Abstract
Background
Academic institutions building capacity for implementation scholarship are also well positioned to build capacity in real world health and human service settings. How practitioners and policy makers are included and trained in implementation capacity-building initiatives, and their impact on building implementation practice capacity is unclear. This scoping review identified and examined features of interventions that build implementation practice capacity across researchers and practitioners or practitioners-in-training.
Methods
Five bibliographic databases were searched. Eligible studies (a) described an implementation capacity building intervention with a connection to an academic institution, (b) targeted researchers and practitioners (including practitioners-in-training, students, or educators), and (c) reported intervention or participant outcomes. Articles that only described capacity building interventions without reporting outcomes were excluded. Consistent with Arksey and O’Malley’s framework, key study characteristics were extracted (target participants, core components, and outcomes) and analyzed using open coding and numerical analysis.
Results
Of 1349 studies identified, 64 met eligibility for full-text review, and 14 were included in the final analysis. Half of the studies described implementation capacity building interventions that targeted health or behavioral health researchers, practitioners, and practitioners-in-training together, and half targeted practitioners or practitioners-in-training only. The most common components included structured didactic activities offered in person or online, mentorship and expert consultation to support implementation, and practical application activities (e.g., field placements, case studies). Knowledge sharing activities and technical assistance were less common. All studies reported favorable outcomes related to knowledge attainment, increased ability to implement evidence, productivity, and satisfaction.
Conclusions
Building implementation capacity among practitioners is critical for integrating insights from implementation science into the field and preventing the “secondary” implementation research-to-practice gap. This scoping review identified several promising implementation practice capacity building interventions that tend to build practitioner capacity via expert led activities which may be relevant for academic institutions seeking to build implementation practice capacity. To avoid widening the implementation research-to-practice gap, implementation capacity building interventions are needed that target policy makers, expand beyond multiple practice settings, and leverage university/community partnerships or on-site academic medical centers. Future studies will also be needed to test the impact on service quality and public health outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13012-022-01216-5.
Keywords: Implementation capacity building interventions, Implementation practice, Academic institutions
Contributions to the literature.
Implementation practice capacity building interventions are needed for integrating insights from implementation science into practice; however, they have received less attention than initiatives focused on building implementation research capacity.
This scoping review identified 14 implementation capacity building interventions that included practitioners or trainees. Results demonstrated how interventions have targeted a range of stakeholders including practice leaders and students, often using traditional didactic or mentored training approaches with a goal of improving implementation knowledge, application, confidence, and productivity.
Implementation capacity building interventions that target policy makers and multiple practice settings are also needed.
Introduction
The exponential and continued growth of the field of implementation science underscores its relevance, importance, and scientific value in bridging the research to practice gap. The adoption of research evidence into routine practice remains complex and influenced by a number of organizational, system, and individual factors [1]. Advances in implementation science have identified and validated strategies using a consistent nomenclature to facilitate the implementation process [2, 3]. Similarly, development of specific theories, models, and frameworks that draw on multiple disciplinary traditions provide a systematic approach to implementation and stimulate interdisciplinary teams of researchers and practitioners that can break down silo-based work to promote and sustain implementation efforts [4, 5]. This team-based approach to implementation requires that practitioners and researchers share resources and a commitment to an evidence-based approach to implementation. Prior reviews of implementation capacity building interventions describe academic training opportunities in implementation and acknowledge a need for greater engagement and attention to implementation practitioners and policy makers [6, 7]. Indeed, building implementation capacity among professionals who are tasked with implementing evidence in routine practice and policy settings is critical for carrying out implementation studies and scaling the benefits of evidence-based interventions. As such, greater understanding is needed for how academic institutions might design or refine their efforts to build capacity among researchers and practitioners—the frontline professionals who are tasked with implementing evidence in routine care.
Across both academic and practice settings, the process of capacity building is ladened with unique challenges. First, implementation science is a rapidly evolving field, making it difficult for capacity building initiatives to reflect the field’s most current discoveries and advancements [8, 9]. Second, the demand for capacity building interventions, including implementation-focused trainings, didactic activities, and workshops, exceeds the availability [10]. Third, well-established capacity building interventions have primarily targeted the implementation research community, resulting a major knowledge gap for how best to build implementation capacity among the practitioners (e.g., nurses, social workers, physicians, therapists, pharmacists) who are responsible for applying evidence in daily practice. Programs such as the Training Institute for Dissemination and Implementation Research in Health [11, 12], the Implementation Research Institute [13], and the Mentored Training for Dissemination and Implementation Research in Cancer [14] are historically comprised of researchers with activities geared towards grantsmanship and mentorship from expert academicians.
Implementation researchers are interested in generating knowledge regarding the processes, strategies and methods that promote uptake of evidence-based interventions by clinicians, organizations, systems, and patients. Implementation practitioners are users of implementation science to accelerate the adoption and application of evidence-based interventions. Importantly, implementation researchers and practitioners are not always mutually exclusive groups, as many actively engage in both generation and integration of the science. Even when capacity building interventions are designed for a multi-stakeholder audience, it remains difficult to tailor such interventions to the unique needs of all attendees given their heterogeneities in implementation experiences, trajectories, and professional backgrounds [12]. These challenges do not represent an exhaustive list but rather depict the complexities of developing, deploying, and sustaining effective capacity building interventions for implementation stakeholders. It is critically important to engage multiple stakeholders at the practice level to prevent development of a “secondary gap,” where the knowledge from implementation science is not applied among front-line teams seeking to implement evidence-based practices in real-world settings [15, 16].
