Abstract
Background:
Extreme heat events are increasing due to climate change. Prior studies, typically limited to urban settings, suggest an association between extreme heat and cardiovascular mortality. But the extent of the burden of cardiovascular deaths associated with extreme heat across the US and in different age, gender, or race and ethnicity subgroups is unclear.
Methods:
County-level daily maximum heat index levels for all counties in the contiguous US in summer months (May through September) and monthly cardiovascular mortality rates for adults 20 years of age and older were obtained. For each county, an extreme heat day was identified if the maximum heat index was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period (1979 to 2007) for that day. Spatial empirical Bayes smoothed monthly cardiovascular mortality rates from 2008 to 2017 were the primary outcome. A Poisson fixed effects regression model was estimated with the monthly number of extreme heat days as the independent variable of interest. The model included time fixed effects, and time varying environmental, economic, demographic and healthcare related variables.
Results:
Across 3,108 counties, from 2008 to 2017, each additional extreme heat day was associated with a 0.12% (95% CI 0.04% to 0.21%, p=0.004) higher monthly cardiovascular mortality rate. Extreme heat was associated with an estimated 5,958 (95% CI 1,847 to 10,069) additional deaths from cardiovascular disease over the study period. In sub-group analyses, extreme heat was associated with a greater relative increase in mortality rates among men compared to women [0.20% (95% CI 0.07% to 0.33%)], and non-Hispanic Black compared to non-Hispanic White adults [0.19% (95% CI 0.01% to 0.37%)]. There was a greater absolute increase among elderly compared to non-elderly adults [16.6 (95% CI 14.6 to 31.8) additional deaths per 10 million individuals per month].
Conclusion:
Extreme heat days were associated with higher adult cardiovascular mortality rates in the contiguous US between 2008 and 2017. This association was heterogeneous among age, gender, race, and ethnicity subgroups. As extreme heat events increase, the burden of cardiovascular mortality may continue to increase and the disparities between demographic subgroups may widen.
Keywords: Climate Change, Extreme Heat, Population Health, Health Status Disparities
Introduction:
Climate change has led to an increase in extreme weather events, including extreme heat, which will play an increasingly important role in the health of communities. Patients with cardiovascular disease are at a high risk of morbidity and mortality from extreme heat. However, the burden of this may fall unequally based on factors such as age, gender, race, and ethnicity. With the projected continued increase in extreme heat events in the United States (US),1 understanding the association between extreme heat and cardiovascular mortality, and identifying vulnerable subgroups, is important.
Extreme heat is associated with health outcomes, including hospitalizations and deaths.2–6 Deaths due to heat stroke are a minority of the overall deaths attributed to extreme heat.7, 8 As patients with cardiovascular disease and risk factors are especially vulnerable to the effects of extreme heat,9, 10 deaths from cardiovascular disease may be an important contributor to overall heat-related deaths. Extreme heat has also been associated with cardiovascular emergency department visits and hospitalizations.2, 10–12 Most previous studies of extreme heat and cardiovascular health in the US have been limited to urban areas.7, 13 Due to the geographically limited nature of these studies, the burden of cardiovascular mortality associated with extreme heat across the US is largely unknown. As the association between extreme heat and health is likely to vary across the country based on factors such as urban development, vegetation, and demographic profiles,14, 15 studying the association across a greater proportion of the country is necessary to understand the extent of the association between extreme heat and cardiovascular mortality.
There may also be heterogeneity among subgroups of age, gender, race, and ethnicity. Elderly individuals are vulnerable to the health effects of extreme heat related, in part, to the higher burden of medical comorbidities.11, 12, 16 In the US racial minorities also experience a disproportionately greater burden of some of the adverse health effects of extreme heat.11, 17, 18 Whether such disparities exist for cardiovascular mortality, particularly across the US, is not as well known. Identifying which subgroups, and to what extent, have a disproportionately greater association between extreme heat and mortality may help in targeted interventions to minimize the potential adverse effects.
To study the association between extreme heat and cardiovascular mortality, and to evaluate heterogeneity across subgroups of interest, we examined county-level occurrence of extreme heat days and cardiovascular mortality rates across the contiguous US from 2008 to 2017.
Methods:
All data used is publicly available from sources listed below. Analytic methods will be made available to other researchers for purposes of reproducing the results upon request. This analysis was exempt from review based on the University of Pennsylvania institutional review board guidelines and informed consent was waived.
Extreme heat
The primary exposure of interest was the monthly number of extreme heat days. Extreme heat refers to temperatures significantly higher than usual for a particular locality.19 To define extreme heat in summer months (May to September) in each county in the contiguous US from 2008 to 2017, we used daily maximum heat index levels obtained from the Centers for Disease Control and Prevention’s (CDC) Environmental Public Health Tracking Program.20 A baseline period from 1979 to 2007 was established, and extreme heat for each summer day from 2008 to 2017 in each county was identified if the maximum heat index on that day was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period for that specific day.
Mortality rates:
County-level, age-adjusted (standardized to the 2000 US Census), monthly cardiovascular mortality rates for all residents 20 years of age and older were first calculated for summer months in the years 2008 to 2017 using data from the National Center for Health Statistics. Death due to cardiovascular diseases was identified if the primary cause of death was due to any diseases of the circulatory system [International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) codes I00 to I99]. In secondary analyses, mortality rates for ischemic heart disease, stroke, and an alternative narrower definition of cardiovascular diseases, were also identified (Supplemental Table S1). Death certificate data identifying the deceased individual’s age, gender, race, and ethnicity was used to calculate mortality rates for different sub-groups of interest. Death certificate information on race/ethnicity has been shown to have near perfect agreement with self-reported Black and White race, and excellent agreement for Hispanic ethnicity (around 97%).21
To account for instability in monthly mortality rate estimates,22 rates were smoothed using spatial empirical Bayes smoothing. This technique creates more stable mortality rate estimates by “borrowing strength or confidence” from mortality rates in neighboring counties.23 Counties with a larger population contribute to a greater degree to the smoothed estimate than counties with a smaller population. Additional details on this technique are in Supplemental Methods 1.
Other data sources used are listed in Supplemental Methods 2.
Outcomes
The primary outcome was the monthly, county-level, age-adjusted, cardiovascular mortality rate for all individuals 20 years of age and older from May to September in the years 2008 to 2017. Secondary outcomes include mortality rates in sub-groups based on age, gender, race, and ethnicity, and deaths due to ischemic heart disease and stroke.
Statistical Analysis
Summary measures for the total number of cardiovascular deaths for all adults, as well as for age, gender, race, and ethnicity subgroups across all of the counties were first calculated. We then calculated summary measures of county-level demographic, clinical and healthcare related variables between counties based on tertiles of the total number of extreme heat days from 2008 to 2017. Population-weighted median cardiovascular mortality rates for each tertile were also calculated.
Poisson fixed effects model
To account for potential time-invariant differences between counties, we fit a Poisson fixed effects regression model with monthly deaths as the outcome and the number of extreme heat days in each month as the predictor of interest. The fixed effects approach controls for both observed and unobserved time-invariant confounders by examining change in the predictor and outcome variables within a given subject (county in this case) over time.24 The Poisson fixed effects estimator was chosen as it is robust to issues of overdispersion.25 A negative binomial fixed effects estimator was not used as it is not considered robust to violations in its assumptions.26 Additional details on the fixed effects model are available in Supplemental Methods 3. Month and year fixed effects were included in the model to account for secular time trends. The model also included additional time-varying covariates that could potentially confound the association between extreme heat and cardiovascular mortality rates, as per the CDC’s National Environmental Public Health Tracking Network, as well as additional important environmental, economic, and healthcare related variables.20 Covariates included in the model are listed in Supplemental Methods 4. State level cluster-robust standard errors were used. Absolute change in mortality rates associated with 1 extreme heat day per month (compared to no extreme heat days) were estimated from the fixed effects model at the mean values of the included covariates. Using the regression coefficients from the fixed effects model, the county population, the number of extreme heat days in each county, and the value of each included covariate, the total number of additional cardiovascular deaths associated with extreme heat across all counties was estimated. The univariate association between each of the covariates included in the model and cardiovascular mortality using fixed effects models, as well as the distribution across all counties, was also examined. The primary model was compared with two alternative versions: 1) including the monthly number of extreme heat days as a quadratic variable and 2) including each of the other covariates as linear splines with 5 knots. Goodness of fit was assessed using the Bayesian information criterion.
