Abstract
A 74-year-old woman presented with progressive dyspnea. Computed tomography revealed a large systemic artery-to-pulmonary artery vascular malformation (VM) on the right chest wall. Embolization of the VM was performed. First, the main drainers of the VM were retrogradely selected from the segmental pulmonary arteries and embolized using microcoils. Second, 2 main feeders of the VM were selected and embolized with N-butyl cyanoacrylate. Thus, marked flow reduction in the VM was achieved, and the patient's symptom improved dramatically. We believe that embolization of both feeders and drainers is an effective technique for treatment of a chest wall systemic artery-to-pulmonary artery VM.
Keywords: Systemic artery-to-pulmonary artery vascular malformation, Chest wall, Embolization
Introduction
Communication between the systemic artery and pulmonary artery (PA) in the absence of chronic lung disease is rare, and few reports have described this entity [1], [2], [3], [4]. Although patients are occasionally asymptomatic, various complications, such as bacterial seeding, hemorrhage, PA hypertension, and congestive heart failure can occur [2]. Surgical management and endovascular embolization have been reported to be useful treatments [2,3]. Embolization of the feeding systemic artery is the most common endovascular embolization technique [1,2,5,6]. Here, we report a case of systemic artery-to-PA vascular malformation (VM) on the chest wall that was successfully treated by embolization of both feeders and drainers.
Case report
A 74-year-old woman presented with progressive dyspnea. The patient had a history of mitral valve stenosis and tricuspid valve regurgitation, which were treated with mitral valve replacement and tricuspid annuloplasty more than 25 years prior. She was diagnosed with pulmonary hypertension and heart failure 3 years prior and was treated with diuretics and home oxygen therapy. Aggravation of pulmonary hypertension and heart failure was considered the cause of the patient's symptoms. Contrast-enhanced computed tomography revealed a large VM between the systemic artery and PA on the right chest wall. The VM had many feeders, including the right internal thoracic artery (ITA), pectoral branch of the right axillary artery, right lateral thoracic artery, right dorsal thoracic artery, multiple right intercostal arteries, right inferior phrenic artery, and right inferior epigastric artery. Among these, the ITA and pectoral branch were the main feeders. The main drainers of the VM were connected to the segmental arteries of segments 3, 4, 5, and 8 (A3, A4, A5, and A8, respectively) (Figs. 1A-C). We assumed that massive blood flow to the right PA through the VM caused pulmonary hypertension and heart failure, and embolization of the VM was planned. N-butyl cyanoacrylate (NBCA) was considered an embolic material suitable for feeder occlusion because long and tortuous feeders made transarterial access to the nidus difficult; however, rapid flow through the VM posed a risk of non-target embolization. It was considered possible to embolize the main drainers of the VM through PA. Thus, we decided to perform retrograde embolization of the main drainers through the PA to decrease VM flow, followed by embolization of the main feeders using NBCA.
Fig. 1.
Oblique axial maximum intensity projection computed tomography images of a systemic artery-to- pulmonary artery (PA) vascular malformation (VM) of the right chest wall. Main drainers of the VM (star) are connected to the PA segment 3 (A3, arrow in A), A4 and A5 (arrows in B), and A8 (arrow in C). Severe cardiomegaly is observed.
Embolization was performed under local anesthesia and conscious sedation. A 5-Fr sheath was placed in the right brachial artery, and a 5.2-F balloon catheter (Selecon MP, balloon diameter 9 mm; Terumo, Tokyo, Japan) was advanced to the right ITA. Angiography of the ITA showed the VM and a drainer connected to A3 (Fig. 2A). An 8-Fr J-shaped sheath was advanced from the right internal jugular vein to the main PA. A 6-Fr balloon catheter (Selecon MP, balloon diameter 20 mm; Terumo) was advanced to the right PA. Referring to the VM shown on angiography of the right ITA, a 1.7-Fr microcatheter was retrogradely advanced from the 6-Fr balloon catheter placed in the right PA to the drainer through segment A3, and the drainer was embolized using detachable microcoils under flow control by inflating the 2 balloon catheters. Then, the 5-Fr balloon catheter was advanced to the pectoral branch, and angiography of the artery showed the VM and several drainers connected to segments A4, A5, and A8 (Figs. 2B and C). Referring to the vascular anatomy shown by this angiography, the drainers were retrogradely selected by the microcatheter through the segmental PAs and embolized in the same manner as the drainer connected to A3. Subsequently, angiography of the ITA and pectoral branch demonstrated marked flow reduction of the VM. The embolization from the 2 main feeders was performed using NBCA mixed with iodized oil (Fig. 3A). The ratios of NBCA to iodized oil were 1:2 and 1:3 for the ITA and pectoral branch, respectively, with 2 mL and 1.5 mL of the mixture used for each, respectively. After embolization, angiography of the right subclavian artery showed marked flow reduction in the VM (Fig. 3B). The embolization procedure is illustrated in Figure 3C. No complications were observed. After 3 months of follow-up, dyspnea on exertion improved dramatically, and the flow rate of home oxygen therapy was reduced.