In an effort to advance implementation capacity, implementation leaders have recently encouraged the development of interventions that build capacity across a diverse group of individual learners and multidisciplinary teams [7, 17]. In particular, Davis and D’Lima’s [7] recent systematic review on implementation research capacity building interventions underscored the critical need to include practitioners, pre-doctoral trainees, and policymakers, especially those in low resource settings with limited access to financial supports and personnel. Indeed, building implementation capacity among researchers without also building capacity among those on the ground who are responsible for implementing new practices potentially widens the divide between implementation research and implementation practice [15, 18]—an ironic gap with potential to restrict the extent to which implementation theories, models, frameworks, and strategies are used in both clinical and community contexts [16]. While the demand for research-based implementation capacity building interventions will continue to grow in academic settings, these interventions should be deliberately designed to also build practice capacity. Doing so will foster collaborations among researchers, practitioners, and trainees, leading to productive partnerships and the development of multidisciplinary implementation networks that span research and practice settings.
Though the concept of building capacity in a multi-contextual manner may garner favorable attention from both researchers and practitioners, little is known about effective interventions that can build implementation practice capacities across these groups of stakeholders simultaneously. Accordingly, the present scoping review aimed to examine interventions and programs designed to build implementation practice capacity in the following formats: (a) collectively among researchers, practitioners, and/or students; (b) among practitioners, and (c) among practitioners-in-training (e.g., graduate students). Identifying these interventions, as well as their core components and outcomes, is a crucial precursor to deploying interventions that effectively build the implementation practice capacity of diverse groups of learners. Addressing practice capacity narrows the gap between implementation science and implementation practice by efficiently moving evidence-based interventions into practice to improve healthcare safety and quality.
Methods
Our scoping review protocol (available upon request) was established a priori and aligned with Arskey and O’Malley’s [19] five-stage framework for review methodology. A scoping review approach was selected given the nascent nature of capacity building interventions in implementation science and, unlike systematic reviews, the scoping review methodology allowed the review team to assess the breadth and depth of the capacity building literature through an iterative search process [20]. The review was conducted by a team with expertise in implementation science, implementation practice, and scoping review methodology. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis, Scoping Review Extension (PRISMA-ScR) was used for organization and presentation of key findings (Additional file 1) [21].
Stage 1: Identifying the research question
Our team of implementation researchers, consisting of researchers and practitioners in the fields of rehabilitation, social work, and nursing, collaborated to develop the current review’s research question: What interventions (e.g., courses, mentorship, workshops) have been used to build implementation capacity among researchers, practitioners, and/or students? Our secondary focus was to assess the types of outcomes measured to determine capacity building intervention effectiveness.
Stage 2: Identifying relevant studies
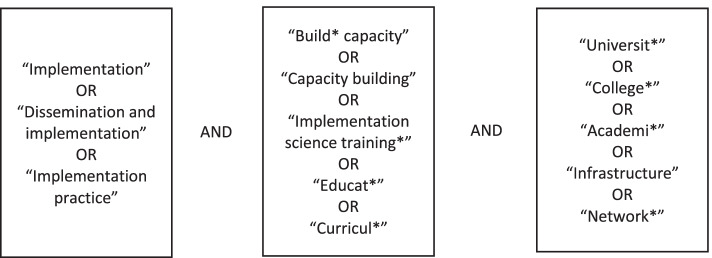
To identify relevant studies, five electronic bibliographic databases were accessed using a librarian assisted search strategy (Academic Search Complete, CINAHL, MEDLINE, PsycINFO, and SocINDEX). We entered search terms that represented dissemination and implementation, capacity building, and academic institutions given that many capacity building interventions have been developed using academic resources. For instance, the following string of search terms was used to search our five databases simultaneously: [“implementation”] AND [“build* capacity”] AND [“university” OR “college” OR “higher education”]. Our full list of search terms can be found in Fig. 1. All eligible studies that were identified through our search strategy were uploaded into the web-based scoping and systematic review program, Covidence [22], prior to initiating stage 3.
Fig. 1.
Search terms for identifying relevant studies
Stage 3: Study selection
Study selection consisted of a two-step process. In step 1, two members of the review team with experience in scoping review methodology and implementation research (LAJ and MLR) screened all eligible titles and abstracts. Team members applied the inclusion and exclusion criteria listed below.
Inclusion criteria:
- Studies that examined capacity building interventions across researchers, practitioners, and practitioners-in-training:
- Examples of interventions included didactic courses, workshops/trainings, mentoring and expert consultation, practical application activities, knowledge sharing activities, and project support
- Studies were included if they examined interventions designed to build implementation capacity collectively across researchers, practitioners, and/or practitioners-in-training (e.g., graduate students of professional programs such as nursing, social work, and other allied health fields)
- Studies were included if they examined interventions designed to build implementation capacity among practitioners
- Studies were included if they examined interventions designed to build implementation capacity among practitioners-in-training
- Studies that had relevance to academic institutions
- Studies that met this criterion had one or more connections to an academic institution, faculty member(s), or academic medical center
Exclusion criteria:
Studies that presented only theories, models, or frameworks for building implementation science capacity
Studies that examined interventions designed to build implementation capacity among researchers only or researchers-in-training (e.g., research doctorate students)
Studies that examined the implementation of a health-related practice, program, intervention, or innovation (e.g., smoking cessation program; cognitive behavioral therapy)
Studies that only described capacity building interventions without reporting participant outcomes
Review studies (e.g., systematic, scoping, rapid, narrative)
Grey literature (e.g., government reports, dissertation/theses, conference proceedings, books)
In step 2 of our study selection process, these inclusion/exclusion criteria were applied to full-text articles by the same two review team members. Members discussed discrepancies on study inclusion until consensus was reached before proceeding to data extraction.
Stage 4: Charting the data
Characteristics from each included study were extracted by the review team using an adapted data charting tool originally proposed by Arksey and O’Malley [19]. We chose to extract the following characteristics from each study given the relevance to our primary and secondary research questions: author and year, study location, target(s) of the capacity building intervention, core intervention components (described in detail in stage 5), intervention objective(s), and main outcomes. Reviewers met on a biweekly basis over the course of 2 months to reconcile discrepancies in data extraction.