Secondary and sensitivity analyses
Secondary analyses included fitting fixed effects models with the following outcomes: cardiovascular mortality rates in different sub-groups [non-elderly (20–64 years of age), elderly (65 years of age and older), men, women, non-Hispanic White, non-Hispanic Black, non-Hispanic other race, and Hispanic (any race)] and stratifications (by county metropolitan status, US Census regions, and by tertiles of counties based on the total number of extreme heat days during the study period), and ischemic heart disease and stroke mortality rates. For each sub-group the outcome was deaths among the specific subgroup in each county and the population of the subgroup in each county was used as the offset variable. The region and tertile stratified models did not use state clustered standard errors due to the small number of states in each stratum. To test whether the associations for the different subgroups and strata were significantly different from each other, we refit additional models which simultaneously estimated the associations for the subgroups of interest and used an interaction term between the subgroup and each of the independent variables.27 We also examined the association for the age, gender, race, and ethnicity subgroups for metropolitan and non-metropolitan counties separately.
As air quality can impact cardiovascular health,28, 29 we refit the primary model with different measures of air quality. We first included the monthly number of days with air quality unhealthy for sensitive groups or worse using the Air Quality Index (AQI). AQI values are calculated for 5 (ozone, particle matter, carbon monoxide, sulfur dioxide, nitrogen dioxide) pollutants. The daily AQI for an area is the highest value for any of the pollutants in a given day.30 Air quality data, obtained from the Environmental Protection Agency (EPA), is measured at monitors located in more populous areas of the country. AQI data was available in 1,019 to 1,027 counties over the study period which included approximately 81% of the contiguous US adult population. In a second model, we included monthly number of days with fine particulate matter (PM2.5) concentration and monthly number of days with ozone concentration above the EPA National Ambient Air Quality Standard thresholds of 35 μg/m3 and 0.07 parts per million respectively.31 As this data includes measurements from both monitoring stations and modeled data, it includes all counties, and was available from 2008 to 2016. We fit an additional model including the percentage of county land with forest cover and the percentage of land developed (available for all counties in 2008, 2011, 2013, and 2016). Additional sensitivity analyses included using alternative definitions of extreme heat (maximum daily heat index ≥90°F (32.2°C) and in the 95th or 90th percentile of the maximum heat index in the baseline period) and cardiovascular mortality (using an alternative set of ICD-10 codes) (Supplemental Table S1). We also assessed the association between cardiovascular mortality and occurrence of a heat wave (three or more consecutive days of extreme heat) in a given month.
Results are presented as means with standard deviations (SD) or 95% confidence intervals (CI) or medians with interquartile range (IQR). All p-values were two-sided and values ≤0.05 were considered statistically significant. Empirical Bayes smoothing was performed using Geoda. Other statistical analyses were conducted using Stata 17 (College Station, TX). The Stata module ppmlhdfe was used to fit the Poisson fixed effects models.32
Results
The analysis included all 3,108 counties in the contiguous US. There were 3,139,134 cardiovascular deaths among adults living in the contiguous US during summer months from 2008 to 2017 [median 337 (IQR 153 to 792)] (Table 1). Of these, 50.0% occurred among women and 80.5% among elderly adults. The median number of deaths was 296 (IQR 128 to 705) for non-Hispanic White adults, 14 (IQR 2 to 87) for non-Hispanic Black adults, 2 (IQR 1 to 9) for non-Hispanic other race adults, and 2 (IQR 1 to 11) for Hispanic adults. From 2008 to 2017, the median number of extreme heat days was 89 (IQR 61 to 122). The median number of extreme heat days was 45 (IQR 75 to 82) in the first tertile, 90 (IQR 92 to 97) in the second tertile, and 133 (122 to 148) in the third tertile of counties (Figure 1, Table 2). The median county adult population was 21,423 (IQR 6,986 to 66,125) in the first tertile, 21,234 (IQR 10,244 to 55,135) in the second tertile, and 16,547 (IQR 8,351 to 35,326) in the third tertile of counties. The median proportion of non-Hispanic White residents was 49.6% (IQR 81.5% to 95.4%) in the first tertile, 89.0% (IQR 70.1% to 96.1%) in the second tertile, and 78.4% (IQR 63.1% to 91.0%) in the third tertile. The median proportion of non-Hispanic Black residents was 0.6% (IQR 0.3% to 2.2%) in the first tertile, 2.6% (IQR 0.5% to 13.3%) in the second tertile, and 6.0% (IQR 1.4% to 21.5%) in the third tertile. The median household income was $43,471 (IQR $38,515 to $49,786) in the first tertile, $42,667 ($36,685 to $48,531) in the second tertile, and $37,595 ($32,979 to $42,832) in the third tertile. Other economic, demographic, and healthcare related variables for each tertile of counties are listed in Table 2.
Table 1:
Total number of cardiovascular deaths across all counties in the contiguous United States during summer months from 2008 to 2017
| Total number of deaths (percentage of all adult deaths) | Median (IQR) number of deaths across all counties during study period | |
