Abstract
BACKGROUND
During the SARS-CoV-2 pandemic, cannabis dispensaries in the United States (US) reported increased sales.
OBJECTIVES
This study assessed changes in cannabis use before to during the pandemic; it was hypothesized that cannabis use increased during the pandemic.
METHODS
A US-based survey of adults assessed patterns of use before and during the pandemic. Participants recruited via social media from 8/2020 to 9/2020 self-reported medical and non-medical cannabis use. Use was categorized as ≤ monthly, weekly, and daily/almost daily; adjusted logistic regressions determined associations between cannabis use before the pandemic with change in frequency during the pandemic.
RESULTS
Of 1,886 respondents (63% male), 1,113 reported non-medical and 603 medical use of cannabis. Those reporting ≤monthly non-medical use before the pandemic had higher odds of increasing use during the pandemic than those using weekly before the pandemic (AOR 3.2 [95% CI 2.2–4.5]). Those reporting ≤ monthly and daily medical cannabis use before the pandemic had higher odds of increasing use during the pandemic than those using weekly before the pandemic (AOR 2.3 [95% 1.3, 3.9]; AOR 2.4 [95% CI 1.2, 5.1] respectively).
CONCLUSIONS
The most notable increases in cannabis use during the pandemic were among those who reported using cannabis least frequently before the pandemic (two to three times odds of increased use among ≤ monthly use compared to weekly). These findings have important implications for potential health consequences related to increased cannabis use both during and after the pandemic, even in populations thought to be protected by minimal use prior to the pandemic.
Keywords: Cannabis, cannabinoids, COVID-19, SARS-CoV-2
Introduction
Nearly 50% of Americans struggle with SARS-CoV-2 (COVID-19) pandemic-related mental health issues, including increases in substance use (1). Before the pandemic, cannabis use was widespread with over 46% of Americans, 12 years of age or older, reporting cannabis use in 2019 (2). This is of concern during the pandemic because cannabis use disorder (CUD), marked by heavy cannabis use, is associated with increased risk of COVID-19 infection (adjusted odds ratios [AOR] = 5.3 [4.3–6.4]) (3). Cannabis inhalation (smoking/vaping) may also increase susceptibility to COVID-19 infection and severity of outcomes (4). During the pandemic, cannabis dispensaries have been deemed essential businesses in many states with some regions reporting increases in cannabis sales (5), yet these statistics do not capture actual changes in use. Recent studies have probed changes in cannabis use during the COVID-19 pandemic but have been restricted to a small population (i.e., <100) of people who primarily use cannabis daily (6), restricted to people who use cannabis for medical reasons (7), or those who did not use cannabis for medical reasons (8). The objective of this study was to assess changes in patterns of both self-reported medical and non-medical cannabis use during the pandemic across a general group of those who use cannabis and to identify variables associated with changes in use. These modifications are important as they may impact COVID-19 related outcomes and likely predict the expected landscape of cannabis use post pandemic and potential health outcomes associated with use.
Methods
Study design
An anonymous US-based web survey collected data on cannabis-related behaviors from August – September 2020 among adults (≥18 years) reporting any cannabis and/or cannabidiol use in the last 12 months through an online HIPAA-compliant Qualtrics XM platform for computer, tablet, and wireless devices. Respondents were a nonrandom convenience sample recruited via Reddit, Bluelight, Craigslist, and Twitter, consented to participate, and provided a $5 incentive upon survey completion; respondents completed the survey once and were restricted to prevent “ballot stuffing” by IP-address. Questions of non-medical and medical cannabis behaviors before the pandemic (January to mid-March 2020) and during the pandemic (past 3 months) were asked separately (9). Participants were included in this analysis if they reported any medical or non-medical cannabis use in the last 12 months. Participants were asked, “In the past year, I used: (Check all that apply)” with answer choices: non-medical cannabis (marijuana); cannabis (marijuana) for medical reasons; CBD only products; none of the above; and declined to answer. Participants who noted CBD only products, none of the above, or declined to answer were excluded for this study. All participants provided online consent. This study received institutional review board approval from the University of California, Los Angeles.
