Abstract
Objective:
To gather information on the (a) types of wearable sensors, particularly personal activity monitors, currently used by occupational safety and health (OSH) professionals, (b) potential benefits of using such technologies in the workplace, and (c) perceived barriers preventing the widespread adoption of wearable sensors in industry.
Background:
Wearable sensors are increasingly being promoted as a means to improve employee health and well-being and there is mounting evidence supporting their use as exposure assessment and personal health tools. Despite this, many workplaces have been hesitant to adopt these technologies.
Methods:
An electronic survey was emailed to 28,428 registered members of the American Society of Safety Engineers (ASSE) and 1,302 professionals certified by the Board of Certification in Professional Ergonomics (BCPE).
Results:
A total of 952 valid responses were returned. Over half of respondents described being in favor of using wearable sensors to track OSH-related risk factors and relevant exposure metrics at their respective workplaces. However, barriers including concerns regarding employee privacy/confidentiality of collected data, employee compliance, sensor durability, the cost/benefit ratio of using wearables, and good manufacturing practice requirements were described as challenges precluding adoption.
Conclusion:
The broad adoption of wearable technologies appears to depend largely on the scientific community’s ability to successfully address the identified barriers.
Application:
Investigators may use the information provided to develop research studies that better address OSH practitioner concerns and that help technology developers operationalize wearable sensors to improve employee health and well-being.
Keywords: Musculoskeletal Disorders; Physical Ergonomics; Work Measurement; Industrial/workplace ergonomics; Tools, Consumer Products
Précis:
A survey of occupational safety and health professionals was conducted to identify perceived barriers preventing the widespread adoption of wearable sensors as tools for improving employee health and well-being. Findings indicate that the most frequently cited concerns were associated with employee privacy/confidentiality of collected data.
INTRODUCTION
Wearable sensors such as smartwatches and physical fitness monitors are becoming increasingly popular in the United States (Page, 2015; Piwek, Ellis, Andrews, & Joinson, 2016; PwC, 2017). They have been used to support wellness initiatives (Amft & Tröster, 2008; Jakicic et al., 2016; Junker, Amft, Lukowicz, & Tröster, 2008), improve social interaction (Cook, Crandall, Singla, & Thomas, 2010; Eagle & Pentland, 2006; Ploderer, Reitberger, Oinas-Kukkonen, & van Gemert-Pijnen, 2014), and monitor clinical and rehabilitation practices (Appelboom et al., 2014; Bonato, 2010; Patel, Park, Bonato, Chan, & Rodgers, 2012). From an occupational safety and health (OSH) perspective, wearable sensors provide ergonomists a means to unobtrusively capture physical exposure information in the workplace; a problem that has challenged the field for several decades (Garg & Kapellusch, 2009; Marras, Cutlip, Burt, & Waters, 2009). Data from wearable sensors secured to adjacent body segments, for example, can be processed to accurately measure joint angles (Cutti, Giovanardi, Rocchi, Davalli, & Sacchetti, 2008; El-Gohary & McNames, 2015; Kim & Nussbaum, 2013; Lebel, Boissy, Nguyen, & Duval, 2017; Morrow, Lowndes, Fortune, Kaufman, & Hallbeck, 2016; Picerno, 2017; Robert-Lachaine, Mecheri, Larue, & Plamondon, 2016; Seel, Raisch, & Schauer, 2014) and be subsequently used to characterize risk for developing adverse health outcomes such as musculoskeletal disorders (MSDs). Information regarding the intensity of occupational and leisure time physical activity (Hallman, Birk Jørgensen, & Holtermann, 2017), physical fatigue (Maman, Yazdi, Cavuoto, & Megahed, 2017), joint kinetics (Faber, Chang, Kingma, Dennerlein, & van Dieën, 2016; Karatsidis et al., 2016; Kim & Nussbaum, 2013), and repetition (Peppoloni, Filippeschi, Ruffaldi, & Avizzano, 2016; Vignais et al., 2013; Wu, Chen, & Fu, 2016) can also be estimated using wearable sensors located on different body segments. The sensors have been applied in several field-based research studies (Arias, Caban-Martinez, Umukoro, Okechukwu, & Dennerlein, 2015; Ohlendorf et al., 2015; Prairie & Corbeil, 2014; Schall Jr, Fethke, Chen, Oyama, & Douphrate, 2016).
Although current trends suggest that the wearable technology market will continue to grow with further technological advancement (Page, 2015), the vast majority of workplaces have not broadly adopted wearable sensors for improving OSH. Concerns regarding cost, confidentiality of collected data, lack of demonstrated utility, and information overload have each been suggested as potential reasons for their limited adoption in the workplace (Reid et al., 2017). However, very little information is available regarding the safety professional’s perspective, and the authors are aware of few previous studies completed to characterize perceptions of barriers to the adoption of wearable technology in the workplace (Choi, Hwang, & Lee, 2017). The objective of this study was to gather information on the (a) types of wearable sensors, particularly personal activity monitors, currently used by OSH professionals, (b) potential benefits of using such technologies in the workplace, and (c) perceived barriers preventing the widespread adoption of wearable sensors in industry.
METHODS
Survey development
A custom, electronic survey was developed using the Qualtrics (Provo, UT, USA) survey engine (Appendix). Questions regarding basic demographic information including age and gender of the respondent, current occupation and industry sector, years worked in current occupation as well as total years in any OSH-related position, highest degree, and current OSH certifications comprised the first part of the survey. Respondents were then asked a series of questions about the types of wearable devices they use at work and away from work. Questions included listing any personal fitness technologies that they owned (make[s] and model[s]), if they wear any of those technologies at work, and describing what they use their personal fitness technologies for at work (if they reported wearing them at work). Respondents were also asked to estimate what percentage of employees at their workplace use wearable sensors at work (although, not necessarily for work purposes). Finally, respondents were asked a series of questions regarding their perceptions of using wearable devices while at work. Questions included asking if they would be in favor of using wearable technologies at their workplace to track OSH risk factors and ranking the types of risk factors respondents were most interested in capturing at work with a wearable device (among six common ergonomic risk factors potentially capable of being assessed with wearable technologies). Respondents were also asked if they would be interested in using a “dashboard” display to track group or departmental exposures to physical risk factors as well as to describe the single biggest concern with using wearable sensors at their workplace. The survey concluded with a free response section for respondents to list any additional comments they had regarding wearable devices and/or the survey.
