Abstract
Interpersonal-motivational models posit that heightened avoidance of aversive social stimuli and diminished approach of appetitive social stimuli increases social withdrawal and reduces positive social interactions, thereby increasing risk for future social anxiety and depression. The current study examined if approach-avoidance biases toward angry and happy faces, measured during the Approach Avoidance Task (AAT), would be associated with the development of adolescent depressive and social anxiety symptoms. At baseline, participants included 129 never-depressed adolescent girls (ages 11–13), two-thirds of whom were at high-risk for internalizing problems due to shy/fearful temperament. Girls reported their depressive and social anxiety symptoms every 6 months for 24 months and completed the AAT at baseline and 24-mo follow-up. Heightened avoidance bias toward angry faces at baseline predicted increases in depressive symptoms across the follow-up, even after accounting for temperament and pubertal status. In contrast, girls with greater depression and social anxiety symptoms at 24-mo follow-up exhibited less avoidance bias for angry faces at the same time point. Findings suggest that avoidance behaviors (i.e., avoiding people or settings associated with angry faces, which are often perceived as hostile, critical, or rejecting) may be a risk factor for depression, above and beyond risk imparted by temperament or advances in puberty. However, with increasing internalizing symptoms, it may become more difficult for adolescents to maintain avoidance for aversive social stimuli, and without the introduction of more adaptive emotion regulation strategies, these biases may continue to increase and maintain risk for internalizing problems.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10802-022-00948-8.
Keywords: Adolescence, Depression, Social anxiety, Temperament, Approach-Avoidance biases, Approach-Avoidance Task (AAT)
Depressive and social anxiety disorders are debilitating psychiatric disorders that often emerge before adulthood (Price & Woody, 2020), with adolescence marking a key sensitive window for their development, particularly among girls (Rapee et al., 2019). For example, during adolescence, rates of major depressive disorder (MDD) rise dramatically, culminating in a 13-point difference in past year prevalence rates between 12- to 17-year-olds (4.8% and 18.5%, respectively) (NIMH, 2017). Gender differences in depression also emerge during this period, as past year prevalence rates are considerably higher among adolescent girls (16.5%) compared to boys (5.4%) (Lu, 2019). Similarly, prevalence rates of social anxiety disorder (SAD) increase to around 10% by the end of adolescence (Leigh & Clark, 2018), and gender differences in SAD are maximal during this time [i.e., girls at > 1.5 times greater risk than boys (Asher et al., 2017)]. Onsets of adolescent depression and social anxiety typically do not appear without warning; the development of subclinical symptoms can serve as a harbinger for later impairment and distress if left unaddressed (Fehm et al., 2008; Gotlib et al., 1995; Pine et al., 1999). Thus, understanding mechanisms that underlie the initial development of subthreshold depressive and social anxiety symptoms in high-risk populations, such as adolescent girls, may provide valuable public health implications for prevention and intervention efforts (Thapar et al., 2012; Woody & Price, 2020).
Longstanding interpersonal models of depression and social anxiety suggest that individuals with, or at high-risk for, these conditions exhibit social behaviors that differ from their peers (Alden & Taylor, 2004; Coyne, 1976). These behaviors may include excessive reassurance-seeking, social withdrawal, and self-denigration, which often evoke negative affect, rejection, and hostility from others. Critically, such interpersonal behaviors (and the reactions they elicit) have been implicated in the development of depression and social anxiety and are considered putative mechanisms of these disorders, rather than just concomitants (Epkins & Heckler, 2011; Rapee & Spence, 2004; Sacco & Vaughan, 2006). Relative to men, women may be at particular risk via interpersonal pathways, in part due to gender differences in exposure to, generation of, and reactivity to social stress (Hammen et al., 2008), which may peak during adolescence (Rose & Rudolph, 2006). For example, evidence suggests that youth who exhibit a shy and/or fearful temperament exhibit higher levels of social inhibition and heightened sensitivity to peer rejection, thereby increasing risk for subsequent adolescent depression and social anxiety (Fox & Kalin, 2014; Silk et al., 2012), especially among early adolescent girls (Rapee et al., 2019). As such, atypical social approach-avoidance behaviors may represent a mechanism linking childhood temperament and these disorders for early adolescent girls.
By their definition, depression and social anxiety reflect diminished approach and heightened avoidance behaviors across symptoms such as anhedonia, fear, and social withdrawal (American Psychiatric Association, 2000). Conceptual models of internalizing disorders often encapsulate two motivational systems: the behavioral inhibition system (BIS) and the behavioral activation system (BAS) (Carver & Scheier, 1990; Higgins, 1987). As a regulator of avoidance behaviors, the BIS is responsible for attention to social rejection/threat and levels of both negative affect and behavioral inhibition; as a regulator of approach behaviors, the BAS is responsible for perception of positive affect and pleasant social interactions, as well as levels of behavioral activation (Bijttebier et al., 2009; Brown, 2007). The BIS and BAS are thought to function as a feedback system, such that when the BIS system is activated, the BAS system is inhibited, leading to more avoidant behaviors (and vice versa) (Corr, 2002).
Early adolescence is a developmental period characterized by major social transitions that impact BIS/BAS motivational systems, which occur in parallel to significant brain maturation and pubertal changes that increasingly prioritize processing of emotionally-salient social cues (Guyer et al., 2016; Ladouceur, 2012). For many adolescents, this phase of development is marked by significant increases in approach behavior, with adolescents seeking out pleasurable experiences and sensations, sometimes to their own detriment via risk-taking (Somerville et al., 2010; Spear, 2011). In contrast, some adolescents exhibit predominantly avoidant behaviors, in part due to fears of peer rejection, which can increase risk for depression and social anxiety during adolescence (Epkins & Heckler, 2011; Silk, Davis, et al., 2012). Notable to interpersonal-motivational models of depression and social anxiety, inhibited and withdrawn interpersonal behaviors may become less acceptable to adolescent peers, relative to younger peers, suggesting that temperamentally inhibited adolescents may be at increased risk for experiencing the peer rejection they fear via their own avoidance (Ladd & Burgess, 1999; Rubin et al., 2018). Therefore, diminished approach and heightened avoidance are thought to contribute to vulnerability to depression and social anxiety by increasing social withdrawal and decreasing positive social interactions, thereby thwarting adaptive social functioning and increasing anxious and depressed mood (Chronis-Tuscano et al., 2009; Fox & Kalin, 2014; Manos et al., 2010; Martell et al., 2001). For example, if an adolescent engages in social withdrawal to avoid peers who they think might reject them, then, in addition to increasing the likelihood that said peers will negatively evaluate such behaviors, the adolescent simultaneously misses out on potential social rewards such as attending parties, making new friends, and falling in love, which could result in reduced positive mood and increased social isolation. And if pervasively experienced over time, these maladaptive social approach-avoidance biases could contribute to issues such as depressed mood, anhedonia, and social anxiety (Hundt et al., 2007; Idson et al., 2004; Ottenbreit & Dobson, 2008). Indeed, adolescents who report engaging in experiential avoidance are also more likely to report higher levels of both cross-sectional and longitudinal depressive (Biglan et al., 2015; Greco et al., 2008; Mellick et al., 2019) and social anxiety symptoms (Papachristou et al., 2018), effects that are often stronger among girls, relative to boys (Howe-Martin et al., 2012; Venta et al., 2012).
