Abstract
Background
Total Knee Arthroplasty (TKA) is an established surgical option for knee osteoarthritis (OA). There are varying perceptions of the most suitable surgical technique for making bone cuts in TKA. Conventional Instrumentation (CI) uses generic cutting guides (extra- and intra-medullary) for TKA; however, patient specific instrumentation (PSI) has become a popular alternative amongst surgeons.
Methods
A literature search of electronic databases Embase, Medline and registry platform portals was conducted on the 16th May 2021. The search was performed using a predesigned search strategy. Eligible studies were critically appraised for methodological quality. The primary outcome measure was Knee Society Function Score. Functional scores were also collected for the secondary outcome measures: Oxford Knee Score (OKS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), Knee Injury and Osteoarthritis Outcome Score (KOOS) and Visual Analog Scale (VAS) for pain. Review Manager 5.3 was used for all data synthesis and analysis.
Results
There is no conclusive evidence in the literature to suggest that PSI or CI instrumentation is better for functional outcomes. 23 studies were identified for inclusion in this study. Twenty-two studies (18 randomised controlled trials and 4 prospective studies) were included in the meta analysis, with a total of 2277 total knee arthroplasties. There were 1154 PSI TKA and 1123 CI TKA. The majority of outcomes at 3-months, 6-months and 12 show no statistical difference. There was statistical significance at 24 months in favour of PSI group for KSS function (mean difference 4.36, 95% confidence interval 1.83–6.89). The mean difference did not exceed the MCID of 6.4. KSS knee scores demonstrated statistical significance at 24 months (mean difference 2.37, 95% confidence interval (CI) 0.42—4.31), with a MCID of 5.9. WOMAC scores were found to be statistically significant favouring PSI group at 12 months (mean difference -3.47, 95% confidence interval (CI) -6.57- -0.36) and 24 months (mean difference -0.65, 95% confidence interval (CI) -1.28—-0.03), with high level of bias noted in the studies and a MCID of 10.
Conclusions
This meta-analysis of level 1 and level 2 evidence shows there is no clinical difference when comparing PSI and CI KSS function scores for TKA at definitive post operative time points (3 months, 6 months, 12 months and 24 months). Within the secondary outcomes for this study, there was no clinical difference between PSI and CI for TKA. Although there was no clinical difference between PSI and CI for TKA, there was statistical significance noted at 24 months in favour of PSI compared to CI for TKA when considering KSS function, KSS knee scores and WOMAC scores. Studies included in this meta-analysis were of limited cohort size and prospective studies were prone to methodological bias. The current literature is limited and insufficiently robust to make explicit conclusions and therefore further high-powered robust RCTs are required at specific time points.
Keywords: Total Knee Arthroplasty, Patient-Specific, Meta-analysis
Background
Knee osteoarthritis (OA) is a leading cause of global disability [1], with Total Knee Arthroplasty (TKA) accepted as a well-recognised and established therapy [2]. It causes considerable pain and debilitation in the elderly, decreasing their quality of life [3]. There is an overall increase in the incidence of TKA over the past 25 years across all age groups [4]. In the UK, the rates for women who have undergone knee replacements has increased from 43 per 100 000 person years in 1991 to 137 per 100 000 person years in 2006 [5]. There is a predicted increase in the demand of TKA in the USA by 673% by the year 2030 [6]. Although there has been a broadening in surgical options including uni-condylar replacements and tibial osteotomies, total knee replacements remain at the centre of surgical management for OA [7].
Conventional instrumentation (CI) and patient-specific instrumentation (PSI) have been used to aid accurate implant placement [8]. CI for TKA is based on the concept of using intramedullary and extramedullary guides for alignment. Satisfactory post-operative alignment is necessary to achieve good functional outcomes and longevity of the prosthesis [9]. Studies have suggested that both function and survivorship are significantly improved if a post-operative alignment of less than three degrees, in the mechanical axis, is obtained [10, 11].
Patient specific instrumentation (PSI) is custom made using data obtained from computed tomography (CT) or magnetic resonance imaging (MRI) to create bespoke cutting blocks. This imaging also allows pre-operative planning of the best size of prosthesis. In addition, long-leg alignment radiographs enable determination of optimal positioning of the prosthesis. Once optimal positioning and sizing are known, the PSI is built in a 3-dimensional (3D) printer allowing instrumentation creation customised to the patient’s anatomy [12].
If the use of custom-made instrumentation can be proven to improve TKA component positioning it should, in theory, translate to better functional outcomes and prosthetic longevity. A recent meta-analysis by Mannan et al. including literature from 2000 to 2015 revealed eight randomised controlled trials (RCT’s) [13] and concluded that there was no conclusive evidence to support PSI or CI for TKA. Simiarly, a pooled meta-analysis found no difference between PSI and CI at less than one year or at more than one year post surgery [14]. In recent years many high quality studies of level I and level II evidence articles have been published with more varied outcome measures over more substantial periods. This allows for a further scrutination of the functional outcome of PSI and CI at definitive time points. This will allow for a direct comparison between PSI and CI at a given time point.
The present study intends to comprehensively scrutinise the literature to ascertain the result of functional outcomes for PSI compared to CI in TKA, when compared at a specific time point post TKA. In order to comprehensively scrutinise the literature and provide robust clinical recommendations, we have conducted the most current meta-analysis to evaluate the functional outcomes of PSI versus CI for total knee arthroplasty.
Methods
Literature search
This systematic review was conducted in accordance with the “Preferred Reporting Items for Systematic reviews and Meta-analyses” (PRISMA) statement [15]. We identified relevant articles through the MEDLINE and Embase databases on the 16th May 2021. A date restriction of January 2004 was specified. The search was performed using MESH terms and free terms for “patient-specific instrumentation” OR “custom-fit” OR “PSI” OR “patient specific instrumentation” AND “total knee arthroplasty” OR “TKA” OR “knee arthroplasty” OR “knee replacement.”
Eligibility criteria
All randomised controlled trials (RCTs) and prospective comparative studies, where at least one of the selected functional outcomes is reported was considered for inclusion in the study. We adopted a three stage screening process (title screening, abstract screening and full-text screening). All titles, abstracts and full text of articles that were deemed suitable for extraction were retrieved and reviewed independently by two of the co-authors (HM & BR). Consensus was gained amongst all five co-authors where there was disagreement regarding included studies. The study protocol was not registered on PROSPERO in time before the data collection was performed.
