Abstract
Introduction
Following the Covid-19 pandemic spread, changes in clinical practice were necessary to limit the pandemic diffusion. Also, oncological practice has undergone changes with radiotherapy (RT) treatments playing a key role.
Although several experiences have been published, the aim of this review is to summarize the current evidence after 2 years of pandemic to provide useful conclusions for clinicians.
Methods
A Pubmed/MEDLINE and Embase systematic review was conducted. The search strategy was “Covid AND Radiotherapy” and only original articles in the English language were considered.
Results
A total of 2.733 papers were obtained using the mentioned search strategy. After the complete selection process, a total of 281 papers were considered eligible for the analysis of the results.
Discussion
RT has played a key role in Covid-19 pandemic as it has proved more resilient than surgery and chemotherapy. The impact of the accelerated use of hypofractionated RT and telemedicine will make these strategies central also in the post-pandemic period.
Keywords: Covid-19, Radiotherapy, Oncological practice
Introduction
An unexpected series of life threating pneumonias and deaths began in Wuhan, China, starting in December 2019, and soon spread worldwide. On 7 January 2020, the World Health Organization (WHO) announced the official name of the disease as “coronavirus disease 2019” (Covid-19) [1, 2].
Analysis of the viral genome revealed that this new coronavirus is phylogenetically close to severe acute respiratory syndrome coronavirus (SARS-CoV) [3].
Globally, at 4:00 pm CET, 28 January 2022, 364.191.494 cases of Covid-19 were confirmed, with 5.631.457 deaths as reported to World Health Organization (WHO) by the national authorities [4].
However, thanks to the effectiveness and spread of Covid-19 vaccines around the world, there has been a decrease in mortality rate [5].
As of 28 January 2022, a total of 9.854.237.363 vaccines doses were administered [4].
The symptomatic severity of Covid-19 infection appeared to worsen with increasing age and the presence of comorbidities. In fact, older patients with basic chronic diseases, such as cancer, were more vulnerable to Covid-19 infection [6–10].
In a recent multicentre study, cancer patients were found to be a highly vulnerable group due to the weakened immune system caused by both tumor growth and anti-cancer treatment. Patients with hematologic cancer, lung cancer, or with metastatic cancer had the highest frequency of severe events. In particular, patients who received surgery had a higher risk of serious events, while patients who received only radiotherapy (RT) showed no significant difference in serious events compared to patients without cancer [11].
RT has played a role in the changes in oncological practice, including an increase in organ-sparing treatment and achieving good local control and improving survival [12].
More than 50% of cancer patients have undergone RT treatment at least one time during their disease [13].
Furthermore, Covid-19 infection had a dramatic impact on cancer diagnosis, prognosis, and therapeutic effects [6]. Serious delays in surgical, chemotherapy and RT treatments due to patients' Covid-19 infection, organizational problems in healthcare facilities and also fear of infection among patients caused a substantial increase in the number of avoidable cancer deaths [14–17].
Covid-19 has also had a great impact on radiation oncologists, and so several measures have been adopted in patient management beginning with the treatment workflow [18, 19].
Many studies related to RT and Covid-19 have been published in these 2 years of the pandemic. Therefore, the aim of this systematic review is to summarize the current evidences after these 2 years, to provide better and useful conclusions for clinicians.
Materials and methods
A systematic database search was conducted using definite keywords, according to Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) guidelines [20].
The search strategy was performed on PubMed, Medline and Embase using the search terms: “Covid AND Radiotherapy” up to date 31/12/2021.
Original studies, editorials, letters to editor, review and case reports focusing on Covid-19 and RT were included in this review.
Studies performed not in English and conference abstract were not take into account.
Results
A total of 2.733 papers were found at the first search, 859 of which were duplicates. Of the 1874 remaining results, 1397 were excluded after a careful screening of abstracts.
477 articles were lastly selected for further accurate analysis. Out of these, 196 were excluded, as they did not directly target Covid-19 and RT. The remaining 281 papers were lastly included in this review.
The review workflow was compliant with the PRISMA guidelines, and the relative flowchart is reported in Fig. 1 [20].
Fig. 1.
Prisma diagram
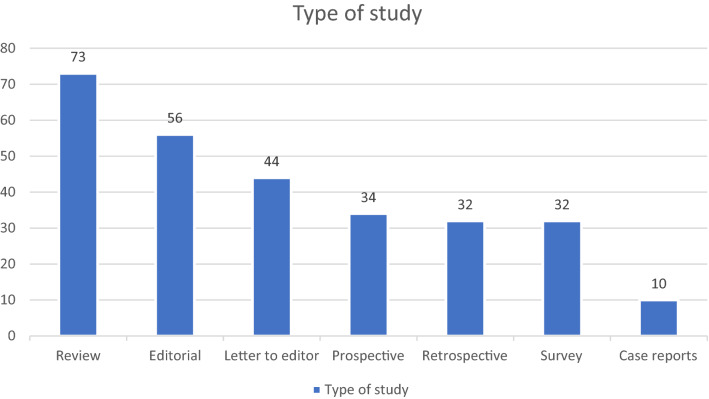
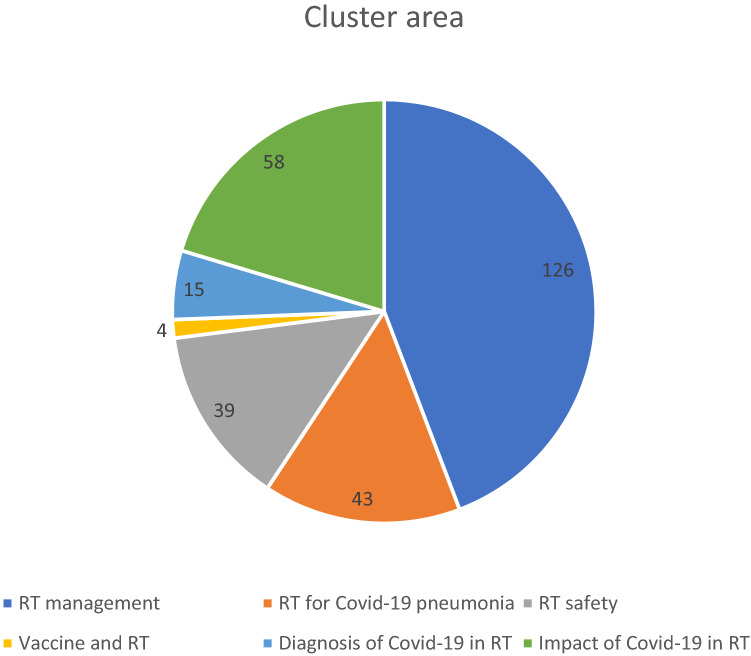
We summarize the main characteristics of the analyzed studies, divided into different cluster areas and study types (Figs. 2, 3). Table 1 resumes the main indications provided for different cancer types.
Fig. 2.
Type of study
Fig. 3.
Cluster area
Table 1.
Summary of main indication for cancer types
| Site | Patient setting | RT management | RT schedules | COVID + (asymptomatic/mild symptomatic) | COVID + (symptomatic) |
|---|---|---|---|---|---|
| Lung cancer [72–82] | General |
Increase HFRT Increase SBRT |
Continue RT(CT) with close monitoring of clinical conditions |
Postpone after confirmed healing Interrupt or preliminarily terminate ongoing treatments |
|
| NSCLC |
Delay post-operative RT Avoid twice-daily treatments |
||||
|
NSLC (early stage) |
Increase SBRT |
50–60 Gy in 5 fr (central tumors) 48 Gy in 4 fr (adjacent/contact with chest wall) |
|||
| SCLC |
Delay PCI Consider delivering PCI during concurrent RT(CT) |
||||
| Hematological cancer [83] | General | Shorten RT course | |||
| Palliative | Omission RT treatments | – | |||
| Localized low-grade |
Omission RT for completely excised Delay for asymptomatic patients |
Delay RT | |||
| Localized nodular LH |
Omission RT for completely excised Delay for asymptomatic patients |
||||
| Diffuse large B/aggressive LNH | Omission RT for consolidation | ||||
| Head & Neck [72, 84–93] | General | Increase HFRT |
Continue RT(CT) with close monitoring of clinical conditions Use surgical mask with immobilization setup |
||
|
Prostate |
General |
Increase HFRT Consider starting RT up to 6 months after OT |
|||
| Low-risk |
Increase HFRT Increase SBRT |
36.25 Gy in 5 fr twice-week | |||
| Gastrointestinal [98, 100–110] | Esophageal cancer | 40 Gy in 15 fr | |||
| Inoperalble Cholangiocarcinoma | Consider SBRT | ||||
| Pancreatic cancer | Consider SBRT in inoperable LAPC | ||||
| Anal cancer | Increase HFRT |
36/40 Gy in 20 fr to elective volume; 50 Gy in 20 fr to primary tumor with SIB |
|||
| Liver cancer |
Carbon ION RT for unresectable disease Consider SBRT for Hepato Cellular Carcinomas |
30–60 Gy in 3–5 fr | |||
| Rectal cancer | Prefer short course treatments | ||||
| Skin [112–116] | General |
Delay or omit adjuvant RT Consider HFRT Consider contact skin RT |
|||
| Breast [98, 117–121] | General |
Delay or omit adjuvant RT in older adult EBC Consider HFRT |
|||
| Soft tissues – Sarcomas [122] | General | Consider HFRT |
30 Gy in 10 fr 30 Gy in 5 fr 28 Gy in 8 fr 25 Gy in 5 fr |
||
| Gynecological [123, 124] | General | Consider HFRT | |||
| Uterine cancer | Do not exceed 6 weeks after surgery for adjuvant RT |
RT radiation therapy, HFRT Hypofractionated radiation therapy, SBRT Stereotactic body radiation therapy, NSCLC Non-small cell lung cancer, SCLC Small cell lung cancer, PCI prophylactic cranial irradiation, LH Hodgkin lymphomas, LNH Non-Hodgkin lymphomas, LAPC Locally advanced pancreatic cancer, SIB simultaneous integrated boost, EBC Early breast cancer
RT general management
Fifty-four studies focused on the RT general management during Covid-19 pandemic [14, 16, 18, 21–71].
Thirteen studies recommended the use of telemedicine [22, 27, 29, 30, 33, 36, 40, 42, 44, 50–53].
Telemedicine shows its helpfulness in the RT field, and patients get the supportive care they need minimizing their access to hospitals [22].
In a single academic radiation oncology session, the physicians interviewed indicated that their experience in using telemedicine has been largely positive, and most of them envision telemedicine as part of their radiation oncology practice in the future [51].
Eight studies analyzed the results suggesting the omission or postponement of RT when possible [14, 21, 23–25, 30, 42, 44].
Indications for RT with limited improvement in oncologic outcomes were viewed critically under conditions of limited health care resources by some expert groups, including RT of low-risk breast cancer in elderly patients and of early-stage Hodgkin’s lymphoma [21].
Twenty-eight studies recommended the use of hypofractionated scheduling [18, 21–23, 25, 28–37, 40–43, 47, 48, 55, 58, 59, 61, 62, 70] and appropriate hypofractionated regimens should be considered during a pandemic to reduce treatment duration and minimize the risk of infection [18].
Six studies discussed organization of work and staff during the pandemic [47, 50, 63–65, 71].
To ensure such continuity of services, the following measures were implemented: patients screening, temperature monitoring, patient and staff education, ensuring adequate medical supplies, continuous use of communication channels, adequate manpower should a staff member fall sick or need to be quarantined as a result of contact with patients with Covid-19, physical segregation of staff across hospitals, physical segregation of patients, formation of separated care teams, remote planning, hygiene and departmental cleaning [47].
RT management—lung cancer
Eleven studies focused on the RT management of Lung Cancer during Covid-19 pandemic [72–82].
All papers suggested an increase in the use of Hypofractionated radiation therapy (HFRT) and Stereotactic body radiation therapy (SBRT).
Liao et al. also suggested the delay of post-operative RT for non-small cell lung cancer, to avoid twice-daily treatments and delay or deliver prophylactic cranial irradiation during radio(chemo)therapy for limited-stage small cell lung cancer [73].
Furthermore, Couñago et al. in their review recommended for non-small-cell lung cancer early-stage central tumors, SBRT with scheme from 10 to 12 Gy/fraction (fr) with a total dose 50–60 Gy. For lesions adjacent or in contact with the chest wall, a dose of up to 48 Gy in 4 fr. For tumors in a safe zone extreme, HFRT with a single fr of 30–34 Gy [76].
The joint European Society for Radiotherapy and Oncology—American Society for Radiation Oncology (ESTRO-ASTRO) established pragmatic and balanced consensus recommendations in common clinical scenarios of RT for lung cancer [72, 82].
In asymptomatic Covid-19 positive patients, radio(chemo)therapy may be continued as planned with precautious measures with caregivers in place to avoid exposure, while in mildly symptomatic Covid-19 positive patients, radio(chemo)therapy may be continued provided the patient is very closely monitored. However, in critically symptomatic Covid-19 positive patients, treatment needs to be postponed, interrupted or even preliminarily terminated [82].
RT management—hematological cancer
One study provided practice guidelines on the RT management of hematological cancers. The authors suggested three potential strategies to reduce the demand for RT during the pandemic:
Omission in a palliative setting, for localized low-grade lymphomas if completely excised, for localized nodular lymphocyte-predominant Hodgkin lymphoma if completely excised, in consolidation RT for diffuse large B-cell lymphoma/aggressive non-Hodgkin lymphoma.
