Abstract
Brukina is a millet based fermented milk product which is consumed as a beverage in Ghana. It is however prone to aflatoxin M1 (AFM1) contamination, which is a serious health challenge for low and middle-income countries in subtropical regions. This study aimed at evaluating AFM1 levels and cancer risks associated with brukina (n = 150) sampled from different locations of the Greater Accra Region of Ghana. AFM1 were measured with High-Performance Liquid Chromatography (HPLC) connected to a Fluorescence Detector (FLD).Cancer risk assessments were also conducted using models prescribed by the Joint FAO/WHO Expert Committee on Additives (JECFA). Out of the 150 samples analyzed for AFM1, 80/150 (53%) tested positive between the range 0.00 ± 0.001–3.14 ± 0.77 µg/kg. Cancer risk assessments of AFM1 produced outcomes which ranged between 0.64 and 1.88 ng/kg bw/day, 0.31–9.40, 0.0323, and 1.94 × 10–3–0.06 for cases/100,000 person/yr for Estimated Daily Intake (EDI), Hazard Index (H.I), Average Potency, and Cancer Risks respectively for all age categories investigated. It was concluded that the consumption of brukina posed adverse health effects on the majority of the age categories in the different locations of Greater Accra Region since the calculated H.Is were greater than one (> 1). Therefore, contamination of brukina with AFM1 should be considered a high priority in public health and Ghana’s cancer risk management actions.
Subject terms: Biochemistry, Biotechnology, Microbiology, Natural hazards
Introduction
Milk is a colloidal liquid substance that flows from the mammary glands of animals1. It is a vital source of both micro- and macronutrients and is naturally used to feed young mammals. Children and pregnant women are predominantly the most beneficiaries of milk1,2. Milk, perhaps due to its rich nutrient composition, is highly susceptible to contamination originating either from the animal, the environment, or milk handlers. It is indeed a high risk product which affords optimal conditions for the proliferation of microorganisms when stored under ambient temperature3. Additionally, chemical contaminants may dominate the milk through the feed or treatment of the cow or through later accidental or deliberately contamination.
Brukina, a type of fermented milk and millet smoothie produced and consumed in Ghana, is no exception. This beverage is produced by mixing milled and steam cooked millet with fermented cow milk and sugar4,5. The milk used is usually fermented spontaneously and in some cases, by back slopping with leftover fermented milk. Brukina gets its name from its country of origin, Burkina Faso, a neighboring country to Ghana where the product is called dèguè3,6. Boakye et al.4, Atinmo et al.7 and Baidoo and Kunadu3 accentuated the nutritional, medicinal, economic, and social benefits of brukina cannot go unnoticed as this mixture product of milk and cereal suggests a good source of essential nutrients and probiotics to support the growth and development. This is particularly important in the African region where malnutrition and hunger are very prominent thus; brukina represents a cost-effective meal that can provide the essential nutrients required for growth and development.
In recent times, brukina has gained so much popularity and patronage in Ghana and is considered one of the most successful indigenous beverages in the country, providing employment for many people especially youth. Due to its high patronage, it contends well with other common local beverages such as nunu, asana, ice-kenkey and sobolo3. The significant risk factors associated with contamination of brukina are a cause of worry. Contamination of this milk product is conjectured to originate in 2 directions; firstly, via fermented milk with AFM1 arising from dairy animals eating feeds contaminated by the fungal genus Aspergillus (flavus and parasiticus)2,8 and secondly via fungal contamination of the millet (cereal)9, ultimately resulting in possible production of AFB1, AFB2, AFG1, AFG2 and in combination with some other mycotoxins.
Aflatoxins are hazardous natural secondary metabolites produced by toxic strains of A. flavus and A. parasiticus (fungi of the genus Aspergillus)9 and to a lesser extent by A. nomius. The presence of aflatoxins in a wide range of foods is well known9. There are five different types; aflatoxins B1, B2, G1, G2, and M1 produced primarily in cow milk by cows eating contaminated silage10. Aflatoxins have been reported to work concomitantly with other mycotoxins or in solitude to worsen the risk of hepatocellular carcinoma (HCC), which is reported to be the fifth most frequently occurring cancer in the world10,11. Epidemiological and animal studies have demonstrated that hepatitis B virus (HBV) and AFM1 surge the likelihood of HCC in people with hepatitis B surface antigen-positive (HBsAg+) by 3.3-fold12,13. Neuveut et al.14 asserted that pre-existing liver disease due to HBV infection compromises the ability of hepatocytes to inactivate carcinogens such as aflatoxins thus increasing the chance of HCC.
Safe limits are often set by many counties to control the quantities of aflatoxins permitted in their foods15. This is done presumably because of the food safety hazards that are associated with its ingestion. In addition to setting regulatory limits for mycotoxins, it is also imperative to conduct health risk assessments in the population due to dietary exposure.
Exposure assessment is defined by the Food and Agriculture Organization/World Health Organization (FAO/WHO)16 as a qualitative and/or quantitative assessment of the likely intake of a chemical agent through food, as well as exposure from other sources, if applicable. The methodology was used to assess scientific data in order to calculate the likelihood and severity of a negative event. Risk assessment is a widely established tool for determining the potential linkages between food chain risks and real human health risk17.
In Ghana, few research has been done on the prevalence of AFM1 in some milk products. Nonetheless, to the best of our knowledge, our work is the only one which attempts to estimate the levels and cancer risk involved with the ingestion of AFM1 through a millet-based fermented milk beverage (brukina) in Accra, Ghana. The outcomes of this paper would be expedient in advising policy makers to put their emphasis in adopting international legislations on food quality parameters and to use tools that will change the mindset of the population on risks involving fungal intoxication. The data could also provide proper health education and put emphasis on designing more effective toxigenic fungi and mycotoxin management strategies for Ghana.
Materials and methods
Data collection instruments
Sampling and sample size determination
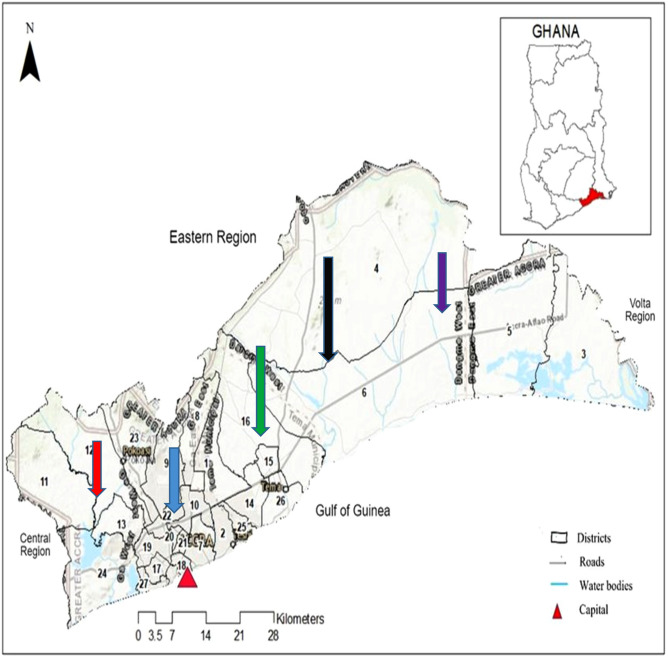
The millet based fermented milk brukina samples were conveniently obtained from local markets in the different locations of Nima, Madina, Kasoa, Ashaiman, and Dodowa in the Greater Accra, Region of Ghana (Table 1 and Fig. 1). These areas are known to have high patronage of milk products due to nomadic inhabitants. Approximately 300 ml each of brukina were bought and stored in an ice chest (Thermos 7750, China) with cold packs at temperature 10 °C under aseptic conditions and transported to the laboratory in batches where they were stored in the freezer compartment of a refrigerator until these were analyzed for AFM1.
Table 1.
Geographical locations and some attributes of the origin of brukina samples obtained from Greater Accra region of Ghana.
| Region | No. of samples | Agro-ecological zones | Coordinates |
|---|---|---|---|
| Nima | 30/150 | Coastal Savannah | 5.5820°N, 0.1984°W |
| Madina | 30/150 | Coastal Savannah | 5.6731°N, 0.1664° W |
| Kasoa | 30/150 | Coastal Savannah/deciduous | 5.5200°N, 2.1450°W |
| Ashaiman | 30/150 | Coastal Savannah | 6.2374°N, 0.4800°W |
| Dodowa | 30/150 | Coastal Savannah/rain forest | 5.8829°N, 0.0980°W |
Figure 1.
Map of Greater Accra Region and neighbouring regions (Adapted from18). Sampling sites are shown in red arrow (Kasoa), blue arrow (Nima), green arrow (Madina), black arrow (Ashaiman), and violet arrow (Dodowa).
A total number of 150 brukina samples were used. This was determined with a Raosoft sample size calculator (http://www.raosoft.com/samplesize.html) with parameters: margin of error (8%), confidence Interval (95%), population of Accra (2,000,000) and response distribution (50%).