Study outcomes were change in cannabis frequency and mode of use before versus during the pandemic. Cannabis use frequency was assessed as: never; once or twice; monthly; weekly; daily or almost daily (9). Those reporting daily use were asked about frequency per day with answer choices: 1–2, 3–5, 6–10, and more than 10 times per day. Change in cannabis use frequency was dichotomized as increasing (increased cannabis use before the pandemic compared to during the pandemic) and stayed the same (no change in use). Participants were also asked if they believed their cannabis use changed during the pandemic compared to before. For non-medical cannabis use, this was asked as “Compared to 3 months before the pandemic (January 2020- mid-March 2020), during the pandemic (since mid-March 2020) I have changed how often I used non-medical cannabis (marijuana):” with answer choices: strongly agree; somewhat agree; neither agree nor disagree; somewhat disagree; and strongly disagree. For medical cannabis use this was asked as “Compared to 3 months before the pandemic (January 2020 – mid-March 2020), during the pandemic (since mid-March 2020) I have changed how often I used cannabis (marijuana) for medical reasons:” with similar answer choices.
Mode of cannabis use was assessed as “I used the following method the most:” with answer choices: smoking; vaporizing plant; vaping oil/concentrates; wax/dab; edibles; other oral products; topicals; or other. Change in mode of use was dichotomized as changed from inhalation (smoking, vaporizing plant, vaping/oil concentrates, wax/dab) to oral (edibles, other oral products) compared to no change in inhalation.
The exposure, frequency of cannabis use before the pandemic, was categorized as no reported use (if a respondent selected ‘never use’ in the 3-month time period before the pandemic), less than or equal to monthly (used once – monthly), weekly, and daily (daily/almost daily [1–10 times per day]).
Participants could indicate medical cannabis use, non-medical cannabis use, or both; however, questions for medical and non-medical cannabis use were asked separately in the survey. Thus, we treated these variables as independent groups for the purpose of this study.
Variables investigated as potential confounders included state’s cannabis regulatory status dichotomized as regulated (adult-use and/or medical use) and unregulated (10), age and sex.
Statistical analyses
Frequency distributions, mean, and standard deviations were calculated for the overall sample and by those self-reporting non-medical and medical cannabis use. Age was continuous and followed a normal distribution. Multivariable logistic regressions compared reported cannabis use before the pandemic to change in use frequency and mode of use during the pandemic. Models adjusted for state’s cannabis regulatory status (10), age, and sex. Separate models were run for medical and non-medical cannabis. Those not reporting cannabis use in the 3-month period before the pandemic were excluded from the statistical models because of small sample size. We identified that those not reporting use 3 months prior to the pandemic were too different from those categorized as less than or equal to monthly use (once – monthly) prior to the pandemic and thus, we omitted these observations from the model instead of collapsing them with less than or equal to monthly use. However, we did report frequency distributions of cannabis use during the pandemic for those who did not report cannabis use in the three months before the pandemic. Age in the models was centered at 34 years (mean age) and rescaled to a 10-unit change. Analyses were conducted using SAS v.9.4 (SAS Institute, Cary, NC).
Results
Of the 2,000 respondents, 1,886 were eligible and completed the survey including 1,113 reporting non-medical and 603 reporting medical cannabis use. Respondents were 63.0% male, non-Hispanic White (52.97%), had an associate’s degree or higher education (59.3%) with mean age 33.7(± 8.8) years. Respondents were primarily from states with regulated cannabis laws (75.6%) and distributed across the US: West (37.7%); Midwest (11.8%); Northeast (17.8%); and South (32.8%). Over 75% of those reporting either non-medical or medical cannabis use somewhat/strongly agreed that they changed how often they used cannabis during the pandemic compared to before (Table 1).
Table 1.
