Abstract
Background
Most of the detected increment in dental caries among children above the age of six years and adolescents is confined to occlusal surfaces of posterior permanent molars. Dental sealants and fluoride varnishes are much used to prevent caries. As the effectiveness of both interventions in controlling caries as compared with no intervention has been demonstrated previously, this review aimed to evaluate their relative effectiveness. It updates a review published originally in 2006 and updated in 2010 and in 2016.
Objectives
Our primary objective was to evaluate the relative effectiveness of dental sealants (i.e. fissure sealant) compared with fluoride varnishes, or fissure sealants plus fluoride varnishes compared with fluoride varnishes alone, for preventing dental caries in the occlusal surfaces of permanent teeth of children and adolescents.
Our secondary objectives were to evaluate whether effectiveness is influenced by sealant material type and length of follow‐up, document and report on data concerning adverse events associated with sealants and fluoride varnishes, and report the cost effectiveness of dental sealants versus fluoride varnish in caries prevention.
Search methods
Cochrane Oral Health's Information Specialist searched the following databases: Cochrane Oral Health's Trials Register (to 19 March 2020), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2020, Issue 2), MEDLINE Ovid (1946 to 19 March 2020) and Embase Ovid (1980 to 19 March 2020). We searched the US National Institutes of Health Trials Registry (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform for ongoing trials. There were no restrictions on the language or date of publication.
Selection criteria
We included randomised controlled trials with at least 12 months of follow‐up comparing fissure sealants, or fissure sealants plus fluoride varnishes, versus fluoride varnishes, for preventing caries in the occlusal surfaces of permanent posterior teeth (i.e. premolar or molar teeth), in participants younger than 20 years of age at the start of the study.
Data collection and analysis
At least two review authors independently screened search results, extracted data from included studies and assessed their risk of bias. We attempted to contact study authors to obtain missing or unclear information. We grouped and analysed studies on the basis of sealant material type: resin‐based sealant or glass ionomer‐based sealant (glass ionomer and resin‐modified glass ionomer sealant), and different follow‐up periods. We calculated the odds ratio (OR) for risk of caries on occlusal surfaces of permanent molar teeth. For trials with a split‐mouth design, we used the Becker‐Balagtas OR. One cluster‐randomised trial provided precise estimates in terms of risk ratio (RR), which we used. For continuous outcomes and data, we used means and standard deviations to obtain mean differences (MD). For meta‐analysis, we used the random‐effects model when we combined data from four or more studies. We presented all measures with 95% confidence intervals (CIs). We assessed the certainty of the evidence using GRADE criteria.
Main results
We included 11 trials with 3374 participants aged five to 10 years when trials started. Three trials are new since the 2016 update. Two trials did not contribute data to our analysis.
Sealant versus fluoride varnish
Resin‐based fissure sealants versus fluoride varnishes
Seven trials evaluated this comparison (five contributing data). We are uncertain if resin‐based sealants may be better than fluoride varnish, or vice versa, for preventing caries in first permanent molars at two to three years' follow‐up (OR 0.67, 95% CI 0.37 to 1.19; I2 = 84%; 4 studies, 1683 children evaluated). One study measuring decayed, missing and filled permanent surfaces (DMFS) and decayed, missing and filled permanent teeth (DMFT) increment at two years suggested a small benefit for fissure sealant (DMFS MD –0.09, 95% CI –0.15 to –0.03; DMFT MD –0.08, 95% CI –0.14 to –0.02; 542 participants), though this may not be clinically significant. One small study, at high risk of bias, reported a benefit for sealant after four years in preventing caries (RR 0.42, 95% CI 0.21 to 0.84; 75 children) and at nine years (RR 0.48, 95% CI 0.29 to 0.79; 75 children). We assessed each of these results as having very low certainty.
Glass ionomer‐based sealants versus fluoride varnishes
Three trials evaluated this comparison: one trial with chemically cured glass ionomer and two with resin‐modified glass ionomer. Studies were clinically diverse, so we did not conduct a meta‐analysis. In general, the studies found no benefit of one intervention over another at one, two and three years, although one study, which also included oral health education, suggested a benefit from sealants over varnish for children at high risk of caries. We assessed this evidence as very low certainty.
Sealant plus fluoride varnish versus fluoride varnish alone
One split‐mouth trial analysing 92 children at two‐year follow‐up found in favour of resin‐based fissure sealant plus fluoride varnish over fluoride varnish only (OR 0.30, 95% CI 0.17 to 0.55), which represented a clinically meaningful effect of a 77% reduction in caries after two years; however, we assessed this evidence as very low certainty.
Adverse events
Five trials (1801 participants) (four using resin‐based sealant material and one using resin‐modified glass ionomer) reported that no adverse events resulted from use of sealants or fluoride varnishes over one to nine years. The other studies did not mention adverse events.
Authors' conclusions
Applying fluoride varnish or resin‐based fissure sealants to first permanent molars helps prevent occlusal caries, but it has not been possible in this review to reach reliable conclusions about which one is better to apply. The available studies do not suggest either intervention is superior, but we assessed this evidence as having very low certainty. We found very low‐certainty evidence that placing resin‐based sealant as well as applying fluoride varnish works better than applying fluoride varnish alone. Fourteen studies are currently ongoing and their findings may allow us to draw firmer conclusions about whether sealants and varnish work equally well or whether one is better than the other.
Plain language summary
Sealants or fluoride varnishes: which treatment is better for preventing decay in the permanent back teeth of children and adolescents?
Why is this question important?
Tooth decay (also called a cavity or caries) is when a small hole develops in a tooth. This happens because bacteria (tiny living organisms) that live in the mouth feed on sugar in the food we eat. As they feed, the bacteria produce acid that attacks teeth. If teeth are not cleaned regularly after eating, or if someone consumes a lot of sugary foods and drinks, the repeated acid attacks can create holes in the hard outer surface of the teeth (enamel). If untreated, these holes can deepen and damage the layer of tooth underneath the surface (dentine).
Many people around the world develop tooth decay at some point in their life. In most adolescents and children over the age of six years, decay damages the biting surfaces of the permanent teeth at the back of the mouth.
To prevent decay, dentists can apply a dental sealant, or a fluoride varnish, directly onto the back teeth. A dental sealant is a coating made from an adhesive material such as resin or glass ionomer, which the dentists applies once to teeth. It seals off the grooves in teeth that tend to collect food, and protects them from the acid. By comparison, a fluoride varnish is a sticky paste that contains high levels of fluoride; fluoride is a mineral naturally present in teeth that protects them from damage. Fluoride varnishes need to be applied to teeth by the dentist two to four times a year.
We reviewed the evidence from research studies to find out whether sealants or fluoride varnishes, or a combination, are better for preventing decay in the permanent back teeth of children and adolescents.
How did we identify and evaluate the evidence?
We searched the medical literature for randomised controlled studies (clinical studies where people are randomly put into one of two or more treatment groups), because these studies provide the most robust evidence about the effects of a treatment. We then compared the results, and summarised the evidence from all the studies. We assessed how certain the evidence was. To do this, we considered factors such as the way studies were conducted, study sizes and consistency of findings across studies. Based on our assessments, we categorised the evidence as being of very low, low, moderate or high certainty.
What did we find?
We found 11 studies that included 3374 children aged between five and 10 years at the start of the studies. Children were randomly assigned to treatment with either sealant or fluoride varnish, or both. They were followed for between one and nine years. Studies compared the number of children who had tooth decay in the dentine of their back teeth in different treatment groups.
The evidence was of very low certainty so we are not able to be confident in the findings.
When we combined four studies that compared resin sealants versus fluoride varnish, we found that neither intervention worked better than the other.
The three individual studies that compared sealants made from glass ionomer versus fluoride varnish could not be combined and had mixed results.
One small study found that using both sealants and fluoride varnish may work better than using fluoride varnish alone.
Five studies reported that no side effects were associated with the use of either sealants or fluoride varnishes. The other studies did not mention whether or not any side effects occurred.
What do these results mean?
At present, we do not know whether it is better to apply sealants or fluoride varnish to prevent tooth decay in children's back teeth. We do know that both interventions are effective for reducing tooth decay, and current evidence does not suggest that one works better than the other.
Fourteen studies are currently underway. Their findings could improve the evidence in future versions of this review.
How‐up‐to date is this review?
The evidence is current to March 2020.
Summary of findings
Background
Description of the condition
Dental caries is a multi‐factorial chronic oral disease that affects most populations throughout the world and has been considered the most important global oral health burden (Petersen 2005). Since the 1970s, a reduction in caries prevalence has occurred in most industrialised countries; and has been attributed to improvements in living conditions and oral hygiene, and public health measures such as widespread use of fluoride tooth paste, fluoride products and better disease management (Splieth 2016). However, dental caries is still a problem for some individuals and populations, for example, in many Eastern European and South American countries, the prevalence of caries among 12‐year‐olds has been reported to be moderate or high (WHO 2014). Dental caries incidence is still considered very high despite the decline in the severity of dentine caries and the slower rate of caries progression into dentine amongst children below the age of 12 years (Frencken 2017).
Dental caries can be explained as an interplay between specific acidogenic bacteria in the plaque biofilm, fermentable carbohydrates and tooth structure. The biofilm bacteria produce organic acids that can cause loss of minerals from the tooth surface (demineralisation). In favourable conditions, a reversal, that is, a mineral gain, is possible (remineralisation). If the demineralisation process prevails, visually detectable caries lesions occur. Development of a caries lesion is a dynamic process that may progress, stop or reverse, and assessment of the grade and activity of the lesion is challenging. The International Caries Detection and Assessment System (ICDAS) integrates a definition of dental caries and a system to measure the caries process (ICDAS 2008). In ICDAS, the codes for coronal caries range from 0 to 6, depending on the severity of the lesion: codes from 0 to 3 involve a sound tooth surface to caries in enamel (with or without micro‐cavitation); codes 4 to 6 involve caries in dentine.
For permanent teeth, caries lesion development is most likely in the first few years after the tooth erupts (Carvalho 2014; Mejàre 2014). Most of the detected increment in dental caries among children above six years of age and adolescents is confined to the pit and fissure surfaces of first molars (Batchelor 2004; Brown 1995; McDonald 1992); their anatomy favours biofilm formation and retention and carious lesions often start before teeth fully erupt (Alves 2014; Zenkner 2013). However, the occlusal surfaces of second permanent molars are also vulnerable. The rate of occlusal caries among young people has not fallen as much as the rate of caries on smooth surfaces (Brown 1995).