Taken together, prior studies suggest that adolescent social approach-avoidance biases play a role in the development of adolescent depression and social anxiety. However, there are remaining limitations that must be addressed by future research. First, given that BIS/BAS motivational systems are thought to influence social approach-avoidance behavior, it would be informative to probe these systems via behavioral measures in order to extend findings generated from self-report questionnaires (Biglan et al., 2015; Greco et al., 2008; Howe-Martin et al., 2012; Mellick et al., 2019; Papachristou et al., 2018; Venta et al., 2012). Second, limited research has examined social approach-avoidance bias in high-risk adolescent samples, which limits understanding of whether social approach-avoidance biases serve as trait-like risk factors and/or are linked to symptom change. For example, there is preliminary evidence that levels of experiential avoidance may act as a trait-like vulnerability for future depression, given that never-depressed adolescent girls at high risk for depression (due to a maternal history of MDD) report higher levels of experiential avoidance compared to their lower-risk peers (Mellick et al., 2017). Because maternal depression is a factor associated with risk for a broad array of psychopathology and maladaptive interpersonal behaviors (Goodman, 2007), future studies could extend these findings by using parental reports of temperament to recruit a high-risk adolescent sample specifically enriched for inhibited and withdrawn social approach-avoidance biases, which could provide additional specificity in examining such social behaviors as a predictor of depressive and social anxiety symptoms. In particular, because of their increased sensitivity to and fear of social threat and rejection, girls with a shy/fearful temperament are more likely to report greater levels of social avoidance and reduced social approach behaviors, which in turn may increase risk for later depression and social anxiety during early adolescence (Allen et al., 2006; Li et al., 2015; Rapee et al., 2019; Silk, Davis, et al., 2012). Finally, longitudinal research is needed to determine whether biases in social approach-avoidance behavior can predict future trajectories of symptoms among high-risk adolescents, given evidence that the rise in subthreshold depressive and social anxiety symptoms before the onset of such disorders may be a critical window for prevention efforts (Thapar et al., 2012; Woody & Price, 2020).
To address the limitations of prior research, the current study employed a behavioral assessment of social approach-avoidance bias to determine if this vulnerability would predict future depressive and social anxiety symptoms among a sample of early adolescent girls enriched for risk via fearful or shy temperament. Specifically, girls were assessed for social approach-avoidance biases using the Approach-Avoidance Task (AAT) using interpersonal stimuli (Heuer et al., 2007). In this version of the AAT, participants view angry and happy facial expressions, which evoke approach-avoidance behaviors in both real life and experimental settings. Participants are asked to react to the emotional faces on a computer screen by either pulling the face toward themselves (approaching) or pushing it away from themselves (avoiding). By comparing reaction times to push versus pull trials for each type of facial expression (happy, angry), researchers can quantify social approach-avoidance biases toward both appetitive and aversive social stimuli (Heuer et al., 2007). Notably, research assessing approach-avoidance biases using the AAT also indicate that the task generates neural activation in BIS/BAS-relevant circuitry. For example, when healthy adults are asked to engage in incongruent social behaviors (e.g., pushing, rather than pulling, in response to happy faces), activation of the anterior/ventrolateral prefrontal cortex (Kaldewaij et al., 2016) and insula are increased (Harlé et al., 2021), suggesting that incongruent approach-avoidance behaviors require increased affective processing, salience detection, and conflict resolution, which slows reaction time responses.
To our knowledge, no studies have examined social approach-avoidance biases using the AAT in an adolescent sample at high-risk for depression and/or social anxiety. However, previous studies using a similar version of the AAT used in the current study have compared performance on the task between adults with and without depression or social anxiety. Focusing first on depression – the majority of studies show that depressed adults are more likely to exhibit an avoidance bias toward angry faces and/or a diminished approach bias toward happy faces compared to their non-depressed peers (Derntl et al., 2011; Seidel et al., 2010; Vrijsen et al., 2013), but it is important to note that others have shown a lack of significant differences between non-depressed and depressed adults (Struijs et al., 2017) or that depressed adults show no dominant approach-avoidance biases compared to their non-depressed peers (Radke et al., 2014). Findings regarding social anxiety are more consistent, such that adults with social anxiety, compared to non-anxious peers, are more likely to exhibit an avoidance bias for both angry and happy faces (Heuer et al., 2007; Lange et al., 2008; Roelofs et al., 2010; Voncken et al., 2012). Together, these studies tentatively suggest that both depression and social anxiety are associated with heightened avoidance of angry faces but differ in approach of happy faces (i.e., diminished approach in depression vs. active avoidance in social anxiety).
There are several limitations of prior AAT research that highlight avenues for future investigation. First, little is known regarding the internal reliability of the AAT, though a few studies have indicated satisfactory internal consistency (Loijen et al., 2020). Reporting psychometrics in future research may help to interpret mixed findings. Relatedly, inconsistent findings from depressed samples might reflect the well-known heterogeneity of depression. Comparing group averages has historically obfuscated significant heterogeneity among depressed individuals, with some research showing that such analyses may not accurately reflect the performance of even a single participant (Molenaar & Campbell, 2009). In response, developmental psychopathologists have long called for research focusing on within-person differences (Cicchetti & Rogosch, 2002). Clearly, future research will benefit from examining the link between behavioral indices of social approach-avoidance biases and adolescent depression and social anxiety using repeated-measures longitudinal designs with reported psychometrics.
To address the gaps and limitations of prior research, our primary aim in the current study was to determine the role of social approach-avoidance biases, generated from the AAT, in the development of depressive and social anxiety symptoms among a sample of never-depressed early adolescent girls enriched for risk via shy/fearful temperament. Girls completed the AAT both at baseline and a 24-mo follow-up and reported their depressive symptoms at 6-mo intervals from baseline to the 24-mo follow-up. Based on longstanding interpersonal-motivational theories of depression and social anxiety, as well as previous research, we hypothesized that girls who exhibited a heightened avoidance bias toward angry faces (i.e., quicker to push away, versus pull toward, angry faces) would report greater longitudinal increases in depressive and social anxiety symptoms across a two-year follow-up. In contrast, for happy faces, we predicted that a diminished approach bias toward happy faces (i.e., smaller differences between pushing versus pulling happy faces) at baseline would be associated with increases in depressive symptoms whereas the opposite (i.e., quicker to push away, versus pull toward, happy faces) would predict social anxiety symptoms. In addition, we planned exploratory analyses to assess if approach-avoidance biases would change from baseline to the two-year follow-up and if biases at follow-up would be contemporaneously associated with depression and social anxiety symptoms at follow-up.
Method
Participants
Participants included 129 early adolescent girls and a participating caregiver recruited for a longitudinal study examining socio-affective risk factors in the development of internalizing problems. At baseline, girls were between the ages of 11 and 13 (M = 12.27) and were required to have no lifetime history of depressive or anxiety disorders. This restricted age range was chosen because it (1) marks the beginning of dramatic rises in rates of depression and anxiety observed during the adolescent period (NIMH, 2017) and (2) is associated with a wide range of variability in pubertal status, which is an important moderator of socio-affective risk for internalizing disorders (Pfeifer & Allen, 2021). Pubertal status was assessed using the Pubertal Development Scale (PDS) (Petersen et al., 1988) according to Shirtcliff and colleagues’ (Shirtcliff et al., 2009) method for approximating adrenarche and menarche that is designed to parallel Tanner stages that are established by a physical exam. Scores ranged from 1 to 5 (M = 3.47, SD = 1.04), indicating that the majority of the sample had entered mid-puberty. Total family income (M = 7.07; SD = 3.19) was reported by caregivers on a scale of 0–10 increments of $10,000 (0 = 0–10,000 to 10 = 100,000+). Regarding adolescents’ race, 2% self-identified as Asian American, 9% as Biracial, 19% as Black/African American, 1% as Native American, 67% as White, and 2% as a race not included in other answer choices (e.g., identifying as Multiracial). Regarding adolescents’ ethnicity, 10% self-identified as Hispanic.