Preparation of samples
After warming at about 37 °C in a water bath, the samples were centrifuged at 2000g to separate fat layers and then filtered. The prepared test portion of 50 mL was transferred into a syringe barrel attached to AFM1 immunoaffinity column and passed at a slow steady flow rate of 1–2 mL/min. The columns were then washed with 20 mL deionized water and the air was passed through the columns to dryness. AFM1 was eluted with 4 mL pure acetonitrile by allowing it to be in contact with the column for not less than 60 s. The eluate was evaporated to dryness using a gentle stream of nitrogen. The residue was dissolved in 500 µL of mobile phase and filtered using a membrane filter before being injected into HPLC for quantification.
Chemicals and standards
The analytical standard of AFM1 was supplied by Sigma-Aldrich (St. Louis, MO, USA). All solvents used for the preparation of the mobile phase were HPLC grade and obtained from Merck (Darmstadt, Germany). All homogenized mixtures and eluates were filtered through Whatman no. 4 and 0.45 mm membrane filters, respectively (Whatman plc, Maidstone, UK). De-ionized water was obtained with a Millipore Elix Essential purification system (Bedford, MA, USA). EASI-EXTRACT AFM1 immunoaffinity columns (stored at 4 °C until use) were supplied by R-Biopharm, Rhone limited, and used for SPE and cleanup.
Preparation of standard solutions
A mother stock solution (0.1 μg/mL) was prepared from a standard solution of AFM1 (0.993 μg/mL in acetonitrile) and stored with care in the freezer. A working stock solution of 0.01 μg/mL was diluted step by step with the combined solution (acetonitrile/water, 75/25, v/v) to prepare a sequence of working solutions that were stored in vials below 4 °C for the calibration curve. Calibration solutions of 0.02 μg/kg, 0.04 μg/kg, 0.06 μg/kg, 0.08 μg/kg, and 0.10 μg/kg were used. Samples with AFM1 amount above the calibration range were diluted and dilution factors were applied for quantification.
Instrumentation
Agilent high-performance liquid chromatography system (HPLC 1260 infinity series) with a quaternary pump and fluorescence detection was used for AFM1 quantification analysis and was carried out as per the method given by EN ISO 14501:200719. Data acquisition and quantification were done using Chem station (Open Lab edition). The Agilent HPLC equipped with a fluorescence detector was set at an excitation wavelength of 360 nm and an emission wavelength of 440 nm and the column compartment (HPLC Column: TC-C18 (2), 170, 5 µm, 4.6 × 250 mm; thus, a pore size of 170, particle size of 5.0 µ, inner diameter of 4.6 mm, length of 250 mm and carbon load of 12%) temperature regulated at 35 °C. The mobile phase was a mixture of water and acetonitrile at ratios of 25:75 (v/v), respectively, and an isocratic delivery mode was employed at a flow rate of 0.8 mL min−1 with an injection volume of 10 µL.
Validation
HPLC-FLD method was validated according to the guidelines of European Commission Decision 657/2002/EC for confirmatory analysis methods and the tested parameters were linearity, limit of detection (LOD), limit of quantification (LOQ), accuracy, precision, and selectivity. The linearity was assessed by constructing five-point solvent matched calibrations in triplicate for AFM1 standard solutions in the concentration range of 0.05 to 0.8 mg/L. Calibration curves were drawn by plotting the peak area against AFM1 concentration, and linearity was evaluated by linear regression analysis expressed as coefficient of determination (r2).
The precision of the method was estimated in terms of % RSD of three identical extractions of brukina samples spiked with AFM1 at the same as well as at three different spiking levels. Method selectivity was evaluated by analyzing AFM1 known negative milk matrix and reagent blank to determine any interference from endogenous substances around the retention time of the target analyte.
Method precision was estimated using intermediate precision and repeatability. For repeatability estimates, 10 different samples were taken from the same lot and each of the 10 samples spiked at the same concentration and analyzed at the same time on the same day. Three replicate measures were made for each of the 10 and the relative standard deviation (RSD) calculated.
For intermediate precision, 6 different samples were taken from the same lot and each of the 6 samples spiked at the same concentration on different days and analyzed by 3 different analysts over a 6-day period. Three replicate measures were made for each of the 6 and RSD calculated.
Mean peak area showed a proportionate increase with that of standard concentration and the calibration curves of AFM1 demonstrated a good regression line (r2 > 0.99) in the range of explored concentrations. For the recovery analysis, samples previously tested to guarantee the nonappearance of the studied mycotoxins were used in the validation procedure. The Limits of Detection for AFM1 ranged between 0.13 and 0.15, while Limits of Quantification ranged between 0.26 and 0.30, respectively, for both.
Human risk assessment of exposure to AFM1 via consumption of brukina milk
Estimation of exposure
Estimated Daily Intake (EDI) was considered by using the mean amount of AFM1 derived from the milk samples, the number of samples consumed daily, and the average body weight. The EDI for mean aflatoxin was premeditated according to the following formula (1) and expressed in μg/kg of body weight/day (μg/kg bw/day)20,21;
| 1 |
The daily intake of milk in Ghana according to Omore et al.22 is approximately 0.0137 kg/day (5.0 kg/year).
The different age categories according to EFSA23 and their corresponding estimated average weights in Ghana used in this study were done as follows; Infants—2.9 (2.5–3.2) kg24,25, Toddler—9.8 (7–12.6) kg26,27, Children—26 (24–28) kg28,29, Adolescents—46.25 (38.5–54) kg30, Adults—60.7 kg31.
Population risk characterization for aflatoxins
Hazard Index (H.I)
Genotoxic and carcinogenic compounds such as aflatoxins have their risk assessment fittingly computed based on the Hazard Index (H.I). The tolerance daily intake (TDI) value for AFM1 was 0.2 ng/kg/day as suggested by Kaur et al.32, which was calculated by multiplying the TD50 (threshold dose/bw) by 5000. If the H.I of AFM1 does not exceed 1, the consumer is presumably safe; however, if the H.I of AFM1 is greater than 1, the consumer may be at risk of liver cancer33.
| 2 |
The HI of AFM1 for the milk and milk products studied was estimated using the formula above.
Estimated liver cancer risk due to consumption of ‘brukina’ samples
The ingestion of aflatoxins can be linked to the onset of liver cancer34,35. Therefore, liver cancer risk estimation for Ghanaian adult consumers was calculated for aflatoxins35,36. This involved estimating the population cancer risk per 100,000, which is a product of the EDI value and the average hepatocellular carcinoma (HCC) potency figure from individual potencies of Hepatitis B surface antigen (HBsAg) (HBsAg-positive and HBsAg-negative groups).
The JECFA37 estimated potency values for AFM1 which corresponded to 0.3 cancers/year/ 100,000 population ng/kg bw/day (uncertainty range: 0.05–0.5) in HBsAg-positive individuals and 0.01 cancers/year/100,000 population ng/kg bw/day (uncertainty range: 0.002–0.03) in HBsAg-negative individuals35 were adopted for this calculation. Moreover, the average HBsAg+ prevalence rate of 7.74% (adult—8.36%, 14.3%—adolescents, 0.55%—children) for Ghana38,39 was adopted and 92.26% (100–7.74%) was extrapolated for HBsAg-negative groups. Hence, the average potency for cancer in Ghana was estimated as follows according to Eq. (7) as prescribed by35 and36:
| 3 |
Thus, cancer risk (cancers per year per 100,000 population per ng aflatoxin /kg bw/day) was estimated using the following formula in Eq. (4)34,36:
Thus, the population risk was estimated using the following formula in Eq. (4):
| 4 |
Statistical analysis
The aflatoxin concentrations were calculated using regression analysis from the curves generated from the standards of aflatoxin M1 with Excel for Microsoft Windows (version 10). One sample t-test was used to compare the means obtained at a 95% confidence interval and 5% level of significance. The statistical results were summarized as median, standard deviation, variance, skewness, standard error of skewness, kurtosis and standard error of kurtosis and mean values (range from the 25th percentile to the 75th percentile). SPSS 22 (Chicago, USA) was used in the analysis of data. Deterministic risk assessment model calculations for aflatoxins, dietary exposure (Estimated Dietary Intake), H.I values, Average potency, and cancer risk were calculated.
Results
The mean recovery percentage of AFM1 in spiked milk samples were found between 80.5 and 84.07% with % RSD from 3.19 to 5.42. Since, the recoveries and % RSD were within the EC regulation.
The summary of statistics of the number of food samples contaminated with AFM1 is presented in Table 2. The level of occurrence of the AFM1 ranged between 0–2.30 µg/kg, 0–3.02 µg/kg, 0–3.14 µg/kg, 0–2.11 µg/kg, and 0–2.14 µg/kg respectively for Nima, Kasoa, Madina, Ashaiman and Dodowa in the Greater Accra Region.
Table 2.
