Abstract
Fatty Liver, one of the most common liver diseases worldwide, usually emerges due to lipid accumulation, mostly triglycerides in hepatocytes. Fat exists in the liver naturally, but if it surpasses 5–10% of the liver's total weight, it can result in fatty liver. In this case, report effect of Ayurveda intervention in grade II fatty liver is reported. Thirty-five-year-old obese male with grade II fatty liver presented with fatigue, abdominal pain, heaviness, and incomplete bowel evacuation to the National Institute of Ayurveda hospital, Jaipur, Rajasthan, India. On examination, there was no significant clinical abnormality except a high body mass index (BMI = 30.2). Hematological examinations revealed altered Alanine transaminase, fasting blood glucose, total cholesterol, low-density lipoprotein, and triglycerides. The patient was diagnosed sonologically with a grade II fatty liver. The patient was given Ayurveda treatment for two months with three treatment regimens. The patient was assessed for improvement in signs and symptoms, hematological parameters, and quality of life using a chronic liver disease questionnaire (CLDQ). After two months, significant improvement was observed in signs and symptoms, BMI (24.7), and CLDQ. No fatty tissue was reported sonologically, and all altered biochemical parameters were within normal limits. Present case highlights the potential of Ayurveda interventions in managing non-alcoholic fatty liver disease and obesity.
Keywords: Ayurveda treatment, Obesity, Fatty liver
1. Introduction
Non-alcoholic fatty liver disease (NAFLD) consists of steatosis and non-alcoholic steatohepatitis (NASH). Steatosis is the accumulation of fat in the liver, and steatohepatitis is a condition with inflammation [1]. NAFLD is a growing epidemic worldwide due to increasing obesity, with prevalence in the general population ranging from 11.2% to 37.2% [2]. Among obese patients, the frequency of NASH ranges from 12.6% to 30.4% [3]. Worldwide, NAFLD cases have increased from 19.34 million to 29.49 million from 1990 to 2017. The greatest burden is in East Asia, followed by South Asia, North Africa, and the Middle East [4].
In Ayurveda, NAFLD is assigned as Yakrit Roga (liver disease) and Medoroga (obesity) [5] (5. Sutra 21/4). Many conditions come under Yakrit Roga, varying from simple steatosis to hepatomegaly to liver cirrhosis. The ancient text of Yogratnakara described that Vidahi (spicy food) and Abhisyandi Ahara (food that blocks the channels) lead to Rakta-Kapha Dushti giving rise to Yakritodara (enlargement of the liver). This case report highlights the treatment effects of Ayurveda interventions in a patient with grade II NAFLD. http://www.care-statement.org
2. Case report
A 35 year-old non-alcoholic, unmarried male patient, relatively obese (BMI = 30.2) from an urban area, came for Ayurveda treatment at our hospital. The patient was 6 feet tall, weighing 90 kg, and looking unwell and tired. The patient mainly complained about fatigue, anorexia, body pain, incomplete bowel evacuation, and abdominal distension. These symptoms have been persisting in the patient for the past 6 months.
2.1. Clinical findings
At the presentation time, the patient's pulse rate was 82/min, blood pressure was 130/80 mmHg, and respiratory rate was 15/min. The body temperature was normal. No abnormal clinical finding for cardiovascular and respiratory systems was observed on examination. His abdomen was distended due to fat and was normally moving with respiration. On palpation, mild tenderness was found in the right lumbar and umbilical regions. Dull sounds were recorded during the percussion on the right lumbar region, and bowel sounds were normal on auscultation. No relevant family, medical and surgical, or psychological illness history was present in the patient. The patient had consulted for similar medical complaints with an allopathic physician 6 months back. Antacids and laxatives were given to control the abdominal distension and bowel evacuation. During this period patient was not recovered completely and due to the reoccurrence of symptoms seek, he for Ayurveda treatment. He was presently not on any medication while the Ayurvedic intervention was ongoing.