Delay for asymptomatic localized low-grade lymphomas, for localized nodular lymphocyte-predominant Hodgkin lymphoma, in a palliative setting for low-grade lymphomas in stable patients, or patients who develop Covid-19 infection prior to commencing RT.
Shortening the RT course [83].
RT management—head & neck cancer
Eleven studies focused on head and neck cancer (H&N) RT management[72, 84–93].
Modest HFRT has been recommended by several authors. The most common schedule is 55 Gy in 20 frs. However, no studies recommended extreme HFRT [85].
Thomson et al. recommended not to stop treatment, especially if patients had already completed the first 2 weeks [55].
Three studies investigated surgical mask use in H&N cancer patients [90–92].
Ding et al. demonstrated in a small prospective study, that the setup error was affected by wearing a surgical mask. They recommended that the immobilization open mask should be used when the patients cannot finish the whole treatment with a surgical mask [90].
Wang et al. in their study revealed that mask wearing for patients undergoing daily RT is feasible and can provide basic protection for patients and staff [92].
RT management—prostate cancer
Five studies dealt with RT management during the Covid-19 pandemic [94–99].
These studies showed that: ultra HFRT is preferred for localized, oligometastatic, and low-volume M1; while moderate HFRT is preferred for postprostatectomy and clinical node positive disease and salvage is preferred to adjuvant radiation [96].
The trial by Barra et al. recommended SBRT at a dose of 36.25 Gy in 5 frs, twice a week, as the preferred treatment option in medical emergencies in low-risk prostate cancer [97].
As regards hormone therapy in unfavorable intermediate-risk, high-risk, or very high-risk prostate cancer patients, later RT initiation up to 6 months after androgen deprivation therapy initiation was not associated with worse overall survival [94].
RT management—gastrointestinal cancer
Twelve studies provided recommendations for the use of RT in managing patients with gastrointestinal malignancies in the era of Covid-19 [98, 100–110]:
In esophageal cancer, the Walsh regimen of 40 Gy in 15 frs can be considered, whereas for inoperable cholangiocarcinoma, SBRT is the acceptable option [101].
For cases of pancreatic cancer that remain borderline resectable even after a complete course of six months of neoadjuvant chemotherapy, SBRT in 5 frs can be considered [101].
Patients with anal cancer who are not candidates to receive concurrent chemotherapy (due to comorbidities or poor performance status) can be treated with a hypofractionated regimen of 36–40 Gy in 20 frs to the elective volume with a simultaneous integrated boost to 50 Gy to the primary tumor [101].
Carbon Ion RT is an optimal treatment strategy for unresectable Liver Cancer [111].
SBRT should be considered for patients with Hepato Cellular Carcinoma from the early stage to the most advanced stages with the total dose of 30–60 Gy in 3–5 fr [101, 106, 108].
Short course RT 25 Gy in 5 fr in rectal cancer is preferable to long course RT [98, 100, 101, 105, 110].
RT management—skin cancer
Five articles discussed RT management in skin cancer patients [112–116].
Omitting or delaying adjuvant RT should be considered where the benefit is likely to be limited [112, 113].
For Non Melanoma Skin Cancer, Veness et al. in their review, recommended HFRT (2.1–5 Gy fr sizes using 8–20 frs) in both the definitive and post-operative settings [114]. Instead, Lancellotta et al. delivered contact skin RT (brachytherapy) in 8 frs of 5 Gy each, twice a day [115].
RT management—breast cancer
According to six studies evaluated RT management in breast cancer patients [98, 117–121],
HFRT should be the standard of care. Partial breast irradiation and ultra- HFRT regimens could be considered in selected cases due to the pandemic [117, 119].
Adjuvant RT might be omitted in a highly selected group of older adult early-stage breast cancer patients with favorable prognostic factors [117].
RT management—sarcoma
A study investigated the use of preoperative HFRT in sarcomas. The authors suggested that HFRT is a promising treatment option providing satisfactory local control with acceptable toxicity. The recommended regimes are 3 Gy for 10 fr, 3.5 Gy for 8 fr, 5 Gy for 5 fr, 6 Gy for 5 fr [122].
RT management—gynecological cancer
An expert consensus recommendation provided guidance for delivering radiation therapy during the Covid-19 pandemic [123].
HFRT should be used when feasible and recommendations regarding radiation dose, timing, and technique have been provided for external beam and brachytherapy treatments [123].
In a letter to editor, Matsuo et al. examined the association between post-hysterectomy RT wait-time and oncologic outcomes in women with early-stage cervical cancer.
They observed a poorer oncologic outcome with longer adjuvant RT wait-time after radical hysterectomy, and suggested the initiation of adjuvant RT within 6 weeks after surgical treatment whenever possible [124].
Interventional radiotherapy (IRT) management
Nine articles focused on the management of IRT during Covid-19 pandemic [99, 115, 125–131].
The use of shorter IRT fractionation schedules will help minimize patient exposure and conserve resources that are important during Covid-19 [115, 127].
Muramaki et al. reported increased number of prostate cancer patients, selecting high dose-rate interstitial brachytherapy in our department [99].
IRT procedure may be a prudent choice used as a first-line treatment in early-stage cervical malignancies. IRT should not be delayed in patients without the Covid-19 symptoms [131].
Practical indications for management of patient candidates for IRT and Intraoperative Radiotherapy (IORT) during Covid-19 pandemic have been provided by AIRO (Italian Association of Radiotherapy and Clinical Oncology) Interventional Radiotherapy Working Group [125].
Palliative RT management
Nine articles focused on the management of Palliative RT during Covid-19 pandemic [132–140].
During the Covid-19 pandemic, a short course was recommended to reduce the risk of viral exposure to all patients and staff, without compromising functional outcomes [135, 136].
Also, other studies focusing on the management of different diseases, about palliative RT recommended a single fractionation of 8–10 Gy [32, 76, 87, 112].
The Palliative Care and Supportive Therapies Working Group (AIRO-palliative) provided a comprehensive summary of the literature guideline indications of palliative RT for Metastatic Epidural Spinal Cord Compression, Hemostasis, Mediastinal Syndrome, Painful or no bone metastasis, Oligometastases Suitable for SBRT, Brain metastases [133].
The GEMO (European Study Group of Bone Metastases) recommended the use of monofractionated RT (8 Gy) for painful bone metastases and Metastatic Epidural Spinal Cord Compression; although, RT may be postponed in Adjuvant bone metastasis RT setting [134].
RT for Covid-19 pneumonia
Forty-three studies investigated treatment of Covid-19 pneumonia with RT [141–183]. Observations from these studies indicate that Low-dose radiotherapy (LDRT) for Covid-19 pneumonia delivers doses between 0.3 and 1 Gy. LDRT does not decrease the viability of virus directly, but it may increase the effectiveness of antiviral immune responses in the early/medium stages of SARS-CoV‑2 infection [141, 146, 151, 164, 167, 171, 177, 179].
Whole-lung LDRT seems to be a promising approach for avoiding or delaying invasive respiratory support with a low risk of toxicity [142, 154, 159].
LDRT induces an anti-inflammatory phenotype that can potentially give therapeutic benefits against Covid-19-related complications [143, 148, 158, 162, 163, 175].
RT safety
Thirty-nine studies focused on RT safety during Covid-19 pandemic [184–222]
In particular, 7 articles discussed RT on Covid-19 positive patients [184–189, 218].
In the study of Beddok et al. the observed acute and late toxicities were ultimately similar to those observed in a population not infected with Covid-19. However, these results do not prompt the modification of standard RT protocols for irradiation of Covid-19 patients [184].
Covid-19 infected cancer patients in RT practice show similar symptoms and demographic characteristics as the general population infected with SARS-CoV-2 virus [186].
Eight studies addressed the side-effects of LDRT treatment [190–194, 220–222].
The prospective trial of Arruda et al. showed that a RT dose ≤ 0.5 Gy provides an acceptable lifetime attributable risk estimate (≤ 1%) for radiation-induced cancer [191].
These studies suggest that RT may have the best benefit-risk balance for older patients with low baseline risk factors [192, 193].
The other studies focused on RT workflow and preventive protection procedures for Covid-19 infection in all patients and healthcare professionals [195, 197–200, 205, 212, 213, 216].
Vaccine and RT
Four studies discussed the correlation between Covid-19 vaccine and RT [223–226].
Three of them were case reports reporting three skin toxicities in treatment fields and one lung toxicity in patients undergoing RT [223, 225, 226].
The prospective study of Scoccianti et al. showed that Moderna mRNA-1273 vaccine produced good results in patients who underwent RT for both early adverse events and late adverse effects [224].
Diagnosis of Covid-19 in RT
Fifteen studies addressed the diagnosis of Covid-19 in patients during RT or its preparation phases [19, 44, 227–239].
Five studies confirmed the benefits of the systematic use of chest computed tomography (CT) screening during CT simulation for patients undergoing RT during the Covid-19 pandemic [19, 227, 228, 232, 237].
Cone Beam CT (CBCT) during the treatment also made it possible to diagnose Covid-19 [233, 239].
Impact of Covid-19 in RT
Fifty-eight studies discussed the impact of Covid-19 in RT [15, 171, 240–296].
These studies were involved in the use of information technologies, RT prioritization, HFRT and protection procedures guarantee between patient care and safety while safeguarding the healthcare staff [243–245, 252, 270].
In a study published in The Lancet, the authors analyzed data relating to RT delivery for cancer patients in English National Health Service, which showed that RT activity fell significantly, but use of HFRT rapidly increased during the first peak of the Covid-19 pandemic. An increase in treatments for some cancers suggests that RT compensated for reduced surgical activity [248].
Teckie et al. emphasized that RT is more effectual compared to surgery and chemotherapy. During the pandemic, their RT department consistently maintained safe, timely and evidence-based standards of care, with very low staff and patient infection rates. While the surgical option was closed for 2 months, chemotherapy showed an increased risk of death from Covid-19 among patients traditionally receiving more aggressive chemotherapy, including those with haematological cancers, lung cancer and metastatic cancer [245].
The Covid-19 pandemic affected the regular RT delivery to oncologic patients, owing to the delay or cancelation of procedures with the likely effect of observing the worsening of local disease control and reduced survival rates in the future [241, 249, 259, 263, 267, 274, 279, 280, 285, 286].
The RT center of Renmin Hospital of Wuhan University was shut down on January 24, and reopened on March 9, 2020. Thus, many patients had impromptu interruptions of their RT treatment plan during this period and it was detected that stage IV was associated with poor prognosis compared with stage I-III [296].
A significant increase in the experience of isolation and a decrease in emotional functions and the general quality of life were observed during the Covid-19 lockdown in cancer patients [15, 253, 254, 264, 268, 273, 277, 278, 282, 287].
A survey among 543 researchers in the field of radiation oncology was carried out during the early weeks of the Covid-19 pandemic, showing a non-negligible impact on both productivity and mental health [258].
Discussion
This is a review of all papers on RT related to the Covid-19 pandemic that have been published in the last 2 years. The search for articles was performed until 31/12/2021, so exactly 2 years after the start of the pandemic.
The importance of the topic is demonstrated by the large number of papers found during the review process.
These studies were performed all over the world, from Africa to America, from Europe to Asia.
We classified the articles into 5 cluster areas:
RT management (divided into subgroups according to pathology).
RT for Covid-19 pneumonia.
RT Safety.
Vaccine and RT.
Diagnosis of Covid-19 in RT.
Impact of Covid-19 in RT.
There was homogeneity in the type of studies published, with a slightly greater tendency for reviews and editorials. This is may be due to the significant attempt to give consensus/guidelines to clinicians during this difficult period.
In fact, the largest cluster areas are those of RT management during Covid-19 pandemic and Impact of Covid on RT.
Many of the articles included in the review focused on strategies for organizing work and screening for Covid-19 infection to guarantee the safety and efficiency of health services. [16, 48, 280].
There was a large general consensus on the implementation of HFRT and SBRT to reduce access to hospital and the risk of infection [70, 75, 106].
Also, concerning palliative RT, there was great concurrence for single fr treatments of 8–10 Gy [133, 136, 297, 298].
In the era of personalized treatment with research and progressive use of Radiomics and predictive dosimetric parameters, the Covid-19 pandemic has accelerated this process, leading to hypofractionation, postponement and eventually omission of treatment by evaluating risks and benefits for each individual patient [299–307].
There is a very similar scenario with regards to the digitization of the healthcare system [22, 51, 53, 308, 309].
Telemedicine was crucial during the Covid-19 pandemic allowing clinical activities to continue even during lockdown [89]. The advantages of telemedicine include its cost-effectiveness and its potential to help mitigate any shortage of physicians. Disadvantages include the lack of technological resources available in some parts of the country and problems with the security of patient data [310].
There is great concern in the literature about the effects of the suboptimal delivery of RT (including delays, interruptions or omissions). This may compromise both local control and survival [14].
The pandemic has also led to a great amount of anxiety and fear among both healthcare staff and patients. This is not to be underestimated because it can affect the proper work of healthcare staff and may contribute to interruptions or refusal of treatment by patients [258, 287]
Several studies have been published on LDRT of Covid-19 pneumonia. Although RT has an effective anti-inflammatory action to avoid or delay invasive respiratory disease, the risk of second tumors, though low, exists. With the advent of the vaccine, which is the real cure for Covid-19, LDRT is a limited treatment option [5, 144, 175].