Stage 5: Collating, summarizing, and reporting the results
All included studies underwent numerical and open coding analyses. Numerical analysis was used to describe the types of studies included, the target audiences of capacity building interventions, and the number of core components integrated into each intervention. Two reviewers assessed the capacity building interventions described in each included study and used open coding to identify core intervention components. The reviewers drew language from Davis and D’Lima’s capacity building systematic review [7] as well as the Expert Recommendations for Implementing Change (ERIC) taxonomy [2] in order to differentiate intervention components. Table 1 lists the main core components extracted from each capacity building intervention and provides component descriptions. Reviewers repeated this open coding process to achieve uniform terminology for the types of outcomes measured to determine capacity building intervention effectiveness (Table 2).
Table 1.
Description of core intervention components
| Core intervention component | Description |
|---|---|
| Didactic activities | In-person or online coursework consisting of lectures, case studies; readings, and/or self-paced modules (e.g., slide-deck presentations) |
| Mentorship and expert consultation | Continued support that is initiated at the start of an implementation project and continued throughout project development and/or deployment; one-on-one or group meetings with leaders and faculty in implementation science and/or practice |
| Practical application activities | Small projects or field placements dedicated to implementing an evidence-based innovation under real-world circumstances |
| Knowledge sharing activities | Group meetings (online or in-person) that encourage networking, reflection, and the discussion of implementation experiences and reflections from implementation projects |
| Technical assistance | Email, phone, or website support for how to deliver an evidence-based innovation or an implementation strategy; specific reference to “technical assistance” or “technical coaching” |
Table 2.
Description of capacity building intervention outcomes
| Outcome | Description |
|---|---|
| Knowledge attainment | Understanding and awareness of implementation models, factors and strategies influencing evidence-based practice implementation; evidence-based practice use |
| Increased ability to implement evidence | Perceived confidence, competence, or self-efficacy in initiating, leading, and/or participating in activities that facilitate evidence implementation |
| Productivity | Formation of implementation project teams; submitted grant proposals or manuscripts with an implementation focus; number of participants |
| Satisfaction | Perceived acceptability, appropriateness, or approval of capacity building intervention structure and content |
Results
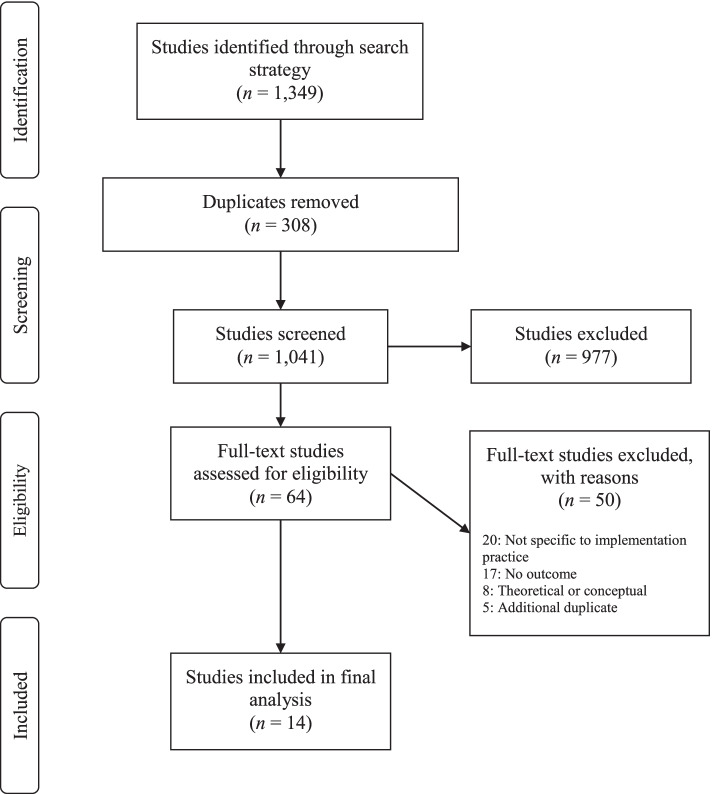
Our initial search strategy yielded 1349 studies that were entered into Covidence for screening. After title/abstract and full-text screening, a total of 14 studies were included in our final analysis (Fig. 2). Reviewers achieved a Cohen’s kappa of 0.49 during the review process, indicating a moderate level of agreement. Common reasons studies were excluded were lack of intervention outcome measurement, description of an intervention not unique to implementation practice capacity, and failure to clearly describe a specific capacity building intervention. The majority of included studies were descriptive in nature and none used experimental or quasi-experimental designs to evaluate the efficacy of the capacity building interventions.
Fig. 2.
PRISMA flow diagram of study selection process
Targets of capacity building interventions
Researchers, practitioners, and practitioners-in-training (e.g., professional program graduate students) were all targets of implementation practice capacity building interventions. A total of eight interventions collectively targeted researchers, practitioners, and practitioners-in-training simultaneously [23–30], three interventions targeted practitioners only [31–33], and the remaining three targeted practitioners-in-training who represented the fields of social work [34], public health [35], and nursing [36].
Researchers, practitioners, and practitioners-in-training interventions
Studies that targeted researchers, practitioners, and practitioners-in-training were conducted in the USA [25–27], Canada [28, 30], South Africa [29], and Sweden [23], and jointly across the USA, Mexico, and India [24]. Each intervention consisted of a combination of core components with the most common interventions including didactic activities, mentorship and expert consultations, knowledge sharing activities, and practical application activities. As an example, from the University of Kentucky, the Value of Innovation to Implementation Program (VI2P) sought to build implementation capacity across its health system and six health professional colleges [25]. The VI2P was also designed to foster a local learning collaborative to facilitate implementation knowledge sharing, similar to the local implementation learning communities developed by the Colorado Research in Implementation Science Program (CRISP [26]) (Table 3).
Table 3.