Summary of statistics of AFM1 in fermented milk beverage brukina obtained from five different areas of Greater Accra region, Ghana.
| Nima | Kasoa | Madina | Ashaiman | Dodowa | |
|---|---|---|---|---|---|
| No. of samples | 30 | 30 | 30 | 30 | 30 |
| Mean | 0.2737 | 0.7973 | 0.5017 | 0.6263 | 0.5780 |
| Std. error of mean | 0.098 | 0.16071 | 0.140 | 0.12131 | 0.12318 |
| Median | 0.0400 | 0.6200 | 0.000 | 0.5850 | 0.0000 |
| Std. deviation | 0.54218 | 0.88022 | 0.767 | 0.6644 | 0.6746 |
| Variance | 0.294 | 0.775 | 0.589 | 0.441 | 0.455 |
| Skewness | 2.493 | 0.821 | 1.834 | 0.615 | 0.612 |
| Std. error of skewness | 0.427 | 0.427 | 0.427 | 0.427 | 0.427 |
| Kurtosis | 6.265 | − 0.360 | 3.762 | − 0.828 | − 0.957 |
| Std. error of kurtosis | 0.833 | 0.833 | 0.833 | 0.833 | 0.833 |
| Range | 2.30 | 3.02 | 3.14 | 2.11 | 2.14 |
| Percentiles | |||||
| 25 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| 50 | 0.040 | 0.6200 | 0.000 | 0.5850 | 0.000 |
| 75 | 0.160 | 1.4750 | 0.930 | 1.1125 | 1.1275 |
Nima recorded comparatively less mean and median values of AFM1 concentrations than all localities (Kasoa, Madina, Ashaiman, and Dodowa) investigated. The skewness and kurtosis were 2.493 and 6.265, respectively and showed that the data set of AFM1 obtained in this town was asymmetrical and heavy-tailed (Table 2). The lower and upper limits were 0.0712 and 0.4761, respectively, and showed significant differences (p < 0.05) (Table 3).
Table 3.
Statistics of the one-sample t-test of brukina samples from different parts of the Greater Accra region, Ghana.
| Positive AFM1 (%) | t | df | Sig. (2-tailed) | Mean difference | 95% confidence interval of the difference | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Nima | 17/30(56.7) | 2.765 | 29 | 0.010 | 0.27367 | 0.0712 | 0.4761 |
| Madina | 12/30(40) | 3.581 | 29 | 0.001 | 0.50167 | 0.2152 | 0.7882 |
| Kasoa | 19/30(63.3) | 4.961 | 29 | 0.000 | 0.79733 | 0.4687 | 1.1260 |
| Ashaiman | 18/30(60) | 5.163 | 29 | 0.000 | 0.62633 | 0.3782 | 0.8744 |
| Dodowa | 14/30(46.7) | 4.692 | 29 | 0.000 | 0.57800 | 0.3261 | 0.8299 |
For Kasoa, greater values of mean and median AFM1 concentrations than Madina, Ashaiman, and Dodowa were recorded from the summary statistics. Values of 0.821 and − 0.360 were recorded as skewness and kurtosis and implied moderate skewness and light-tailed. The upper and lower limits were 0.4687 and 1.1260. Values significantly differed (p < 0.05) (Tables 2 and 3).
The mean and median concentrations of AFM1 recorded in Madina were comparatively greater than Nima but lesser than Kasoa, Ashaiman, and Dodowa. While the data set showed symmetrical and light-tailed as, the skewness and kurtosis were 1.834 and 3.762, respectively (Table 2). Values of 0.2152 and 0.7882 were recorded as upper and lower limits. There were significant differences (p < 0.05) observed (Table 3).
For Ashaiman, we recorded greater mean and median concentrations of AFM1 than Dodowa, Madina, and Nima. However, the values were lesser than Kasoa, data set for Ashaiman was fairly symmetrical and light-tailed; 0.615 and − 0.67 for skewness and kurtosis, respectively. Upper and lower limits of 0.3782 and 0.8744 were, respectively, recorded. There were significant differences (p < 0.05) (Tables 2 and 3).
Lastly, for Dodowa, we recorded lesser mean and median values of the concentrations of AFM1 than Kasoa and Ashaiman but not Nima and Madina. The data set for Dodowa was fairly symmetrical and light-tailed; 0.612 and − 0.597 for skewness and kurtosis, respectively. Upper and lower limits of 0.3261 and 0.8299 were, respectively, recorded. There were significant differences (p < 0.05) (Tables 2 and 3).
Regarding the frequency and (percentage %) of positive AFM1 in contaminated brukina samples, values recorded for overall positive samples was 80/150 (53%) while the different locations recorded values of 17/30 (56.7%), 12/30 (40%), 19/30 (63.3%), 18/30 (60%) and 14/30 (46.7) for Nima, Madina, Kasoa, Ashaiman and Dodowa respectively (Table 3).
Risk assessment
The Estimated Daily Intakes (EDI) of AFM1 in the brukina samples from Nima were 0.64, 0.38, 0.14, 0.079, and 0.061 ng/kg bw/day for infants, toddlers, children, adolescents, and adults respectively. The Harzard Index (H.I) values recorded were 3.20, 1.90, 0.70, 0.40, and 0.31, respectively, and implied an adverse health risk for infants and toddlers. The average potency of the aflatoxins was 0.0323 aflatoxins ng/kg bw/day and produced cancer risks of 0.0206, 0.0122, 4.52 × 10–3, 2.55 × 10–3, and 1.97 × 10–3 cases/100,000 person/yr respectively (Table 4).
Table 4.
Risk evaluation for AFM1 via consumption of brukina samples obtained from Greater Accra region of Ghana.
| Locality | Av. body wgt. (kg) | Estimated daily intake (EDI) (ng/kg bw/day) | Hazard Index (H.I) | Cancer risk (cases/100,000 person/yr) | |
|---|---|---|---|---|---|
| Nima | Infants (0–11 mths) | 2.9 | 0.64 | 3.2 | 0.0206 |
| Toddlers (12–35 mths) | 9.8 | 0.38 | 1.90 | 0.0122 | |
| Children (36 mths–10 yrs) | 26 | 0.14 | 0.70 | 4.52 × 10–3 | |
| Adolescents (11–17 yrs) | 46.25 | 0.079 | 0.40 | 2.55 × 10–3 | |
| Adults (18–64 yrs) | 60.7 | 0.061 | 0.31 | 1.97 × 10–3 | |
| Madina | Infants (0–11 mths) | 2.9 | 1.185 | 5.93 | 0.038 |
| Toddler (12–35 mths) | 9.8 | 0.70 | 3.50 | 0.02261 | |
| Children (36 mths–11 yrs) | 26 | 0.264 | 1.30 | 8.52 × 10–3 | |
| Adolescents (11–17 yrs) | 46.25 | 0.149 | 0.75 | 4.813 × 10–3 | |
| Adults (18–64 yrs) | 60.7 | 0.113 | 0.57 | 3.65 × 10–3 |
Mean of AFM1—Nima = 0.27 µg/kg, Madina = 0.5017 µg/kg.
Daily intake of milk for infants was halved (0.5 × 0.0137 kg).
Average body weights were obtained from the different ranges referenced by the authors.
Average potency for AFM1 = 0.0323.
1 µg = 1000 ng.
H.I Hazard Index.
Madina recorded EDI values of 1.185, 0.70, 0.264, 0.149, and 0.113 ng/kg bw/day for infants, toddlers, children, adolescents, and adults respectively. H.I values were 5.93, 3.50, 1.30, 0.75, and 0.57 and pointed at an adverse health risk for infants, toddlers, and children. The average potency was the same. Cancer risks of 0.038, 0.02261, 8.52 × 10–3, 4.813 × 10–3, and 3.65 × 10–3 cases/100,000 person/yr respectively for these age categories were recorded (Table 4).
For Kasoa, the EDI values recorded for infants, toddlers, children, adolescents, and adults were 1.88, 1.1142, 0.420, 0.236, and 0.180 ng/kg bw/day respectively. H.I values recorded were 9.40, 5.57, 2.10, 1.18, and 0.90, respectively, which showed adverse health risk for infants, toddlers, children, and adolescents. The average potency was the same as other regions, while the cancer risks were 0.07, 0.04, 0.014, 8.08 × 10–3, and 6.14 × 10–3 cases/100,000 person/yr respectively (Table 5).
Table 5.