Participants
An electronic invitation to the survey was emailed to 28,428 registered members of the American Society of Safety Engineers (ASSE) and 1,302 professionals certified by the Board of Certification in Professional Ergonomics (BCPE). The invitation email described the purpose of the survey and provided a link to the survey’s website (delivered via the Qualtrics survey engine). Potential subjects were informed that the survey should be completed by the person to whom the email was addressed, and that their participation was completely voluntary. Informed consent was obtained from each participant. This research complied with the American Psychological Association Code of Ethics and tenets of the Declaration of Helsinki and was approved by the Institutional Review Board at Auburn University (Protocol #17-007 EX 1702).
Analysis
Descriptive statistics were performed using the Qualtrics survey engine and were used to characterize the frequency and percentage of valid responses from respondents. Open-ended text responses were searched and categorized using combinations of common strings and the logical operators AND and OR. For example, one search string for the question regarding “the single biggest concern regarding use of wearable technology in the workplace” was COST or MONEY or EXPENSE. All categorizations were made following a consensus approach which included three complete passes through all survey responses.
RESULTS
Of the 28,428 email invitations sent to registered ASSE members, 7,867 (27.7%) of the emails were opened and 996 responses were recorded (12.7% of opened emails, 3.5% of emails sent). Of the 1,302 emails sent to BCPE members, 155 responses were recorded (11.9% of emails sent). It is unknown how many emails distributed to BCPE members were opened. Of the 1,151 survey responses, 952 responses were considered sufficiently complete (i.e., valid) for subsequent analyses. Assuming that all BCPE emails were opened, the overall survey yield rate was 10.4% of emails opened and 3.2% of emails sent.
The mean age of the respondents was 48.7 years (SD = 12.2) and 70.4% were male. Characteristics of the respondents are reported in Table 1, including certifications, job titles, industry of employment, highest degree type, and field of study of degree. Respondents tended to be experienced OSH professionals, reporting an average of 19.1 years (SD = 11.6) of experience in an OSH related position and an average of 7.7 years (SD = 7.9) in their current position.
Table 1.
Characteristics of the survey respondents.
| Response Frequency n (%) | |
|---|---|
| Current Job Title | |
| Safety Professional | 554 (58.2) |
| Ergonomist | 91 (9.6) |
| Consultant | 74 (7.8) |
| Manager | 69 (7.3) |
| Industrial Hygienist | 48 (5.0) |
| Other | 116 (12.2) |
| Industry Currently Working | |
| Manufacturing | 244 (25.7) |
| Construction | 117 (12.3) |
| Oil, Energy, or Gas | 84 (8.8) |
| Insurance | 81 (8.5) |
| Academia/Research | 80 (8.4) |
| Government | 67 (7.0) |
| Healthcare | 36 (3.8) |
| Transportation | 20 (2.1) |
| Food Processing | 20 (2.1) |
| Other | 202 (21.2) |
| Highest Degree Received | |
| Doctorate | 88 (9.3) |
| Master’s | 374 (39.5) |
| Bachelor’s | 368 (38.9) |
| Associate’s | 39 (4.1) |
| Some College | 78 (8.2) |
| Field of Study for Highest Degree | |
| Public/Occupational/Environmental Health | 294 (37.2) |
| Science/Technology/Engineering | 242 (30.6) |
| Business/Management | 128 (16.2) |
| Psychology | 33 (4.2) |
| Other | 93 (11.8) |
| Certifications a | |
| Certified Safety Professional | 348 (36.6) |
| Certified Professional Ergonomist | 118 (12.4) |
| Associate Safety Professional | 106 (11.1) |
| Certified Industrial Hygienist | 51 (5.4) |
| Construction Health and Safety Technician | 41 (4.3) |
| Associates in Risk Management | 23 (2.4) |
| Certified Hazardous Materials Manager | 23 (2.4) |
| Occupational Health and Safety Technologist | 23 (2.4) |
| Associate Ergonomics Professional | 22 (2.4) |
| Other | 186 (19.5) |
| None | 130 (13.7) |
| Did not respond to question | 47 (4.9) |
Represents percentage of respondents with certification. Does not sum to 100% as some respondents reported multiple certifications.
Over half of the respondents (50.5%; 481 of 952) who answered the question “do you own any personal fitness technologies (e.g., Fitbit, Garmin, Polar, etc.)?” reported owning at least one device. Of those that responded yes, 75.1% (361 of 481) reported wearing at least one of their devices while at work. The most common reason for wearing the device at work was to monitor personal activity (e.g., “count steps”) and remind them to be more active at work (90.4%; 319 of 353 respondents to this question). Overall, respondents estimated that 27.9% (SD = 21.4) of employees at their facility used wearable technologies while at work; however, not necessarily for work purposes. Over half of the respondents (53.5%; 509 of 952) indicated that they would be in favor of using wearable technologies at their workplace to track relevant metrics for several common OSH risk factors. An additional 27.3% of respondents expressed that they might be interested in using wearable technologies at their workplace to track relevant metrics for OSH risk factors. Respondents estimated that their organization would be willing to spend an average of $72.21 (SD = $67.78) per person for a wearable device.
Table 2 describes the results for select survey items characterized by industry sectors with at least 20 respondents. Industry specific responses were generally consistent with those of the entire sample. Respondents working in the food processing industry reported owning fewer personal fitness technologies than any other industry and were second least in favor (just behind the healthcare industry) of using wearable technologies at work to track OSH relevant risk factors. Respondents in the food processing industry also estimated that their organization would be willing to spend less per person for a wearable device ($52.68) than any other industry. Conversely, respondents in the transportation ($83.18) and oil, energy, or gas ($86.9) industries estimated that their organization would be willing to spend more per person for wearable devices than the other industries.
Table 2.