2.2. Diagnosis
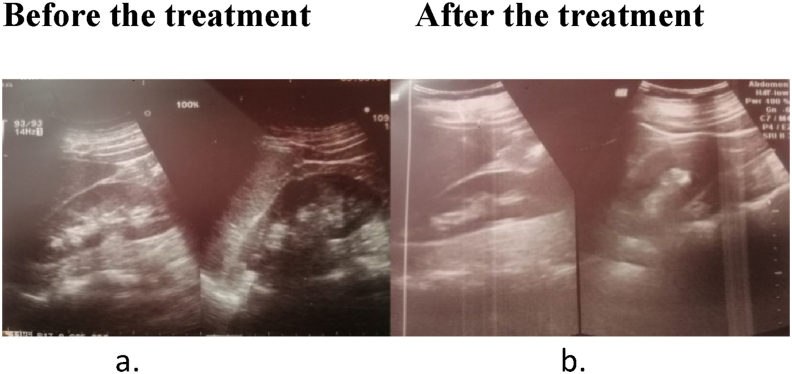
The patient was referred to a sonologist for ultrasonography of the whole abdomen, and the patient was found to be having grade II fatty liver (Fig. 1a.). No other abnormal sonographic finding was reported. The patient was thus diagnosed with grade II NAFLD with obesity. The Ayurvedic diagnosis was Yakrit Roga (liver disease), associated with Medoroga (obesity).
Fig. 1.
a – USG before the treatment, b – USG after the treatment.
2.3. Intevention
The patient was given Ayurvedic medication for 60 days. All the interventions are presented in Table 1.
Table 1.
| Treatment regimen | Duration | Drug | Dose and frequency | Route of administration |
|---|---|---|---|---|
| One | Day 1–15 | Avipattikara Churna | 3 g twice a day | Oral |
| Punarnava Mandoor | 250 mg twice a day | Oral | ||
| Sankha Bhasma | 250 mg twice a day | Oral | ||
| Tarunikusumakara Churna | 3 g once a day at bedtime | Oral | ||
| Two | Day 16–30 | Avipattikara Churna | 3 g twice a day | Oral |
| Punarnava Mandoor | 250 mg twice a day | Oral | ||
| Sankha Bhasma | 250 mg twice a day | Oral | ||
| Triphala Churna | 3 g once a day at bedtime | Oral | ||
| Three | Day 31–60 | Avipattikara Churna | 3 g twice a day | Oral |
| Punarnava Mandoor | 250 mg twice a day | Oral | ||
| Sankha Bhasma | 250 mg twice a day | Oral | ||
| Kutaki Churna | 1 g once a day at bedtime | Oral |
2.4. Diet
No specific diet or exercise schedule was given to the patient during the treatment period of two months.
3. Timeline of treatment:
The patient had treatment for three months. The timeline of the treatment is presented in Table 2.
Table 2.
Timeline of the treatment.
| Health event | Timeline |
|---|---|
| First USG of the abdomen and diagnosis of grade II fatty liver | 2021 August 07 |
| Approached for Ayurveda treatment | 2021 August 08 |
| Assessment and examination were done. The treatment regimen first started | 2021 August 09 |
| Assessment on first follow-up and treatment regimen two started | 2021 August 24 |
| Assessment on second follow-up and treatment regimen three started | 2021 September 08 |
| Assessment of third follow-up and follow-up USG abdomen was advised | 2021 October 08 |
4. Results
4.1. Observations
The patient was observed for improvement in symptoms related to Yakrit Roga and Medo Roga on the four-point grading system (none, mild, moderate, and severe). Details of the recorded observations are presented in Table 3.
Table 3.