Risk evaluation for AFM1 via consumption of brukina samples obtained from Greater Accra region of Ghana.
| Locality | Av. body wgt. (kg) | Estimated daily intake (EDI) (ng/kg bw/day) | Hazard Index (H.I) | Cancer risk (cases/100,000 person/yr) | |
|---|---|---|---|---|---|
| Kasoa | Infants (0–11 mths) | 2.9 | 1.88 | 9.40 | 0.0607 |
| Toddlers (12–35 mths) | 9.8 | 1.1142 | 5.57 | 0.0359 | |
| Children (36 mths–10 yrs) | 26 | 0.420 | 2.10 | 0.01356 | |
| Adolescents (11–17 yrs) | 46.3 | 0.236 | 1.18 | 7.62 × 10–3 | |
| Adults (18–64 yrs) | 60.7 | 0.180 | 0.90 | 5.814 × 10–3 | |
| Ashaiman | Infants (0–11 mths) | 2.9 | 1.479 | 7.40 | 0.05 |
| Toddlers (12–35 mths) | 9.8 | 0.875 | 4.38 | 0.03 | |
| Children (36 mths–10 yrs) | 26 | 0.330 | 1.65 | 0.01 | |
| Adolescents (11–17 yrs) | 46.3 | 0.185 | 0.93 | 6.46 × 10–3 | |
| Adults (18–64 yrs) | 60.7 | 0.141 | 0.71 | 4.85 × 10–3 | |
| Dodowa | Infants (0–11 mths) | 2.9 | 1.365 | 6.83 | 0.044 |
| Toddlers (12–35 mths) | 9.8 | 0.808 | 4.04 | 0.0260 | |
| Children (36 mths–10 yrs) | 26 | 0.305 | 1.53 | 9.85 × 10–3 | |
| Adolescents (11–17 yrs) | 46.3 | 0.171 | 0.86 | 5.523 × 10–3 | |
| Adults (18–64 yrs) | 60.7 | 0.130 | 0.65 | 4.199 × 10–3 |
Means of aflatoxins M1—Kasoa—0.79 µg/kg, Ashaiman—0.62 µg/kg, Dodowa—0.5780 µg/kg.
Daily intake of milk for infants was halved (0.5 × 0.0137 kg).
Average Body weights were obtained from the different ranges referenced by the authors.
Average potency for AFM1 = 0.0323.
1 µg = 1000 ng.
H.I Hazard Index.
At Ashaiman, the EDI values recorded for infants, toddlers, children, adolescents, and adults were 1.479, 0.875, 0.330, 0.185, and 0.141 ng/kg bw/day respectively. H.I values recorded were 7.40, 4.38, 1.65, 0.93, and 0.71, respectively, implying an adverse health risk for infants, toddlers, and children. The average potency was the same as other regions, while the cancer risks were 0.05, 0.03, 0.01, 6.46 × 10–3, and 4.85 × 10–3 cases/100,000 person/yr respectively (Table 5).
Lastly, for Dodowa, the EDI values recorded for infants, toddlers, children, adolescents, and adults were 1.88, 1.114, 0.42, 0.236, and 0.180 ng/kg bw/day respectively. H.I values recorded were 9.40, 5.57, 2.10, 1.18, and 0.90, respectively, and suggested an adverse health risk for infants, toddlers, children, and adolescents. The average potency was the same as other regions, while the cancer risks were 0.044, 0.0260, 9.85 × 10–3, 5.523 × 10–3, and 4.199 × 10–3 cases/100,000 person/yr respectively (Table 5).
Discussion
According to Bhaskar40, all around the globe, consumption of unsafe food results in approximately 420,000 deaths annually and is the cause of more than 200 diseases ranging from diarrhoea to cancer. Brukina is consumed by most Ghanaians as a beverage served chilled with ice blocks and is conjectured to be prepared under unhygienic conditions. Again, the milk used for its preparation is repeatedly prone to contamination with AFM1 making it unsafe. In these present investigations, Nima had a comparatively low mean concentration of 0.27 µg/kg and significantly differed (p < 0.05) from the mean concentrations of the other towns which had greater (> 0.5) concentrations. Conversely, there was an observed a greater number of positive samples got from Nima, Kasoa as well as Ashaiman. Our results point at comparatively moderate levels of AFM1 contamination in brukina samples from different locations of Greater Accra region of Ghana. They were within the range of 0–3.14 µg/kg (3140 ng/kg) and compared satisfactorily well with some published findings of some researchers around the globe.
From Ghana, Addo-Boadu41 recorded AFM1 levels in a range of 0.35–3.76 µg/L (350–3760 ng/L) in raw milk and milk products samples from the Greater Accra Region. In Tanzania, studies conducted on raw cow milk samples revealed 83.3% (31/37) of aflatoxin contamination in cows that fed on sunflower cake in the range of 0.026–2.007 µg/kg (26–2007 ng/kg) (exceeding both Tanzania’s and EC allowable value which is 0.05 µg/kg42.
Several studies have reported the occurrence of AFM1 in milk and dairy products. Milk samples from urban centers in Kenya contained AFM1 up to 6800 ng/L43. In Sudan, 95% of milk was contaminated with AFM1 ranging between 220 and 6800 ng/L44, whereas 6–527 ng/L of AFM1 was detected in 15% of cow milk samples from Cameroon45. The concentration of AFM1 varied between 150 and 170 ng/L in commercial and rural milk in South Africa46, while 100% of milk samples in Nigeria contained AFM1 and the levels were within the range of 0.004–0.845 µg/L (4–8450 ng/l). Goncalves et al.47 reported AFM1 levels in fresh bovine milk to be in between the range of 0.09–3.385 µg/L (90–3385 ng/L) per their work. The least amount of data is available from African countries, nonetheless the available data suggest the highest prevalence and frequent detection levels48. Lower values were recorded by49 in milk from Sudan and found 33% of the milk samples with the highest occurrence (82.4%) in cow milk (35.3% ranged between 0.05 and 0.1 μ/kg and 47.1% ranged between 0.1 and 0.15 μ/kg) and milk samples from a camel in semi-intensive systems (15.6% ranged between 0.05 and 0.1 μg/kg). Again, all samples of milk from traditional nomadic systems indicated an absence of AFM1.
Makun et al.50 also reported contamination of raw cow milk with AFM1 at levels higher than the EU permitted levels in Nigeria. In their study, contamination of raw cow milk (from a nomadic cow) with AFM1 ranged from 0.0109 to 1.3543 µg/L (10.9–1354.3 ng/L) with and an average concentration of 0.5308 ± 0.0938 µg/L (530.8 ng/L). For commercial cow’s milk, AFM1 contamination ranged between 0.0464–0.0992 (46.4–99.2 ng/L) and 0.0584 ± 0.0052 µg/L (58 ng/L) as the mean. A similar trend regarding levels of AFM1 contamination of 0.05 µg/kg has also been reported in a study conducted in Brazil by51. From Egypt, Amer et al.52 reported a prevalence of 38 positive samples with a range of 0.023–0.073 µg/L (23–73 ng/L) in raw milk. Also, Rahimi et al.53 reported mean values of 0.0601, 0.0319, 0.0190, 0.0281, and 0.0301 µg/L (60.1, 31.9, 19.0, 28.1, and 30.1 ng/L) respectively for raw cow, water buffalo, camel, sheep, and goat milk from Iran.
Milk in Europe is time and again analyzed for AFM1 and is also averred to be the safest54. From Portugal, Duarte et al.55 reported values of range n.d–0.069 µg/L (nd–69.0 ng/L) in 99.4% positive raw milk samples. From Spain, Rodriguez-Blanco et al.56 and Cano-Sancho et al.57 reported ranges of n.d–0.2 µg/L (n.d–200 ng/L) and 0.009–1.36 µg/L (9–1360 ng/L) respectively for raw milk samples. From Serbia, Kos et al.58 and Tomasevic et al.59 reported ranges of 0.01–1.2 µg/L (10–1200 ng/L) and 0.09–0.145 µg/L (90–1450 ng/L) respectively for milk. Furthermore, in Croatian milk, values of 0.006–0.027 µg/L (6–27 ng/L) were reported by60. AFM1 levels were recorded in Italy by61 and62, all pointed at results below 0.05 µg/kg. Available data shows an irregular pattern of results which does not portray low levels to suggest total safety as no amount of AFM1 is Generally Regarded as Safe (GRAS).
In other parts of the world, Iha et al.63 from Brazil, reported 83% of the milk samples tested positive for AFM1, in a range of 0.008 to 0.760 ng/g and in India, almost half of the analyzed milk was contaminated, with 44% being above EU limit64. Greater quantities of AFM1 have been reported across the globe. Lee et al.65 from South Korea reported values of 0.22–6.9 µg/l (220–6900 ng/L) in raw milk. From Pakistan, Iqbal et al.66 reported values of 0.02–3.09 µg/l (20–3090 ng/L).
The contamination rate and levels of AFM1 in fermented milk obtained in this study may be because dairy animals kept in local dairy farms were fed with compound rations stored under poor conditions and may have favored the growth of toxicogenic fungi expressly Aspergillus sp. which can in due course, be contaminated with aflatoxins. Again, hot and humid climatic conditions are very conducive for fungal invasion, growth, and production of mycotoxins including aflatoxins in food and feed commodities67. Unseasonal rains and related flash floods are widespread, and this increases the moisture content of the grains and other feedstuff, and therefore its vulnerability to fungal attacks. Indeed, several previous reports indicated the presence of high levels of aflatoxins in dairy animals' feed and ingredients from Ghana.
