Abstract
Background:
Per- and polyfluoroalkyl substances (PFAS) are ubiquitous synthetic chemicals that may disrupt blood pressure controls; however, human evidence to support this hypothesis is scant. We examined the association between serum concentrations of PFAS and risks of developing hypertension.
Methods:
This study included 1,058 midlife women initially free of hypertension from the multi-racial/ethnic Study of Women’s Health Across the Nation (SWAN) with annual follow-up visits between 1999 and 2017. Hypertension was defined as blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic or receiving anti-hypertensive treatment. Cox proportional hazards models were utilized to calculate hazards ratios (HRs) and 95% confidence intervals (CIs). Quantile g-computation was implemented to evaluate the joint effect of PFAS mixtures.
Results:
During 11,722 person-years of follow-up, 470 participants developed incident hypertension (40.1 cases per 1000 person-years). Compared with the lowest tertile, women in the highest tertile of baseline serum concentrations had adjusted HRs of 1.42 (95% CI: 1.19–1.68) for perfluorooctane sulfonate (PFOS) (P-trend=0.01), 1.47 (95% CI: 1.24–1.75) for linear perfluorooctanoate (n-PFOA) (P-trend=0.01), and 1.42 (95% CI: 1.19–1.70) for 2-(N-ethyl-perfluorooctane sulfonamido) acetate (EtFOSAA) (P-trend=0.01). No significant associations were observed for perfluorononanoate (PFNA) and perfluorohexane sulfonate (PFHxS). In the mixture analysis, women in the highest tertile of overall PFAS concentrations had an HR of 1.71 (95% CI: 1.15–2.54) (P-trend=0.008), compared with those in the lowest tertile.
Conclusions:
Several PFAS showed positive associations with incident hypertension. These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk.
Keywords: Per- and polyfluoroalkyl substances (PFAS), Perfluorooctanoate (PFOA), Perfluorooctane sulfonate (PFOS), Hypertension, Women
Graphical Absract
INTRODUCTION
Human exposure to per- and polyfluoroalkyl substances (PFAS) is of significant public health concern because PFAS are persistent in the environment and many also persist in humans.1 PFAS, synthetic chemicals widely used in industrial applications and consumer products, have been estimated to contaminate drinking water consumed by more than 200 million Americans.2 Data from the National Health and Nutrition Examination Survey (NHANES) demonstrate the ubiquity of PFAS exposure, as nearly all Americans have detectable concentrations of at least one PFAS in their blood.3 Due to their structural similarity to fatty acids, PFAS may interfere with the action of peroxisome proliferator-activated receptors (PPARs), specifically PPAR-α and PPAR-γ, and their signaling pathways, and thus, modulate metabolic pathways.4,5 Toxicological studies have also revealed that PFAS exposure is related to oxidative stress and endothelial dysfunction.6,7 As a result, the cardiovascular system is vulnerable to PFAS toxicity. PFAS have been associated with higher risks of cardiovascular disease (CVD) and peripheral arterial disease (PAD),8,9 as well as several CVD risk factors including thyroid disease,10–12 elevated total cholesterol and low-density lipoprotein levels,13–15 higher body mass index,16–20 and altered glucose homeostasis.21–23 However, far less is known about whether PFAS may disrupt blood pressure controls and increase the risk of developing hypertension.
Hypertension, a condition that affects more than one billion adults worldwide, is one of the most important risk factors for CVD.24 Hypertension is also the leading cause of death and disability-adjusted life years globally.25 Until recently, only one study has investigated the associations between PFAS exposure and incident hypertension,26 with no relationship detected in a prospective cohort of 660 pre-diabetic and overweight adults. Three cross-sectional studies have linked certain PFAS to increased prevalence of hypertension and elevated blood pressure,27–29 but three separate studies reported no association or even suggested protective effects of PFAS.30–32
Given the ubiquitous nature of PFAS exposure, even a modest association between PFAS and hypertension would place a large number of people at increased risks for cardiovascular morbidity and mortality. To better understand the relationship between PFAS and hypertension, we used data from the Study of Women’s Health Across the Nation (SWAN), which is a prospective study with approximately annual follow-up visits over 18 years. The menopausal transition marks a period of decline in follicle numbers and characteristic fluctuations in hormone levels. Furthermore, the menopausal transition is well-described as a period of increasing hypertension and cardiovascular disease risk.33 The present study examined PFAS individually, and jointly as mixtures. We hypothesized that higher serum PFAS concentrations would be associated with higher risks of incident hypertension.
METHODS
Study Design and Study Population
SWAN is a multi-site, multi-racial/ethnic, community-based longitudinal study designed to characterize physiological and psychosocial changes among women transitioning through menopause. The study design and procedures, including recruitment and enrollment, have been described in detail elsewhere.34 Between November 1995 and October 1997, a total of 3,302 pre-or early perimenopausal women aged 42–52 years were recruited from seven geographically distinct sites across the United States. All sites enrolled Non-Hispanic White women in addition to one additional racial/ethnic group. For the Boston, MA; Chicago, IL; Pittsburgh, PA; and Southeast Michigan, black women were enrolled, while Chinese women were enrolled at the Oakland, CA, Hispanic women from Newark, NJ; Chicago, IL, and Japanese women from Los Angeles, CA. Eligibility criteria for SWAN included age 42–52 years upon entry, presence of an intact uterus, at least one menstrual period in the prior three months, and not taking hormone medications within the prior three months. All participants provided written informed consent at each study visit, and all protocols used in SWAN were approved by the institutional review board at each participating site.
The SWAN Multi-Pollutant Study (MPS) was initiated in 2016 to examine metabolic and reproductive health effects of multiple environmental pollutants including PFAS in midlife women. The study designs of the SWAN MPS were described elsewhere.35–37 We used repository samples available from the third SWAN follow-up (visit 03 or the MPS baseline, 1999–2000) for environmental exposure assessments (n=2,694). MPS required women to have both blood and urine samples. Hispanic women were not eligible because urine samples were not collected (n=646). We also excluded women with insufficient serum or urine samples (n=648). Among 1,400 SWAN MPS participants, we excluded women with missing information on hypertension (n=18), those who had already had hypertension (n=306) at MPS baseline (visit 03), and those with missing values for other covariates (n=18), yielding a final analytic sample of 1,058 followed up from 1999 to 2017 (Figure S1).
Participant characteristics were significantly different between those included vs. not included in the SWAN MPS due to insufficient biospecimens (Table S1). Therefore, we used inverse probability weighting to address the issue of potential selection bias. The details of inverse probability weighting are shown in the Supplemental Materials.
Outcomes
Information on blood pressure and anti-hypertensive medication use was collected at each visit (approximately annually). The present study included data from 1999–2000 (SWAN follow-up visit 3, MPS baseline) through 2016–2017 (SWAN follow-up visit 16), with up to 13 time points included in the analysis. Blood pressure was measured according to a standardized protocol, with readings taken on the right arm, with the respondent seated and feet flat on the floor for at least 5 minutes prior to measurement. Respondents were asked not to smoke or consume any caffeinated beverage within 30 minutes of blood pressure measurement. Appropriate cuff size was determined based on arm circumference. A standard mercury sphygmomanometer was used to record systolic blood pressure (SBP) and diastolic blood pressure (DBP) at the first and fifth phase Korotkoff sounds. Two sequential blood pressure values were completed, with a minimum two-minute rest period between measures. The average of these measures was employed in these analyses. Hypertension was defined as SBP≥140 mmHg or DBP≥90 mmHg or use of antihypertensive medications, in accordance with the definitions used in the sixth and seventh reports of the Joint National Committee on Prevention, Detection, Treatment and Control of High Blood Pressure (JNC-6, JNC-7).38,39
Assessment of Serum PFAS Concentrations
Serum samples collected at the MPS baseline (1999–2000) were sent to the Division of Laboratory Sciences, National Center for Environmental Health, Centers for Disease Control and Prevention (CDC). The CDC laboratory’s involvement did not constitute engagement in human-subjects research. We quantified perfluorohexane sulfonate (PFHxS), n-PFOS, sum of branched isomers of PFOS (Sm-PFOS), n-PFOA, sum of branched PFOA (Sb-PFOA), perfluorononanoate (PFNA), perfluorodecanoate (PFDA), perfluoroundecanoate (PFUnDA), perfluorododecanoate (PFDoDA), and 2-(N-ethyl-perfluorooctane sulfonamido) acetate (EtFOSAA), and 2-(N-methyl-perfluorooctane sulfonamido) acetate (MeFOSAA) in 0.1 mL of serum, using an online solid phase extraction-high performance liquid chromatography-isotope dilution-tandem mass spectrometry.40 The analytic methods and quality control procedures have been described elsewhere.36 The coefficient of variation of low- and high-quality controls ranged from 6% to 12%, depending on the analyte. The limit of detection (LOD) was 0.1 ng/mL for all the analytes. Concentrations below the LODs were substituted with .41 Total PFOS (PFOS) was computed as the sum of n-PFOS and Sm-PFOS.