The efficacy of any caries‐preventive intervention depends on the actual caries risk of an individual (and population), that is, if the risk of developing new lesions within a certain follow‐up period is small even without intervention, then any efficacy estimate of the additional preventive method will be small. Current methods for caries risk assessment comprise a range of strategies such as past caries experience, information about sociodemography, oral hygiene and dietary habits, oral bacteria and saliva characteristics (Mejàre 2014). However, the factors are not stable, for example, oral hygiene and dietary habits can change during follow‐up, decreasing or increasing caries risk.
The evidence on the validity of existing systems to predict future caries risk is limited (Tellez 2013). A review by Twetman 2016, summarising the findings of systematic reviews, concluded that there is no clearly superior method to predict future caries, whereas a systematic review by Mejàre 2014 found that baseline caries experience of the child was the most accurate single predictor for future caries development (moderate/good accuracy in preschool children and limited accuracy in school children/adolescents).
Oral disorders affect 3.5 billion people worldwide, with substantial burden on quality of life, as well as costs to the healthcare system, patients and society. In 2015 alone, the estimated direct costs of providing dental health care were USD 356.8 billion, corresponding to 4.6% of global health expenditure, with a further estimated USD 187.6 billion in indirect costs (Righolt 2018). Much of that expenditure is used to treat largely preventable disease among children and adolescents, with significant cost burden to healthcare payers (patients, governments, insurance). In 2015/2016 alone, tooth decay was the most common reason for hospitalisation among children aged five to nine years in England (Public Health England 2019). In 2018/2019 the national schedule of reference costs data for England, covering secondary care costs, indicated that over 70,000 episodes of care took place to deal with surgical extraction of teeth in people aged 18 years and under, at a total cost of GBP 65.7 million, at a mean cost per procedure of GBP 932, weighted for procedure complexity. A further GBP 4.3 million was spent on hospital‐provided restorations for children (NHS England). There are also substantial costs to primary dental care services. In Scotland, 2018/2019 data showed that there were 186,179 permanent fillings, 4002 endodontics treatments and 136,459 extractions (treatment codes 14, 15, 21) provided for children in primary dental care alone at a total cost of almost GBP 4 million (Public Health Scotland 2019). The cost burden further extends to families with respect to time off work, childcare, lost school days and to society in terms of lost productivity for time spent taking children to receive avoidable complex dental care.
Description of the intervention
Dental sealants
Dental sealants were introduced for preventing caries on occlusal surfaces, but are now considered active agents for controlling and managing initial caries lesions on occlusal surfaces (Splieth 2010), and on approximal surfaces (Dorri 2015; Ekstrand 2012; Splieth 2010). There are numerous occlusal sealant materials, but resins/composites and glass ionomers comprise the main material types.
Options of occlusal sealant materials are numerous but resins/composites and glass ionomers comprise the main material types. A resin material, bisphenol A glycidyl methacrylate (BIS‐GMA), forms the basis for numerous resin‐based dental sealants and composites that are now available. The effectiveness of resin‐based sealants is closely related to the longevity of sealant coverage (i.e. clinical retention) (Ripa 1993). The development of sealants has progressed from first‐generation sealants, which were activated with ultraviolet light, through to second‐ and third‐generation sealants, which are autopolymerised and visible‐light activated, and fourth‐generation sealants, which contain fluoride. First‐generation sealants are no longer marketed. Reports have considered possible adverse oestrogen‐like effects of resin‐based materials including bisphenol A (BPA) (e.g. Azarpazhooh 2008a; Fleisch 2010; Joskow 2006). This synthetic chemical resin is widely used in the production of plastic products intended for everyday use, but its use in dental materials is quite rare (ADA 2003). Although some dental resins can include low‐levels of BPA (e.g. trace material from resin production) (ADA 2016), evidence suggests that use of these resin‐based sealants does not place people at risk of harmful effects (ADA 2016; Azarpazhooh 2008a; Fleisch 2010).
The other main type of sealant is made from glass ionomer cements (combination of silicate and polyacrylate cement system). There is a wide range of glass ionomer materials available. Glass ionomer cements may be used as the original chemically cured type or as the light‐cured type, which is modified with resin, for example, for rapid initiation of the curing process (resin‐modified glass ionomers).
Novel materials called compomers, which were introduced in the 1990s to combine benefits of resins and those of glass ionomer cements, have also been applied as sealants (Nicholson 2007; Ruse 1999).
Allergic reactions to sealant materials are possible but rare (Hallstrom 1993).
Fluoride varnishes
The aim of topical fluoride varnish application is to treat hard tooth surfaces in such a way that caries is arrested or reversed. Although fluoride varnishes have a very high fluoride concentration (e.g. 22,660 ppm in Duraphat fluoride varnish), their use is considered safe because they have a quick‐setting base, release fluoride slowly over time and require comparatively small amounts of varnish for the whole dentition (Petersson 1993). Only a small dose of fluoride is swallowed over several hours, and risk of acute toxic reactions (e.g. nausea, vomiting) is minimal (Bawden 1998; Seppä 1999). Contact allergies to fluoride varnish due to colophony are possible but have been reported in only two cases (Chu 2006; Isaksson 1993).
Sometimes topical fluoride has been combined with sealant application to strengthen overall effectiveness in the prevention of dental caries.
How the intervention might work
Fluoride acts to prevent caries in three ways: 1. by inhibiting the demineralisation, 2. promoting the remineralisation of dental enamel and 3. by inhibiting acid formation by plaque bacteria (Shellis 1994; Ten Cate 1997). It can be applied in various ways; a varnish has the advantage of relative longevity. Dental sealant is applied to a tooth surface to provide a physical barrier that prevents growth of biofilm by blocking nutrition. Resin‐based and composite materials are used most commonly, with glass ionomer cements having the added element of containing fluoride that is released over a prolonged period.
The cost of preventive care is small in comparison to the extensive cost to primary, but especially secondary, care services of complex restorative and surgical dental treatment. Therefore, if preventive measures, such as fissure sealants or fluoride varnish, can demonstrate effectiveness in terms of reduced tooth decay, and can avert long‐term need for restorations and extractions, there is great potential for cost savings to payers (insurance, patients and the health system) and cost‐effectiveness.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 and this review was identified as a priority title by the paediatric dentistry expert panel (see oralhealth.cochrane.org/priority-reviews) (Worthington 2015). Several systematic reviews have shown the substantial effectiveness of resin‐based sealants and fluoride varnishes in preventing or controlling occlusal decay as compared with no intervention (sealants: Ahovuo‐Saloranta 2017; Griffin 2008; Llodra 1993; Mejàre 2003; varnish: Azarpazhooh 2008b; Helfenstein 1994; Marinho 2013; Petersson 2004), but the relative effectiveness remains unclear. Application of sealants is more technique sensitive than application of fluoride varnish; however, sealants usually are applied only once and should be reapplied if failed and maintained based on caries risk, whereas fluoride varnish is applied several times, depending on the caries activity of an individual.
Statement on cost‐effectiveness of these preventive measures
To make evidence‐based decisions about the effective and efficient allocation of scarce funding resources, policy makers require information about the potential cost‐effectiveness of different preventive interventions to determine if the additional money spent on prevention is an effective and efficient use of scarce funding resources in the longer term. It is also necessary to determine which preventive measures are the most cost‐effective (can achieve greatest benefit for least cost) to ensure dental funding is allocated in the most efficient way possible. This review includes a brief economic commentary (BEC) to add an economic lens to the interpretation of the results.
The aim of this systematic review is to compare the relative effectiveness of fissure sealants and fluoride varnishes alone, or fissure sealants combined with fluoride varnishes and fluoride varnishes alone, for preventing dental caries in children and adolescents.
Objectives
Primary objective
To evaluate the relative effectiveness of dental sealants (i.e. fissure sealant) compared with fluoride varnishes, or fissure sealants plus fluoride varnishes compared with fluoride varnishes alone, for preventing dental caries in the occlusal surfaces of permanent teeth of children and adolescents.
Secondary objectives
To evaluate whether effectiveness is influenced by sealant material type and length of follow‐up.
To document and report on data concerning adverse events associated with sealants and fluoride varnishes.
To report the cost effectiveness of dental sealants versus fluoride varnish in caries prevention.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with at least of 12 months' follow‐up, in which fissure sealants, or fissure sealants plus fluoride varnishes, were compared with fluoride varnishes alone for preventing caries in occlusal surfaces of permanent teeth of children and adolescents. We included both parallel‐group and split‐mouth study designs. The unit of randomisation could be the individual, the group (e.g. school, school class), or the tooth or tooth pair.
Types of participants
Children and adolescents from the general population, younger than 20 years of age at the start of the study.
Types of interventions
Pit and fissure sealants of all materials (except first‐generation resin‐based sealants) versus fluoride varnish.
Pit and fissure sealants plus fluoride varnish versus fluoride varnish.
Intervention group was either the sealant group or the sealant plus fluoride varnish group. The control group was the fluoride varnish group.
We included studies in which applications were placed on occlusal surfaces of permanent posterior teeth for the purpose of preventing caries, regardless of who did the application. Materials could be applied on sound surfaces or on enamel lesions (if scored using the ICDAS II scale, codes 0, 1, 2 and 3 were accepted). The sealant application method used in the study could consist of direct application to the tooth surface or application after mechanical preparation of the enamel surface.
Types of outcome measures
Primary outcomes
Occurrence of new dentinal carious lesions on treated occlusal surfaces of molars or premolars observed within 12 months from the initial treatment: assessed by visual‐tactile clinical assessment as a dichotomous measure using the participant as the unit of analysis in parallel studies and the tooth pair within an individual to be the unit of measurement (yes or no) in split‐mouth studies.
Changes from baseline in decayed, missing and filled (DMF) figures at surface, tooth and whole‐mouth levels.
Progression of dentinal carious lesions into dentine on treated occlusal surfaces of molars or premolars, observed within 12 months from the initial treatment: assessed by visual‐tactile clinical assessment as a dichotomous measure using a tooth/individual/pair of teeth as the unit of measurement.
Secondary outcomes
Time taken to apply pit and fissure sealant or fluoride varnish (minutes).