Characteristics of capacity building interventions for a combination of researchers, practitioners, and/or practitioners-in-training
| Country | Participants | Core components | Training objectives | Measurement | Outcomes | |
|---|---|---|---|---|---|---|
| Carlfjord et al., 2017 [23] | Sweden | Researchers, allied health professionals | Didactic activities, knowledge sharing | To build understanding of implementation theory and practice in healthcare | Post-test survey | ↑ knowledge; high satisfaction with program |
| Galaviz et al., 2016 [24] | USA, Mexico, and India | Mid-career professionals, researchers, and public health workers | Didactic activities, mentorship and expert consultation, practical activities | To build implementation capacity in LMICs | Pre-post survey at baseline and completion; total projects developed | ↑ confidence in implementation research and leadership; development of 53 collaborative implementation projects |
| Li et al., 2019 [25] | USA | Researchers, practitioners, QI experts, community stakeholders | Mentorship and expert consultation, practical application activities, knowledge sharing activities | To foster a learning collaborative related to D&I capacity | Total implementation teams formed | Formation of 26 teams collaborating on implementation projects |
| Morrato et al., 2015 [26] | USA | Researchers, healthcare professionals/public health workers, graduate students | Didactic activities, mentorship and expert consultation, knowledge sharing activities | To adapt national D&I training programs and foster a local learning community | Pre-post survey at baseline, 1-week post, and 6-months post | ↑ knowledge of D&I; ↑ development of D&I grants, papers, and projects |
| Norton 2014 [27] | USA | Researchers and public health students | Didactic activities, mentorship and expert consultation | To teach public health students and academic researchers about D&I | Post-test survey | ↑ knowledge and confidence with D&I; high satisfaction with collaborative learning approach |
| Park et al., 2018 [28] | Canada | Healthcare professionals, researchers, managers | Didactic activities, mentorship and expert consultation, practical application | To build capacity for KT practice | Pre-post survey at baseline, 6-, 12-, 18-, and 24-months; interviews and focus groups |
↑ self-efficacy, confidence, and knowledge in KT principles ↑ implementation of KT principles in practice |
| Ramaswamy et al., 2020 [29] | South Africa | Public health students and public health workers | Didactic activities, mentorship and expert consultation, practical application activities, knowledge sharing activities | To build implementation capacity in South Africa | Post-test survey; interviews | Reports of high satisfaction among participants |
| Straus et al., 2011 [30] | Canada | Researchers, healthcare professionals, graduate students | Didactic activities, mentorship and expert consultation, practical application activities, knowledge sharing activities | To build capacity in science and practice of KT | # of attendees | No data yet other than # of summer institute attendees (n = 90) |
LMICs low- and middle-income countries, QI quality improvement
Practitioners
Three capacity building interventions targeted practitioners comprised of healthcare providers [31], clinical leaders and managers in behavioral health settings [32], and individuals in community-based service delivery [33] and were conducted in Canada [31] and the USA [32, 33]. All of these practitioner-only interventions incorporated didactic activities as a core intervention component with other common components including knowledge sharing activities and practical application exercises. For instance, intervention developers of the Training in Implementation Practice Leadership (TRIPLE) led activities to build implementation capacity among clinicians or administrators in behavioral health practice settings using the term “practice leader” to describe intervention targets. Core components of the TRIPLE intervention included the facilitation of knowledge sharing activities, didactic activities, consultations with implementation experts, practical application activities, and the provision of technical assistance [32] (Table 4).
Table 4.
Characteristics of capacity building interventions for practitioners only
| Country | Participants | Core components | Training objectives | Measurement | Outcomes | |
|---|---|---|---|---|---|---|
| Moore et al., 2018 [31] | Canada | Healthcare professionals | Didactic activities, mentorship and expert consultation, knowledge sharing activities | To provide training on the use of evidence and application of IS in healthcare | Pre-post survey at baseline, 3-, 6-, and 12-months; interviews | ↑ knowledge and self-efficacy in implementation; high satisfaction |
| Proctor et al., 2019 [32] | USA | Clinical leaders and managers | Didactic activities, Knowledge sharing activities, mentorship and expert consultation, practical application activities, technical assistance | To promote leadership and organizational change and promote EBP implementation | Pre-post survey at baseline and completion |
↑ competence High levels of program acceptability and appropriateness |
| Ramanadhan et al., 2017 [33] | USA | Community-based practitioners | Didactic activities, knowledge sharing activities, technical assistance | To promote EBP use in community-based organizations | Post-test survey and social network survey | ↑ use of evidence in practice; reports of information sharing across CBO networks |
CBO community-based organization
Practitioners-in-training
A total of three interventions, all delivered in the USA, described graduate-level academic work aimed at engaging students in implementation for professional careers in social work [34], public health [35], and nursing [36]. For instance, nurse practitioner students applied implementation concepts during their doctoral practice to gain experience leading efforts to implement evidence in practice [36]. Similarly, public health students engaged in opportunities to assess implementation determinants, strategies, and outcomes during in real-world contexts [33]. Masters of social work students developed implementation capacity by examining the delivery of a specific evidence-based practice at an assigned field site over a 16-week field rotation (Table 5).
Table 5.
Characteristics of capacity building interventions for practitioners-in-training
| Country | Participants | Core components | Training objectives | Measurement | Outcomes | |
|---|---|---|---|---|---|---|
| Bertram et al., 2018 [34] | USA | MSW graduate students | Mentorship and expert consultation, practical application activities, knowledge sharing activities | To enhance MSW students’ confidence implementing evidence-based social work practice | Qualitative review of student portfolios | ↑ knowledge and confidence understanding program implementation |
| Ramaswamy et al., 2019 [35] | USA | MPH students | Didactic activities, knowledge sharing activities | To build implementation practice capacity among MPH students | End-of-semester evaluations; online discussions | High satisfaction, per student evaluation comments |
| Riner at al., 2015 [36] | USA | DNP students | Didactic activities, mentorship and expert consultation, practical application activities, knowledge sharing | To build implementation capacity of future nurse practitioners | Alumni surveys | ↑ perceived ability to lead implementation efforts |
MSW masters of social work, MPH masters of public health, DNP doctor of nursing practice
Summary of capacity building intervention components
Our analysis yielded five common components of capacity building interventions across studies. These core components included didactic activities, mentorship and expert consultation, practical application activities, knowledge sharing activities, and technical assistance.