Covariates
Given careful review of the literature for important variables associated with both PFOS exposure and hypertension risk,35,42 we selected a comprehensive set of confounders. We obtained the following data from participants’ standardized interviews conducted at each visit. Sociodemographic variables included age at baseline (in years), self-defined race/ethnicity (Black, Chinese, Japanese, White), study site (Southeast Michigan, Boston, Pittsburgh, Oakland, Los Angeles), education (high school or less, some college, college degree or higher), and financial strain (very hard, somewhat hard, not hard at all). Time-varying covariates included self-reported lifestyle factors, namely smoking status (never smoker, past smoker, current smoker), environmental tobacco smoking (0, 1–4, ≥5 person-hours),43 total calorie intake (in kcal), and alcohol intake (<1 drink/month, >1 drink/month and ≤1/week, >1 drink/week). Physical activity was assessed in various domains, including sports/exercise, household/caregiving and daily routine, with a range of 3 to 15 (15 indicating the highest level of activity).44 Menopausal status was categorized into surgical postmenopausal, natural postmenopausal, late perimenopausal, early perimenopausal, premenopausal, or unknown due to hormone therapy (HT) using bleeding patterns and information about HT use. The SWAN has a small proportion (<5%) of missing data on time-varying covariates. To deal with missing data, we simply carried forward last observations.
Statistical Analysis
Descriptive statistics were calculated for participant characteristics and serum concentrations of PFAS at MPS baseline. Spearman correlation coefficients were calculated among multiple PFAS compounds. Cox proportional hazards (PH) regression model were utilized to calculate hazards ratio (HR) and 95% confidence interval (95% CI). We employed age instead of follow-up time as the time scale.45 Serum concentrations of PFAS were categorized into tertiles. HRs and 95% CIs were calculated comparing the second and the highest tertiles of PFAS concentrations with the lowest tertile (the reference). We also examined the log-linear relationships using log2-transformed PFAS concentrations. In this case, HRs and 95% CIs were interpreted as changes per doubling in PFAS concentrations. Covariates considered in multivariable adjustments included race/ethnicity, educational attainment, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status. We included in data analyses n-PFOS, Sm-PFOS, n-PFOA, PFHxS, PFNA, EtFOSAA and MeFOSAA that were detected in >97% of samples. Sb-PFOA, PFDA, and PFUnDA with relatively low detection frequencies (<50%) were modeled as detect vs. non-detect. PFDoDA with extremely low detection frequencies (3.7%) was not included in the analysis. As the menopausal transition contribute to the increase in hypertension risks,33 we also examined the whether the relationships of PFAS and hypertension differed by menopausal status, by including interaction terms between PFAS and menopausal status (premenopause, perimenopause, and natural postmenopause).
As an additional exploratory analysis, we utilized quantile g-computation to evaluate the overall effects of exposure to PFAS mixtures on incident hypertension.46 Quantile g-computation is a valuable tool designed for estimating the joint effects of correlated chemical mixtures. This approach combined the inferential ability of weighted quantile sum (WQS) regression47 with the flexibility of g-computation, a method of causal effect estimation. In the current study, all PFAS mixture components were first transformed into tertiles. Then a Cox PH regression was fit for PFAS, covariates and incident hypertension, which defined the weights for each PFAS. Weights represented the association between each PFAS and incident hypertension. The sum of weights was constructed as the quantile g-computation estimator. The mixture effect of PFAS was calculated using the quantile g-computation estimator and interpreted as the HR and 95% CI per tertile increase in all PFAS concentrations, adjusting for covariates described above for the individual PFAS models. To be consistent with the individual associations, we calculated and interpreted HRs comparing the highest and second tertiles to the lowest tertile. The mixture analyses were conducted in the R package ‘qgcomp’. Given that the ‘qgcomp.cox’ function in the ‘qgcomp’ package may yield invalid results using counting-process style data, we decided to use wide format data to conduct quantile g-computation as an exploratory analysis. Details of the quantile g-computation and R codes are provided in the supplemental materials.
Additionally, we performed a sensitivity analysis with further adjustment for BMI and weight change over time. We did not consider BMI and weight change over time as a confounder in the primary analysis in case of over-adjustment bias because PFAS may contribute to increased BMI and weight gain.16–20,48 Furthermore, we evaluated the association between PFAS and changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP) in women without anti-hypertensive medication use or hypertension using linear mixed models to understand which of two measurements might drive the development of hypertension. Moreover, we modeled time to hypertension using parametric method, i.e., accelerated failure time models, to examine the robustness of our findings. Finally, we replicated the analysis using wide-format data with baseline covariates rather than counting-process data. All the analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, North Carolina) and R (version 4.0.0. R Foundation for Statistical Computing).
RESULTS
At MPS baseline, the median age was 49.2 years, 54.5% were White women, 16.8% held a high school diploma or had not completed high school, 29.9% reported being very hard or somewhat hard paying for basics, 35.7% were past or current smokers, 37.8% were exposed to environmental tobacco smoke, and 24.9% were high-frequency alcohol drinkers (Table 1). In addition, 30% of women were postmenopausal. The median serum concentrations of PFAS at MPS baseline were 24.1 (IQR: 17.3, 34.8) ng/mL for PFOS, 17.2 (IQR: 12.2, 24.1) ng/mL for n-PFOS, 7.1 (IQR: 4.6, 10.7) ng/mL for Sm-PFOS, 4.1 (IQR: 2.8, 5.9) ng/mL for n-PFOA, 1.5 (IQR: 1.0, 2.4) ng/mL for PFHxS, 0.6 (IQR: 0.4, 0.8) ng/mL for PFNA, 1.2 (IQR: 0.6, 2.2) ng/mL for EtFOSAA, and 1.4 (IQR: 0.9, 2.3) ng/mL for MeFOSAA (Table S2). Spearman correlation coefficients among these compounds ranged from 0.11 to 0.82 (Figure S2). Of the 1,058 participants, 470 women developed hypertension over 11,722 person-years (40.1 cases per 1000 person years). The median follow-up time was 12.4 (IQR: 5.1, 16.4) years.
Table 1.
