Abstract
Stomach cancer is a common public health problem in South East Asia including Bhutan. Chronic infection with Helicobacter pylori is regarded as the principal cause of stomach cancer. Herein, we present the incidence of stomach cancer in Bhutan for eight years (from 2014 to 2021). We also discuss the steps taken for the prevention and early detection of stomach cancer.
Keywords: Stomach cancers, Helicobacter pylori, Triple therapy
Introduction
In 2020, stomach cancer ranked fifth commonest cancer in incidence and fourth for mortality worldwide [1]. In Bhutan, stomach cancer is the commonest cancer in men and the second commonest cancer in women with an incidence of 8.3 and 5.2 per 100,000 population respectively [2].
Helicobacter pylori (H. pylori) is a highly infectious gram-negative bacterium and is microaerophilic in nature that colonizes the gastrointestinal mucosa [3, 4]. It is implicated widely in the development of the disease of the stomach and duodenum with varying clinical symptoms and conditions, notable of which is stomach cancer [5].
Correction of potential risk factors and eradication of H. pylori infection are the best methods for reducing the development of stomach cancers [6]. Endoscopy remains the main modality of investigation to detect early stomach cancer [7].
The treatment of H. pylori infection with a combination of various antibiotics is the key to reducing the number of stomach cancers associated with this infection [8]. However, an increasing trend in the development of antibiotic-resistant H. pylori infection is a cause of concern as stated by the WHO (World Health Organization) [9].
Herein, we present the incidence of stomach cancer in Bhutan for 8 years (from 2014 to 2021) and steps taken for prevention and early detection of stomach cancer.
Endoscopic Services in Bhutan
The constitution of Bhutan mandates free health care services to its citizen [10]. The health care system of Bhutan is a three-tiered system consisting of primary, secondary, and tertiary levels since the 1960s [11]. Jigme Dorji Wangchuck National Referral Hospital (JDWNRH), which is the national referral hospital of Bhutan, is located in Thimphu. There are two regional referral hospitals located in the eastern and central Bhutan which also provide general specialized services. Other 28 hospitals with numerous basic health units and outreach clinics cater their services to the people at the community level.
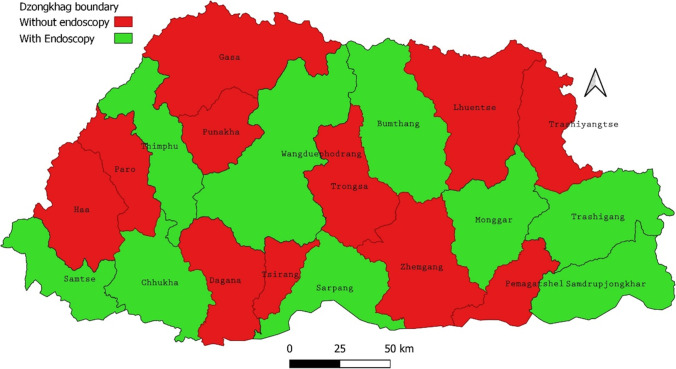
The endoscopic service in Bhutan was established since 1987 [12]. The endoscopy service was mainly provided at JDWNRH initially, which was gradually expanded across the country (Fig. 1). General surgeons and medical specialists are involved in performing endoscopy, of which the majority of the endoscopy is performed by the former group. Until 2018, there were only 10 general surgeons, one gastroenterologist, and one internal medicine specialist who could perform and provide endoscopic services for the whole country. As of now, 20 general surgeons spread across the nation are providing endoscopy services. Overseas volunteers from Japan helped strengthen the existing human resources by training our surgeons on endoscopy, especially in detecting early stomach cancers.
Fig. 1.
Map of Bhutan showing endoscopy service centers as of June 2022 (with permission of Policy and Planning Division, Ministry of Health, Thimphu, Bhutan)
Earlier, the H. pylori screening was mostly focused on the patients who were advised upper gastrointestinal endoscopy by the prescribers. The breath test and stool antigen tests were not available in any of the health centers across the country.