Number of visits to the dentist for repair of sealant or fluoride varnish application.
Safety of using sealants and fluoride varnishes assessed by presence or absence of adverse events.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials (CCTs). There were no language, publication year or publication status restrictions:
Cochrane Oral Health's Trials Register (searched 19 March 2020) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 2) in the Cochrane Library (searched 19 March 2020) (Appendix 2);
MEDLINE Ovid (1946 to 19 March 2020) (Appendix 3);
Embase Ovid (1980 to 19 March 2020) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying RCTs and CCTs as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
We searched the following trial registries for ongoing studies (see Appendix 5):
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 19 March 2020);
World Health Organization (WHO) International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 19 March 2020).
We searched the reference lists of included studies and relevant systematic reviews for further studies.
We checked that none of the included studies in this review were retracted due to error or fraud.
We did not perform a separate search for adverse effects of interventions used; we considered adverse effects described in included studies only.
On 19 March 2020, Cochrane Oral Health's information specialist undertook an additional search for cost‐effectiveness studies. MEDLINE Ovid and Embase Ovid were searched using the search strategies presented in Appendix 6.
For previous versions of this review, we also searched SCISEARCH, CAplus, INSPEC, JICST‐EPLUS, NTIS, PASCAL, DARE, HTA and OpenSIGLE (see Appendix 7). However, we decided not to update these searches at this time because in previous versions of the review, these searches yielded no additional information.
Data collection and analysis
Selection of studies
The 2020 update search results were imported into Covidence. Two review authors (WK, PG) independently selected papers on the basis of title, keywords and abstract, and decided on eligibility. The search was designed to be sensitive and include controlled clinical trials; these were filtered out early in the selection process if they were not randomised. We obtained the full text of every study considered for inclusion. If information relevant to the inclusion criteria was not available in the abstract, or if the title was relevant but the abstract was not available, we obtained the full text of the report. Two review authors (WK, PG) independently gathered information and recorded data, and resolved disagreements by discussion with a third review author (HW).
We contacted trial authors to request additional information if the study seemed to fulfil the inclusion criteria for this review but information in the report was insufficient to allow final assessment of inclusion or exclusion. We sought translation for one Dutch trial (Vermaire 2015)), which we later excluded, and one Chinese study (Tang 2014), which is included in this review.
We decided to consider only studies with a full‐text report. We excluded studies reported only as abstracts because methodological research has suggested discrepancies between data reported in an abstract and those provided in the final published full report, and because information on trial quality indicators is often lacking (Chokkalingam 1998; Hopewell 2006). Thus, we decided that the full‐text report was required to ensure reliable data extraction and assessment of risk of bias. To diminish the risk of publication bias, we contacted authors of relevant abstracts to ask whether a full‐text report of the study (unpublished or published) was available.
Data extraction and management
Two review authors (WK, PG) independently extracted relevant data from included studies. The two review authors were in full agreement about data, and discussion with a third review author was not needed. We attempted to contact study authors to request missing information or clarification when necessary.
We extracted the following information on study methods.
Trial design.
Study duration (years of follow‐up).
Year the study began.
We extracted the following characteristics of participants.
Location where study was conducted (country and setting where participants were recruited).
Criteria for accepting participants into the study (intact surfaces and surfaces with enamel lesion allowed).
Age (range and mean age at start) and sex.
Baseline caries prevalence of participants (caries severity at start (mean number of decayed, missing and filled deciduous teeth (dmft); decayed, missing and filled deciduous surfaces (dmfs); decayed, missing and filled permanent surfaces (DMFS); decayed, filled permanent surfaces (DFS); or other measure)).
Number of randomly assigned participants and number of teeth in treatment at study start and follow‐up.
Number of evaluated participants.
We extracted the following characteristics of interventions.
Intervention comparisons (sealant versus fluoride varnish, or sealant plus fluoride varnish versus fluoride varnish).
Sealant and fluoride varnish products used in the study.
Reapplication of sealants and frequency of fluoride varnish application.
Information on who applied sealants and fluoride varnishes (dentist with or without assistant or dental hygienist).
Co‐interventions (e.g. background exposure to other fluoride sources (toothpaste, water, etc.)).
We extracted the following characteristics of outcomes.
Description of outcomes.
Description of outcome measurements.
We extracted the following additional information.
Information related to calibration of examiners and kappa statistics.
Sealant retention figures at follow‐up.
Funding source.
Caries prevalence of population in study area.
Outcome information was extracted for the number of dentinal carious lesions or non‐carious lesions on occlusal surfaces of treatment and control teeth at different follow‐up times. If a filling had been put on the occlusal surface or the tooth had been extracted as the result of caries during the study, we coded it as caries. If the data were not presented in tables, we extracted data presented in graphs and figures when needed.
We presented data from the included studies in Table 4. For the split‐mouth studies, we extracted the 2×2 cross tabulation for the paired data, or the incorrectly reported simple prevalence by independent group, prior to calculation of the treatment effects. For the cluster trial, we obtained the cluster corrected effect estimates and standard errors from the authors.
1. Caries data from studies with binary outcome.
| Resin FS vs FV: at 2–3 years | ||||||
| Split‐mouth studies | Both sound |
FS sound FV carious |
FS carious FV sound |
Both carious | Proportion of decayed FV tooth surfaces to total FV surfaces | Becker‐Balagtas marginal OR (95% CI) |
|
Raadal 1984 (sealant better) |
131 | 31 | 15 | 31 | 0.30 | 0.67 (0.48 to 0.93) P = 0.02 ICC 0.44 |
| Parallel‐group studies | Description of data | OR (95% CI) | ||||
|
Bravo 2005 (sealant better) |
Calculated OR from data presented in Bravo 1996 (25/238 occlusal surfaces carious in sealant group; 71/252 surfaces carious in fluoride varnish group) | 0.30 (0.18 to 0.49) | ||||
|
Liu 2012 (no difference) |
OR based on model of multi‐level GEE logistic regression Additional information obtained from study author 124 children in sealant group, 116 in varnish group |
0.87 (0.34 to 2.20) |
||||
| Chestnutt 2017 (no difference) | The results presented as the proportion of children who developed dentine caries (D4-6MFT) on ≥ 1 FPM at 36 months (19.6% in FS arm and 17.5% in FV arm). Sex and baseline caries prevalence were used to balance the randomisation. An adjusted model was also performed and taken as the primary analysis. 418 children in sealant group, 417 in varnish group |
1.15 (0.81 to 1.63) |
||||
| Pooled | OR 0.67 (0.37 to 1.19) |
|||||
| Resin FS vs FV: 4 years | ||||||
| Parallel‐group studies | Description of data | RR (95% CI) | ||||
|
Bravo 2005 (sealant better) |
Results presented as RRs with cluster‐corrected standard error. A school class is a cluster, but several sealed and fluoride‐varnished teeth were present per child. Study authors calculated cluster‐corrected effect estimates when requested. | 0.42 (0.21 to 0.84) P = 0.01 |
||||
| Resin FS vs FV: 9 years | ||||||
| Parallel‐group studies | Description of data | |||||
|
Bravo 2005 (sealant better) |
Results presented as RRs with cluster‐corrected standard error. A school class is a cluster, but several sealed and fluoride‐varnished teeth were present per child. Study authors calculated cluster‐corrected effect estimates when requested. 26.6% of FS teeth and 55.8% of FV teeth had developed caries after 9 years (76.7% of control teeth without treatments) |
0.48 (0.29 to 0.79) P = 0.004 |
||||
| Resin‐modified glass ionomer FS vs FV: 1 year | ||||||
| Parallel‐group studies | Description of data | OR (95% CI) | ||||
|
Florio 2001 (no difference) |
Clustered data (several teeth per child). Data decided to analyse at a child level (i.e. data were dichotomised – did a child have caries or not) because decayed teeth were very few. Additional information obtained from study author indicated that the 2 decayed surfaces in the FV group were present in different children. 31 children in sealant group, 11 in varnish group Detailed data (Analysis 2.1) |
0.18 (0.01 to 4.27) P = 0.29 |
||||
| Resin FS + FV vs FV: 2 years | ||||||
| Split‐mouth studies | Both sound |
FS + FV sound FV carious |
FS + FV carious FV sound |
Both carious | Proportion of decayed control tooth surfaces to total control surfaces | Becker‐Balagtas marginal OR (95% CI) |
|
Splieth 2001 (FS + FV better than FV alone) |
129 | 32 | 7 | 7 | 0.22 | 0.30 (0.17 to 0.55) P < 0.0001 |
CI: confidence interval; FPM: first permanent molar; FS: fissure sealant; FV: fluoride varnish; GEE: generalised estimating equation; ICC: intracluster correlation coefficient; OR: odds ratio.
In addition, we recorded caries increments as changes in decayed, missing and filled permanent surfaces (DMFS)/decayed, missing and filled permanent teeth (DMFT) scores and as progression of caries lesions in enamel or dentine when study authors reported them. We recorded the following secondary outcomes when reported: time taken to apply pit and fissure sealant or fluoride varnish and number of visits to the dentist for repair or reapplication of sealant or fluoride varnish application. We recorded any adverse events reported, such as signs of allergic reaction (tingling, swelling, skin rash) or any other symptoms if it occurred within the first 24 hours of application of the intervention, or any longer‐term adverse events.
In some studies, results were provided at more than one period of follow‐up. We extracted data at one, two, three, four, five years, etc. (annually), and based our analyses on available data at these preselected times.
Assessment of risk of bias in included studies
Two review authors (WK, PG) independently assessed the risk of bias of included studies using the Cochrane tool (Higgins 2011a). We resolved disagreements by consensus. We contacted the authors of included studies to request additional information when required. We assessed seven methodological domains: random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other sources of bias (e.g. baseline comparability). For each study, we judged each domain as having 'low', 'high' or 'unclear' risk of bias, with the latter indicating lack of information or uncertainty over the potential for bias. See Table 5 for the detailed criteria we used in our assessment. We considered the blinding of outcome assessment to be at high risk of bias in all studies as the presence or absence of the sealant would reveal the intervention.