|---|---|---|
| All adults (20 years and older) | 3,139,134 | 337 (153 to 792) |
| Non-elderly (20 to 64 years old) | 610,919 (19.5) | 66 (27 to 162) |
| Elderly (65 years and older) | 2,528,215 (80.5) | 272 (123 to 641) |
| Female | 1,568,899 (50.0) | 166 (75 to 388) |
| Male | 1,570,235 (50.0) | 177 (79 to 404) |
| Non-Hispanic Black | 381,737 (12.2) | 14 (2 to 87) |
| Non-Hispanic White | 2,496,154 (79.5) | 296 (128 to 705) |
| Non-Hispanic other race | 76,787 (2.4) | 2 (1 to 9) |
| Hispanic (any race) | 175,057 (5.6) | 2 (1 to 11) |
Figure 1 –
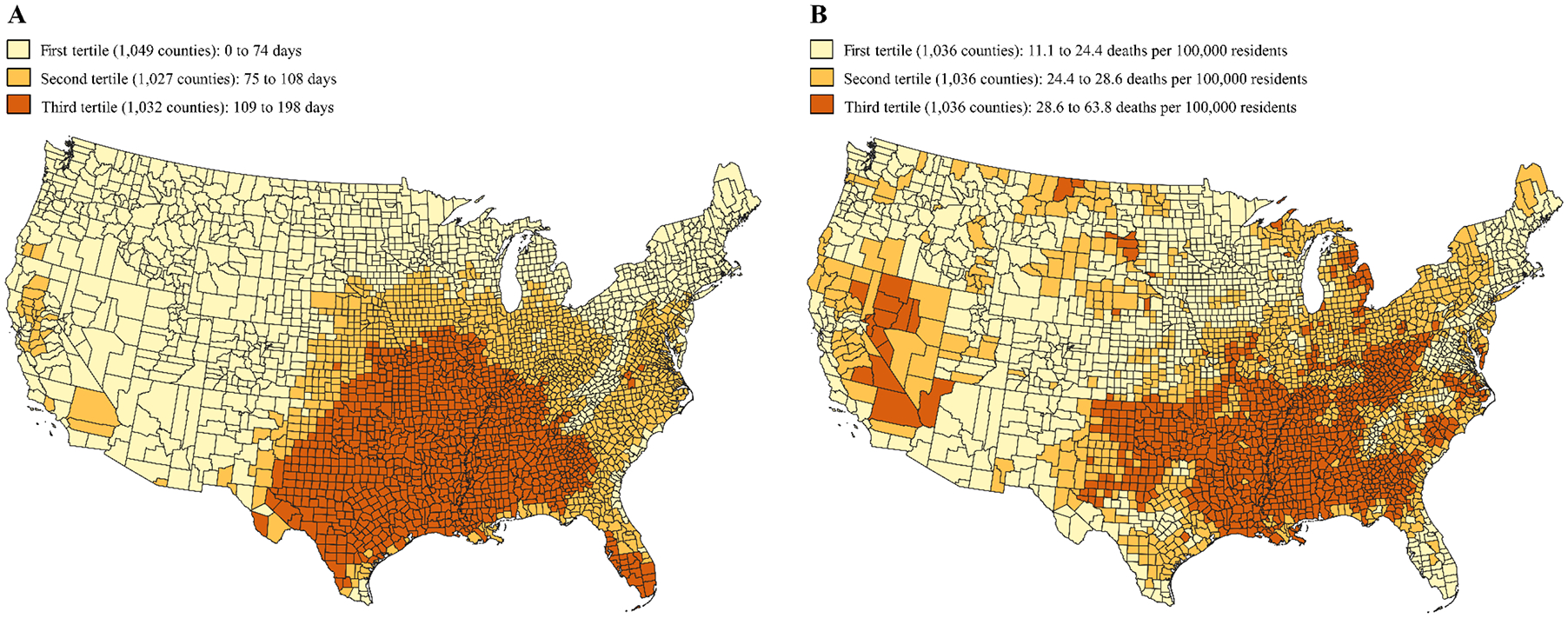
US County map of total number of extreme heat days and mean, summer, monthly cardiovascular mortality rates from 2008 to 2017
Panel A – Tertiles of US counties by total number of extreme heat days in summer months (May to September) from 2008 to 2017
Panel B – Tertiles of US counties by mean monthly age-adjusted cardiovascular mortality rates (after spatial empiric Bayes smoothing) in summer months (May to September) from 2008 to 2017 among adults 20 years of age and older
Extreme heat day designated if maximum heat index on that day was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period (1979 to 2007)
Table 2:
County characteristics by tertile of total number of extreme heat days*
| First Tertile | Second Tertile | Third quartile | |||
|---|---|---|---|---|---|
| Number of counties | 1,049 | 1,027 | 1,032 | ||
| Median (IQR) | |||||
| Total number of extreme heat days from 2008 to 2017† | 45 (17, 82) | 90 (92, 97) | 133 (122, 148) | ||
| Population (20 years and older) | 21,424 (6,986, 66,126) | 21,234 (10,244, 55,135) | 16,547 (8,351, 35,326) | ||
| Percentage | |||||
| Proportion of county adult residents | |||||
| Elderly (65 years and older) | 23.4 (20.0, 27.1) | 21.9 (19.3, 24.6) | 22.4 (19.5, 25.1) | ||
| Female | 50.4 (49.4, 51.3) | 51.2 (50.4, 51.9) | 51.4 (50.3, 52.2) | ||
| Male | 49.6 (48.7, 50.6) | 48.8 (48.1, 49.6) | 48.6 (47.8, 49.7) | ||
| Non-Hispanic Black | 0.6 (0.3, 2.2) | 2.6 (0.5, 13.3) | 6.0 (1.4, 21.5) | ||
| Non-Hispanic White | 91.7 (81.6, 95.4) | 89.0 (70.1, 96.1) | 78.4 (63.1, 91.0) | ||
| Non-Hispanic other race | 2.7 (1.7, 4.8) | 1.7 (1.2, 2.9) | 1.8 (1.4, 2.7) | ||
| Hispanic (any race) | 2.9 (1.4, 7.3) | 2.9 (1.5, 5.8) | 2.8 (1.5, 8.6) | ||
| Unemployment rate | 6.6 (5.1, 8.0) | 7.0 (5.2, 8.4) | 7.1 (5.8, 8.5) | ||
| Poverty rate | 13.9 (11.0, 17.1) | 14.5 (11.2, 19.5) | 18.3 (15.0, 22.0) | ||
| Non-elderly (18 to 64 year old) adults without health insurance | 15.9 (12.1, 19.8) | 16.9 (13.4, 20.3) | 22.1 (18.4, 25.4) | ||
| Percentage of adults with diabetes | 8.0 (7.2, 9.1) | 9.8 (8.5, 11.3) | 10.7 (9.3, 12.1) | ||
| Metropolitan counties‡ | 34.5 | 42.8 | 34.7 | ||
| US Census Regions | |||||
| Midwest | 35.5 | 44.0 | 22.4 | ||
| Northeast | 17.5 | 3.3 | 0 | ||
| South | 10.8 | 49. 6 | 77.5 | ||
| West | 36.3 | 3.1 | 0.1 | ||
| Median household income ($)§ | 43,472 (38,515, 49,786) | 42,667 (36,685, 48,531) | 37,595 (32,979, 42,832) | ||
| Number of primary care providers per 100,000 adult residents | 77.8 (52.2, 108.1) | 64.3 (43.5, 90.0) | 53.9 (34.4, 77.6) | ||
| Number of hospital beds per 100,000 adult residents | 295.6 (139.2, 522.5) | 264.2 (105.8, 508.3) | 288.3 (119.9, 521.3) | ||
Extreme heat day designated if maximum heat index on that day was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period (1979 to 2007). All values are averaged over the study period (2008 to 2017)
In summer months (May to September)
County metropolitan status based on the 2013 National Center for Health Statistics Urban-Rural Classification Scheme
Inflation adjusted to 2008 US dollars
Primary analysis
Mean monthly cardiovascular mortality rates for each county over the study period are shown in Figure 1. The population-weighted median monthly cardiovascular mortality rate was 22.8 (IQR 20.4 to 25.8) deaths per 100,000 individuals in the first tertile, 24.9 (IQR 22.4 to 27.4) in the second tertile, and 26.2 (IQR 23.5 to 30.3) in the third tertile. Median mortality rates, over the study period, for each of the 5 summer months for the 3 tertiles of counties are displayed in Figure 2 (Supplemental Table S2). In the Poisson fixed effects regression model, 1 additional extreme heat day per month was associated with 0.12% (95% CI 0.04% to 0.21%, p=0.004) higher monthly cardiovascular mortality rates and 3.14 (95% CI 1.04 to 5.24) additional deaths per 10 million adults per month (Table 3). Extreme heat was associated with an estimated 5,958 (95% CI 1,847 to 10,069) additional cardiovascular deaths in summer months from 2008 to 2017 in the contiguous US among adults. Annual number of estimated excess deaths ranged from 331 (95% CI 104 to 558) in 2008 to 1,014 (95% CI 321 to 1,707) in 2011 (Figure 3, Supplemental Table S3). Trends by US Census region are displayed in Figure 4 (Supplemental Table S4).
Figure 2 –
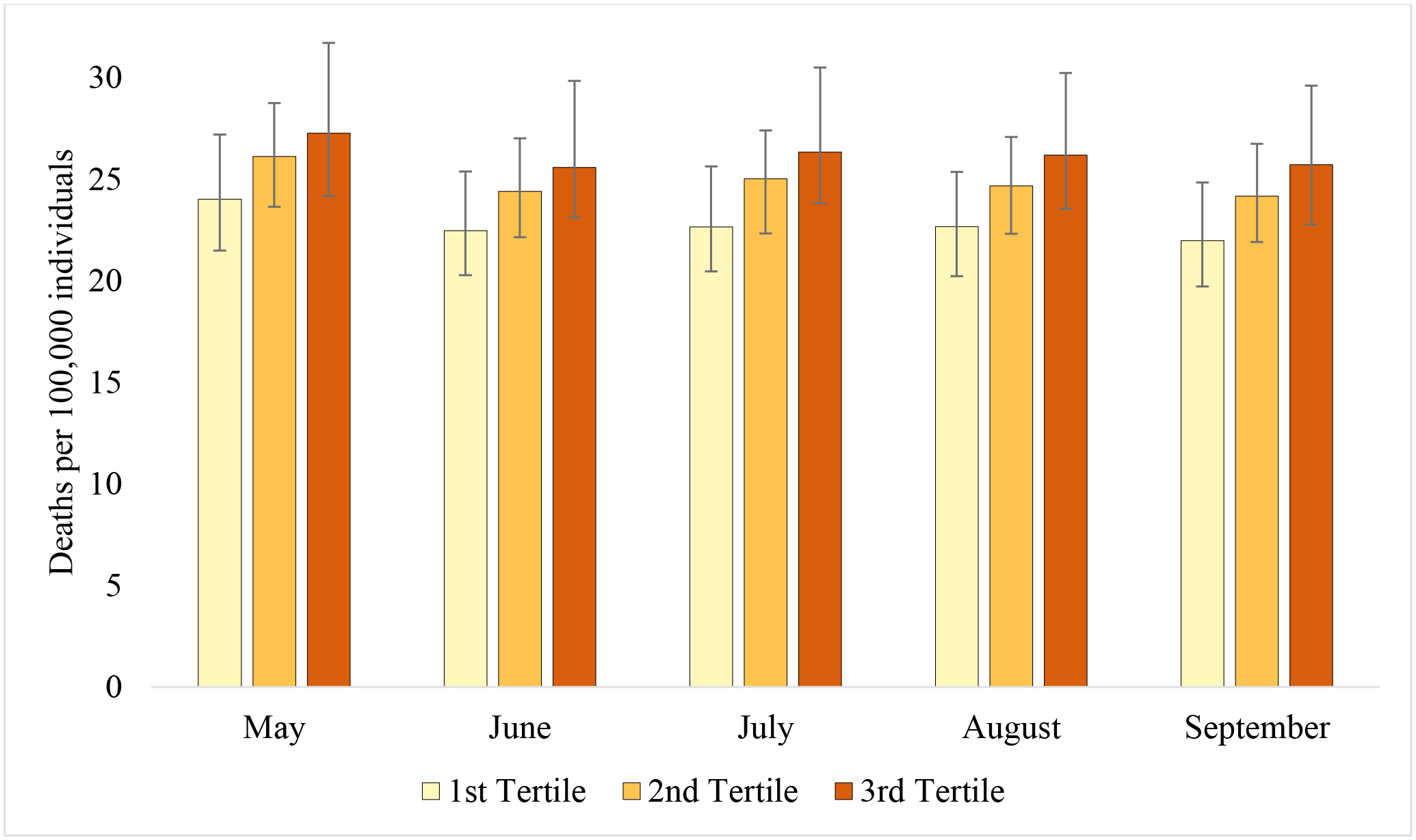
County-level median monthly cardiovascular mortality rates by tertiles of total number of extreme heat days from 2008 to 2017*†
* Tertiles of US counties by total number of extreme heat days in summer months (May to September) from 2008 to 2017. 1st tertile : 0 to 74 days, 2nd tertile 75 to 108 days, 3rd tertile: 109 to 198 days. Extreme heat day designated if maximum heat index on that day was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period (1979 to 2007)
† Age-adjusted cardiovascular mortality rates for all adults 20 years of age and older. Mortality rates smoothed with spatial empirical Bayes smoothing. Median values weighted by county adult population.