Frequency distribution of demographics overall and by cannabis use (medical/non-medical) among a national cannabis using population, August 2020 - September 2020
| Overall | Non-Medical Cannabis* | Medical Cannabis* | |
|---|---|---|---|
|
|
|||
| n (%) | n (%)** | n (%)** | |
| Total | 1886 (100.0) | 1113 (100.0) | 603 (100.0) |
| Demographics | |||
| Age, years | |||
| Mean (Standard Deviation) | 33.7 (8.8) | 33.5 (9.4) | 35.2 (10.1) |
| Age, years | |||
| 18-24 | 153 (8.11) | 117 (10.51) | 39 (6.47) |
| 25-34 | 1039 (55.09) | 624 (56.06) | 310 (51.41) |
| 34-44 | 488 (25.87) | 246 (22.10) | 164 (27.20) |
| 45-54 | 100 (5.30) | 61 (5.48) | 38 (6.30) |
| 55-64 | 59 (3.12) | 36 (3.23) | 32 (5.31) |
| 65-74 | 18 (0.95) | 15 (1.35) | 11 (1.82) |
| Sex | |||
| Female | 666 (35.31) | 374 (33.60) | 215 (35.66) |
| Male | 1189 (63.04) | 724 (65.05) | 379 (62.85) |
| Other | 2 (0.11) | 2 (0.18) | 1 (0.17) |
| Sexual orientation | |||
| Straight/Heterosexual | 1270 (67.34) | 753 (67.65) | 387 (64.18) |
| Gay | 272 (14.42) | 152 (13.66) | 84 (13.93) |
| Lesbian | 158 (8.38) | 89 (8.00) | 63 (10.45) |
| Bisexual | 101 (5.36) | 70 (6.29) | 42 (6.97) |
| Other | 45 (2.39) | 29 (2.61) | 15 (2.49) |
| Race/Ethnicity | |||
| Hispanic/Latino | 511 (27.09) | 330 (29.65) | 178 (29.52) |
| Non-Hispanic Asian | 36 (1.91) | 24 (2.16) | 8 (1.33) |
| Non-Hispanic Black | 202 (10.71) | 94 (8.45) | 70 (11.61) |
| Non-Hispanic American Indian or Alaska Native | 51 (2.70) | 18 (1.62) | 20 (3.32) |
| Non-Hispanic Native Hawaiian or Pacific Islander | 17 (0.90) | 7 (0.63) | 9 (1.49) |
| Non-Hispanic White | 999 (52.97) | 593 (53.28) | 296 (49.09) |
| Non-Hispanic Other | 24 (1.27) | 18 (1.62) | 8 (1.33) |
| Unknown | 46 (2.44) | 29 (2.61) | 14 (2.32) |
| Education | |||
| Less than High School | 160 (8.48) | 107 (9.61) | 37 (6.14) |
| High school | 215 (11.40) | 144 (12.94) | 49 (8.13) |
| Some college credit, no degree | 357 (18.93) | 218 (19.59) | 126 (20.90) |
| Associates degree | 530 (28.10) | 272 (24.44) | 194 (32.17) |
| College graduate or higher | 589 (31.23) | 355 (31.90) | 188 (31.18) |
| Region | |||
| West | 711 (37.70) | 418 (37.56) | 219 (36.32) |
| Midwest | 222 (11.77) | 137 (12.31) | 63 (10.45) |
| Northeast | 335 (17.76) | 215 (19.32) | 142 (23.55) |
| South | 618 (32.77) | 343 (30.82) | 179 (29.68) |
| State’s Legality | |||
| Fully Regulated | 836 (44.33) | 535 (48.07) | 271 (31.67) |
| Medical Only | 589 (31.23) | 325 (29.20) | 191 (22.55) |
| CBD Only | 434 (23.01) | 240 (21.56) | 136 (22.55) |
| Unregulated | 27 (1.43) | 13 (1.17) | 5 (0.83) |
| Cannabis Behavior | |||
| Changed cannabis use frequency during pandemic | |||
| Strongly agree/Somewhat agree | -- | 852 (76.55) | 454 (75.42) |
| Neither agree not disagree | -- | 141 (12.67) | 87 (14.45) |
| Somewhat disagree/Strongly disagree | -- | 120 (10.78) | 61 (10.13) |
| Mode of use (before; during) | |||
| Inhalation | -- | 938 (87.66); 915 (85.51) | 421 (75.18); 413 (72.84) |
| Oral | -- | 132 (12.34); 155 (14.49) | 139 (24.82); 154 (27.16) |
Not mutually exclusive categories;
May not add to 100% because of missing data
