ABSTRACT
Invasive species related to climate change and/or globalization may be associated with novel forms of kidney disease. This is the case for wasps. Several species of Asian wasps are increasingly found in America (e.g. Asian giant hornet, Vespa mandarinia) and Europe (e.g. yellow-legged Asian hornet, V. velutina; black shield hornet, V. bicolor; and Oriental hornet, V. orientalis). Some of these species have been associated with human deaths and acute kidney injury. The literature on wasps and acute kidney injury is scarce and mostly originates from Asia, so nephrologists outside Asia are not familiar with this health problem. In a recent issue of ckj, Liu et al. describe a simple, four-item Wasp Sting Severity Score (WSS) developed from 1131 wasp sting patients. Vespa mandarinia and V. velutina were among those causing hospitalization, although most cases were caused by the black-bellied hornet (V. basalis). Liu et al. propose that a WSS ≥3 should guide early (<24 h after stings) plasma exchange, as plasma exchange was associated with lower mortality in severely affected patients but continuous venovenous haemofiltration and haemoperfusion were not. The WSS will require external validation. This manuscript should raise awareness about the potentially fatal consequences of stings by wasp species making their way into America and Europe.
Keywords: acute kidney injury, continuous venovenous haemofiltration, mortality, sting, wasp
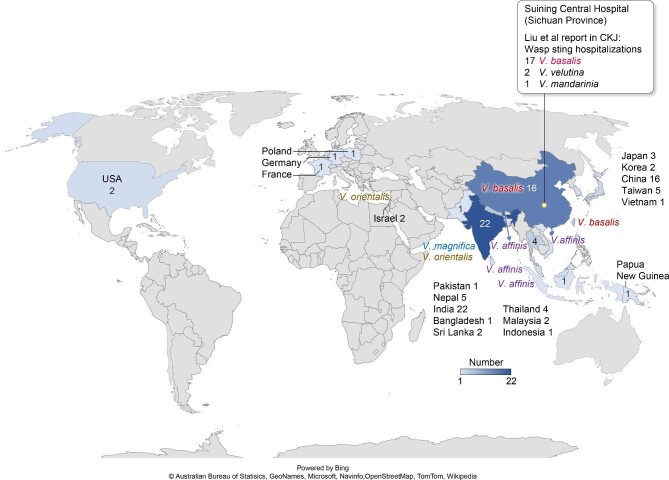
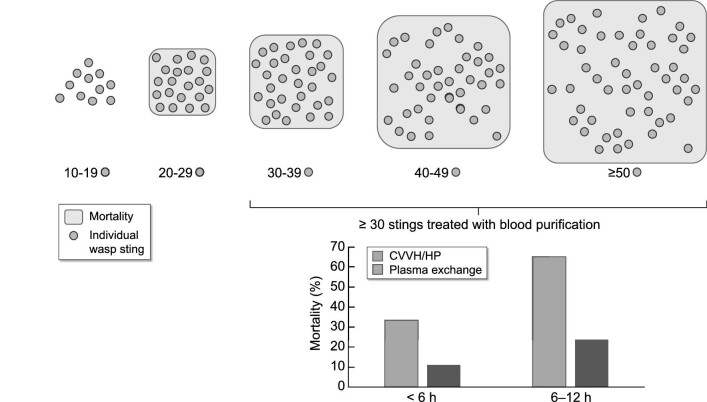
The earliest PubMed-listed manuscript retrieved by the search ‘wasp AND (acute kidney injury OR acute renal failure)’ dates to 1972, which is a relatively recent date for a health issue that is likely to have existed for millennia [1]. This first report was from Thailand, and most reports since have been from Asia (Supplementary data, Table S1). Indeed, as of 10 January 2022, PubMed listed 73 reports from 19 countries, 15 of them in Asia. Thus, nephrologists in Europe and North America may not be familiar with a health issue that is increasingly recognized, as 2022 was the year on record with the most reports on wasp stings and acute kidney injury (AKI) (Fig. 1). Most reports emerged from South and East Asia and involved mainly Vespa magnifica and V. orientalis (India), V. basalis (China and Taiwan) and V. affinis (Southeast Asia) (Fig. 2). However, nephrologists may be more familiar with news bulletins on invasive wasp species in America and Europe. News such reports as ‘Murder Hornets’ in the USA referring to the Asian giant hornet, V. mandarinia, and ‘Spain tourist warning as killer wasp spreads at unstoppable rate’ referring to the yellow-legged Asian hornet (V. velutina) may have drawn their attention [1–3]. Indeed, V. mandarinia has been detected since 2019 in western British Columbia, Canada and Washington State and the USA, and constitutes a problem for honeybees and humans [4]. In Europe, V. velutina arrived in Bordeaux in 2005 and has since expanded to Italy, Germany, Belgium, the Netherlands, the UK and Portugal, where it kills honeybees [5]. Both species can induce AKI and/or be lethal [5, 6]. Additionally, the black shield hornet (V. bicolor) and Oriental hornet (V. orientalis) have also been detected in Spain [6]. However, nephrologists should be familiar with local wasp species and with the kidney and extrarenal complications of wasp stings, as they may be involved in care for wasp sting patients early on in the course of the disease, when they are requested to provide blood purification services, or after wasp sting patients develop AKI.