Responses by industry sector for select survey questions.
| Own a personal fitness technology | Wear their personal fitness technology at work | In favor of using wearable technologies at work to track OSH risk factors | Estimated amount (in US $) that their organization would be willing to spend per person for a wearable device | ||
|---|---|---|---|---|---|
| Industry Sector | N | n (%) | n (%) | n (%) | mean (SD) |
| Manufacturing | 244 | 122 (50.0) | 92 (75.4) | 132 (54.1) | 68.67 (61.4) |
| Construction | 117 | 47 (40.2) | 33 (70.2) | 67 (57.3) | 63.17 (49.1) |
| Oil, Energy, or Gas | 84 | 42 (50.0) | 30 (71.4) | 44 (52.4) | 86.90 (73.1) |
| Insurance | 81 | 47 (58.0) | 32 (68.1) | 40 (49.4) | 72.81 (62.8) |
| Academia/Research | 80 | 47 (58.8) | 39 (83.0) | 45 (56.3) | 64.39 (68.4) |
| Government | 67 | 27 (40.3) | 18 (66.7) | 40 (59.7) | 74.72 (76.6) |
| Healthcare | 36 | 20 (55.6) | 15 (75.0) | 14 (38.9) | 64.81 (64.3) |
| Transportation | 20 | 12 (60.0) | 10 (83.3) | 12 (60.0) | 83.18 (74.0) |
| Food Processing | 20 | 8 (40.0) | 7 (87.5) | 8 (40.0) | 52.68 (35.6) |
Note. OSH = occupational safety and health.
Tables 3 describes the risk factors respondents selected as those they would be the most interested in capturing with wearable sensors in the workplace. Capturing exposure to awkward postures and forceful exertions had the lowest average ranks (i.e., were of greatest interest to respondents), followed by repetition and physical fatigue. Mental fatigue and vibration were the risk factors of least interest in being captured. An industry specific breakdown of the average ranks is presented in Table 4. Not surprisingly, the lowest average rank (i.e., greatest interest to respondents) of all industry sector risk factors was repetition in the food processing industry. The highest average rank (i.e., least interest to respondents) was observed for vibration among respondents in the healthcare industry. Interestingly, despite the documented association between whole-body vibration and MSDs common to transportation, respondents in the transportation sector listed vibration last among all risk factors they would be interested in capturing with a wearable sensor at their place of work. Physical and mental fatigue were the two risk factors of greatest interest in that sector.
Table 3.
Risk factors selected as those respondents would be most interested in capturing with a wearable sensor at their workplace.
| Rank | Avg. | 1 | 2 | 3 | 4 | 5 | 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk Factor | Rank | % | n | % | n | % | n | % | n | % | n | % | n | |
| 1 | Awkward Postures | 2.7 | 22.8 | 209 | 28.1 | 258 | 21.4 | 196 | 15.8 | 145 | 7.2 | 66 | 4.8 | 44 |
| 2 | Forceful Exertions | 2.8 | 29.3 | 269 | 20.3 | 186 | 19.8 | 182 | 11.7 | 107 | 13.1 | 120 | 5.9 | 54 |
| 3 | Repetition | 3.1 | 19.2 | 176 | 20.0 | 184 | 22.8 | 209 | 17.4 | 160 | 14.4 | 132 | 6.2 | 57 |
| 4 | Physical Fatigue | 3.3 | 15.4 | 141 | 16.1 | 148 | 18.6 | 171 | 26.9 | 247 | 19.2 | 176 | 3.8 | 35 |
| 5 | Mental Fatigue | 4.2 | 10.8 | 99 | 10.5 | 96 | 9.7 | 89 | 13.7 | 126 | 23.8 | 218 | 31.6 | 290 |
| 6 | Vibration | 4.9 | 2.6 | 24 | 5.0 | 46 | 7.7 | 71 | 14.5 | 133 | 22.4 | 206 | 47.7 | 438 |
Note. Rank of 1 = most interested; Rank of 6 = least interested.
Table 4.
Average rank for risk factors selected as those respondents would be most interested in capturing with a wearable sensor at their workplace by industry.
| Rank | Average Rank | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Risk Factor | Manufacturing | Healthcare | Food Processing | Insurance | Academia/ Research | Construction | Oil, Energy, or Gas | Transportation | Government | |
| 1 | Awkward Postures | 2.6 | 2.1 | 2.4 | 2.3 | 2.6 | 3.5 | 3.0 | 3.1 | 2.5 |
| 2 | Forceful Exertions | 2.6 | 3.0 | 2.3 | 2.9 | 3.1 | 2.7 | 2.5 | 3.2 | 2.8 |
| 3 | Repetition | 2.9 | 2.7 | 1.8 | 2.8 | 3.1 | 3.4 | 3.9 | 4.4 | 3.0 |
| 4 | Physical Fatigue | 3.6 | 3.6 | 4.2 | 3.6 | 3.3 | 2.9 | 2.9 | 2.5 | 3.5 |
| 5 | Mental Fatigue | 4.6 | 4.1 | 5.0 | 4.2 | 3.8 | 4.2 | 3.7 | 2.8 | 4.2 |
| 6 | Vibration | 4.8 | 5.6 | 5.3 | 5.1 | 5.1 | 4.4 | 5.0 | 5.1 | 4.9 |
Note. Rank of 1 = most interested; Rank of 6 = least interested.
When asked to describe their single greatest concern with using wearable sensors at their workplace, respondents indicated that employee privacy/confidentiality was the most frequently cited obstacle (Figure 1). Issues related to employee compliance with wearing the devices as trained, sensor durability, the cost/benefit of the devices, and good manufacturing practice (GMP) standards were also described. Respondents in the food processing, general manufacturing, transportation, and construction sectors cited common concerns with sensor durability while government, academia/research, and insurance cited employee privacy concerns most frequently (Figure 2). Respondents in the oil, energy, or gas industry frequently cited concerns regarding the safety of the devices for their work environments.
Figure 1.