Inclusion criteria
Level I and Level II (prospective comparative studies) evidence;
Subjects of any country of origin;
Patients undergoing primary total knee arthroplasty;
A minimum of ten participants in each study arm;
Exclusion criteria
Studies primarily evaluating kinematic or radiographic alignment;
Studies of a foreign language were excluded, unless a translation was available;
Cutting guide or implant positioning studies;
Case reports;
Outcome measures
The primary outcome measures of interest for this review was Knee Society Score – Function.
The secondary outcome measures of interest for this review were as follows:
Knee Society Score (KSS)—Knee
Knee Society Score – Global
Oxford Knee Score (OKS)
WOMAC (Western Ontario and McMaster Universities arthritis Index)
Pain score
KOOS: KOOS pain, KOOS symptoms, KOOS Sports, KOOS Activities of Daily Living (ADL), KOOS Quality of Life (QOL)
Searching other resources
The trials register at ClinicalTrials.gov (http://clinicaltrials.gov/) and the World Health Organisation (WHO) International Clinical Trials Registry Platform search portal (http://apps.who.int/trialsearch/) were reviewed for any ongoing or planned trials. Results were screened based on their abstracts and compared against the inclusion and exclusion criteria.
Data extraction
The data from each study were entered into Microsoft Excel (2007). Data extracted included name of journal, type of patient specific instrumentation used, follow up period, study design and origin, image acquisition, sample size, age of population and outcome measures considered. Data was independently extracted by two co-authors (BR & HM) and verified by another author (NP).
Data synthesis and statistical analysis
All outcome measures were continuous. A mean difference between PSI and CI groups was determined. The minimal clinically important difference (MCID) was used for all outcomes which were deemed statistically significant. This ensured clinical relevance to the outcomes assessed. The MCID was calculated with linear regression to minimise bias [16].
Review Manager 5.3 was used for all data synthesis and analysis. The “random effects model” was applied if high heterogeneity existed between the compared studies. Final results for each parameter were displayed in a forest plot. Confidence intervals were also displayed. Heterogeneity was formally determined with I2 (where 0 to 25% indicates low heterogeneity, 25% to 75% indicates moderate heterogeneity, and > 75% suggests high heterogeneity).
For this meta-analysis, only level 1 and level 2 evidence was used. This ensured improved levels of methodological homogeneity. Clinical heterogeneity – based on characteristics table – similar age group across all studies. Timings of outcomes were delineated to ensure high level of homogeneity.
Methodological quality assessment
All RCT’s and prospective comparative studies were reviewed independently for quality by two of the co-authors (BR & NP). Where there was any difference in quality assessment, the senior author (SB) made the final decision. The quality of the methods was assessed by the trial quality characteristics and associated risk of bias. For randomised controlled trials, six parameters were used:
Randomisation method
Allocation Concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome measures
Selective reporting bias
Each parameter was labelled as low risk of bias, unclear or high risk of bias. For non-randomised studies, the methodological index for non-randomised studies (MINORS) criteria [17] was used to scrutinise the study against a validated scoring method.
Results
Literature search results
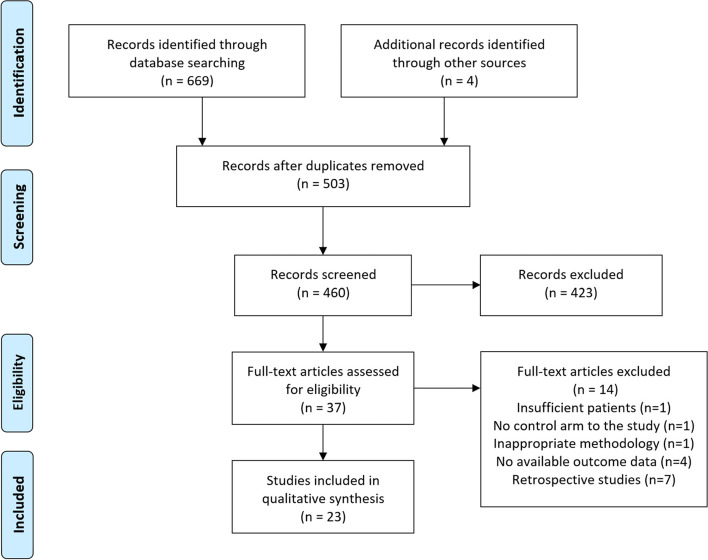
The initial search of the databases yielded 669 results. Four articles were added by identifying suitable articles through other sources. The PRISMA flow diagram for this search is shown in Fig. 1. In total, 23 studies with a total of 2277 total knee arthroplasties were included in the review. There were 1154 PSI TKA and 1123 CI TKA. In the study, 18 RCT’s and 5 prospective studies were included (Fig. 1). 22 studies underwent qualitative review as Moorthy et al. [18] was the only study to report 5 year PROM outcomes.
Fig. 1.
The Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) flow diagram to show study selection
Quality assessment
The majority of studies described suitable random sequence generation and randomisation methods. However, there was variable levels of bias due to the methods of allocation concealment across the RCT’s considered. All studies were affected by high risk of bias for the blinding of both participants and personnel. This was partly due to inherent inability to blind the operative team. In addition, patients receiving PSI underwent MRI or CT. This could have led to the patient being aware of the requirement for MRI or CT for a custom made block.
The risk of bias assessment across all the randomised controlled trials of included studies is displayed in Table 1. All non-randomised studies were assessed against the MINORS criteria for comparative studies with a subjective score given out of 24 [17]. A table illustrating the scores is shown in Table 2.
Table 1.