Didactic activities
Most often, capacity building interventions consisted of structured didactic activities that were delivered in-person, online, or in a hybrid format using a combination of lectures, readings, case studies, and self-paced modules. In-person didactic content was delivered in the form of university-level courses [23, 27, 34–36] or through workshop events led by implementation science experts [26, 28, 30–33]. Duration of in-person didactic workshops ranged from one and a half to 2 days. Hybrid didactic content was highly variable in structure and length. For instance, the PH-LEADER program lasted a total of 1 year consisting of a 2-month preparation period, a 3-week, in-person summer short course, and an in-country mentored project phase. Throughout the program, participants received didactic instruction from expert faculty as well as through recorded webinars [24]. Didactic content to build implementation capacity was also provided in an ongoing manner, such as through the Knowledge Translation Strategic Training Initiative in Canada [30]. The only didactic content delivered entirely online was structured in the form of a four-course series to build implementation capacity through the University of North Carolina Chapel Hill’s Gillings School of Global Public Health [35].
Mentorship and expert consultation
Across capacity building interventions, 11 included descriptions of formal mentorship and/or consultations from implementation experts to researchers, practitioners, or practitioners-in-training. Mentorship and expert consultation were provided to increase participants’ capacity to understand implementation principles and/or lead implementation-focused projects at their respective organizations. Mentorship and consultation activities occurred in settings such as academic institutions [25–27, 32, 34–36] and specialized institutes [28, 30, 31]. One global model of mentorship consisted of implementation faculty who provided training to field mentors. As part of this model, public health students and practitioners then completed implementation projects related to HIV/AIDS research in South Africa and received routine mentorship from their trained field mentors with a focus on implementation determinants, strategies, and outcomes [29].
Practical application activities
Interventions to build implementation capacity also included development and deployment of practical application activities. These activities allowed intervention participants to lead their own implementation projects in real-world contexts through pilot projects or evaluations of implementation determinants. Practical application activities were completed through graduate student field placements [34, 36], as well as small scale implementation projects [24, 28, 30, 32, 35]. In the academic medical center setting, Li et al. [23] facilitated practical application of implementation principles by convening an informal network of implementation researchers, practitioners, students, quality improvement experts, and community stakeholders. Individuals within this network formed implementation teams who submitted grant applications (funded through the University of Kentucky) to complete implementation-related projects by partnering with medical center affiliates. Of the 26 teams who submitted applications, four projects were funded as of 2019, allowing teams to gain practical experience conducting projects informed by implementation methodologies.
Knowledge sharing activities
Knowledge sharing took the form of small group reflections and exercises, expert panel discussions, breakout activity sessions, and the development of learning collaboratives [25, 26, 29, 30, 32, 33, 35, 36] Among practitioners-in-training, as one example, social work graduate students examined the implementation of evidence-based practices over a 16-week field placement, and students completed weekly field portfolios that described the process of implementing specific evidence-based practices. Weekly cohort seminars allowed students to share content from their portfolios and their experiences implementing evidence within their field placement sites [34]. For practitioners involved in the Practicing Knowledge Translation program, participants were encouraged to engage in small group discussions and share their progress towards completing their implementation and learning goals [31].
Technical assistance
Capacity building interventions also provided technical assistance to facilitate the development of implementation projects and grant proposals. Two studies described using this type of assistance—referred to explicitly as technical assistance or technical support—which included building implementation support networks, identifying appropriate implementation projects to deploy in the community setting, and facilitating implementation training opportunities for participants [32, 33]. Specifically, the TRIPLE program aimed to build implementation capacity among behavioral health organizations and provided technical support to assist mid-level organization leaders in their implementation of evidence-based practices at their own agencies. Technical assistance (e.g., developing project activities; planning for outcome measurement) was offered by TRIPLE faculty who provided coaching on the development of implementation projects, the theories, models, and frameworks that inform implementation, strategies for implementing change, and methods for conducting organizational change evaluations [32].
Outcomes of capacity building interventions
All interventions included in this review described favorable outcomes. Outcomes were categorized into the following groups that are described in further detail below: knowledge attainment, increased perceived ability to implement evidence, productivity, and satisfaction.
Knowledge attainment
Six studies in the review explicitly gathered data on overall knowledge of implementation [23, 26, 28, 31, 34, 37], defined as the understanding and awareness of implementation models, factors, and strategies influencing evidence use. Moore and colleagues [31], for example, conducted a longitudinal study of practitioners’ knowledge and application of implementation principles at intervals over a year; all subjects showed a significant increase of knowledge, which Moore et al. associated with improved application of implementation methodologies to local projects. Bertram and colleagues [34] built implementation capacity through graduate coursework and found that the course components led to increased knowledge and understanding of implementation models, factors influencing program implementation, and implementation interventions.
Increased perceived ability to implement evidence
A total of seven studies had outcomes specifically targeting participants’ ability to implement evidence into practice, as measured through self-efficacy, confidence, and competence in evidence implementation [24, 28, 31–34, 36]. Of these studies, only four measured self-efficacy or confidence at multiple time points [24, 28, 31, 32], whereas the two academic courses targeting social work [34] and nursing [36] students used student feedback in the form of narrative course evaluation comments to assess outcomes. Tools used at baseline and follow-up included the Evidence-Based Practice Confidence Scale [38], a 3-item tool measuring intentions to use evidence [39], the Implementation Leadership Scale [40], the Implementation Climate Scale [41], and the Organizational Readiness for Implementing Change scale [42] as well as original surveys that were created by capacity building intervention developers.