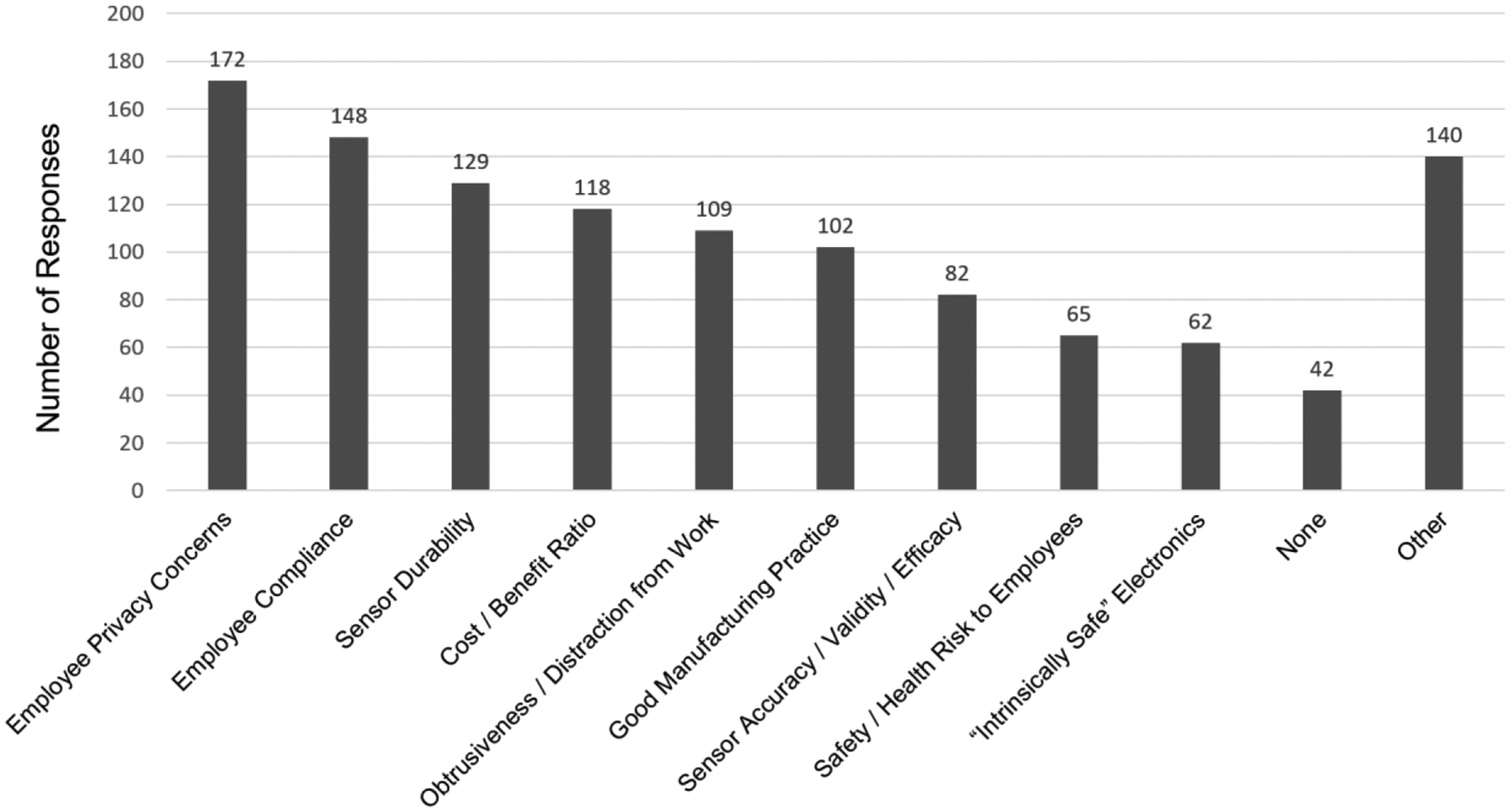
Single greatest concern regarding use of wearable technology in the workplace.
Figure 2.
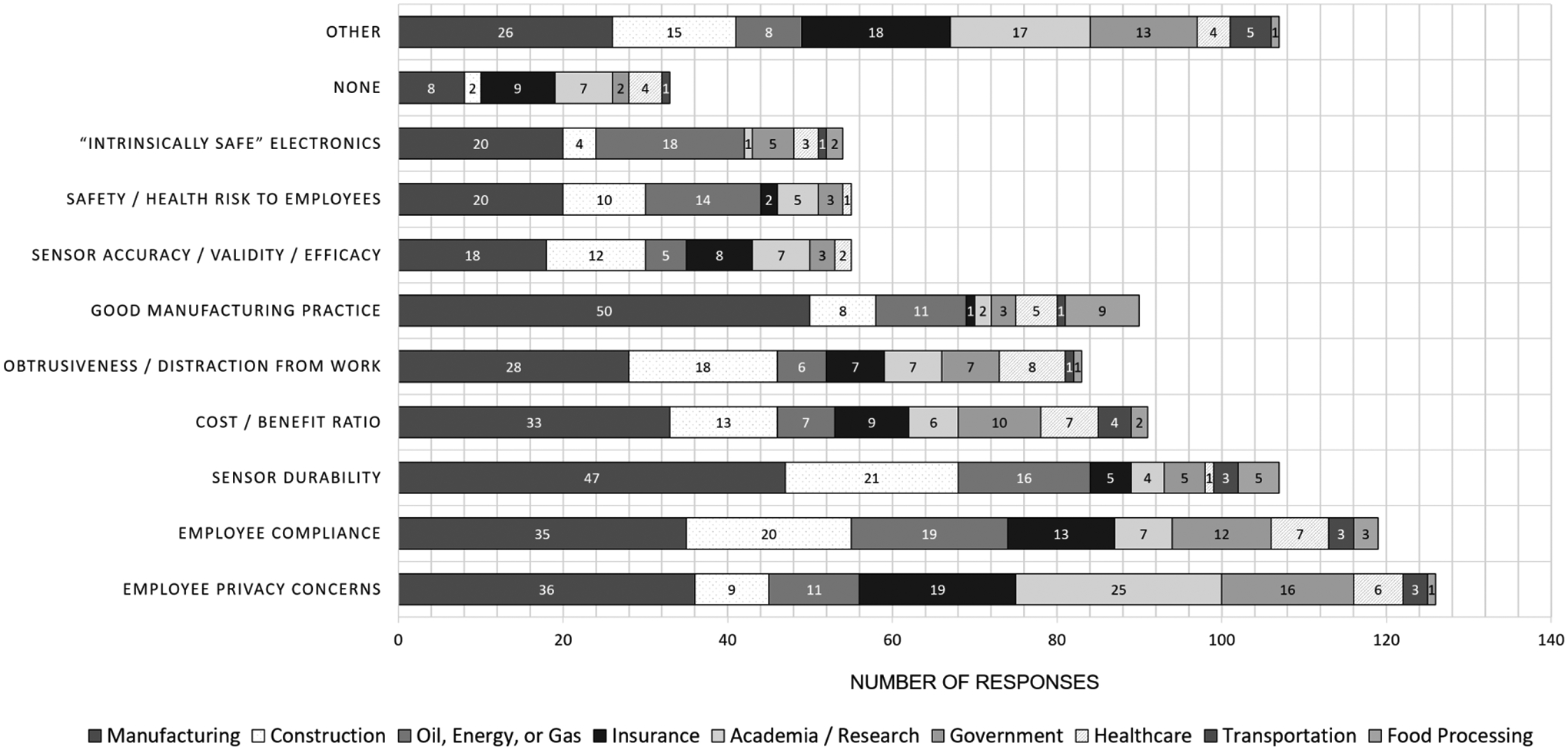
Single greatest concern regarding use of wearable technology in the workplace by industry sector.