A table displaying the risk of bias for each of the included randomized studies. The colour represents the quality in the each of the domains (Red = High risk, Yellow = uncertain and Green = low risk)
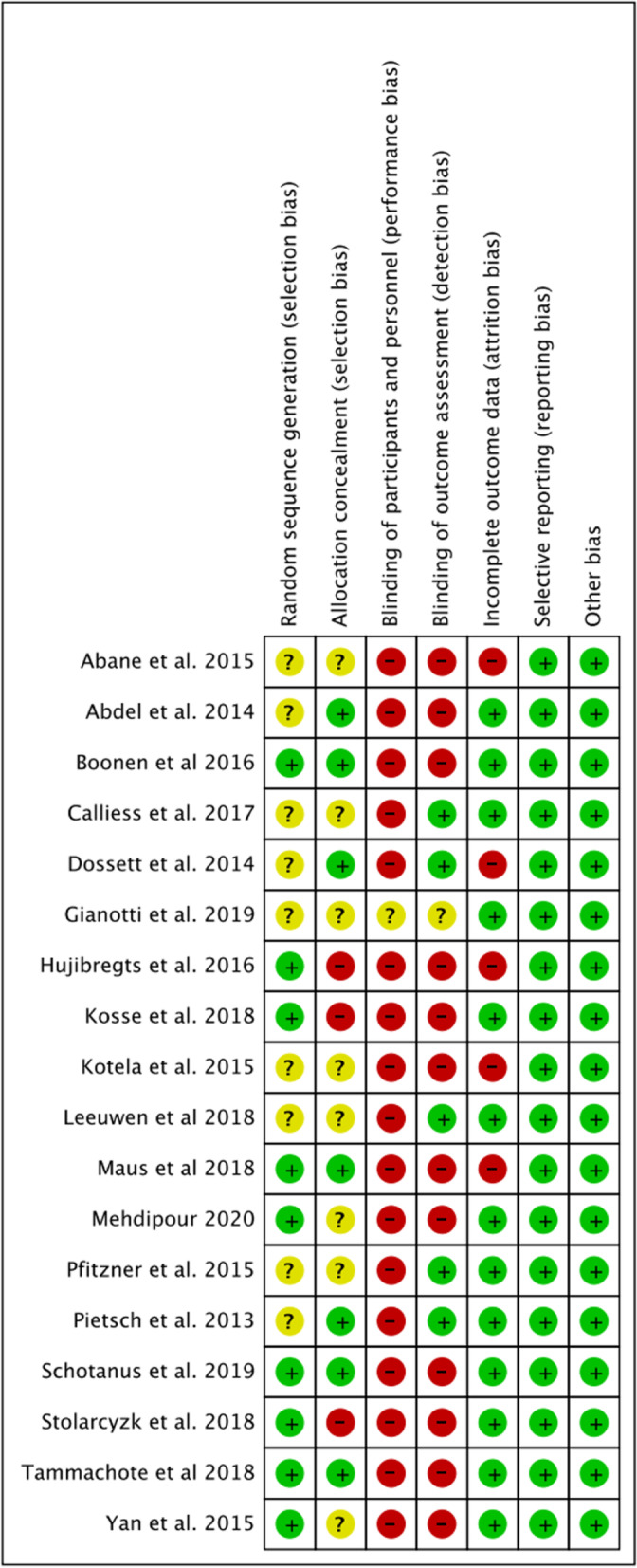
Table 2.
A table to illustrate the methodological index for non-randomised studies (MINORS) criteria [17]
Characteristics of studies included
The details of the 23 studies (18 RCTs and 5 prospective studies) included in the systematic review are summarised in Table 3. Twenty-two studies (18 RCTs and 4 prospective studies) were involved in the meta-analysis.
Table 3.
Characteristics of publications included in the present study
| Author | Journal | System used | Follow up | Type of study | Image acquisition | Location | Number of PSI | Number of CI | Mean age |
|---|---|---|---|---|---|---|---|---|---|
| Pietsch et al. 2013 [23] | Knee surgery sports traumatology and Arthroscopy | Materialise | 3 months | RCT | MRI | Austria | 40 | 40 | 71.4(6.6):69.2(9.4) |
| Pfitzner et al. 2014 [24] | Clinical orthopaedic and related research | Visionaire | 3 months | RCT | MRI/CT | Germany | 60 | 30 | 64.0(54–74): 64.0(54–74) |
| Yaffe et al. 2014 [21] | Int Journal of Computer assisted radiology and surgery | PSI | 6 months | Prospective comparative | MRI | USA | 44 | 40 | 68.3:64 |
| Abdel et al. 2014 [25] | Clinical orthopaedic and related research | Materialise | 3 months | RCT | MRI | France | 20 | 20 | 71.0(61–81) 71(55–83) |
| Dossett et al. 2014 [26] | The Bone and Joint Journal | Visionaire | 2 years | RCT | MRI | USA | 44 | 44 | 66.0(7.7): 66.0(8.6) |
| Abane et al. 2015 [27] | Bone and Joint Journal | Visionaire | 3 months | RCT | MRI | France | 70 | 70 | 67.8(47–84): 70.4(54–83) |
| Yan et al. 2015 [28] | Knee surgery sports traumatology | Materialise | 3 months | RCT | MRI | Hong Kong | 30 | 30 | 67.5(8.0): 69.5(8.4) |
| Kotela et al. 2015 [29] | Biomed research international | Signature | 12 months | RCT | CT | Poland | 49 | 46 | 66.1(8.4): 68.6(9.9) |
| Chen et al. 2015 [20] | Journal of arthroplasty | PSI | 2 years | Prospective comparative | MRI | Singapore | 29 | 30 | 65.0(8.0) 65.0(8.0) |
| Anderl et al. 2016 [19] | Knee surgery sports traumatology | MyKnee | 2 years | Prospective comparative | CT | Austria | 114 | 108 | 68.7(8.2): 67.7(9.6) |
| Hujibregts et al. 2016 [30] | The Bone and Joint Journal | Visionaire | 1 year | RCT | CT | Holland | 69 | 64 | 66.7:69 |
| Boonen et al. 2016 [31] | Bone and Joint Journal | Signature | 44 months | RCT | MRI | Netherlands | 90 | 90 | 69.0(8.0):65.0(8.8) |
| Calliess et al. 2017 [32] | Knee surgery sports traumatology | Stryker Shapematch | 12 months | RCT | MRI | Germany | 100 | 100 | 70(8):67(8) |
| Zhu et al. 2017 [22] | Knee surgery sports traumatology and Arthroscopy | Trumatch | 2 years | Prospective comparative | CT | Singapore | 42 | 48 | 69.3(7.2):66.8(5.9) |
| Van Leeuwen et al. 2018 [33] | Acta Orthopaedics | Signature | 2 years | RCT | MRI | Norway | 44 | 50 | 67(8.8):64(6.9) |