Figure 1:
Number reports per year found by the PubMed search ‘wasp AND (acute kidney injury OR acute renal failure)’ on 10 January 2022.
Figure 2:
Geographical distribution and wasp species identified in reports found by the PubMed search ‘wasp AND (acute kidney injury OR acute renal failure)’ on 10 January 2022. Details provided in Supplementary data, Table S1. The Asian wasp V. mandarinia has been found in America, while V. velutina and V. orientalis have been found in Europe. The location of Suining Central Hospital (Sichuan Province) and the species reported by Liu et al. to be associated with hospitalization are also indicated [7].
In a recent issue of ckj, Liu et al. describe their experience at Suining Central Hospital (Sichuan Province, southwest China) where they treat 100–200 wasp sting patients per year and now report the experience with 1284 patients from 2011 to 2020 [7]. Consistent with other reports from China, most cases were due to V. basalis stings (Fig. 2). However, stings by species found to be invasive in America (V. mandarinia) and Europe (V. velutina) were also involved. The manuscript provides images of these species that may be helpful for physicians unfamiliar with this health issue. Given the frequency of the diagnosis, Suining Central Hospital developed a protocolized approach consistent of antiallergic or antishock treatment (adrenaline, corticosteroids and antihistamines), local treatment (removal of stingers, local dexamethasone and lidocaine), toxin elimination and prevention of AKI caused by rhabdomyolysis and haemolysis (hydration, diuretics and urine alkalinization), analgesia and tetanus antitoxin. Additionally, in severe patients with multiple stings, they have used continuous venovenous haemofiltration (CVVH), haemoperfusion (HP) or plasma exchange to improve the prognosis of severe wasp sting patients. The rationale for the extracorporeal blood purification is to remove toxins that may lead to organ failure.
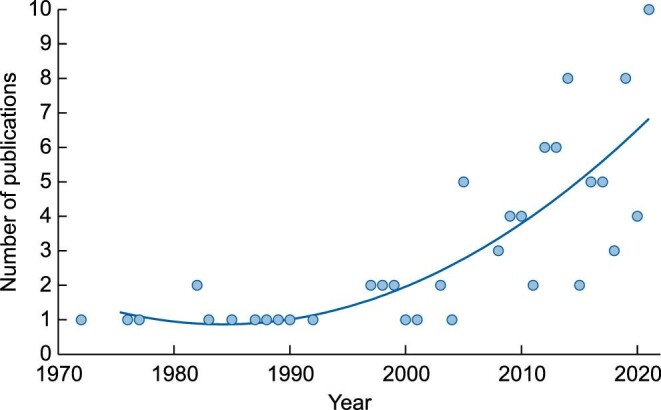
The number of wasp stings was associated with mortality (Fig. 3), but there were other factors related to the impact of the stings on each patient. Thus, Liu et al. developed a simple Wasp Sting Severity Score (WSS) from 1131 wasp sting patients from 2011 to 2019 and validated it in 153 patients from 2020. The WSS has four items: tea-coloured urine, number of stings, lactate dehydrogenase and total bilirubin. Severe cases were defined as those that required blood purification due to haemolysis, rhabdomyolysis or manifested organ dysfunction (Sequential Organ Failure Assessment score ≥2). A high (≥3) WSS value had an area under the curve of 0.918 (95% confidence interval 0.873–0.962) to predict the need of blood purification in the prospective validation cohort.