Participants were recruited through (1) internet ads posted to Facebook and Instagram; (2) postcards sent to local residential areas; (3) flyers postered to local commercial businesses, hospitals, and outpatient settings; and (4) internet flyers advertised through the University of Pittsburgh CTSI research portal. Some advertisements were designed to encourage general community engagement (e.g., “Do you have an 11-to-13-year-old daughter?) whereas others were designed to recruit shy or fearful girls (e.g., “Do you have a daughter who is healthy, but sometimes hesitant?”). Via this targeted recruitment strategy, the sample was enriched for risk for future depression and social anxiety such that roughly two-thirds of adolescent girls (n = 85) were classified as having fearful or shy temperament at baseline. To be classified as high-risk, girls had to score 0.75 SD above norms on either the Shyness (≥ 2.99) or Fear (≥ 3.12) subscale of the Early Adolescent Temperament Scale – Revised (EATQ-R), which was administered during a screening phone call. Girls scoring below these EATQ-R thresholds were considered to be at lower risk for future internalizing disorders. Of note, EATQ-R scores were not used as part of exclusion criteria for the study.
Participants were excluded from the study if they met current or lifetime DSM 5 diagnostic criteria for major depressive disorder, any anxiety disorder (with the exception of specific phobia), or any autism spectrum disorder or psychotic disorder. Diagnostic criteria were determined by administration of the Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS-PL; Kaufman et al., 2016; updated from the 1997 version to align with the DSM-5). Participants with an IQ less than 70 were excluded from the current study, as determined by the Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999). Based on caregiver and child report, participants were also excluded if they had: (1) presence of head injury or neurological anomalies; (2) the presence of MRI contraindications (e.g., metal in body, including braces); (3) psychoactive or endocrine disrupting medications (except stimulants); (4) ongoing ocular conditions or uncorrected vision problems; and (5) acute suicidal risk or risk of harming self or others. Three hundred and seventy families completed a phone screen for the study, of whom 133 (36%) were determined to be ineligible due to exclusion criteria. One hundred and eighty-seven families attended subsequent clinical interviews in the laboratory, of whom 47 (25%) were determined to be ineligible.
Procedure
All study procedures were approved by the University of Pittsburgh’s Institutional Review Board, and upon arrival at the laboratory, caregivers were asked to provide informed consent and adolescents were asked to provide verbal assent to be in the study. At baseline, adolescents completed the Mood and Feelings Questionnaire (MFQ) (Angold et al., 1987) to assess current depressive symptoms, the Screen for Child Anxiety Related Emotional Disorders social anxiety subscale (SCARED-SA) (Birmaher et al., 1997) to assess current social anxiety symptoms, and the AAT to assess social approach-avoidance biases. Remote administration of the MFQ and SCARED-SA occurred 6, 12, and 18 months after the baseline assessment. Finally, at the 24-mo follow-up, girls returned to the lab and completed the MFQ, SCARED-SA, and the AAT again. Adolescents and caregivers were compensated for their time.
Measures
Self-Reported Depressive Symptoms. Adolescents’ self-reported depressive symptoms over the previous two weeks were measured using the self-report version of the MFQ. On the MFQ, participants rated 33 statements as 0 (not true), 1 (sometimes true), or 2 (true). All items were summed, with a higher score indicating greater depressive symptoms. The MFQ has demonstrated excellent internal consistency and validity in previous research in both community and clinical samples of youth (Banh et al., 2012; Burleson Daviss et al., 2006; Kent et al., 1997; Sund et al., 2001; Wood et al., 1995). Past research has suggested that a cut-off score of 27 or above on the MFQ can be used to classify the presence of clinical depression with the greatest combination of sensitivity and specificity (Wood et al., 1995). The MFQ was administered at each of the assessment points (α’s = 0.90-0.95 across all time points). Mean MFQ scores from each visit can be found in Table 1.
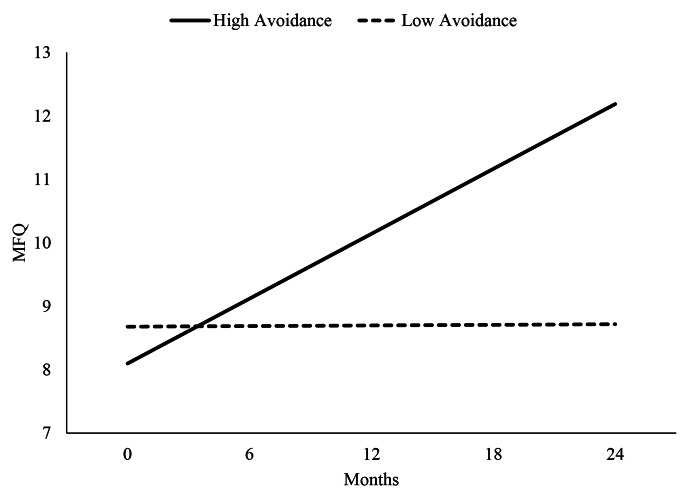
Fig. 1.
Trajectories of Depressive Symptoms among Girls Exhibiting High versus Low Avoidance Bias toward Angry Faces
Self-Reported Social Anxiety Symptoms. Adolescents’ self-reported social anxiety symptoms over the past week were measured using the self-report version of the SCARED-SA. On the SCARED-SA, participants rated 7 statements as 0 (not true/hardly ever true), 1 (somewhat true/sometimes true), or 2 (very true/often true). All items were summed, with a higher score indicating greater social anxiety symptoms. The SCARED-SA has demonstrated excellent internal consistency and validity in previous research (Birmaher et al., 1999). A cut-off score of 8 or above on the SCARED-SA has been established to classify the presence of clinical social anxiety (Birmaher et al., 1999). The SCARED-SA was administered at each of the assessment points (α’s = 0.68-0.75 across all time points). Mean SCARED-SA scores from each visit can be found in Table 1.
Approach-Avoidance Bias. Both at baseline and 24-mo follow-up, the Approach-Avoidance Task (AAT) (Roelofs et al., 2010) was administered to assess approach-avoidance biases toward emotional faces. Participants were presented with oval cut-out photographs of adults displaying emotional facial expressions (i.e., angry and happy faces with direct or averted gaze) on a computer screen with a resolution of 1024 × 768 pixels. A Logitech Attack 3 joystick was placed between the monitor and the participants, so that the participant could pull the joystick toward their body (approach) and push the joystick away (avoid) with ease. Each trial was self-paced; participants were told to press a button on the keyboard when the joystick was in an upwards resting position and the screen was blank. After pressing the button, the face would appear in the center of the screen. Participants were asked to respond as quickly and accurately as possible to each face by either pushing or pulling the joystick. Pushing the joystick would cause the picture of the face to shrink in size and disappear from the screen, whereas pulling would cause the picture to enlarge. In Block 1 of the AAT, participants were told to push the joystick in response to angry faces and pull the joystick in response to happy faces. In Block 2, participants were told to pull the joystick in response to angry faces and push the joystick in response to happy faces. A practice phase of 18 trials preceded every block, which each consisted of 64 trials (for a total of 164 trials during the AAT).
Reaction times (RTs) during each trial were recorded as the time (ms) between the stimulus onset and the apex of the maximum joystick displacement. To calculate RT indices of approach-avoidance bias, outliers were filtered by excluding RTs outside of 2 ½ standard deviations from each participant’s RT mean. For each participant, the means of the remaining RTs for correct responses (M = 90%; Range = 68–100%) were calculated per condition [defined by Emotion (i.e., angry, happy), Gaze (i.e., direct, averted), and Correct Response Type (i.e., push, pull)]. Preliminary analyses demonstrated that facial stimulus gaze type (i.e., direct or averted) did not differentially influence responses to push versus pull trials or angry versus happy trials (see Supplement), and thus for subsequent missing data estimation and analyses, data were collapsed responses across gaze conditions.