| Stolarczyk et al. 2018 [34] | Clinical and Experimental Biomedcine | Visionaire | 3 months | RCT | MRI | Poland | 30 | 30 | 70.2(5.9):69.6(7.1) |
| Maus et al. 2018 [35] | Knee surgery sports traumatology and Arthroscopy | Imprint | 3 months | RCT | MRI | Germany | 59 | 66 | 68.1(8.5):71.5(8.1) |
| Tammachote et al. 2018 [36] | The Journal of Arthroplasty | Visionaire | 2 years | RCT | MRI | Thailand | 54 | 54 | 72.0(7.0):72.0(8.0) |
| Kosse et al. 2018 [37] | Knee Surgery Sports Traumatology and Arthroscopy | Visionare | 12 months | RCT | MRI | Netherlands | 21 | 21 | 62.7(4.5):63.4(4.2) |
| Schotanus et al. 2019 [38] | Knee surgery sports traumatology | Signature | 5 years | RCT | MRI | Holland | 83 | 80 | 71.8 |
| Giannotti et al. 2019 [12] | Musculoskeletal surgery | PSI | 2 months | RCT | MRI | Italy | 20 | 20 | 71:73 |
| Mehdipour et al. 2020 [39] | Archives of Bone and Joint Surgery | PSI | 2 years | RCT | CT | Iran | 12 | 12 | 60.3:62.6 |
| Moorthy et al. 2021 [18] | Archives of Orthopaedic and Trauma Surgery | Zimmer PSI | 5 years | Prospective comparative | MRI | Singapore | 30 | 30 | NR |
Primary outcome
Outcome 1: Knee Society Score (KSS) – Function
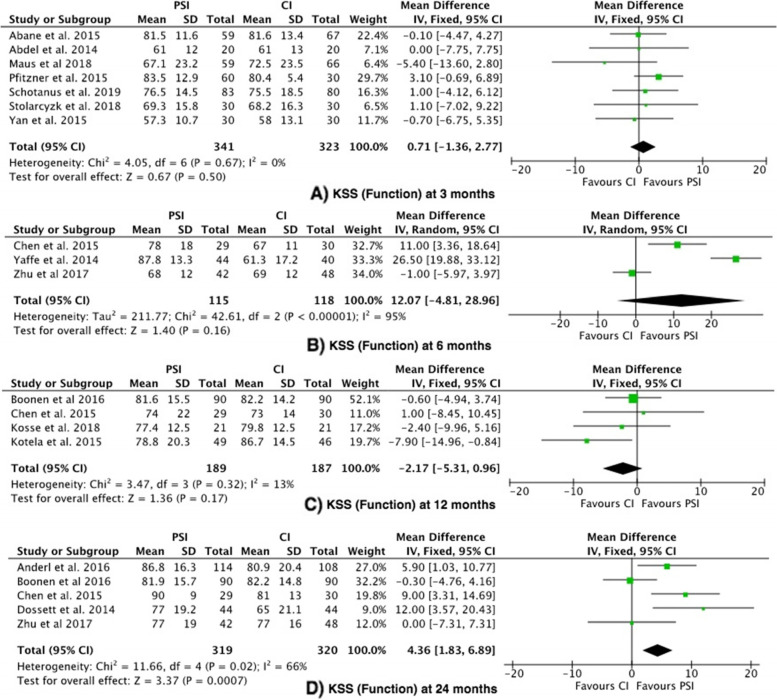
The Knee Society Score was reported in 16 studies [19–29, 31, 34, 35, 37, 38]. KSS Functional score was significantly higher in the PSI group (favouring PSI) at 24 months in the 5 studies compared (mean difference 4.36, 95% confidence interval 1.83–6.89), with moderate heterogeneity (I2 = 66%) [19, 20, 22, 26, 31]. Three out of the 5 studies reported a statistical significance in the difference between PSI and CI, with regards to KSS function scores [19, 20, 26]. The mean difference (4.36) was less than the MCID (6.4). There was no statistically significant difference observed at 3, 6 or 12 months (Fig. 2).
Fig. 2.
Forest plots of the comparison of KSS (Function) scores at (A) 3 Months, (B) 6 Months and (C) 12 to 24 Months. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
Secondary outcomes
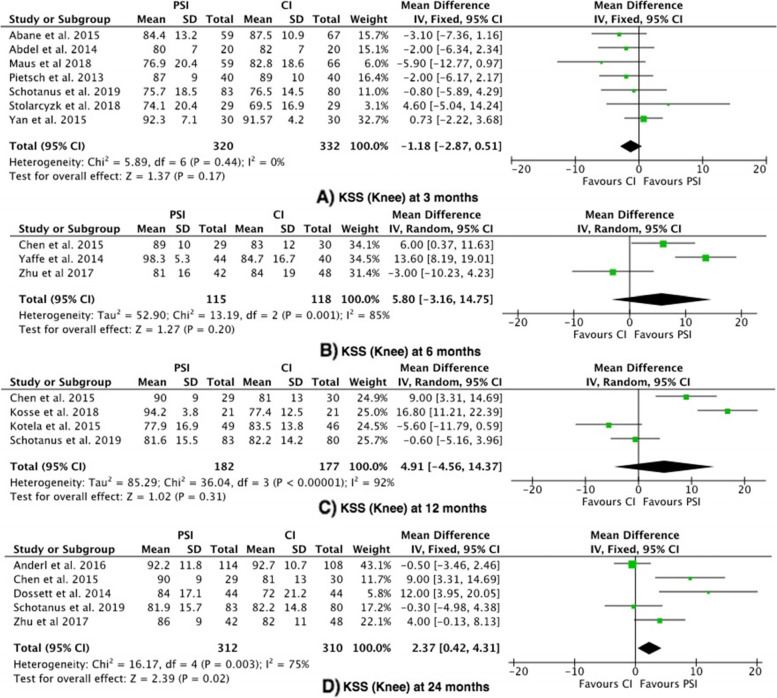
Outcome 2: Knee Society Score (KSS)—Knee
The KSS Knee score was reported in 14 studies [19–23, 25–29, 34, 35, 37, 38]. There was no significant difference observed at 3, 6 or 12 months. The KSS Knee score was significantly higher in the PSI group (favouring PSI) at 24 months in the 5 studies compared (mean difference 2.37, 95% confidence interval (CI) 0.42—4.31), with moderate heterogeneity (I2 = 75%) (Fig. 3) [19, 20, 22, 26, 38]. The mean difference (2.37) did not exceed the MCID (5.9).
Fig. 3.
Forest plots of the comparison of KSS (Knee) scores at (A) 3 Months, (B) 6 Months and (C) 12 to 24 Months. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
Four out of the 14 studies were non-randomised prospective studies, which reported MINORS criteria scores ranging from 17–20 out of 24 (Table 22). This shows a high probability of bias in these studies.