From the analysis of the included studies, except for only 3 case reports of mild toxicity, there was no real risk of interactivity between RT and vaccine. Therefore, the vaccine seems to be safe during RT [223, 225, 226]. The only prospective study by Scoccianti et al. confirms this statement [224].
With regards to safety, just like the vaccine, RT in Covid-19 patients appears to be safe. Although, there seems to be no correlation between Covid-19 infection and RT. Therefore, if the patient has no severe Covid symptoms and is to continue radiation treatment, no adjustments of technique or dose should be made for his safety.
A really interesting cluster area was the Diagnosis. Several articles emphasized the usefulness and importance of simulation CT and CBCT in detecting suspicious interstitial pneumonias by Covid-19 [227, 233].
The most common observations on CT are ground-glass opacification air bronchograms, crazy-paving patterns, and thickening of the adjacent pleura [311].
CBCT is a medical imaging technique with inferior image quality (compared to diagnostic CT) used routinely for image guided radiotherapy (IGRT) to ensure proper positioning and visualization of any anatomical changes [230].
In conclusion, the Covid-19 pandemic has certainly caused innumerable deaths and injuries in the last two years. The RT world has reacted promptly by developing high quality screening and work safety systems. RT has played a key role in this period as it has proved to be more effective treatment option when compared to surgical procedures and chemotherapy. The accelerated use of HFRT and telemedicine due to the pandemic is already an added value to our discipline and will probably remain so in the years to follow.
Abbreviations
- RT
Radiotherapy
- WHO
World Health Organization
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta‐analyses
- HFRT
Hypofractionated radiation therapy
- SBRT
Stereotactic body radiation therapy
- ESTRO
European Society for Radiotherapy and Oncology
- ASTRO
American Society for Radiation Oncology
- H&N
Head and Neck
- IRT
Interventional Radiotherapy
- IORT
Intraoperative Radiotherapy
- GEMO
European Study Group of Bone Metastases
- LDRT
Low-dose Radiotherapy
- CT
Computed Tomography
- CBCT
Cone Beam CT
Author contributions
AP: Content planning, literature review, writing and editing. VV: literature search, literature review and writing. ADA: literature search, literature review and writing. DC: content planning and editing. SP: content planning and editing. AD: content planning and editing. LB: content planning and editing.
Funding
All authors received no specific funding for this work.
Data availability
The data presented in this study are available on request from the corresponding author.
Declarations
Conflict of interest
All authors declare no conflicts of interests.
Ethical approval and consent to participate
No Ethical approval was needed due to the design of the study.
Consent for publication
No consent to publication was needed due to the design of the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahn D-G, Shin H-J, Kim M-H, et al. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (Covid-19) J Microbiol Biotechnol. 2020;30:313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu R, Zhao X, Li J, et al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Coronavirus (Covid-19) Dashboard. https://covid19.who.int. Accessed 30 Jan 2022.
- 5.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu C, Zhao Y, Okwan-Duodu D, et al. Covid-19 in cancer patients: risk, clinical features, and management. Cancer Biol Med. 2020;17:519–527. doi: 10.20892/j.issn.2095-3941.2020.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (Covid-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 8.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian Y, Qiu X, Wang C, et al. Cancer associates with risk and severe events of Covid-19: a systematic review and meta-analysis. Int J Cancer. 2021;148:363–374. doi: 10.1002/ijc.33213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the Covid-19 outbreak. Cancer Discov. 2020;10:783–791. doi: 10.1158/2159-8290.CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russell NS, Bartelink H. Radiotherapy: the last 25 years. Cancer Treat Rev. 1999;25:365–376. doi: 10.1053/ctrv.1999.0141. [DOI] [PubMed] [Google Scholar]
- 13.Borras JM, Lievens Y, Grau C. The need for radiotherapy in Europe in 2020: not only data but also a cancer plan. Acta Oncol. 2015;54:1268–1274. doi: 10.3109/0284186X.2015.1062139. [DOI] [PubMed] [Google Scholar]
- 14.Nagar H, Formenti SC. Cancer and Covid-19 - potentially deleterious effects of delaying radiotherapy. Nat Rev Clin Oncol. 2020;17:332–334. doi: 10.1038/s41571-020-0375-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rades D, Narvaez CA, Dziggel L, et al. Emotional problems prior to adjuvant radiation therapy for breast cancer. In Vivo. 2021;35:2763–2770. doi: 10.21873/invivo.12561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Belkacemi Y, Loaganadane G, Grellier N, et al. Radiation therapy department reorganization during the coronavirus disease 2019 (Covid-19) outbreak: keys to securing staff and patients during the first weeks of the crisis and impact on radiation therapy practice from a single institution experience. Adv Radiat Oncol. 2020;5:644–650. doi: 10.1016/j.adro.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maringe C, Spicer J, Morris M, et al. The impact of the Covid-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lancia A, Bonzano E, Bottero M, et al. Radiotherapy in the era of Covid-19. Expert Rev Anticancer Ther. 2020;20:625–627. doi: 10.1080/14737140.2020.1785290. [DOI] [PubMed] [Google Scholar]
- 19.Vitullo A, De Santis MC, Marchianò A, et al. The simulation-CT: radiotherapy’s useful tool in the race against Covid-19 pandemic. A serendipity approach. Radiother Oncol. 2020;147:151–152. doi: 10.1016/j.radonc.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vordermark D. Shift in indications for radiotherapy during the Covid-19 pandemic? A review of organ-specific cancer management recommendations from multidisciplinary and surgical expert groups. Radiat Oncol. 2020;15:140. doi: 10.1186/s13014-020-01579-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Franco R, Borzillo V, D’Ippolito E, et al. Covid-19 and radiotherapy: potential new strategies for patients management with hypofractionation and telemedicine. Eur Rev Med Pharmacol Sci. 2020;24:12480–12489. doi: 10.26355/eurrev_202012_24044. [DOI] [PubMed] [Google Scholar]
- 23.Janssens GO, Mandeville HC, Timmermann B, et al. A rapid review of evidence and recommendations from the SIOPE radiation oncology working group to help mitigate for reduced pediatric radiotherapy capacity during the Covid-19 pandemic or other crises. Radiother Oncol. 2020;148:216–222. doi: 10.1016/j.radonc.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horsley PJ, Back M, Lamoury G, et al. Radiation oncology during Covid-19: strategies to avoid compromised care. Asia Pac J Clin Oncol. 2021;17:24–28. doi: 10.1111/ajco.13456. [DOI] [PubMed] [Google Scholar]
- 25.Franco P, Kochbati L, Siano M, De Bari B. Suggestions for radiation oncologists during the Covid-19 pandemic. Biomed Res Int. 2020;2020:4892382. doi: 10.1155/2020/4892382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Price P, Barney SE. Initiation of the global coalition for radiotherapy during the Covid-19 pandemic. Lancet Oncol. 2020;21:752–753. doi: 10.1016/S1470-2045(20)30281-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Slotman BJ, Lievens Y, Poortmans P, et al. Effect of Covid-19 pandemic on practice in European radiation oncology centers. Radiother Oncol. 2020;150:40–42. doi: 10.1016/j.radonc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meattini I, Franco P, Belgioia L, et al. Radiation therapy during the coronavirus disease 2019 (Covid-19) pandemic in Italy: a view of the nation’s young oncologists. ESMO Open. 2020;5:e000779. doi: 10.1136/esmoopen-2020-000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Upadhyay R, Shankar A. Implementing continued radiation therapy for cancer management in low resource countries during and after the Covid-19 crisis. Expert Rev Anticancer Ther. 2021;21:251–255. doi: 10.1080/14737140.2021.1860761. [DOI] [PubMed] [Google Scholar]
- 30.Rathod S, Dubey A, Bashir B, et al. Bracing for impact with new 4R’s in the Covid-19 pandemic—a provincial thoracic radiation oncology consensus. Radiother Oncol. 2020;149:124–127. doi: 10.1016/j.radonc.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Starling MTM, de Silva ARN, SE, Pereira APA,, et al. Recommendations for radiotherapy during the novel coronavirus pandemic. Rev Assoc Med Bras. 2020;1992(66):359–365. doi: 10.1590/1806-9282.66.3.359. [DOI] [PubMed] [Google Scholar]
- 32.Barik SK, Dhar SS, Majumdar SKD, Parida DK. Tweaking of radiation and chemotherapy schedules is the new normal during the Covid-19 crisis: perspective from oncologists at a tertiary care health institute. Ecancermedicalscience. 2021;15:1177. doi: 10.3332/ecancer.2021.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tan BF, Tuan JKL, Yap SP, et al. Managing the Covid-19 pandemic as a national radiation oncology center in Singapore. Clin Oncol (R Coll Radiol) 2020;32:e155–e159. doi: 10.1016/j.clon.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Combs SE, Belka C, Niyazi M, et al. First statement on preparation for the Covid-19 pandemic in large German speaking university-based radiation oncology departments. Radiat Oncol. 2020;15:74. doi: 10.1186/s13014-020-01527-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Shamsi HO, Abu-Gheida I, Rana SK, et al. Challenges for cancer patients returning home during SARS-COV-19 pandemic after medical tourism—a consensus report by the emirates oncology task force. BMC Cancer. 2020;20:641. doi: 10.1186/s12885-020-07115-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Odei B, Quick A. The implications of Covid-19 in radiation oncology in the United States. Curr Oncol. 2020;27:279–280. doi: 10.3747/co.27.7095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aghili M, Ghalehtaki R, Mousavi Darzikolaee N, et al. Radiotherapy and Covid-19: practical recommendations from Iran. Radiother Oncol. 2020;149:70–71. doi: 10.1016/j.radonc.2020.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simcock R, Thomas TV, Estes C, et al. Covid-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang B, Zhu J, Wu X-Y, Gao X-H. Should patients stop their radiotherapy or chemotherapy during the Covid-19 pandemic. Am J Cancer Res. 2020;10:1518–1521. [PMC free article] [PubMed] [Google Scholar]
- 40.Gupta M, Ahuja R, Gupta S, et al. Running of high patient volume radiation oncology department during Covid-19 crisis in India: our institutional strategy. Radiat Oncol J. 2020;38:93–98. doi: 10.3857/roj.2020.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iorio GC, Ricardi U, Dal Pra A. Radiation-induced lymphopenia beyond the Covid-19 pandemic. Front Oncol. 2020;10:617302. doi: 10.3389/fonc.2020.617302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siavashpour Z, Goharpey N, Mobasheri M. Radiotherapy based management during Covid-19 pandemic—a systematic review of presented consensus and guidelines. Crit Rev Oncol Hematol. 2021;164:103402. doi: 10.1016/j.critrevonc.2021.103402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kochbati L, Vanderpuye V, Moujahed R, et al. Cancer care and Covid-19: tailoring recommendations for the African radiation oncology context. Ecancermedicalscience. 2020;14:1144. doi: 10.3332/ecancer.2020.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sun R, Ammari S, Bockel S, et al. Optimization of patient management during the Covid-19 pandemic: chest CT scan and PCR as gatekeepers of the radiation therapy workflow. Front Oncol. 2020;10:556334. doi: 10.3389/fonc.2020.556334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Price P, Fleurent B, Barney SE. The role of the global coalition for radiotherapy in political advocacy for radiation therapy as a cost-effective and underfunded modality around the world. Int J Radiat Oncol Biol Phys. 2021;111:23–26. doi: 10.1016/j.ijrobp.2021.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abuhijla F, Abuhijlih R, Mohamad I. Radiation oncology practice during Covid-19 pandemic in developing countries. World J Clin Cases. 2021;9:7292–7296. doi: 10.12998/wjcc.v9.i25.7292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tey J, Ho S, Choo BA, et al. Navigating the challenges of the Covid-19 outbreak: perspectives from the radiation oncology service in Singapore. Radiother Oncol. 2020;148:189–193. doi: 10.1016/j.radonc.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Amaoui B, Semghouli S, Benjaafar N. Organization of a radiotherapy service during the Covid-19 epidemic: experience of regional center of oncology of Agadir, Morocco. Radiography (Lond) 2020;26:e312–e314. doi: 10.1016/j.radi.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suárez-Gironzini V, Moreno-Olmedo E, Pérez M, et al. Spanish risk management framework across 17 radiation oncology centers during Covid-19 pandemic. Radiother Oncol. 2020;148:267–269. doi: 10.1016/j.radonc.2020.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bi N, Yi J, Dai J, et al. Managing a radiotherapy center safely and efficiently using risk-adaptive strategies during coronavirus disease pandemic: experience from national cancer center of China. Radiother Oncol. 2020;148:243–244. doi: 10.1016/j.radonc.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang H, Cha EE, Lynch K, et al. Radiation oncologist perceptions of telemedicine from consultation to treatment planning: a mixed-methods study. Int J Radiat Oncol Biol Phys. 2020;108:421–429. doi: 10.1016/j.ijrobp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nguyen NP, Vinh-Hung V, Baumert B, et al. Older cancer patients during the Covid-19 epidemic: practice proposal of the international geriatric radiotherapy group. Cancers (Basel) 2020;12:E1287. doi: 10.3390/cancers12051287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jensen K, Dalby RB, Bouchelouche K, et al. Telehealth in multidisciplinary target delineation for radiotherapy during the Covid-19 pandemic. a review and a case. Semin Nucl Med. 2022;52:79–85. doi: 10.1053/j.semnuclmed.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hall E, Lewis R, Snowdon C. Life after Covid-19 for cancer clinical trials. Int J Radiat Oncol Biol Phys. 2020;108:486–488. doi: 10.1016/j.ijrobp.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thomson DJ, Yom SS, Saeed H, et al. Radiation fractionation schedules published during the Covid-19 pandemic: a systematic review of the quality of evidence and recommendations for future development. Int J Radiat Oncol Biol Phys. 2020;108:379–389. doi: 10.1016/j.ijrobp.2020.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mukundan H, Vats P. Advances in radiotherapy in 2020: hypofractionation - less is more in times of Covid-19. Indian J Cancer. 2021;58:41–44. doi: 10.4103/ijc.IJC_1345_20. [DOI] [PubMed] [Google Scholar]