The majority of respondents (58.3%, 550 of 944) expressed an interest in using a “dashboard” display to track group or department exposures to physical risk factors at their workplace. An additional 28.4% of respondents expressed that they might be interested in using a “dashboard” display in the work environment. The remaining 13.3% of respondents were against the use of a “dashboard” in the work environment for reasons largely consistent with those described for not using wearables in the workplace in general (e.g., confidentiality, compliance, maintaining devices, safety, etc.).
DISCUSSION
The majority of OSH professionals surveyed in this study indicated that they were in favor of using wearable technologies to objectively measure aspects of employee health risk while at work. Not surprisingly, exposure to awkward postures, forceful exertions, and repetition, three common physical risk factors associated with the development of work-related musculoskeletal health outcomes (da Costa & Vieira, 2010; van Rijn, Huisstede, Koes, & Burdorf, 2010), were identified as the risk factors the OSH professionals were most interested in capturing. Recent research has indicated that wearable sensors may be used to accurately and reliably quantify kinematics necessary to estimate exposure to non-neutral working postures (Cutti et al., 2008; El-Gohary & McNames, 2015; Kim & Nussbaum, 2013; Lebel et al., 2017; Morrow et al., 2016; Picerno, 2017; Robert-Lachaine et al., 2016; Seel et al., 2014) and assist in the assessment of repetitive motions (Peppoloni et al., 2016; Vignais et al., 2013; Wu et al., 2016). Robust, repeatable calibration procedures have been identified and continue to undergo evaluation to assist in the accurate ascertainment of such measures (Ligorio, Zanotto, Sabatini, & Agrawal, 2017; Robert-Lachaine, Mecheri, Larue, & Plamondon, 2017). While force has been more difficult to assess, wearable sensors have been successfully applied to estimate joint forces and moments during occupationally-relevant activities such as manual material handling (Faber et al., 2016; Kim & Nussbaum, 2013, 2014), gait (Chen, Lach, Lo, & Yang, 2016; Karatsidis et al., 2016; Tao, Liu, Zheng, & Feng, 2012), and extravehicular activity (McFarland & Nguyen, 2017; Reid & McFarland, 2015). Smart textiles (Stoppa & Chiolerio, 2014) and other promising wearables that combine accelerometer and gyroscope measurements with surface electrophysiological sensors (e.g., the BioStampRC, MC10 Inc., Cambridge, MA; Jang et al., 2016; Patel et al., 2016), may provide practitioners methods for unobtrusively estimating force using methods that have been largely limited to research and laboratory settings.
Despite the growing body of evidence suggesting that wearable technologies are both accurate and reliable for assessing exposure to physical risk factors of interest, a large contingent of respondents still acknowledged concerns regarding the validity and overall efficacy of wearable technologies. One explanation for the lack of confidence in the technologies may be related to a lack of experience using wearable devices to assess kinematics beyond common physical activity metrics such as step counts. The overwhelming majority of respondents described that their primary motivation for using their personal activity monitor at work was to track their physical activity. Fitbit devices were the most common personal activity monitor owned (58.1% of 339 responses). While variations of the Fitbit have been observed to be valid and reliable for measuring step counts (Evenson, Goto, & Furberg, 2015) and have also been observed to be well accepted and associated with increased physical activity (Cadmus-Bertram, Marcus, Patterson, Parker, & Morey, 2015), the focus of such devices has not been on measuring physical risk factors such as exposure to non-neutral postures. Additional research establishing the efficacy of the most common wearable devices may be beneficial. Development of more practitioner-friendly sensor protocols and broader dissemination of the knowledge regarding the capabilities of “research-grade” wearable technologies is also needed to improve adoption.
Although sensor efficacy and validity were common concerns, the most frequently cited concern of the survey respondents was that employees may react negatively to a perception of being monitored. Twenty-three responses explicitly used the term big brother when describing their apprehension. The second most frequently cited concern was that employees may not comply with organizational guidelines of how and when to wear the devices, potentially in an act of retaliation for having their privacy disrupted. Interestingly, these two issues appear to conflict with recent research indicating that employees welcome greater employer engagement in their personal health, particularly personalized guidance in workplace health promotion programs (McCleary et al., 2017). Along these lines, 49% of respondents in a recent survey conducted by PricewaterhouseCoopers believed that wearable technology would increase workplace efficiency (PwC, 2017). These conflicting results contribute to a growing body of evidence suggesting a paradoxical relationship between information privacy and behavior (Norberg, Horne, & Horne, 2007; Piwek et al., 2016; Smith, Dinev, & Xu, 2011). Further research is needed to gain a greater understanding of user privacy concerns associated with the use of wearable devices in the workplace. Mitigation strategies must also be developed as further insights into privacy concerns are realized.
Current wearables may be more effectively applied in a supportive role in which employees do not share their collected data with their employer (Lidynia, Brauner, & Ziefle, 2017). Workplace health promotion programs that uses wearable devices to promote physical activity, but allow employee participation and data sharing to be optional may be one approach. Interestingly, only nine respondents (0.3%) in this study explicitly reported using wearable technology as a component of a workplace wellness program designed to improve employee health. The relative infancy of non-invasive, cost effective wearable sensors may partially explain the limited number of comments related to using wearables as a component of a workplace health promotion program. Another potential reason may be that many organizations execute their wellness programs through their Human Resources department rather than an OSH department. The surveyed OSH professionals may have been less aware of potential programs offered by their Human Resources department. A “Total Worker Health” approach that integrates employee health protection and health promotion through the application of wearable technologies may be more effective (Schill & Chosewood, 2013). Additional research is needed, however, to evaluate the efficacy of workplace wellness programs that use wearable technologies as well as the efficacy of “Total Worker Health” approaches in general (Anger et al., 2015). Studies examining user perceptions pre- and post-introduction of wearable technologies in the workplace would also be valuable to better understand the apparent paradox that surrounds using wearable devices to improve OSH.