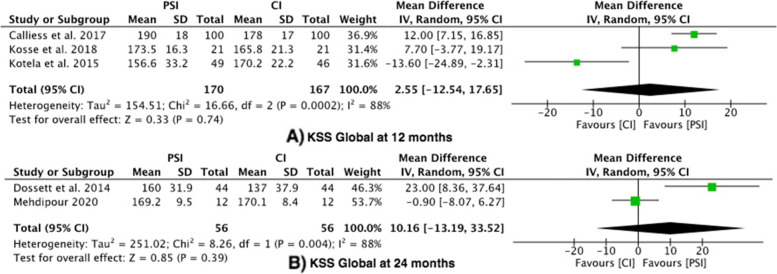
Outcome 3: Knee Society Score – Global
Five studies reported the Knee Society Score – global [26, 29, 32, 37, 39], with a high level of heterogeneity (I2 -88%). There was no difference between the PSI group and the conventional group at 12 months (mean difference 2.55, 95% confidence interval (CI) -12.54 – 17.65) or 24 months (mean difference 10.16, 95% confidence interval (CI) -13.19 – 33.52) (Fig. 4).
Fig. 4.
Forest plots of the comparison of KSS (Global) scores at (A) 12 Months and (B) 24 Months. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
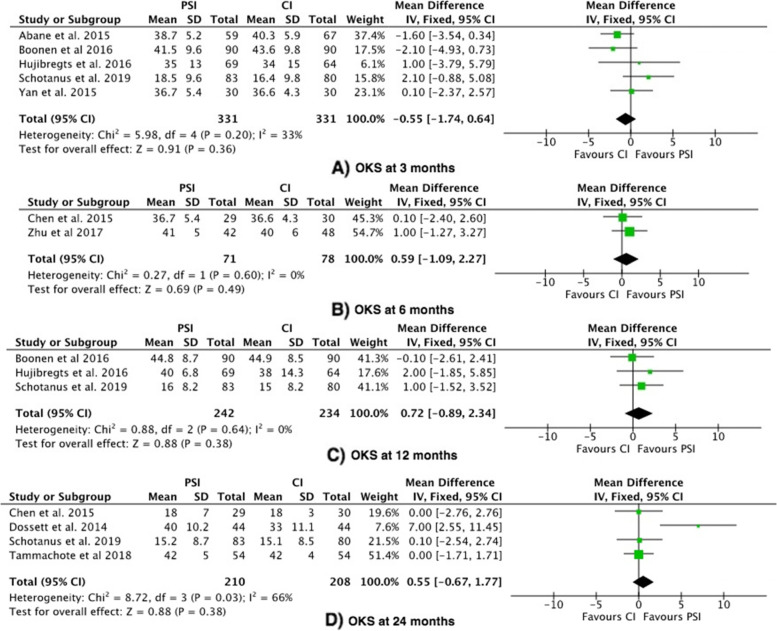
Outcome 4: Oxford Knee Score (OKS)
The Oxford Knee Score was reported in 9 studies [20, 22, 26–28, 30, 31, 36, 38]. The OKS showed no significant difference between PSI vs. CI at 3 months, 6 months or 12–24 months (Fig. 5) [5].
Fig. 5.
Forest plots of the comparison of OKS scores at (A) 3 Months, (B) 6 Months, (C) 12 Months and (D) 24 Months. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
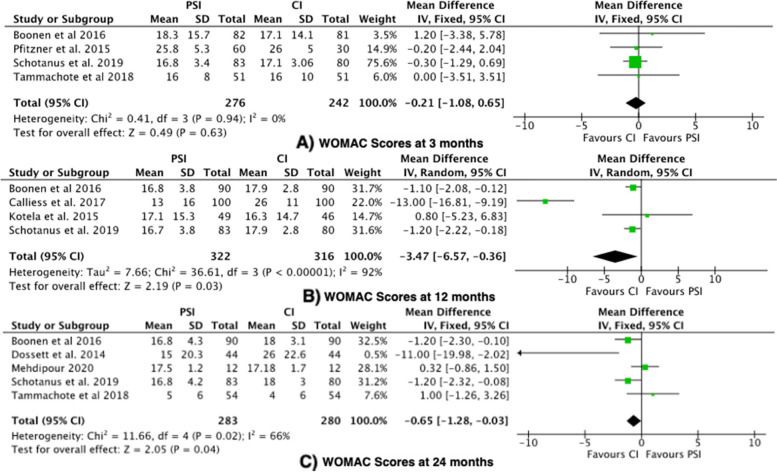
Outcome 5: Western Ontario and McMaster Universities arthritis Index (WOMAC)
The WOMAC Index was reported in 8 studies [24, 26, 29, 31, 32, 36, 38, 39]. The WOMAC score was significantly higher in the CI group (favouring PSI) at 12 months (mean difference -3.47, 95% confidence interval (CI) -6.57—-0.36), with a high level of heterogeneity (I2 = 92%). The WOMAC score was significantly higher in the CI group (favouring PSI) at 24 months (mean difference -0.65, 95% confidence interval (CI) -1.28—-0.03), with a moderate level of heterogeneity (I2 = 66%) (Fig. 6). Two RCTs showed that the CI group had significantly higher WOMAC scores, where lower scores imply improved function [26, 32]. The mean difference at 12 months and 24 months did not exceed the MCID value of 10 for WOMAC scores.
Fig. 6.
Forest plots of the comparison of WOMAC scores at (A) 3 Months, (B) 12 Months and (C) 24 Months. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
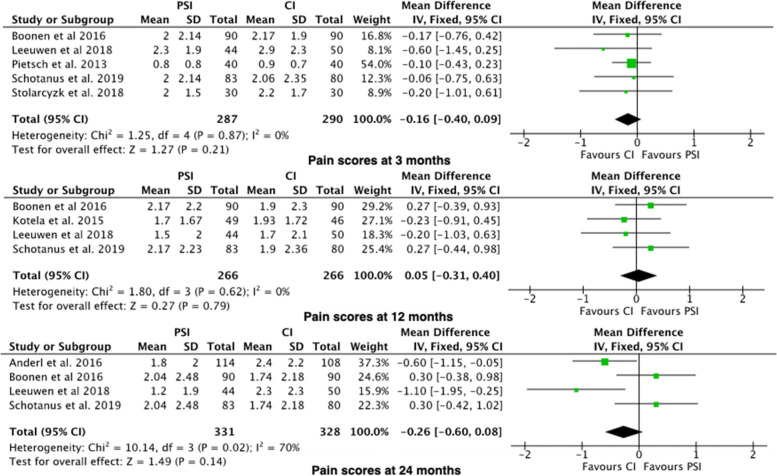
Outcome 6: Pain Score
The Pain Score was reported in 7 studies [19, 23, 29, 31, 33, 34, 38]. Pain Scores was adjusted proportionally to a 100-point scale. There was no significant difference between PSI vs. CI at 3 months, 6 months or 12–24 months (Fig. 7).