Table 3:
Poisson fixed effects regression model
| Population | Percent change in monthly mortality rate associated with 1 additional extreme heat day per month (95% CI)* | p-value | Deaths per 10 million individuals per month associated with 1 extreme heat day per month (95% CI)*† | Estimated total number of deaths associated with extreme heat days from 2008 to 2017 (95% CI)†‡ |
|---|---|---|---|---|
| Outcome: Cardiovascular mortality: | ||||
| All adults | 0.13 (0.04 to 0.21) | 0.004 | 3.14 (1.04 to 5.25) | 5,958.1 (1847.4 to 10,068.8) |
| Non-elderly adults (20 to 64 years old) | 0.20 (0.07 to 0.33) | 0.003 | 1.28 (0.41 to 2.16) | 1,749.0 (558.3 to 2,939.7) |
| Elderly adults (65 years and older) | 0.12 (0.02 to 0.21) | 0.02 | 13.08 (2.87 to 23.29) | 4,834.0 (900.6 to 8,767.5) |
| Female | 0.021 (−0.07 to 0.11) | 0.64 | 0.45 (−1.45 to 2.34) | 429.8 (−1,388.5 to 2,248.1) |
| Male | 0.22 (0.10 to 0.34) | <0.001 | 6.56 (3.03 to 10.08) | 6,083.4 (2,748.0 to 9,418.7) |
| Non-Hispanic Black | 0.29 (0.12 to 0.46) | 0.001 | 10.10 (4.07 to 16.14) | 2,582.4 (1,053.0 to 4,111.9) |
| Non-Hispanic White | 0.10 (0.005 to 0.19) | 0.04 | 2.45 (0.13 to 4.77) | 3,090.5 (125.5 to 6,055.5) |
| Non-Hispanic other race | 0.41 (−0.07 to 0.89) | 0.09 | 5.82 (−1.30 to 12.95) | 647.5 (−145.4 to 1,440.5) |
| Hispanic (any race) | 0.07 (−0.14 to 0.27) | 0.54 | 0.84 (−1.84 to 3.52) | 319.4 (−705.4 to 1,344.3) |
| County metropolitan status (all adults) § ‖ | ||||
| Metropolitan | 0.15 (0.06 to 0.24) | 0.001 | 3.64 (1.48 to 5.80) | 5,856.9 (2,250.7 to 9,463.1) |
| Non-metropolitan | 0.05 (−0.06 to 0.17) | 0.35 | 1.54 (−1.68 to 4.77) | 451.8 (−495.5 to 1,399.2) |
| Regions (all adults) | ||||
| Midwest | 0.12 (0.003 to 0.24) | 0.04 | 3.13 (0.09 to 6.16) | 1,302.1 (33.0 to 2,571.2) |
| Northeast | 0.18 (−0.03 to 0.40) | 0.10 | 4.47 (−0.82 to 9.76) | 1,121.2 (−212.7 to 2,455.1) |
| South | 0.12 (0.05 to 0.18) | <0.001 | 2.94 (1.32 to 4.56) | 3,094.7 (1,377.4 to 4,812.1) |
| West | 0.36 (0.17 to 0.55) | <0.001 | 8.36 (3.86 to 12.86) | 1,644.3 (766.8 to 2,521.9) |
| Tertiles of total extreme heat days (all adults) ‖ # | ||||
| First tertile | 0.34 (0.22 to 0.47) | <0.001 | 7.99 (5.02 to 10.97) | 3,791.4 (2,360.5 to 5,222.3) |
| Second tertile | 0.14 (0.04 to 0.25) | 0.01 | 3.48 (1.02 to 5.94) | 2,313.5 (673.3 to 3,953.8) |
| Third tertile | 0.09 (0.13 to 0.16) | 0.02 | 2.39 (0.36 to 4.42) | 1,784.2 (264.0 to 3,304.4) |
| Alternate extreme heat definitions (all adults) | ||||
| 95th percentile | 0.09 (0.03 to 0.14) | 0.002 | 2.15 (0.79 to 3.52) | 7,144.4 (4,015.9 to 10,272.9) |
| 90th percentile | 0.07 (0.02 to 0.11) | 0.01 | 1.61 (0.47 to 2.75) | 7,184.1 (3,604.6 to 10,763.6) |
| Occurrence of a heat wave during a month** | 0.16 (0.07 to 0.26) | 0.001 | 4.10 (1.83 to 6.37) | 2,407.8 (998.9 to 3,816.6) |
| Outcome: Ischemic heart disease mortality | ||||
| All adults | 0.19 (0.07 to 0.31) | 0.002 | 2.27 (0.85 to 3.69) | 4,156.1 (1,458.4 to 6,853.7) |
| Outcome: Stroke mortality | ||||
| All adults | 0.04 (−0.12 to 0.20) | 0.60 | 0.15 (−0.37 to 0.66) | 367.4 (−1,031.1 to 1,766.0) |
Extreme heat day designated if maximum heat index on that day was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period (1979 to 2007).
Confidence interval crossing 0 indicates estimate for number of deaths not statistically significantly different from 0.
Estimates based on fixed effects regression coefficients, annual adult population, monthly number of extreme heat days, and value of each covariate in each county from 2008 to 2017.
County metropolitan status based on the 2013 National Center for Health Statistics Urban-Rural Classification Scheme
State-level clustered standard errors not used due to the small number of states in each stratum
Tertiles of US counties by total number of extreme heat days in summer months (May to September) from 2008 to 2017. 1st tertile : 0 to 74 days, 2nd tertile 75 to 108 days, 3rd tertile: 109 to 198 days.
Heat wave defined as three or more consecutive days of extreme heat in a month
Figure 3:
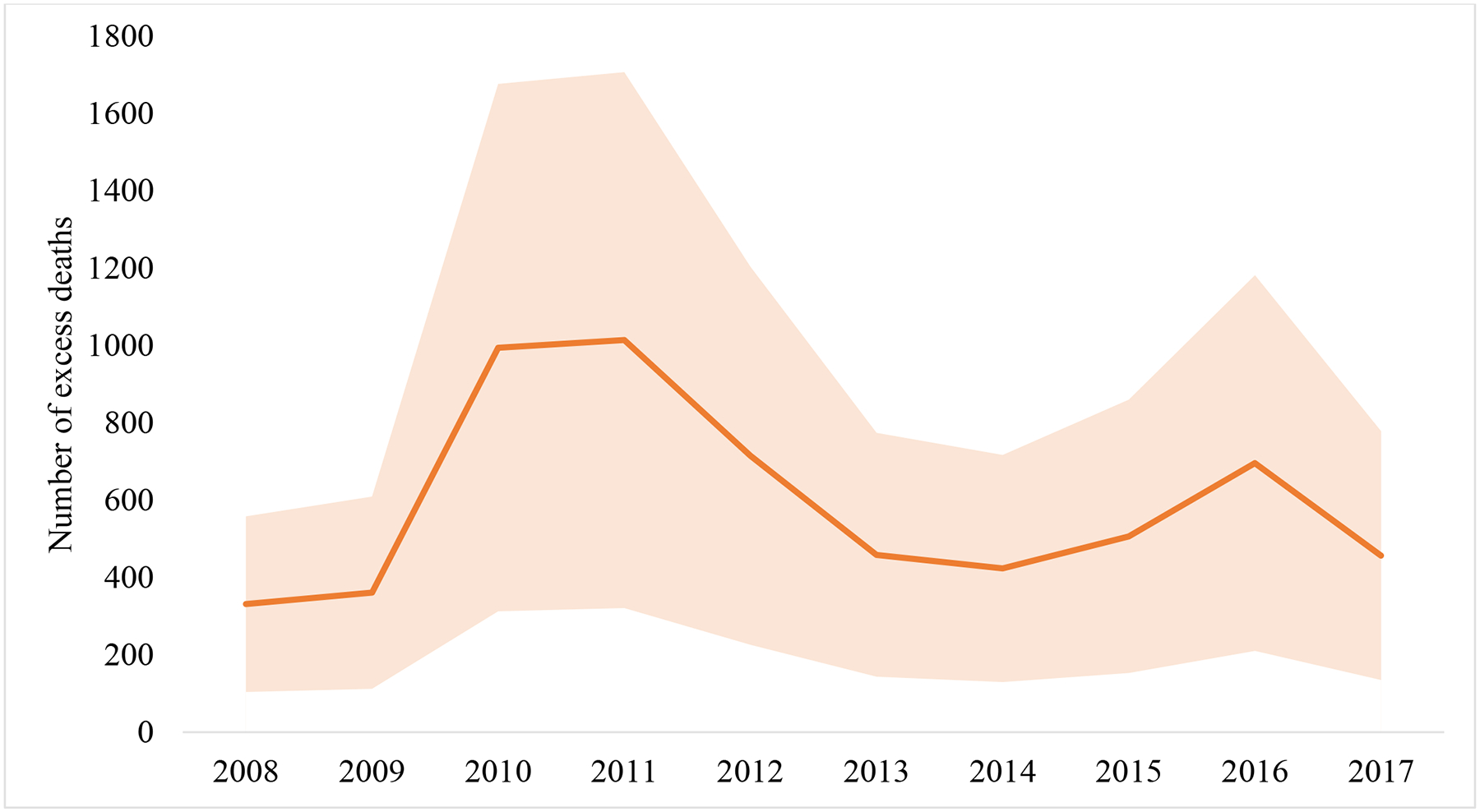
Estimated annual number of excess cardiovascular deaths associated with extreme heat during summer months from 2008 to 2017*†‡
* Age-adjusted cardiovascular mortality rates for all adults 20 years of age and older. Mortality rates smoothed with spatial empirical Bayes smoothing.