Productivity
Productivity was not clearly defined as an outcome in the included studies but represents the number of researchers, practitioners, and practitioners-in-training whose implementation-related productivity changed as a result of participating in capacity building interventions. Measures of productivity were often reported in lieu of other objective outcomes, such as self-efficacy and knowledge. Examples of productivity included the development of over 50 collaborative implementation projects in low- and middle-income countries after public health professionals and researchers participated in a global capacity building intervention [24]. Similarly, Li et al.’s [25] implementation network facilitated the formation of 26 teams who submitted internal grant applications to conduct implementation studies with academic medical center partners. Studies that did not measure team or project formation reported productivity in the form of the number of participants reached [30] and the amount of implementation knowledge shared across organizations [33].
Satisfaction
Satisfaction with capacity building interventions was measured through both qualitative and quantitative methods. Student evaluation reports indicated high levels of satisfaction with online implementation coursework [23, 35], and program evaluations indicated favorable satisfaction with practical application activities [29] and collaborative learning exercises [27]. Proctor et al. [32] was the only study that quantitatively evaluated participants’ perceptions of their TRIPLE program by using the Training Acceptability and Appropriateness Scale which was administered at the post-test time point only. The Training Acceptability and Appropriateness Scale is an unpublished, 14-item measure with high internal consistency that assesses the extent to which a training intervention is acceptable, feasible, and appropriate for participants based on their self-perceived needs.
Discussion
As the field of implementation science has grown over the past 15 years, new insights about the complexities and strategies for moving effective interventions into routine care settings highlight a range of implementation skills and capacities for practitioner and policy leaders. Academic institutions building capacity for implementation scholarship are also well positioned to build capacity among those in real world health and human service settings, although how practitioners are included and trained in these initiatives is unclear [7]. This scoping review identified 14 studies of implementation capacity building interventions that included practitioner stakeholders and also had ties to academic institutions. Results demonstrate how initiatives have targeted a range of stakeholders including practice leaders and students, often using traditional didactic or mentored training approaches with a goal of improving implementation knowledge, self-efficacy, skills, and capacities. Institution-wide efforts to build connections among implementation teams of practitioners and researchers were rare but might offer important opportunities to build capacity for implementation research and practice in concert. These results have direct implications for how other academic institutions design implementation capacity building interventions.
It is important to note that the capacity building interventions identified in this review target an array of practitioner and student/trainee stakeholders by pairing them with an expert in implementation science in a variety of settings. Additionally, the capacity building interventions reported building student or practice leader capacity via expert-led initiatives, which tended to be formal and structured programs. While these were generally effective, few programs described leveraging existing university/practice partnerships (perhaps even within their own healthcare systems) to create collaborative learning and network building to support implementation science approaches across practice settings. This is an important gap to highlight, as expanding current partnerships to build capacity for implementation science and application is a feasible approach with potential for immense gains [43].
Intervention components
Didactic activities, either online or in person, as well as expert consultation, continue to be used most often in implementation practice capacity building interventions. Didactic coursework models typically rely upon centralized implementation experts who are responsible for training and supporting participants. Other larger initiatives are often housed within an institution or system and focus on building networks and sharing knowledge across teams and stakeholders. Within this larger model, expertise is often distributed under the assumption that capacity is built by connecting teams and stakeholders to share their knowledge and expertise across settings. Structured learning activities provide opportunities to gain important skills while also encouraging network building among participants. These intervention components are similar to other collaborative learning models (e.g., [44]) suggesting their promise for developing implementation practice capacity among diverse stakeholders.
Outcomes
A number of outcomes were reported across studies included in our review. Outcomes included knowledge of implementation and/or its application, self-efficacy and confidence implementing evidence in practice, collaborations with researchers and practitioners, and participant satisfaction. Productivity was reported mostly in numbers of projects and teams created. While most programs reported positive gains across outcomes measures, there was wide heterogeneity in methods of measurement and time points for evaluation. Several interventions reported on immediate educational outcomes or included a singular point in time for follow-up measures. Because many initiatives are often designed with the long-term goal of improving implementation in real-world settings, additional implementation outcomes that might be especially relevant to practitioners may include adoption, fidelity, penetration, and sustainability [45]. Future program descriptions and evaluations should consider use of these additional outcomes measures to better detect degree of impact and diffusion of capacity building interventions over time and across a variety of practice settings.
Limitations
There are inherent limitations to this scoping review summary. The primary limitation is that findings are limited to only published studies of academic/practice-based capacity building interventions. As such, content does not include current or ongoing implementation practice programming for practitioners that is delivered in non-academic settings, has yet to be evaluated, or has yet to be published in the academic literature. Another limitation to the interventions described in our review was that nearly all included reports were descriptive, which is important for informing designs in other settings, but does not allow for inferences about their effectiveness. Future work in this area would benefit from more rigorous designs for examining the educational and implementation outcomes of capacity building interventions. Lastly, there was substantial variation in how capacity building interventions components (e.g., didactic activities) and outcomes were described. While our open coding analysis with two reviewers aimed to address this limitation, it should be noted that the definitions of intervention components and outcomes were established by the review team rather than by the original capacity building intervention developers.
Implications and future directions
The field of implementation science has generated important knowledge to streamline integration of research evidence into a multitude of practice settings. After over 15 years of focused research advancements in this field, additional attention is now needed to integrate this knowledge into educational programs in health and allied healthcare fields to prepare future leaders and practitioners in the practice of science-based implementation. Simultaneously, programming for building capacity should also target existing practice leaders who have potential and reach to integrate skills into their agencies and teams. Training non-provider leaders can also bring needed support and resources to busy practice settings. Notably, none of the capacity building interventions in this review identified targeted policy makers, despite their role in generating policies and regulations to support the adoption and sustainability of evidence-based interventions. Working with policy makers to expand their implementation knowledge and skills for using research evidence might be an area for innovative partnerships that has potential to lead to needed studies of policy implementation strategies, and changes to policy practices that support implementation [46, 47]. Building this type of implementation capacity across current and future academic, practice, and policy settings will prevent development of a secondary implementation research to practice gap.