2. Criteria for 'Risk of bias' assessment.
| Random sequence generation (selection bias) | Was the method used to generate the allocation sequence appropriate to produce comparable groups? | We graded this domain to 'low' risk of bias if study authors described a random component in the sequence generation process (e.g. random number table, coin tossing, drawing of lots). If information about the random sequence generation process was not provided or was insufficient, we graded this domain to 'unclear' risk. |
| Allocation concealment (selection bias) | Was the method used to conceal the allocation sequence appropriate to prevent the allocation from being known in advance of, or during, enrolment? | We graded this domain to 'low' risk of bias if study authors described adequate concealment (e.g. by means of central randomisation, or sequentially numbered, opaque and sealed envelopes) and to 'high' risk of bias if inadequate concealment was documented (e.g. alternation, use of case record numbers, date of birth or day of the week) or if allocation concealment was not used. If insufficient or no information on allocation concealment was provided, the judgement was graded 'unclear' risk. |
| Blinding (performance bias) | Performance bias is looked at differently for the parallel‐group and split‐mouth studies. | Due to characteristics of each intervention, both participants and personnel are aware which of the 2 active preventive treatments has been applied. For parallel‐group studies, it was not possible to ensure that both groups followed a similar oral hygiene routine. The risk of bias was high. However, for the split‐mouth studies it is unlikely that the children undertook different oral hygiene practices in different areas of the mouth so performance bias was assumed to be of low risk. |
| Blinding of outcome assessment (detection bias) | Were outcome assessors blinded to the intervention a participant had received? | As sealant materials are visible, blinding of the outcome assessor is possible only if a sealant has been lost. Thus, outcome measurement is related to sealant retention and blinding of outcome assessor is usually impossible. However, it is difficult to assess how likely (or unlikely) it is that the outcome measurement is influenced by lack of blinding of outcome assessors in preventive sealant studies. Although the outcome assessors could not be blinded, the potential for bias could not be ignored. We decided to grade this domain as having 'low' risk of bias if study authors stated that the outcome assessor was not involved in the study design, and as having 'unclear' risk of bias if the study simply reported blinded outcome assessment or if blinding was indicated (e.g. examinations performed independently of previous records, outcome assessors not involved in applying treatments). If a trial reported nothing about blinding of outcome measurement, our judgement was 'high' risk of bias in this domain. |
| Incomplete outcome data (attrition bias) | How complete were the outcome data for primary caries outcomes? Were dropout rates and reasons for withdrawals reported? Were missing data imputed appropriately? | In caries prevention studies, follow‐up times can last several years. Studies with long follow‐up have the problem of high dropout rates causing uncertainty about data. We decided to base the judgement of this domain on caries efficacy outcome at 24 or 36 months (commonly used follow‐up times in sealant studies). When both follow‐up times were reported, we based our judgement on 24 months. If either of these 2 follow‐up times was not reported, we based our judgement on the first caries efficacy outcome reported in the study (which in this review should be ≥ 1 year). The risk of bias was assessed separately and was reported in the 'Risk of bias' table for caries outcomes for all reported follow‐up times. These assessments were taken into account in the overall risk of bias assessment for caries outcomes within a study. We decided to grade this domain as having 'low' risk of bias if the total proportion of missing outcome data was marginal (< 5%); or if the proportion of missing outcome data was < 25% regardless of the follow‐up time and groups (in parallel‐group studies) were balanced in numbers for missing data; or if missing data had been imputed using appropriate methods. If no information on reasons for dropout across intervention groups was provided, or if the proportion of missing data was documented as total proportion (5–25%), not by group in parallel‐group studies, our judgement was 'unclear' risk. Classifying missing data > 25% as having 'high' risk of bias in all study designs was a pragmatic approach to this domain to make the judgement uniform and transparent. If several teeth were sealed in a child's mouth (a child is a cluster), missing outcome data had to be stated (or counted) at child level (not at tooth level). |
| Selective reporting (reporting bias) | Were appropriate outcomes reported and were key outcomes missing? | To be included in this review, caries outcomes had to be reported. However, studies could report the outcome in different ways, e.g. incidence of dentinal carious lesion on treated occlusal surfaces of molars or premolars (yes or no); changes in mean figures of decayed, missing and filled surfaces (DMFS); or progression of caries lesion into enamel or dentine. In this review, selective outcome reporting was graded as 'low' risk of bias if the study's prespecified caries outcomes had been reported in the prespecified way. |
| Other sources of bias | This domain included information on comparability of intervention and control groups, and possible use of co‐interventions by group |
Comparability of groups
We decided to base our judgement of comparability of groups on baseline information given to groups available at follow‐up times because if only information provided at the start of the study is available, it is impossible to assess whether groups are balanced with each other after follow‐up time as well. The comparability of groups after follow‐up is especially problematic when small studies include children with several teeth and the dropout rate is high, even if dropouts are balanced in numbers and reasons between groups. If no information on the groups was available at follow‐up time, we decided that if the dropout rate (regardless of follow‐up time) was < 25% and dropouts were balanced in numbers and reasons by group, our judgement would be based on information given for groups at the start of the study. We decided to grade this domain as having 'low' risk of bias if groups were balanced in demographic characteristics (such as sex, age and social class) and in baseline caries risk level, or if possible imbalance of groups at baseline or after follow‐up (or both) had been taken adequately into account in the analyses. If baseline characteristics in parallel‐group studies were not given to groups available at follow‐up and the dropout rate was > 25%, we graded the study as having 'unclear' risk. Co‐interventions We decided to grade this domain as having 'low' risk of bias if groups were balanced in number and quality of co‐interventions, or if no co‐interventions were included in the protocol, and as having 'high' risk of bias if groups received different numbers or quality of co‐interventions during the trial. If no information was provided on co‐interventions, our judgement was 'unclear' risk. |
Summary assessments of 'Risk of bias'
To draw conclusions about the overall risk of bias for caries outcomes within a study, we classified the studies into three categories: studies with low, unclear or high risk of bias. We determined caries outcomes from data of the included studies (all caries data were extracted at preselected times – annually, at one, two, three, four, five years, etc.).
Our classification was based on the seven domains that we deemed most fundamental in assessing risk of study bias: random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other sources of bias .
We assessed performance bias as at high risk of bias for the parallel‐group studies, but not for the split‐mouth studies. In relation to blinding of outcome assessment, we considered this to be at high risk of bias in all of the included studies as we strongly believe that blinding cannot be achieved with these interventions because the examiner will see the sealant on the occlusal surfaces of the included teeth unless it has been lost.
We defined overall risk of bias categories as follows; however, all studies will be deemed as at high risk of bias due to the unavoidable presence of detection bias.
Low risk of bias (plausible bias unlikely to seriously alter results) if all domains defined above were graded as low risk of bias.
Unclear risk of bias (plausible bias that raises some doubt about results) if all of the domains were graded as low or unclear risk of bias.
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more domains were graded as high risk of bias.
Measures of treatment effect
We calculated odds ratios (ORs) for differences in sealant and fluoride varnish groups as to whether occlusal surfaces were carious, along with appropriate standard errors and 95% confidence intervals (CIs), using Review Manager 2014. For split‐mouth studies, we calculated ORs using the Becker‐Balagtas method (BB OR) outlined in Curtin 2002. We chose the Becker‐Balagtas method because we intended to pool data from split‐mouth studies and parallel‐group studies in the same meta‐analyses, and the Becker‐Balagtas method facilitates this data synthesis (as outlined by Stedman 2011). The split‐mouth studies included in the review presented paired data by tooth pairs, and the intracluster correlation coefficient (ICC) (needed for BB OR calculations) could be calculated from paired data. If we had included split‐mouth studies presenting data only in marginals (as parallel‐group studies, not as cross‐classification), we would have chosen the conservative ICC of 0.5, and in parallel‐group studies, an ICC of 0. The authors of a cluster‐randomised study provided risk ratio (RR) values that took the clustering into account, and as this was the best estimate, we used these values for the four‐year and nine‐year data for this study (Bravo 2005).
For continuous outcomes and data, we used means and standard deviations (SD) to obtain mean differences (MDs) and 95% CIs.
Unit of analysis issues
In parallel‐group studies and cluster‐randomised studies, we chose the individual to be the unit of analysis.
In split‐mouth studies, we chose the tooth pair within an individual to be the unit of analysis. In some studies, more than one pair of tooth surfaces per child might be treated. These pairs are not independent and should be analysed as 'paired data' on a per‐child basis. However, we were unable to do this from the data presented in these studies. This means that CIs are slightly narrower than they should be, and this was taken into consideration when we interpreted the results.
Dealing with missing data
We contacted trial authors to retrieve missing data when necessary or feasible. We performed analyses using an available‐case data analysis approach, as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Higgins 2011b). This approach for calculating response rates uses as a denominator the total number of participants for whom data were recorded for the outcome in question.
In caries‐prevention studies, follow‐up times can be several years. Studies with long follow‐up have the problem of high dropout rates, causing uncertainty in the data. The identified reasons for dropout in the included studies were that children moved away from the study area, moving from the town/city or school change. In Chestnutt 2017, one dropout was because parents decided to not continue in the trial without giving any reason. We decided to include, in the analyses, data from all studies (regardless of dropout rates). We assessed studies with a high dropout rate (i.e. greater than 25% regardless of follow‐up time) to be at high risk of bias. We had intended to evaluate in the sensitivity analyses the effect of risk of bias judgement on study results.
Assessment of heterogeneity
If a sufficient number of studies had been included in any meta‐analyses, we would have assessed clinical heterogeneity by examining the characteristics of studies and the similarity between types of participants (especially baseline caries prevalence levels), interventions and outcomes as specified in the criteria for included studies.
We assessed the significance of discrepancies in estimates of treatment effects from various studies using Cochrane's test for heterogeneity and the I2 statistic. The I2 statistic describes the percentage of variability in effect estimates that is due to heterogeneity rather than to sampling error. A value greater than 50% may represent substantial heterogeneity (Higgins 2003).
Assessment of reporting biases
If sufficient numbers of trials had been included in any meta‐analysis, we would have assessed the risk of publication bias according to the recommendations on testing for funnel plot asymmetry provided in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Sterne 2011). If asymmetry had been identified, we would have examined possible causes.
Data synthesis
We grouped and analysed studies on the basis of sealant material type (resin‐based sealant and glass ionomer‐based sealant: glass ionomer and resin‐modified glass ionomer) and follow‐up period (short term (up to 12 months); medium term (from 12 months to three years); long term (more than four years). We conducted meta‐analyses in Review Manager 2014, using the generic inverse variance method. In meta‐analyses that included two or three studies, we planned to use the fixed‐effect model, and in meta‐analyses with four or more studies, we planned to use the random‐effects model. We planned to pool data from studies in each comparison regardless of the risk of bias classification of these studies.