Moreover, most of the dairy farmers prefer to feed cereals (maize, wheat, etc.) or agricultural or oilseed byproducts (peanuts, soybean, etc.) to their dairy animals, and such aflatoxin susceptible feed materials constitute more than 70% of cattle feed67. Therefore, if such high aflatoxin contaminated feedstuff is included in the diet of dairy animal's, there is always a great possibility of AFM1 appearing in milk at high levels. Other probable factors which may play an important role in the high levels of AFM1 in milk in this study include poor farm management practices especially feed storage practices, no legal limits of aflatoxins exist for livestock feed, and lack of knowledge among dairy farmers concerning aflatoxins.
Aflatoxin exposure early in life has been associated with impaired growth, particularly stunting68. Furthermore, early exposure to aflatoxins is a potential risk for synergistic interactions with other toxins as subjects grow69,70. Weaning is a transition period of a child from breast milk to other sources of food, which often results in a marked decrease in nutrient intake in developing countries71. One possible variable contributing to poor child health in developing countries is the increased exposure to aflatoxin-contaminated foods following weaning72.
Comparatively greater quantities of AFM1 were detected in other parts of the world by other researchers. In the global context, AFM1 levels found in Ghanaian milk are moderate. Flores-Flores et al.48 have reviewed the presence of AFM1 in cow's milk from various parts of the world. Of the 22,189 milk samples analyzed that were taken into account, at least 9.8% of them (2190 samples) exceeded the maximum AFM1 content established by the EU. Regarding the number of noncompliant samples per continent, 1709 came from Asia, 253 from Africa, 119 from Europe, and 109 from America. Gizachew et al.73 and Skrbic et al.74 emphasized several factors such as geographical region, season, type and quality of feed, feed storage conditions, and processing methods and conditions that are responsible for the variability of AFM1 in milk and dairy products. Lack of fresh forage as feed might have led to longer storage of hay or feed leading to contamination of Aspergillus sp. leading to AFB1 contamination.
Risk assessment
The public health significance of AFM1 levels in milk has never been fully revealed. The risk of cancer development involved with the prolonged ingestion of mycotoxin, which is by and large linked to its concentration. In the present study, the age categories of infants, toddlers, children, and adolescents were found to be the most at risk of adverse health effects (Hepatocellular carcinoma) while the adult populations were not at risk. Whereas some research works have found an association between stunting and aflatoxins75, proof of its causes is still absent. In Kenya, an association between AFM1 exposure and lower height-forage scores. Similarly, a study in Iran showed that infants of mothers which had AFM1 in their breast milk had lower height-for-age scores76. A recent scoping review by Soriano et al.77 showed the presence of these aflatoxins appeared in greater proportion in kwashiorkor in children and in different organs and biological samples including brain78, heart79, kidney80, liver79, lung81, serum82, stool83 and urine45,82 whereas in the marasmic-kwashiorkor they were detected in similar parts.
Aflatoxins are unaffected by many food processing techniques such as boiling or pasteurization, etc. as they are heat stable84. There is always a risk involved with their association with food or feed. Risk estimations as explained by Liu and Wu85 as well as Kuiper-Goodman86 are modeled to predict the magnitude of adverse health implications of mycotoxin exposure and guide food regulators to set thresholds for these toxins in foodstuffs. H.I results obtained in this study implied a high risk for infants, toddlers, children, and adolescents (total aflatoxins).
Considering the EDI values obtained in a study by Addo-Boadu41 in Ghana for infants i.e., 3.679 ± 2.213 and 2.445 ± 2.001 ng/kg bw/day, it exceeded 1 ng/kg bw/day by far and indicated the serious risk of AFM1 through raw cow milk consumption for this age category.
Our findings corroborated published findings of Kaur et al.32, which indicated EDI and HCC values of 2.30 and a range of 0.0020–0.0106, respectively. Their health risk assessment revealed that customers in the research area, particularly youngsters, are at a higher risk of AFM1 infection due to their low body weight and increased milk consumption.
Recently from Malawi, Njombwa et al.13 reported a probable mean daily exposure to AFM1 for adults as 4.98 ± 7.25 ng/kg bw/day and almost double for children (8.28 ± 11.82 ng/kg bw/day). The estimated risk of AFM1-induced HCC associated with consumption of milk among children and adults were 0.038 and 0.023 cases per 100,000 individuals per year, respectively. Their results suggested a low risk of hepatocellular carcinoma (HCC).
The incidence of liver cancer in Iran was 3.53 cancers per year per 105 persons or 3530 cancers/yr/108 persons87 and AFM1 intake through yogurt contributed 0.023–0.048 cancers/yr/108 person for mean consumers and 0.028–0.069 cancers/yr/108 person for high consumers. Therefore, their findings indicated AFM1 in yogurt contributed a slight part to the overall incidence of liver cancer in the Iranian population. The intake of AFM1 and liver cancer incidence due to the consumption of this mycotoxin through yogurt and milk have been reported in other countries including China, Spain, Greece, and Serbia57,88,89.
The range of liver cancer incidence or hepatocellular carcinoma (HCC) due to AFM1 intake through milk and yogurt was 0.025–0.033 case or cancers/yr/108 person in China, was similar to the results of this study in Serbia and Greece was 3.6–0.4.7 and 0.7–0.9 case or cancers/yr/108 person, respectively that it was higher than the current study. These distributes were related to the AFM1 level and consumption value of yogurt.
Studies by Serraino et al.90 from Italy, the EDI of AFM1 in different population groups were in the range of 0.025–0.328 ng/kg bw/day, based on the average consumption levels and weighted mean contamination of milk in the study period. The estimated fractions of HCC incidences attributable to AFM1 intake were 0.005 and 0.004 cases per 100,000 individuals in the 0–0.9 and 1–2.9-year age groups, respectively, and below 0.004 cases in the other age categories which posed adverse health consequences.
Trevisani et al.91 in a related study, reported 0.011–0.057 cases/100,000 people in different age categories in an Italian population. The estimated fraction of the incidence of HCC in the Italian population projected a slight increase in cases due to milk consumption.
The Survey of the AFM1 contamination level of commercially available pasteurized milk and raw milk in Japan showed that the average concentration ± standard deviation of AFM1 was 0.009 ± 0.0004 μg/kg in commercially available milk and 0.0074 ± 0.0047 μg/kg in raw milk. The survey of the AFM1 contamination level of powdered infant formula indicated that the average The concentration of AFM1 was 0.002 μg/kg when converted to the concentration in the formula.
Estimation of carcinogenic risk based on the lifetime exposure to AFM1 calculated from these values suggest that the risk is extremely low in the present situation92.
It is worthy to note that despite the higher AFM1 levels found in milk of African origin, presumably due to the ability of Aspergillus species to flourish better under tropical climate93,94 thus producing the parent compound AFB1, which is metabolized into AFM1 by mammals and subsequently secreted into milk95 viz-a-vis industrialized countries in temperate regions, it appears that the dietary exposure could generally be low due to low amount of milk consumed. For instance, JECFA96,97 estimated milk consumption per person at 42 mL/day for African countries, which was about 8–9 times lower compared to a consumer in the industrialized countries. Thus, at 60 kg body weight, average daily exposures were lower in African countries (0.002 ng/kg bw/day) compared to 0.11 ng/kg bw/day for consumers in developed countries96,97. For the reason that, to a large extent aflatoxins possess carcinogenic potential, JECFA98 established that daily exposure, not exceeding 1 ng/kg bw, contributes to the risk of liver cancer. In the face of the anticipated risk of cancer incidence that can be gotten from AFM1 in this study, the effects of AFM1 on health, and especially the combined effects of mixtures of mycotoxins, the additive effects of aflatoxins, other dietary contaminants, alcohol consumption, and poor diet on cancer risk remains largely unknown.
The range of results for AFM1 in brukina obtained from Greater Accra region may vary from that of different regions since conditions of silage storage and feed that influence the growth and survival of the Aspergillus species, may change and therefore change the contamination levels.
Conclusion
From the findings of this study, it can be deduced that a moderate percentage 53% of millet- based fermented milk beverage brukina samples collected in different locations of Greater Accra Region of Ghana proved to have AFM1 contents, it further showed a public health concern considering the adverse health especially hepatocellular carcinoma (HCC) outcome of the health risk assessments since the calculated H.Is were greater than one (> 1) in mostly infants (all localities), toddlers (all localities), children (Madina, Kasoa, Ashaiman, Dodowa) and adolescents (Kasoa, Dodowa) age categories.
In spite of the important role of milk, especially dairy products in the human diet, there is a great concern about the presence of AFM1 in milk and dairy products. Additional negative health effects of AFM1 justify its continuous monitoring and update of risk assessment. Hence, it is imperative to use fast methods in the detection of AFM1 in brukina as well as milk and dairy products. Ghanaian public health authorities have to monitor ceaselessly to detect AFM1 contamination and need to be suppressed to an ALARA (as low as reasonably achievable) level.
Although the sampling sites chosen in the present study were representative enough of Accra to draw sufficient statistical conclusions, many more sites could have been added. Again, brukina samples cannot be obtained in all areas but only in particular areas where cattle are reared and so makes it difficult to access.