Observation of Signs and symptoms related to liver and obesity.
| Parameter | Day 1 | Day 15 | Day 30 | Day 60 |
|---|---|---|---|---|
| Yakrit Roga related signs and symptoms | ||||
| Udarshoola (pain in the abdomen) | Mild | None | None | None |
| Utkleśha (feeling of nausea and vomiting) | Severe | Mild | None | None |
| Aruchi (loss of appetite) | Severe | Mild | None | None |
| Hṛitkaṇṭahadāha (heartburn) | Severe | Moderate | Mild | None |
| Height, weight, and BMI | ||||
| Height (feet) | 6 | 6 | 6 | 6 |
| Weight (kg) | 98 | 94 | 88 | 80 |
| Body Mass Index (BMI) | 30.2 | 29 | 27.2 | 24.7 |
| Obesity-related signs and symptoms | ||||
| Ayusho Hrasa (deficient in longevity) | Severe | Moderate | Mild | None |
| Javoparadha (Slow in movement) | Severe | Moderate | Mild | Mild |
| Krichchavyavaya (difficult to indulge in sexual intercourse) | Severe | Moderate | Mild | None |
| Daurbalyam (weak) | Severe | Moderate | Mild | No |
| Daurgandhya (Bad smell) | None | None | None | None |
| Swedabadha (much sweating) | None | None | None | None |
| Ati Kshudha (excessive hunger) | Severe | Mild | None | None |
| Ati Pipasa (excessive thirst) | Severe | Moderate | Mild | None |
4.2. Quality of life
Quality of life assessment was done using the chronic liver disease questionnaire (CLDQ) [8]. The evaluation was done on day 1, day 15, day 30, and day 60. Data are presented in Table 4.
Table 4.
Assessment of quality of life.
| Parameter | Day 1 | Day 15 | Day 30 | Day 60 | Improvement % |
|---|---|---|---|---|---|
| Abdominal symptoms (3) | 4/21 | 13/21 | 17/21 | 20/21 | 76.2 |
| Fatigue (5) | 7/35 | 12/35 | 20/35 | 30/35 | 65.7 |
| Systemic symptoms (5) | 26/35 | 28/35 | 30/35 | 33/35 | 20 |
| Activity (3) | 12/21 | 18/21 | 21/21 | 21/21 | 43 |
| Emotional function (8) | 42/56 | 48/56 | 50/56 | 52/56 | 18 |
| Worry (5) | 27/35 | 29/35 | 30/35 | 34/35 | 20 |
| Total (29) | 118/203 | 148/203 | 168/203 | 190/203 | 35.4 |
Before initiating the treatment, the total quality of life score was 118 out of 203, which improved to 190 over 203 (35.4%). After 60 days of treatment, more than 50% improvement was observed in abdominal symptoms and fatigue.
4.3. Patient perspective
The patient was satisfied with the treatment given and the improvement in his digestion, appetite, bowel evacuation, lethargic condition, and weight reduction. After two months of the treatment, the patient was feeling energetic, and actively doing his daily activities.
5. Effect on biochemical parameters
Biochemical parameters were assessed before starting the treatment and after two months. Data is presented in Table 5.
Table 5.
Effect of treatment on Biochemical parameters.
| Parameter | Day 1 | Day 60 | % Improvement |
|---|---|---|---|
| Aspartate aminotransferase (U/L) | 30 | 29 | 3.3 |
| Alanine transaminase (U/L) | 66 | 50 | 24.2 |
| Fasting blood glucose (mg/dl) | 115 | 75 | 34.7 |
| Total cholesterol (mg/dl) | 255 | 191 | 25.1 |
| High density lipoprotein (mg/dl) | 53 | 57 | 7.5 |
| Low density lipoprotein (mg/dl) | 185 | 117 | 36.7 |
| Triglycerides (mg/dl) | 180 | 84 | 53.3 |
| Serum gamma-glutamyl transferase (IU/L) | 22 | 21 | 4.5 |
| Serum amylase (U/L) | 70 | 65 | 7.1 |
After two months of Ayurveda interventions, significant improvement was observed in all the laboratory parameters, and they were in the normal range. However, the effect was more pronounced on Alanine transaminase, total cholesterol, low-density lipoprotein, and triglyceride levels.