Fig. 7.
Forest plots of the comparison of pain scores at (A) 3 Months, (B) 12 Months and (C) 24 Months. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
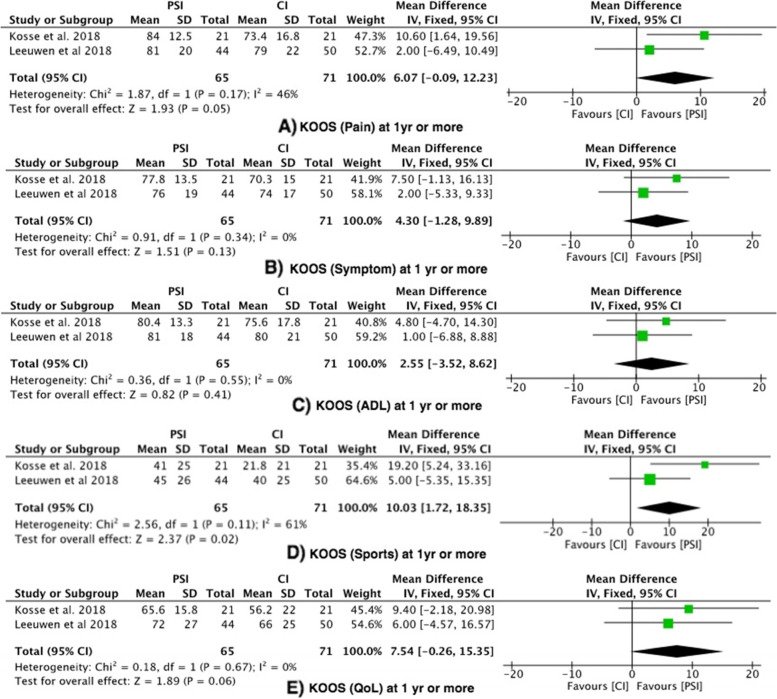
Outcome 7: KOOS
Two studies assessed KOOS pain, KOOS symptoms, KOOS ADL, KOOS Sports and KOOS QOL at 3 months and 1 year or more [25, 33] (Fig. 8).
Fig. 8.
Forest plots of the comparison of KOOS (A) Pain, (B) Symptom, (C) ADL, (D) Sports and (E) QoL. Abbreviations: CI: Confidence Interval; IV: Independent Variable; M-H: Mantel–Haenszel
KOOS pain
There was no significant difference between the PSI group and the conventional group at 3 months or at 1 year or more.
KOOS symptoms
There was no significant difference between the PSI group and the conventional group at 3 months or at 1 year or more.
KOOS ADL
There was no significant difference between the PSI group and the conventional group at 3 months or at 1 year or more.
KOOS Sports
KOOS sports reported no significant difference between the PSI group and the conventional group at 3 months. At 1 year or more, there was a statistically significant difference favouring the PSI group, with moderate heterogeneity (I2 = 61%).
KOOS QOL
There was no significant difference between the PSI group and the conventional group at 3 months or at 1 year or more.
Sensitivity analysis
We performed a sensitivity analysis for all statistically significant results.
KSS knee at 24 months favours PSI. No significant difference between the groups was noted when Chen et al. [20], Dossett et al. [26] and Zhu et al. [22] studies are individually removed. KSS Function at 24 months was found to be statistically significant regardless of individual studies being removed.
WOMAC scores were demonstrated at 12 months and 24 months to favour PSI. When Boonen et al. [31], Dossett et al. . [26] and Schotanus et al. [38] were removed individually, the results were noted to be statistically insignificant. The studies were reviewed individually and deemed suitable for inclusion in the analysis.
Discussion
This systematic review and meta-analysis included 22 studies (18 RCT’s and 4 prospective studies) to evaluate the functional benefit of TKA using PSI compared to conventional TKA for patients with end stage knee OA. Functional outcomes were assessed at 3 months, 6 months, 12 months and 24 months where published. Only Level 1 and Level 2 evidence were considered for this systematic review to ensure a robust review of the literature.
The primary outcome looked at KSS function scores, which showed PSI was favoured statistically compared to CI at 24 months (mean difference 4.36, 95% confidence interval 1.83–6.89), with no exceedance of the MCID (6.4). Therefore, there was no clinical difference found between PSI and CI. Notably, 3 prospective studies were included in the PSI group at 24 months, which provides an element of bias [19, 20, 22].
For KSS knee scores at 3 months, 6 months and 12 months, there was no statistically significant difference between PSI and CI groups. At 24 months, there was a statistical difference between PSI and CI groups in the 5 studies compared [19, 20, 22, 26, 38], which did not exceed the MCID for KSS knee score. It is noted that 3 out of the 5 studies (n = 371) [19, 20, 22] were prospective comparative studies. This results in considerable bias, which is demonstrated by a minors criteria score of 17–20 (Table 2). WOMAC scores were demonstrated to have a statistical difference at 12 months (mean difference -3.47, 95% confidence interval (CI) -6.57—-0.36) and 24 months favouring PSI (mean difference -0.65, 95% confidence interval (CI) -1.28—-0.03), with no exceedance of the MCID value of 10 for WOMAC scores. Two RCTs showed that the CI group had significantly higher WOMAC scores, where lower scores imply improved function [26, 32]. Both RCT’s were randomised adequately, however, allocation concealment and blinding of participants was not performed by Calliess et al. 2017 [32]. This demonstrates substantial bias in the findings found for 12 month WOMAC scores.
Interestingly, KSS global scores demonstrated no statistically significant results at 12 and 24 months. This is similarly shown in the OKS scores at 3,6,12 and 24 months.
A recent meta-analysis by Mannan et al. including literature from 2000 to 2015 revealed eight randomised controlled trials (RCT’s); data were collated to produce a meta-analysis looking at PSI versus CI for functional outcomes [13] at specific time points. Since 2015, many high quality studies of level I and level II evidence articles have been published with more varied outcome measures over more substantial periods [12, 18, 22, 32–39]. A recent meta-analysis by Kizaki et al. [14] conducted pooled analysis of PROMs for PSI vs conventional TKA, which showed PSI did not improve PROM more than TKA. Of note, KSS knee, KSS function, OKS and WOMAC scores were shown to have no statistical difference at less than 1 year or greater than 1 year [14]. These findings corroborate with previous meta-analyses regarding no difference in PROMS irrespective of PSI or conventional TKA. However, the pooled analysis at any time point less than a year and more than a year may result in nuances in the functionality of patients being missed. Our study delineates the time points of post operative PROM to show that there is no clinical difference at definitive time points on the functional outcome.