When feasible, we pooled in the same meta‐analysis ORs from parallel‐group studies and from split‐mouth studies by using BB ORs in split‐mouth studies, as outlined in the article by Stedman 2011.
Subgroup analysis and investigation of heterogeneity
If a sufficient number of studies had been included in any meta‐analyses, we would have examined the relative effectiveness of sealants and fluoride varnishes at different caries prevalence levels. As data were insufficient, it was not possible to create subgroups for further analyses.
Sensitivity analysis
If a sufficient number of studies had been included in any meta‐analyses, we would have undertaken sensitivity analyses to assess the robustness of results (for caries outcomes) by excluding studies with unclear or high risk of overall bias.
Summary of findings and assessment of the certainty of the evidence
We generated 'Summary of findings' tables, in which we planned to present data related to the occurrence of new dentine carious lesions on occlusal surfaces of permanent molars and data related to any adverse event. No adverse event was reported as a result of applying FV, FS or both of them together. We followed GRADE methods (GRADE 2004) and used GRADEpro GDT software to provide overall grading of the certainty of evidence for caries outcomes for the following comparisons: resin‐based sealant versus fluoride varnish (Table 1); glass ionomer or resin‐modified glass ionomer sealant versus fluoride varnish (Table 2); and resin‐based sealant plus fluoride varnish versus fluoride varnish alone (Table 3). We assessed the certainty of the body of evidence with reference to overall risk of bias of included studies at each outcome, directness of evidence, consistency of results, precision of estimates and risk of publication bias.
Summary of findings 1. Resin‐based fissure sealant compared with fluoride varnish for preventing dental caries.
| Resin‐based fissure sealant compared with fluoride varnish for preventing dental caries | ||||||
|
Population: children and adolescents Setting: preventive dentistry Intervention: resin‐based fissure sealant applications on occlusal tooth surfaces of permanent first molars Comparison: fluoride varnish applications on occlusal tooth surfaces of permanent first molars | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Fluoride varnish | Resin‐based fissure sealant | |||||
|
Dentine caries in permanent molars (yes/no) Follow‐up: 2–3 years |
228 per 1000 | 63 fewer per 1000 (from 32 more to 129 fewer) |
OR 0.67 (95% CI 0.37 to 1.19) |
1683 (4 studies) |
⊕⊝⊝⊝ Very lowa,b,c |
Data from 1 other study measuring DMFS and DMFT suggested a very small benefit for fissure sealants at 2‐year follow‐up. 4‐ and 9‐year data came from 1 study at high risk of bias and suggested a benefit for fissure sealants. |
| Adverse effects | None reported | |||||
| *The basis for the assumed risk was the median risk in the fluoride varnish group. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; DMFS: decayed, missing and filled permanent surfaces; DMFT: decayed, missing and filled permanent teeth; OR: odds ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level as studies at high risk of detection bias. bDowngraded one level due to severe heterogeneity (I2 = 84%). cDowngraded one level for imprecision.
Summary of findings 2. Glass ionomer fissure sealant or resin‐modified glass ionomer fissure sealant compared with fluoride varnish for preventing dental caries.
| Glass ionomer fissure sealant or resin‐modified glass ionomer fissure sealant compared with fluoride varnish for preventing dental caries | ||||
|
Population: children and adolescents Setting: preventive dentistry Intervention: glass ionomer or resin‐modified glass ionomer sealant applications on occlusal tooth surfaces of permanent first molars Comparison: fluoride varnish applications on occlusal tooth surfaces of permanent first molars | ||||
| Outcomes | Results | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments |
| Dentine caries in permanent molars Follow‐up: 1, 2 and 3 years | No evidence of a difference between interventions in caries after 1, 2 and 3 years | 995 (3 studies) | ⊕⊝⊝⊝ Very lowa,b,c,d |
Studies were clinically different so we did not combine them in meta‐analyses. 1 study included oral health education in both arms and found a benefit for sealant among children at high risk of caries. |
| Adverse effects | None reported | |||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||
aOne study with high risk of bias comparing resin‐modified glass ionomer versus fluoride varnish after 1 year (Florio 2001). bThe other two studies at two years, with incomplete information and analyses, compared chemically cured glass ionomer versus fluoride varnish (Ji 2007). The third study actually evaluated whether additional benefit was derived by using resin‐modified glass ionomer sealants and fluoride varnishes among children receiving regular oral health education (Tagliaferro 2011). cOne study at three years comparing chemically cured glass ionomer versus fluoride varnish, assessed as having high risk of bias (extensive incomplete information and analyses) (Ji 2007). dDowngraded because a small number of trials had high risk of bias and used different designs and follow‐up times.
Summary of findings 3. Resin‐based fissure sealant plus fluoride varnish versus fluoride varnish alone for preventing dental caries.
| Resin‐based fissure sealant plus fluoride varnish compared with fluoride varnish alone for preventing dental caries | ||||||
|
Population: children and adolescents at school in Germany Setting: preventive dentistry Intervention: resin‐based fissure sealant + fluoride varnish applications on occlusal tooth surfaces of permanent first molars Comparison: fluoride varnish applications to occlusal tooth surfaces of permanent first molars | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Fluoride‐varnished teeth | Sealed + fluoride‐varnished teeth | |||||
| Dentine caries in permanent molars Follow‐up: 2 years | 223 per 1000 | 144 fewer per 1000 (from 87 fewer to 176 fewer) | OR 0.30 (95% CI 0.17 to 0.55) | 92 (1 study) | ⊕⊝⊝⊝ Very lowa,b,c |
— |
| Adverse effects | Not measured | |||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; OR: odds ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aStudy conducted in the 1990s (Splieth 2001). bNo information on caries incidence among control teeth without treatment. Baseline caries of the study population (children five to eight years of age): mean decayed, missing and filled permanent surfaces 0.2. cDowngraded three levels because a single study (92 analysed participants) was conducted as early as the 1990s without information on caries incidence among control teeth without treatment, and although the study was otherwise well conducted, lack of blinding to outcome measurement caused further uncertainty about results.
Incorporating economic evidence
We have provided a "brief economic commentary" (BEC) to incorporate an economic perspective into the review. The methodology for the BEC follows that described in Chapter 20 of the Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (Shemilt 2019). The aim was to summarise the availability and principal findings of trial‐ and model‐based full economic evaluations (defined as a comparative assessment of costs and outcomes within a cost‐effectiveness, cost‐utility or cost‐benefit analysis framework.
Full economic evaluations that compared fissure sealants with fluoride varnish or fissure sealant plus fluoride varnish compared to fluoride varnish alone in children or adolescents up to age 20 years with at least one permanent molar were included for the BEC. The BEC focuses on the principal findings of the eligible economic evaluations and discusses the likely implications regarding whether the considered preventive approaches are likely to be cost‐effective, and if so, which approaches offer the best value for money from a health system, patient and societal perspective.
An initial search of PubMed was conducted to identify cost‐of‐illness studies describing, measuring and valuing the total resources used in the management of the most common oral diseases, with a focus on data reported for children and adolescents. The results of this search were used to inform the Background section of the review. A supplementary search strategy was conducted to identify relevant health economic evaluations to inform the BEC. The search process to identify full economic evaluation studies included a search of NHSEED up until March 2015 and a supplementary search of MEDLINE (1946 to March 2020) and Embase (1980 to March 2020) using the Scottish Intercollegiate Guideline Network filters for identifying economic studies. The full search strategy for the identification of economic evidence is available in Appendix 6.
The review author who is a health economist (DB) screened the articles and extracted basic data on study characteristics, including the analytical framework (trial‐ or model‐based analysis), type of economic valuation (cost‐effectiveness, cost‐utility, cost‐benefit analysis), analytical perspectives, time horizon, setting, main cost items (including currency and price year). He also extracted the principal findings of analyses including verbatim text on conclusions drawn by authors and text that summarised any uncertainty surrounding the authors’ principal conclusions (in the form of the results of any sensitivity analyses conducted).
We did not critically appraise any identified economic evaluations. The BEC is simply intended to focus on the extent to which principal findings of eligible economic evaluations indicated that different preventive interventions might be judged favourably (or unfavourably) over others from an economic perspective. A narrative summary of the findings of the BEC are provided in the Effects of interventions section of the review.
Results
Description of studies
Results of the search
From the database searches for this update, we identified 141 records after duplicates were removed. We identified two other potential studies. We rejected 106 records after reading the title or abstract, and we obtained the full text of 37 reports to assess eligibility for inclusion, contacting authors if additional information was required. We translated all non‐English language reports for study assessment. Review authors could read reports in English, German and Scandinavian. For this update, we consulted translators to identify and assess the non‐English reports that had potential for inclusion: Dutch (Vermaire 2015) and Chinese (Liu 2014) studies, which were excluded, and another Chinese study, which was included (Tang 2014).
Of the 37 full‐text reports, we excluded 20 because they had ineligible study design, participant population or setting (see Characteristics of excluded studies tables), and 14 were ongoing studies (see Characteristics of ongoing studies table). We identified three new studies for inclusion (Chestnutt 2017; Kalnina 2016; Tang 2014). We brought forward eight studies from the previous version, bringing the total number of included studies to 11 (15 references). See Figure 1.
1.