Flagship Program
The Royal Government of Bhutan instituted a Health Flagship program in 2020 covering three cancers of the stomach, cervix, and breast, with ultimate goal to reduce the incidence and mortality associated with these cancers through early screening and detection [2, 13]. With regard to the stomach cancer, the following targets were framed by the program [2]:
All target populations (18–75) to be screened for H. pylori
All screened populations (H. pylori-positive) to receive triple therapy treatment
All high-risk target populations (40–75 years) are screened for stomach cancer and managed accordingly
With these strategies in place, the program aims to achieve 100% screening and treatment of H. pylori infection by the end of 2023. In terms of implementation, the set interventions are carried out through the ongoing nationwide mobile camps for a period of 3 years (2020–2023). The stool antigen test for H. pylori screening is done using the H. pylori Quik Chek™ stool testing kit or the H. pylori Chek™ ELISA test. Fresh stool samples or frozen stool samples are collected which are stored or transported in Cary Blair transport medium and the tests performed as per the standard operating procedure [14]. All screen positives are treated with triple antibiotic therapy of amoxycillin, clarithromycin, and pantoprazole for 14 days and with tetracycline, bismuth, pantoprazole, and tinidazole quadruple therapy as the second-line drugs for retested subjects who turn positive again [13]. In spite of the retreatment if the retest result turned positive, the subject is then referred for upper gastrointestinal endoscopy. Endoscopic procedures are carried out as per the age-specific target groups with history of atrophic gastritis, H. pylori infection, family history of stomach cancers, dyspepsia with alarm features, smoking, chewing tobacco, and alcohol intake history [13].
Situation Analysis of Stomach Cancers at the JDWNRH, Bhutan
The surgical oncology services are available only at JDWNRH, because the lone surgical oncologist is stationed in there. All the patients suspected or confirmed as cases of stomach cancers across the country are ultimately referred to JDWNRH, since both the curative and palliative services for stomach cancer patients are available.
The Population Based Cancer Registry (PBCR) in Bhutan, maintained at JDWNRH, was established in 2014 in collaboration with the Tata Memorial Hospital (TMH) in Mumbai, the Registry hub for South East Asian Regional Office (SEARO), and IARC in Lyon, France. The registry uses Canreg5 software. We have accessed data from the PBCR.
Over the last 8 years, 786 stomach cancer cases were recorded from across the country. There were 466 men and 320 women with a 1.5:1 men preponderance (Fig. 2). The population of Bhutan stands at 727,145 as of 2017 [15]. This gives an overall incidence of stomach cancer of 13.5/10,000 population per year (786 cases/8 years/727,145 population). Nearly 50% of the patients were less than 65 years of age in terms of incidence (Fig. 3). With the initial record of 117 cases in the first year of the establishment of the cancer registry, the case sharply dropped to 67 in 2016 and again picked up in 2019 with 118 cases (Fig. 4). This was probably and mostly because the endoscopy unit in JDWNRH during that period of time was also manned by the expats from Japan who have more experience in detecting stomach cancers. Since then, the cases have steadily increased with 124 cases recorded in 2021. The stage was not recorded for all cases of stomach cancers. Many patients died within days or weeks of diagnosis, before any staging or treatment could be done. Surgical treatments done were mostly palliative.
Fig. 2.

Bar graph showing the gender distribution of stomach cancer in Bhutan from 2014 to 2021
Fig. 3.

Bar graph showing the age-wise distribution of stomach cancer in Bhutan from 2014 to 2021
Fig. 4.