Consistent with prior research, we examined approach-avoidance behavior by creating bias scores for each emotion condition (Roelofs et al., 2010). We subtracted individual mean RTs for pull trials from the individual means for push trials, separately for angry and happy trials. More positive bias scores represent an approach bias (i.e., less response caution when pulling an emotional face toward yourself versus pushing it away) and more negative bias scores represented an avoidant bias (i.e., more response caution when pulling versus pushing). This approach has been effective in linking AAT approach-avoidance biases to internalizing disorders that disrupt social behavior and individual differences in self-reported social approach and inhibition behaviors [for reviews, see (Fricke & Vogel, 2020; Loijen et al., 2020)]. Mean AAT response time bias scores from each visit can be found in Table 1. Of note, approach-avoidance bias scores for angry faces were significantly lower than zero at baseline, t(128) = -2.28, p = .02, 95% CI (-43.92, -3.14), and 24-mo follow-up, t(128) = -3.69, p < .001, 95% CI (-48.10, -14.53), suggesting that girls across the sample exhibited a true avoidance bias for angry faces at both timepoints. In contrast, approach-avoidance bias scores for happy faces were significantly higher than zero at baseline, t(128) = 9.10, p < .001, 95% CI (70.85, 110.21), and 24-mo follow-up, t(128) = 8.67, p < .001, 95% CI (44.57, 70.93), suggesting a true approach bias for happy faces at both time points.
Approach-avoidance bias scores for angry faces exhibited acceptable split-half reliability (> 0.70) at the baseline and follow-up assessment (Spearman-Brown coefficients were 0.75 and 0.71, respectively). Approach-avoidance bias scores for happy faces exhibited less than acceptable split-half reliability at baseline and follow-up (Spearman-Brown coefficients were 0.57 to 0.63, respectively). Because biases for happy faces did not demonstrate adequate levels of internal consistency, further analyses examining approach-avoidance bias for happy faces are reported in the Supplement. Finally, because the AAT was only administered at baseline and 24-mo follow-up, a time lapse of two years was considered too long to obtain a psychometrically adequate measure of test-retest reliability. However, because changes across development are of interest here, we examined correlations between AAT bias scores at baseline versus 24-mo-follow (see Table 1). There was a small-to-medium negative association between avoidance bias to angry faces at baseline versus follow-up (r = − .29, p < .001), indicating that this bias is subject to within-person change from early to mid-adolescence.
Analysis Plan.
Missing Data. Of the 129 girls participating in the initial assessment, 122, 120, 118, and 96 participated in the 6, 12, 18, and 24-mo follow-ups, respectively (see also Table S1 in the Supplement). Notably, attrition at the 24-mo follow-up visit was higher due to the COVID-19 pandemic. Twenty-six girls completed their 24-mo follow-up following the onset of the pandemic. Girls who completed the 24-mo follow-up before versus after the pandemic did not significantly differ in age, pubertal status, temperamental risk, 24-mo AAT performance, or 24-mo depressive or social anxiety symptoms (lowest p = .26). We examined the pattern of missing data and found that Little’s missing completely at random (MCAR) test was nonsignificant, χ2(229) = 231.94, p = .43, suggesting that observed data were missing at random. Given this, maximum likelihood estimates of missing data were created and used in all subsequent analyses reported in the main text [see (Schafer & Graham, 2002)].
Prediction of Depressive and Anxiety Symptoms. We planned hierarchical linear modeling (HLM) (Raudenbush & Bryk, 2002) to test the hypothesis that girls’ levels of approach-avoidance biases to angry faces at baseline would predict prospective changes in both depressive and social anxiety symptoms. Preliminary analyses demonstrated that depressive symptoms increased significantly in a linear, but not quadratic fashion, whereas social anxiety symptoms significantly increased quadratically, but not linearly (see Supplement). Thus, we planned to examine MFQ and SCARED-SA trajectories in separate models so that the appropriate linear versus quadratic functions could be applied.
The Level 1 models for these HLM analyses were:
MFQtij = π0j + π1j (Timeij) + eij.
SCARED-SAtij = π2j + π3j (Timeij) + π4j (Time2ij) + eij.
where MFQtij and SCARED-SAtij represents levels of depressive and social anxiety symptoms, respectively, reported by girls at time t for assessment i and participant j, π0j is the MFQ intercept (reflecting each girl’s depressive symptoms at the initial assessment point), π1j is the slope of the linear relation between Time (in months) and depressive symptoms across the follow-up for participant j, π2j is the SCARED-SA intercept (reflecting each girl’s social anxiety symptoms at the initial assessment point), π3j is the slope of the linear relation between Time (in months) and social anxiety symptoms across the follow-up for participant j, π4j is the slope of the quadratic relation between Time2 (in months) and social anxiety symptoms across the follow-up for participant j, and eij represents the error terms.
The Level 2 models were:
π0j = β00 + β01(Approach-Avoidance Bias) + β02(Temperament) + β03(Puberty) + r0j.
π1j = β10 + β11(Approach-Avoidance Bias) + β12(Temperament) + β13(Puberty) + r1j.
π2j = β20 + β21(Approach-Avoidance Bias) + β22(Temperament) + β23(Puberty) + r2j.
where β01 is the cross-level interaction term representing the effect of Approach-Avoidance Bias score on the outcome intercept, β11 is the cross-level interaction term representing the effect of Approach-Avoidance Bias score on linear change in outcome across the follow-up, and β21 is the cross-level interaction term representing the effect of Approach-Avoidance Bias score on quadratic change in outcome across the follow-up (applicable only to SCARED-SA models). Finally, β00,β10,β20 are the intercept terms for each of their respective equations, and r0j,r1j, and r2j are the error terms. In addition, because the study’s recruitment strategy centered on these two variables, both baseline pubertal status and temperamental risk (high vs. lower) were included in each Level 2 model to examine the effects of approach-avoidance bias over and beyond puberty- and temperament-related changes in symptom trajectories.
Contemporaneous associations between approach-avoidance bias and symptoms at follow-up. We planned linear regression models to test the association between girls’ approach-avoidance bias to angry faces at the 24-mo follow-up and contemporaneous depressive and social anxiety symptoms. Respective symptom scores at the 24-mo follow-up were included as the dependent variable and 24-mo AAT approach-avoidance bias scores for angry faces were entered as independent variables. Temperamental risk status and pubertal status were included as covariates.
Results
Prediction of Depressive Symptoms. We found that although approach-avoidance bias for angry faces was not significantly related to depressive symptoms at baseline, t(125) = 0.55, p = .58, reffect size = 0.05, it did predict the trajectory of depressive symptoms over time, t(125) = -2.16, p = .03, reffect size = 0.19. Specifically, more avoidance bias to angry faces at baseline predicted significantly greater increases in depressive symptoms across follow-ups. These findings are visually depicted in Fig. 1 and model details are provided in Table 2. Notably, this finding was maintained even when family income, age, and race were included as covariates in the model, t(122) = -2.21, p = .03, reffect size = 0.19. In addition, this model revealed that temperamental risk was associated with depressive symptoms at baseline, t(125) = 2.13, p = .04, reffect size = 0.19, indicating that girls at high, compared to average, temperamental risk for internalizing problems reported higher depressive symptoms at the baseline visit. However, temperament did not moderate the time slope for depressive symptoms, t(125) = 0.38, p = .71, reffect size = 0.03, indicating that the initial difference in symptoms was maintained over the course of follow-up. In contrast, pubertal status was not significant related to any symptoms at baseline or across follow-ups (lowest p = .22).
Table 1.
Clinical Characteristics of the Sample. (Note Scores are reported as M (SD); T00 = Baseline, T06 = 6-mo follow-up, T12 = 12-mo follow-up, T18 = 18-mo follow-up, T24 = 24-mo follow-up; AAT = Approach-Avoidance Task; MFQ = Mood and Feelings Questionnaire (potential scores range from 0 to 66; clinical cut-off ≥ 27); SCARED-SA = Screen for Child Anxiety Related Disorders - Social Anxiety (potential scores range from 0 to 14; clinical cut-off ≥ 8).)