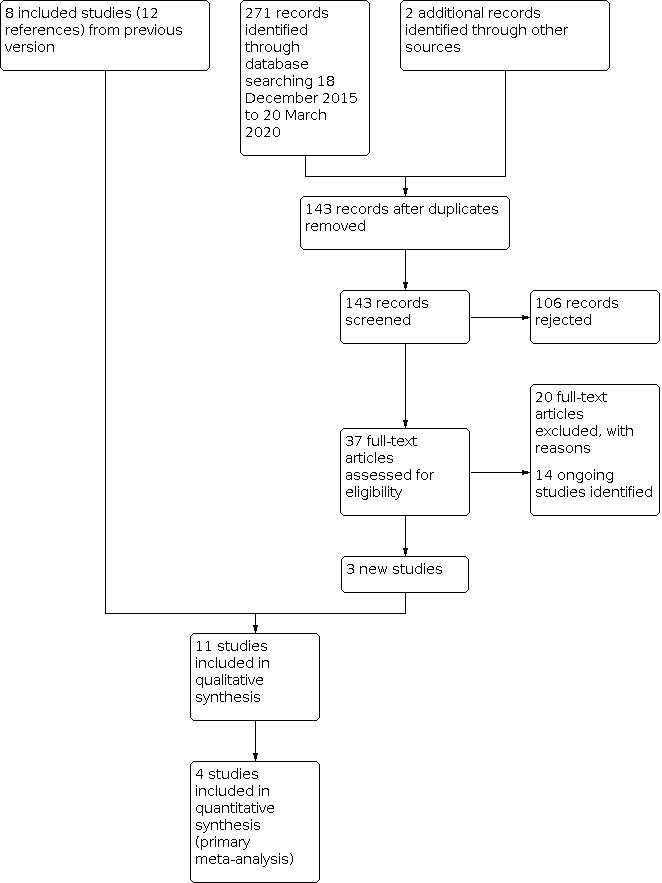
Study flow diagram.
The search for cost‐effectiveness studies retrieved 87 references, 38 remained after the removal of duplicates.
Included studies
This update includes 11 studies (Bravo 2005; Chestnutt 2017; Florio 2001; Ji 2007; Kalnina 2016; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011; Tang 2014).
The 11 included studies evaluated the relative effectiveness of fissure sealants (resin based or glass ionomer) compared with fluoride varnishes, or fissure sealants plus fluoride varnishes compared with fluoride varnishes alone, for preventing dental caries in the occlusal surfaces of permanent molars and premolars of children and adolescents. Dentinal caries means caries of a level of severity that would require intervention with restorative treatment.
Comparisons
Pit and fissure sealants versus fluoride varnishes: resin‐based fissure sealant versus fluoride varnish (seven studies) (Bravo 2005; Chestnutt 2017; Kalnina 2016; Liu 2012; Raadal 1984; Salem 2014; Tang 2014).
-
Glass ionomer fissure sealant versus fluoride varnish (one study) (Ji 2007); and resin‐modified glass ionomer fissure sealant versus fluoride varnish (two studies) (Florio 2001; Tagliaferro 2011).
Tagliaferro 2011 actually evaluated whether additional benefit is derived by using sealants and fluoride varnish among children receiving regular oral health education (the evaluation was carried out separately in populations with high risk and low risk of caries).
Pit and fissure sealant plus fluoride varnish versus fluoride varnish alone: resin‐based fissure sealant plus fluoride varnish versus fluoride varnish alone (one study) (Splieth 2001).
Study designs
Six of the 11 studies were of parallel‐group design (Chestnutt 2017; Florio 2001; Ji 2007; Kalnina 2016; Liu 2012; Tagliaferro 2011), two were split‐mouth studies, in which the two interventions (fissure sealant versus fluoride varnish (Raadal 1984) and fissure sealant plus fluoride varnish versus fluoride varnish alone (Splieth 2001)) were randomly allocated to teeth within a tooth pair. The studies by Bravo 2005, Salem 2014 and Tang 2014 were cluster‐randomised trials, the cluster being the school class. Details of studies are summarised in the Characteristics of included studies table.
Settings
Two studies were conducted in Brazil (Florio 2001; Tagliaferro 2011), three in China (Ji 2007; Liu 2012; Tang 2014), one in Germany (Splieth 2001), one in Iran (Salem 2014), one in Latvia (Kalnina 2016), one in Norway (Raadal 1984), one in Spain (Bravo 2005), and one in the UK (Chestnutt 2017). In 10 studies, children were recruited from public dental clinics or schools, and in the other study, children were enrolled from a private dental practice (Splieth 2001). The age range of the children in the studies was five to 10 years.
Interventions
In 10 studies, sealants and fluoride varnishes were applied to occlusal surfaces of permanent first molars. In one study, sealants and fluoride varnishes were applied to occlusal surfaces of premolars (Kalnina 2016); however, this study did not contribute data to our analyses as caries outcomes were zero in both groups at 12 months. Applications were done on sound surfaces (Bravo 2005; Ji 2007; Kalnina 2016; Salem 2014; Tagliaferro 2011), on surfaces with enamel lesions (Florio 2001), or in the same study on sound surfaces or on surfaces with enamel lesions (Chestnutt 2017; Liu 2012; Raadal 1984; Splieth 2001). In Raadal 1984, surfaces with initial caries in enamel to be sealed were prepared mechanically and caries removed before sealant was applied. In Tang 2014, sealants were applied for the permanent premolars or molars and sealant used only on sound surfaces or on enamel lesions (if scored using the ICDAS II scale, codes 0, 1, 2 and 3 are accepted); surface should not be sealed before.
The sealant material in Ji 2007 was glass ionomer; Florio 2001 and Tagliaferro 2011 used resin‐modified glass ionomer; and the other seven studies used resin‐based sealant materials: light‐polymerised resin sealant (Bravo 2005; Chestnutt 2017; Salem 2014; Splieth 2001; Tang 2014), light‐polymerised resin sealant with fluoride (Kalnina 2016; Liu 2012), and autopolymerised resin sealant (Raadal 1984). Five studies reported reapplication of sealants: Bravo 2005 reapplied sealants if partial or total loss had occurred since the previous examination after six, 12, 18, 24 and 36 months; Salem 2014 repaired or reapplied partially and completely lost sealants once if needed after six months; Splieth 2001 examined children semi‐annually for two years, and resealed sealants if necessary; Chestnutt 2017 examined the sealants six, 12, 18, 24 and 36 months, and reapplied if the existing sealant had become detached; and Kalnina 2016 resealed surfaces after six months if necessary.
Complete retention of resin‐based sealants after three years was 74.5% in maxillary molars and 91.4% in mandibular molars (Chestnutt 2017); after two years, complete retention of resin‐based sealants varied from 43% (Salem 2014) to 81% (Splieth 2001). Bravo 2005, with longer follow‐up time, reported complete resin sealant retention of 63% after four years and 39% after nine years. Retention of glass ionomer sealants was fairly high (66% complete retention after one year (Florio 2001 with resin‐modified glass ionomer); 84% after two years (Tagliaferro 2011 with resin‐modified glass ionomer); and 61% after three years (Ji 2007 with chemically cured glass ionomer)).
The fluoride varnishes used were: Durafluor 5% sodium fluoride (Medicom Worldwide Inc., Morrisville, PA, USA) (Salem 2014); Fluor Protector S (0.1%, or 1000 ppm fluoride) (Ivoclar Vivadent Inc., Amherst, NY, USA) (Ji 2007); Fluocal solute (Septodont, France) (Kalnina 2016); and Duraphat (5% sodium fluoride) (Colgate Oral Pharmaceuticals, New York, NY, USA) in the other seven studies. Eight studies applied fluoride varnish biannually to teeth of children in the varnish groups (Chestnutt 2017; Florio 2001; Ji 2007; Kalnina 2016; Liu 2012; Raadal 1984; Salem 2014; Tagliaferro 2011), and one study biannually to all teeth (Splieth 2001). Bravo 2005 applied Duraphat to newly erupted molars and reapplied it to all molars that had remained healthy after six, 12, 18, 24, 30, 36 and 42 months.
Co‐interventions
Six studies included other interventions in combination with the sealants and varnish. In Florio 2001, tap water was fluoridated and all children received professional prophylaxis during dental examination visits. In Raadal 1984, participants followed a fluoride rinsing programme at schools during follow‐up, and use of fluoride tablets was recommended. Splieth 2001 reported that 5% of children used fluoride tablets during the trial; however, it was not clear which participants were involved. Six studies reported motivation and instruction of participants towards good oral hygiene and use of fluoridated toothpaste (Florio 2001; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011).
Participants
Age and sex
The studies randomised 3374 children aged five to 10 years to sealant or varnish groups, and evaluated 2553 children. All studies included both boys and girls.
Caries prevalence at baseline
All studies except Ji 2007 and Salem 2014 stated the baseline caries prevalence of the study population. The only study from the 1980s stated that initial mean decayed, missing, filled deciduous teeth (dmft) was 4.7 (SD 3.3) (Raadal 1984).
The three studies conducted in the 1990s stated baseline caries prevalence as follows: in Florio 2001, mean dmfs in the sealant group was 3.8 (SD 2.5), and in the fluoride varnish group 4.5 (SD 2.7); and in Splieth 2001, initial mean DMFS was 0.2. In Bravo 2005, baseline mean decayed, filled deciduous teeth (dft) in the sealant group was 2.2 (SD 2.6), and in the varnish group 2.4 (SD 3.3).
The five studies from the 2010s stated baseline caries prevalences as follows: in Tagliaferro 2011, the baseline mean DMFT index was 4.51 (SD 2.81) for the HRS group (high‐caries‐risk children receiving sealants) and 4.28 (SD 2.54) for the HRV group (high‐caries‐risk children receiving fluoride varnishes), and in low‐caries‐risk groups, dmft plus DMFT was zero. In Liu 2012, baseline mean dmft in the sealant group was 3.19 (SD 2.68) and in the varnish group 3.58 (SD 2.25) for children eight to 10 years of age. In Tang 2014, the baseline mean DMFT index for seven‐ to eight‐year‐old children was 0.08. In Kalnina 2016, the baseline mean DMFT index for 10‐year‐old school children was 1.97. In Chestnutt 2017, the baseline mean DMFT index for six‐ to seven‐year‐old children was 3.2.
Dietary habits
Four studies gave information on diet (e.g. snacking habits of children). In Splieth 2001, during the trial, the mean frequency of cariogenic food intake per day was 15%, including a large number of sweetened drinks. In Liu 2012, at study baseline, 13% of children in the sealant group and 31% in the fluoride varnish group frequently consumed snacks twice a day or more (no information was provided on snacking habits during the trial). In Kalnina 2016, at study baseline, about 90% of children in both groups consumed snacks (with a mean of 2.06 times in sealant group and of 2.6 times in varnish group). Chestnutt 2017 distributed a questionnaire to the participants' parents and used it to collect information about dietary intake and habit, fluoride exposure and dental attendance. At baseline, about 60% of participants who responded to the questionnaire showed that children consumed a cariogenic diet (e.g. chocolate and sweets) between never and four to six times per week, with no significant differences between comparison groups. Throughout the study, there were no significant differences between intervention groups related to diet or other oral health‐related habits.