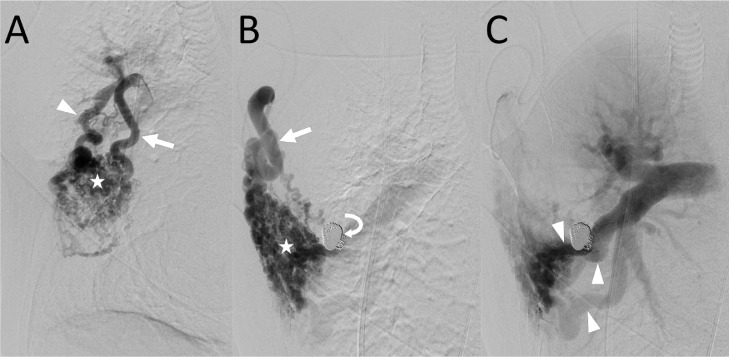
Fig. 2.
Angiography of 2 main feeders of the systemic artery-to-pulmonary artery (PA) vascular malformation (VM) of the right chest wall. (A) Angiography of the right internal thoracic artery (arrow) shows the VM (star) and a drainer (arrowhead) connected to the PA segment 3 (A3). (B) Angiography of the pectoral branch (arrow) at the arterial phase shows the VM (star). Coils (curved arrow) placed for embolization of the drainer connected to the A3 are observed. (C) Angiography of the pectoral branch at the late arterial phase shows drainers (arrowheads) connected to the A4, A5, and A8. The right PA is retrogradely opacified.
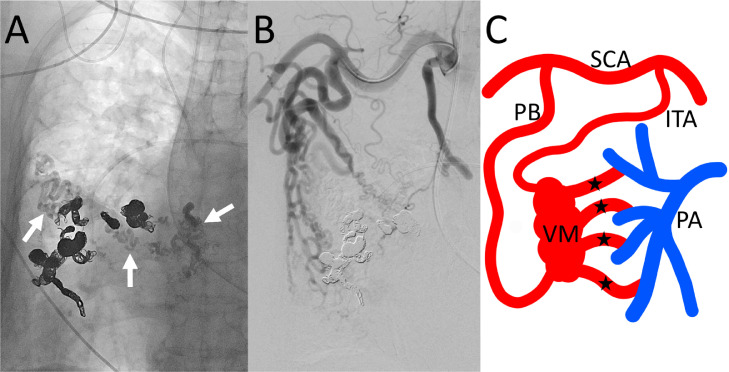
Fig. 3.
Radiograph and angiography after embolization of systemic artery-to-pulmonary artery (PA) vascular malformation (VM) of the right chest wall. (A) Radiograph shows coils placed in drainers and N-butyl cyanoacrylate cast (arrows) injected from the internal thoracic artery and the pectoral branch. (B) Angiography of the right subclavian artery shows decreased enhancement of the VM. (C) Schematic drawing of the embolization procedure. Main drainers (stars) of VM were connected to segmental PAs. These drainers were embolized to coils through the segmental PAs. Then, N-butyl cyanoacrylate mixed with iodized oil was injected from the 2 main feeders: internal thoracic artery and pectoral branch.
ITA, internal thoracic artery; PA, pulmonary artery; PB, pectoral branch; SCA, subclavian artery; VM, vascular malformation.
Discussion
In the present case, we performed retrograde embolization of VM drainers via the PA followed by embolization of the systemic feeders. Transvenous embolization has been reported to be an effective treatment for arteriovenous malformations (AVMs) with a dominant draining vein [7,8]. Occlusion of the dominant draining vein reduces blood flow through the nidus, causing thrombosis [8]. Although the present case had a VM with multiple drainers, which was anatomically different from an AVM with a dominant draining vein, we speculated that embolization of multiple drainers was an effective method of decreasing the blood flow of the VM and performed embolization.