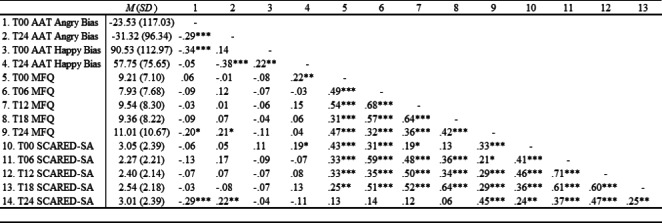
Table 2.
HLM Models Predicting Symptom Trajectories
| Fixed Effect | Coefficient | SE | t | p | |||
|---|---|---|---|---|---|---|---|
| MFQ | For π0j (baseline) | ||||||
| Intercept | 4.08 | 2.17 | 1.88 | 0.06 | |||
| Angry Bias | 0.00 | 0.00 | 0.55 | 0.58 | |||
| Temperament | 0.28 | 0.13 | 2.13 | 0.04 | |||
| Pubertal Status | 0.69 | 0.56 | 1.23 | 0.22 | |||
| For π1j (linear slope) | |||||||
| Intercept | 0.16 | 0.12 | 1.29 | 0.20 | |||
| Angry Bias | 0.00 | 0.00 | -2.16 | 0.03 | |||
| Temperament | 0.00 | 0.01 | 0.38 | 0.71 | |||
| Pubertal Status | − 0.03 | 0.03 | -1.02 | 0.31 | |||
| SCARED-SA | For π0j (baseline) | ||||||
| Intercept | 1.80 | 0.77 | 2.35 | 0.02 | |||
| Angry Bias | 0.00 | 0.00 | -1.22 | 0.23 | |||
| Temperament | 0.16 | 0.04 | 3.88 | < 0.001 | |||
| Pubertal Status | 0.00 | 0.18 | − 0.03 | 0.98 | |||
| For π1j (linear slope) | |||||||
| Intercept | − 0.28 | 0.12 | -2.24 | 0.03 | |||
| Angry Bias | 0.00 | 0.00 | 1.03 | 0.30 | |||
| Temperament | 0.00 | 0.01 | − 0.22 | 0.82 | |||
| Pubertal Status | 0.05 | 0.03 | 1.91 | 0.06 | |||
| For π2j (quadratic slope) | |||||||
| Intercept | 0.01 | 0.00 | 2.63 | 0.01 | |||
| Angry Bias | 0.00 | 0.00 | -1.44 | 0.15 | |||
| Temperament | 0.00 | 0.00 | − 0.02 | 0.98 | |||
| Pubertal Status | 0.00 | 0.00 | -2.25 | 0.03 | |||
Note. MFQ = Mood and Feelings Questionnaire; SCARED-SA = Screen for Child Anxiety Related Disorders - Social Anxiety
Prediction of Anxiety Symptoms. We found that avoidance bias for angry faces was not significantly related to social anxiety symptoms at baseline, t(125) = -1.22, p = .23, reffect size = 0.11 or to linear, t(125) = 1.03, p = .30, reffect size = 0.09, or quadratic, t(125) = -1.44, p = .15, reffect size = 0.13, growth in symptoms. This model also revealed that temperamental risk was associated with social anxiety symptoms at baseline, t(125) = 3.88, p < .001, reffect size = 0.34, indicating that girls at high, compared to average, temperamental risk reported higher social anxiety symptoms at the baseline visit. However, temperament did not moderate the linear, t(125) = − 0.22, p = .82, reffect size = 0.02, or quadratic, t(125) = − 0.02, p = .98, reffect size = 0.00, time slope for social anxiety symptoms, indicating that the initial difference in symptoms was maintained over the course of follow-up. In addition, pubertal status was not significantly related to any symptoms at baseline, t(125) = − 0.03, p = .98, reffect size = 0.00 but significantly moderated the time slope of the quadratic effect, t(125) = -2.25, p = .03, reffect size = 0.20, indicating that the relation between pubertal status and social anxiety symptom trajectories was curvilinear (see Figure S1 in the Supplement for details).
Contemporaneous associations between approach-avoidance bias and symptoms at follow-up. Results indicated that individuals with less avoidance of angry faces at the 24-mo follow-up reported significantly higher contemporaneous depressive, t(125) = 3.00, p = .003, rpart = 0.25, and social anxiety symptoms, t(125) = 3.18, p = .002, rpart = 0.27.
Discussion
The current findings support avoidance of aversive social stimuli during early adolescence as a predictor of the development of later depressive symptoms, such that 11–13 year old girls who exhibited heightened avoidance bias toward angry faces at baseline showed the largest increases in depressive symptoms across a two-year period. These results suggest that avoidance biases for interpersonal stimuli that reflect anger, hostility, or criticism (e.g., angry faces) are closely linked to the development of depressive symptoms among adolescents at high risk for internalizing disorders. Findings from the current study are consistent with prior research showing that adolescent girls at high-risk for depression due to maternal MDD are more likely to report engaging in experiential avoidance (i.e., the tendency to escape or avoid situations that cause distress or discomfort), compared to their lower-risk peers (Mellick et al., 2017) and that such self-reported behaviors predict longitudinal trajectories of adolescent depression in the community (Mellick et al., 2019). Together, these past and current findings suggest that avoidance biases toward aversive social stimuli may act as a vulnerability that increases risk for future depression among adolescent girls.
Because the current study used repeated administration of the AAT to assess change in approach-avoidance biases in a risk-enriched sample of adolescents, our findings are uniquely placed to extend previous research. When considering change across the sample, we found no significant change in avoidance bias for angry faces from baseline to two-year follow-up and observed that girls, on average, showed a “true” avoidance bias for angry faces at both time points (i.e., RT difference scores for push vs. pull trials that were significantly below zero). However, when considering within-person change, we found that girls who exhibited the most avoidance bias at baseline demonstrated the least avoidance bias two years later. This is notable when considering the observed associations between avoidance bias for angry faces at two-year follow-up and both depression and social anxiety symptoms at the same time point; those with greater depression and social anxiety symptoms at follow-up exhibited a less pronounced avoidance bias for angry faces. When taken together with findings showing that greater avoidance bias for angry faces at baseline predicted greater increases in depressive symptom across the two-year follow-up, a nuanced picture of the role of avoidance of aversive social stimuli in internalizing problems from early to mid-adolescence begins to emerge.
Findings in the current study may be best explained by the negative potentiation hypothesis of depression, which suggests that depression is associated with negative self-schemas (e.g., belief systems focused on disconnection and rejection, such as “I am unlovable”) that potentiate significant distress and negative affect when triggered by events perceived to validate the schema (Beck, 1967). For individuals who have not yet experienced clinical depression but who are at high-risk for future onset, these negative schema are often already developed but can remain latent via avoidance, which allows the individual to circumvent the negative triggering events that potentiate negative affect in the short-term (Leahy, 2012). However, pervasive use of avoidance to evade feelings of disconnection and rejection is thought to inadvertently reinforce negative schemas and ultimately increase risk for later depression (Rezaei & Ghazanfari, 2016), which is consistent with our findings that although baseline avoidance of angry faces was not associated with baseline depressive symptoms, it did predict symptom trajectories across the two-year follow-up. Further, some cognitive informational processing models have suggested that with the progression of depressive symptoms and disorders, avoidance of negative stimuli can become increasingly difficult to maintain, which allows triggering events to further potentiate negative affect via affective priming of elaborative processing of and attention to negative information (Gibb et al., 2016; Trew, 2011). This theory may explain why adolescents, who at baseline exhibited the most avoidance bias for angry faces, paradoxically exhibited less avoidance bias and increased depression and social anxiety symptoms at follow-up. Because adolescents with heightened avoidance bias for angry faces at baseline were at greatest risk for increased depression symptoms across the two-year follow-up, this accelerated trajectory of depressive symptoms may have been associated with increased difficulty maintaining avoidance of angry faces at follow-up. Although a strength of the current study was its repeated assessment of the AAT, because it was only administered twice, it was not possible to conduct lagged analyses to better understand the temporal links between avoidance biases and internalizing symptoms, which remains an important question for future research.
