Abstract
Context:
It is well established that rural communities face geographic and socioeconomic challenges linked to higher rates of health disparities across the United States, though the coronavirus disease 2019 (COVID-19) impact on rural communities is less certain.
Objective:
To understand the COVID-19 pandemic's impact on rural communities in Tennessee, investigate differences in rural-urban mortality rates after controlling for confounding variables, and inform state pandemic response policy.
Design:
A cross-sectional analysis of cumulative COVID-19 morality rates.
Setting/Participants:
Tennessee county-level COVID-19 mortality data from March 1, 2020, to January 31, 2021, were matched with county-level sociodemographic and health data from public datasets: Agency for Healthcare Research and Quality Social Determinants of Health, PLACES: Local Data for Better Health County Data, and the US Census Bureau. County status was defined using the 2013 National Center for Health Statistics Urban-Rural Classification.
Main Outcome Measures:
A negative binomial regression model estimated adjusted incidence rate ratio and 95% confidence intervals (CI) for rural compared with urban mortality. Unadjusted rate ratios and rate differences for COVID-19 mortality in rural versus urban counties were compared with those for influenza and pneumonia and all-cause mortality over the past 5 years.
Results:
During the study period, 9650 COVID-19 deaths occurred across 42 urban and 53 rural counties. Controlling for county-level sociodemographic characteristics, health care access, and comorbidities, incidence rate ratio was 1.13 (95% CI, 1.00-1.28, P < .05) for rural as compared with urban deaths. Unadjusted COVID-19 mortality risk difference between rural and urban counties was greater (61.85, 95% CI, 54.31-69.31) than 5-year influenza and pneumonia rural-urban risk difference (12.57, 95% CI, 11.16-13.00) during 2015-2019.
Conclusions:
COVID-19 mortality rates were greater for populations living in Tennessee's rural as compared with urban counties during the study period. This differential impact must be considered in public health decision making to mitigate COVID-19.
Keywords: COVID-19, health disparities, mortality rates, rural health
The United States faces geographical disparities in health and disease. Reduction of health inequities, including those between rural and urban counties, remains an important public health policy goal and an emphasis of the Centers for Disease Control and Prevention's (CDC) health equity strategy.1–3 Since the first documented case of COVID-19 in the United States in January 2020, weekly incidence has differed between urban and rural areas.4 Early in the pandemic, from mid-March to mid-May 2020, cumulative incidence was highest among residents of large urban areas where the virus was initially introduced. As the course of the pandemic progressed, however, cumulative incidence increased steadily in rural areas,4 followed closely by rising mortality rates.5
Rural communities make up a sizeable proportion in many states. This includes Tennessee, with a majority of the land area and approximately 22% of the resident population in rural areas in 2019.6 Tennessee has notable differences between urban and rural communities in population size, demographics, culture, infrastructure, and population health. Health care access also varies; rural hospital access has declined over recent years, including throughout the COVID-19 pandemic. Like other southern US states, Tennessee has seen a large effect from rural hospital closures, losing 9 hospitals over the last 5 years alone.7 Due in part to geographic and socioeconomic challenges, many rural communities experience higher rates of health disparities (including COVID-19 mortality differences) attributed to socioeconomic status,8 racial disparities,9,10 social determinants of health,11,12 age differences,13 and urbanization patterns.14
To provide additional insight into rural communities' vulnerability to COVID-19, influenza and pneumonia death rates can serve as a historical comparator in rural regions. Commonly observed clinical signs in COVID-19 (eg, fever, cough, shortness of breath) are similar to those of other respiratory viral diseases including influenza.15 In addition, there are also similarities in the modes of transmission and populations at highest risk.16 Previous studies have identified rural-urban disparities in influenza and pneumonia mortality rates; these have widened over time, with rural areas showing increased mortality from influenza and pneumonia.17 While rural-urban inequalities in COVID-19 mortality rates might reflect disparities across multiple factors, we expect some of these factors to be similar when comparing differences in rural-urban mortality rates for COVID-19 with influenza and pneumonia.