Figure 3:
Relationship between number of stings and mortality. This conceptual figure summarizes data presented in Fig. 1D from [7]. Fewer than 20 stings were not associated with mortality, but mortality increased with a higher number of stings and peaked with 50 or more stings. The size of each square represents mortality, which ranged from <10% for 20–29 stings to >60% for 50 or more stings. Each circle represents one sting and the number of circles within each mortality square represents the start number for the category (i.e. 20 circles represent 20–29 stings).
The authors suggest that the WSS should guide the early institution of plasma exchange. As soon as the WSS value is ≥3, plasma exchange should be initiated—at the latest, within 24 h of the wasp stings. The rationale for such suggestion is that in their observational study, plasma exchange was associated with lower mortality, but CVVH and HP were not. Thus, the effect of blood purification within 24 h after admission on mortality was explored in patients with >30 wasp stings. Among these patients, mortality was 35–45%, but among those receiving plasma exchange within the first 24 h, mortality was 14%. Indeed, the introduction of plasma exchange in 2017 was associated with a drop in mortality. However, comparing older with more recent cases has an implicit bias regarding factors such as improved overall medical technology, resources and knowledge. A further observation was a numerical trend to higher mortality when blood purification as started after 6 h (Fig. 3). While differences were not statistically significant, these data should serve as guidance for a potentially lethal disease for which information is scarce. This underlies the suggestion to start plasma exchange as soon as possible after the WSS hits 3.
There is some debate as to what constitutes a severe case of wasp stings and what numbers of stings are potentially lethal. The wasp species is a key factor. Native American and European species are considerably less toxic than Asian species. As examples referenced by Liu et al., the USA reports of a lethal dose of 20 stings/kg [8, 9] do not apply to Asian wasps that may kill with as few as >20 stings per person [7]. As Asian wasps invade America and Europe, the report by Liu et al. on how to identify severe wasp sting cases very early in the course of the disease and how to proceed thereafter becomes of universal interest.
While we have focused our comments on wasp stings, bee stings may also cause AKI and death, and the geographical distribution differs from that of wasp stings, as Africa and America are overrepresented. Cases have mostly involved the East African lowland honeybee (Apis mellifera scutellata) in Africa, and Africanized honeybees, resulting from the crossbreeding of the East African lowland honeybee with European subspecies of the western honeybee (A. mellifera). African and Africanized honeybees are more aggressive towards humans and other animals, and attacks can result in hundreds to over a thousand bee stings, i.e. almost a degree of magnitude higher number than for severe wasp stings. Initial reports of AKI came from Africa [10]. However, since the introduction of the East African lowland honeybee to Brazil in the 1950s, Africanized honeybees spread throughout South America and arrived in North America in 1985, leaving a string of reports of cases of AKI and deaths, frequently in Spanish and Portuguese [11, 12]. In fact, one of those attacks in Colombia leading to AKI in a 17-year-old woman arouses the interest in nephrology for one of the authors of the present manuscript (S.C.).
Supplementary Material
Contributor Information
Sol Carriazo, IIS-Fundacion Jimenez Diaz UAM, Madrid, Spain; RICORS2040, Madrid, Spain; Department of Medicine, School of Medicine, Universidad Autonoma de Madrid, Madrid, Spain.
Alberto Ortiz, IIS-Fundacion Jimenez Diaz UAM, Madrid, Spain; RICORS2040, Madrid, Spain; Department of Medicine, School of Medicine, Universidad Autonoma de Madrid, Madrid, Spain.