- 57.Tabrizi S, Trippa L, Cagney D, et al. Assessment of simulated SARS-CoV-2 infection and mortality risk associated with radiation therapy among patients in 8 randomized clinical trials. JAMA Netw Open. 2021;4:e213304. doi: 10.1001/jamanetworkopen.2021.3304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Portaluri M, Barba MC, Musio D, et al. Hypofractionation in Covid-19 radiotherapy: a mix of evidence based medicine and of opportunities. Radiother Oncol. 2020;150:191–194. doi: 10.1016/j.radonc.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Larrea L, López E, Antonini P, et al. Covid-19: hypofractionation in the radiation oncology department during the “state of alarm”: first 100 patients in a private hospital in Spain. Ecancermedicalscience. 2020;14:1052. doi: 10.3332/ecancer.2020.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Swanson W, Kamwa F, Samba R, et al. Hypofractionated Radiotherapy in African cancer centers. Front Oncol. 2020;10:618641. doi: 10.3389/fonc.2020.618641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ng SSW, Ning MS, Lee P, et al. Single-fraction stereotactic body radiation therapy: a paradigm during the coronavirus disease 2019 (Covid-19) pandemic and beyond? Adv Radiat Oncol. 2020;5:761–773. doi: 10.1016/j.adro.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tripathi M, Deora H, Sadashiva N, et al. Adaptations in radiosurgery practice during COVID crisis. Neurol India. 2020;68:1008–1011. doi: 10.4103/0028-3886.299161. [DOI] [PubMed] [Google Scholar]
- 63.Riegel AC, Chou H, Baker J, et al. Development and execution of a pandemic preparedness plan: therapeutic medical physics and radiation dosimetry during the Covid-19 crisis. J Appl Clin Med Phys. 2020;21:259–265. doi: 10.1002/acm2.12971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Knutson NC, Kavanaugh JA, Li HH, et al. Radiation oncology physics coverage during the Covid-19 pandemic: successes and lessons learned. J Appl Clin Med Phys. 2021;22:4–7. doi: 10.1002/acm2.13225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sezen D, Selek U, Akdemir EY, et al. Surveying the adaptations during the Covid-19 outbreak in Turkish radiotherapy practice. Turk J Oncol. 2021 doi: 10.5505/tjo.2021.3328. [DOI] [Google Scholar]
- 66.Mummudi N, Ghosh-Laskar S, Tibdewal A, Agarwal JP. Radiotherapy practice during the Covid-19 pandemic and nation-wide lockdown: the Indian scenario. Indian J Cancer. 2021;58:140–142. doi: 10.4103/ijc.IJC_603_20. [DOI] [PubMed] [Google Scholar]
- 67.Jereczek-Fossa BA, Pepa M, Zaffaroni M, et al. Covid-19 safe and fully operational radiotherapy: an AIRO survey depicting the Italian landscape at the dawn of phase 2. Radiother Oncol. 2021;155:120–122. doi: 10.1016/j.radonc.2020.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wei S, Wang J. How to manage tumor radiotherapy during Covid-19 pandemic? Eur J Cancer Care (Engl) 2020;29:e13288. doi: 10.1111/ecc.13288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ashcroft S, Meeking K, Price P. Flash survey on the effect of Covid-19 on radiotherapy services in the UK - the benefit of social media for rapid information gathering for the radiotherapy community and government. Clin Oncol (R Coll Radiol) 2021;33:e88. doi: 10.1016/j.clon.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Franzin A, Spatola G, Giudice L, et al. Maintaining stereotactic radio surgical treatments during Covid-19 outbreak: the case of the gamma knife unit in Brescia - Italy. Br J Neurosurg. 2020;34:353–354. doi: 10.1080/02688697.2020.1758297. [DOI] [PubMed] [Google Scholar]
- 71.Vagelli G, Garrè ML, Garaventa A, et al. Specific pathways to prevent SARS-CoV-2 infection in case of repeated hospital admissions for radiotherapy. Pediatr Blood Cancer. 2020;67:e28463. doi: 10.1002/pbc.28463. [DOI] [PubMed] [Google Scholar]
- 72.Guckenberger M, Belka C, Bezjak A, et al. Practice recommendations for lung cancer radiotherapy during the Covid-19 pandemic: an ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;146:223–229. doi: 10.1016/j.radonc.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liao Z, Rivin Del Campo E, Salem A, et al. Optimizing lung cancer radiation treatment worldwide in Covid-19 outbreak. Lung Cancer. 2020;146:230–235. doi: 10.1016/j.lungcan.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Faivre-Finn C, Fenwick JD, Franks KN, et al. Reduced fractionation in lung cancer patients treated with curative-intent radiotherapy during the Covid-19 pandemic. Clin Oncol (R Coll Radiol) 2020;32:481–489. doi: 10.1016/j.clon.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mayne NR, Lin BK, Darling AJ, et al. Stereotactic body radiotherapy versus delayed surgery for early-stage non-small-cell lung cancer. Ann Surg. 2020;272:925–929. doi: 10.1097/SLA.0000000000004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Couñago F, Navarro-Martin A, Luna J, et al. GOECP/SEOR clinical recommendations for lung cancer radiotherapy during the Covid-19 pandemic. World J Clin Oncol. 2020;11:510–527. doi: 10.5306/wjco.v11.i8.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Banfill K, Croxford W, Fornacon-Wood I, et al. Changes in the management of patients having radical radiotherapy for lung cancer during the first wave of the Covid-19 pandemic in the UK. Clin Oncol (R Coll Radiol) 2022;34:19–27. doi: 10.1016/j.clon.2021.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mou B, Hyde D, Araujo C, et al. Implementation of single-fraction lung stereotactic ablative radiotherapy in a multicenter provincial cancer program during the Covid-19 pandemic. Cureus. 2021;13:e15598. doi: 10.7759/cureus.15598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kidane B, Spicer J, Kim JO, et al. SABR-BRIDGE: Stereotactic ABlative Radiotherapy Before Resection to AvoId Delay for Early-Stage LunG cancer or OligomEts during the Covid-19 pandemic. Front Oncol. 2020;10:580189. doi: 10.3389/fonc.2020.580189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Borghetti P, Toraci C, Imbrescia J, et al. The potential role of SPECT/CT in the clinical management of Covid-19 lung cancer patients undergoing radiotherapy. Ann Nucl Med. 2021;35:1174–1176. doi: 10.1007/s12149-021-01662-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Magrini SM, Borghetti P, Filippi AR, et al. Letter to the editor regarding ESTRO-ASTRO guidelines on lung cancer radiotherapy during Covid-19 pandemic. Radiother Oncol. 2020;147:229–230. doi: 10.1016/j.radonc.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Troost EGC, Nestle U, Putora PM, Bussink J. Practice recommendations for lung cancer radiotherapy during the Covid-19 pandemic: an ESTRO-ASTRO consensus statement. Radiother Oncol. 2020;147:227–228. doi: 10.1016/j.radonc.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yahalom J, Dabaja BS, Ricardi U, et al. ILROG emergency guidelines for radiation therapy of hematological malignancies during the Covid-19 pandemic. Blood. 2020;135:1829–1832. doi: 10.1182/blood.2020006028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Huang SH, O’Sullivan B, Su J, et al. Hypofractionated radiotherapy alone with 2.4 Gy per fraction for head and neck cancer during the Covid-19 pandemic: the Princess Margaret experience and proposal. Cancer. 2020;126:3426–3437. doi: 10.1002/cncr.32968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Alterio D, Volpe S, Marvaso G, et al. Head and neck cancer radiotherapy amid Covid-19 pandemic: report from Milan, Italy. Head Neck. 2020;42:1482–1490. doi: 10.1002/hed.26319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.De Felice F, D’Angelo E, Ingargiola R, et al. A snapshot on radiotherapy for head and neck cancer patients during the Covid-19 pandemic: a survey of the Italian association of radiotherapy and clinical oncology (AIRO) head and neck working group. Radiol Med. 2021;126:343–347. doi: 10.1007/s11547-020-01296-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Alterio D, Volpe S, Bacigalupo A, et al. Head and neck radiotherapy amid the Covid-19 pandemic: practice recommendations of the Italian association of radiotherapy and clinical oncology (AIRO) Med Oncol. 2020;37:85. doi: 10.1007/s12032-020-01409-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gupta T, Ghosh-Laskar S, Agarwal JP. Resource-sparing curative-intent hypofractionated-accelerated radiotherapy in head and neck cancer: More relevant than ever before in the COVID era. Oral Oncol. 2020;111:105045. doi: 10.1016/j.oraloncology.2020.105045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kang JJ, Wong RJ, Sherman EJ, et al. The 3 Bs of cancer care amid the Covid-19 pandemic crisis: “be safe, be smart, be kind”-a multidisciplinary approach increasing the use of radiation and embracing telemedicine for head and neck cancer. Cancer. 2020;126:4092–4104. doi: 10.1002/cncr.33031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ding Y, Ma P, Li W, et al. Effect of surgical mask on setup error in head and neck radiotherapy. Technol Cancer Res Treat. 2020;19:1533033820974021. doi: 10.1177/1533033820974021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yanagihara TK, Holland RE, Chera B. Practical Challenges of mask-to-mask encounters with patients with head and neck cancers amid the coronavirus disease 2019 pandemic. Adv Radiat Oncol. 2020;5:651–655. doi: 10.1016/j.adro.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang Y-M, Hsieh Y-W, Huang B-S, et al. Medical mask wearing during treatment for patients undergoing radiotherapy in Covid-19 pandemic - an experience of protocol setup and dosimetric evaluation for particle/proton beam therapy. Risk Manag Healthc Policy. 2021;14:869–873. doi: 10.2147/RMHP.S286404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rocha BA, Mendes PA, Lima LMC, et al. Why it is crucial to maintain oral care for patients undergoing head and neck radiotherapy during the Covid-19 pandemic. J Stomatol Oral Maxillofac Surg. 2021;122:223–224. doi: 10.1016/j.jormas.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dee EC, Mahal BA, Arega MA, et al. Relative timing of radiotherapy and androgen deprivation for prostate cancer and implications for treatment during the Covid-19 pandemic. JAMA Oncol. 2020;6:1630–1632. doi: 10.1001/jamaoncol.2020.3545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Detti B, Ingrosso G, Becherini C, et al. Management of prostate cancer radiotherapy during the Covid-19 pandemic: a necessary paradigm change. Cancer Treat Res Commun. 2021;27:100331. doi: 10.1016/j.ctarc.2021.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zaorsky NG, Yu JB, McBride SM, et al. Prostate cancer radiation therapy recommendations in response to Covid-19. Adv Radiat Oncol. 2020;5:26–32. doi: 10.1016/j.adro.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Barra S, Guarnieri A, di Monale E, Bastia MB, et al. Short fractionation radiotherapy for early prostate cancer in the time of Covid-19: long-term excellent outcomes from a multicenter Italian trial suggest a larger adoption in clinical practice. Radiol Med. 2021;126:142–146. doi: 10.1007/s11547-020-01216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ling DC, Vargo JA, Beriwal S. Breast, prostate, and rectal cancer: should 5–5-5 be a new standard of care? Int J Radiat Oncol Biol Phys. 2020;108:390–393. doi: 10.1016/j.ijrobp.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Murakami N, Nakamura S, Kashihara T, et al. Increased number of prostate cancer patients selecting high dose-rate interstitial brachytherapy during the Covid-19 pandemic. Radiother Oncol. 2021;154:274–275. doi: 10.1016/j.radonc.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lewis S, Talapatra K. Radiotherapy management of rectal cancer in the backdrop of the COVID pandemic. Cancer Rep (Hoboken) 2021;4:e1320. doi: 10.1002/cnr2.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tchelebi LT, Haustermans K, Scorsetti M, et al. Recommendations for the use of radiation therapy in managing patients with gastrointestinal malignancies in the era of Covid-19. Radiother Oncol. 2020;148:194–200. doi: 10.1016/j.radonc.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Inchingolo R, Acquafredda F, Tedeschi M, et al. Worldwide management of hepatocellular carcinoma during the Covid-19 pandemic. World J Gastroenterol. 2021;27:3780–3789. doi: 10.3748/wjg.v27.i25.3780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cellini F, Gambacorta MA, Mattiucci GC, Valentini V. Role of neoadjuvant radiochemotherapy for esophageal cancers over pre/peri-operative chemotherapy in the era of Covid-19 and beyond. Radiother Oncol. 2021;154:e15–e16. doi: 10.1016/j.radonc.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tchelebi LT, Goodman K. Response to, “Role of neoadjuvant radiochemotherapy for esophageal cancers over pre/peri-operative chemotherapy in the era of Covid-19 and beyond”. Radiother Oncol. 2021;154:e17. doi: 10.1016/j.radonc.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Marijnen CAM, Peters FP, Rödel C, et al. International expert consensus statement regarding radiotherapy treatment options for rectal cancer during the COVID 19 pandemic. Radiother Oncol. 2020;148:213–215. doi: 10.1016/j.radonc.2020.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Scorsetti M, Goodman KA, Seong J, et al. Hepatocellular carcinoma in the Covid-19 era: primetime for stereotactic body radiotherapy and a lesson for the future? Oncologist. 2020;25:e1249–e1250. doi: 10.1634/theoncologist.2020-0416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Denaro N, Merlotti AM, Merlano MC, Russi E. Coronavirus disease 19 (Covid-19) during chemoradiation for locally advanced oropharyngeal squamous cell carcinoma (LA-OPSCC) Oral Oncol. 2020;107:104801. doi: 10.1016/j.oraloncology.2020.104801. [DOI] [PubMed] [Google Scholar]