Conclusion
While D&I trainings for researchers have proliferated in recent years, it is unclear whether and how comparable parallel efforts have targeted communities of practitioners to integrate insights from implementation science about planning, strategies, adaptation, or sustainability of best practices. For instance, the field lacks evidence or descriptions of how implementation science insights have been integrated into professional graduate training programs, continuing education workshops, and other professional development opportunities for practice leaders. It is also unclear whether the majority of capacity building interventions train community practitioners and researchers to collaborate in service of generating new evidence about strategies for integrating effective interventions within local contexts and the degree of diffusion of those findings across similar networks. Ultimately, the goal of any capacity building initiative is to yield long-term, sustainable impact over time and across settings and teams. This includes increasing the number of evidence-based interventions that are implemented and evaluated, reducing the time it takes for integration into real-world practice. As participants in capacity building interventions build knowledge, skills, and competencies, program initiatives may need to evolve to incorporate more advanced or sustained components and supports. As such, long term evaluations of these programs over time is necessary.
Supplementary Information
Acknowledgements
None
Authors’ contributions
LJ, AB, MM, and ST were jointly responsible for conceptualizing the purpose of this review and refining the search strategy. LJ and MR screened all articles, selected articles that met inclusion criteria, and completed data extraction activities. LJ was responsible for drafting the manuscript and incorporating revisions and additions from AB, MM, MR, and ST. All authors read and approved the manuscript’s final version.
Funding
Not applicable
Availability of data and materials
Not applicable as extracted data from study articles are included in Tables 1, 2, and 3
Declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Li S-A, Jeffs L, Barwick M, Stevens B. Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: a systematic integrative review. Syst Rev. 2018;7:72. doi: 10.1186/s13643-018-0734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:109. doi: 10.1186/s13012-015-0295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53. doi: 10.1186/s13012-015-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palinkas LA, Aarons GA, Chorpita BF, Hoagwood K, Landsverk J, Weisz JR. Cultural exchange and the implementation of evidence-based practices: two case studies. Res Soc Work Pract. 2009;19:602–612. doi: 10.1177/1049731509335529. [DOI] [Google Scholar]
- 6.Boehm LM, Stolldorf DP, Jeffery AD. Implementation science training and resources for nurses and nurse scientists. J Nurs Scholarsh. 2020;52:47–54. doi: 10.1111/jnu.12510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis R, D’Lima D. Building capacity in dissemination and implementation science: a systematic review of the academic literature on teaching and training initiatives. Implement Sci. 2020;15:97. doi: 10.1186/s13012-020-01051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Armstrong R, Sales A. Welcome to implementation science communications. Implement Sci Commun. 2020;1:1. doi: 10.1186/s43058-020-00018-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. 2020;283:112376. doi: 10.1016/j.psychres.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 10.Proctor EK, Chambers DA. Training in dissemination and implementation research: a field-wide perspective. Transl Behav Med. 2017;7:624–635. doi: 10.1007/s13142-016-0406-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vinson CA, Clyne M, Cardoza N, Emmons KM. Building capacity: a cross-sectional evaluation of the US Training Institute for Dissemination and Implementation Research in Health. Implement Sci IS. 2019;14:97. doi: 10.1186/s13012-019-0947-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chambers DA, Proctor EK, Brownson RC, Straus SE. Mapping training needs for dissemination and implementation research: lessons from a synthesis of existing D&I research training programs. Transl Behav Med. 2017;7:593–601. doi: 10.1007/s13142-016-0399-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Proctor EK, Landsverk J, Baumann AA, Mittman BS, Aarons GA, Brownson RC, et al. The implementation research institute: training mental health implementation researchers in the United States. Implement Sci IS. 2013;8:105. doi: 10.1186/1748-5908-8-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Padek M, Mir N, Jacob RR, Chambers DA, Dobbins M, Emmons KM, et al. Training scholars in dissemination and implementation research for cancer prevention and control: a mentored approach. Implement Sci IS. 2018;13:18. doi: 10.1186/s13012-018-0711-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Albers B, Shlonsky A, Mildon R, editors. Implementation Science 3.0 [Internet]. Springer International Publishing; 2020 [cited 2020 May 11]. Available from: https://www.springer.com/us/book/9783030038731
- 16.Westerlund A, Sundberg L, Nilsen P. Implementation of implementation science knowledge: the research-practice gap paradox. Worldviews Evid Based Nurs. 2019;16:332–334. doi: 10.1111/wvn.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leeman J, Calancie L, Hartman MA, Escoffery CT, Herrmann AK, Tague LE, et al. What strategies are used to build practitioners’ capacity to implement community-based interventions and are they effective?: a systematic review. Implement Sci. 2015;10:80. doi: 10.1186/s13012-015-0272-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Albers B, Shlonsky A, Mildon R, editors. Implementation Science 3.0 [Internet]. Springer International Publishing; 2020 [cited 2021 Apr 19]. Available from: https://www.springer.com/gp/book/9783030038731
- 19.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 20.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 22.Goulas G. How can I cite Covidence? [Internet]. 2021 [cited 2022 Apr 15]. Available from: https://support.covidence.org/help/how-can-i-cite-covidence