To better characterize the effects of the COVID-19 pandemic on communities in Tennessee and address rural health concerns, we investigated differences in urban and rural mortality rates attributed to COVID-19 prior to widespread COVID-19 vaccine availability. We compared differences in COVID-19 mortality rates for the study period with influenza and pneumonia mortality and all-cause mortality rates from 2015 to 2019 by county type, respectively, for additional insight into understanding rural community vulnerability. Our objective was to further inform current and future state health policy decisions and provide data for public health planning, resource allocation, equitable vaccine distribution, and future response efforts.
Methods
Data sources
Data on deaths attributed to COVID-19 at the county level reported from March 1, 2020, to January 31, 2021, were obtained from the Tennessee Department of Health.18 County-level sociodemographic data were obtained from public datasets including the Agency for Healthcare Research and Quality (AHRQ) database on Social Determinants of Health,19 the PLACES: Local Data for Better Health County Data 2020 Release,20 the Census Bureau 2015-2019 county population data,21 and the Underlying Cause of Death, 1999-2019 dataset provided through the National Center for Health Statistics (NCHS).22
Outcome and exposure
The outcome measure was mortality rate attributed to COVID-19 for each county; death count included confirmed and probable COVID-19 deaths by day. Death data for notifiable diseases were collected in the Tennessee National Electronic Disease Surveillance System Base System (NBS). Both confirmed deaths and probable deaths due to COVID-19 were confirmed by direct hospital medical record reporting to public health, vital records review of death certificates, or by meeting clinical criteria for infection at the time of death using the CDC criteria.23
Counties were designated as urban (metropolitan) or rural (nonmetropolitan) according to the 2013 NCHS Urban-Rural Classification Scheme for Counties.6 The methodology used to construct the 2013 NCHS scheme assigns all US counties to 1 of 6 levels: large central metro, large fringe metro, medium metro, small metro, micropolitan, and noncore. For this analysis, we combined the 4 metropolitan designations as “urban.” The 2 nonmetropolitan designations were combined as “rural.”
Covariates
We treated county-level population characteristics and health care resources as potential confounders based on prior studies.24–26 County demographics were included using US Census Bureau 2018 population data, as described later. Age was included using percentage of people 65 years of age and older. Gender and race were also collected from US Census Data. American Indian, Asian, Native Hawaiian, and multiple races were combined as “Other” due to low overall percentages. Ethnicity was included separately as percent Hispanic or non-Hispanic.
To account for socioeconomic confounders, a social vulnerability index (SVI) score was included for each county using CDC's SVI 2018 Documentation.25,27 The SVI scores incorporate socioeconomic status, household composition and disability, minority status and language, housing type, and transportation availability data. Social vulnerability index was ranked against the entire United States based on percentiles from 0 to 1, where higher value indicates greater vulnerability. Separately, we accounted for variation in primary care health care access using county-level health professional shortage area (HPSA) designations, as determined by US Health Resources & Services Administration.28 The 2018 HPSA code for each county was divided into 3 categories: none of the county, whole county, or 1 or more parts designated an area with a shortage of primary care physicians. The HPSA designation was included as a covariate in our model as it is associated with both exposure and outcome, though primary care access is not directly on the causal pathway for COVID-19 mortality.
County-level percentage of individuals with self-reported diagnoses of high blood pressure, diabetes (any type), or obesity among adults 18 years of age and older was included using PLACES: Local Data for Better Health, County Data Release 2020.20 These comorbidities are known risk factors for COVID-19 mortality29 and are unevenly distributed among people living in rural and urban counties.30
Influenza and pneumonia and all-cause mortality data were used from the Underlying Cause of Death database, which contains mortality and population counts for all US counties based on death certificates for US residents as collected by NCHS.22 These data were available through 2019. International Classification of Diseases, Tenth Revision (ICD-10) Codes J09-J18 (influenza and pneumonia) and combined codes for all-cause mortality for years 2015-2019 were used.
Statistical analysis
We reported categorical variables as frequency and percentage; continuous variables were reported as mean and standard deviation. Mortality rates were computed as the number of confirmed and probable deaths attributed to COVID-19 per 100 000 population. Descriptive analyses were first completed to enable graphical comparison of the trend of unadjusted COVID-19 mortality rates statewide and by exposure of rural or urban county residence per month during the study period.