Baseline characteristics and blood pressure in midlife women from the Study of Women’s Health Across the Nation Multi-Pollutant Study (n=1,058).
| Characteristics | Median (IQR) or N (%) |
|---|---|
| Age, year | 49.2 (47.2, 51.3) |
| Race/ethnicity | |
| White | 577 (54.5%) |
| Black | 161 (15.2%) |
| Chinese | 149 (14.1%) |
| Japanese | 171 (16.2%) |
| Study site | |
| Southeast Michigan | 149 (14.1%) |
| Boston | 172 (16.2%) |
| Oakland | 261 (24.7%) |
| Los Angeles | 299 (28.3%) |
| Pittsburgh | 177 (16.7%) |
| Education | |
| ≤High school | 177 (16.7%) |
| High school | 317 (30.0%) |
| College | 273 (25.8%) |
| Post-college | 291 (27.5%) |
| Difficulty paying for basics | |
| Very hard | 58 (5.5%) |
| Somewhat hard | 257 (24.3%) |
| Not hard at all | 753 (70.2%) |
| Smoking status | |
| Never smoked | 681 (64.4 %) |
| Past smoker | 278 (26.3%) |
| Current smoker | 99 (9.4%) |
| Environmental tobacco smoke | |
| 0 person-hrs | 658 (62.2%) |
| 1–4 person-hrs | 238 (22.5%) |
| ≥5 person-hrs | 162 (15.3%) |
| Alcohol intake | |
| None/Low use | 538 (50.8%) |
| Moderate use | 257 (24.3%) |
| High use | 263 (24.9%) |
| Physical activity score | 8.0 (6.7, 9.1) |
| Menopausal status | |
| Surgical post | 30 (2.8%) |
| Natural post | 114 (10.8%) |
| Late perimenopausal | 78 (7.4%) |
| Early perimenopausal | 548 (51.8%) |
| Premenopausal | 138 (13.0%) |
| Unknown with hormone therapy | 150 (14.2%) |
| Total calorie intake, kcal | 1694 (1352, 2161) |
| BMI, kg/m2 | 25.1 (22.1, 29.9) |
| Systolic blood pressure, mmHg | 108 (101, 117) |
| Diastolic blood pressure, mmHg | 71 (66, 77) |
We found positive associations of PFOS, n-PFOA, and EtFOSAA with hypertension incidence (Table 2). Comparing the highest tertile of serum concentrations with the lowest, HRs of hypertension were 1.42 (95% CI: 1.19, 1.68) for PFOS (P for trend<0.0001), 1.40 (95% CI: 1.18, 1.66) for n-PFOS (P for trend<0.0001), 1.49 (95% CI: 1.25, 1.78) for Sm-PFOS (P for trend<0.0001), 1.47 (95% CI: 1.24, 1.75) for n-PFOA (P for trend<0.0001), and 1.42 (95% CI: 1.19, 1.70) for EtFOSAA (P for trend=0.0003), after adjusting for race/ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status. Adjusted survival curves for each PFAS are shown in Figures S3-S10. We also detected significant log-linear relationships of PFOS, EtFOSAA and MeFOSAA with incident hypertension. Multivariable-adjusted HRs for a doubling in serum concentrations were 1.18 (95% CI: 1.09, 1.28) for total PFOS, 1.17 (95% CI: 1.08, 1.27) for n-PFOS, 1.16 (95% CI: 1.08, 1.25) for Sm-PFOS, 1.17 (95% CI: 1.07, 1.27) for n-PFOA, 1.09 (95% CI: 1.04, 1.15) for EtFOSAA, and 1.10 (95% CI: 1.03, 1.19) for MeFOSAA. Although we found significant associations of PFOS, n-PFOA, and EtFOSAA with hypertension, we observed no interactions of these chemicals with menopausal status (Table S3), except for MeFOSAA. The HR of hypertension was 1.36 (95% CI: 1.12, 1.65) for premenopause, 0.98 (95% CI: 0.89, 1.08) for perimenopause, and 1.34 (95% CI: 1.08, 1.67) for natural postmenopause (P for interaction=0.0009).
Table 2.
Hazard ratios (HR) (95% confidence intervals, 95% CI) of incident hypertension with tertile changes and per doubling in serum concentrations of PFAS.
| PFAS | Tertile of PFAS concentrations | p value for trend |
Per doubling increase HR (95%CI) |
p value | ||
|---|---|---|---|---|---|---|
| Tertile 1 HR (95%CI) |
Tertile 2 HR (95%CI) |
Tertile 3 HR (95%CI) |
||||
| PFOS | ||||||
| Median (IQR), ng/mL | 14.5 (11.6, 17.1) | 24.0 (21.8, 27.2) | 41.9 (34.8, 53.9) | |||
| No. cases/person-years | 133/4212 | 156/4009 | 181/3501 | |||
| Model 1* | Ref | 1.23 (1.03, 1.46) | 1.54 (1.31, 1.82) | <0.0001 | 1.21 (1.13, 1.31) | <0.0001 |
| Model 2† | Ref | 1.11 (0.93, 1.33) | 1.42 (1.19, 1.68) | <0.0001 | 1.18 (1.09, 1.28) | <0.0001 |
| n-PFOS | ||||||
| Median (IQR), ng/mL | 10.5 (8.3, 12.2) | 17.2 (15.7, 19.0) | 28.6 (24.2, 37.6) | |||
| No. cases/person-years | 133/4096 | 152/4166 | 185/3460 | |||
| Model 1* | Ref | 1.14 (0.96, 1.35) | 1.50 (1.27, 1.77) | <0.0001 | 1.20 (1.11, 1.30) | <0.0001 |
| Model 2† | Ref | 1.00 (0.84, 1.19) | 1.40 (1.18, 1.66) | <0.0001 | 1.17 (1.08, 1.27) | 0.0002 |
| Sm-PFOS | ||||||
| Median (IQR), ng/mL | 3.9 (2.9, 4.6) | 7.1 (6.2, 8.1) | 13.1 (10.7, 17.2) | |||
| No. cases/person-years | 133/4202 | 156/3867 | 181/3653 | |||
| Model 1* | Ref | 1.24 (1.05, 1.48) | 1.63 (1.37, 1.92) | <0.0001 | 1.19 (1.11, 1.28) | <0.0001 |
| Model 2† | Ref | 1.14 (0.95, 1.36) | 1.49 (1.25, 1.78) | <0.0001 | 1.16 (1.08, 1.25) | <0.0001 |
| n-PFOA | ||||||
| Median (IQR), ng/mL | 2.4 (1.9, 2.9) | 4.1 (3.7, 4.5) | 6.8 (5.8, 8.9) | |||
| No. cases/person-years | 141/4103 | 150/3900 | 179/3719 | |||
| Model 1* | Ref | 1.34 (1.13, 1.59) | 1.52 (1.29, 1.80) | <0.0001 | 1.19 (1.10, 1.29) | <0.0001 |
| Model 2† | Ref | 1.37 (1.15, 1.63) | 1.47 (1.24, 1.75) | <0.0001 | 1.17 (1.07, 1.27) | 0.0005 |
| PFNA | ||||||
| Median (IQR), ng/mL | 0.3 (0.3, 0.4) | 0.6 (0.5, 0.7) | 1.0 (0.9, 1.1) | |||
| No. cases/person-years | 138/3708 | 188/4796 | 144/3218 | |||
| Model 1* | Ref | 0.95 (0.81, 1.11) | 1.05 (0.89, 1.25) | 0.53 | 1.06 (0.98, 1.15) | 0.17 |
| Model 2† | Ref | 0.93 (0.79, 1.09) | 1.00 (0.83, 1.19) | 0.97 | 1.05 (0.97, 1.14) | 0.24 |
| PFHxS | ||||||
| Median (IQR), ng/mL | 0.8 (0.6, 1.0) | 1.5 (1.3, 1.7) | 3.2 (2.4, 4.8) | |||
| No. cases/person-years | 150/3854 | 149/4005 | 171/3863 | |||
| Model 1* | Ref | 0.86 (0.72, 1.02) | 1.06 (0.90, 1.25) | 0.37 | 0.99 (0.94, 1.04) | 0.71 |
| Model 2† | Ref | 0.84 (0.71, 1.00) | 1.06 (0.89, 1.25) | 0.38 | 0.98 (0.93, 1.04) | 0.56 |
| EtFOSAA | ||||||
| Median (IQR), ng/mL | 0.5 (0.4, 0.6) | 1.2 (0.9, 1.4) | 3.0 (2.3, 4.7) | |||
| No. cases/person-years | 127/4136 | 164/3996 | 179/3590 | |||
| Model 1* | Ref | 1.47 (1.24, 1.76) | 1.57 (1.32, 1.87) | <0.0001 | 1.12 (1.07, 1.18) | <0.0001 |
| Model 2† | Ref | 1.39 (1.16, 1.66) | 1.42 (1.19, 1.70) | 0.0003 | 1.09 (1.04, 1.15) | 0.0005 |
| MeFOSAA | ||||||
| Median (IQR), ng/mL | 0.7 (0.5, 0.9) | 1.4 (1.2, 1.7) | 2.8 (2.3, 3.6) | |||
| No. cases/person-years | 134/4016 | 149/4027 | 187/3679 | |||
| Model 1* | Ref | 0.96 (0.81, 1.15) | 1.24 (1.04, 1.48) | 0.006 | 1.14 (1.06, 1.22) | 0.0004 |
| Model 2† | Ref | 0.91 (0.76, 1.09) | 1.15 (0.96, 1.37) | 0.06 | 1.10 (1.03, 1.19) | 0.009 |
Model 1 was adjusted for race/ethnicity and study site with inverse probability weight.