We performed embolization of the systemic feeders after embolization of the drainers. Since the nidus of the VM was far from the origin of the feeders and could not be accessed with a microcatheter, we selected NBCA as an embolic agent to achieve occlusion of the feeders as close as possible to the nidus and, if possible, to embolize the nidus itself. NBCA has been reported to be a useful agent for vessel occlusion in the treatment of AVM [9,10]. One disadvantage of liquid embolic agents is the risk of non-target embolization. We attempted to lower this risk by performing embolization of the drainers prior to injection of NBCA into the feeders. One previous report described the same kind of technique in a case of systemic artery-to-PA VM [4].
In conclusion, embolization of both feeders and drainers is considered an effective technique for the treatment of chest wall systemic artery-to-PA VM.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Institutional Review Board approval was not required for the study because it was a case report.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Consent for publication was obtained for every individual person's data included in the study.
Patient consent
Written consent for publication was obtained from the patient.
Footnotes
Funding: This study was not supported by any funding.
Competing Interests: All authors declare no conflict of interest.
References
- 1.Lawler LP, Fishman EK. Arteriovenous malformations and systemic lung supply: evaluation by multidetector CT and three-dimensional volume rendering. AJR Am J Roentgenol. 2002;178(2):493–495. doi: 10.2214/ajr.178.2.1780493. [DOI] [PubMed] [Google Scholar]
- 2.Itano H, Lee S, Kulick DM, Williams DM, Orringer MB. Nontraumatic chest wall systemic-to-pulmonary artery fistula. Ann Thorac Surg. 2005;79(5):e29–e31. doi: 10.1016/j.athoracsur.2005.01.035. [DOI] [PubMed] [Google Scholar]
- 3.Alsafi A, Shovlin CL, Jackson JE. Transpleural systemic artery-to-pulmonary artery communications in the absence of chronic inflammatory lung disease. A case series and review of the literature. Clin Radiol. 2021;76(9):711e9–711e15. doi: 10.1016/j.crad.2021.03.016. [DOI] [PubMed] [Google Scholar]
- 4.Geyik S, Yavuz K, Keller FS. Unusual systemic artery to pulmonary artery malformation without evidence of systemic disease, trauma or surgery. Cardiovasc Intervent Radiol. 2006;29(5):897–901. doi: 10.1007/s00270-004-0289-9. [DOI] [PubMed] [Google Scholar]
- 5.Cantasdemir M, Kantarci F, Islak C, Kocer N, Saltuk L, Numan F. Transcatheter coil embolization of an intercostal artery to pulmonary artery fistula. Eur Radiol. 2002;12(2):454–457. doi: 10.1007/s003300100974. [DOI] [PubMed] [Google Scholar]
- 6.Iwazawa J, Nakamura K, Hamuro M, Nango M, Sakai Y, Nishida N. Systemic artery to pulmonary artery fistula associated with mitral regurgitation: successful treatment with endovascular embolization. Cardiovasc Intervent Radiol. 2008;31(suppl 2):S99–103. doi: 10.1007/s00270-007-9241-0. [DOI] [PubMed] [Google Scholar]
- 7.Jackson JE, Mansfield AO, Allison DJ. Treatment of high-flow vascular malformations by venous embolization aided by flow occlusion techniques. Cardiovasc Intervent Radiol. 1996;19(5):323–328. doi: 10.1007/BF02570183. [DOI] [PubMed] [Google Scholar]
- 8.Conway AM, Qato K, Drury J, Rosen RJ. Embolization techniques for high-flow arteriovenous malformations with a dominant outflow vein. J Vasc Surg Venous Lymphat Disord. 2015;3(2):178–183. doi: 10.1016/j.jvsv.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Kitagawa A, Izumi Y, Hagihara M, Kamei S, Ikeda S, Katsuda E, et al. Ethanolamine oleate sclerotherapy combined with transarterial embolization using n-butyl cyanoacrylate for extracranial arteriovenous malformations. Cardiovasc Intervent Radiol. 2014;37(2):371–380. doi: 10.1007/s00270-013-0653-8. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert P, Dubois J, Giroux MF, Soulez G. New treatment approaches to arteriovenous malformations. Semin Intervent Radiol. 2017;34(3):258–271. doi: 10.1055/s-0037-1604299. [DOI] [PMC free article] [PubMed] [Google Scholar]