To evaluate the association between urban and rural county designation and COVID-19 mortality, we fit a negative binomial regression model with total deaths attributed to COVID-19 (March 2020 to January 2021) as the outcome variable and urban or rural status as the primary exposure. Model covariates were percentage of county population age of 65 years and older, percent female, percent Black, percent Hispanic, SVI percentile, HPSA score, and percentage of self-reported obesity, hypertension, and diabetes. Urban counties were used as the reference group. An offset term was included in the model to account for the population in each county. All variables were continuous except HPSA score and rural-urban designation. Results are presented as incidence rate ratios and 95% confidence intervals (95% CI), where greater values indicate a greater COVID-19 mortality incidence rate.
We additionally calculated the unadjusted rate ratio and rate difference with 95% CI for COVID-19 mortality rates, 5-year influenza and pneumonia mortality rates (2015-2019), and 5-year all-cause mortality rates (2015-2019) between urban and rural counties to provide context into how these compare with COVID-19 mortality rates. Five years was chosen for calculation of mortality rates for influenza and pneumonia to allow for a historical comparator over multiple influenza seasons. The same time frame for all-cause mortality was chosen for consistency. All statistical analysis was performed using SAS 9.4 (SAS Institute, Inc, Cary, North Carolina). This study was approved by the Tennessee Department of Health Institutional Review Board and reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.*
Results
We identified 42 urban counties with a total population of 514 9879 and 53 rural counties with a total population of 150 1210, according to the NCHS Classification scheme. Rural counties contained 22.6% of the total state population in 2018, and an average of 19.6% (SD: 2.8%) was of age 65 years and older (see Supplemental Digital Content Table 1, available at http://links.lww.com/JPHMP/A926, which demonstrates differences between rural and urban Tennessee counties). Half of the population living in both urban and rural counties was female (50.7%, SD: 1.6% and 50.1%, SD: 2.6%, respectively). Urban counties were more racially and ethnically diverse. The SVI percentile—where higher value indicates greater vulnerability—was greater for rural counties, which had a mean percentile of 0.7 (SD: 0.2) compared with urban counties with a mean SVI percentile of 0.5 (SD: 0.2). More rural counties were designated as an HPSA, with 16 (30.2%) designated as a shortage area for the entire county compared with 4 (9.5%) urban counties. Rural counties had a greater percentage of reported comorbidities, with 37.5% (SD: 2.4%) reporting obesity, 43.2% (SD: 2.4%) with hypertension, and 15.3% (SD: 1.5%) with diabetes.
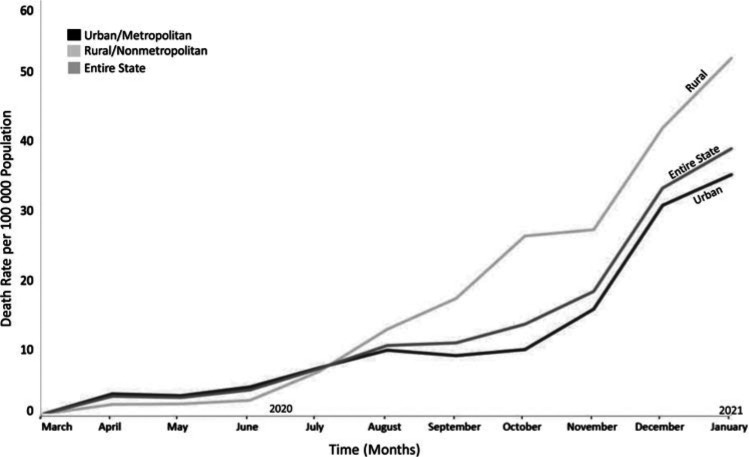
There were 9650 total deaths attributed to COVID-19 during the observation period. COVID-19 mortality rates for urban and rural counties increased monthly from March 2020 through January 2021 (Figure). Mortality rate was slightly greater for urban as compared with rural counties from March through July, with a mortality rate difference between urban and rural counties ranging from 0.6 to 1.8 per 100 000 population. Beginning in August, mortality rates in rural counties consistently exceeded in urban counties, with a mortality rate difference between rural and urban counties increasing from 3.1 to 16.9 per 100 000 population from August through January.