Several limitations of this study should be considered when interpreting the results. The use of self-reported responses may have introduced bias. Specifically, it is plausible that the respondents were more interested in wearable technologies and, therefore, more likely to respond than those uninterested in wearable technologies. The relatively low response rate (3.2% of emails sent, 10.4% of emails read) limits the generalizability of the results. In particular, industry specific results may be affected by a relatively small number of respondents from that industry. Furthermore, the targeted respondents were OSH professionals whose acceptance of programs that use wearable sensors would likely be necessary for successful implementation. In addition to OSH professionals, senior managers as well as the employees that would wear the devices themselves should be surveyed. It may also be difficult for safety professionals to estimate the percentage of workers who may use wearable technologies in the workplace as many are not worn in visible locations. However, even crude estimates of the current use of wearable technologies may be suggestive of the overall willingness of employees to use wearable technologies for safety-related purposes. Finally, the term wearable technology is rather broad and refers to many forms of technology. Although we did not provide a specific definition of wearable technology and/or personal activity monitors to respondents, some questions and the list of possible responses provided context to the respondents that we were generally defining wearable technologies in this study as devices similar to personal activity monitors. Additional research is needed to evaluate perceptions of using other forms of wearable technology such as augmented reality headsets (Kim, Nussbaum, & Gabbard, 2016; Wiedenmaier, Oehme, Schmidt, & Luczak, 2003), exoskeletons (Bosch, van Eck, Knitel, & de Looze, 2016; De Looze, Bosch, Krause, Stadler, & O’Sullivan, 2016; de Looze, Krause, & O’Sullivan, 2017), and smartphones (Amick, Chaparro, Patterson, & Jorgensen, 2015; Boissy et al., 2017; Nath, Akhavian, & Behzadan, 2017; Yang, Grooten, & Forsman, 2017) in the workplace as their functionality and practicality continues to increase.
Supplementary Material
PRACTICAL IMPLICATIONS.
Wearable sensors will continue to evolve as technology advances and computing power increases. The potential benefits of using wearable sensors in the workplace include reduced risk of injury and illness and increased employee satisfaction, wellness, and productivity. The broad adoption of wearable technologies, however, largely depends on the scientific community’s ability to successfully address barriers regarding privacy/confidentiality of collected data, employee compliance, sensor durability, GMP standards, and ensuring a positive cost/benefit outcome for organizations considering their use. Opportunities for additional research include developing less obtrusive, practitioner-friendly sensors with easy-to-use calibration protocols and associated algorithms. The OSH community must gain a greater understanding of user privacy concerns to develop strategies to meaningfully address them. A better understanding of implementation barriers will contribute to better workplace policies and programs that simultaneously promote injury and illness prevention and worker well-being.
KEY POINTS.
Eighty-one percent of respondents would consider using wearables to help track risk factors at work.
Fifty-one percent of respondents reported owning at least one wearable device.
Seventy-five percent of those who owned a device reported wearing the device while at work.
Concerns regarding privacy were the most frequently cited barrier preventing adoption.
Respondents estimated that their organization would spend an average of $72 per person per wearable.
Acknowledgments:
This study was supported by the American Society for Safety Engineers (ASSE) Foundation grant entitled “ASSIST: Advancing Safety Surveillance using Individualized Sensor Technology”. The study was also supported by the Deep South Center for Occupational Health and Safety Education Research Center (Grant: 2 T42 OH008436-13). The authors would like to acknowledge the American Society for Safety Engineers (ASSE) and Board of Certification in Professional Ergonomics (BCPE) for their assistance distributing this survey.
Contributor Information
Mark C. Schall, Jr., Auburn University, Department of Industrial and Systems Engineering, 3323E Shelby Center for Engineering Technology, Auburn, AL 36849.
Richard F. Sesek, Auburn University, Department of Industrial and Systems Engineering, 3341-A Shelby Center for Engineering Technology, Auburn, AL 36849.
Lora A. Cavuoto, University at Buffalo, State University of New York, Department of Industrial and Systems Engineering, 324 Bell Hall, Buffalo, NY 14260.
References
- Amft O, & Tröster G (2008). Recognition of dietary activity events using on-body sensors. Artificial intelligence in medicine, 42(2), 121–136. [DOI] [PubMed] [Google Scholar]
- Amick RZ, Chaparro A, Patterson JA, & Jorgensen MJ (2015). Test-retest reliability of the sway balance mobile application. Journal of Mobile Technology in Medicine, 4(2), 40–47. [Google Scholar]
- Anger WK, Elliot DL, Bodner T, Olson R, Rohlman DS, Truxillo DM, et al. (2015). Effectiveness of Total Worker Health Interventions. Journal of Occupational Health Psychology, 20(2), 226–247. [DOI] [PubMed] [Google Scholar]
- Appelboom G, Camacho E, Abraham ME, Bruce SS, Dumont EL, Zacharia BE, et al. (2014). Smart wearable body sensors for patient self-assessment and monitoring. Archives of Public Health, 72(1), 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias OE, Caban-Martinez AJ, Umukoro PE, Okechukwu CA, & Dennerlein JT (2015). Physical activity levels at work and outside of work among Commercial Construction Workers. Journal of Occupational and Environmental Medicine, 57(1), 73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boissy P, Diop-Fallou S, Lebel K, Bernier M, Balg F, & Tousignant-Laflamme Y (2017). Trueness and Minimal Detectable Change of Smartphone Inclinometer Measurements of Shoulder Range of Motion. Telemedicine and e-Health, 23(6), 503–506. [DOI] [PubMed] [Google Scholar]
- Bonato P (2010). Wearable sensors and systems. IEEE Engineering in Medicine and Biology Magazine, 29(3), 25–36. [DOI] [PubMed] [Google Scholar]