†Summer months – May to September
‡Estimates based on fixed effects regression coefficients, annual adult population, monthly number of extreme heat days, and value of each covariate in each county. Shaded areas indicate 95% confidence intervals of the annual estimates.
Figure 4:
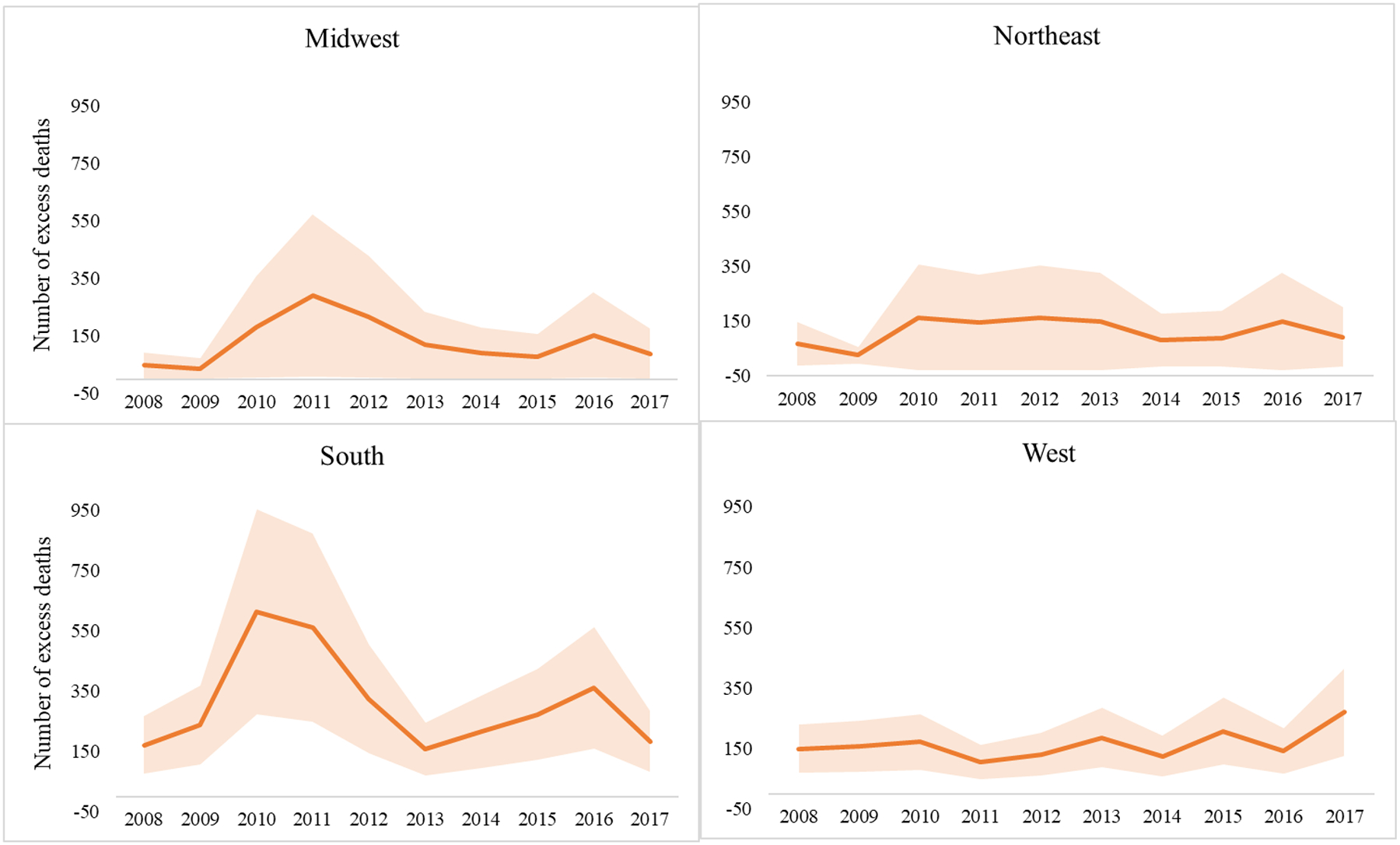
Estimated annual number of excess cardiovascular deaths associated with extreme heat during summer months from 2008 to 2017 by US Census region*†‡
* Age-adjusted cardiovascular mortality rates for all adults 20 years of age and older. Mortality rates smoothed with spatial empirical Bayes smoothing.
†Summer months – May to September
‡Estimates based on fixed effects regression coefficients, annual adult population, monthly number of extreme heat days, and value of each covariate in each county. Shaded areas indicate 95% confidence intervals of the annual estimates.
The univariate association, and distribution across all counties, of each of the included covariates in the primary model are included in Supplemental Table S5 and Supplemental Figures. Comparing the primary model to two alternatives models – including the number of extreme heat days as a quadratic term and including linear splines of the covariates – the association between the extreme heat days and cardiovascular mortality did not change substantially [0.14% (95% CI 0.03% to 0.25%) and 0.13% (95% CI 0.05% to 0.21%), respectively] and goodness of fit did not improve (Supplemental Table S6).
Secondary and sensitivity analyses
One additional extreme heat day was associated with 0.19% (95% CI 0.07% to 0.33%) higher monthly cardiovascular mortality rates among non-elderly adults and 0.12% (95% CI 0.02% to 0.21%) among elderly adults (Table 3). The relative change in monthly mortality did not statistically significantly differ between the two groups, but the absolute increase in mortality rates was statistically significantly greater in the elderly compared to the non-elderly adult population [16.6 (95% CI 14.6 to 31.8) additional deaths per 10 million individuals per month]. (Table 4). The association between extreme heat and cardiovascular mortality rates was statistically significant among men [0.22% (95% CI 0.10% to 0.34%)] but not women [0.02% (95% CI −0.07% to 0.11%)]. This association was statistically significant for non-Hispanic Black and non-Hispanic White adults [0.29% (95% CI −0.12% to 0.46%) and 0.10% (95% CI −0.12% to 0.46%) respectively], but not for non-Hispanic adults of other races or for Hispanic adults [0.41% (95% CI −0.07% to 0.89%) and 0.07% (95% CI −0.14% to 0.27%) respectively]. Compared to non-Hispanic White adults, non-Hispanic Black adults had a significantly greater increase in mortality rates associated with extreme heat [0.19% (95% CI 0.01% to 0.37%)]. The association did not differ significantly between non-Hispanic White adults and the other race and ethnicity subgroups.
Table 4:
Comparison of association between the number of extreme heat days per month and monthly cardiovascular mortality rates between sub-groups*
| Populations | Additional percent change in monthly cardiovascular mortality rate associated with 1 additional extreme heat day per month compared to reference group (95% CI)† | p-value | Difference in additional deaths per 10 million individuals per month associated with 1 extreme heat day per month compared to reference group (95% CI)‡ |
|---|---|---|---|
| Age subgroups | |||
| Non-elderly (20 to 64 years old | Reference | ||
| Elderly (65 years and older) | −0.08 (−0.25 to 0.09) | 0.35 | 16.63 (14.61 to 31.80) |
| Gender subgroups | |||
| Female | Reference | ||
| Male | 0.20 (0.07 to 0.33) | 0.002 | 9.01 (3.66 to 14.35) |
| Race and ethnicity subgroups | |||
| Non-Hispanic White | Reference | ||
| Non-Hispanic Black | 0.19 (0.01 to 0.37) | 0.04 | 8.55 (1.29 to 15.82) |
| Non-Hispanic other race | 0.31 (−0.18 to 0.80) | 0.22 | 0.91 (−5.34 to 7.15) |
| Hispanic (any race) | −0.03 (−0.26 to 0.19) | 0.76 | −1.40 (−8.40 to 5.61) |
| County metropolitan status (all adults) § ‖ | |||
| Non-metropolitan | Reference | ||
| Metropolitan | 0.10 (−0.02 to 0.21) | 0.11 | 3.81 (−0.21 to 7.82) |
| Regions (all adults) | |||
| Midwest | Reference | ||
| Northeast | 0.06 (−0.18 to 0.31) | 0.61 | 1.34 (−4.97 to 7.65) |
| South | −0.004 (−0.14 to 0.13) | 0.96 | 0.75 (−3.12 to 4.62) |
| West | 0.24 (0.02 to 0.46) | 0.03 | 4.98 (−0.83 to 10.79) |
| Tertiles of total extreme heat days (all adults) ‖ # | |||
| First tertile | Reference | ||
| Second tertile | −0.20 (−0.36 to −0.04) | 0.02 | −3.30 (−8.05 to 1.45) |
| Third tertile | −0.26 (−0.41 to −0.11) | 0.001 | −5.11 (−9.29 to −0.93) |
Extreme heat day designated if maximum heat index on that day was ≥90°F (32.2°C) and in the 99th percentile of the maximum heat index in the baseline period (1979 to 2007).