FIGURE.
Trend of Unadjusted COVID-19 Mortality Rates per 100 000 Population Shown by Urban or Rural County Designation in Tennessee by Montha
aCOVID-19 mortality rate per 100 000 population for the entire state of Tennessee is also shown. Mortality rates are per month, independent of previous months. Gray scale and labels designate urban, rural, or total state mortality rates.
Results from the negative binomial regression for association between rural-urban county designation and COVID-19 mortality after controlling for county-level characteristics are shown in Table 1. We observed an incidence rate ratio of 1.13 (95% CI, 1.00-1.28; P < .05) for rural as compared with urban counties. Comparisons between unadjusted rate ratio and rate differences per 100 000 person-years between rural and urban counties are shown in Table 2. The unadjusted COVID-19 mortality rate ratio from March 1, 2020, to January 31, 2021 (1.50; 95% CI, 1.44-1.57) and influenza and pneumonia mortality rate ratio from 2015 to 2019 (1.60; 95% CI, 1.53-1.69) were similar. The unadjusted rate difference for COVID-19 mortality between rural and urban counties was 61.85 (95% CI, 54.31-69.31), greater than the rate difference for influenza and pneumonia mortality between rural and urban counties (12.57; 95% CI, 11.16-13.00).
TABLE 1. Results of Negative Binomial Regression Model Estimating Association Between Rural-Urban County Designation and COVID-19 Deaths in Tennessee From March 1, 2020, to January 31, 2021.
| Adjusted Incidence Rate Ratioa | |||
|---|---|---|---|
| IRR | 95% Confidence Interval | ||
| County designation | |||
| Urban | Reference | Reference | Reference |
| Rural | 1.13 | 1.00 | 1.28b |
| Characteristic, % | |||
| ≥65 y | 1.01 | 0.97 | 1.04 |
| Female | 1.01 | 0.98 | 1.04 |
| Black | 1.00 | 1.00 | 1.01 |
| Hispanic | 1.00 | 0.98 | 1.03 |
| SVI percentilec | 1.43 | 0.96 | 2.14 |
| HPSA scored | |||
| None of county in shortage area | Reference | Reference | Reference |
| One or more parts of county in shortage area | 0.91 | 0.69 | 1.20 |
| Whole county in shortage area | 0.81 | 0.59 | 1.13 |
| Comorbidities, %e | |||
| Obesity | 0.99 | 0.97 | 1.02 |
| Hypertension | 1.03 | 0.98 | 1.09 |
| Diabetes | 1.03 | 0.96 | 1.11 |
Abbreviations: HPSA, health professional shortage area; IRR, incidence rate ratio; SVI, social vulnerability index.
aAdjusted for all covariates listed in the table.
bP < .05.
cPercentile ranking uses Tennessee census tracts ranked against the entire US based on percentiles from 0 to 1, where higher value indicates greater vulnerability.
dHPSA ranking scores included 1 of 3 options: None of the county designated as a shortage area, whole county designated as a shortage area, or 1 or more parts of the county designated as shortage area.
ePLACES: Local Data for Better Health, County Data Release 2020; county-level percentage of individuals with self-reported diagnoses of high blood pressure, diabetes (any type), or obesity among adults 18 years of age and older was included.
TABLE 2. Unadjusted Rate Ratios and Rate Differences Between Deaths Attributed to COVID-19, 5-Year Influenza and Pneumonia, and 5-Year All-Cause Mortality for Rural as Compared With Urban Counties in Tennessee.
| Rural | Urban | Rate Ratioa | 95% CI | Rate Differencea | 95% CI | |
|---|---|---|---|---|---|---|
| COVID-19b | 1.50 | 1.44-1.57 | 61.85 | 54.31-69.31 | ||
| Total reported deaths | 2827 | 6560 | ||||
| Crude mortality rate | 185.50 | 123.70 | ||||
| Influenza and pneumonia, 5 yc | 1.60 | 1.53-1.69 | 12.57 | 11.16-13.00 | ||
| Total reported deaths | 2506 | 5370 | ||||
| Crude mortality rate | 33.20 | 20.60 | ||||
| All-cause mortality, 5 yd | 1.37 | 1.36-1.38 | 350.44 | 341.46-359.42 | ||
| Total reported deaths | 98 635 | 248 901 | ||||
| Crude mortality rate | 1307.00 | 956.60 |
Abbreviation: CI, confidence interval.