Reported prevalence of less than or equal to monthly non-medical cannabis use before the pandemic decreased by 12.32% while 40.81% increased and 46.87% stayed the same during the pandemic. Weekly non-medical cannabis use decreased by 21.47%, 16.38% increased and 62.15% remained the same. Finally, daily cannabis use decreased by 29.57% whereas 20.43% increased and 50.00% stayed the same (Table 2). In a more detailed assessment, 33.33% of those who reported using non-medical cannabis once or twice before the pandemic (n = 228) reported monthly use, 16.23% reported weekly use, and 1.75% reported daily use during the pandemic. Of those who reported monthly use before the pandemic (n = 267), 27.72% reported weekly use and 4.12% reported daily use during the pandemic. Of those who reported weekly use before the pandemic (n = 354), 16.38% reported daily use during the pandemic; of which, 59.65% reported using 1–2 times per day, 29.82% reported using 3–5 times a day, 7.02% reported using 6–10 times per day; and 3.51% reported using more than 10 times per day. Moreover, of those who reported not using non-medical cannabis 3 months before the pandemic (n = 34), 14.71% reported using once or twice, 14.71% reported monthly use, 11.76% reported weekly use, and 11.76% reported daily use during the pandemic (data not shown). After controlling for age, sex, and state’s cannabis regulatory status, those reporting less than or equal to monthly non-medical cannabis use before the pandemic had higher odds of reporting increased use during the pandemic compared to those reporting weekly use (AOR 3.2 [95%] CI 2.2–4.5). Being female and from a regulated cannabis state were positively associated with increasing use during the pandemic (Figure 1).
Table 2.
Frequency distribution of change in cannabis use by non-medical and medical use among a national cannabis using population, August 2020 - September 2020
| Change in Non-Medical Cannabis | Change in Medical Cannabis | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Decrease n (%) | Stay the same n (%) | Increase n (%) | Decrease n (%) | Stay the same n (%) | Increase n (%) | |
| Cannabis Behavior | ||||||
| Frequency of use before COVID-19 | ||||||
| Did not report use | -- | 16 (47.06) | 18 (52.94) | -- | 12 (42.86) | 16 (57.14) |
| Once or twice use | 8 (3.51) | 103 (45.18) | 117 (51.32) | 4 (2.70) | 81 (54.73) | 63 (42.57) |
| Monthly use | 53 (19.85) | 129 (48.31) | 85 (31.84) | 56 (28.43) | 98 (49.75) | 43 (21.83) |
| Weekly use | 76 (21.47) | 220 (62.15) | 58 (16.38) | 27 (21.09) | 79 (61.72) | 22 (17.19) |
| Daily or almost daily use | 68 (29.57) | 115 (50.0) | 47 (20.43) | 27 (27.84) | 40 (41.24) | 30 (30.93) |
| Frequency of use before COVID-19 (Categorized) | ||||||
| Less than or equal to monthly | 61 (12.32) | 232 (46.87) | 202 (40.81) | 60 (17.39) | 179 (51.88) | 106 (30.72) |
| Weekly | 76 (21.47) | 220 (62.15) | 58 (16.38) | 27 (21.09) | 79 (61.72) | 22 (17.19) |
| Daily or almost daily | 68 (29.57) | 115 (50.00) | 47 (20.43) | 27 (27.84) | 40 (41.24) | 30 (30.93) |
Less than or equal to monthly=once/twice or monthly use;
Figure 1.