- 108.Aitken K, Good J, Hawkins M, et al. Liver stereotactic ablative radiotherapy: an effective and feasible alternative to surgery during the Covid-19 pandemic. Clin Oncol (R Coll Radiol) 2020;32:477. doi: 10.1016/j.clon.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Barcellini A, Vitolo V, Cobianchi L, et al. Pancreatic cancer: does a short course of carbon ion radiotherapy worth during Covid-19 outbreak? Pancreatology. 2020;20:1004–1005. doi: 10.1016/j.pan.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mirnezami R, Knowles J, Kar A, Glynne-Jones R. Preoperative radiotherapy for locally advanced rectal cancer during and after the Covid-19 pandemic. Br J Surg. 2020;107:e263. doi: 10.1002/bjs.11725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Li Z, Li Q, Wang X, et al. Carbon ion radiotherapy acts as the optimal treatment strategy for unresectable liver cancer during the coronavirus disease 2019 crisis. Front Public Health. 2021;9:767617. doi: 10.3389/fpubh.2021.767617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rembielak A, Sykes AJ, Fife K, et al. Radiotherapy and systemic treatment for non-melanoma skin cancer in the Covid-19 pandemic. Clin Oncol (R Coll Radiol) 2020;32:417–419. doi: 10.1016/j.clon.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Baumann BC, MacArthur KM, Brewer JD, et al. Management of primary skin cancer during a pandemic: multidisciplinary recommendations. Cancer. 2020;126:3900–3906. doi: 10.1002/cncr.32969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Veness MJ. Hypofractionated radiotherapy in patients with non-melanoma skin cancer in the post Covid-19 era: time to reconsider its role for most patients. J Med Imaging Radiat Oncol. 2020;64:591–594. doi: 10.1111/1754-9485.13070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lancellotta V, D’Aviero A, Fionda B, et al. Contact skin radiotherapy (brachytherapy) for the treatment of non-melanoma skin cancers during Covid-19 pandemic. Dermatol Ther. 2021 doi: 10.1111/dth.15276. [DOI] [PubMed] [Google Scholar]
- 116.Spigariolo CB, Piccinno R. Phototherapy and dermatologic radiotherapy during the Covid-19 emergency: the experience from the frontline of Milan. Photodermatol Photoimmunol Photomed. 2021 doi: 10.1111/phpp.12762. [DOI] [PubMed] [Google Scholar]
- 117.Palumbo I, Borghesi S, Gregucci F, et al. Omission of adjuvant radiotherapy for older adults with early-stage breast cancer particularly in the COVID era: a literature review (on the behalf of Italian association of radiotherapy and clinical oncology) J Geriatr Oncol. 2021;12:1130–1135. doi: 10.1016/j.jgo.2021.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Grellier N, Hadhri A, Bendavid J, et al. Regional lymph node irradiation in breast cancer may worsen lung damage in coronavirus disease 2019 positive patients. Adv Radiat Oncol. 2020;5:722–726. doi: 10.1016/j.adro.2020.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Machiels M, Weytjens R, Bauwens W, et al. Accelerated adaptation of ultrahypofractionated radiation therapy for breast cancer at the time of the Covid-19 Pandemic. Clin Oncol (R Coll Radiol) 2021;33:e166–e171. doi: 10.1016/j.clon.2020.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hanumanthappa N, Goldsmith C, Sawyer E, et al. Adjuvant breast radiotherapy at an academic center during the Covid-19 pandemic: reassuringly safe. Clin Oncol (R Coll Radiol) 2021;33:e221. doi: 10.1016/j.clon.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Montagna E, Bellerba F, Sangalli C, et al. Management of breast cancer patients during the peak of the COVID 19 pandemic. Eur J Surg Oncol. 2021;47:2694–2695. doi: 10.1016/j.ejso.2021.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Spałek MJ, Rutkowski P. Coronavirus disease (Covid-19) outbreak: hypofractionated radiotherapy in soft tissue sarcomas as a valuable option in the environment of limited medical resources and demands for increased protection of patients. Front Oncol. 2020;10:993. doi: 10.3389/fonc.2020.00993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Elledge CR, Beriwal S, Chargari C, et al. Radiation therapy for gynecologic malignancies during the Covid-19 pandemic: International expert consensus recommendations. Gynecol Oncol. 2020;158:244–253. doi: 10.1016/j.ygyno.2020.06.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Matsuo K, Shimada M, Matsuzaki S, et al. Wait-time for adjuvant radiotherapy and oncologic outcome in early-stage cervical cancer: a treatment implication during the coronavirus pandemic. Eur J Cancer. 2021;148:117–120. doi: 10.1016/j.ejca.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Vavassori A, Tagliaferri L, Vicenzi L, et al. Practical indications for management of patients candidate to interventional and intraoperative radiotherapy (brachytherapy, IORT) during Covid-19 pandemic - a document endorsed by AIRO (Italian association of radiotherapy and clinical oncology) interventional radiotherapy working group. Radiother Oncol. 2020;149:73–77. doi: 10.1016/j.radonc.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Brunnhoelzl D, Hanania AN, Echeverria A, et al. Paracervical blocks facilitate timely brachytherapy amidst Covid-19. Brachytherapy. 2021;20:284–289. doi: 10.1016/j.brachy.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Williams VM, Kahn JM, Harkenrider MM, et al. Covid-19 impact on timing of brachytherapy treatment and strategies for risk mitigation. Brachytherapy. 2020;19:401–411. doi: 10.1016/j.brachy.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Jiang Y, Li G, Xing B, et al. Brachytherapy care during the Covid-19 pandemic: practice statement from a cancer center in Wuhan, China. Brachytherapy. 2021;20:279–283. doi: 10.1016/j.brachy.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Miriyala R, Mahantshetty U. Brachytherapy in cervical cancer radiotherapy during Covid-19 pandemic crisis: problems and prospects. J Contemp Brachytherapy. 2020;12:290–293. doi: 10.5114/jcb.2020.96873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Aghili M, Jafari F, Vand Rajabpoor M. Brachytherapy during the coronavirus disease 2019 - lessons from Iran. Brachytherapy. 2020;19:412–414. doi: 10.1016/j.brachy.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kumar D, Dey T. Recapitulating intracavitary brachytherapy in cervical cancer patients during the Covid-19 pandemic: a viewpoint. Future Oncol. 2020;16:2143–2146. doi: 10.2217/fon-2020-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nieder C, Haukland EC, Mannsaker B, Yobuta R. Palliative radiotherapy during the last month of life: have Covid-19 recommendations led to reduced utilization? In Vivo. 2021;35:649–652. doi: 10.21873/invivo.12304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Cellini F, Di Franco R, Manfrida S, et al. Palliative radiotherapy indications during the Covid-19 pandemic and in future complex logistic settings: the NORMALITY model. Radiol Med. 2021;126:1619–1656. doi: 10.1007/s11547-021-01414-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Thureau S, Faivre JC, Assaker R, et al. Adapting palliative radiation therapy for bone metastases during the Covid-19 pandemic: GEMO position paper. J Bone Oncol. 2020;22:100291. doi: 10.1016/j.jbo.2020.100291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jacobson G, Kaidar-Person O, Haisraely O, et al. Palliative radiation therapy for symptomatic advance breast cancer. Sci Rep. 2021;11:5282. doi: 10.1038/s41598-021-84872-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yerramilli D, Xu AJ, Gillespie EF, et al. Palliative radiation therapy for oncologic emergencies in the setting of Covid-19: approaches to balancing risks and benefits. Adv Radiat Oncol. 2020;5:589–594. doi: 10.1016/j.adro.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Crisà FM, Leocata F, Arienti VM, et al. Gamma knife radiosurgery for treatment of brain metastases during the Covid-19 outbreak. Stereotact Funct Neurosurg. 2020;98:319–323. doi: 10.1159/000510271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Miura H, Hioki K, Ozawa S, et al. Uncertainty in the positioning of patients receiving treatment for brain metastases and wearing surgical mask underneath thermoplastic mask during Covid-19 crisis. J Appl Clin Med Phys. 2021;22:274–280. doi: 10.1002/acm2.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rinaldi CG, Ippolito E, Greco C, et al. Radiotherapy for pain relief from bone metastases during coronavirus (Covid-19) pandemic. Eur J Pain. 2020;24:1211–1212. doi: 10.1002/ejp.1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chufal KS, Ahmad I, Chowdhary RL. Palliative stereotactic radiotherapy for metastases during Covid-19: relief when cure is implausible. BMJ Support Palliat Care. 2021 doi: 10.1136/bmjspcare-2020-002758. [DOI] [PubMed] [Google Scholar]
- 141.Rödel F, Arenas M, Ott OJ, et al. Low-dose radiation therapy for Covid-19 pneumopathy: what is the evidence? Strahlenther Onkol. 2020;196:679–682. doi: 10.1007/s00066-020-01635-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Del Castillo R, Martinez D, Sarria GJ, et al. Low-dose radiotherapy for Covid-19 pneumonia treatment: case report, procedure, and literature review. Strahlenther Onkol. 2020;196:1086–1093. doi: 10.1007/s00066-020-01675-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Dhawan G, Kapoor R, Dhawan R, et al. Low dose radiation therapy as a potential lifesaving treatment for Covid-19-induced acute respiratory distress syndrome (ARDS) Radiother Oncol. 2020;147:212–216. doi: 10.1016/j.radonc.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Prasanna PG, Woloschak GE, DiCarlo AL, et al. Low-dose radiation therapy (LDRT) for Covid-19: benefits or risks? Radiat Res. 2020;194:452–464. doi: 10.1667/RADE-20-00211.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lara PC, Burgos J, Macias D. Low dose lung radiotherapy for Covid-19 pneumonia. the rationale for a cost-effective anti-inflammatory treatment. Clin Transl Radiat Oncol. 2020;23:27–29. doi: 10.1016/j.ctro.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Salomaa S, Bouffler SD, Atkinson MJ, et al. Is there any supportive evidence for low dose radiotherapy for Covid-19 pneumonia? Int J Radiat Biol. 2020;96:1228–1235. doi: 10.1080/09553002.2020.1786609. [DOI] [PubMed] [Google Scholar]
- 147.Ameri A, Rahnama N, Bozorgmehr R, et al. Low-dose whole-lung irradiation for Covid-19 pneumonia: short course results. Int J Radiat Oncol Biol Phys. 2020;108:1134–1139. doi: 10.1016/j.ijrobp.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Nasir A, Agrawal D, Pathak J, Theodoulou I. Low-dose X-ray therapy for Covid-19: lessons from the past. Br J Radiol. 2021;94:20200581. doi: 10.1259/bjr.20200581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Montero A, Arenas M, Algara M. Low-dose radiation therapy: could it be a game-changer for Covid-19? Clin Transl Oncol. 2021;23:1–4. doi: 10.1007/s12094-020-02401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sanmamed N, Alcantara P, Cerezo E, et al. Low-dose radiation therapy in the management of coronavirus disease 2019 (Covid-19) pneumonia (LOWRAD-Cov19): preliminary report. Int J Radiat Oncol Biol Phys. 2021;109:880–885. doi: 10.1016/j.ijrobp.2020.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ameri A, Ameri P, Rahnama N, et al. Low-dose whole-lung irradiation for Covid-19 pneumonia: final results of a pilot study. Int J Radiat Oncol Biol Phys. 2021;109:859–866. doi: 10.1016/j.ijrobp.2020.11.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hanna CR, Robb KA, Blyth KG, et al. Clinician attitudes to using low-dose radiation therapy to treat Covid-19 lung disease. Int J Radiat Oncol Biol Phys. 2021;109:886–890. doi: 10.1016/j.ijrobp.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Koosha F, Pourbagheri-Sigaroodi A, Bakhshandeh M, Bashash D. Low-dose radiotherapy (LD-RT) for Covid-19-induced pneumopathy: a worth considering approach. Int J Radiat Biol. 2021;97:302–312. doi: 10.1080/09553002.2021.1864049. [DOI] [PubMed] [Google Scholar]