aUnadjusted mortality rate ratio and rate difference per 100 000 person-years.
bCOVID-19 deaths reported, March 2020 to January 2021.
cInfluenza and pneumonia mortality from ICD-10 codes for underlying causes of death; J09-J18 (influenza and pneumonia) 2015-2019 per year.
dAll-cause mortality from all ICD-10 codes, 2015-2019 per year.22
Discussion
COVID-19 continues to have variable impact across communities. Similar to national trends,5 the COVID-19 mortality rate in Tennessee was greater in urban than in rural areas early in the pandemic. However, as the COVID-19 pandemic progressed, mortality rates became greater for populations living in rural Tennessee as compared with urban counties, even after controlling for factors known to impact health in rural communities. These findings have implications for public health policy, planning, and resource allocation for current and future pandemic response.
We observed a transition as cases spread to less densely populated areas and rural counties experienced higher mortality rates beginning in August 2020. While rural geography and dispersed populations likely delayed introduction and spread of the virus early in the pandemic, this factor was negated over time. We observed a difference in the adjusted mortality rate attributed to COVID-19, which remained greater for populations living in rural as compared with urban counties. We modeled this association controlling for county-level primary care access, percent 65 years and older, gender and other sociodemographic characteristics, and comorbidities including hypertension, diabetes, and obesity among adults from March 2020 to January 2021. Our findings are consistent with the work of previous studies that identified increased social vulnerability8,9,12,26 contributing to increased COVID-19 mortality rate in rural areas. However, our analyses show that disparities in COVID-19 mortality exist even when controlling for race, ethnicity, and socioeconomic status.
The rate of difference in COVID-19 mortality emphasizes that rural communities experienced the worst health outcomes in Tennessee.26,31 One contributing factor not accounted for in our model may be limited rural hospital and intensive care access during the pandemic. The COVID-19 pandemic has compounded already strained finances of critical access hospitals, causing multiple hospital closures in the southern United States and 4 in Tennessee alone during 2020.7 Rural hospitals in the southern United States are vulnerable to closure in part because of the high rates of poverty and uninsured populations, which contribute to financial challenges of medical care and sustainability. Decreased hospital access occurs because of geographic isolation in rural communities and may increase mortality rates through delay in seeking care or emergency access after onset of COVID-19 symptoms. In addition, rural medical providers face different challenges than their urban counterparts with far fewer subspecialists and resources to manage complicated patients. Notably, the ability to transfer patients too sick to manage locally was slowed by the inpatient burden at urban medical centers during peaks of the pandemic, a phenomenon that has not been uncommon throughout the United States.32,33
Trends in rural-urban disparities in all-cause and cause-specific mortality in the United States have widened over time,17 and long-standing disparities in mortality from influenza and pneumonia are a historical comparator for COVID-19 mortality. We observed that the unadjusted COVID-19 absolute mortality risk between rural and urban counties was greater than 5-year influenza and pneumonia rural-urban absolute risk. Rural counties had 61.85 additional deaths due to COVID-19 per 100 000 population compared with urban counties. This may represent fundamental differences in preparedness during the pandemic response. Rural counties have less robust public health and health care infrastructure, resource allocation, and hospital access.34–36 Staffing needs in health departments and hospitals in rural regions have also remained a challenge, with differences in wages and training across rural-urban practice settings stretching the workforce.37 In addition, the response to the COVID-19 pandemic has varied in community prevention methods and health policy responses at the local level (eg, masking policies, social distancing, and business closures). Previous studies have shown that differences in prevention behaviors among communities impact the spread of disease,38–41 but changing health behaviors in communities can be challenging. Tennessee public health and health policy officials should continue to support proposals for implementation and enforcement of community mitigation measures, informed by state and local public health data monitoring, hospital capacity, and ongoing community spread. Collaboration with partners at the local level on implementation of safety measures is important in helping slow the spread of COVID-19.