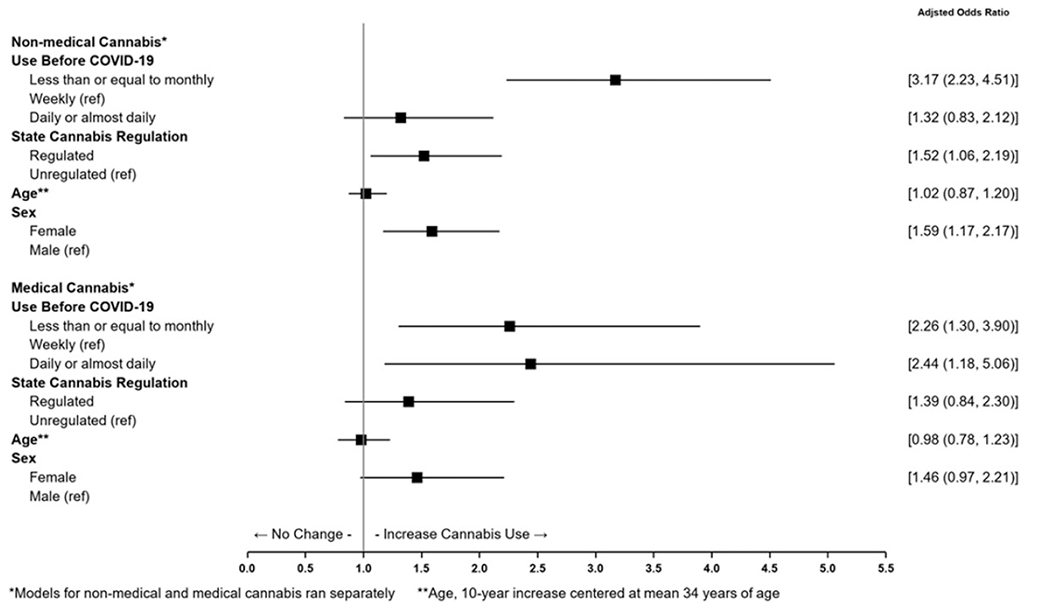
Adjusted logistic regression of non-medical and medical cannabis frequency of use before to during the pandemic among a cannabis using population, August-September 2020. Data were collected on those whoreported cannabis and/or cannabidiol use in the United States in a single web-based survey to assess cannabis behaviors before and during the COVID-19 pandemic. Multivariable logistic regressions were conducted to assess the association of cannabis behaviors before the pandemic to changes in behaviors during the pandemic. Figure 1 shows cannabis use before the COVID-19 pandemic on change in cannabis use during the COVID-19 pandemic. Change in cannabis use during the COVID-19 pandemic was dichotomized as increased or stayed the same (reference). Models for non-medical and medical cannabis use were conducted separately (denoted with a * in Figure 1). Adjusted odds ratio and 95% confidence intervals (denoted as 95% CI in Figure 1) are presented and displayed in a forest plot. State’s cannabis regulatory status, participant’s age, and participant’s sex were adjusted for in the models. Age was recentered at mean age and rescaled per 10-unit increase (denoted as Age** in Figure 1). Sample sizes for the models were: non-medical cannabis (n = 848); medical cannabis (n = 474).
Reported prevalence of less than or equal to monthly medical cannabis use before the pandemic decreased by 17.39% whereas 30.72% increased use and 51.88% stayed the same during the pandemic. A majority of those reporting weekly medical use before the pandemic (61.72%) remained the same during the pandemic while 17.19% increased. Finally, 30.93% of those reporting daily medical cannabis use increased their use whereas 41.24% remained the same and 27.84% decreased their use (Table 2). Of those reporting medical cannabis use once or twice before the pandemic (n = 148), 29.73% reported monthly use, 8.11% reported weekly use, and 4.73% reported daily use during the pandemic. Of those reporting monthly use before the pandemic (n = 197), 17.26% reported weekly use and 4.57% reported daily use during the pandemic. And, of those reporting weekly use before the pandemic (n = 128), 17.19% reported daily use during the pandemic; of which 54.55% reported using 1–2 times per day, 31.82% reported using 3–5 times per day, and 13.64% reported using 6 to 10 times per day. Similarly, of those not reporting use of medical cannabis before the pandemic (n = 28), 14.29% reported using once or twice, 17.86% reported monthly use, 7.14% reported weekly use, and 17.86% reported daily use during the pandemic (data not shown). Among those reporting medical cannabis use, those with less than or equal to monthly and daily cannabis use before the pandemic had higher odds of reporting increased medical use during the pandemic than those reporting weekly use (AOR 2.3 [95% CI 1.3, 3.9] and AOR 2.4 [95% CI 1.2, 5.1] respectively) (Figure 1).