Line diagram showing the trend of stomach cancer incidence in Bhutan from 2014 to 2021
Discussion
The constitution of Bhutan mandates free health care and services to all its citizens [16]. Healthcare and access had been always a top priority to the govenrment of Bhutan. Therefore, Bhutan becoming a signatory to the Alma-Ata declaration in 1978 wre timely and visionary [17]. In the backdrop of free healthcare, sustainability is a hurdle and challenge as healthcare is becoming more complex [18]. Among all the cancers, stomach cancer is the commonest cancer in Bhutan with a 5-year prevalence of 20.74 stomach cancers per 100,000 [19]. Almost 95% of stomach cancer diagnosed in Bhutan were in an advanced stage, thereby negatively affecting the survival and quality of life [20].
Epidemiologic studies have shown that H. pylori bacteria are transmitted via oral-oral, feco-oral, and gastro-oral routes [5, 21, 22]. The prevalence of H. pylori infection is comparatively low in the developed nations (40% in North America and Europe) than in the developing nations (82%) [21]. This is probably because hygiene and sanitation are poor in the developing nations which contribute to the higher rate of transmission. As of today, about 63% of Bhutanese have access to basic sanitation services [23]. The prevalence of H. pylori in Bhutan is found to be 73.4% which is very high compared to most of the countries in the region [24–26].
Peptic ulcer disease had been one of the top ten diseases for the last 5 years (2016–2020) in Bhutan [27]. Since H. pylori infection is largely implicated in the pathogenesis of peptic ulcer disease, this correlation holds as indicated by findings of the high prevalence of H. pylori infection in Bhutan [24]. Earlier, although the government hospital’s provided screening services for H. pylori, government pharmacies hardly provided the eradication treatment since some of the drugs are not in essential drug list (EDL) until recently [28]. Therefore, some patients purchased from the private pharmacies while some remained untreated probably due to the cost issues as the clarithromycin-based triple treatment available in the market was expensive. This was important because it indicate a programmatic failure to subdue the causal link between gastric cancer and H. pylori infection. The carcinogenic property of H. pylori is a major concern as over half the world’s population is infected by H. pylori and Bhutan’s prevalence of H. pylori infection is 73.4% [8, 24]. The high prevalence of stomach cancer in Bhutan is attributed to the high prevalence of H. pylori infection and stomach mucosal atrophy [20, 24, 25, 29]. However, on the contrary, the high prevalence of H. pylori infection in Africa and India does not translate to a higher incidence of stomach cancer [25, 30]. In a study by Matsunari et al., 90% of H. pylori bacterium in Bhutan possessed the highly virulent East Asian-type CagA [29]. This finding is significant as the higher incidence of stomach cancer in Bhutan is supposedly linked to this virulent bacterium.
In Bhutan, stomach cancer is the most common cancer in men and the second most common cancer in women after cervical cancer [2, 31]. Therefore, the initiation of the flagship program at this hour is timely. However, programmatic problems such as a smaller number of endoscopists, pathologists, and professionally trained endoscopic nurses are challenges in the present context and it will probably remain for the next few years until human resources are trained by the ministry of health and relevant organizations. In terms of capacity building, the flagship program partnered with the Khesar Gyalpo University of Medical Sciences of Bhutan (KGUMSB) and the Japan International Cooperation Agency (JICA) to train our local endoscopists [32].
The number of newly diagnosed stomach cancers noted a sharp drop in the initial period (Fig. 4). However, the trend does not indicate a declining number of cases owing to improved screening and early detection. With limited human resources in terms of local endoscopists and the departure of a full-time overseas endoscopist, the downward trend continued. Beginning in 2017, the endoscopic service expanded to other hospitals in the country and this probably explained the upward trend in newly diagnosed stomach cancers.