The results of this study may be additionally informative to public health decision makers in Tennessee in the postvaccine era by informing decisions related to vaccine resources and providing additional foundation for addressing rural-urban disparities. Large studies incorporating data from the United States have shown adult COVID-19 vaccination coverage to be lower in rural counties than in urban counties,42 a trend that has been consistently observed in Tennessee and neighboring southern states.43 Differences in prevention behaviors are further emphasized when considering vaccination in rural communities, where widespread vaccine hesitancy represents a major public health concern.44 Unvaccinated communities have made a major contribution to new COVID-19 infections and hospitalizations in Tennessee,43 creating a disproportional burden in rural communities further exacerbated by vaccine hesitancy in these regions. Public health must continue to find ways to reach our rural communities to identify and address barriers to COVID-19 prevention.
This study has several limitations inherent in cross-sectional study designs. First, all data are provided at a county-level and can be used to estimate population-level risk only. Important individual risk factors for mortality, such as demographic or medical comorbidities that vary within counties, are lost by combining data at this level for analysis. In addition, medical comorbidity data were obtained through self-report and may be subject to error related to noncoverage, nonresponse, or measurement bias. Misclassification of deaths due to COVID-19 was also possible and likely represents an underestimate of true deaths due to COVID-19 early in the pandemic. Confounders not considered in this analysis include other possible medical comorbidities that may make the rural-urban populations unequal. These data incorporate the first 11 months and the peak of COVID-19 mortality rates to date. Longer-term analysis could show different results. In addition, use of medical billing codes for influenza and pneumonia and all-cause mortality are also likely a substantial underrepresentation of deaths due to these causes; although if all are an equal underrepresentation of true all- and cause-specific mortality, rate comparisons would still be reliable. Results presenting rate ratios and rate differences between deaths attributed to COVID-19, 5-year influenza and pneumonia, and 5-year all-cause mortality for rural as compared with urban counties in Tennessee are unadjusted measures of effect, which limits interpretation. These were intended to provide context for COVID-19 mortality rates and were not part of the primary aim. Finally, because these data represent only those individuals in Tennessee, results may not be generalizable elsewhere in the country.
Implications for Policy & Practice
Rural communities are faced with long-standing disparities in health care infrastructure, resource allocation, and hospital access in Tennessee, which frequently lead to delay in receiving care and reduced access to specialized care.
Rural communities also face disparities that may make implementation of COVID-19 pandemic response planning more challenging. Policy makers should consider rural COVID-19 mortality rates when developing eligibility criteria for resource allocation during the pandemic response, including criteria for external assistance and support for community hospitals.
More sparsely populated counties may demonstrate different pandemic response behaviors as compared with urban counties (eg, less compliance with mask wearing, social distancing, large gatherings), and these should be considered in public health programmatic development to address local needs and education about prevention measures. Public health officials should continue to consider patient location, community spread, and hospital impacts when planning pandemic response.
Conclusions
This cross-sectional study demonstrated COVID-19 mortality rates in Tennessee to be greater for populations living in rural as compared with urban counties after controlling for confounding variables. While it is not the only factor, rurality is an important consideration in public health response and health policy decision making. The pandemic has shown that public health planning for delivery of health services and response efforts must include contingencies to address disparities in mortality outcomes for rural counties.
241(d); 5 USC §552a; 44 USC §3501 et seq.
This study was supported by the Centers for Disease Control and Prevention's Emerging Infections Program Cooperative Agreement 1U50CK000491.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors declare no conflicts of interests.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (http://www.JPHMP.com).
Contributor Information
Heather N. Grome, Email: QDS9@cdc.gov.
Rameela Raman, Email: r.raman@vanderbilt.edu.
Benjamin D. Katz, Email: ben.katz@tn.gov.
Mary-Margaret Fill, Email: mary-margaret.fill@tn.gov.
Timothy F. Jones, Email: Tim.F.Jones@tn.gov.
William Schaffner, Email: william.schaffner@vumc.org.
John Dunn, Email: John.Dunn@tn.gov.