Model 2: Model 1 + education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status with inverse probability weight.
HRs (95% CIs) were computed from Cox proportional hazards model with age as the time scale.
Abbreviations: PFOS, perfluorooctane sulfonate; PFOA, perfluorooctanoate; PFNA, perfluorononanoate; PFHxS, perfluorohexane sulfonate; EtFOSAA, 2-(N-ethyl-perfluorooctane sulfonamido) acetate; MeFOSAA, 2-(N-methyl-perfluorooctane sulfonamido) acetate.
In the sensitivity analyses, the effect estimates remained similar after further adjustment for weight change over time (Tables S4-S5). No significant associations were observed for Sb-PFOA, PFDA, and PFUnDA with relatively low detection frequencies (Table S6). Furthermore, when examining blood pressure among women before receiving anti-hypertensive medications or developing hypertension, we found significant associations of PFOS, EtFOSAA and MeFOSAA with SBP and DBP (Tables S7-S8). Using parametric accelerated failure time models, we observed significant associations of PFOS, n-PFOS, Sm-PFOS, n-PFOA, and EtFOSAA with shorter time to the development of hypertension (Table S9).
The quantile g-computation estimated beta coefficients for all PFAS, as shown in Table S6, including n-PFOS (β=0.051), Sm-PFOS (β=0.115), EtFOSAA (β=0.049), MeFOSAA (β=0.0092), n-PFOA (β=0.032), PFNA (β=0.086), and PFHxS (β=−0.074). These beta coefficients were then incorporated as the weights into the construction of quantile g-computation estimator. Compared to those with the lowest tertile of overall PFAS concentrations, women with the second tertile and highest tertile were 1.31 (95% CI: 1.07, 1.59) and 1.71 (95% CI: 1.15, 2.54) times more likely to develop hypertension during the follow-up (P for trend=0.008), respectively (Figure 1).
Figure 1.
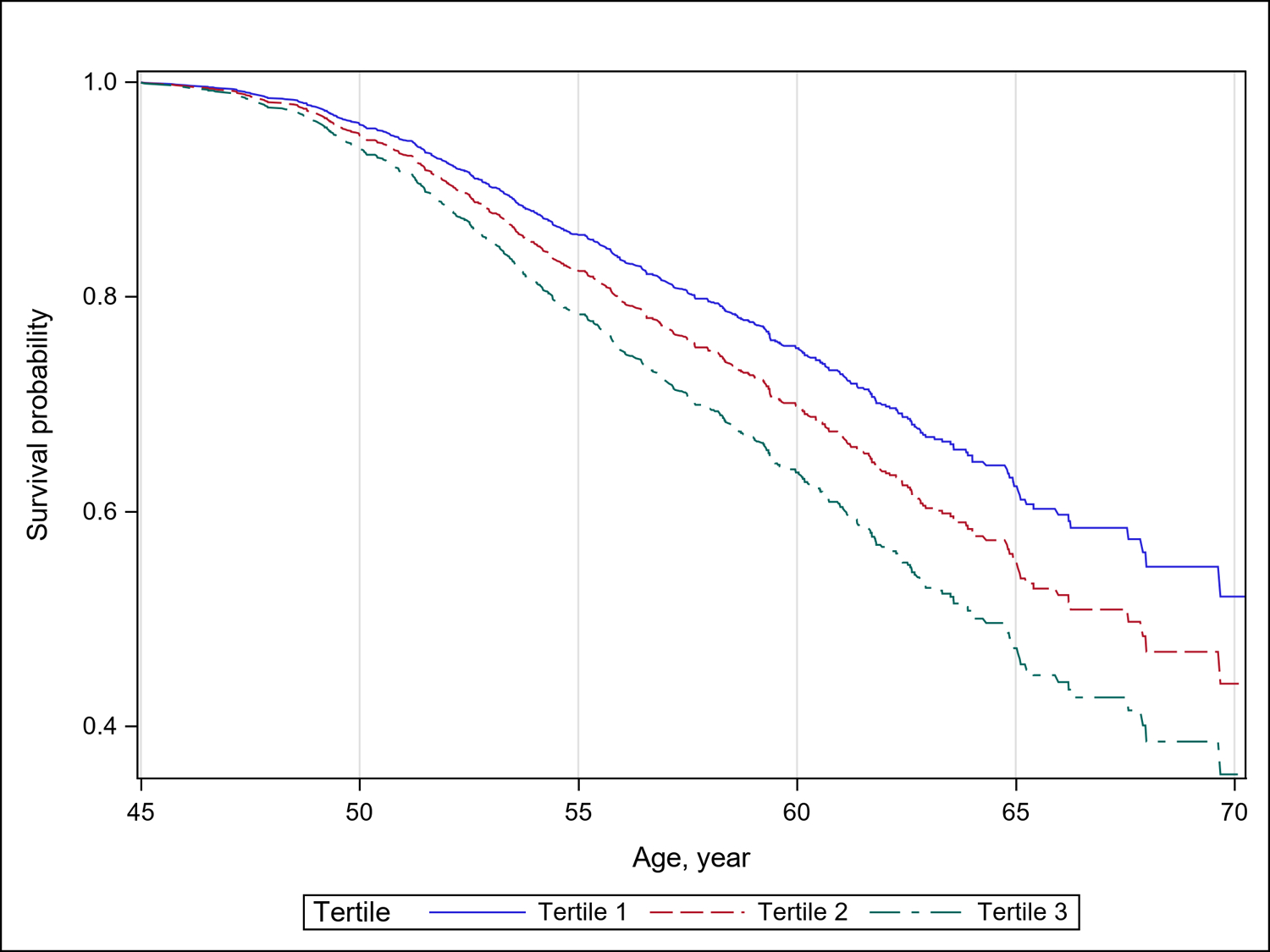
Adjusted survival curves for incident hypertension by tertiles of serum concentrations of PFAS mixtures from quantile g-computation. The model was adjusted for race/ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status, with inverse probability weighting. The adjusted hazards ratio of incident hypertension was 1.31 (95% CI: 1.07, 1.59) for Tertile 2 and 1.71 (95% CI: 1.15, 2.54) for Tertile 3, compared with those in Tertile 1 (P for trend=0.008).
DISCUSSION
In this 18-year prospective cohort of 1,058 women with 11,722 person-years of observations in annual follow-up visits, we found that PFOS, n-PFOA, EtFOSAA and MeFOSAA individually were associated with an increased incidence of hypertension. In the mixture analysis, women with higher overall PFAS concentrations were also more likely to develop hypertension. Taken together, our findings suggest PFAS may be an underappreciated contributing factor to women’s CVD risks.