Eradication of H. pylori infection to reduce or prevent stomach cancer is a controversial subject. However, the method had shown to reduce the cancer incidence significantly [33, 34]. Treatment of H. pylori involves a combination of antimicrobial agents and antisecretory agents. Standard triple therapy consists of a proton pump inhibitor (PPI) and two antibiotics (clarithromycin and amoxycillin/metronidazole) as the first-line therapy and levofloxacin-based rescue therapy if the first line failed [35]. However, 81% of H. pylori strains in the studies conducted in Bhutan demonstrated a high resistance pattern to metronidazole [36]. The absence of resistance to amoxycillin and low-resistance pattern to levofloxacin (8.1%), clarithromycin (2%), and tetracycline( 0.6%) are reassuring [36]. The prescribers of the country need to be mindful of these findings so that our triple therapy regimen of clarithromycin-based regimen used currently has to be sustained to achieve the goals of the flagship program. Eradication of H. pylori bacterium can not only reduce the stomach cancer burden but also reduce hospital admission and cost associated with its treatment in patients with H. pylori-associated peptic ulcer disease which accounts for one of the top ten diseases for the last many years in Bhutan [22, 27].
The COVID-19 pandemic disrupted many developmental activities in the country including the flagship program activities. The country had undergone numerous nationwide lockdown to curb the spread of COVID-19 [37–39]. This could have hampered achieving the target outlined in the flagship program in a given stipulated period. About 50% of the targets are achieved in last 2 years and 4 months post-implementation of activities as per the program analyst. Despite the COVID-19 situation, the flagship program is actively being implemented across the nation. Upscaling of program activities is needed to meet the set targets against the limited time frame. We recommend initiating off-hour endoscopic clinics in health centers where the routine endoscopic services are currently provided. As an interim corporate business model, the program in turn could provide off-hour remuneration to the health care workers involved in providing such services. Another attractive option to meet the target deadline is the public–private partnership. The program could provide certain remuneration to the private diagnostic centers whenever clients are long overdue for screening appointment at the government run endoscopic units. Another long-term intervention is to strengthen surgical education for residents and newly recruited endoscopists by setting up endoscopic simulation laboratory in collaboration with KGUMSB, JDWNRH, and relevant development partners. Task sharing and shifting concept could be utilized as well. In this method, we would recommend to provide short term training in endoscopy to the medical officers. It could be used to address the shortage of endoscopist and expand endoscopic services in strategic locations. Since many countries are now relaxing COVID-19 protocols, the flagship program should also capitalize on training endoscopists to detect early stomach cancers in expert centers in the region.
Conclusion
Recognizing the dual burden of H. pylori and stomach cancer as a growing public health problem in Bhutan is apt and timely. While the targets and interventions are set and implemented at the policy level, the program must coordinate with the agencies at the technical and field level. Constraints in terms of human resources and financing have to be addressed while opportunities for expansion of endoscopic services should be explored for the sustainability of the program.
Author contribution
TC was involved in the conception and design, acquisition, analysis, and interpretation of data, revising it critically for important intellectual content, final approval of the version to be published, and agreed to be accountable for all aspects of the work. ST was involved in the conception and design, revising it critically for important intellectual content, final approval of the version to be published, and agreed to be accountable for all aspects of the work. ND was involved in the conception and design, revising it critically for important intellectual content, final approval of the version to be published, and agreed to be accountable for all aspects of the work. UT was involved in the conception and design, revising it critically for important intellectual content, final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Declarations
Ethical approval
Ethical approval is not needed for the review articles as per the institution policy. Approval has been obtained from the head of the cancer registry on the use of the registry’s data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Thukten Chophel, Email: thuktenc@gmail.com.
Sangay Tshering, Email: sangaytshering6080@gmail.com.
Namkha Dorji, Email: namji2002@gmail.com.