References
- 1.Koh HK, Blakey CR, Roper AY. Healthy People 2020: a report card on the health of the nation. JAMA. 2014;311(24):2475–2476. [DOI] [PubMed] [Google Scholar]
- 2.Matthews KA, Croft JB, Liu Y, et al. Health-related behaviors by urban-rural county classification—United States, 2013. MMWR Surveill Summ. 2017;66(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. CDC COVID-19 Response Health Equity Strategy: Accelerating Progress Towards Reducing COVID-19 Disparities and Achieving Health Equity. Atlanta, GA: Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 4.Centers for Disease Control and Prevention, National Center for Health Statistics. COVID-19 Stats: COVID-19 incidence, by urban-rural classification. MMWR Morb Mortal Wkly Rep. 2020;69(46):1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews KA, Ullrich F, Gaglioti AH, Dugan S, Chen MS, Hall DM. Nonmetropolitan COVID-19 incidence and mortality rates surpassed metropolitan rates within the first 24 weeks of the pandemic declaration: United States, March 1-October 18, 2020. J Rural Health. 2021;37(2):272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2014;(166):1–73. [PubMed] [Google Scholar]
- 7.Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill. Data From: Rural Hospital Closures, 2005-2021. Chapel Hill, NC; NC Rural Health Research Program, UNC Sheps Center; 2021. [Google Scholar]
- 8.Liao TF, De Maio F. Association of social and economic inequality with coronavirus disease 2019 incidence and mortality across US counties. JAMA Netw Open. 2021;4(1):e2034578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dalsania AK, Fastiggi MJ, Kahlam A, et al. The relationship between social determinants of health and racial disparities in COVID-19 mortality [published online ahead of print January 5, 2021]. J Racial Ethn Health Disparities. 2022;9(1):288–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng KJG, Sun Y, Monnat SM. COVID-19 death rates are higher in rural counties with larger shares of Blacks and Hispanics. J Rural Health. 2020;36(4):602–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fielding-Miller RK, Sundaram ME, Brouwer K. Social determinants of COVID-19 mortality at the county level. medRxiv. https://www.medrxiv.org/content/10.1101/2020.05.03.20089698v2. Published 2020. Accessed March 13, 2022. [DOI] [PMC free article] [PubMed]
- 12.Seligman B, Ferranna M, Bloom DE. Social determinants of mortality from COVID-19: a simulation study using NHANES. PLoS Med. 2021;18(1):e1003490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cross SH, Califf RM, Warraich HJ. Rural-urban disparity in mortality in the US from 1999 to 2019. JAMA. 2021;325(22):2312–2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed R, Williamson M, Hamid MA, Ashraf N. United states county-level COVID-19 death rates and case fatality rates vary by region and urban status. Healthcare (Basel). 2020;8(3):330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qu J, Chang LK, Tang X, et al. Clinical characteristics of COVID-19 and its comparison with influenza pneumonia. Acta Clin Belg. 2020;75(5):348–356. [DOI] [PubMed] [Google Scholar]
- 17.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. J Urban Health. 2014;91(2):272–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tennessee Department of Health Communicable and Environmental Diseases and Emergency Preparedness. County new dataset. https://www.tn.gov/content/dam/tn/health/documents/cedep/novel-coronavirus/datasets/Public-Dataset-County-New.XLSX. Published 2020. Accessed April 15, 2021.
- 19.Agency for Healthcare Research and Quality. Social determinants of health database (beta version). https://www.ahrq.gov/sdoh/data-analytics/sdoh-data.html. Published 2020. Accessed April 15, 2021.
- 20.Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. PLACES: Local Data for Better Health, county data 2020 release. https://chronicdata.cdc.gov/500-Cities-Places/PLACES-Local-Data-for-Better-Health-County-Data-20/swc5-untb. Accessed April 15, 2021.
- 21.United States Census Bureau ACS. 2015-2019: ACS 1-year estimates detailed tables. https://data.census.gov/cedsci/table?q=United%20States&tid=ACSDT1Y2019.B01003&hidePreview=false. Accessed April 15, 2021.
- 22.Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999-2019 on CDC WONDER Online Database, released in 2020. Data are from the Multiple Cause of Death Files, 1999-2019, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. https://wonder.cdc.gov/ucd-icd10.html. Accessed September 30, 2021.
- 23.Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). 2020 interim case definition, approved August 5, 2020. https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/08/05/. Accessed March 15, 2021.