Mode of cannabis use did not significantly change during the pandemic (Figure 2); inhalation was reported as the primary mode of use before and during the pandemic (87.7% vs. 85.5% non-medical and 75.2% vs 72.8% medical respectively).
Figure 2.
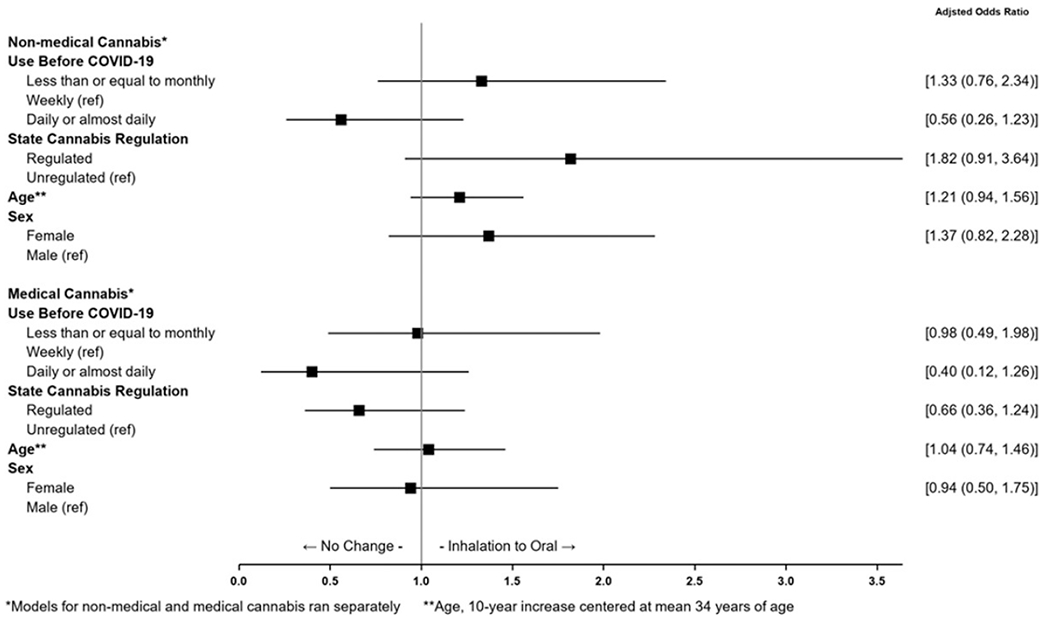
Adjusted logistic regression of non-medical and medical cannabis frequency of use before the pandemic on change in mode of cannabis use during the pandemic among a cannabis using population, August-September 2020. Data were collected on those who reported cannabis and/or cannabidiol use in the United States in a single web-based survey to assess cannabis behaviors before and during the COVID-19 pandemic. Multivariable logistic regressions were conducted to assess the association of cannabis behaviors before the pandemic to changes in behaviors during the pandemic. Figure 2 shows cannabis use before the COVID-19 pandemic on change in mode of use during the COVID-19 pandemic. Change in mode of use was dichotomized as change from inhalation to oral or did not change from inhalation to oral (reference). Models for non-medical and medical cannabis use were conducted separately (denoted with a * in Figure 2). Adjusted odds ratio and 95% confidence intervals (denoted as 95% CI in Figure 2) are presented and displayed in a forest plot. State’s cannabis regulatory status, participant’s age, and participant’s sex were adjusted for in the models. Age was recentered at mean age and rescaled per 10-unit increase (denoted as Age** in Figure 2). Sample sizes for the models were: non-medical cannabis (n = 894); medical cannabis (n = 406).