6. Ultrasonography of the whole abdomen (USG)
Before treatment, the liver was bright and echogenic, and the portal venous radicle's echogenicity was also lost (Fig. 1a). After two months, there was a complete remission of the lesion in the liver parenchyma. In addition, intrahepatic biliary radicals and portal vein radicals showed no abnormalities after two months of treatment (Fig. 1b).
7. Discussion
Fatty liver is commonly encountered in routine clinical practice. The majority of the cases do not suffer much, but some may progress to steatosis, steatohepatitis, and fibrosis. In some cases, it may develop hepatocellular carcinoma. Fatty liver is the common cause of the liver dysfunction, and compared to alcoholic fatty liver, few cases of NAFLD seem to develop chronic liver disease [9]. In this study, we have treated a non-alcoholic, obese patient who had grade II fatty liver. According to Ayurveda, Santarpana (overeating and sedentary lifestyle) is responsible for the vitiation of Kapha and Meda, which are the main Dosha and Dushya involved in the pathogenesis of Sthaulya (obesity) [10]. Our practice shows that persons with vitiated Kapha and Meda (fat) are prone to develop fatty liver and altered lipid profiles. A similar clinical picture was observed in the present case. Agni Deepana (enhancing the digestive fire), Ama Pacana (eliminating the toxins from the body), and Virechana (laxative) were the main principles applied in this case (5. Sutrasthana 21/5-9). Most of the ingredients of Avipattikara Churna have Ama Pacana (eliminating the toxins from the body), Mriduvirechaka (mild laxative), and Lekhaniya (which scrapes excess fats) properties (5. Sutrasthana 21/21) (5. Sutrasthana 4/8-9). Powder of Pichrorhiza kurroa Royle ex Benth. having Tikta Rasa Pradhana is also helpful in Ama Pacana (eliminating the toxins from the body) and Lekhaniya (which scrapes the excess fat) [11,12]. Pichrorhiza kurroa Royle ex. Benth has shown potent hepatoprotective and immune-modulatory properties [13]. Ingredients of Avipattikara Churna and Punarnava Mandura have digestive, hepatoprotective, metabolism-enhancing, and antioxidant properties. In this case, improved digestion and metabolism were observed within a few days of initiating the treatment, which probably improved biochemical parameters related to liver functions and lipid metabolism [[14], [15], [16]]. A daily laxative was also prescribed to ease the expulsion of solid water from the colon. Daily purgation is also an important line of treatment in managing Udara Roga (abdomen-related disorders). The beneficial effects of satisfactory bowel evacuations were observed in the present case. Further, sonographic evidence, showed a reduction in fat deposited in the liver and periportal area. These findings highlights the usefulness of prescribed treatment in managing obesity and non-alcoholic fatty liver conditions.
8. Conclusion
On the basis of the results, we can conclude that Ayurvedic interventions used in the present case have shown a significant effect on weight reduction and management of non-alcoholic fatty liver. The results observed in this case are encouraging, and further well-designed clinical trials may be carried out to test the efficacy of these interventions in similar conditions.
Informed consent
Informed consent for the publication of the data was taken from the patient.
Funding sources
Nil.