FUNDING
FIS/Fondos FEDER (PI18/01366, PI19/00588, PI19/00815, PI21/00251, DTS18/00032, ERA-PerMed-JTC2018) (KIDNEY ATTACK AC18/00064 and PERSTIGAN AC18/00071, ISCIII-RETIC REDinREN RD016/0009), Sociedad Española de Nefrología, FRIAT, Comunidad de Madrid en Biomedicina B2017/BMD-3686 CIFRA2-CM. Instituto de Salud Carlos III (ISCIII) RICORS programme to RICORS2040 (RD21/0005/0001), FEDER funds.
CONFLICT OF INTEREST STATEMENT
A.O. has received consultancy or speaker fees or travel support from Astellas, AstraZeneca, Amicus, Amgen, Fresenius Medical Care, Bayer, Sanofi-Genzyme, Menarini, Kyowa Kirin, Alexion, Otsuka and Vifor Fresenius Medical Care Renal Pharma and is Director of the Catedra Mundipharma-UAM of diabetic kidney disease and the Catedra AstraZeneca-UAM of chronic kidney disease and electrolytes. A.O. is the Editor-in-Chief of ckj.
REFERENCES
- 1. Sitprija V, Boonpucknavig V. Renal failure and myonecrosis following wasp-stings. Lancet 1972; 1: 749–750 [DOI] [PubMed] [Google Scholar]
- 2.‘Murder Hornets’ in the U.S. https://www.nytimes.com/2020/05/02/us/asian-giant-hornet-washington.html (10 January 2022, date last accessed) [Google Scholar]
- 3. Spain tourist warning as killer wasp spreads at unstoppable rate. https://www.express.co.uk/travel/articles/1513104/spain-tourist-warning-deadly-killer-wasp-costa-del-sol-latest#:∼:text=The%20killer%20wasps%20were%20responsible,are%20allergic%20to%20the%20sting (10 January 2022, date last accessed) [Google Scholar]
- 4. Zhu G, Gutierrez Illan J, Looney Cet al. Assessing the ecological niche and invasion potential of the Asian giant hornet. Proc Natl Acad Sci USA 2020; 117: 24646–24648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feás X. Human fatalities caused by hornet, wasp and bee stings in Spain: epidemiology at state and sub-state level from 1999 to 2018. Biology (Basel) 2021; 10: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yanagawa Y, Morita K, Sugiura Tet al. Cutaneous hemorrhage or necrosis finding after Vespa mandarinia (wasp) stings may predict the occurrence of multiple organ injury: a case report and review of literature. Clin Toxicol 2007; 45: 803–807 [DOI] [PubMed] [Google Scholar]
- 7. Liu Y, Shu H, Long Yet al. Development and internal validation of a Wasp Sting Severity Score to assess severity and indicate blood purification in persons with Asian wasp stings. Clin Kidney J 2022; 15: 320–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fitzgerald KT, Flood AA. Hymenoptera stings. Clin Tech Small Anim Pract 2006; 21: 194–204 [DOI] [PubMed] [Google Scholar]
- 9. Schmidt JO. Clinical consequences of toxic envenomations by Hymenoptera. Toxicon 2018; 150: 96–104 [DOI] [PubMed] [Google Scholar]
- 10. Humblet Y, Sonnet J, van Ypersele de Strihou C. Bee stings and acute tubular necrosis. Nephron 1982; 31: 187–188 [DOI] [PubMed] [Google Scholar]
- 11. Silva GBD Jr, Vasconcelos AG Jr, Rocha AMTet al. Acute kidney injury complicating bee stings - a review. Rev Inst Med Trop Sao Paulo 2017; 59: e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mejía Vélez G. Insuficiencia renal aguda por picadura múltiple de abejas Africanizadas. Comunicación de 43 casos [Acute renal failure due to multiple stings by Africanized bees. Report on 43 cases]. Nefrologia 2010; 30: 531–538 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.