To date, only one epidemiologic study has examined the effect of PFAS on incident hypertension. In a longitudinal cohort of adults who were pre-diabetic and overweight in the United States with three follow-up visits from 1996 to 2013, Lin et al. did not observe an association between plasma PFAS and incident hypertension; but did report modest associations between PFOA and SBP (β=1.49 mmHg, 95% CI: 0.29, 2.70 mmHg higher per doubling in PFOA), and between MeFOSAA and prevalent hypertension (OR=1.09, 95% CI: 1.01, 1.19 per doubling in MeFOSAA). PFAS concentrations in our study were similar to those in Lin et al. People with obesity were excluded in the Lin et al. study which might account for the discrepancy between our results.
Findings from cross-sectional studies are inconsistent. Three cross-sectional studies reported significant positive associations of specific PFAS with prevalent hypertension and elevated blood pressure.27–29 In a study of 2,934 adults who participated in the 2003–2004 and 2005–2006 NHANES, the adjusted odds for prevalent hypertension was two and a half-fold higher in those at the 80th vs. the 20th percentiles of PFOA concentrations; no relationship was found for other PFAS.27 A cross-sectional study of 1,612 Chinese adults aged 22–96 years reported significant relationships of prevalent hypertension with PFOS, PFOA, PFNA and perfluorobutanoate, with more pronounced effects observed in females; whereas no associations were detected for other compounds.28 Similarly, in a cross-sectional study of 16,224 adults aged 20–39 years living in Italy who were exposed to PFAS-contaminated drinking water, PFOA was associated with higher SBP in men and DBP in women; on the other hand, significant associations of PFOA, PFOS, PFHxS and PFNA with prevalent hypertension were observed only in men.29 Other cross-sectional studies reported no associations of PFAS with prevalent hypertension and blood pressure,30–32 while one cross-sectional study of 154 male anglers aged 50 years and older in Wisconsin30 found an inverse association between PFNA and prevalent hypertension. All these studies considered similar sets of confounders, including demographic factors, socioeconomic status, and lifestyle factors in their analyses. It is unlikely that confounding could account for the discrepancies in the results from previous cross-sectional studies. The differences in the study results are likely attributable to differences in age. Women tend to get diagnosis with hypertension later in their midlife so that the differences in age would in differences in the study results.
A potential biological mechanism relating exposure to PFAS to hypertension may be metabolic disturbances of PFAS on fatty acid metabolism, likely through activation of multiple nuclear receptors such as PPARs.4,5 PPARα is abundantly expressed in tissues with a high capacity for mitochondrial fatty acid oxidation, such as the heart.49,50 Certain PFAS share structural similarity to fatty acids. Although human PPARα appears to be less responsive to PFAS exposure than mouse PPARα, most perfluoroalkyl carboxylates (e.g., PFOA) and sulfonates (e.g., PFOS) activate PPARα in mouse and human models.51,52 The ability of PFAS to interfere with PPARα has been put forward as an explanation for PFAS-induced cardiovascular disturbances. Further, hypertension has been associated with thyroid dysfunction, with a high prevalence in hypothyroidism.53 PFAS were associated with decreased circulating thyroid hormone levels and an interruption of the thyroid hormone signaling pathways in human studies; however, contradictory results were reported.10,54
Experimental studies have also demonstrated that PFAS exposure is related to oxidative stress and endothelial dysfunction.6,7 Oxidative stress has been proposed as a cause of hypertension. A disturbance of ROS production may account for reduced vasodilation, which in turn can trigger the development of hypertension.6 Exposure of human microvascular endothelial cells to different concentrations (10–100 μM) of PFOS in vitro increased the production of ROS and induced an alteration in endothelial permeability.7 PFOS has also been shown to induce the formation of intracellular ROS and lipid peroxidation in isolated rat hepatocytes.55 Oral administration with PFOS at 1 or 10 mg/kg body weight for 28 consecutive days increased intracellular ROS formation and nitric oxide production in rats, and also inhibited the activities of antioxidant enzymes (including catalase and superoxide dismutase).56 Overall, activation of nuclear receptors, interference with fatty acid metabolism, disruption of thyroid hormone homeostasis, and oxidative stress may be partly responsible for PFAS-induced elevated blood pressure and hypertension.
Notably, studies that analyzed results by sex observed a more pronounced association in women.28 Age at the final menstrual period may be a marker not only for reproductive aging but also for somatic aging. Lower levels of estrogens during the menopausal transition may increase the risks of hypertension and CVD.57 PFAS as endocrine-disrupting chemicals may accelerate ovarian aging,58,59 and contribute to increased risks of hypertension and CVD during the sensitive and critical time window in a woman’s life.
We observed consistent associations of PFOS, n-PFOA, EtFOSAA and MeFOSAA individually and PFAS mixtures with hypertension, while PFAS mixtures had a greater risk of incident hypertension compared to individual PFAS. Our findings are in agreement with previous toxicological studies that reported mixture effects of PFAS.60,61 Exposure to multiple PFAS is of great interest as PFAS are commonly found in drinking water, food, and a wide range of consumer and industrial products. As such, there is a pressing need to investigate how these compounds jointly affect the development of hypertension.62–66
The primary strengths of this study included prospective determination of hypertension status, a large cohort of community-based women of various racial/ethnic groups, and long follow-up for up to 18 years. The prospective design also minimized the possibility of reverse causation. Frequent follow-up visits with objective measures of blood pressure and information on hypertension medication use, instead of a one-time questionnaire, provided reliable estimates of time to hypertension. The temporal relationship established by the long follow-up and repeated assessment of blood pressure provides evidence for the positive associations between PFAS concentrations and incident hypertension. To our knowledge, this is also the first study to examine the association of PFAS mixtures with hypertension. Our mixture analysis was powered by the well-established quantile g-computation, while handling complex correlations structures among pollutants.
The findings from this study must be interpreted in light of some limitations. First, we only included midlife women. It is unknown whether these findings are applicable to men or to other women, including women of reproductive age. As described in the Methods section, the SWAN included sampling of Chinese and Japanese women at only one study site. It is possible that women at a given site may not be representative of their racial/ethnic group as a whole. In addition, we did not include Hispanic women due to lack of biologic samples. There are racial/ethnic disparities in hypertension, with higher prevalence in the Black population compared to other racial/ethnic groups.67 Causes of racial/ethnic disparities are multifactorial, and primary determinants are social factors such as education, access to healthcare, and insurance coverage.68 In SWAN, there are racial/ethnic disparities in PFAS body burden, with Black participants having higher serum concentrations of PFOS.35,36 These differences may be due to living near areas contaminated with PFAS exposure such as airports and industrial areas.69 This exposure disparity reflects the ongoing marginalization of the Black community in the United States which often lives in more environmentally vulnerable areas, reflecting decades of structural racism. Future work needs more efforts to explore these racial/ethnic differences in both exposure and outcome patterning to understand the impact of these differential exposures on minority populations. Further, we did not collect information on family history of hypertension so we cannot examine effect modification by family history of hypertension. Finally, we did not consider pregnancy-related outcomes (i.e., preeclampsia, gestational diabetes) in our analysis because this data was not available. No participants became pregnant during the follow-up period. We measured PFAS concentration later in life and did not have the data to assess susceptibility from early-life exposure to PFAS.
PERSPECTIVES
In a large, prospective cohort of midlife women with annual follow-up visits from 1999 to 2017, higher serum PFAS concentrations are associated with a higher risk of hypertension. Our findings suggest that PFAS are potentially modifiable risk factors for hypertension. If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD.
Supplementary Material
NOVELTY AND RELEVANCE.
What is new?
This is the first study to evaluate the effects of PFAS on incident hypertension among midlife women, using a prospective cohort of 1,058 women initially free of hypertension with annual follow-up visits from 1999 to 2017.
What is Relevant?