The current study also provided opportunities to examine the effects of temperamental risk on depression and social anxiety symptom trajectories. Consistent with prior research (Essex et al., 2010; Fox & Kalin, 2014; Silk, Davis, et al., 2012), a shy or fearful temperament was associated with higher depressive and social anxiety symptoms at baseline, an effect that was maintained across the follow-up. In contrast, avoidance bias toward angry faces was not associated with baseline symptoms but did predict increased symptom trajectories across the follow-up and fluctuated with later changes in symptoms. This suggests that a fearful or shy temperament is associated with chronic and stable elevations in depressive and social anxiety outcomes, whereas the risk imparted by social avoidance biases (above and beyond temperamental risk factors) may be influenced by the relevant social, affective, biological changes that unfold from early to mid-adolescence (Guyer et al., 2016; Ladouceur, 2012; Rapee et al., 2019).
One of the main limitations of the current study was that approach bias toward happy faces did not demonstrate acceptable split-half reliability; thus, planned analyses using these bias scores were moved to the Supplement given concerns about a lack of internal consistency. Inconsistent with motivational-interpersonal theories of internalizing disorders (Carver & Scheier, 1990; Higgins, 1987), these supplementary analyses demonstrated that approach bias toward happy faces did not significantly predict trajectories of depressive or social anxiety symptoms. However, because the observed lack of internal reliability may result in limited power for these analyses, there are still unresolved questions regarding whether social approach biases toward appetitive stimuli exert influence in the development of depression and social anxiety trajectories. Future research will be necessary.
The current study also had several other limitations. First, symptom severity remained somewhat restricted even across follow-ups, which may limit the generalizability of current findings to adolescents exhibiting greater symptom severity. However, examining trajectories of subclinical depressive and social anxiety symptoms in high-risk populations remains valuable for future prevention and interventions efforts as they are one of the most robust predictors of subsequent onset and impairment (Gotlib et al., 1995; Pine et al., 1999; Thapar et al., 2012; Woody & Price, 2020). Second, the current study used adult faces to probe adolescent girls’ social approach-avoidance biases. For use in adolescent samples, future research may benefit from the inclusion of an AAT task that use adolescent faces instead. Relatedly, although consistent with past research (Heuer et al., 2007; Roelofs et al., 2010) the AAT task in the current study only examined approach-avoidance biases to angry and happy faces. Future researchers could consider the inclusion of additional emotional faces (e.g., sad and fearful) that are associated with greater specificity to symptoms of depression versus social anxiety (Gibb et al., 2016). Further, future paradigms might test if faces idiographically matched to the sociocultural identities of participants could impact responses. Finally, the ecological validity of the AAT is relatively limited. Thus, much like attempts to increase the ecological validity of tasks assessing responses to peer acceptance and rejection (e.g., Chatroom Interact Task) (Silk, Stroud, et al., 2012), future efforts should be made to simulate more realistic social approach-avoidance behaviors during computer-based laboratory tasks. Future research could also examine whether behavioral indices of social approach-avoidance biases are associated with reduced approach behavior in daily life using ecological momentary assessment (EMA), which could illuminate the proposed relation between aversive and appetitive responses and depressed/socially anxious mood with greater temporal sensitivity. Clearly, future repeated-measures longitudinal research is necessary to better understand the role of social approach-avoidance biases in depression and social anxiety.
In conclusion, our findings are informative for interpersonal and motivational models of internalizing disorders, which posit that BIS/BAS systems play a critical role in shaping the interpersonal deficits that increase risk for, and maintain, depression and social anxiety. Specifically, the current study provides evidence that, among a sample enriched for future risk via a shy or fearful temperament, early adolescent girls who exhibit heightened avoidance bias toward angry faces at baseline showed the largest increases in depressive symptoms across a two-year period. In regard to real-world implications, these findings suggest that early adolescent girls who are more likely to avoid people or settings associated with angry faces, which are often interpreted to be rejecting, critical, or threatening, may be at increased risk for developing later subthreshold depressive symptoms. However, our results also indicate that as high-risk adolescents grow older and experience increasing symptoms of depression or social anxiety, their reliance on avoidant coping strategies may become increasingly difficult to maintain, and without the introduction of more adaptive coping skills in its place, their negative affect may be further potentiated. Finally, in a world increasingly lived through screens, understanding how high-risk adolescents approach and avoid online social stimuli (e.g., profile pictures, sponsored media advertisements) may help inform mental health specialists in treating depression and social anxiety during a sensitive developmental window.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alden LE, Taylor CT. Interpersonal processes in social phobia. Clinical Psychology Review. 2004;24(7):857–882. doi: 10.1016/j.cpr.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Allen JP, Insabella G, Porter MR, Smith FD, Land D, Phillips N. A social-interactional model of the development of depressive symptoms in adolescence. Journal of consulting and clinical psychology. 2006;74(1):55. doi: 10.1037/0022-006X.74.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Weissman MM, John K, Merikancas KR, Prusoff BA, Wickramaratne P, Warner V. Parent and child reports of depressive symptoms in children at low and high risk of depression. Journal of Child Psychology and Psychiatry. 1987;28(6):901–915. doi: 10.1111/j.1469-7610.1987.tb00678.x. [DOI] [PubMed] [Google Scholar]
- Asher M, Asnaani A, Aderka IM. Gender differences in social anxiety disorder: A review. Clinical Psychology Review. 2017;56:1–12. doi: 10.1016/j.cpr.2017.05.004. [DOI] [PubMed] [Google Scholar]
- Banh MK, Crane PK, Rhew I, Gudmundsen G, Vander Stoep A, Lyon A, McCauley E. Measurement equivalence across racial/ethnic groups of the mood and feelings questionnaire for childhood depression. Journal of abnormal child psychology. 2012;40(3):353–367. doi: 10.1007/s10802-011-9569-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. (1967). Depression: Clinical, experimental, and theoretical aspects. Hoeber Medical Division, Harper & Row
- Biglan A, Gau JM, Jones LB, Hinds E, Rusby JC, Cody C, Sprague J. The role of experiential avoidance in the relationship between family conflict and depression among early adolescents. Journal of Contextual Behavioral Science. 2015;4(1):30–36. doi: 10.1016/j.jcbs.2014.12.001. [DOI] [Google Scholar]
- Bijttebier P, Beck I, Claes L, Vandereycken W. Gray’s Reinforcement Sensitivity Theory as a framework for research on personality–psychopathology associations. Clinical Psychology Review. 2009;29(5):421–430. doi: 10.1016/j.cpr.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of abnormal psychology. 2007;116(2):313. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Burleson Daviss W, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the Mood and Feelings Questionnaire for depressive episodes in clinic and non-clinic subjects. Journal of Child Psychology and Psychiatry. 2006;47(9):927–934. doi: 10.1111/j.1469-7610.2006.01646.x. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. Origins and functions of positive and negative affect: a control-process view. Psychological review. 1990;97(1):19. doi: 10.1037/0033-295X.97.1.19. [DOI] [Google Scholar]
- Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, Fox NA. Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(9):928–935. doi: 10.1097/CHI.0b013e3181ae09df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of consulting and clinical psychology. 2002;70(1):6. doi: 10.1037/0022-006X.70.1.6. [DOI] [PubMed] [Google Scholar]
- Corr PJ. JA Gray’s reinforcement sensitivity theory: Tests of the joint subsystems hypothesis of anxiety and impulsivity. Personality and individual differences. 2002;33(4):511–532. doi: 10.1016/S0191-8869(01)00170-2. [DOI] [Google Scholar]
- Coyne JC. Depression and the response of others. Journal of abnormal psychology. 1976;85(2):186. doi: 10.1037/0021-843X.85.2.186. [DOI] [PubMed] [Google Scholar]
- Derntl B, Seidel EM, Eickhoff SB, Kellermann T, Gur RC, Schneider F, Habel U. Neural correlates of social approach and withdrawal in patients with major depression. Social Neuroscience. 2011;6(5–6):482–501. doi: 10.1080/17470919.2011.579800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epkins CC, Heckler DR. Integrating etiological models of social anxiety and depression in youth: Evidence for a cumulative interpersonal risk model. Clinical child and family psychology review. 2011;14(4):329–376. doi: 10.1007/s10567-011-0101-8. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Klein MH, Slattery MJ, Goldsmith HH, Kalin NH. Early risk factors and developmental pathways to chronic high inhibition and social anxiety disorder in adolescence. American Journal of Psychiatry. 2010;167(1):40–46. doi: 10.1176/appi.ajp.2009.07010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehm L, Beesdo K, Jacobi F, Fiedler A. Social anxiety disorder above and below the diagnostic threshold: prevalence, comorbidity and impairment in the general population. Social Psychiatry and Psychiatric Epidemiology. 2008;43(4):257–265. doi: 10.1007/s00127-007-0299-4. [DOI] [PubMed] [Google Scholar]
- Fox AS, Kalin NH. A translational neuroscience approach to understanding the development of social anxiety disorder and its pathophysiology. American Journal of Psychiatry. 2014;171(11):1162–1173. doi: 10.1176/appi.ajp.2014.14040449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fricke K, Vogel S. How interindividual differences shape approach-avoidance behavior: Relating self-report and diagnostic measures of interindividual differences to behavioral measurements of approach and avoidance. Neuroscience & Biobehavioral Reviews. 2020;111:30–56. doi: 10.1016/j.neubiorev.2020.01.008. [DOI] [PubMed] [Google Scholar]
- Gibb BE, McGeary JE, Beevers CG. Attentional biases to emotional stimuli: Key components of the RDoC constructs of sustained threat and loss. American Journal of Medical Genetics: Neuropsychiatric Genetics. 2016;171(1):65–80. doi: 10.1002/ajmg.b.32383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH. Depression in mothers. Annu Rev Clin Psychol. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. Journal of consulting and clinical psychology. 1995;63(1):90. doi: 10.1037/0022-006X.63.1.90. [DOI] [PubMed] [Google Scholar]
- Greco LA, Lambert W, Baer RA. Psychological inflexibility in childhood and adolescence: development and evaluation of the Avoidance and Fusion Questionnaire for Youth. Psychological assessment. 2008;20(2):93. doi: 10.1037/1040-3590.20.2.93. [DOI] [PubMed] [Google Scholar]
- Guyer AE, Silk JS, Nelson EE. The neurobiology of the emotional adolescent: From the inside out. Neuroscience & Biobehavioral Reviews. 2016;70:74–85. doi: 10.1016/j.neubiorev.2016.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Keenan-Miller D. Patterns of adolescent depression to age 20: The role of maternal depression and youth interpersonal dysfunction. Journal of abnormal child psychology. 2008;36(8):1189–1198. doi: 10.1007/s10802-008-9241-9. [DOI] [PubMed] [Google Scholar]
- Harlé KM, Simmons AN, Bomyea J, Spadoni AD, Taylor CT. Higher affective congruency in the approach-avoidance task is associated with insular deactivation to dynamic facial expressions. Neuropsychologia. 2021;151:107734. doi: 10.1016/j.neuropsychologia.2020.107734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuer K, Rinck M, Becker ES. Avoidance of emotional facial expressions in social anxiety: The approach–avoidance task. Behaviour research and therapy. 2007;45(12):2990–3001. doi: 10.1016/j.brat.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Higgins ET. Self-discrepancy: a theory relating self and affect. Psychological review. 1987;94(3):319. doi: 10.1037/0033-295X.94.3.319. [DOI] [PubMed] [Google Scholar]
- Howe-Martin LS, Murrell AR, Guarnaccia CA. Repetitive nonsuicidal self‐injury as experiential avoidance among a community sample of adolescents. Journal of Clinical Psychology. 2012;68(7):809–829. doi: 10.1002/jclp.21868. [DOI] [PubMed] [Google Scholar]
- Hundt NE, Nelson-Gray RO, Kimbrel NA, Mitchell JT, Kwapil TR. The interaction of reinforcement sensitivity and life events in the prediction of anhedonic depression and mixed anxiety-depression symptoms. Personality and individual differences. 2007;43(5):1001–1012. doi: 10.1016/j.paid.2007.02.021. [DOI] [Google Scholar]
- Idson LC, Liberman N, Higgins ET. Imagining how you’d feel: The role of motivational experiences from regulatory fit. Personality and Social Psychology Bulletin. 2004;30(7):926–937. doi: 10.1177/0146167204264334. [DOI] [PubMed] [Google Scholar]
- Kaldewaij, R., Koch, S. B., Volman, I., Toni, I., & Roelofs, K. (2016). On the control of social approach–avoidance behavior: Neural and endocrine mechanisms.Social behavior from rodents to humans,275–293 [DOI] [PubMed]
- Kent L, Vostanis P, Feehan C. Detection of major and minor depression in children and adolescents: evaluation of the Mood and Feelings Questionnaire. Journal of Child Psychology and Psychiatry. 1997;38(5):565–573. doi: 10.1111/j.1469-7610.1997.tb01543.x. [DOI] [PubMed] [Google Scholar]
- Ladd GW, Burgess KB. Charting the relationship trajectories of aggressive, withdrawn, and aggressive/withdrawn children during early grade school. Child development. 1999;70(4):910–929. doi: 10.1111/1467-8624.00066. [DOI] [PubMed] [Google Scholar]
- Ladouceur CD. Neural systems supporting cognitive-affective interactions in adolescence: the role of puberty and implications for affective disorders. Frontiers in Integrative Neuroscience. 2012;6:65. doi: 10.3389/fnint.2012.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange WG, Keijsers G, Becker ES, Rinck M. Social anxiety and evaluation of social crowds: Explicit and implicit measures. Behaviour research and therapy. 2008;46(8):932–943. doi: 10.1016/j.brat.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Leahy RL. Introduction: Emotional schemas, emotion regulation, and psychopathology. International Journal of Cognitive Therapy. 2012;5(4):359–361. doi: 10.1521/ijct.2012.5.4.359. [DOI] [Google Scholar]
- Leigh E, Clark DM. Understanding social anxiety disorder in adolescents and improving treatment outcomes: Applying the cognitive model of Clark and Wells (1995) Clinical child and family psychology review. 2018;21(3):388–414. doi: 10.1007/s10567-018-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Xu Y, Chen Z. Effects of the behavioral inhibition system (BIS), behavioral activation system (BAS), and emotion regulation on depression: A one-year follow-up study in Chinese adolescents. Psychiatry Research. 2015;230(2):287–293. doi: 10.1016/j.psychres.2015.09.007. [DOI] [PubMed] [Google Scholar]
- Loijen A, Vrijsen JN, Egger JI, Becker ES, Rinck M. Biased approach-avoidance tendencies in psychopathology: A systematic review of their assessment and modification. Clinical Psychology Review. 2020;77:101825. doi: 10.1016/j.cpr.2020.101825. [DOI] [PubMed] [Google Scholar]
- Lu W. Adolescent depression: national trends, risk factors, and healthcare disparities. American journal of health behavior. 2019;43(1):181–194. doi: 10.5993/AJHB.43.1.15. [DOI] [PubMed] [Google Scholar]