Outcome measures
An overview of the outcomes reported in each study is given in Table 6.
3. Outcomes for each study.
| Study | New caries lesion (yes/no) | Changes in caries from baseline DMFS on occlusal surfaces | Changes in caries from baseline DMFS on all surfaces | Changes in caries from baseline DMFT on all teeth | Progression of enamel carious lesions into dentine on treated occlusal surfaces | Time taken to apply intervention | Number of visits to repair sealant or apply varnish | Adverse events |
| Bravo 2005 | Yes at 2, 4, 9 years | — | — | — | — | — | Yes, over 4 years | Yes, over 4 years |
| Chestnutt 2017 | Yes, at 3 years | — | — | — | — | — | — | Yes, over 3 years |
| Florio 2001 | Yes, at 1 year | — | — | — | Yes, at 1 year | — | — | — |
| Ji 2007 | Yes, at 3 years | — | — | — | — | — | — | — |
| Kalnina 2016 | Yes, at 1 year but unable to use as 0 in both groups | — | — | — | — | — | — | Yes, over 1 year |
| Liu 2012 | Yes, at 2 years | — | — | — | — | — | — | Yes, over 2 years |
| Raadal 1984 | Yes, at 2 years | — | — | — | — | — | — | — |
| Salem 2014 | Yes, at 2 years but unable to use data | — | — | — | — | — | — | — |
| Splieth 2001 | Yes, at 2 years | — | Yes | — | — | Yes, over 2 years | — | Yes, over 2 years |
| Tagliaferro 2011 | — | Yes, at 2 years | — | — | — | — | — | — |
| Tang 2014 | — | — | Yes, at 2 years | Yes, at 2 years | — | — | — | — |
DMFS: decayed, missing and filled permanent surfaces; DMFT: decayed, missing and filled permanent teeth.
Ten studies reported the incidence of dentinal carious lesions on treated occlusal surfaces of first permanent molars in dichotomous form (yes/no). Tagliaferro 2011 reported data in continuous form as mean DMF increments. All studies used visual‐tactile caries diagnostic methods; In addition to visual‐tactile methods, some of the studies used additional methods to assess the caries progression. One study reported the endoscopic examination to be used (Florio 2001); and three studies reported X‐rays: digital X‐rays (Florio 2001), traditional X‐rays (Raadal 1984), and bitewing X‐rays were taken at baseline and after 12 months (Kalnina 2016). Salem 2014 reported caries incidences using two visual‐tactile measures: the WHO criteria (DMF) (WHO 1997) and Nyvad criteria (Nyvad 1999).
Other outcomes reported were caries progression rate (Florio 2001), changes in DMF scores on a whole‐mouth level (Splieth 2001), mean treatment time for sealing and varnish application (Splieth 2001), and mean DMFS (Tang 2014). Five studies considered adverse events (Bravo 2005; Chestnutt 2017; Kalnina 2016; Liu 2012; Tagliaferro 2011). The reported secondary outcomes in Florio 2001 were the number of permanent first molars remaining free of dentinal caries per child for those molars included in the trial; the caries status of treated or untreated caries on each surface of each first molar and the binary outcome of caries occurrence on occlusal versus non‐occlusal surfaces of each included first molar.
Details of all outcomes reported for each study are given in the Characteristics of included studies table.
Five studies stated intra‐examiner and inter‐examiner agreement for caries diagnosis: Liu 2012 reported the Kappa coefficient for intra‐examiner reliability to be over 0.9, Tagliaferro 2011 over 0.90, Salem 2014 about 0.8, and Bravo 2005 greater than 0.68. In Chestnutt 2017, inter‐ and intra‐examiner reproducibility were both high, with mean kappa scores of 0.82 for inter‐examiner and 0.89 for intra‐examiner.
Funding source
Six studies were supported by governmental or academic sources or by independent research foundations (Bravo 2005; Chestnutt 2017; Florio 2001; Liu 2012; Salem 2014; Tagliaferro 2011). The other five studies provided no information on funding.
Excluded studies
We excluded 20 for reasons presented in the Characteristics of excluded studies table. Reasons for exclusion varied, and for some studies, we identified several reasons for exclusion. The main reasons were: no randomisation or no mention of randomisation; not comparing sealant with fluoride varnish and flaws in outcome data.
Risk of bias in included studies
We contacted the authors of seven studies to request additional information for assessment of risk of bias, as information in the report was insufficient to permit final decisions (Bravo 2005; Florio 2001; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011). The studies by Ji 2007 and Tang 2014 were translated and data extracted by translators. 'Risk of bias' assessments for each individual study are presented in the 'Risk of bias' tables included under Characteristics of included studies, and results are presented graphically by domain over all studies (Figure 2) and by individual study (Figure 3).
2.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation was adequate, indicating low risk of bias in eight studies (72%) (Chestnutt 2017; Florio 2001; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011; Tang 2014). Random sequence was generated most often by using random numbers or tossing coins. We assessed one study at high risk of bias (Bravo 2005), and two at unclear risk of bias (Ji 2007; Kalnina 2016).
We graded allocation concealment at low risk of bias in six studies (Chestnutt 2017; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011). In four studies, allocation concealment was unclear (Florio 2001: Ji 2007; Kalnina 2016; Tang 2014), and in one study, it was at high risk of bias (Bravo 2005).
Blinding
Performance bias is possible in parallel trials (see Table 5) because personnel and participants are likely to know which of the two active preventive treatments a child is given, though it could be argued it is unlikely to affect dental behaviour of a child during the trial, especially when follow‐up is long (one or more years in this review). In split‐mouth trials, performance bias less of a risk as participants are very unlikely to perform oral hygiene differently in different parts of the mouth (Raadal 1984; Splieth 2001).
We assessed blinding of outcome measurement/assessment as high in all studies as the presence or absence of the sealant reveals if it has been used, assuming it has not been lost.
Incomplete outcome data
Two studies had follow‐up of 12 months: we assessed them at high risk of bias because dropout rates were unevenly distributed between study groups (Florio 2001; Kalnina 2016). The studies providing data at 24 months of follow‐up were at low risk of attrition bias (Ji 2007; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011; Tang 2014). The two studies providing data at 36 months of follow‐up were at low risk of bias in this domain (Chestnutt 2017; Ji 2007). The only study providing data at 48 months of follow‐up was at unclear risk of bias because no information on dropouts was provided by study group (there was 18% dropout across the study) (Bravo 2005). Bravo 2005 also measured outcomes at nine years of follow‐up and was at high risk of attrition bias at this time point as the proportion of participants assessed and included in the analysis was only 33%.
Selective reporting
All studies reported their prespecified outcomes adequately so were at low risk of bias.
Other potential sources of bias
Baseline imbalance
We assessed the comparability of study groups and possible co‐interventions during the trial as balanced between study groups in six studies (Bravo 2005; Liu 2012; Raadal 1984; Salem 2014; Splieth 2001; Tagliaferro 2011). Two of the six studies were of split‐mouth design, where conditions are the same for both teeth within a tooth pair (Raadal 1984; Splieth 2001); the other four studies were parallel‐group studies (Bravo 2005; Liu 2012; Salem 2014; Tagliaferro 2011). There was no information on comparability of study groups in Ji 2007, so our judgement was unclear risk of bias. Study groups in Kalnina 2016 were comparable in terms of age, sex and baseline caries, with no significant differences in caries risk factors (i.e. child's toothbrushing habits, snacking habits and family‐related factors); however, it was assessed as at unclear risk of bias as there was no information about randomisation and concealment 15 participants dropped out. We assessed Florio 2001 at high risk of bias due to imbalance at baseline.
Overall risk of bias
The overall risk of bias was high for all studies due to being unable to blind the interventions when undertaking outcome assessment.
Effects of interventions
See: Table 1; Table 2; Table 3
We present a summary of main results for the following comparisons: resin‐based sealant versus fluoride varnish (Table 1); glass ionomer or resin‐modified glass ionomer fissure sealant versus fluoride varnish (Table 2); and resin‐based fissure sealant plus fluoride varnish versus fluoride varnish alone (Table 3).
Results from nine studies are incorporated in this review (Bravo 2005; Chestnutt 2017; Florio 2001; Ji 2007; Liu 2012; Raadal 1984; Splieth 2001; Tagliaferro 2011; Tang 2014). Although the study by Salem 2014 met the inclusion criteria, results and data (complex multi‐level model with teeth nested in a child nested in a school class nested in a school) were not provided in useable form. In addition, the study by Kalnina 2016 met the inclusion criteria; however, the caries outcomes for both groups of fissure sealant and fluoride varnish at 12 months were zero so this did not contribute to the analysis. Kalnina 2016 applied interventions to the occlusal surfaces of premolars, but all other studies applied sealants and fluoride varnish to occlusal surfaces of permanent first molars.
Sealant versus fluoride varnish
Primary outcome – occurrence of new dentinal carious lesion on treated occlusal surfaces of molars or premolars
Resin fissure sealant versus fluoride varnish
Five studies compared resin‐based fissure sealant versus fluoride varnish: three reported results at two years (the split‐mouth study by Raadal 1984 and the parallel‐group studies by Liu 2012 and Tang 2014); one parallel‐group study reported results at three years (Chestnutt 2017); and one parallel‐group study reported results at two, four and nine years (Bravo 2005) (see Table 4).
In order to provide a more useful summary estimate of effect (rather than several single estimates of effect), we pooled the data for four studies with follow‐up periods between two and three years. This assumes that the OR, which is a relative measure, does not change over the follow‐up time period of two or three years. This meta‐analysis pooling the effect estimates of Bravo 2005, Chestnutt 2017, Liu 2012, and Raadal 1984, showed that we are uncertain whether resin fissure sealants are better than fluoride varnish in preventing dentinal carious lesions on treated occlusal surfaces of molars or premolars within the period of two to three years after initial treatment (OR 0.67, 95% CI 0.37 to 1.19; 1683 evaluated participants; Analysis 1.1). It should be stressed that these studies assessed odds of caries at different levels – person/child (Chestnutt 2017; Bravo 2005), tooth (Liu 2012), and surfaces (Raadal 1984), which could have affected precision of different estimates. There was high heterogeneity (I2 = 84%). We judged the certainty of the evidence to be very low. Tang 2014 found slight benefit of resin‐based sealant with DMFT at two‐year follow‐up (MD 0.08, 95% CI –0.14 to –0.02; 542 participants). The slight benefit that was observed in DMFT seems not to be clinically important on a scale from 0 to 28/32; however, if only existing permanent teeth of a child are taken into account when assessing this index, the difference could be relevant (Analysis 1.4).