Some novel risk assessment approaches like simulated distribution, Log-N, and some others could be employed or adapted as possible tools or areas for future studies.
Acknowledgements
We acknowledge and sincerely extend our heartfelt appreciation to Mr. Francis Nyasem and Mr. Precious Agbemeseli, both Department of Nutrition and Dietetics, University of Health and Allied Sciences for their enormous efforts in data collection. A big thank you also goes to the staff of Food Chemistry and Nutrition Research Division, CSIR- Food Research Institute, Ghana for the AFM1 analysis.
Abbreviations
- AFM1
Aflatoxin M1
- HPLC-FLD
High perfomance liquid chromatographer-flourescence detector
- WHO
World Health Organization
- FAO
Food and Agriculture Organization
- JECFA
Joint Expert Committee on Food Additives
- SPSS
Statistical package for social sciences
- EDI
Estimated daily intake
- TDI
Tolerable daily intake
- HCC
Hepatocellular carcinoma
- LOD
Limit of detection
- LOQ
Limit of quantification
- HBsAg+
Hepatitis B surface antigen positive
- HBsAg−
Hepatitis B surface antigen negative
- ALARA
As low as reasonably allowed
Author contributions
N.K.K., T.A., A.A.B., E.K.E., and C.O.T. performed the experiments and wrote the manuscript. N.K.K., V.K.-B., E.K.E. were responsible for statistical analysis. N.K.K., V.K.-B., and A.A.B. helped conceive the experiments and prepared the manuscript. N.K.K., T.A., E.K.E., and C.O.T. conceived the original study and V.K.-B., N.K.K., and E.K.E. led the sampling and study in Ghana. All authors read and approved the final manuscript.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dror DK, Allen LH. The importance of milk and other animal-source foods for children in low-income countries. Food Nutr. Bull. 2011;32:227–243. doi: 10.1177/156482651103200307. [DOI] [PubMed] [Google Scholar]
- 2.Lindahl JF, Kagera I, Grace D. Aflatoxin M 1 levels in different marketed milk products in Nairobi, Kenya. Mycotoxin Res. 2018;34:289–295. doi: 10.1007/s12550-018-0323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baidoo W, Kunadu AP-H. Using low technology to improve the safety of informal-vended brukina—A fermented milk and millet smoothie in Ghana. Afr. J. Food Agric. Nutr. Dev. 2018;18:13646–13663. [Google Scholar]
- 4.Boakye, A., Tettey, C. & Mackay, L. Microbial evaluation of fermented milk and millet beverage (brukina) produced in Ghana by culture-independent technique. J. Food Sci. Nutr.3(6), 1–9. 2 J. Food Sci. Nutr. 3(6), 3 (2020).
- 5.Otwey, R. Processing options for brukina milk beverage. Undergraduate Thesis University Of Ghana (2015).
- 6.Tawiah, U. Microbiological and proximate composition of brukina drink, MPhil thesis, Kwame Nkrumah University of Science and Technology, (2015).
- 7.Atinmo T, Mirmiran P, Oyewole OE, Belahsen R, Serra-Majem L. Breaking the poverty/malnutrition cycle in Africa and the Middle East. Nutr. Rev. 2009;67:S40–S46. doi: 10.1111/j.1753-4887.2009.00158.x. [DOI] [PubMed] [Google Scholar]
- 8.Bervis N, et al. Field monitoring of aflatoxins in feed and milk of high-yielding dairy cows under two feeding systems. Toxins. 2021;13:201. doi: 10.3390/toxins13030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kortei NK, Asiedu P, Annan T, Deku JG, Boakye AA. Fungal diversity of “solom” a Ghanaian traditional beverage of millet (Pennisetum glaucum) Food Sci. Nutr. 2021;9:811–821. doi: 10.1002/fsn3.2045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu P, et al. Longitudinal study of aflatoxin exposure in the development of primary liver cancer in patients with chronic hepatitis. Zhonghua Yi Xue Za Zhi. 2010;90:1665–1669. [PubMed] [Google Scholar]
- 11.Xiang X, et al. Expression of P62 in hepatocellular carcinoma involving hepatitis B virus infection and aflatoxin B1 exposure. Cancer Med. 2017;6:2357–2369. doi: 10.1002/cam4.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun Z, et al. Increased risk of hepatocellular carcinoma in male hepatitis B surface antigen carriers with chronic hepatitis who have detectable urinary aflatoxin metabolite M1. Hepatology. 1999;30:379–383. doi: 10.1002/hep.510300204. [DOI] [PubMed] [Google Scholar]
- 13.Njombwa CA, Moreira V, Williams C, Aryana K, Matumba L. Aflatoxin M 1 in raw cow milk and associated hepatocellular carcinoma risk among dairy farming households in Malawi. Mycotoxin Res. 2021;37:89–96. doi: 10.1007/s12550-020-00417-5. [DOI] [PubMed] [Google Scholar]
- 14.Neuveut C, Wei Y, Buendia MA. Mechanisms of HBV-related hepatocarcinogenesis. J. Hepatol. 2010;52:594–604. doi: 10.1016/j.jhep.2009.10.033. [DOI] [PubMed] [Google Scholar]
- 15.European Food Safety Authority (EFSA) Opinion of the scientific committee on a request from EFSA related to exposure assessments. EFSA J. 2005;3:249. doi: 10.2903/j.efsa.2005.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.FAO/WHO. Application of risk analysis to food Standards issues: Report of the joint FAO/WHO Expert consultation. (FAO/WHO, 1995).
- 17.FAO-WHO (Food and Agriculture Organisation of United Nations-World Health Organization). Food safety risk analysis. A guide for national food safety Authorities. FAO food and nutrition paper No 87 (2006). [PubMed]
- 18.Donkor, E. et al. Bayesian spatio-temporal analysis of malaria in the Greater Accra Region of Ghana from 2015 to 2019. Preprint (2021) 10.21203/rs.3.rs-143819/v1. [DOI] [PMC free article] [PubMed]
- 19.Tabari M, Karim G, Ghavami M, Chamani M. Method validation for aflatoxin M1 determination in yoghurt using immunoaffinity column clean-up prior to high-performance liquid chromatography. Toxicol. Ind. Health. 2011;27:629–635. doi: 10.1177/0748233710394236. [DOI] [PubMed] [Google Scholar]
- 20.dos Santos JS, et al. Natural occurrence of deoxynivalenol in wheat from Paraná State, Brazil and estimated daily intake by wheat products. Food Chem. 2013;138:90–95. doi: 10.1016/j.foodchem.2012.09.100. [DOI] [PubMed] [Google Scholar]
- 21.Chain, E. P. o. C. i. t. F. et al. Risk assessment of aflatoxins in food. EFSA J. 2020;18:e06040. doi: 10.2903/j.efsa.2020.6040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Omore, A. O. et al. Employment generation through small-scale dairy marketing and processing: experiences from Kenya, Bangladesh and Ghana: a joint study by the ILRI Market-oriented Smallholder Dairy Project and the FAO Animal Production and Health Division. (Food & Agriculture Org., 2004).