- 24.Paul R, Arif AA, Adeyemi O, Ghosh S, Han D. Progression of COVID-19 from urban to rural areas in the United States: a spatiotemporal analysis of prevalence rates. J Rural Health. 2020;36(4):591–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karim SA, Chen HF. Deaths from COVID-19 in rural, micropolitan, and metropolitan areas: a county-level comparison. J Rural Health. 2021;37(1):124–132. [DOI] [PubMed] [Google Scholar]
- 26.Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021;4(1):e2036462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention Agency for Healthcare Research and Quality. CDC SVI 2018 documentation—1/31/2020. https://www.atsdr.cdc.gov/placeandhealth/svi/documentation/SVI_documentation_2018.html. Accessed March 15, 2021.
- 28.Health Resources & Services Administration. Health Professional Shortage Area (HPSA) designations 2018. https://data.hrsa.gov/tools/shortage-area/hpsa-find. Accessed April 15, 2021.
- 29.Kim L, Garg S, O'Halloran A, et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET). Clin Infect Dis. 2021;72(9):e206–e214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O'Connor A, Wellenius G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health. 2012;126(10):813–820. [DOI] [PubMed] [Google Scholar]
- 31.Alberti PM, Lantz PM, Wilkins CH. Equitable pandemic preparedness and rapid response: lessons from COVID-19 for pandemic health equity. J Health Polit Policy Law. 2020;45(6):921–935. [DOI] [PubMed] [Google Scholar]
- 32.Tennessee Department of Health. Tennessee COVID-19 hospital resource status. https://www.tn.gov/health/cedep/ncov/data/hospitalization-data/hospital-capacity.html. Published July 2021. Accessed July 1, 2021.
- 33.Lee S, Santarelli A, Choi H, Ashurst J. Impact of the COVID-19 pandemic on emergency department transfers to a higher level of care. West J Emerg Med. 2021;22(3):561–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Skoufalos A, Clarke JL, Ellis DR, Shepard VL, Rula EY. Rural aging in America: proceedings of the 2017 connectivity summit. Popul Health Manag. 2017;20(S2):S1–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carr BG, Bowman AJ, Wolff CS, et al. Disparities in access to trauma care in the United States: a population-based analysis. Injury. 2017;48(2):332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davoodi NM, Healy M, Goldberg EM. Rural America's hospitals are not prepared to protect older adults from a surge in COVID-19 cases. Gerontol Geriatr Med. 2020;6:2333721420936168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Odahowski CL, Crouch EL, Zahnd WE, Probst JC, McKinney SH, Abshire DA. Rural-urban differences in educational attainment among registered nurses: implications for achieving an 80% BSN workforce. J Prof Nurs. 2021;37(2):404–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang X, Ferro EG, Zhou G, Hashimoto D, Bhatt DL. Association between universal masking in a health care system and SARS-CoV-2 positivity among health care workers. JAMA. 2020;324(7):703–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mitze T, Kosfeld R, Rode J, Wälde K. Face masks considerably reduce COVID-19 cases in Germany. Proc Natl Acad Sci U S A. 2020;117(51):32293–32301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gallaway MS, Rigler J, Robinson S, et al. Trends in COVID-19 incidence after implementation of mitigation measures—Arizona, January 22-August 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(40):1460–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Van Dyke ME, Rogers TM, Pevzner E, et al. Trends in county-level COVID-19 incidence in counties with and without a mask mandate—Kansas, June 1-August 23, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(47):1777–1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murthy BP, Sterrett N, Weller D, et al. Disparities in COVID-19 vaccination coverage between urban and rural counties—United States, December 14, 2020-April 10, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(20):759–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alcendor DJ. Targeting COVID vaccine hesitancy in rural communities in Tennessee: implications for extending the COVID-19 pandemic in the south. Vaccines (Basel). 2021;9(11):1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gatwood J, McKnight M, Fiscus M, Hohmeier KC, Chisholm-Burns M. Factors influencing likelihood of COVID-19 vaccination: a survey of Tennessee adults. Am J Health Syst Pharm. 2021;78(10):879–889. [DOI] [PMC free article] [PubMed] [Google Scholar]