Higher PFOS, PFOA, and EtFOSAA are associated with 42%, 47%, and 42% higher risks of hypertension, respectively, comparing the highest to the lowest tertile.
Participants with higher overall PFAS concentrations are associated with a 71% increase in the risk of hypertension.
Clinical/Pathophysiological Implications?
PFAS are potentially modifiable risk factors for hypertension and cardiovascular disease. Our findings are of significant public health concern since PFAS are ubiquitous in humans and the environment.
ACKNOWLEDGMENTS
The Study of Women’s Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants U01NR004061; U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495). The study was supported by the SWAN Repository (U01AG017719).
This study was also supported by grants from the National Institute of Environmental Health Sciences (NIEHS) R01-ES026578, R01-ES026964 and P30-ES017885, and by the Center for Disease Control and Prevention (CDC)/National Institute for Occupational Safety and Health (NIOSH) grant T42-OH008455.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH. The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC). Use of trade names is for identification only and does not imply endorsement by the CDC, the Public Health Service, or the U.S. Department of Health and Human Services.
Clinical Centers:
University of Michigan, Ann Arbor – Siobán Harlow, PI 2011 – present, MaryFran Sowers, PI 1994–2011; Massachusetts General Hospital, Boston, MA – Joel Finkelstein, PI 1999 – present; Robert Neer, PI 1994 – 1999; Rush University, Rush University Medical Center, Chicago, IL – Howard Kravitz, PI 2009 – present; Lynda Powell, PI 1994 – 2009; University of California, Davis/Kaiser – Ellen Gold, PI; University of California, Los Angeles – Gail Greendale, PI; Albert Einstein College of Medicine, Bronx, NY – Carol Derby, PI 2011 – present, Rachel Wildman, PI 2010 – 2011; Nanette Santoro, PI 2004 – 2010; University of Medicine and Dentistry – New Jersey Medical School, Newark – Gerson Weiss, PI 1994 – 2004; and the University of Pittsburgh, Pittsburgh, PA – Karen Matthews, PI.
NIH Program Office:
National Institute on Aging, Bethesda, MD – Chhanda Dutta 2016- present; Winifred Rossi 2012–2016; Sherry Sherman 1994 – 2012; Marcia Ory 1994 – 2001; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory:
University of Michigan, Ann Arbor – Daniel McConnell (Central Ligand Assay Satellite Services).
CDC Laboratory:
Division of Laboratory Sciences, National Center for Environmental Health, Centers for Disease Control and Prevention, Atlanta, GA.
SWAN Repository:
University of Michigan, Ann Arbor – Siobán Harlow 2013 - Present; Dan McConnell 2011 – 2013; MaryFran Sowers 2000 – 2011.
Coordinating Center:
University of Pittsburgh, Pittsburgh, PA – Maria Mori Brooks, PI 2012 - present; Kim Sutton-Tyrrell, PI 2001 – 2012; New England Research Institutes, Watertown, MA - Sonja McKinlay, PI 1995 – 2001.
Steering Committee:
Susan Johnson, Current Chair
Chris Gallagher, Former Chair
We thank the study staff at each site and all the women who participated in SWAN.
NON-STANDARD ABBREVIATIONS AND ACRONYMS
- EtFOSAA
2-(N-ethyl-perfluorooctane sulfonamido) acetate
- MeFOSAA
2-(N-methyl-perfluorooctane sulfonamido) acetate
- N-PFOA
Linear perfluorooctanoate
- N-PFOS
Linear perfluorooctane sulfonate
- PFAS
Per- and polyfluoroalkyl substances
- PFHxS
Perfluorohexane sulfonate
- PFNA
Perfluorononanoate
- Sm-PFOS
Sum of branched isomers of perfluorooctane sulfonate
Footnotes
Disclosure: The authors declare no competing financial interest.
REFERENCES
- 1.ATSDR. Toxicological Profile for Trichloroethylene.; 2021. Accessed May 8, 2020. https://www.atsdr.cdc.gov/toxprofiles/tp200.pdf [PubMed]
- 2.Andrews DQ, Naidenko OV. Population-Wide Exposure to Per- And Polyfluoroalkyl Substances from Drinking Water in the United States. Environ Sci Technol Lett. 2020;7(12):931–936. doi: 10.1021/acs.estlett.0c00713 [DOI] [Google Scholar]
- 3.CDC. Fourth National Report on Human Exposure to Environmental Chemicals.; 2021. Accessed July 5, 2021. https://www.cdc.gov/exposurereport/pdf/FourthReport_UpdatedTables_Volume2_Mar2021-508.pdf [PubMed] [Google Scholar]
- 4.Bjork JA, Butenhoff JL, Wallace KB. Multiplicity of nuclear receptor activation by PFOA and PFOS in primary human and rodent hepatocytes. Toxicology. 2011;288(1–3):8–17. doi: 10.1016/j.tox.2011.06.012 [DOI] [PubMed] [Google Scholar]
- 5.Hines EP, White SS, Stanko JP, Gibbs-Flournoy EA, Lau C, Fenton SE. Phenotypic dichotomy following developmental exposure to perfluorooctanoic acid (PFOA) in female CD-1 mice: Low doses induce elevated serum leptin and insulin, and overweight in mid-life. Mol Cell Endocrinol. 2009;304:97–105. doi: 10.1016/j.mce.2009.02.021 [DOI] [PubMed] [Google Scholar]
- 6.Ceriello A. Possible Role of Oxidative Stress in the Pathogenesis of Hypertension. Published online 2008. doi: 10.2337/dc08-s245 [DOI] [PubMed] [Google Scholar]
- 7.Qian Y, Ducatman A, Ward R, et al. Perfluorooctane sulfonate (PFOS) induces reactive oxygen species (ROS) production in human microvascular endothelial cells: Role in endothelial permeability. J Toxicol Environ Heal - Part A Curr Issues. 2010;73(12):819–836. doi: 10.1080/15287391003689317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shankar A, Xiao J, Ducatman A. Perfluorooctanoic acid and cardiovascular disease in US adults. Arch Intern Med. 2012;172(18):1397–1403. doi: 10.1001/archinternmed.2012.3393 [DOI] [PubMed] [Google Scholar]
- 9.Huang M, Jiao J, Zhuang P, Chen X, Wang J, Zhang Y. Serum polyfluoroalkyl chemicals are associated with risk of cardiovascular diseases in national US population. Environ Int. 2018;119:37–46. doi: 10.1016/j.envint.2018.05.051 [DOI] [PubMed] [Google Scholar]
- 10.Kim MJ, Moon S, Oh BC, et al. Association between perfluoroalkyl substances exposure and thyroid function in adults: A meta-analysis. Soares P, ed. PLoS One. 2018;13(5):e0197244. doi: 10.1371/journal.pone.0197244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melzer D, Rice N, Depledge MH, Henley WE, Galloway TS. Association between serum perfluorooctanoic acid (PFOA) and thyroid disease in the U.S. National Health and Nutrition Examination Survey. Environ Health Perspect. 2010;118(5):686–692. doi: 10.1289/ehp.0901584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrestha S, Bloom MS, Yucel R, et al. Perfluoroalkyl substances and thyroid function in older adults. Environ Int. 2015;75:206–214. doi: 10.1016/j.envint.2014.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winquist A, Steenland K. Modeled PFOA exposure and coronary artery disease, hypertension, and high cholesterol in community and worker cohorts. Environ Health Perspect. 2015;122(12):1299–1305. doi: 10.1289/ehp.1307943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin PID, Cardenas A, Hauser R, et al. Per- and polyfluoroalkyl substances and blood lipid levels in pre-diabetic adults—longitudinal analysis of the diabetes prevention program outcomes study. Environ Int. 2019;129:343–353. doi: 10.1016/j.envint.2019.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Starling AP, Engel SM, Whitworth KW, et al. Perfluoroalkyl substances and lipid concentrations in plasma during pregnancy among women in the Norwegian Mother and Child Cohort Study. Environ Int. 2014;62:104–112. doi: 10.1016/j.envint.2013.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson JW, Hatch EE, Webster TF. Exposure to polyfluoroalkyl chemicals and cholesterol, body weight, and insulin resistance in the general U.S. population. Environ Health Perspect. 2010;118(2):197–202. doi: 10.1289/ehp.0901165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tian YP, Zeng XW, Bloom MS, et al. Isomers of perfluoroalkyl substances and overweight status among Chinese by sex status: Isomers of C8 Health Project in China. Environ Int. 2019;124:130–138. doi: 10.1016/j.envint.2019.01.006 [DOI] [PubMed] [Google Scholar]