Regression coefficient is the interaction between indicator for sub-group and the number of extreme heat days per month
Confidence interval crossing 0 indicates estimate for number of deaths not statistically significantly different from 0.
County metropolitan status based on the 2013 National Center for Health Statistics Urban-Rural Classification Scheme
State-level clustered standard errors not used due to the small number of states in each stratum
Tertiles of US counties by total number of extreme heat days in summer months (May to September) from 2008 to 2017. 1st tertile : 0 to 74 days, 2nd tertile 75 to 108 days, 3rd tertile: 109 to 198 days.
When stratified by county metropolitan status, the association between extreme heat was statistically significant in metropolitan counties [0.15% (95% CI 0.06% to 0.24%)] but not in non-metropolitan counties [0.05% (95% CI −0.06% to 0.17%)]. The association was significant across all US Census regions, except the Northeast [Midwest: 0.12% (95% CI 0.06% to 0.24%), Northeast: 0.18% (95% CI −0.03% to 0.40%), South: 0.12% (95% CI 0.05% to 0.18%), and West: 0.36% (95% CI 0.17% to 0.55%)]. When stratified by tertiles of counties based on the total number of extreme heat days from 2008 to 2017, the association between extreme heat and cardiovascular mortality was statistically significant for all three tertiles [first tertile: 0.34% (95% CI 0.22% to 0.47%), second tertile: 0.14% (95% CI 0.04% to 0.24%), and third tertile: 0.09% (95% CI 0.01% to 0.16%). Compared to the first tertile, the association was significantly smaller in the third tertile [−0.26% (95% CI −0.41% to −0.11%)].
In metropolitan counties, among subgroups of age, gender, race, and ethnicity, the association between extreme heat and cardiovascular mortality was statistically significant for non-elderly and elderly adults, men, non-Hispanic Black, non-Hispanic White, and non-Hispanic other race adults (Supplemental Table S7). In non-metropolitan counties, the association was statistically significant among men, but none of the other subgroups. Among metropolitan counties, non-Hispanic Black adults had a significantly greater increase in the absolute number of deaths compared to non-Hispanic White adults [8.03 (95% CI 0.55 to 15.5) additional deaths per 10 million individuals], although the relative change was not statistically significantly different [0.17% (95% CI −0.01% to 0.36%)] (Supplemental Table S8).
The association of extreme heat was statistically significant for ischemic heart disease mortality [0.19% (95% CI 0.07% to 0.31%)] but not stroke mortality [0.04% (95% CI −0.12% to 0.20%)] (Table 3). Using a narrower definition of cardiovascular disease, the association with extreme heat and cardiovascular mortality was similar to the primary model [0.14% (95% CI 0.03% to 0.25%)]. Including measures of air quality in the primary model did not substantially change the estimate of the association between extreme heat and cardiovascular mortality [including monthly number of days with air quality unhealthy for sensitive groups or worse (AQI >100): 0.15% (95% CI 0.07% to 0.24%), including number of days with PM2.5 and number of days with ozone concentrations above national thresholds: 0.14% (95% CI 0.05% to 0.23%)]. The association was 0.18% (95% CI 0.04% to 0.32%) after including the proportion of land that was developed and proportion covered by forest in the primary model.
The association between extreme heat and cardiovascular mortality rates was statistically significant when alternative definitions of extreme heat (daily maximum heat index in the 95% or 90% percentile of the baseline period instead of 99% percentile) were used [0.09% (95% CI 0.03% to 0.14%) and 0.07% (95% CI 0.02% to 0.11%) respectively] (Table 3). The estimated total number of deaths associated with extreme heat during the study period were 7,144 (95% CI 4,015 to 10,273) and 7,184 (95% CI 3,605 to 10,764) respectively. The association between the occurrence of a heat wave in a month and monthly cardiovascular mortality rates was 0.16% (95% CI 0.07% to 0.26%).
Discussion:
From 2008 to 2017, across all counties in the contiguous US, extreme heat days were associated with statistically significantly higher monthly cardiovascular mortality rates among adults, with 5,958 (95% CI 1,847 to 10,069) to 7,144 (95% CI 4,016 to 10,273) excess deaths associated with extreme heat during the study period, depending on the definition of extreme heat used. There were statistically significant differences in this association among subgroups of age, gender, race, and ethnicity. Men and non-Hispanic Black individuals had a significantly greater relative and absolute increase, and elderly adults had a significantly greater absolute increase in cardiovascular mortality associated with extreme heat.
Although the burden of cardiovascular mortality across the US associated with extreme heat has not been well studied, studies limited to certain urban areas have noted the association between extreme heat and deaths from cardiovascular diseases.7, 13 Some studies have estimated the burden of all-cause deaths associated with extreme heat, however, due to differences in methodologies, comparison across studies is challenging. One study examining non-optimal heat and all-cause mortality estimated approximately 20,000 deaths per year related to heat in Canada and the US from 2008 to 2017.33 This analysis used data from 211 US cities from 1976 to 2006. As there is evidence that communities may have begun to adapt to extreme heat over time, such as with increased air conditioning use,34 using data from previous years may overestimate the number of heat-related deaths. Additionally, as this study examined deaths associated with non-optimal, rather than extreme, heat, comparison with our analysis is challenging. Another study examining all-cause mortality due to extreme heat across 297 US counties (accounting for 60% of the population) noted a lower estimate of approximately 2,300 deaths per year from 1997 to 2006.3 Regarding extreme heat and cardiovascular deaths, one study noted that from 2004 to 2018, there were 2,112 deaths where major cardiovascular disease was the primary cause of death and heat exposure was noted as a contributor on the death certificate.18 In our analysis, extreme heat was associated with 5,958 (95% CI 1,847 to 10,069) to 7,144 (95% CI 4,016 to 10,273) excess deaths from cardiovascular disease among adults from 2008 to 2017 across the contiguous US, depending on the definition of extreme heat used. When examining the association by tertiles of counties based on the total number of extreme heat days, there was a significantly greater increase in cardiovascular mortality among counties with the fewest number of extreme heat days compared to counties with the greatest number of extreme heat days. This suggests that areas where fewer extreme heat days typically occur may not be as well adapted to extreme heat and may be more vulnerable to its potential adverse effects.
There are several biological mechanisms by which extreme heat is associated with cardiovascular health, such as an increase in cardiac strain due to increases in heart rate and contractility and an upregulation of inflammatory mediators that can increase the risk of thrombosis.35 The use of medications such as beta-blockers and diuretics can also alter thermoregulation.8, 36, 37 When examining subgroups of cardiovascular disease, we noted a significant association between extreme heat and deaths due to ischemic heart disease, but not stroke. There is some evidence that extreme heat may be associated with greater number of strokes in certain populations.38 However, due to the smaller number of stroke deaths, there may not have been a sufficient number of deaths in many counties to detect variations in monthly mortality rates associated with extreme heat days. Additionally, it is possible that there may be an association between heat and non-fatal strokes, which were not examined in our analysis.
The association between extreme heat and cardiovascular mortality differed significantly between demographic subgroups. Notably, we found that there was a greater increase in cardiovascular mortality rates associated with extreme heat among non-Hispanic Black compared to non-Hispanic White adults. A study of cardiovascular deaths associated with extreme heat in Michigan found a greater risk among Black compared to White individuals.39 Non-Hispanic Black adults in the US may be more vulnerable, on an individual level, to the adverse health effects of extreme heat due a higher burden of cardiovascular risk factors and cardiovascular disease, as well as inequities in care access.40, 41 Additionally, aspects of the built environment may play an important role in this disparity. Black residents of New York City are more likely to live in buildings with higher levels of indoor heat and humidity.42 Compared to non-Hispanic Whites, minority populations are also more likely to live in areas with a greater degree of urban heat island effect (the phenomenon of built environments being hotter than surrounding rural areas).43 In our analysis, even when limited to metropolitan areas, there was a greater increase in cardiovascular deaths associated with extreme heat among non-Hispanic Black, compared to non-Hispanic White adults. Although our analysis cannot make inferences at the individual or sub-county level, it is possible that both greater vulnerability to cardiovascular disease at the individual level and the segregation of minority communities into neighborhoods that are particularly vulnerable to the adverse effects of extreme heat may contribute to the differences noted.