- Bosch T, van Eck J, Knitel K, & de Looze M (2016). The effects of a passive exoskeleton on muscle activity, discomfort and endurance time in forward bending work. Applied ergonomics, 54, 212–217. [DOI] [PubMed] [Google Scholar]
- Cadmus-Bertram LA, Marcus BH, Patterson RE, Parker BA, & Morey BL (2015). Randomized trial of a Fitbit-based physical activity intervention for women. American journal of preventive medicine, 49(3), 414–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Lach J, Lo B, & Yang G-Z (2016). Toward pervasive gait analysis with wearable sensors: a systematic review. IEEE journal of biomedical and health informatics, 20(6), 1521–1537. [DOI] [PubMed] [Google Scholar]
- Choi B, Hwang S, Lee S (2017). What drives construction workers’ acceptance of wearable technologies in the workplace? Indoor localization and wearable health devices for occupational safety and health. Automation in Construction, 84, 31–41. [Google Scholar]
- Cook DJ, Crandall A, Singla G, & Thomas B (2010). Detection of social interaction in smart spaces. Cybernetics and Systems: An International Journal, 41(2), 90–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutti AG, Giovanardi A, Rocchi L, Davalli A, & Sacchetti R (2008). Ambulatory measurement of shoulder and elbow kinematics through inertial and magnetic sensors. Medical & biological engineering & computing, 46(2), 169–178. [DOI] [PubMed] [Google Scholar]
- da Costa BR, & Vieira ER (2010). Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. American Journal of Industrial Medicine, 53(3), 285–323. [DOI] [PubMed] [Google Scholar]
- De Looze MP, Bosch T, Krause F, Stadler KS, & O’Sullivan LW (2016). Exoskeletons for industrial application and their potential effects on physical work load. Ergonomics, 59(5), 671–681. [DOI] [PubMed] [Google Scholar]
- de Looze MP, Krause F, & O’Sullivan LW (2017). The Potential and Acceptance of Exoskeletons in Industry. In Wearable Robotics: Challenges and Trends (pp. 195–199): Springer. [Google Scholar]
- Eagle N, & Pentland AS (2006). Reality mining: sensing complex social systems. Personal and ubiquitous computing, 10(4), 255–268. [Google Scholar]
- El-Gohary M, & McNames J (2015). Human joint angle estimation with inertial sensors and validation with a robot arm. Biomedical Engineering, IEEE Transactions on, 62(7), 1759–1767. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Goto MM, & Furberg RD (2015). Systematic review of the validity and reliability of consumer-wearable activity trackers. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faber G, Chang C, Kingma I, Dennerlein J, & van Dieën J (2016). Estimating 3D L5/S1 moments and ground reaction forces during trunk bending using a full-body ambulatory inertial motion capture system. Journal of biomechanics, 49(6), 904–912. [DOI] [PubMed] [Google Scholar]
- Garg A, & Kapellusch JM (2009). Applications of biomechanics for prevention of work-related musculoskeletal disorders. Ergonomics, 52(1), 36–59. [DOI] [PubMed] [Google Scholar]
- Hallman DM, Birk Jørgensen M, & Holtermann A (2017). Objectively measured physical activity and 12-month trajectories of neck–shoulder pain in workers: A prospective study in DPHACTO. Scandinavian Journal of Public Health, 45(3), 288–298. [DOI] [PubMed] [Google Scholar]
- Jakicic JM, Davis KK, Rogers RJ, King WC, Marcus MD, Helsel D, et al. (2016). Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: the IDEA randomized clinical trial. Jama, 316(11), 1161–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang KI, Jung HN, Lee JW, Xu S, Liu YH, Ma Y, et al. (2016). Ferromagnetic, Folded Electrode Composite as a Soft Interface to the Skin for Long‐Term Electrophysiological Recording. Advanced Functional Materials, 26(40), 7281–7290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junker H, Amft O, Lukowicz P, & Tröster G (2008). Gesture spotting with body-worn inertial sensors to detect user activities. Pattern Recognition, 41(6), 2010–2024. [Google Scholar]
- Karatsidis A, Bellusci G, Schepers HM, de Zee M, Andersen MS, & Veltink PH (2016). Estimation of ground reaction forces and moments during gait using only inertial motion capture. Sensors, 17(1), 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S, & Nussbaum MA (2013). Performance evaluation of a wearable inertial motion capture system for capturing physical exposures during manual material handling tasks. Ergonomics, 56(2), 314–326. [DOI] [PubMed] [Google Scholar]
- Kim S, & Nussbaum MA (2014). An evaluation of classification algorithms for manual material handling tasks based on data obtained using wearable technologies. Ergonomics, 57(7), 1040–1051. [DOI] [PubMed] [Google Scholar]
- Kim S, Nussbaum MA, & Gabbard JL (2016). Augmented Reality “Smart Glasses” in the Workplace: Industry Perspectives and Challenges for Worker Safety and Health. IIE transactions on occupational ergonomics and human factors, 4(4), 253–258. [Google Scholar]
- Lebel K, Boissy P, Nguyen H, & Duval C (2017). Inertial measurement systems for segments and joints kinematics assessment: towards an understanding of the variations in sensors accuracy. Biomedical engineering online, 16(1), 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidynia C, Brauner P, & Ziefle M (2017). A Step in the Right Direction–Understanding Privacy Concerns and Perceived Sensitivity of Fitness Trackers. In: Ahram T, Falcão C (eds) Advances in Human Factors in Wearable Technologies and Game Design. AHFE 2017. Advances in Intelligent Systems and Computing, vol 608. Springer, Cham [Google Scholar]
- Ligorio G, Zanotto D, Sabatini A, & Agrawal S (2017). A novel functional calibration method for real-time elbow joint angles estimation with magnetic-inertial sensors. Journal of Biomechanics, 54, 106–110. [DOI] [PubMed] [Google Scholar]
- Maman ZS, Yazdi MAA, Cavuoto LA, & Megahed FM (2017). A data-driven approach to modeling physical fatigue in the workplace using wearable sensors. Applied Ergonomics, 65, 515–529. [DOI] [PubMed] [Google Scholar]
- Marras WS, Cutlip RG, Burt SE, & Waters TR (2009). National occupational research agenda (NORA) future directions in occupational musculoskeletal disorder health research. Applied ergonomics, 40(1), 15–22. [DOI] [PubMed] [Google Scholar]