- 18.Cardenas A, Hauser R, Gold DR, et al. Association of Perfluoroalkyl and Polyfluoroalkyl Substances With Adiposity. JAMA Netw open. 2018;1(4):e181493. doi: 10.1001/jamanetworkopen.2018.1493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu G, Dhana K, Furtado JD, et al. Perfluoroalkyl substances and changes in body weight and resting metabolic rate in response to weight-loss diets: A prospective study. PLoS Med. 2018;15(2). doi: 10.1371/journal.pmed.1002502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ding N, Karvonen-Gutierrez CA, Herman WH, Calafat AM, Mukherjee B, Park SK. Perfluoroalkyl and polyfluoroalkyl substances and body size and composition trajectories in midlife women: the study of women’s health across the nation 1999–2018. Int J Obes. Published online 2021. doi: 10.1038/s41366-021-00848-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin CY, Chen PC, Lin YC, Lin LY. Association among serum perfluoroalkyl chemicals, glucose homeostasis, and metabolic syndrome in adolescents and adults. Diabetes Care. 2009;32(4):702–707. doi: 10.2337/dc08-1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lind L, Zethelius B, Salihovic S, Van Bavel B, Lind PM. Circulating levels of perfluoroalkyl substances and prevalent diabetes in the elderly. Diabetologia. 2014;57(3):473–479. doi: 10.1007/s00125-013-3126-3 [DOI] [PubMed] [Google Scholar]
- 23.Cardenas A, Hivert MF, Gold DR, et al. Associations of perfluoroalkyl and polyfluoroalkyl substances with incident diabetes and microvascular disease. Diabetes Care. 2019;42(9):1824–1832. doi: 10.2337/dc18-2254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carey RM, Whelton PK, Aronow WS, et al. Prevention, detection, evaluation, and management of high blood pressure in adults: Synopsis of the 2017 American College of Cardiology/American Heart Association Hypertension Guideline. Ann Intern Med. 2018;168(5):351–358. doi: 10.7326/M17-3203 [DOI] [PubMed] [Google Scholar]
- 25.Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115mmHg, 1990–2015. JAMA - J Am Med Assoc. 2017;317(2):165–182. doi: 10.1001/jama.2016.19043 [DOI] [PubMed] [Google Scholar]
- 26.Lin PID, Cardenas A, Hauser R, et al. Per- and polyfluoroalkyl substances and blood pressure in pre-diabetic adults—cross-sectional and longitudinal analyses of the diabetes prevention program outcomes study. Environ Int. 2020;137:105573. doi: 10.1016/j.envint.2020.105573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Min JY, Lee KJ, Park JB, Min KB. Perfluorooctanoic acid exposure is associated with elevated homocysteine and hypertension in US adults. Occup Environ Med. 2012;69(9):658–662. doi: 10.1136/oemed-2011-100288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bao WW, Qian Z, Geiger SD, et al. Gender-specific associations between serum isomers of perfluoroalkyl substances and blood pressure among Chinese: Isomers of C8 Health Project in China. Sci Total Environ. 2017;607–608: 1304–1312. doi: 10.1016/j.scitotenv.2017.07.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pitter G, Zare Jeddi M, Barbieri G, et al. Perfluoroalkyl substances are associated with elevated blood pressure and hypertension in highly exposed young adults. Environ Heal 2020 191. 2020;19(1):1–11. doi: 10.1186/S12940-020-00656-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Christensen KY, Raymond M, Thompson BA, Anderson HA. Perfluoroalkyl substances in older male anglers in Wisconsin. Environ Int. 2016;91:312–318. doi: 10.1016/j.envint.2016.03.012 [DOI] [PubMed] [Google Scholar]
- 31.Donat-Vargas C, Bergdahl IA, Tornevi A, et al. Associations between repeated measure of plasma perfluoroalkyl substances and cardiometabolic risk factors. Environ Int. 2019;124:58–65. doi: 10.1016/j.envint.2019.01.007 [DOI] [PubMed] [Google Scholar]
- 32.Geiger SD, Xiao J, Shankar A. No association between perfluoroalkyl chemicals and hypertension in children. Integr Blood Press Control. 2014;7(1):1–7. doi: 10.2147/IBPC.S47660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El Khoudary SR, Aggarwal B, Beckie TM, et al. Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association. Circulation. 2020;142:506–532. doi: 10.1161/CIR.0000000000000912 [DOI] [PubMed] [Google Scholar]
- 34.Santoro N, Taylor ES, Sutton-Tyrrell K. The SWAN Song: Study of Women’s Health Across the Nation’s Recurring Themes. Obstet Gynecol Clin North Am. 2011;38(3):417–423. doi: 10.1016/j.ogc.2011.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park SK, Peng Q, Ding N, Mukherjee B, Harlow SD. Determinants of per- and polyfluoroalkyl substances (PFAS) in midlife women: Evidence of racial/ethnic and geographic differences in PFAS exposure. Environ Res. 2019;175:186–199. doi: 10.1016/j.envres.2019.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ding N, Harlow SD, Batterman S, Mukherjee B, Park SK. Longitudinal trends in perfluoroalkyl and polyfluoroalkyl substances among multiethnic midlife women from 1999 to 2011: The Study of Women′s Health Across the Nation. Environ Int. 2020;135:105381. doi: 10.1016/j.envint.2019.105381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang X, Mukherjee B, Batterman S, Harlow SD, Park SK. Urinary metals and metal mixtures in midlife women: The Study of Women’s Health Across the Nation (SWAN). Int J Hyg Environ Health. 2019;222(5):778–789. doi: 10.1016/j.ijheh.2019.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carey RM, Cutler J, Friedewald W, et al. The 1984 report of the joint national committee on detection, evaluation and treatment of high blood pressure. Nurse Pract. 1985;10(7):9–33. doi: 10.1097/00006205-198507000-000033974955 [DOI] [Google Scholar]
- 39.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. J Am Med Assoc. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 40.Kato K, Basden BJ, Needham LL, Calafat AM. Improved selectivity for the analysis of maternal serum and cord serum for polyfluoroalkyl chemicals. J Chromatogr A. 2011;1218(15):2133–2137. doi: 10.1016/j.chroma.2010.10.051 [DOI] [PubMed] [Google Scholar]
- 41.Hornung RW, Reed LD. Estimation of Average Concentration in the Presence of Nondetectable Values. Appl Occup Environ Hyg. 1990;5(1):46–51. doi: 10.1080/1047322X.1990.10389587 [DOI] [Google Scholar]
- 42.Wassertheil-Smoller S, Anderson G, Psaty BM, et al. Hypertension and Its Treatment in Postmenopausal Women. Hypertension. 2000;36(5):780–789. doi: 10.1161/01.HYP.36.5.780 [DOI] [PubMed] [Google Scholar]