- 23.Carlfjord S, Roback K, Nilsen P. Five years’ experience of an annual course on implementation science: an evaluation among course participants. Implement Sci. 2017;12:1–8. doi: 10.1186/s13012-017-0618-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galaviz KI, Venkat Narayan KM, Manders O, McFarland DA, Goenka S, Torres-Mejía G, et al. The public health leadership and implementation academy (PH-LEADER) for non-communicable diseases. Health Syst Reform. 2016;2:222–228. doi: 10.1080/23288604.2016.1224452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li J, Williams MV, Page C, Cassis L, Kern PA, DiPaola RS. The Value of Innovation to Implementation Program (VI 2 P): a strategic approach to aligning and leveraging academic research and clinical care missions. Learn Health Syst. 2019;3:e10199. doi: 10.1002/lrh2.10199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morrato EH, Rabin B, Proctor J, Cicutto LC, Battaglia CT, Lambert-Kerzner A, et al. Bringing it home: expanding the local reach of dissemination and implementation training via a university-based workshop. Implement Sci. 2015;10:1–12. doi: 10.1186/s13012-015-0281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Norton WE. Advancing the science and practice of dissemination and implementation in health: a novel course for public health students and academic researchers. Public Health Rep Wash DC. 1974;2014(129):536–542. doi: 10.1177/003335491412900613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park JS, Moore JE, Sayal R, Holmes BJ, Scarrow G, Graham ID, et al. Evaluation of the “Foundations in Knowledge Translation” training initiative: preparing end users to practice KT. Implement Sci. 2018;13:N.PAG. doi: 10.1186/s13012-018-0755-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramaswamy R, Chirwa T, Salisbury K, Ncayiyana J, Ibisomi L, Rispel L, et al. Developing a field of study in implementation science for the Africa region: the Wits–UNC AIDS Implementation Science Fogarty D43. Pedagogy Health Promot. 2020;6:46–55. doi: 10.1177/2373379919897088. [DOI] [Google Scholar]
- 30.Straus SE, Brouwers M, Johnson D, Lavis JN, Légaré F, Majumdar SR, et al. Core competencies in the science and practice of knowledge translation: description of a Canadian strategic training initiative. Implement Sci IS. 2011;6:127. doi: 10.1186/1748-5908-6-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore JE, Rashid S, Park JS, Khan S, Straus SE. Longitudinal evaluation of a course to build core competencies in implementation practice. Implement Sci. 2018;13:N.PAG. doi: 10.1186/s13012-018-0800-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Proctor E, Ramsey AT, Brown MT, Malone S, Hooley C, McKay V. Training in Implementation Practice Leadership (TRIPLE): evaluation of a novel practice change strategy in behavioral health organizations. Implement Sci IS. 2019;14:66. doi: 10.1186/s13012-019-0906-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramanadhan S, Minsky S, Martinez-Dominguez V, Viswanath K. “Building practitioner networks to support dissemination and implementation of evidence-based programs in community settings”: Erratum. Transl Behav Med. 2017;7:542. doi: 10.1007/s13142-017-0518-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bertram RM, Choi S-W, Elsen, M. Integrating Implementation Science and Evidence-Based Practice Into Academic and Field Curricula. J Soc Work Edu. 2018;54:S20–30.
- 35.Ramaswamy R, Mosnier J, Reed K, Powell BJ, Schenck AP. Building capacity for Public Health 3.0: introducing implementation science into an MPH curriculum. Implement Sci IS. 2019;14:18. doi: 10.1186/s13012-019-0866-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riner ME. Using implementation science as the core of the doctor of nursing practice inquiry project. J Prof Nurs. 2015;31:200–207. doi: 10.1016/j.profnurs.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 37.Norton WE, McCannon CJ, Schall MW, Mittman BS. A stakeholder-driven agenda for advancing the science and practice of scale-up and spread in health. Implement Sci. 2012;7:118–123. doi: 10.1186/1748-5908-7-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salbach NM, Jaglal SB, Williams JI. Reliability and validity of the evidence-based practice confidence (EPIC) scale. J Contin Educ Health Prof. 2013;33:33–40. doi: 10.1002/chp.21164. [DOI] [PubMed] [Google Scholar]
- 39.Boyko JA, Lavis JN, Dobbins M, Souza NM. Reliability of a tool for measuring theory of planned behaviour constructs for use in evaluating research use in policymaking. Health Res Policy Syst. 2011;9:29. doi: 10.1186/1478-4505-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aarons GA, Ehrhart MG, Farahnak LR, Finn N. Implementation leadership: confirmatory factor analysis and supervisor-clinician discrepancy in ratings on the Implementation Leadership Scale (ILS) Implement Sci. 2015;10:A70. doi: 10.1186/1748-5908-10-S1-A70. [DOI] [Google Scholar]
- 41.Ehrhart MG, Aarons GA, Farahnak LR. Assessing the organizational context for EBP implementation: the development and validity testing of the Implementation Climate Scale (ICS) Implement Sci. 2014;9:157. doi: 10.1186/s13012-014-0157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shea CM, Jacobs SR, Esserman DA, Bruce K, Weiner BJ. Organizational readiness for implementing change: a psychometric assessment of a new measure. Implement Sci IS. 2014;9:7. doi: 10.1186/1748-5908-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pellecchia M, Mandell DS, Nuske HJ, Azad G, Benjamin Wolk C, Maddox BB, et al. Community–academic partnerships in implementation research. J Community Psychol. 2018;46:941–952. doi: 10.1002/jcop.21981. [DOI] [PubMed] [Google Scholar]
- 44.Nadeem E, Gleacher A, Beidas RS. Consultation as an implementation strategy for evidence-based practices across multiple contexts: unpacking the black box. Adm Policy Ment Health. 2013;40:439–450. doi: 10.1007/s10488-013-0502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38:65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cervantes PE, Seag DEM, Nelson KL, Purtle J, Hoagwood KE, Horwitz SM. Academic-policy partnerships in evidence-based practice implementation and policy maker use of child mental health research. Psychiatr Serv. 2021;72:1076–1079. doi: 10.1176/appi.ps.202000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Purtle J, Nelson KL, Horwitz SMC, McKay MM, Hoagwood KE. Determinants of using children’s mental health research in policymaking: variation by type of research use and phase of policy process. Implement Sci. 2021;16:13. doi: 10.1186/s13012-021-01081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable as extracted data from study articles are included in Tables 1, 2, and 3