- 23.EFSA Panel on Dietetic Products, N. & Allergies Scientific Opinion on the appropriate age for introduction of complementary feeding of infants. EFSA J. 2009;7:1423. doi: 10.2903/j.efsa.2009.1423. [DOI] [Google Scholar]
- 24.Lartey A, Manu A, Brown K, Peerson J, Dewey K. Predictors of growth from 1 to 18 months among breast-fed Ghanaian infants. Eur. J. Clin. Nutr. 2000;54:41–49. doi: 10.1038/sj.ejcn.1600891. [DOI] [PubMed] [Google Scholar]
- 25.Abubakari A, Kynast-Wolf G, Jahn A. Prevalence of abnormal birth weight and related factors in Northern region, Ghana. BMC Pregnancy Childbirth. 2015;15:1–8. doi: 10.1186/s12884-015-0790-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glover-Amengor M, et al. Nutritional status of children 0–59 months in selected intervention communities in northern Ghana from the africa RISING project in 2012. Arch. Public Health. 2016;74:1–12. doi: 10.1186/s13690-016-0124-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abeshu MA, Lelisa A, Geleta B. Complementary feeding: review of recommendations, feeding practices, and adequacy of homemade complementary food preparations in developing countries–lessons from Ethiopia. Front. Nutr. 2016;3:41. doi: 10.3389/fnut.2016.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization . WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. World Health Organization; 2006. [Google Scholar]
- 29.Biritwum R, Gyapong J, Mensah G. The epidemiology of obesity in Ghana. Ghana Med. J. 2005;39:82. [PMC free article] [PubMed] [Google Scholar]
- 30.Afrifa-Anane E, Agyemang C, Codjoe SNA, Ogedegbe G, Aikins AD-G. The association of physical activity, body mass index and the blood pressure levels among urban poor youth in Accra, Ghana. BMC Public Health. 2015;15:1–9. doi: 10.1186/s12889-015-1546-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walpole SC, et al. The weight of nations: An estimation of adult human biomass. BMC Public Health. 2012;12:1–6. doi: 10.1186/1471-2458-12-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaur S, Bedi JS, Dhaka P, Vijay D, Aulakh RS. Exposure assessment and risk characterization of aflatoxin M1 through consumption of market milk and milk products in Ludhiana, Punjab. Food Control. 2021;126:107991. doi: 10.1016/j.foodcont.2021.107991. [DOI] [Google Scholar]
- 33.Bahrami R, Shahbazi Y, Nikousefat Z. Aflatoxin M1 in milk and traditional dairy products from west part of Iran: Occurrence and seasonal variation with an emphasis on risk assessment of human exposure. Food Control. 2016;62:250–256. doi: 10.1016/j.foodcont.2015.10.039. [DOI] [Google Scholar]
- 34.Ishikawa AT, Takabayashi-Yamashita CR, Ono E, Bagatin AK, Rigobello FF, Kawamura O, Hirooka EY, Itano EN. Exposure assessment of infants to Aflatoxin M1 through consumption of breast milk and infant powdered milk in Brazil. Toxins. 2016;8:246. doi: 10.3390/toxins8090246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kortei NK, et al. The occurrence of aflatoxins and human health risk estimations in randomly obtained maize from some markets in Ghana. Sci. Rep. 2021;11:1–13. doi: 10.1038/s41598-020-79139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shephard GS. Risk assessment of aflatoxins in food in Africa. Food Addit. Contam. 2008;25:1246–1256. doi: 10.1080/02652030802036222. [DOI] [PubMed] [Google Scholar]
- 37.Joint, F., Additives, W. E. C. o. F. & Organization, W. H. Evaluation of certain food additives and contaminants: forty-ninth report of the Joint FAO/WHO Expert Committee on Food Additives. (World Health Organization, 1999). [PubMed]
- 38.Abesig J, Chen Y, Wang H, Sompo FM, Wu IX. Prevalence of viral hepatitis B in Ghana between 2015 and 2019: A systematic review and meta-analysis. PLoS ONE. 2020;15:e0234348. doi: 10.1371/journal.pone.0234348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ofori-Asenso R, Agyeman AA. Hepatitis B in Ghana: A systematic review & meta-analysis of prevalence studies (1995–2015) BMC Infect. Dis. 2016;16:1–15. doi: 10.1186/s12879-016-1467-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bhaskar, S. Foodborne diseases—disease burden. In Food Safety in the 21st Century 1–10 (Elsevier, 2017).
- 41.Addo-Boadu, C. Aflatoxin M1 Contamination of Raw Cow Milk, Milk Products and Dietary Exposure. (2019).
- 42.Mohammed S, Munissi JJ, Nyandoro SS. Aflatoxin M1 in raw milk and aflatoxin B1 in feed from household cows in Singida, Tanzania. Food Addit. Contam. Part B. 2016;9:85–90. doi: 10.1080/19393210.2015.1137361. [DOI] [PubMed] [Google Scholar]
- 43.Kang'ethe EK, Lang'a K. Aflatoxin B1 and M1 contamination of animal feeds and milk from urban centers in Kenya. Afr. Health Sci. 2009;9:218–226. [PMC free article] [PubMed] [Google Scholar]
- 44.Elzupir AO, Elhussein AM. Determination of aflatoxin M1 in dairy cattle milk in Khartoum State, Sudan. Food Control. 2010;21:945–946. doi: 10.1016/j.foodcont.2009.11.013. [DOI] [Google Scholar]
- 45.Tchana AN, Moundipa PF, Tchouanguep FM. Aflatoxin contamination in food and body fluids in relation to malnutrition and cancer status in Cameroon. Int. J. Environ. Res. Public Health. 2010;7:178–188. doi: 10.3390/ijerph7010178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mulunda M, Mike D. Occurrence of aflatoxin M1 from rural subsistence and commercial farms from selected areas of South Africa. Food Control. 2014;39:92–96. doi: 10.1016/j.foodcont.2013.11.011. [DOI] [Google Scholar]
- 47.Goncalves L, et al. Incidence of aflatoxin M1 in fresh milk from small farms. Food Sci. Technol. 2017;37:11–15. doi: 10.1590/1678-457x.06317. [DOI] [Google Scholar]
- 48.Flores-Flores ME, Lizarraga E, de Cerain AL, González-Peñas E. Presence of mycotoxins in animal milk: A review. Food Control. 2015;53:163–176. doi: 10.1016/j.foodcont.2015.01.020. [DOI] [Google Scholar]
- 49.Yousof S, El Zubeir I. Chemical composition and detection of Aflatoxin M1 in camels and cows milk in Sudan. Food Addit. Contam. Part B. 2020;13:298–304. doi: 10.1080/19393210.2020.1796826. [DOI] [PubMed] [Google Scholar]
- 50.Makun H, et al. Comparative study of aflatoxin M1 in livestock livers from Minna, Nigeria. J. Liver. 2017;6:1–5. doi: 10.4172/2167-0889.1000205. [DOI] [Google Scholar]
- 51.Jager A, Tedesco M, Souto P, Oliveira C. Assessment of aflatoxin intake in São Paulo, Brazil. Food Control. 2013;33:87–92. doi: 10.1016/j.foodcont.2013.02.016. [DOI] [Google Scholar]
- 52.Amer AA, Ibrahim ME. Determination of aflatoxin M1 in raw milk and traditional cheeses retailed in Egyptian markets. J. Toxicol. Environ. Health Sci. 2010;2:50–52. doi: 10.1007/BF03216513. [DOI] [Google Scholar]
- 53.Rahimi E, Bonyadian M, Rafei M, Kazemeini H. Occurrence of aflatoxin M1 in raw milk of five dairy species in Ahvaz, Iran. Food Chem. Toxicol. 2010;48:129–131. doi: 10.1016/j.fct.2009.09.028. [DOI] [PubMed] [Google Scholar]
- 54.Ahlberg S, Grace D, Kiarie G, Kirino Y, Lindahl J. A risk assessment of aflatoxin M1 exposure in low and mid-income dairy consumers in Kenya. Toxins. 2018;10:348. doi: 10.3390/toxins10090348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Duarte S, et al. Aflatoxin M1 in marketed milk in Portugal: Assessment of human and animal exposure. Food Control. 2013;30:411–417. doi: 10.1016/j.foodcont.2012.08.002. [DOI] [Google Scholar]
- 56.Rodríguez-Blanco M, Marín Sillué S, SanchísAlmenar V, Ramos Girona AJ. Mycotoxin contamination and fungal populations in silages for dairy cows in Spain. Toxins. 2019;11(7):21–22. [Google Scholar]
- 57.Cano-Sancho G, Marin S, Ramos AJ, Peris-Vicente J, Sanchis V. Occurrence of aflatoxin M1 and exposure assessment in Catalonia (Spain) Rev. Iberoam. Micol. 2010;27:130–135. doi: 10.1016/j.riam.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 58.Kos J, Lević J, Đuragić O, Kokić B, Miladinović I. Occurrence and estimation of aflatoxin M1 exposure in milk in Serbia. Food Control. 2014;38:41–46. doi: 10.1016/j.foodcont.2013.09.060. [DOI] [Google Scholar]
- 59.Tomašević I, et al. Two year survey on the occurrence and seasonal variation of aflatoxin M1 in milk and milk products in Serbia. Food Control. 2015;56:64–70. doi: 10.1016/j.foodcont.2015.03.017. [DOI] [Google Scholar]
- 60.Bilandžić N, Varenina I, Solomun B. Aflatoxin M1 in raw milk in Croatia. Food Control. 2010;21:1279–1281. doi: 10.1016/j.foodcont.2010.03.003. [DOI] [Google Scholar]