- 43.Coghlin J, Hammond SK, Gann PH. Development of epidemiologic tools for measuring environmental tobacco smoke exposure. Am J Epidemiol. 1989;130(4):696–704. doi: 10.1093/oxfordjournals.aje.a115391 [DOI] [PubMed] [Google Scholar]
- 44.Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med (Baltim). 1999;28(3):313–323. doi: 10.1006/pmed.1998.0470 [DOI] [PubMed] [Google Scholar]
- 45.Thiébaut ACM, Bénichou J. Choice of time-scale in Cox’s model analysis of epidemiologic cohort data: A simulation study. Stat Med. 2004;23(24):3803–3820. doi: 10.1002/sim.2098 [DOI] [PubMed] [Google Scholar]
- 46.Keil AP, Buckley JP, O’Brien KM, Ferguson KK, Zhao S, White AJ. A quantile-based g-computation approach to addressing the effects of exposure mixtures. Environ Health Perspect. 2020;128(4). doi: 10.1289/EHP5838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carrico C, Gennings C, Wheeler DC, Factor-Litvak P. Characterization of Weighted Quantile Sum Regression for Highly Correlated Data in a Risk Analysis Setting. J Agric Biol Environ Stat. 2015;20(1):100–120. doi: 10.1007/s13253-014-0180-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ding N, Karvonen-Gutierrez CA, Herman WH, Calafat AM, Mukherjee B, Park SK. Associations of perfluoroalkyl and polyfluoroalkyl substances (PFAS) and PFAS mixtures with adipokines in midlife women. Int J Hyg Environ Health. 2021;235. doi: 10.1016/J.IJHEH.2021.113777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barger PM, Kelly DP. PPAR signaling in the control of cardiac energy metabolism. Trends Cardiovasc Med. 2000;10(6):238–245. doi: 10.1016/S1050-1738(00)00077-3 [DOI] [PubMed] [Google Scholar]
- 50.Gilde AJ, Van der Lee KAJM, Willemsen PHM, et al. Peroxisome proliferator-activated receptor (PPAR) α and PPARβ/δ, but not PPARγ, modulate the expression of genes involved in cardiac lipid metabolism. Circ Res. 2003;92(5):518–524. doi: 10.1161/01.RES.0000060700.55247.7C [DOI] [PubMed] [Google Scholar]
- 51.Wolf CJ, Takacs ML, Schmid JE, Lau C, Abbott BD. Activation of mouse and human peroxisome proliferator-activated receptor alpha by perfluoroalkyl acids of different functional groups and chain lengths. Toxicol Sci. 2008;106(1):162–171. doi: 10.1093/toxsci/kfn166 [DOI] [PubMed] [Google Scholar]
- 52.Takacs ML, Abbott BD. Activation of mouse and human peroxisome proliferator-activated receptors (α, β/δ, γ) by perfluorooctanoic acid and perfluorooctane sulfonate. Toxicol Sci. 2007;95(1):108–117. doi: 10.1093/toxsci/kfl135 [DOI] [PubMed] [Google Scholar]
- 53.Danzi S, Klein I. Thyroid Hormone and Blood Pressure Regulation. Published online 2003. [DOI] [PubMed]
- 54.Ballesteros V, Costa O, Iñiguez C, Fletcher T, Ballester F, Lopez-Espinosa MJ. Exposure to perfluoroalkyl substances and thyroid function in pregnant women and children: A systematic review of epidemiologic studies. Environ Int. 2017;99:15–28. doi: 10.1016/j.envint.2016.10.015 [DOI] [PubMed] [Google Scholar]
- 55.Khansari MR, Yousefsani BS, Kobarfard F, Faizi M, Pourahmad J. In vitro toxicity of perfluorooctane sulfonate on rat liver hepatocytes: probability of distructive binding to CYP 2E1 and involvement of cellular proteolysis. Environ Sci Pollut Res. 2017;24(29):23382–23388. doi: 10.1007/s11356-017-9908-2 [DOI] [PubMed] [Google Scholar]
- 56.Han R, Hu M, Zhong Q, et al. Perfluorooctane sulphonate induces oxidative hepatic damage via mitochondria-dependent and NF-KB/TNF-A-mediated pathway. Chemosphere. 2018;191:1056–1064. doi: 10.1016/j.chemosphere.2017.08.070 [DOI] [PubMed] [Google Scholar]
- 57.Zhao D, Guallar E, Ouyang P, et al. Endogenous Sex Hormones and Incident Cardiovascular Disease in Post-Menopausal Women. J Am Coll Cardiol. 2018;71(22):2555–2566. doi: 10.1016/j.jacc.2018.01.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ding N, Harlow SD, Randolph JF, et al. Associations of Perfluoroalkyl Substances with Incident Natural Menopause: The Study of Women’s Health across the Nation. J Clin Endocrinol Metab. 2020;105(9):E3169–E3182. doi: 10.1210/clinem/dgaa303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harlow SD, Hood MM, Ding N, et al. Per- and Polyfluoroalkyl Substances and Hormone Levels During the Menopausal Transition. J Clin Endocrinol Metab. 2021;106(11):e4427–e4437. doi: 10.1210/CLINEM/DGAB476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.G D, J Z, Y C, et al. Combined effects of PFOS and PFOA on zebrafish (Danio rerio) embryos. Arch Environ Contam Toxicol. 2013;64(4):668–675. doi: 10.1007/S00244-012-9864-2 [DOI] [PubMed] [Google Scholar]
- 61.Ojo AF, Peng C, Ng JC. Combined effects and toxicological interactions of perfluoroalkyl and polyfluoroalkyl substances mixtures in human liver cells (HepG2). Environ Pollut. 2020;263:114182. doi: 10.1016/J.ENVPOL.2020.114182 [DOI] [PubMed] [Google Scholar]
- 62.Wang X, Karvonen-Gutierrez CA, Herman WH, Mukherjee B, Harlow SD, Park SK. Urinary metals and incident diabetes in midlife women: Study of Women’s Health Across the Nation (SWAN). BMJ Open Diabetes Res Care. 2020;8(1):e001233. doi: 10.1136/BMJDRC-2020-001233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang X, Mukherjee B, Karvonen-Gutierrez CA, et al. Urinary metal mixtures and longitudinal changes in glucose homeostasis: The Study of Women’s Health Across the Nation (SWAN). Environ Int. 2020;145:106109. doi: 10.1016/j.envint.2020.106109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang X, Karvonen-Gutierrez CA, Herman WH, Mukherjee B, Harlow SD, Park SK. Urinary Heavy Metals and Longitudinal Changes in Blood Pressure in Midlife Women: The Study of Women’s Health Across the Nation. Hypertension. Published online 2021:543–551. doi: 10.1161/HYPERTENSIONAHA.121.17295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang X, Mukherjee B, Park SK. Associations of cumulative exposure to heavy metal mixtures with obesity and its comorbidities among U.S. adults in NHANES 2003–2014. Environ Int. 2018;121:683–694. doi: 10.1016/j.envint.2018.09.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang X, Mukherjee B, Park SK. Does Information on Blood Heavy Metals Improve Cardiovascular Mortality Prediction? J Am Heart Assoc. 2019;8(21):e013571. doi: 10.1161/JAHA.119.013571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American College of Cardiology/American Heart Association Task Force on Clinical practice guidelines. Hypertension. 2018;71(6):E13–E115. doi: 10.1161/HYP.0000000000000065/-/DC2 [DOI] [PubMed] [Google Scholar]
- 68.Gu A, Yue Y, Desai RP, Argulian E. Racial and Ethnic Differences in Antihypertensive Medication Use and Blood Pressure Control Among US Adults With Hypertension: The National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovasc Qual Outcomes. 2017;10(1). doi: 10.1161/CIRCOUTCOMES.116.003166 [DOI] [PubMed] [Google Scholar]
- 69.Hu XC, Andrews DQ, Lindstrom AB, et al. Detection of Poly- and Perfluoroalkyl Substances (PFASs) in U.S. Drinking Water Linked to Industrial Sites, Military Fire Training Areas, and Wastewater Treatment Plants. Environ Sci Technol Lett. 2016;3(10):344–350. doi: 10.1021/acs.estlett.6b00260 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