Authors contribution
Concept; AK Sahu. Design; AK Sahu, A Upadhyay, H Bhakuni, AMHS Attanayake, P Sharma. Manuscript Preparation; AK Sahu, A Upadhyay, H Bhakuni, AMHS. Attanayake. Manuscript editing; A Upadhyay, AMHS. Attanayake. Manuscript review; Guarantee. Other; AK Sahu, A Upadhyay, AMHS Attanayake.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Abbreviations
- NAFLD
non-alcoholic fatty liver disease
- NASH
non-alcoholic steatohepatitis
- BMI
body mass index
- USG
ultrasonography
References
- 1.Huang D.Q., El-Serag H.B., Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2021;18(4):223–238. doi: 10.1038/s41575-020-00381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benedict M., Zhang X. Nonalcoholic fatty liver disease: an expanded review. World J Hepatol. 2017;9(16):715–732. doi: 10.4254/wjh.v9.i16.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Younossi Z.M., Koenig A.B., Abdelatif D., Fazel Y., Henry L., Wymer M. Global epidemiology of non-alcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 4.Zhang X., Wu M., Liu Z., Yuan H., Wu X., Shi T., et al. Increasing prevalence of NAFLD/NASH among children, adolescents and young adults from 1990 to 2017: a population-based observational study. BMJ Open. 2021;11(5):e042843. doi: 10.1136/bmjopen-2020-042843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma R.K., Dash B., editors. Charaka Samhita text with English translation and critical exposition based on Cakrapani Datta's Ayurveda Dipika. 1st ed. Chowkhamba Sanskrit Series Office; Varanasi: 2019. [Google Scholar]
- 6.Mishra S.B., editor. 1st ed. vol. III. Chaukhambha Sanskrit Sansthan publishers; Varanasi: 2017. p. 117. (Bhashajyarathnavali of Sri Govinda Dasji). Chapter 56, Verse 25-29. [Google Scholar]
- 7.Murthy P.H.C. 1st ed. vol. 33. Chowkhamba Sanskrit Series office; Varanasi: 2018. (Sarangadara Samhita of Sarangadharacarya). Chapter 4, Verse 3-4. [Google Scholar]
- 8.Dam-Larsen S., Franzmann M., Andersen I.B., Christoffersen P., Jensen L.B., Sørensen T.I., et al. Long term prognosis of fatty liver: risk of chronic liver disease and death. Gut. 2004;53(5):750–755. doi: 10.1136/gut.2003.019984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Younossi Z.M., Guyatt G., Kiwi M., Boparai N., King D. Development of a disease-specific questionnaire to measure health-related quality of life in patients with chronic liver disease. Gut. 1999;45:295–300. doi: 10.1136/gut.45.2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singhal P., Nesari T., Gupta G.S. Efficacy of herbo-mineral compounds and pathya (Ayurvedic dietary regime and physical exercise) in the management of Yakṛt Roga (Non-alcoholic fatty liver disease) Anc Sci Life. 2015;34(4):216–222. doi: 10.4103/0257-7941.160866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sastry J.L.N. vol. 2. Chaukhambha Orientalia; Varanasi: 2017. p. 391. (Illustrated Dravyaguna Vijnana (study of the essential medical plants in Ayurveda)). [Google Scholar]
- 12.Tarapure S., Tubaki B.R., Khot S. Elastographic liver evaluation of Katukyadi churna in the management of Non-Alcoholic Steatohepatitis (NASH) – a single arm clinical trial. J Ayurveda Integr Med. 2021;12(1):136–142. doi: 10.1016/j.jaim. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verma P.C., Basu V., Gupta V., Saxena G., Rahman L.U. Pharmacology and chemistry of a potent hepatoprotective compound Picroliv isolated from the roots and rhizomes of Picrorhiza kurroa royle ex benth. (kutki) Curr Pharm Biotechnol. 2009 Sep;10(6):641–649. doi: 10.2174/138920109789069314. [DOI] [PubMed] [Google Scholar]
- 14.Pandya M.G., Dave A.R. A clinical study of Punarnava Mandura in the management of Pandu Roga in old age (geriatric anemia) Ayu. 2014;35(3):252–260. doi: 10.4103/0974-8520.153735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rawat A.K., Mehrotra S., Tripathi S.C., Shome U. Hepatoprotective activity of Boerhaavia diffusa L. roots – a popular Indian ethnomedicine. J Ethnopharmacol. 1997 Mar;56(1):61–66. doi: 10.1016/s0378-8741(96)01507-3. [DOI] [PubMed] [Google Scholar]
- 16.Wei X., Luo C., He Y., Huang H., Ran F., Liao W., et al. Hepatoprotective effects of different extracts from Triphala against CCl4-induced acute liver injury in mice. Front Pharmacol. 2021;12 doi: 10.3389/fphar. [DOI] [PMC free article] [PubMed] [Google Scholar]