Limitations
Although this study demonstrates that there is no clinical difference between PSI and CI in regards to KSS function scores, there are limitations to this paper. The functional outcomes obtained from the studies were from RCTs with limited cohort sizes and qualitative studies. There was a risk of bias in the studies included in this meta-analysis, largely due to inadequacies in the blinding of participants and operating surgeons. The observed heterogeneity is likely due to a wide-range of presenting patient groups and deformities. It may also be attributable to data that is collected from a vast array of surgical centres, operating surgeons of variable experience levels and differing instrument manufacturers. It is appreciated that this paper only looks at functional outcomes in regards to PROMs for comparing PSI to CI. Therefore, this study should provide an impetus for further study on time specific comparisons for PROMs in PSI and CI for TKA.
Recent advances in both navigation and robotic-assisted surgical procedures may also provide a useful tool to assist the surgeon with accuracy of component implantation in TKR. Surgical robotics has been slow to gain acceptance by the majority of practicing surgeons but may hold advantages over conventional knee arthroplasty, or even patient specific instrumentation. Similar RCTs and meta-analysis in this field may ultimately provide these answers.
Conclusion
The results of this meta-analysis show that when comparing PSI and CI in terms of functional outcomes, the current literature is inadequate to demonstrate superiority of one technique over the other. It is important to appreciate that these findings are limited by the significant level of bias that was observed in the studies reviewed. We appreciate the limitations of the included data, and that PSI may confer benefits in other outcomes not included in this study, including longevity. The literature requires larger, more robust RCT’s on this subject in order to achieve substantial conclusions. In order to establish whether a true functional advantage exists with one instrumentation technique, long-term data is essential.
Acknowledgements
To the best of our knowledge, no conflict of interest, financial or other.
Abbreviations
- OA
Osteoarthritis
- TKA
Total Knee Arthroplasty
- UK
United Kingdom
- USA
United States America
- CI
Conventional Instrumentation
- PSI
Patient specific instrumentation
- CT
Computer Tomography
- 3D
3 Dimensional
- RCT
Randomised controlled trial
- KSS
Knee Society Score
- OKS
Oxford Knee Score
- WOMAC
Western Ontario and McMaster Universities arthritis index
- WHO
World Health Organisation
- MINORS
Methodological Index for non-randomised studies
- PROM
Patient related outcome measure
- MRI
Magnetic resonance imaging
Authors’ contributions
All authors listed have contributed sufficiently to be included, and all those who are qualified to be authors are listed. All authors have contributed equally to this paper. HM has carried out the majority of statistical analysis. BR has undertaken the literature search, data collection and statistical analysis, which has been assisted by NP. AW and SB were involved in the write-up and editing process. All authors have read and approved the final submitted manuscript.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors whose names are listed immediately below certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Branavan Rudran, Email: b.rudran@imperial.ac.uk.
Henry Magill, Email: henry.magill@nhs.net.
Nikhil Ponugoti, Email: nikhil.ponugoti@nhs.net.
Andy Williams, Email: Andy.williams@fortiusclinic.com.
Simon Ball, Email: Simon.Ball@fortiusclinic.com.
References
- 1.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001;388:10–17. doi: 10.1097/00003086-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Sofat N, Ejindu V, Kiely P. What makes osteoarthritis painful? The evidence for local and central pain processing. Rheumatology (Oxford) 2011;50(12):2157–2165. doi: 10.1093/rheumatology/ker283. [DOI] [PubMed] [Google Scholar]
- 4.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2012;379(9823):1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 5.Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ, 3rd, Kurland RL, et al. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85(10):898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/00004623-200704000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Van Manen MD, Nace J, Mont MA. Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners. J Am Osteopath Assoc. 2012;112(11):709–715. [PubMed] [Google Scholar]
- 8.Sassoon A, Nam D, Nunley R, Barrack R. Systematic review of patient-specific instrumentation in total knee arthroplasty: new but not improved. Clin Orthop Relat Res. 2015;473(1):151–158. doi: 10.1007/s11999-014-3804-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonner TJ, Eardley WG, Patterson P, Gregg PJ. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surgery Br. 2011;93(9):1217–1222. doi: 10.1302/0301-620X.93B9.26573. [DOI] [PubMed] [Google Scholar]
- 10.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 11.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Rel Res. 1994(299):153–6. https://pubmed.ncbi.nlm.nih.gov/8119010/. [PubMed]
- 12.Giannotti S, Sacchetti F, Citarelli C, Bottai V, Bianchi N, Agostini G, et al. Single-use, patient-specific instrumentation technology in knee arthroplasty: a comparative study between standard instrumentation and PSI efficiency system. Musculoskelet Surg. 2019;104(2):195–200. [DOI] [PubMed]
- 13.Mannan A, Akinyooye D, Hossain F. A Meta-analysis of Functional Outcomes in Patient-Specific Instrumented Knee Arthroplasty. J Knee Surg. 2017;30(7):668–674. doi: 10.1055/s-0036-1593869. [DOI] [PubMed] [Google Scholar]
- 14.Kizaki K, Shanmugaraj A, Yamashita F, Simunovic N, Duong A, Khanna V, et al. Total knee arthroplasty using patient-specific instrumentation for osteoarthritis of the knee: a meta-analysis. BMC Musculoskelet Disord. 2019;20(1):561. doi: 10.1186/s12891-019-2940-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maredupaka S, Meshram P, Chatte M, Kim WH, Kim TK. Minimal clinically important difference of commonly used patient-reported outcome measures in total knee arthroplasty: review of terminologies, methods and proposed values. Knee Surg Relat Res. 2020;32(1):19. doi: 10.1186/s43019-020-00038-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 18.Moorthy V, Chen JY, Liow MHL, Chin PL, Chia SL, Lo NN, et al. Mid-term functional outcomes of patient-specific versus conventional instrumentation total knee arthroplasty: a prospective study. Arch Orthop Trauma Surg. 2021;141(4):669–674. doi: 10.1007/s00402-020-03729-4. [DOI] [PubMed] [Google Scholar]
