication to health disparities for minority patients with asthma. Chest, 132(5), 802S–809S. [DOI] [PubMed] [Google Scholar]
- 21.Gellad WF, Haas JS, & Safran DG (2007). Race/ethnicity and nonadherence to prescription medications among seniors: Results of a national study. Journal of General Internal Medicine, 22(11), 1572–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ly DP, & Glied SA (2010). Disparities in service quality among insured adult patients seen in physicians’ offices. Journal of General Internal Medicine, 25(4), 357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mandelblatt JS, Yabroff KR, & Kerner JF (1999). Equitable access to cancer services: A review of barriers to quality care. Cancer: Interdisciplinary International Journal of the American Cancer Society, 86(11), 2378–2390. [PubMed] [Google Scholar]
- 24.Carroll JK, Moorhead A, Bond R, LeBlanc WG, Petrella RJ, & Fiscella K (2017). Who uses mobile phone health apps and does use matter? A secondary data analytics approach. Journal of Medical Internet Research, 19(4), e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gibbons MC (2011). Use of health information technology among racial and ethnic underserved communities. Perspectives in Health Information Management/AHIMA. Illinois: American Health Information Management Association. [PMC free article] [PubMed] [Google Scholar]
- 26.Krebs P, & Duncan DT (2015). Health app use among US mobile phone owners: A national survey. JMIR mHealth and uHealth, 3(4), e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell UA, Chebli PG, Ruggiero L, & Muramatsu N (2018). The digital divide in health-related technology use: The significance of race/ethnicity. The Gerontologist, 59(1), 6–14. [DOI] [PubMed] [Google Scholar]
- 28.Chung AE, Shoenbill K, Mitchell SA, Dueck AC, Schrag D, Bruner DW, et al. (2019). Patient free text reporting of symptomatic adverse events in cancer clinical research using the National Cancer Institute’s Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE). Journal of the American Medical Informatics Association, 26(4), 276–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flynn KE, Lin L, Cyranowski JM, Reeve BB, Reese JB, Jeffery DD, et al. (2013). Development of the NIH PROMIS® sexual function and satisfaction measures in patients with cancer. The Journal of Sexual Medicine, 10, 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khanna D, Hays RD, Shreiner AB, Melmed GY, Chang L, Khanna PP, et al. (2017). Responsiveness to change and minimally important differences of the patient-reported outcomes measurement information system gastrointestinal symptoms scales. Digestive Diseases and Sciences, 62(5), 1186–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spiegel BM, Hays RD, Bolus R, Melmed GY, Chang L, Whitman C, et al. (2014). Development of the NIH patient-reported outcomes measurement information system (PROMIS) gastrointestinal symptom scales. The American Journal of Gastroenterology, 109(11), 1804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pilkonis PA, Yu L, Dodds NE, Johnston KL, Maihoefer CC, & Lawrence SM (2014). Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS®) in a three-month observational study. Journal of Psychiatric Research, 56, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, et al. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lai J-S, Cella D, Choi S, Junghaenel DU, Christodoulou C, Gershon R, et al. (2011). How item banks and their application can influence measurement practice in rehabilitation medicine: A PROMIS fatigue item bank example. Archives of Physical Medicine and Rehabilitation, 92(10), S20–S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, et al. (2012). Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behavioral Sleep Medicine, 10(1), 6–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buysse DJ, Yu L, Moul DE, Germain A, Stover A, Dodds NE, et al. (2010). Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep, 33(6), 781–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gilbert SM, Wood DP, Dunn RL, Weizer AZ, Lee CT, Montie JE, et al. (2007). Measuring health-related quality of life outcomes in bladder cancer patients using the Bladder Cancer Index (BCI). Cancer, 109(9), 1756–1762. [DOI] [PubMed] [Google Scholar]
- 38.Wei JT, Dunn RL, Litwin MS, Sandler HM, & Sanda MG (2000). Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology, 56(6), 899–905. [DOI] [PubMed] [Google Scholar]
- 39.Fetters MD, Curry LA, & Creswell JW (2013). Achieving integration in mixed methods designs—principles and practices. Health Services Research, 48, 2134–2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ivankova NV, Creswell JW, & Stick SL (2006). Using mixed-methods sequential explanatory design: From theory to practice. Field methods, 18(1), 3–20. [Google Scholar]
- 41.Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, & Baker DW (2011). Disparities in enrollment and use of an electronic patient portal. Journal of General Internal Medicine, 26(10), 1112–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rogers EM (1961). Bibliography on the diffusion of innovations. New York: Free Press of Glencoe. [Google Scholar]
- 43.Wejnert B (2002). Integrating models of diffusion of innovations: A conceptual framework. Annual Review of Sociology, 28(1), 297–326. [Google Scholar]
- 44.Walker DM, Hefner JL, Fareed N, Huerta TR, & McAlearney AS (2019). Exploring the digital divide: Age and race disparities in use of an inpatient portal. Telemedicine and e-Health. 10.1089/tmj.2019.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bol N, Helberger N, & Weert JC (2018). Differences in mobile health app use: A source of new digital inequalities? The Information Society, 34(3), 183–193. [Google Scholar]
- 46.De Brey C, Musu L, McFarland J, Wilkinson-Flicker S, Diliberti M, Zhang A, et al. (2019). Status and trends in the education of racial and ethnic groups 2018 (NCES 2019–038). Washington, DC: US Department of Education. National Center for Education Statistics. Retrieved from https://nces.ed.gov/pubs2019/2019038.pdf. [Google Scholar]
- 47.Health U. D. o., & Services H (2008). America’s health literacy: Why we need accessible health information. An issue brief from the US Department of Health and Human Services. [Google Scholar]
- 48.Mamedova S, Pawlowski E, & Hudson L (2018). A description of US adults who are not digitally literate Stats in Brief. Washington DC: US Department of Education. [Google Scholar]
- 49.Weekes CV (2012). African Americans and health literacy: A systematic review. ABNF Journal, 23(4), 76–80. [PubMed] [Google Scholar]
- 50.Balsa AI, & McGuire TG (2003). Prejudice, clinical uncertainty and stereotyping as sources of health disparities. Journal of Health Economics, 22(1), 89–116. [DOI] [PubMed] [Google Scholar]
- 51.Balsa AI, Seiler N, McGuire TG, & Bloche MG (2003). Clinical uncertainty and healthcare disparities. Am. JL & Med, 29, 203. [PubMed] [Google Scholar]
- 52.Black N, Varaganum M, & Hutchings A (2014). Relationship between patient reported experience (PREMs) and patient reported outcomes (PROMs) in elective surgery. BMJ Qual Saf, 23(7), 534–542. [DOI] [PubMed] [Google Scholar]
- 53.Kingsley C, & Patel S (2017). Patient-reported outcome measures and patient-reported experience measures. Bja Education, 17(4), 137–144. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