Discussion
Overall, there were slight increases in frequency of cannabis use during the COVID-19 pandemic among those who were using cannabis before the pandemic. These do not appear to represent major changes in patterns of use but are more suggestive of small transitions in levels of frequency. Those reporting weekly and daily use sustained their patterns of use during the pandemic. The most notable changes were among those who reported using non-medical cannabis the least frequently (i.e. “occasionally”) before the pandemic. Those reporting less than or equal to monthly non-medical use were 3 times more likely to increase use during the pandemic than those reporting weekly use. Those reporting less than or equal to monthly and daily medical use were more than 2 times likely to increase use during the pandemic than those reporting weekly use, a pattern of change on both ends of the spectrum of use. Additionally, there was an increase of non-medical and medical cannabis among those who did not report cannabis use for either purpose in the 3 months before the pandemic. Particularly, 52.94% of those who reported not using non-medical cannabis 3 months before the pandemic reported increase use during the pandemic. Similarly, 57.14% of those who reported not using medical cannabis 3 months before the pandemic reported increased use during the pandemic. Increases in cannabis use during the pandemic may be two-fold. First, these increases may be due to a direct or indirect effect of the COVID-19 pandemic, increased time at home, or anxiety related to the pandemic. On the other hand, increases may be due to the rising trend of cannabis use, availability, and accessibility as cannabis laws continue to shift in the United States (11). It was believed that cannabis uptake may substantially increase during the pandemic, but in our sample that was not the case (12–14).
Findings of note included that individuals from states with regulated cannabis were more likely to increase their cannabis use than individuals from other states with unregulated cannabis. This may be due to cannabis accessibility during the pandemic. Additionally, women were more likely to report increased cannabis use during the pandemic. This finding reflects recent national annual trends of increasing use among females compared to males for both medical and non-medical cannabis use (2,15,16). Because COVID-19 is a respiratory illness and cannabis inhalation may negatively impact COVID-19 outcomes (4), it was expected, but not observed, that there would have been a change from inhalation to oral mode of administration. Changes in mode of cannabis use may be detectable in a larger and more diverse sample.
This study has limitations including that respondents were a nonrandom convenience sample of cannabis using participants who self-selected into a web-based survey and were primarily White and educated. As such, results may not be generalized to all those who use cannabis in the United States, nor may we make conclusions to those who newly initiated cannabis use. Second, data for this study period were captured before the peak of the COVID-19 pandemic in many of the states in the US. Therefore, it would be important to reevaluate changes in cannabis use behavior at subsequent time points during the pandemic. Third, the small sample size for change in mode of use may have meant not enough power to capture such changes. Fourth, as in all studies of self-reported behaviors, respondents may have suffered from recall bias resulting in misclassification of frequency of use. Fifth, CUD was not assessed limiting conclusions related to changes in CUD severity. Moreover, we did not have data on sociopolitical or economic disparities that individuals may have faced before and during the pandemic and therefore could not control for these factors. Finally, participants self-reported whether their cannabis use was non-medical or medical use. We could not confirm whether a participant received a physician’s recommendation for medical cannabis use. This may lead to misclassification of medical cannabis use, but we do not believe this impacts the general conclusions made in this study.
This study highlights the course of changes in cannabis use from before and during the pandemic for non-medical and medical cannabis and variables associated with these changes. It was hypothesized that the pandemic will lead to large increases of cannabis use, but that may have not been the case. In our sample, those reporting weekly and daily use before the pandemic maintained their use patterns during the pandemic. What is unknown is whether the pandemic created new users, or how the use of cannabis affected those using other substances such as alcohol, tobacco, and opioids. Because cannabis use has been associated with the presence and severity of CUD (17) and early signals demonstrate that CUD increases COVID-19 susceptibility (3), it is important to monitor cannabis use in different populations during the pandemic. Moreover, monitoring frequency of use should continue since little is known about the impact of non-medical and medical cannabis use on pandemic-related mental health consequences. Because the most notable changes in frequency of use were seen among those who did not use much before the pandemic, there is a need to identify general and mental health outcomes associated with cannabis use even in populations thought to be protected by minimal use prior to the pandemic. It will be important to follow whether these such increases will continue and to carefully observe the outcomes among this sizable population.