Ugyen Tshomo, Email: utshomo509@gmail.com.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/CAAC.21660. [DOI] [PubMed] [Google Scholar]
- 2.Health Flagship Project | Ministry of Health. https://www.moh.gov.bt/hspd/health-flagship/. Accessed 22 Apr 2022
- 3.Gu H. Role of flagella in the pathogenesis of Helicobacter pylori. Curr Microbiol. 2017;74:863–869. doi: 10.1007/s00284-017-1256-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Timothy L, Cover MJB. Helicobacter pylori in health and disease. Gastroenterology. 2013;23:1–7. doi: 10.1053/j.gastro.2009.01.073.Helicobacter. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kusters JG, Van Vliet AHM, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19:449–490. doi: 10.1128/CMR.00054-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eusebi LH, Telese A, Marasco G, et al. Gastric cancer prevention strategies: a global perspective. J Gastroenterol Hepatol. 2020;35:1495–1502. doi: 10.1111/jgh.15037. [DOI] [PubMed] [Google Scholar]
- 7.Pasechnikov V, Chukov S, Fedorov E, et al. Gastric cancer: prevention, screening and early diagnosis. World J Gastroenterol. 2014;20:13842–13862. doi: 10.3748/wjg.v20.i38.13842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sukri A, Hanafiah A, Zin NM, Kosai NIKR (2020) Epidemiology and role of Helicobacter pylori virulence factors in gastric cancer carcinogenesis. 150–161. 10.1111/apm.13034 [DOI] [PubMed]
- 9.Tacconelli E, Carrara E, Savoldi A et al (2017) Articles discovery , research , and development of new antibiotics : the WHO priority list of antibiotic-resistant bacteria and tuberculosis. 3099:1–10. 10.1016/S1473-3099(17)30753-3 [DOI] [PubMed]
- 10.Constitution of Bhutan – GOV.BT. https://www.gov.bt/constitution-of-bhutan/. Accessed 4 Apr 2022
- 11.Systems H, Vol T (2017) The Kingdom of Bhutan health system review
- 12.Dr. Sonam Dukpa honored as SAARC Icon of Surgery | Just Thoughts. https://sunnytobgay.blogspot.com/2011/12/dr-sonam-dukpa-honored-as-saarc-icon-of.html. Accessed 6 Jul 2022
- 13.Health Flagship Project, Ministry of Health RG of B (2020) Guideline for screening gastric cancer, Cervical cancer and Breast cancer
- 14.Ministry of Health Royal Government of Bhutan (2021) Standard operating procedure for H. pylori antigen testing in stool
- 15.Bureau NS. Statistical Yearbook of Bhutan. 2021;2021:1–184. [Google Scholar]
- 16.Constitution of Bhutan – gov.bt. https://www.gov.bt/constitution-of-bhutan/. Accessed 21 Apr 2022
- 17.Tobgay T, Dorji T, Pelzom D, Gibbons R V (2011) Progress and delivery of health care in Bhutan , the Land of the Thunder Dragon and Gross National Happiness. 16:731–736. 10.1111/j.1365-3156.2011.02760.x [DOI] [PubMed]
- 18.Sustainability of Bhutan’s Health Services | The Druk Journal. http://drukjournal.bt/sustainability-of-bhutans-health-services/. Accessed 5 Apr 2022
- 19.Bhutan (2021) The global cancer observatory-All Rights Reserved
- 20.Dendup T, Richter JM, Yamaoka Y et al (2015) Geographical distribution of the incidence of gastric cancer in Bhutan. 21:10883–10889. 10.3748/wjg.v21.i38.10883 [DOI] [PMC free article] [PubMed]
- 21.Quaglia NC, Dambrosio A (2018) Helicobacter pylori : a foodborne pathogen ? 24:3472–3487. 10.3748/wjg.v24.i31.3472 [DOI] [PMC free article] [PubMed]