- McCleary K, Goetzel RZ, Roemer EC, Berko J, Kent K, & De La Torre H (2017). Employer and Employee Opinions About Workplace Health Promotion (Wellness) Programs: Results of the 2015 Harris Poll Nielsen Survey. Journal of Occupational and Environmental Medicine, 59(3), 256–263. [DOI] [PubMed] [Google Scholar]
- McFarland S & Nguyen D (2017). Analysis of Potential Glove-Induced Hand Injury Metrics During Typical Neutral Buoyancy Training Operations. Paper presented at the 47th International Conference on Environmental Systems (ICES), Charleston, S.C. [Google Scholar]
- Morrow MM, Lowndes B, Fortune E, Kaufman KR, & Hallbeck S (2016). Validation of Inertial Measurement Units for Upper Body Kinematics. Journal of applied biomechanics, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nath ND, Akhavian R, & Behzadan AH (2017). Ergonomic analysis of construction worker’s body postures using wearable mobile sensors. Applied Ergonomics, 62, 107–117. [DOI] [PubMed] [Google Scholar]
- Norberg PA, Horne DR, & Horne DA (2007). The privacy paradox: Personal information disclosure intentions versus behaviors. Journal of Consumer Affairs, 41(1), 100–126. [Google Scholar]
- Ohlendorf D, Schwarzer M, Rey J, Hermanns I, Nienhaus A, Ellegast R, et al. (2015). Medical work assessment in German hospitals: a study protocol of a movement sequence analysis (MAGRO-MSA). Journal of Occupational Medicine and Toxicology, 10(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page T (2015). A Forecast of the Adoption of Wearable Technology. International Journal of Technology Diffusion (IJTD), 6(2), 12–29. [Google Scholar]
- Patel S, McGinnis RS, Silva I, DiCristofaro S, Mahadevan N, Jortberg E, et al. (2016). A wearable computing platform for developing cloud-based machine learning models for health monitoring applications. Paper presented at the 38th Annual International Conference of the Engineering in Medicine and Biology Society (EMBC). [DOI] [PubMed] [Google Scholar]
- Patel S, Park H, Bonato P, Chan L, & Rodgers M (2012). A review of wearable sensors and systems with application in rehabilitation. Journal of neuroengineering and rehabilitation, 9(1), 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peppoloni L, Filippeschi A, Ruffaldi E, & Avizzano C (2016). A novel wearable system for the online assessment of risk for biomechanical load in repetitive efforts. International Journal of Industrial Ergonomics, 52, 1–11. [Google Scholar]
- Picerno P (2017). 25 years of lower limb joint kinematics by using inertial and magnetic sensors: A review of methodological approaches. Gait & posture, 51, 239–246. [DOI] [PubMed] [Google Scholar]
- Piwek L, Ellis DA, Andrews S, & Joinson A (2016). The rise of consumer health wearables: promises and barriers. PLoS Medicine, 13(2), e1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ploderer B, Reitberger W, Oinas-Kukkonen H, & van Gemert-Pijnen J (2014). Social interaction and reflection for behaviour change: Springer. [Google Scholar]
- Prairie J, & Corbeil P (2014). Paramedics on the job: Dynamic trunk motion assessment at the workplace. Applied ergonomics, 45(4), 895–903. [DOI] [PubMed] [Google Scholar]
- PwC P (2017). The Wearable Life 2.0: Connected living in a wearable world.
- Reid CR, Schall MC Jr, Amick RZ, Schiffman JM, Lu M-L, Smets M, et al. (2017). Wearable Technologies: How Will We Overcome Barriers to Enhance Worker Performance, Health, And Safety? Paper presented at the Human Factors and Ergonomics Society’s 2017 International Annual Meeting, Austin, TX. [Google Scholar]
- Reid CR, & McFarland SM (2015). Feasibility Assessment of an Extravehicular Activity Glove Sensing Platform to Evaluate Potential Hand Injury Risk Factors. Paper presented at the 45th International Conference on Environmental Systems (ICES); Bellevue, WA; United States. [Google Scholar]
- Robert-Lachaine X, Mecheri H, Larue C, & Plamondon A (2016). Validation of inertial measurement units with an optoelectronic system for whole-body motion analysis. Medical & Biological Engineering & Computing, 1–11. [DOI] [PubMed] [Google Scholar]
- Robert-Lachaine X, Mecheri H, Larue C, & Plamondon A (2017). Accuracy and repeatability of single-pose calibration of inertial measurement units for whole-body motion analysis. Gait & Posture, 54, 80–86. [DOI] [PubMed] [Google Scholar]
- Schall MC Jr, Fethke NB, Chen H, Oyama S, & Douphrate DI (2016). Accuracy and repeatability of an inertial measurement unit system for field-based occupational studies. Ergonomics, 59(4), 591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schill AL, & Chosewood LC (2013). The NIOSH Total Worker Health™ program: an overview. Journal of Occupational and Environmental Medicine, 55, S8–S11. [DOI] [PubMed] [Google Scholar]
- Seel T, Raisch J, & Schauer T (2014). IMU-based joint angle measurement for gait analysis. Sensors, 14(4), 6891–6909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith HJ, Dinev T, & Xu H (2011). Information privacy research: an interdisciplinary review. MIS quarterly, 35(4), 989–1016. [Google Scholar]
- Stoppa M, & Chiolerio A (2014). Wearable electronics and smart textiles: a critical review. Sensors, 14(7), 11957–11992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao W, Liu T, Zheng R, & Feng H (2012). Gait analysis using wearable sensors. Sensors, 12(2), 2255–2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rijn RM, Huisstede BMA, Koes BW, & Burdorf A (2010). Associations between work-related factors and specific disorders of the shoulder – a systematic review of the literature. Scandinavian Journal of Work, Environment and Health, 36(3), 189–201. [DOI] [PubMed] [Google Scholar]
- Vignais N, Miezal M, Bleser G, Mura K, Gorecky D, & Marin F (2013). Innovative system for real-time ergonomic feedback in industrial manufacturing. Applied ergonomics, 44(4), 566–574. [DOI] [PubMed] [Google Scholar]
- Wiedenmaier S, Oehme O, Schmidt L, & Luczak H (2003). Augmented reality (AR) for assembly processes design and experimental evaluation. International journal of Human-Computer interaction, 16(3), 497–514. [Google Scholar]
- Wu Y, Chen K, & Fu C (2016). Natural Gesture Modeling and Recognition Approach Based on Joint Movements and Arm Orientations. IEEE Sensors Journal, 16(21), 7753–7761. [Google Scholar]
- Yang L, Grooten WJ, & Forsman M (2017). An iPhone application for upper arm posture and movement measurements. Applied Ergonomics, 65, 492–500. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