- 154.Hess CB, Nasti TH, Dhere VR, et al. Immunomodulatory low-dose whole-lung radiation for patients with coronavirus disease 2019-related pneumonia. Int J Radiat Oncol Biol Phys. 2021;109:867–879. doi: 10.1016/j.ijrobp.2020.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Schaue D, McBride WH. Flying by the seat of our pants: is low dose radiation therapy for Covid-19 an option? Int J Radiat Biol. 2020;96:1219–1223. doi: 10.1080/09553002.2020.1767314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kumar R, Haresh KP, Sharma DN, et al. Low-dose radiotherapy for COVID 19: a radioimmunological perspective. J Cancer Res Ther. 2021;17:295–302. doi: 10.4103/jcrt.JCRT_1045_20. [DOI] [PubMed] [Google Scholar]
- 157.Wilson GD, Mehta MP, Welsh JS, et al. Investigating low-dose thoracic radiation as a treatment for Covid-19 patients to prevent respiratory failure. Radiat Res. 2020;194:1–8. doi: 10.1667/RADE-20-00108.1. [DOI] [PubMed] [Google Scholar]
- 158.Li JJ. Mitigating coronavirus-induced acute respiratory distress syndrome by radiotherapy. iScience. 2020;23:101215. doi: 10.1016/j.isci.2020.101215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Moreno-Olmedo E, Suárez-Gironzini V, Pérez M, et al. Covid-19 pneumonia treated with ultra-low doses of radiotherapy (ULTRA-COVID study): a single institution report of two cases. Strahlenther Onkol. 2021;197:429–437. doi: 10.1007/s00066-020-01743-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bonet M, Vázquez S, García E, et al. Saving time in the radiotherapy procedures for Covid-19 pneumonia treatment. a single-institution experience. Clin Transl Oncol. 2021;23:2344–2349. doi: 10.1007/s12094-021-02634-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Algara M, Arenas M, Marin J, et al. Low dose anti-inflammatory radiotherapy for the treatment of pneumonia by Covid-19: a proposal for a multi-centric prospective trial. Clin Transl Radiat Oncol. 2020;24:29–33. doi: 10.1016/j.ctro.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hanekamp YN, Giordano J, Hanekamp JC, et al. Immunomodulation through low-dose radiation for severe Covid-19: lessons from the past and new developments. Dose Response. 2020;18:1559325820956800. doi: 10.1177/1559325820956800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Meziani L, Robert C, Classe M, et al. Low doses of radiation increase the immunosuppressive profile of lung macrophages during viral infection and pneumonia. Int J Radiat Oncol Biol Phys. 2021;110:1283–1294. doi: 10.1016/j.ijrobp.2021.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gupta S, Ahuja R, Sharma N, et al. Low dose lung radiotherapy for Covid-19 pneumonia: a potential treatment. Respir Med. 2021;186:106531. doi: 10.1016/j.rmed.2021.106531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Abdollahi H, Shiri I, Bevelacqua JJ, et al. Low dose radiation therapy and convalescent plasma: how a hybrid method may maximize benefits for Covid-19 patients. J Biomed Phys Eng. 2020;10:387–394. doi: 10.31661/jbpe.v0i0.2006-1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Papachristofilou A, Finazzi T, Blum A, et al. Low-dose radiation therapy for severe Covid-19 pneumonia: a randomized double-blind study. Int J Radiat Oncol Biol Phys. 2021;110:1274–1282. doi: 10.1016/j.ijrobp.2021.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lara PC, Nguyen NP, Macias-Verde D, et al. Whole-lung low dose irradiation for SARS-Cov2 induced pneumonia in the geriatric population: an old effective treatment for a new disease? Recommendation of the international geriatric radiotherapy group. Aging Dis. 2020;11:489–493. doi: 10.14336/AD.2020.0506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Cuttler JM, Bevelacqua JJ, Mortazavi SMJ. Unethical not to investigate radiotherapy for Covid-19. Dose Response. 2020;18:1559325820950104. doi: 10.1177/1559325820950104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hadjiyiannakis D, Dimitroyannis D, Eastlake L, et al. Personal view: low-dose lung radiotherapy should be evaluated as a treatment for severe Covid-19 lung disease. Clin Oncol (R Coll Radiol) 2021;33:e64–e68. doi: 10.1016/j.clon.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Hess CB, Eng TY, Nasti TH, et al. Whole-lung low-dose radiation therapy (LD-RT) for non-intubated oxygen-dependent patients with Covid-19-related pneumonia receiving dexamethasone and/or remdesevir. Radiother Oncol. 2021;165:20–31. doi: 10.1016/j.radonc.2021.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yu J, Azzam EI, Jadhav AB, Wang Y. Covid-19: the disease, the immunological challenges, the treatment with pharmaceuticals and low-dose ionizing radiation. Cells. 2021;10:2212. doi: 10.3390/cells10092212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ghaznavi H. Effectiveness of low-dose radiation therapy to improve mortality of Covid-19. J Cancer Res Clin Oncol. 2021;147:2621–2624. doi: 10.1007/s00432-021-03707-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sharma DN, Guleria R, Wig N, et al. Low-dose radiation therapy for Covid-19 pneumonia: a pilot study. Br J Radiol. 2021;94:20210187. doi: 10.1259/bjr.20210187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Arenas M, Algara M, De Febrer G, et al. Could pulmonary low-dose radiation therapy be an alternative treatment for patients with Covid-19 pneumonia? Preliminary results of a multicenter SEOR-GICOR nonrandomized prospective trial (IPACOVID trial) Strahlenther Onkol. 2021;197:1010–1020. doi: 10.1007/s00066-021-01803-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kapoor R, Welsh JS, Dhawan V, et al. Low-dose radiation therapy (LDRT) for Covid-19 and its deadlier variants. Arch Toxicol. 2021;95:3425–3432. doi: 10.1007/s00204-021-03124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ganesan G, Ponniah S, Sundaram V, et al. Whole lung irradiation as a novel treatment for Covid-19: interim results of an ongoing phase 2 trial in India. Radiother Oncol. 2021;163:83–90. doi: 10.1016/j.radonc.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Dunlap NE, van Berkel V, Cai L. Covid-19 and low-dose radiation therapy. Radiat Med Prot. 2021;2:139–145. doi: 10.1016/j.radmp.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Mousavi Darzikolaee N, Kolahdouzan K, Abtahi H, et al. Low-dose whole-lung irradiation in severe Covid-19 pneumonia: a controlled clinical trial. J Med Radiat Sci. 2021;68:396–406. doi: 10.1002/jmrs.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ganesan G, Ponniah S, Sundaram V, et al. Whole lung irradiation as a novel treatment for Covid-19: final results of the prospective randomized trial (WINCOVID trial) Radiother Oncol. 2021;167:133–142. doi: 10.1016/j.radonc.2021.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Roa D, Moyses H, Leon S, et al. Rationale for using a C-arm fluoroscope to deliver a kilo voltage radiotherapy treatment to Covid-19 patients. Med Dosim. 2021;46:1–2. doi: 10.1016/j.meddos.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Chakrabarti D, Verma M. Low-dose radiotherapy for SARS-CoV-2 pneumonia. Strahlenther Onkol. 2020;196:736–737. doi: 10.1007/s00066-020-01634-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Corry PM, Griffin RJ. A radiation mitigator as a potential treatment for Covid-19. Radiat Res. 2020;193:505. doi: 10.1667/RADE-20-000PC. [DOI] [PubMed] [Google Scholar]
- 183.Kefayat A, Ghahremani F. Low dose radiation therapy for Covid-19 pneumonia: a double-edged sword. Radiother Oncol. 2020;147:224–225. doi: 10.1016/j.radonc.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Beddok A, Chevrier M, Calugaru V, et al. Acute and late toxicities of patients infected with SARS-CoV-2 and treated for cancer with radiation therapy during the Covid-19 pandemic. Int J Radiat Biol. 2021;97:1436–1440. doi: 10.1080/09553002.2021.1956008. [DOI] [PubMed] [Google Scholar]
- 185.Ning MS, McAleer MF, Jeter MD, et al. Mitigating the impact of Covid-19 on oncology: clinical and operational lessons from a prospective radiation oncology cohort tested for Covid-19. Radiother Oncol. 2020;148:252–257. doi: 10.1016/j.radonc.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Stepanović A, Arsenijevic T, Stankovic V, et al. Clinical analysis of Covid-19 positive cancer inpatients in national cancer center in Serbia. J Infect Dev Ctries. 2021;15:1286–1292. doi: 10.3855/jidc.15104. [DOI] [PubMed] [Google Scholar]
- 187.LaPlant Q, Thor M, Shaverdian N, et al. Association of prior radiation dose to the cardiopulmonary system with Covid-19 outcomes in patients with cancer. Radiother Oncol. 2021;161:115–117. doi: 10.1016/j.radonc.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Allali S, Servois V, Beddok A, et al. Evaluation of the early adverse effects of radiotherapy in breast cancer patients with Covid-19: prospective single institutional study. Breast J. 2021;27:824–827. doi: 10.1111/tbj.14282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Weltman E, Kotecha R. Early-onset symptomatic radiation necrosis after stereotactic radiosurgery in the setting of Covid-19 infection. Med Dosim. 2021;46:374–376. doi: 10.1016/j.meddos.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.García-Hernández T, Romero-Expósito M, Sánchez-Nieto B. Low dose radiation therapy for Covid-19: effective dose and estimation of cancer risk. Radiother Oncol. 2020;153:289–295. doi: 10.1016/j.radonc.2020.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Arruda GV, Weber RRDS, Bruno AC, Pavoni JF. The risk of induced cancer and ischemic heart disease following low dose lung irradiation for Covid-19: estimation based on a virtual case. Int J Radiat Biol. 2021;97:120–125. doi: 10.1080/09553002.2021.1846818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Shuryak I, Kachnic LA, Brenner DJ. Lung cancer and heart disease risks associated with low-dose pulmonary radiotherapy to Covid-19 patients with different background risks. Int J Radiat Oncol Biol Phys. 2021;111:233–239. doi: 10.1016/j.ijrobp.2021.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Little MP, Zhang W, van Dusen R, Hamada N. Pneumonia after bacterial or viral infection preceded or followed by radiation exposure: a reanalysis of older radio biologic data and implications for low-dose radiation therapy for coronavirus disease 2019 pneumonia. Int J Radiat Oncol Biol Phys. 2021;109:849–858. doi: 10.1016/j.ijrobp.2020.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Joseph N, Choudhury A. Lymphocytopenia and radiotherapy treatment volumes in the time of Covid-19. Clin Oncol (R Coll Radiol) 2020;32:420–422. doi: 10.1016/j.clon.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Wei W, Zheng D, Lei Y, et al. Radiotherapy workflow and protection procedures during the coronavirus disease 2019 (Covid-19) outbreak: experience of the Hubei cancer hospital in Wuhan, China. Radiother Oncol. 2020;148:203–210. doi: 10.1016/j.radonc.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wang W, Hu K, Qiu J, Zhang F. Radiotherapy after the easing of public restrictions during Covid-19 epidemic. Radiat Oncol. 2020;15:166. doi: 10.1186/s13014-020-01612-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Pezzulla D, Macchia G, Taccari F, et al. Radiotherapy in Southern Italy at the time of Covid-19: options for radiation oncology units. Int J Gynecol Cancer. 2020;30:917–919. doi: 10.1136/ijgc-2020-001523. [DOI] [PubMed] [Google Scholar]
- 198.Montesi G, Di Biase S, Chierchini S, et al. Radiotherapy during Covid-19 pandemic. how to create a no fly zone: a Northern Italy experience. Radiol Med. 2020;125:600–603. doi: 10.1007/s11547-020-01217-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Wang W, Liu X, Zhang F, et al. Radiation therapy during the Covid-19 pandemic: experience from Beijing, China. In Vivo. 2020;34:1675–1680. doi: 10.21873/invivo.11960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Mohindra P, Buckey CR, Chen S, et al. Radiation therapy considerations during the Covid-19 pandemic: literature review and expert opinions. J Appl Clin Med Phys. 2020;21:6–12. doi: 10.1002/acm2.12898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Viscariello N, Evans S, Parker S, et al. A multi-institutional assessment of Covid-19-related risk in radiation oncology. Radiother Oncol. 2020;153:296–302. doi: 10.1016/j.radonc.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Deantonio L, Bosetti D, Cima S, et al. #Stayathome: smart working for radiation oncologists during the corona pandemic. Strahlenther Onkol. 2020;196:1094–1095. doi: 10.1007/s00066-020-01683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Hasford F, Sosu EK, Awua AK, et al. Knowledge and perception on the transmission and control of SARS-COV-2 infection among allied radiation medicine professionals in Ghana. Health Technol (Berl) 2020 doi: 10.1007/s12553-020-00507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Wei W, Jiang H, Chen W, et al. How should we implement radiotherapy for cancer patients in China during the endemic period of Covid-19? Radiother Oncol. 2020;147:100–102. doi: 10.1016/j.radonc.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Tamari K, Nagata Y, Nishiki S, et al. Nationwide survey of Covid-19 prevention measures in Japanese radiotherapy departments via online questionnaire for radiation oncologists. Radiother Oncol. 2020;149:219–221. doi: 10.1016/j.radonc.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Kearney M, Coffey M, Rossi M, et al. Future-proof Radiation therapist (RTT) practice in a pandemic - lessons learnt from Covid-19. Tech Innov Patient Support Radiat Oncol. 2021;17:18–24. doi: 10.1016/j.tipsro.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zhang D, Li T, Wang P, et al. Experts consensus on epidemic prevention and control in radiotherapy centers during the Covid-19 outbreak: experiences from Sichuan Province. Clin Transl Radiat Oncol. 2020;24:88–91. doi: 10.1016/j.ctro.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Jereczek-Fossa BA, Palazzi MF, Tonoli S, et al. Almost one year of Covid-19 pandemic: how radiotherapy centers have counteracted its impact on cancer treatment in Lombardy. Italy CODRAL/AIRO-L study Tumori. 2021 doi: 10.1177/03008916211009974. [DOI] [PubMed] [Google Scholar]