- Manos RC, Kanter JW, Busch AM. A critical review of assessment strategies to measure the behavioral activation model of depression. Clinical Psychology Review. 2010;30(5):547–561. doi: 10.1016/j.cpr.2010.03.008. [DOI] [PubMed] [Google Scholar]
- Martell, C. R., Addis, M. E., & Jacobson, N. S. (2001). Depression in context: Strategies for guided action. WW Norton & Co
- Mellick, W. H., Mills, J. A., Kroska, E. B., Calarge, C. A., Sharp, C., & Dindo, L. N. (2019). Experiential avoidance predicts persistence of major depressive disorder and generalized anxiety disorder in late adolescence.The Journal of Clinical Psychiatry, 80(6) [DOI] [PMC free article] [PubMed]
- Mellick WH, Vanwoerden S, Sharp C. Experiential avoidance in the vulnerability to depression among adolescent females. Journal of Affective Disorders. 2017;208:497–502. doi: 10.1016/j.jad.2016.10.034. [DOI] [PubMed] [Google Scholar]
- Molenaar PC, Campbell CG. The new person-specific paradigm in psychology. Current Directions in Psychological Science. 2009;18(2):112–117. doi: 10.1111/j.1467-8721.2009.01619.x. [DOI] [Google Scholar]
- NIMH (2017). Major depression among adolescents. Retrieved from https://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adolescents.shtml
- Ottenbreit, N. D., & Dobson, K. S. (2008). Avoidance. Risk factors in depression (pp. 447–470). Elsevier
- Papachristou H, Theodorou M, Neophytou K, Panayiotou G. Community sample evidence on the relations among behavioural inhibition system, anxiety sensitivity, experiential avoidance, and social anxiety in adolescents. Journal of Contextual Behavioral Science. 2018;8:36–43. doi: 10.1016/j.jcbs.2018.03.001. [DOI] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of youth and adolescence. 1988;17(2):117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Pfeifer JH, Allen NB. Puberty initiates cascading relationships between neurodevelopmental, social, and internalizing processes across adolescence. Biological Psychiatry. 2021;89(2):99–108. doi: 10.1016/j.biopsych.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS, Cohen E, Cohen P, Brook J. Adolescent depressive symptoms as predictors of adult depression: moodiness or mood disorder? American Journal of Psychiatry. 1999;156(1):133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- Price, R. B., & Woody, M. L. (2020). Emotional disorders in development. In S. Della, & Sala (Eds.), Encyclopedia of Behavioral Neuroscience (2 ed.). Elsevier Science
- Radke S, Güths F, André JA, Müller BW, de Bruijn ER. In action or inaction? Social approach–avoidance tendencies in major depression. Psychiatry Research. 2014;219(3):513–517. doi: 10.1016/j.psychres.2014.07.011. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Oar EL, Johnco CJ, Forbes MK, Fardouly J, Magson NR, Richardson CE. Adolescent development and risk for the onset of social-emotional disorders: A review and conceptual model. Behaviour research and therapy. 2019;123:103501. doi: 10.1016/j.brat.2019.103501. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Spence SH. The etiology of social phobia: Empirical evidence and an initial model. Clinical Psychology Review. 2004;24(7):737–767. doi: 10.1016/j.cpr.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical linear models: Applications and data analysis methods (1 vol.). sage
- Rezaei M, Ghazanfari F. The role of childhood trauma, early maladaptive schemas, emotional schemas and experimental avoidance on depression: A structural equation modeling. Psychiatry Research. 2016;246:407–414. doi: 10.1016/j.psychres.2016.10.037. [DOI] [PubMed] [Google Scholar]
- Roelofs K, Putman P, Schouten S, Lange WG, Volman I, Rinck M. Gaze direction differentially affects avoidance tendencies to happy and angry faces in socially anxious individuals. Behaviour research and therapy. 2010;48(4):290–294. doi: 10.1016/j.brat.2009.11.008. [DOI] [PubMed] [Google Scholar]
- Rose AJ, Rudolph KD. A review of sex differences in peer relationship processes: potential trade-offs for the emotional and behavioral development of girls and boys. Psychological Bulletin. 2006;132(1):98. doi: 10.1037/0033-2909.132.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, K. H., Bowker, J. C., Barstead, M. G., & Coplan, R. J. (2018). Avoiding and withdrawing from the peer group.
- Sacco, W. P., & Vaughan, C. A. (2006). Depression and the Response of Others. A Social-Cognitive Interpersonal Process Model
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7(2):147. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Seidel EM, Habel U, Finkelmeyer A, Schneider F, Gur RC, Derntl B. Implicit and explicit behavioral tendencies in male and female depression. Psychiatry Research. 2010;177(1–2):124–130. doi: 10.1016/j.psychres.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Dahl RE, Pollak SD. Pubertal development: correspondence between hormonal and physical development. Child development. 2009;80(2):327–337. doi: 10.1111/j.1467-8624.2009.01263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Davis S, McMakin DL, Dahl RE, Forbes EE. Why do anxious children become depressed teenagers? The role of social evaluative threat and reward processing. Psychological medicine. 2012;42(10):2095–2107. doi: 10.1017/S0033291712000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Stroud LR, Siegle GJ, Dahl RE, Lee KH, Nelson EE. Peer acceptance and rejection through the eyes of youth: pupillary, eyetracking and ecological data from the Chatroom Interact task. Social cognitive and affective neuroscience. 2012;7(1):93–105. doi: 10.1093/scan/nsr044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH, Jones RM, Casey B. A time of change: behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain and cognition. 2010;72(1):124–133. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP. Rewards, aversions and affect in adolescence: emerging convergences across laboratory animal and human data. Developmental cognitive neuroscience. 2011;1(4):390–403. doi: 10.1016/j.dcn.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Struijs SY, Lamers F, Vroling MS, Roelofs K, Spinhoven P, Penninx BW. Approach and avoidance tendencies in depression and anxiety disorders. Psychiatry Research. 2017;256:475–481. doi: 10.1016/j.psychres.2017.07.010. [DOI] [PubMed] [Google Scholar]
- Sund AM, Larsson B, Wichstrøm L. Depressive symptoms among young Norwegian adolescents as measured by the Mood and Feelings Questionnaire (MFQ) European child & adolescent psychiatry. 2001;10(4):222–229. doi: 10.1007/s007870170011. [DOI] [PubMed] [Google Scholar]
- Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. The Lancet. 2012;379(9820):1056–1067. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trew JL. Exploring the roles of approach and avoidance in depression: An integrative model. Clinical Psychology Review. 2011;31(7):1156–1168. doi: 10.1016/j.cpr.2011.07.007. [DOI] [PubMed] [Google Scholar]
- Venta A, Sharp C, Hart J. The relation between anxiety disorder and experiential avoidance in inpatient adolescents. Psychological assessment. 2012;24(1):240. doi: 10.1037/a0025362. [DOI] [PubMed] [Google Scholar]
- Voncken M, Rinck M, Deckers A, Lange WG. Anticipation of social interaction changes implicit approach-avoidance behavior of socially anxious individuals. Cognitive therapy and research. 2012;36(6):740–749. doi: 10.1007/s10608-011-9408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrijsen JN, van Oostrom I, Speckens A, Becker ES, Rinck M. Approach and avoidance of emotional faces in happy and sad mood. Cognitive therapy and research. 2013;37(1):1–6. doi: 10.1007/s10608-012-9436-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood A, Kroll L, Moore A, Harrington R. Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: a research note. Journal of Child Psychology and Psychiatry. 1995;36(2):327–334. doi: 10.1111/j.1469-7610.1995.tb01828.x. [DOI] [PubMed] [Google Scholar]
- Woody, M. L., & Price, R. B. (2020). Targeting Neurodevelopmental Mechanisms in Emotional Disorders Through Intervention. In S. D. Sala (Ed.), Encyclopedia of Behavioral Neuroscience (2 ed.). Elsevier Science
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.