Funding
This study was supported by the National Institute on Drug Abuse Grants DA047296, U01DA036267, and U24DA044554 DA047296 and the Semel Charitable Foundation.
Footnotes
Disclosure statement
Dr. Cooper reports serving on the scientific advisory board of FSD Pharma. The submitted work is independent of this role. No other disclosures were reported.
References
- [1].Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24 –30, 2020. MMWR Morb Mortal Wkly Rep. 2020. Aug 14;69:1049–57. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Substance Abuse and Mental Health Services Administration. 2019 NSDUH detailed tables [Internet]. 2020. Sep [accessed 2020 Nov9]. https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables.
- [3].Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry [Internet]. 2020. Sep 14 [accessed 2020 Nov8]. http://www.nature.com/articles/s41380-020-00880-7. [DOI] [PMC free article] [PubMed]
- [4].Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 2020. Jul 7;173:61–62. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Michigan Marijuana Regulatory Agency. Marijuana Regulatory Agency Statistical Report [Internet]. 2020. [accessed 2020 Nov10]. https://www.michigan.gov/mra/0,9306,7-386-93032-497635–,00.html.
- [6].Miller K, Laha-Walsh K, Albright DL, McDaniel J. Cannabis use during the COVID-19 pandemic: results from a longitudinal study of cannabis users. J Subst Use. 2021. Feb 14. 1–5. . [Google Scholar]
- [7].Vidot DC, Islam JY, Camacho-Rivera M, Harrell MB, Rao DR, Chavez JV, G. Ochoa L, Hlaing WM, Weiner M, Messiah SE, et al. The COVID-19 cannabis health study: results from an epidemiologic assessment of adults who use cannabis for medicinal reasons in the United States. J Addict Dis. 2020. Dec 1;39:26–36. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].van Laar MW, Oomen PE, van Miltenburg CJA, Vercoulen E, Freeman TP, Hall WD. Cannabis and COVID-19: reasons for Concern. Front Psychiatry. 2020. Dec 21;11:601653. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Group WAW. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility: ASSIST: development, reliability and feasibility. Addiction. 2002. Sep;97:1183–94. . [DOI] [PubMed] [Google Scholar]
- [10].Britannica ProCon. Legal medical marijuana states and DC [Internet]. [accessed Dec 27]. https://medicalmarijuana.procon.org/legal-medical-marijuana-states-and-dc/.
- [11].Hasin D, Walsh C. Trends over time in adult cannabis use: a review of recent findings. Curr Opin Psychol. 2021. Apr;38:80–85. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ashby NJS. Anonymized location data reveals trends in legal cannabis use in communities with increased mental health risks at the start of the COVID-19 pandemic. J Addict Dis. 2021;39:436–440. [DOI] [PubMed] [Google Scholar]
- [13].Tortolani P Why the pandemic was a breakout moment for the cannabis industry. New York Times [Internet]. 2021. May 31 [accessed 2021 Jul 6]. https://www.nytimes.com/2021/05/31/business/cannabis-marijuana-industry-pandemic-dispensaries.html
- [14].Price E Covid-19 is helping make 2020 a record year for cannabis sales. Forbes [Internet]. 2020. Aug 3 [accessed 2021 Jul 6]. https://www.forbes.com/sites/emilyprice/2020/08/03/covid-is-helping-make-2020-a-record-year-for-cannabis-sales/.
- [15].Cooper ZD, Adinoff B. Necessity of addressing motivations for cannabis use to guide research. Am J Drug Alcohol Abuse. 2019;45:547–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cooper ZD, Craft RM. Sex-dependent effects of cannabis and cannabinoids: a translational perspective. Neuropsychopharmacology. 2018. Jan;43:34—51. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, Jung J, Zhang H, Grant BF. Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the national epidemiologic survey on alcohol and related conditions–III. Am J Psychiatry. 2016. Jun; 173:588–99. . [DOI] [PMC free article] [PubMed] [Google Scholar]