Similar differences in the association between other subgroups and non-Hispanic White adults were not noted. When examining metropolitan counties, non-Hispanic adults of other races did have a significant association between extreme heat and cardiovascular mortality. However, we did not detect a similar association for Hispanic adults. This may be due to the small number of cardiovascular deaths among Hispanic adults noted across most counties. Previous studies have also noted a “Hispanic paradox” i.e., despite having a higher burden of cardiovascular risk factors and lower socioeconomic status on average, Hispanic individuals have a lower burden of cardiovascular disease and higher life expectancy compared to non-Hispanic White individuals,44 which may in part explain the lack of association in this population. Another study examining extreme heat associated hospital admissions and mortality among patients with end-stage renal disease, also did not find a significant association for Hispanic individuals.6 Whether these findings are due to individual level differences or structural factors, requires further investigation.
Identifying disparities in outcomes related to extreme heat may allow for a more targeted approach in creating policies to mitigate the adverse health effects of climate change. Although, evidence for whether certain strategies can attenuate the adverse effects of extreme heat on human health and reduce disparities is limited, studies have noted a significant association between air conditioning use and heat related mortality, and racial disparities in access to air conditioning.45, 46 Other potential strategies include making cooling centers accessible to vulnerable populations and increasing tree cover in urban neighborhoods.15
The number of deaths due to cardiovascular conditions associated with extreme heat may continue to increase and the noted disparities between groups may widen as extreme heat events in the US are projected to increase. Most areas in the US are projected to experience 20–30 additional extremely hot days per year over the next 2–3 decades.1 However, due to the complex nature of climate change, and its impact on a vast number of environmental phenomena, predicting how mortality will change related to climate change is challenging. Along with the association between extreme heat and cardiovascular mortality, an association between extreme cold and cardiovascular events has also been seen.47 As the number of extreme cold days has declined over the past several decades,48 it is possible that the increase in cardiovascular events associated with more extreme heat days may be attenuated by fewer extreme cold days. However, some studies have suggested that climate change may be associated with a higher frequency of extreme cold events in certain parts of the US.49, 50 Therefore estimating how climate change may be associated with cardiovascular health in the coming decades in the US will require a more complete understanding of how extreme weather events, both hot and cold, will change in different parts of the country.
Limitations
This analysis has some limitations. Due to the observational nature of the study, causality cannot be assumed. As this is a county-level ecological study, individual-level inferences are not possible. Although the longitudinal fixed effects regression model accounts for differences between counties that are time invariant, residual time-varying confounding is still possible despite the inclusion of several important potential time-varying environmental, economic, demographic, and healthcare related covariates. As only monthly mortality data was available, it is not possible to directly attribute cardiovascular deaths in a particular month to the extreme heat days that occurred in that month, as a death may have occurred either prior to, or significantly after, the occurrence of an extreme heat day. Our analysis found that a greater number of extreme heat days in a month were associated with higher monthly cardiovascular mortality rates. Whether there are unmeasured environmental or socioeconomic factors that could lead to such an association between extreme heat days and mortality in a particular month is unclear. As monthly mortality rates are more stable than daily estimates, a small numbers of deaths occurring after an extreme heat event may not cause significant variation in the monthly rate, which may underestimate the association between extreme heat days and mortality. However, most localities in the US do not have daily mortality data available as rates from areas with small populations are particularly prone to statistical instability and there also may be privacy concerns. There is a possibility that the cause of death from death certificate data could be misclassified. To address this, we performed an alternative analysis using a narrower definition of cardiovascular disease which had similar results as the primary analysis. As the CDC Environmental Public Health Tracking Program tracks extreme heat days only in summer months (May to September) and was the source of the temperature data for this analysis, our analysis does not account for extreme heat days, and associated deaths, outside of these months. The definition of extreme heat was based on the baseline period of 1979 to 2007. Alternative definitions of extreme heat likely may result in different estimates of the association between extreme heat and cardiovascular mortality.
Conclusion
Extreme heat was associated with significantly higher adult cardiovascular mortality rates across all counties in the US from 2008 to 2017. However, there was significant heterogeneity based on age, gender, race, and ethnicity; elderly, male and non-Hispanic Black adults having a significantly greater increase in cardiovascular mortality associated with extreme heat. With extreme heat events projected to increase in frequency over the next several decades due to climate change, the adverse cardiovascular health effects of extreme heat on the US population may increase further without efforts to mitigate them.
Supplementary Material
Clinical Perspective.
What Is New?
The number of extreme heat days in a month were associated with a statistically significant relative and absolute increase in monthly cardiovascular mortality rates across the contiguous United States from 2008 to 2017.
The association varied significantly among subgroups, with a greater association noted among elderly, male, and non-Hispanic Black adults.
Between 2008 and 2017, extreme heat was associated with an estimated 5,958 (95% CI 1,847 to 10,069) to 7,144 (95% CI 4,016 to 10,273) excess cardiovascular deaths, depending on the definition of extreme heat used.
What Are the Clinical Implications?
As the climate continues to warm, and extreme heat days increase in frequency, the role that extreme heat plays in the cardiovascular health of US adults will continue to increase.
Extreme heat may also exacerbate pre-existing disparities in cardiovascular health notably between non-Hispanic Black and non-Hispanic White communities.
Identifying communities particularly vulnerable to the association between extreme heat and cardiovascular mortality may allow for more targeted interventions to mitigate the potential adverse effects of extreme heat.
Acknowledgements:
Funding/Support:
Dr. Khatana receives grant funding from the National Heart, Lung, and Blood Institute (5K23HL153772-02) and the American Heart Association (20CDA35320251).
Non-standard Abbreviations and Acronyms:
- US
United States
- CDC
Centers for Disease Control and Prevention
- ICD
International Statistical Classification of Diseases and Related Health Problems
- AQI
Air Quality Index
- EPA
Environmental Protection Agency
- SD
Standard Deviation
- CI
Confidence Interval
- IQR
Interquartile Range
Footnotes
Conflicts of interests:
None
Supplemental Material
Supplemental Methods: Supplemental Methods 1–4
Supplemental Tables: Supplemental Table S1–S8
References:
- 1.Vose R, Easterling D, Kunkel K, LeGrande A and Wehner M. Temperature changes in the United States. Climate Science Special Report: Fourth National Climate Assessment, Volume I US Global Change Research Program. Climate Science Special Report: Fourth National Climate Assessment, Volume I. 2017:185–206. [Google Scholar]
- 2.Bobb JF, Obermeyer Z, Wang Y and Dominici F. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA. 2014;312:2659–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinberger KR, Harris D, Spangler KR, Zanobetti A and Wellenius GA. Estimating the number of excess deaths attributable to heat in 297 United States counties. Environ Epidemiol. 2020;4:e096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bobb JF, Peng RD, Bell ML and Dominici F. Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect. 2014;122:811–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng J, Xu Z, Bambrick H, Prescott V, Wang N, Zhang Y, Su H, Tong S and Hu W. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ Res. 2019;177:108610. [DOI] [PubMed] [Google Scholar]
- 6.Remigio RV, Jiang C, Raimann J, Kotanko P, Usvyat L, Maddux FW, Kinney P and Sapkota A. Association of Extreme Heat Events With Hospital Admission or Mortality Among Patients With End-Stage Renal Disease. JAMA Netw Open. 2019;2:e198904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, Howe HL and Wilhelm JL. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335:84–90. [DOI] [PubMed] [Google Scholar]
- 8.Argaud L, Ferry T, Le QH, Marfisi A, Ciorba D, Achache P, Ducluzeau R and Robert D. Short- and long-term outcomes of heatstroke following the 2003 heat wave in Lyon, France. Arch Intern Med. 2007;167:2177–83. [DOI] [PubMed] [Google Scholar]
- 9.Moon J The effect of the heatwave on the morbidity and mortality of diabetes patients; a meta-analysis for the era of the climate crisis. Environ Res. 2021;195:110762. [DOI] [PubMed] [Google Scholar]
- 10.Semenza JC, McCullough JE, Flanders WD, McGeehin MA and Lumpkin JR. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999;16:269–77. [DOI] [PubMed] [Google Scholar]
- 11.Lin S, Luo M, Walker RJ, Liu X, Hwang SA and Chinery R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20:738–46. [DOI] [PubMed] [Google Scholar]
- 12.Fuhrmann CM, Sugg MM, Konrad CE 2nd and Waller A. Impact of Extreme Heat Events on Emergency Department Visits in North Carolina (2007–2011). J Community Health. 2016;41:146–56. [DOI] [PubMed] [Google Scholar]
- 13.Barnett AG, Hajat S, Gasparrini A and Rocklov J. Cold and heat waves in the United States. Environ Res. 2012;112:218–24. [DOI] [PubMed] [Google Scholar]
- 14.Chow WTL, Chuang W-C and Gober P. Vulnerability to Extreme Heat in Metropolitan Phoenix: Spatial, Temporal, and Demographic Dimensions. The Professional Geographer. 2012;64:286–302. [Google Scholar]
- 15.Sinha P, Coville RC, Hirabayashi S, Lim B, Endreny TA and Nowak DJ. Variation in estimates of heat-related mortality reduction due to tree cover in U.S. cities. J Environ Manage. 2022;301:113751. [DOI] [PubMed] [Google Scholar]
- 16.Rey G, Jougla E, Fouillet A, Pavillon G, Bessemoulin P, Frayssinet P, Clavel J and Hemon D. The impact of major heat waves on all-cause and cause-specific mortality in France from 1971 to 2003. Int Arch Occup Environ Health. 2007;80:615–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharpe JD and Wolkin AF. The Epidemiology and Geographic Patterns of Natural Disaster and Extreme Weather Mortality by Race and Ethnicity, United States, 1999–2018. Public Health Rep. 2021:333549211047235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vaidyanathan A, Malilay J, Schramm P and Saha S. Heat-Related Deaths - United States, 2004–2018. MMWR Morb Mortal Wkly Rep. 2020;69:729–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaidyanathan A, Kegler SR, Saha SS and Mulholland JA. A Statistical Framework to Evaluate Extreme Weather Definitions from A Health Perspective: A Demonstration Based on Extreme Heat Events. Bull Am Meteorol Soc. 2016;97:1817–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Indicator: Historical Temperature & Heat Index. 2021.