- 22.Goh K, Chan W, Shiota S, Yamaoka Y (2011) Epidemiology of Helicobacter pylori Infection and Public Health Implications. 16:1–9 [DOI] [PMC free article] [PubMed]
- 23.WASH: Water, Sanitation and Hygiene | UNICEF Bhutan. https://www.unicef.org/bhutan/wash-water-sanitation-and-hygiene/maternal-newborn-and-child-health/wash-water-sanitation-and-0-0-1. Accessed 18 Apr 2022
- 24.Vilaichone R, Mahachai V, Shiota S et al (2013) Extremely high prevalence of Helicobacter pylori infection in Bhutan. 19:2806–2810. 10.3748/wjg.v19.i18.2806 [DOI] [PMC free article] [PubMed]
- 25.Shiota S, Mahachai V, Vilaichone R et al (2013) Seroprevalence of Helicobacter pylori infection and gastric mucosal atrophy in Bhutan , a country with a high prevalence of gastric cancer. 1571–1578. 10.1099/jmm.0.060905-0 [DOI] [PMC free article] [PubMed]
- 26.Fock KM, Ang TL (2010) Epidemiology of Helicobacter pylori infection and gastric cancer in Asia. 25:479–486. 10.1111/j.1440-1746.2009.06188.x [DOI] [PubMed]
- 27.Annual Health Bulletin | Ministry of Health. https://www.moh.gov.bt/about/program-profiles/national-suicide-prevention-program/plans-orders-activities/reports__trashed/annual-health-bulletin/. Accessed 22 Apr 2022
- 28.National Essential Medicine List of Bhutan (2018) - Google Sheets. https://docs.google.com/spreadsheets/d/1Z3EpV9JFCMC14XqUeTnx4QSmxvd6kbN5SBqImJmvVNw/edit#gid=190915248. Accessed 8 Jul 2022
- 29.Matsunari O, Miftahussurur M, Shiota S, Suzuki R (2016) Rare Helicobacter pylori virulence genotypes in Bhutan. Nat Publ Gr 1–11. 10.1038/srep22584 [DOI] [PMC free article] [PubMed]
- 30.Article R (2013) Helicobacter pylori Infection in the general population: A Middle Eastern perspective [PMC free article] [PubMed]
- 31.Bhutan cancer control strategy (2019-2025) | ICCP Portal. https://www.iccp-portal.org/plans/bhutan-cancer-control-strategy-2019-2025. Accessed 22 Apr 2022
- 32.Press release on pilot project on eradication of gastric cancer associated with Helicobacter pylori in Bhutan | Khesar Gyalpo University of Medical Sciences of Bhutan. https://www.kgumsb.edu.bt/?p=2017. Accessed 17 Apr 2022
- 33.Ogura K, Hirata Y, Yanai A, Shibata W (2008) The effect of Helicobacter pylori eradication on reducing the incidence of gastric cancer. 42:279–283 [DOI] [PubMed]
- 34.Ford AC, Yuan Y, Moayyedi P (2020) Helicobacter pylori eradication therapy to prevent gastric cancer : systematic review and meta- analysis. 1–9. 10.1136/gutjnl-2020-320839 [DOI] [PubMed]
- 35.Yang J, Lu C, Lin C (2014) Treatment of Helicobacter pylori infection : current status and future concepts. 20:5283–5293. 10.3748/wjg.v20.i18.5283 [DOI] [PMC free article] [PubMed]
- 36.Vilaichone R, Aumpan N, Ratanachu-ek T. International journal of infectious diseases population-based study of Helicobacter pylori infection and antibiotic resistance in Bhutan. Int J Infect Dis. 2020;97:102–107. doi: 10.1016/j.ijid.2020.05.077. [DOI] [PubMed] [Google Scholar]
- 37.Nationwide lockdown – Prime Minister’s Office. https://www.pmo.gov.bt/timeline/nationwide-lockdown/. Accessed 21 Apr 2022
- 38.22/12/20: Second nationwide lockdown – PMO - information on COVID-19. https://www.gov.bt/covid19/22-12-20-second-nationwide-lockdown-pmo/. Accessed 21 Apr 2022
- 39.Thimphu lockdown to continue until January 22 | Kuensel Online. https://kuenselonline.com/thimphu-lockdown-to-continue-until-january-22/. Accessed 22 Apr 2022