- 19.Anderl W, Pauzenberger L, Kolblinger R, Kiesselbach G, Brandl G, Laky B, et al. Patient-specific instrumentation improved mechanical alignment, while early clinical outcome was comparable to conventional instrumentation in TKA. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):102–111. doi: 10.1007/s00167-014-3345-2. [DOI] [PubMed] [Google Scholar]
- 20.Chen JY, Chin PL, Tay DK, Chia SL, Lo NN, Yeo SJ. Functional Outcome and Quality of Life after Patient-Specific Instrumentation in Total Knee Arthroplasty. J Arthroplasty. 2015;30(10):1724–1728. doi: 10.1016/j.arth.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Yaffe M, Luo M, Goyal N, Chan P, Patel A, Cayo M, et al. Clinical, functional, and radiographic outcomes following total knee arthroplasty with patient-specific instrumentation, computer-assisted surgery, and manual instrumentation: a short-term follow-up study. Int J Comput Assist Radiol Surg. 2014;9(5):837–844. doi: 10.1007/s11548-013-0968-6. [DOI] [PubMed] [Google Scholar]
- 22.Zhu M, Chen JY, Chong HC, Yew AKS, Foo LSS, Chia SL, et al. Outcomes following total knee arthroplasty with CT-based patient-specific instrumentation. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2567–2572. doi: 10.1007/s00167-015-3803-5. [DOI] [PubMed] [Google Scholar]
- 23.Pietsch M, Djahani O, Zweiger C, Plattner F, Radl R, Tschauner C, et al. Custom-fit minimally invasive total knee arthroplasty: effect on blood loss and early clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2234–2240. doi: 10.1007/s00167-012-2284-z. [DOI] [PubMed] [Google Scholar]
- 24.Pfitzner T, Abdel MP, von Roth P, Perka C, Hommel H. Small improvements in mechanical axis alignment achieved with MRI versus CT-based patient-specific instruments in TKA: a randomized clinical trial. Clin Orthop Relat Res. 2014;472(10):2913–2922. doi: 10.1007/s11999-014-3784-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdel MP, Parratte S, Blanc G, Ollivier M, Pomero V, Viehweger E, et al. No benefit of patient-specific instrumentation in TKA on functional and gait outcomes: a randomized clinical trial. Clin Orthop Relat Res. 2014;472(8):2468–2476. doi: 10.1007/s11999-014-3544-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J. 2014;96-b(7):907–13. doi: 10.1302/0301-620X.96B7.32812. [DOI] [PubMed] [Google Scholar]
- 27.Abane L, Anract P, Boisgard S, Descamps S, Courpied JP, Hamadouche M. A comparison of patient-specific and conventional instrumentation for total knee arthroplasty: a multicentre randomised controlled trial. Bone Joint J. 2015;97-b(1):56–63. doi: 10.1302/0301-620X.97B1.34440. [DOI] [PubMed] [Google Scholar]
- 28.Yan CH, Chiu KY, Ng FY, Chan PK, Fang CX. Comparison between patient-specific instruments and conventional instruments and computer navigation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3637–3645. doi: 10.1007/s00167-014-3264-2. [DOI] [PubMed] [Google Scholar]
- 29.Kotela A, Lorkowski J, Kucharzewski M, Wilk-Franczuk M, Sliwinski Z, Franczuk B, et al. Patient-Specific CT-Based Instrumentation versus Conventional Instrumentation in Total Knee Arthroplasty: A Prospective Randomized Controlled Study on Clinical Outcomes and In-Hospital Data. Biomed Res Int. 2015;2015:165908. doi: 10.1155/2015/165908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huijbregts HJ, Khan RJ, Fick DP, Hall MJ, Punwar SA, Sorensen E, et al. Component alignment and clinical outcome following total knee arthroplasty: a randomised controlled trial comparing an intramedullary alignment system with patient-specific instrumentation. Bone Joint J. 2016;98-b(8):1043–9. doi: 10.1302/0301-620X.98B8.37240. [DOI] [PubMed] [Google Scholar]
- 31.Boonen B, Schotanus MG, Kerens B, van der Weegen W, Hoekstra HJ, Kort NP. No difference in clinical outcome between patient-matched positioning guides and conventional instrumented total knee arthroplasty two years post-operatively: a multicentre, double-blind, randomised controlled trial. Bone Joint J. 2016;98-b(7):939–44. doi: 10.1302/0301-620X.98B7.37274. [DOI] [PubMed] [Google Scholar]
- 32.Calliess T, Bauer K, Stukenborg-Colsman C, Windhagen H, Budde S, Ettinger M. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1743–1748. doi: 10.1007/s00167-016-4136-8. [DOI] [PubMed] [Google Scholar]
- 33.Van Leeuwen J, Snorrason F, Röhrl SM. No radiological and clinical advantages with patient-specific positioning guides in total knee replacement. Acta Orthop. 2018;89(1):89–94. doi: 10.1080/17453674.2017.1393732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stolarczyk A, Nagraba L, Mitek T, Stolarczyk M, Deszczyński JM, Jakucinski M. Does Patient-Specific Instrumentation Improve Femoral and Tibial Component Alignment in Total Knee Arthroplasty? A Prospective Randomized Study. Adv Exp Med Biol. 2018;1096:11–17. doi: 10.1007/5584_2018_193. [DOI] [PubMed] [Google Scholar]
- 35.Maus U, Marques CJ, Scheunemann D, Lampe F, Lazovic D, Hommel H, et al. No improvement in reducing outliers in coronal axis alignment with patient-specific instrumentation. Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2788–2796. doi: 10.1007/s00167-017-4741-1. [DOI] [PubMed] [Google Scholar]
- 36.Tammachote N, Panichkul P, Kanitnate S. Comparison of customized cutting block and conventional cutting instrument in total knee arthroplasty: a randomized controlled trial. J Arthroplasty. 2018;33(3):746–51.e3. doi: 10.1016/j.arth.2017.09.055. [DOI] [PubMed] [Google Scholar]
- 37.Kosse NM, Heesterbeek PJC, Schimmel JJP, van Hellemondt GG, Wymenga AB, Defoort KC. Stability and alignment do not improve by using patient-specific instrumentation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1792–1799. doi: 10.1007/s00167-017-4792-3. [DOI] [PubMed] [Google Scholar]
- 38.Schotanus MGM, Boonen B, van der Weegen W, Hoekstra H, van Drumpt R, Borghans R, et al. No difference in mid-term survival and clinical outcome between patient-specific and conventional instrumented total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1463–1468. doi: 10.1007/s00167-018-4968-5. [DOI] [PubMed] [Google Scholar]
- 39.Mehdipour S, Qoreishi M, Keipourfard A. Comparison of Clinical, Functional, and Radiological Outcomes of Total Knee Arthroplasty Using Conventional and Patient-Specific Instrumentation. Arch Bone Jt Surg. 2020;8(5):625–632. doi: 10.22038/abjs.2020.41571.2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.