- 61.Bellio A, et al. Aflatoxin M1 in cow’s milk: Method validation for milk sampled in northern Italy. Toxins. 2016;8:57. doi: 10.3390/toxins8030057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.De Roma A, Rossini C, Ritieni A, Gallo P, Esposito M. A survey on the Aflatoxin M1 occurrence and seasonal variation in buffalo and cow milk from Southern Italy. Food Control. 2017;81:30–33. doi: 10.1016/j.foodcont.2017.05.034. [DOI] [Google Scholar]
- 63.Iha MH, Barbosa CB, Okada IA, Trucksess MW. Aflatoxin M1 in milk and distribution and stability of aflatoxin M1 during production and storage of yoghurt and cheese. Food Control. 2013;29:1–6. doi: 10.1016/j.foodcont.2012.05.058. [DOI] [Google Scholar]
- 64.Nile SH, Park SW, Khobragade C. Occurrence and analysis of aflatoxin M1 in milk produced by Indian dairy species. Food Hydrocolloids. 2016;27:358–366. [Google Scholar]
- 65.Lee JE, Kwak B-M, Ahn J-H, Jeon T-H. Occurrence of aflatoxin M1 in raw milk in South Korea using an immunoaffinity column and liquid chromatography. Food Control. 2009;20:136–138. doi: 10.1016/j.foodcont.2008.03.002. [DOI] [Google Scholar]
- 66.Iqbal SZ, Asi MR. Assessment of aflatoxin M1 in milk and milk products from Punjab, Pakistan. Food Control. 2013;30:235–239. doi: 10.1016/j.foodcont.2012.06.026. [DOI] [Google Scholar]
- 67.Schöneberg T, et al. Influence of temperature, humidity duration and growth stage on the infection and mycotoxin production by Fusarium langsethiae and Fusarium poae in oats. Plant. Pathol. 2019;68:173–184. doi: 10.1111/ppa.12922. [DOI] [Google Scholar]
- 68.Gong YY, et al. Dietary aflatoxin exposure and impaired growth in young children from Benin and Togo: Cross sectional study. BMJ. 2002;325:20–21. doi: 10.1136/bmj.325.7354.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kew MC. Synergistic interaction between aflatoxin B1 and hepatitis B virus in hepatocarcinogenesis. Liver Int. 2003;23:405–409. doi: 10.1111/j.1478-3231.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 70.Asare GA, Bronz M, Naidoo V, Kew MC. Interactions between aflatoxin B1 and dietary iron overload in hepatic mutagenesis. Toxicology. 2007;234:157–166. doi: 10.1016/j.tox.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 71.Kumi J, Dotse E, Asare GA, Ankrah N-A. Urinary aflatoxin M1 exposure in Ghanaian children weaned on locally prepared nutritional food. Afr. J. Sci. Res. 2015;4:28–32. [Google Scholar]
- 72.Gong Y, et al. Determinants of aflatoxin exposure in young children from Benin and Togo, West Africa: The critical role of weaning. Int. J. Epidemiol. 2003;32:556–562. doi: 10.1093/ije/dyg109. [DOI] [PubMed] [Google Scholar]
- 73.Gizachew D, Szonyi B, Tegegne A, Hanson J, Grace D. Aflatoxin contamination of milk and dairy feeds in the Greater Addis Ababa milk shed, Ethiopia. Food Control. 2016;59:773–779. doi: 10.1016/j.foodcont.2015.06.060. [DOI] [Google Scholar]
- 74.Škrbić B, Antić I, Živančev J. Presence of aflatoxin M1 in white and hard cheese samples from Serbia. Food Control. 2015;50:111–117. doi: 10.1016/j.foodcont.2014.08.031. [DOI] [Google Scholar]
- 75.Khlangwiset P, Shephard GS, Wu F. Aflatoxins and growth impairment: A review. Crit. Rev. Toxicol. 2011;41:740–755. doi: 10.3109/10408444.2011.575766. [DOI] [PubMed] [Google Scholar]
- 76.Mahdavi R, Nikniaz L, Arefhosseini S, Jabbari MV. Determination of aflatoxin M 1 in breast milk samples in Tabriz-Iran. Matern. Child Health J. 2010;14:141–145. doi: 10.1007/s10995-008-0439-9. [DOI] [PubMed] [Google Scholar]
- 77.Soriano JM, Rubini A, Morales-Suarez M, Merino-Torres JF, Silvestre D. Aflatoxins in organs and biological samples from children affected by kwashiorkor, marasmus and marasmic-kwashiorkor: A scoping review. Toxicon. 2020;185:174–183. doi: 10.1016/j.toxicon.2020.07.010. [DOI] [PubMed] [Google Scholar]
- 78.Oyelami O, Maxwell S, Adelusola K, Aladekoma T, Oyelese A. Aflatoxins in the autopsy brain tissue of children in Nigeria. Mycopathologia. 1995;132:35–38. doi: 10.1007/BF01138602. [DOI] [Google Scholar]
- 79.Oyelami O, Maxwell S, Aladekomo T, Adelusola K. Two unusual cases of kwashiorkor: Can protein deficiency explain the mystery? Ann. Trop. Paediatr. 1995;15:217–219. doi: 10.1080/02724936.1995.11747775. [DOI] [PubMed] [Google Scholar]
- 80.Adelusola OOSMK, Oyelese TAA. Aflatoxins in autopsy kidney specimens from children in Nigeria. J. Toxicol. Environ. Health Part A. 1998;55:317–323. doi: 10.1080/009841098158368. [DOI] [PubMed] [Google Scholar]
- 81.Oyelami O, Maxwell S, Adelusola K, Aladekoma T, Oyelese A. Aflatoxins in the lungs of children with kwashiorkor and children with miscellaneous diseases in Nigeria. J. Toxicol. Environ. Health. 1997;51:623–628. doi: 10.1080/00984109708984048. [DOI] [PubMed] [Google Scholar]
- 82.Onyemelukwe GC, Ogoina D, Ibiam G, Ogbadu G. Aflatoxins in body fluids and food of Nigerian children with protein-energy malnutrition. Afr. J. Food Agric. Nutr. Dev. 2012;12:6553–6566. [Google Scholar]
- 83.De Vries H, Maxwell S, Hendrickse R. Aflatoxin excretion in children with kwashiorkor or marasmic kwashiorkor—a clinical investigation. Mycopathologia. 1990;110:1–9. doi: 10.1007/BF00442763. [DOI] [PubMed] [Google Scholar]
- 84.Kuboka MM, et al. Occurrence of aflatoxin M1 in raw milk traded in peri-urban Nairobi, and the effect of boiling and fermentation. Infect. Ecol. Epidemiol. 2019;9:1625703. doi: 10.1080/20008686.2019.1625703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu Y, Wu F. Global burden of aflatoxin-induced hepatocellular carcinoma: A risk assessment. Environ. Health Perspect. 2010;118:818–824. doi: 10.1289/ehp.0901388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kuiper-Goodman T. Uncertainties in the risk assessment of three mycotoxins: Aflatoxin, ochratoxin, and zearalenone. Can. J. Physiol. Pharmacol. 1990;68:1017–1024. doi: 10.1139/y90-155. [DOI] [PubMed] [Google Scholar]
- 87.Fazli Z, Fatemeh S, Abdi A, Pourhosseingholi M, Taghinejad H. Studying of liver cancer mortality and morbidity burden in Iran. Sci. J. Ilam Univ. Med. Sci. 2012;4:117–122. [Google Scholar]
- 88.Guo Y, Yuan Y, Yue T. Aflatoxin M1 in milk products in China and dietary risk assessment. J. Food Prot. 2013;76:849–853. doi: 10.4315/0362-028X.JFP-12-419. [DOI] [PubMed] [Google Scholar]
- 89.Udovicki B, Djekic I, Kalogianni EP, Rajkovic A. Exposure assessment and risk characterization of aflatoxin M1 intake through consumption of milk and yoghurt by student population in Serbia and Greece. Toxins. 2019;11:205. doi: 10.3390/toxins11040205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Serraino A, et al. Occurrence of aflatoxin M1 in raw milk marketed in Italy: Exposure assessment and risk characterization. Front. Microbiol. 2019;10:2516. doi: 10.3389/fmicb.2019.02516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Trevisani, M., Serraino, A., Canever, A., Varisco, G. & Boni, P. Quantitative risk assessment of aflatoxicosis associated with milk consumption in Italy (2000–2004). Towards a risk-based chain control, 91–114 (2006).
- 92.Oozone, M. Risk assessment report-Aflatoxin M1 in milk and aflatoxin B1 in feeds. マイコトキシン65, 27–29 (2015).
- 93.Driehuis F, Spanjer M, Scholten J, Te Giffel M. Occurrence of mycotoxins in feedstuffs of dairy cows and estimation of total dietary intakes. J. Dairy Sci. 2008;91:4261–4271. doi: 10.3168/jds.2008-1093. [DOI] [PubMed] [Google Scholar]
- 94.European Food Safety Authority (EFSA) Opinion of the Scientific Panel on contaminants in the food chain [CONTAM] related to Aflatoxin B1 as undesirable substance in animal feed. EFSA J. 2004;2:39. doi: 10.2903/j.efsa.2004.39. [DOI] [Google Scholar]
- 95.Li S, et al. Occurrence of aflatoxin M1 in raw milk from manufacturers of infant milk powder in China. Int. J. Environ. Res. Public Health. 2018;15:879. doi: 10.3390/ijerph15050879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bolger, M. Safety evaluation of certain mycotoxins in food. In Prepared by the 56th Meeting of the Joint FAO/WHO Expert Committee on Food Additives (JECFA), 2001, Geneva, Switzerland. (WHO).
- 97.Joint Committee on Food Additives, World Health Organization, W. H. Evaluation of certain veterinary drug residues in food: fifty-fourth report of the Joint FAO/WHO Expert Committee on Food Additives. (2001).
- 98.Meeting, J. F. W. E. C. o. F. A., Additives, J. F. W. E. C. o. F. & Organization, W. H. Evaluation of certain mycotoxins in food: Fifty-Sixth report of the Joint FAO/WHO Expert Committee on Food Additives. Vol. 56 (World Health Organization, 2002). [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.