- 209.Donkor A, Atuwo-Ampoh VD, Opie C, et al. Novel coronavirus mitigation measures implemented by radiotherapy centers in low and middle-income countries: a systematic review. Rep Pract Oncol Radiother. 2021;26:303–315. doi: 10.5603/RPOR.a2021.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhang L, Zheng Z, Hu G, Yuan X. Prevention and control measure to avoid cross infection during radiotherapy in coronavirus disease 2019 (Covid-19) epidemic in Wuhan, China. Radiother Oncol. 2020;149:104–106. doi: 10.1016/j.radonc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Tsang Y, Duffton A, Leech M, et al. Meeting the challenges imposed by Covid-19: guidance document by the ESTRO radiation therapist committee (RTTC) Tech Innov Patient Support Radiat Oncol. 2020;15:6–10. doi: 10.1016/j.tipsro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Jan I, Chen K, Sayan M, et al. Prevalence of surface contamination with SARS-CoV-2 in a radiation oncology clinic. JAMA Oncol. 2020;6:1632–1634. doi: 10.1001/jamaoncol.2020.3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Gonnelli A, Montrone S, Cocuzza P, et al. Radiotherapy in the Covid-19 pandemic era. In Vivo. 2020;34:3731–3734. doi: 10.21873/invivo.12222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Di Lalla V, Patrick H, Siriani-Ayoub N, et al. Satisfaction among cancer patients undergoing radiotherapy during the Covid-19 pandemic: an institutional experience. Curr Oncol. 2021;28:1507–1517. doi: 10.3390/curroncol28020142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Lian X, Shen J, Sun Y, et al. Under the coronavirus disease 2019 (Covid-19) pandemic circumstance, how to administrate cancer patients with fever during radiotherapy. Radiother Oncol. 2020;150:15–17. doi: 10.1016/j.radonc.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sachan A, Gupta S, Ghosh A, Singh N. Catering the needs of cancer contemporary to this contagious corona catastrophe: institution based changes in cancer management and protection procedures. J Biomed Phys Eng. 2021;11:403–406. doi: 10.31661/jbpe.v0i0.2011-1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Matuschek C, Fischer JC, Combs SE, et al. Measures of infection prevention and incidence of SARS-CoV-2 infections in cancer patients undergoing radiotherapy in Germany, Austria and Switzerland. Strahlenther Onkol. 2020;196:1068–1079. doi: 10.1007/s00066-020-01681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Kurosaki H, Utsumi N, Miura K. A case of suspected radiation recall pneumonitis After a Covid-19 infection. Cureus. 2021;13:e13688. doi: 10.7759/cureus.13688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Cella L, Gagliardi G, Hedman M, Palma G. Injuries from asymptomatic Covid-19 disease: new hidden toxicity risk factors in thoracic radiation therapy. Int J Radiat Oncol Biol Phys. 2020;108:394–396. doi: 10.1016/j.ijrobp.2020.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lazzari G, Silvano G. RILI model and the Covid-19 pneumonia: the radiation oncologist point of view. Radiother Oncol. 2020;147:222–223. doi: 10.1016/j.radonc.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Kirkby C, Mackenzie M. Response to: RILI model and the Covid-19 pneumonia: the radiation oncologist point of view. Radiother Oncol. 2020;149:72. doi: 10.1016/j.radonc.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Boon IS, Au Yong TPT, Boon CS. Radiotherapy for Covid-19: primum non nocere. Radiother Oncol. 2020;149:236–237. doi: 10.1016/j.radonc.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Soyfer V, Gutfeld O, Shamai S, et al. Covid-19 vaccine-induced radiation recall phenomenon. Int J Radiat Oncol Biol Phys. 2021;110:957–961. doi: 10.1016/j.ijrobp.2021.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Scoccianti S, Delli Paoli C, Grilli Leonulli B, et al. Acute tolerance of moderna mRNA-1273 vaccine against Covid-19 in patients with cancer treated with radiotherapy. Lancet Oncol. 2021;22:1212–1214. doi: 10.1016/S1470-2045(21)00427-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Steber CR, Ponnatapura J, Hughes RT, Farris MK. Rapid Development of clinically symptomatic radiation recall pneumonitis immediately following Covid-19 vaccination. Cureus. 2021;13:e14303. doi: 10.7759/cureus.14303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Afacan E, Öğüt B, Üstün P, et al. Radiation recall dermatitis triggered by inactivated Covid-19 vaccine. Clin Exp Dermatol. 2021;46:1582–1584. doi: 10.1111/ced.14786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Sun R, Achkar S, Ammari S, et al. Systematic screening of Covid-19 disease based on chest CT and RT-PCR for cancer patients undergoing radiation therapy in a coronavirus French hotspot. Int J Radiat Oncol Biol Phys. 2021;110:947–956. doi: 10.1016/j.ijrobp.2021.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.McGinnis GJ, Ning MS, Nitsch PL, et al. Rapid detection of asymptomatic coronavirus disease 2019 by computed tomography image guidance for stereotactic ablative radiotherapy. J Thorac Oncol. 2020;15:1085–1087. doi: 10.1016/j.jtho.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Warren GW, Lim V-S, Chowdhary M, et al. New pulmonary infiltrates observed on computed tomography-based image guidance for radiotherapy warrant diagnostic workup for coronavirus disease 2019. J Thorac Oncol. 2021;16:1946–1951. doi: 10.1016/j.jtho.2021.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Suppli MH, Riisgaard de Blanck S, Elgaard T, et al. Early appearance of coronavirus disease 2019 associated pulmonary infiltrates during daily radiotherapy imaging for lung cancer. J Thorac Oncol. 2020;15:1081–1084. doi: 10.1016/j.jtho.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Prabhu RS, Dhakal R, Hicks AS, et al. Implementation, adherence, and results of systematic SARS-CoV-2 testing for asymptomatic patients treated at a tertiary care regional radiation oncology network. Radiat Oncol. 2021;16:28. doi: 10.1186/s13014-021-01760-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Zeng Q, Tang C, Deng L, et al. Differential diagnosis of Covid-19 pneumonia in cancer patients received radiotherapy. Int J Med Sci. 2020;17:2561–2569. doi: 10.7150/ijms.46133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Clough A, Sanders J, Banfill K, et al. A novel use for routine CBCT imaging during radiotherapy to detect Covid-19. Radiography (Lond) 2022;28:17–23. doi: 10.1016/j.radi.2021.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Magrini SM, Guerini AE, Borghetti P, et al. Universal testing for Covid-19 in patients undergoing cancer treatment during the second outbreak in Brescia. Tumori. 2021 doi: 10.1177/03008916211034917. [DOI] [PubMed] [Google Scholar]
- 235.Warren GW, Adjei AA. A call for rapid submission of data for aggregate review: can daily radiotherapy imaging be used as a potential screen for coronavirus disease 2019? J Thorac Oncol. 2020;15:876–877. doi: 10.1016/j.jtho.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Lazzari G, Chiara Resta E, Magli M, et al. Are there overlapping clinical features between thoracic radiotherapy side effects and Covid-19 pneumonia? Radiation pneumonitis outside the radiation ports: Three case reports. Clin Transl Radiat Oncol. 2020;25:107–111. doi: 10.1016/j.ctro.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Manca A, Bellizzi S, Gatti M, et al. Routine immediate lung assessment during CT conceived for other purposes (thoracic spine CT, simulation CT for radiotherapy, PET-CT): a costless screening and surveillance tool for lung opacities in the Covid-19 era. Disaster Med Public Health Prep. 2021;15:e38–e39. doi: 10.1017/dmp.2020.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Boldrini L, Dinapoli N, Valentini V. Radiotherapy imaging: an unexpected ally in fighting COVID 19 pandemic. Radiother Oncol. 2020;148:223–224. doi: 10.1016/j.radonc.2020.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Kinj R, Bennassi A, Romano E, et al. Detection of an asymptomatic Covid-19 patient on CBCT-imaging. Radiother Oncol. 2021;156:199–200. doi: 10.1016/j.radonc.2020.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Jereczek-Fossa BA, Pepa M, Marvaso G, et al. Covid-19 outbreak and cancer radiotherapy disruption in Italy: survey endorsed by the Italian association of radiotherapy and clinical oncology (AIRO) Radiother Oncol. 2020;149:89–93. doi: 10.1016/j.radonc.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.de Carvalho H, A, Vasconcelos KGMC, Gomes HC, Salvajoli JV, Impact of Covid-19 pandemic on a daily-based outpatient treatment routine: experience of a radiotherapy department of a tertiary public/university hospital in Brazil. Clinics (Sao Paulo) 2020;75:e2298. doi: 10.6061/clinics/2020/e2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Akuamoa-Boateng D, Wegen S, Ferdinandus J, et al. Managing patient flows in radiation oncology during the Covid-19 pandemic : reworking existing treatment designs to prevent infections at a German hot spot area university hospital. Strahlenther Onkol. 2020;196:1080–1085. doi: 10.1007/s00066-020-01698-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Martinez D, Sarria GJ, Wakefield D, et al. COVID’s impact on radiation oncology: a Latin American survey study. Int J Radiat Oncol Biol Phys. 2020;108:374–378. doi: 10.1016/j.ijrobp.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Datta NR, Datta S, Samiei M. Strategies to maximize available resources with minimum cost escalation for improving radiation therapy accessibility in the post-coronavirus disease 2019 era: an analysis for Asia. Adv Radiat Oncol. 2021;6:100565. doi: 10.1016/j.adro.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Teckie S, Koffler D, Potters L. The resilience of radiation oncology in the COVID era and beyond. Int J Radiat Oncol Biol Phys. 2020;108:364–369. doi: 10.1016/j.ijrobp.2020.06.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Leonardi MC, Montagna E, Galimberti VE, et al. Breast adjuvant radiotherapy amid the Covid-19 crisis in a hub cancer center, Lombardy, Italy. Breast Care (Basel) 2020;5:1–7. doi: 10.1159/000513227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Roberge D, Delouya G, Bohigas A, Michalowski S. Catching the wave: quantifying the impact of COVID on radiotherapy delivery. Curr Oncol. 2020;28:152–158. doi: 10.3390/curroncol28010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Spencer K, Jones CM, Girdler R, et al. The impact of the Covid-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22:309–320. doi: 10.1016/S1470-2045(20)30743-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Tramacere F, Asabella AN, Portaluri M, et al. Impact of the Covid-19 pandemic on radiotherapy supply. Radiol Res Pract. 2021;2021:5550536. doi: 10.1155/2021/5550536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Caravatta L, Rosa C, Di Sciascio MB, et al. Covid-19 and radiation oncology: the experience of a two-phase plan within a single institution in central Italy. Radiat Oncol. 2020;15:226. doi: 10.1186/s13014-020-01670-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Desideri I, Francolini G, Ciccone LP, et al. Impact of Covid-19 on patient-doctor interaction in a complex radiation therapy facility. Support Care Cancer. 2021;29:2931–2937. doi: 10.1007/s00520-020-05793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Jereczek-Fossa BA, Pepa M, Marvaso G, et al. Back to (new) normality-A CODRAL/AIRO-L survey on cancer radiotherapy in Lombardy during Italian Covid-19 phase 2. Med Oncol. 2020;37:108. doi: 10.1007/s12032-020-01434-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Nieder C, Johnsen SK, Winther AM. Symptom burden in patients treated with palliative radiotherapy before and during the Covid-19 pandemic. Anticancer Res. 2021;41:1971–1974. doi: 10.21873/anticanres.14964. [DOI] [PubMed] [Google Scholar]