- 21.Arias E, Heron M, National Center for Health S, Hakes J and Bureau USC. The Validity of Race and Hispanic-origin Reporting on Death Certificates in the United States: An Update. Vital Health Stat 2. 2016:1–21. [PubMed] [Google Scholar]
- 22.Mollié A Bayesian mapping of disease. Markov chain Monte Carlo in practice. 1996;1:359–379. [Google Scholar]
- 23.Anselin L, Lozano N and Koschinsky J. Rate transformations and smoothing. Urbana. 2006;51:61801. [Google Scholar]
- 24.Gunasekara FI, Richardson K, Carter K and Blakely T. Fixed effects analysis of repeated measures data. Int J Epidemiol. 2014;43:264–9. [DOI] [PubMed] [Google Scholar]
- 25.Wooldridge JM. Distribution-free estimation of some nonlinear panel data models. Journal of Econometrics. 1999;90:77–97. [Google Scholar]
- 26.Allison PD and Waterman RP. Fixed–Effects Negative Binomial Regression Models. Sociological Methodology. 2002;32:247–265. [Google Scholar]
- 27.Mize TD, Doan L and Long JS. A general framework for comparing predictions and marginal effects across models. Sociological Methodology. 2019;49:152–189. [Google Scholar]
- 28.Lee BJ, Kim B and Lee K. Air pollution exposure and cardiovascular disease. Toxicol Res. 2014;30:71–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cosselman KE, Navas-Acien A and Kaufman JD. Environmental factors in cardiovascular disease. Nat Rev Cardiol. 2015;12:627–42. [DOI] [PubMed] [Google Scholar]
- 30.Technical Assistance Document for the Reporting of Daily Air Quality – the Air Quality Index (AQI). 2018.
- 31.National Ambient Air Quality Standards Table. 2022.
- 32.Correia S, Guimarães P and Zylkin T. Fast Poisson estimation with high-dimensional fixed effects. The Stata Journal. 2019;20:115–95. [Google Scholar]
- 33.Zhao Q, Guo Y, Ye T, Gasparrini A, Tong S, Overcenco A, Urban A, Schneider A, Entezari A, Vicedo-Cabrera AM, Zanobetti A, Analitis A, Zeka A, Tobias A, Nunes B, Alahmad B, Armstrong B, Forsberg B, Pan SC, Iniguez C, Ameling C, De la Cruz Valencia C, Astrom C, Houthuijs D, Dung DV, Roye D, Indermitte E, Lavigne E, Mayvaneh F, Acquaotta F, de’Donato F, Di Ruscio F, Sera F, Carrasco-Escobar G, Kan H, Orru H, Kim H, Holobaca IH, Kysely J, Madureira J, Schwartz J, Jaakkola JJK, Katsouyanni K, Hurtado Diaz M, Ragettli MS, Hashizume M, Pascal M, de Sousa Zanotti Stagliorio Coelho M, Valdes Ortega N, Ryti N, Scovronick N, Michelozzi P, Matus Correa P, Goodman P, Nascimento Saldiva PH, Abrutzky R, Osorio S, Rao S, Fratianni S, Dang TN, Colistro V, Huber V, Lee W, Seposo X, Honda Y, Guo YL, Bell ML and Li S. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet Health. 2021;5:e415–e425. [DOI] [PubMed] [Google Scholar]
- 34.Nordio F, Zanobetti A, Colicino E, Kloog I and Schwartz J. Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environ Int. 2015;81:80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chaseling GK, Iglesies-Grau J, Juneau M, Nigam A, Kaiser D and Gagnon D. Extreme Heat and Cardiovascular Health: What a Cardiovascular Health Professional Should Know. Can J Cardiol. 2021;37:1828–1836. [DOI] [PubMed] [Google Scholar]
- 36.Pescatello LS, Mack GW, Leach CN Jr. and Nadel ER. Effect of beta-adrenergic blockade on thermoregulation during exercise. J Appl Physiol (1985). 1987;62:1448–52. [DOI] [PubMed] [Google Scholar]
- 37.Balmain BN, Sabapathy S, Jay O, Adsett J, Stewart GM, Jayasinghe R and Morris NR. Heart Failure and Thermoregulatory Control: Can Patients With Heart Failure Handle the Heat? J Card Fail. 2017;23:621–627. [DOI] [PubMed] [Google Scholar]
- 38.Pan WH, Li LA and Tsai MJ. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet. 1995;345:353–5. [DOI] [PubMed] [Google Scholar]
- 39.Gronlund CJ, Berrocal VJ, White-Newsome JL, Conlon KC and O’Neill MS. Vulnerability to extreme heat by socio-demographic characteristics and area green space among the elderly in Michigan, 1990–2007. Environ Res. 2015;136:449–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Dyke M, Greer S, Odom E, Schieb L, Vaughan A, Kramer M and Casper M. Heart Disease Death Rates Among Blacks and Whites Aged >/=35 Years - United States, 1968–2015. MMWR Surveill Summ. 2018;67:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McWilliams JM, Meara E, Zaslavsky AM and Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009;150:505–15. [DOI] [PubMed] [Google Scholar]
- 42.Uejio CK, Tamerius JD, Vredenburg J, Asaeda G, Isaacs DA, Braun J, Quinn A and Freese JP. Summer indoor heat exposure and respiratory and cardiovascular distress calls in New York City, NY, U.S. Indoor Air. 2016;26:594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hsu A, Sheriff G, Chakraborty T and Manya D. Disproportionate exposure to urban heat island intensity across major US cities. Nat Commun. 2021;12:2721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Medina-Inojosa J, Jean N, Cortes-Bergoderi M and Lopez-Jimenez F. The Hispanic paradox in cardiovascular disease and total mortality. Prog Cardiovasc Dis. 2014;57:286–92. [DOI] [PubMed] [Google Scholar]
- 45.Sera F, Hashizume M, Honda Y, Lavigne E, Schwartz J, Zanobetti A, Tobias A, Iniguez C, Vicedo-Cabrera AM, Blangiardo M, Armstrong B and Gasparrini A. Air Conditioning and Heat-related Mortality: A Multi-country Longitudinal Study. Epidemiology. 2020;31:779–787. [DOI] [PubMed] [Google Scholar]
- 46.O’Neill MS, Zanobetti A and Schwartz J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J Urban Health. 2005;82:191–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guo Y, Li S, Zhang Y, Armstrong B, Jaakkola JJ, Tong S and Pan X. Extremely cold and hot temperatures increase the risk of ischaemic heart disease mortality: epidemiological evidence from China. Heart. 2013;99:195–203. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Y, Li Q, Ge Y, Du X and Wang H. Growing prevalence of heat over cold extremes with overall milder extremes and multiple successive events. Communications Earth & Environment. 2022;3:1–13. [Google Scholar]
- 49.Cohen J, Pfeiffer K and Francis JA. Warm Arctic episodes linked with increased frequency of extreme winter weather in the United States. Nat Commun. 2018;9:869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cohen J, Agel L, Barlow M, Garfinkel CI and White I. Linking Arctic variability and change with extreme winter weather in the United States. Science. 2021;373:1116–1121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