- 254.Bartels MMTJ, Gal R, van der Velden JM, et al. Impact of the Covid-19 pandemic on quality of life and emotional wellbeing in patients with bone metastases treated with radiotherapy: a prospective cohort study. Clin Exp Metastasis. 2021;38:209–217. doi: 10.1007/s10585-021-10079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Francolini G, Desideri I, Stocchi G, et al. Impact of Covid-19 on workload burden of a complex radiotherapy facility. Radiol Med. 2021;126:717–721. doi: 10.1007/s11547-021-01338-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Achard V, Aebersold DM, Allal AS, et al. A national survey on radiation oncology patterns of practice in Switzerland during the Covid-19 pandemic: present changes and future perspectives. Radiother Oncol. 2020;150:1–3. doi: 10.1016/j.radonc.2020.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Wakefield DV, Sanders T, Wilson E, et al. Initial impact and operational response of radiation oncology practices to the Covid-19 pandemic in the United States, Europe, and Latin America. Int J Radiat Oncol Biol Phys. 2020;108:1402–1403. doi: 10.1016/j.ijrobp.2020.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Dhont J, Di Tella M, Dubois L, et al. Conducting research in radiation oncology remotely during the Covid-19 pandemic: coping with isolation. Clin Transl Radiat Oncol. 2020;24:53–59. doi: 10.1016/j.ctro.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Slotman BJ, Cremades V, Kirby AM, Ricardi U. European radiation oncology after one year of Covid-19 pandemic. Clin Transl Radiat Oncol. 2021;28:141–143. doi: 10.1016/j.ctro.2021.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Lewis PJ, Morris EJA, Chan CSK, et al. COVID RT - assessing the impact of Covid-19 on radiotherapy in the UK. A national cancer research institute clinical and translational radiotherapy research working group initiative in partnership with the royal college of radiologists, the society of radiographers and the institute of physics and engineering in medicine. Clin Oncol (R Coll Radiol) 2021;33:e69–e72. doi: 10.1016/j.clon.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Anacak Y, Onal C, Ozyigit G, et al. Changes in radiotherapy practice during Covid-19 outbreak in Turkey: a report from the Turkish society for radiation oncology. Radiother Oncol. 2020;150:43–45. doi: 10.1016/j.radonc.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Selvaraja VK, Gudipudib DK. Impact of the Covid-19 pandemic on work routine, practice and mental state of radiation oncologists in India: an online survey. Ecancermedicalscience. 2021;15:1165. doi: 10.3332/ecancer.2021.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Vaandering A, Ben Mustapha S, Lambrecht M, et al. Impact of the Covid-19 pandemic on patients and staff in radiation oncology departments in Belgium: a national survey. Front Oncol. 2021;11:654086. doi: 10.3389/fonc.2021.654086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Nardone V, Reginelli A, Vinciguerra C, et al. Mood disorder in cancer patients undergoing radiotherapy during the Covid-19 outbreak. Front Psychol. 2021;12:568839. doi: 10.3389/fpsyg.2021.568839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Corrao G, Bergamaschi L, Zaffaroni M, et al. Covid-19 impact in radiotherapy practice in an oncology hub: a screenshot from Lombardy, Italy. Tumori. 2021;107:498–503. doi: 10.1177/0300891620980065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.He J, Yang L, Tao Z, et al. Impact of the 2019 novel coronavirus disease (Covid-19) epidemic on radiotherapy-treated patients with cancer: a single-center descriptive study. Cancer Manag Res. 2021;13:37–43. doi: 10.2147/CMAR.S281323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Yang Y, Shen C, Hu C. Effect of Covid-19 epidemic on delay of diagnosis and treatment path for patients with nasopharyngeal carcinoma. Cancer Manag Res. 2020;12:3859–3864. doi: 10.2147/CMAR.S254093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Rades D, Narvaez CA, Schild SE, et al. Sleep disorders before and during the Covid-19 pandemic in patients assigned to adjuvant radiotherapy for breast cancer. In Vivo. 2021;35:2253–2260. doi: 10.21873/invivo.12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Herrscher H, Sauer B, Truntzer P, Robert C. Abscopal antitumor effect in a patient with melanoma and coronavirus disease 2019. Eur J Cancer. 2021;149:91–93. doi: 10.1016/j.ejca.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Galofaro E, Malizia C, Ammendolia I, et al. Covid-19 pandemic-adapted radiotherapy guidelines: are they really followed? Curr Oncol. 2021;28:3323–3330. doi: 10.3390/curroncol28050288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Xie J, Qi W, Cao L, et al. Predictors for fear of cancer recurrence in breast cancer patients referred to radiation therapy during the Covid-19 pandemic: a multi-center cross-section survey. Front Oncol. 2021;11:650766. doi: 10.3389/fonc.2021.650766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Lee S, Heo J. Covid-19 pandemic: a new cause of unplanned interruption of radiotherapy in breast cancer patients. Med Oncol. 2021;39:5. doi: 10.1007/s12032-021-01604-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Chen F, Zhan W, Xu H, et al. Changes in the psychological state of medical personnel in the department of radiotherapy at a tertiary care teaching hospital in China during the epidemic. Ann Work Expo Health. 2021;65:1004–1008. doi: 10.1093/annweh/wxab015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Malicki J, Martenka P, Dyzmann-Sroka A, et al. Impact of Covid-19 on the performance of a radiation oncology department at a major comprehensive cancer center in Poland during the first ten weeks of the epidemic. Rep Pract Oncol Radiother. 2020;25:820–827. doi: 10.1016/j.rpor.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Buglione M, Spiazzi L, Guerini AE, et al. Two months of radiation oncology in the heart of Italian “red zone” during Covid-19 pandemic: paving a safe path over thin ice. Radiat Oncol. 2020;15:191. doi: 10.1186/s13014-020-01631-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Marconi E, Chiesa S, Dinapoli L, et al. A radiotherapy staff experience of gratitude during Covid-19 pandemic. Tech Innov Patient Support Radiat Oncol. 2021;18:32–34. doi: 10.1016/j.tipsro.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Morassaei S, Di Prospero L, Ringdalen E, et al. A survey to explore the psychological impact of the Covid-19 pandemic on radiation therapists in Norway and Canada: a tale of two countries. J Med Radiat Sci. 2021;68:407–417. doi: 10.1002/jmrs.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Corrao G, Bergamaschi L, Zaffaroni M, et al. Covid-19 and radiotherapy: impact on work and personal life of Lombardy residents during first lockdown, survey endorsed by AIRO Young. Tumori. 2021 doi: 10.1177/03008916211000826. [DOI] [PubMed] [Google Scholar]
- 279.Reuter-Oppermann M, Müller-Polyzou R, Wirtz H, Georgiadis A. Influence of the pandemic dissemination of Covid-19 on radiotherapy practice: a flash survey in Germany, Austria and Switzerland. PLoS One. 2020;15:e0233330. doi: 10.1371/journal.pone.0233330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Handoko, Permata TBM, Giselvania A, et al. Ensuring safety and sustainability of radiotherapy services during the Covid-19 pandemic in resources constrain country: an Indonesian experience. Radiother Oncol. 2020;150:57–60. doi: 10.1016/j.radonc.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Oliveira HF, Yoshinari GH, Veras IM, et al. Impact of the Covid-19 pandemic on radiation oncology departments in Brazil impact of Covid-19 on Brazilian radiotherapy. Adv Radiat Oncol. 2021 doi: 10.1016/j.adro.2021.100667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Rykers K, Tacey M, Bowes J, et al. Victoria (Australia) radiotherapy response to working through the first and second wave of Covid-19: strategies and staffing. J Med Imaging Radiat Oncol. 2021;65:374–383. doi: 10.1111/1754-9485.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Xie C, Wang X, Liu H, et al. Outcomes in radiotherapy-treated patients with cancer during the Covid-19 outbreak in Wuhan, China. JAMA Oncol. 2020;6:1457–1459. doi: 10.1001/jamaoncol.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Chekhun VF, Domina EA. Can SARS-CoV-2 change individual radiation sensitivity of the patients recovered from Covid-19? (experimental and theoretical background) Exp Oncol. 2021;43:277–280. doi: 10.32471/exp-oncology.2312-8852.vol-43-no-3.16554. [DOI] [PubMed] [Google Scholar]
- 285.Mallick I, Chakraborty S, Baral S, et al. Prioritizing delivery of cancer treatment during a Covid-19 lockdown: the experience of a clinical oncology service in India. JCO Glob Oncol. 2021;7:99–107. doi: 10.1200/GO.20.00433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Teckie S, Andrews JZ, Chen WC-Y, et al. Impact of the Covid-19 pandemic surge on radiation treatment: report from a multicenter New York area institution. JCO Oncol Pract. 2021;17:e1270–e1277. doi: 10.1200/OP.20.00619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Yang L, Yang J, He J, et al. Analysis of anxiety and depression status in patients undergoing radiotherapy during the Covid-19 epidemic. Front Psychiatry. 2021;12:771621. doi: 10.3389/fpsyt.2021.771621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.De Felice F, Moriconi F. Covid-19 and cancer: implications for survival analysis. Ann Surg Oncol. 2021;28:5446–5447. doi: 10.1245/s10434-021-09792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.De B, Kaiser KW, Ludmir EB, et al. Radiotherapy clinical trial enrollment during the Covid-19 pandemic. Acta Oncol. 2021;60:312–315. doi: 10.1080/0284186X.2020.1865564. [DOI] [PubMed] [Google Scholar]
- 290.Mummudi N, Ghosh-Laskar S, Tibdewal A, Agarwal JP. Covid-19 pandemic and nationwide lockdown - implications of the double trouble on radiotherapy practice in India. Clin Oncol (R Coll Radiol) 2020;32:e219. doi: 10.1016/j.clon.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Orazem M, Ratosa I. Covid-19 pandemic as an opportunity for the radiotherapy department. Clin Oncol (R Coll Radiol) 2020;32:e175–e176. doi: 10.1016/j.clon.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Higgins E, Walters S, Powell E, Staffurth J. The impact of the acute phase of Covid-19 on radiotherapy demand in South East Wales. Clin Oncol (R Coll Radiol) 2020;32:e217. doi: 10.1016/j.clon.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Sriwijitalai W, Wiwanitkit V. Covid-19, radiotherapy and cancer. Radiother Oncol. 2020;149:48. doi: 10.1016/j.radonc.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Jereczek-Fossa BA, Palazzi MF, Soatti CP, et al. Covid-19 outbreak and cancer radiotherapy disruption in Lombardy, Northern Italy. Clin Oncol (R Coll Radiol) 2020;32:e160–e161. doi: 10.1016/j.clon.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Samper Ots PM, Zapatero Ortuño J, Pedraza Fernández S, et al. Impact of Covid-19 on patients in radiotherapy oncology departments in Spain. Radiother Oncol. 2021;161:148–151. doi: 10.1016/j.radonc.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Yu D, Hu W, Chen L, et al. Effect of radiotherapy interruption due to Covid-19 outbreak. Radiother Oncol. 2021;155:1–2. doi: 10.1016/j.radonc.2020.09.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Massaccesi M, Boldrini L, Piras A, et al. Spatially fractionated radiotherapy (SFRT) targeting the hypoxic tumor segment for the intentional induction of non-targeted effects: an in silico study to exploit a new treatment paradigm. Tech Innov Patient Support Radiat Oncol. 2020;14:11–14. doi: 10.1016/j.tipsro.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Sahgal A, Myrehaug SD, Siva S, et al. Stereotactic body radiotherapy versus conventional external beam radiotherapy in patients with painful spinal metastases: an open-label, multicenter, randomized, controlled, phase 2/3 trial. Lancet Oncol. 2021;22:1023–1033. doi: 10.1016/S1470-2045(21)00196-0. [DOI] [PubMed] [Google Scholar]
- 299.Cusumano D, Boldrini L, Yadav P, et al. Delta radiomics analysis for local control prediction in pancreatic cancer patients treated using magnetic resonance guided radiotherapy. Diagnostics. 2021;11:72. doi: 10.3390/diagnostics11010072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Caudell JJ, Torres-Roca JF, Gillies RJ, et al. The future of personalized radiotherapy for head and neck cancer. Lancet Oncol. 2017;18:e266–e273. doi: 10.1016/S1470-2045(17)30252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Catucci F, Alitto AR, Masciocchi C, et al. Predicting radiotherapy impact on late bladder toxicity in prostate cancer patients: an observational study. Cancers (Basel) 2021;13:175. doi: 10.3390/cancers13020175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Cusumano D, Catucci F, Romano A, et al. Evaluation of an early regression index (ERITCP) as predictor of pathological complete response in cervical cancer: a pilot-study. Appl Sci. 2020;10:8001. doi: 10.3390/app10228001. [DOI] [Google Scholar]
- 303.Gardin I, Grégoire V, Gibon D, et al. Radiomics: principles and radiotherapy applications. Crit Rev Oncol Hematol. 2019;138:44–50. doi: 10.1016/j.critrevonc.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 304.Widmark A, Gunnlaugsson A, Beckman L, et al. Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomized, non-inferiority, phase 3 trial. Lancet. 2019;394:385–395. doi: 10.1016/S0140-6736(19)31131-6. [DOI] [PubMed] [Google Scholar]
- 305.Piras A, Boldrini L, Menna S, et al. Hypofractionated radiotherapy in head and neck cancer elderly patients: a feasibility and safety systematic review for the clinician. Front Oncol. 2021;11:761393. doi: 10.3389/fonc.2021.761393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Brunt AM, Haviland JS, Wheatley DA, et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-forward): 5-year efficacy and late normal tissue effects results from a multicenter, non-inferiority, randomized, phase 3 trial. The Lancet. 2020;395:1613–1626. doi: 10.1016/S0140-6736(20)30932-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Piras A, Menna S, D’Aviero A, et al. New fractionations in breast cancer: a dosimetric study of 3D-CRT versus VMAT. J Med Radiat Sci. 2021 doi: 10.1002/jmrs.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Fionda B, Alitto AR, Frascino V, et al (2020) PROPHECY: Patient reported outcomes in prostate cancer, a mobile-health experience in radiotherapy.
- 309.Fionda B, Piras A, D’Aviero A, et al. The “PC-WIRED” study: patient centered evolution of websites of Italian radiotherapy departments. Patient Educ Couns. 2021;104:2152–2153. doi: 10.1016/j.pec.2021.02.014. [DOI] [PubMed] [Google Scholar]
- 310.Kichloo A, Albosta M, Dettloff K, et al. Telemedicine, the current Covid-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8:e000530. doi: 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with Covid-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.