1.1. Analysis.

Comparison 1: Resin fissure sealant versus fluoride varnish, Outcome 1: Dentinal caries at 2–3 years (yes/no)
1.4. Analysis.

Comparison 1: Resin fissure sealant versus fluoride varnish, Outcome 4: Increment in decayed, missing and filled permanent teeth at 2 years
Bravo 2005 found a significant difference in favour of visible‐light‐polymerised resin sealant compared with fluoride varnish, with an RR of 0.42 (95% CI 0.21 to 0.84; Analysis 1.2) at four years and 0.48 (95% CI 0.29 to 0.79; Analysis 1.3) at nine years of follow‐up (five years after the four years of active intervention; Analysis 1.3). As expected, dropout rates were high after nine years of follow‐up in Bravo 2005.
1.2. Analysis.

Comparison 1: Resin fissure sealant versus fluoride varnish, Outcome 2: Dentinal caries at 4 years (yes/no)
1.3. Analysis.

Comparison 1: Resin fissure sealant versus fluoride varnish, Outcome 3: Dentinal caries at 9 years (yes/no)
Glass ionomer fissure sealant versus fluoride varnish
Three studies evaluated glass ionomer fissure sealant versus fluoride varnish (Florio 2001; Ji 2007; Tagliaferro 2011). We were unable to perform any meta‐analyses and assessed the certainty of the evidence to be very low.
Resin‐modified glass ionomer fissure sealant versus fluoride varnish at one year
One small study, at high risk of bias, provided results for one year of follow‐up (Florio 2001; Table 4). This study found no significant difference between intervention groups at one year of follow‐up (OR 0.18, 95% CI 0.01 to 4.27; Analysis 2.1). All occlusal surfaces under examination had enamel lesions before applications.
2.1. Analysis.

Comparison 2: Resin‐modified glass ionomer fissure sealant versus fluoride varnish, Outcome 1: Dentinal caries at 12 months (yes/no)
Glass ionomer fissure sealant versus fluoride varnish at two years and three years
One study with incomplete information and analyses compared glass ionomer fissure sealant versus fluoride varnish at two years and three years (Ji 2007). In the statistical analyses of this study, clustering of teeth within a child was not taken into account (with adequate standard errors of estimates), and no information on numbers of children at follow‐up times was available for re‐analysis of data. However, because the numbers of decayed teeth were small in both groups, we decided to report the absolute numbers of decayed tooth surfaces in sealant and fluoride varnish groups without effect estimates (ignoring the clustered data). We noted no significant differences in rates of caries development between groups (at 24 months, 11/321 (3.4%) sealed surfaces and 13/320 (4.1%) fluoride‐varnished surfaces were decayed, and at 36 months, 22/311 (7.1%) sealed surfaces and 24/320 (7.5%) fluoride‐varnished surfaces were decayed). The rate of caries in the control group without intervention was 14% (48/348) at 24 months and 21% (71/340) at 36 months.
Resin‐modified glass ionomer cement plus oral health education versus fluoride varnish plus oral health education at two years
One study provided results for comparison of resin‐modified glass ionomer cement plus oral health education every three months versus fluoride varnish application biannually plus oral health education every three months (Tagliaferro 2011). The comparison was performed separately for high‐caries‐risk children and for low‐caries‐risk children. Groups to be compared were HRS (high‐risk children with sealant application plus oral health education) versus HRV (high‐risk children with fluoride varnish application plus oral health education); and LRS (low‐risk children with sealant application plus oral health education) versus LRV (low‐risk children with fluoride varnish application plus oral health education).
Investigators reported results as follows: after 24 months, the HRS group showed significantly smaller caries increments when compared with the HRV group (mean DMF increments on occlusal surfaces of first permanent molars was 0.06 (SD 0.25) in the HRS group and 0.29 (SD 0.68) in the HRV group (MD 0.23, 95% CI 0.02 to 0.44; P = 0.03). For low‐risk groups, there were no statistically significant differences among treatments with mean DMF increment of 0.02 (SD 0.15) for LRS and 0.09 (SD 0.29) for LRV groups (MD 0.07, 95% CI –0.03 to 0.17; P = 0.16). Study authors concluded "that in a 2‐year period, oral health education was sufficient to control occlusal caries in low‐risk children while for high‐risk children, sealant application in addition to oral health education was considered the best strategy."
Heterogeneity
Results of the meta‐analysis of four studies evaluating fissure sealants versus fluoride varnishes at two to three years showed no evidence that one intervention is more effective than another although the result is uncertain (Bravo 2005; Chestnutt 2017; Liu 2012; Raadal 1984). It should be noted that the superiority of sealants noted in the Norwegian split‐mouth study by Raadal 1984 may have been influenced by the carry‐over effect of fluoride varnish, even though this is unlikely due to a fast‐setting base and a small amount of fluoride varnish applied to one or two control teeth. Further, this split‐mouth study provided no information on caries incidence in control teeth without treatment and was conducted in early 1980s. It might be the possibility that the risk of caries was higher in 1980s have influenced the superiority of sealants noted in the Norwegian split‐mouth study by Raadal 1984.
In the British study by Chestnutt 2017, the fissure sealants were placed on sound occlusal surfaces of first permanent molars and reapplied when partially or totally lost during the 36 months of follow‐up, whereas the fluoride varnish was applied biannually. The sealant retention at 36 months was reported as 74.5% in maxillary first permanent molars and 91.4% in mandibular first permanent molars. The proportion of children who developed dentine caries dmft on at least one molar at 36 months was generally similar in both intervention arms (19.6% the fissure sealant arm and 17.5% in the fluoride varnish arm).
In the Chinese study conducted by Liu 2012, numbers of decayed tooth surfaces in all groups were small (at 24 months of follow‐up, proportions of pit/fissure sites with dentine caries in the sealant group was 1.6%, fluoride varnish group 2.4% and control group 4.6%). In Liu 2012, the low incidence of fissure caries in the control group without treatment may be explained in part by today's slower dental caries progression rate (Frencken 2017).
Two studies included surfaces with enamel caries lesions, in addition to sound surfaces (Liu 2012; Raadal 1984). Raadal 1984 opened surfaces with enamel lesions mechanically before sealant application, but researchers provided no information on the number of such surfaces included. In the study by Liu 2012, 35% of tooth sites had early‐stage caries at baseline. In the study by Raadal 1984, retention of sealants after 23 months of follow‐up was better (63%) than in the study by Liu 2012, which reported 46% retention of sealants. Both studies reported prevalence of caries in primary teeth at baseline, and it was slightly lower in Liu 2012 (baseline mean dmft 3.19 (SD 2.68) in sealant group and 3.58 (2.25) in fluoride varnish group). In Raadal 1984, the mean dmft was 4.7 (SD 3.3).
The Spanish study by Bravo 2005 (started in 1990), which placed sealants on sound surfaces and reapplied them when partially or totally lost during the four‐year active preventive programme, found resin sealants better than fluoride varnishes at four years and nine years of follow‐up. Complete sealant retention was 63% at four years and 39% at nine years. The incidence of caries in the control group after nine years was 77% on occlusal surfaces, whereas 26.6% of sealant teeth and 55.8% of fluoride‐varnished teeth had developed caries at nine years. Caries prevalence among primary teeth at baseline was stated as mean dmft in the sealant group 2.24 (SD 2.59) and in the fluoride varnish group 2.42 (SD 3.26). The total dropout rate of Bravo 2005 at nine years of follow‐up was high (67%), undermining the reliability of results.
The Chinese study by Tang 2014 applied the fluoride varnish biannually (four times in two years) and placed fissure sealants once on sound occlusal surfaces of first permanent molars. Sealant retention was 90.12% at two years. The increment of dental caries was less in the sealant group (DMFT 0.06 (SD 0.26); DMFS 0.06 (SD 0.26)) compared to the varnish group (DMFT 0.14 (SD 0.44); DMFS 0.15 (SD 0.45)).
Primary outcome – changes from baseline in decayed, missing and filled figures at surface, tooth and whole‐mouth levels
The studies did not report changes from baseline in DMF figures at surface, tooth and whole‐mouth levels.
Primary outcome – progression of dentinal carious lesions into enamel or dentine
One study, which compared resin‐modified glass ionomer fissure sealant versus fluoride varnish at one year, included at baseline only enamel caries lesions and reported at 12 months whether arrestment of enamel caries lesions or progression into dentine caries with both interventions (Analysis 2.1) (Florio 2001). We are uncertain if the sealant is better than fluoride varnish in preventing the progression of caries on treated surfaces from enamel to dentin as the effect was very imprecise due to small sample size (OR 0.18, 95% CI 0.01 to 4.27).
Secondary outcome – time taken to apply pit and fissure sealant or fluoride varnish
None of the studies measured time taken to apply pit and fissure sealant or fluoride varnish.
Secondary outcome – number of visits to the dentist for repair of sealant or fluoride varnish application
One study directly reported the number of visits for repair or reapplication of sealants or fluoride varnish applications (Bravo 2005). The mean number of treatment visits per child during the active phase of the programme was 2.2 (SD 1.1) (maximum 6) for children in the resin sealant group and 7.3 (SD 1.0) (maximum 8) for children in the varnish group (MD 5.02, 95% CI 4.55 to 5.94; fewer visits in the sealant group). This difference is great because the sealant was reapplied only when partial or total loss occurred, whereas the varnish was systematically reapplied.
Secondary outcome – safety of using sealants and fluoride varnishes assessed by presence or absence of adverse events
Five studies considered adverse events associated with sealants and fluoride varnishes (Bravo 2005; Chestnutt 2017; Kalnina 2016; Liu 2012; Tagliaferro 2011). Participants detected and reported no adverse events.
Sealant plus fluoride varnish versus fluoride varnish alone
One split‐mouth study compared resin‐based fissure sealant plus fluoride varnish versus fluoride varnish alone, and analysed 92 children after two years (Splieth 2001).
Primary outcome – occurrence of new dentinal carious lesions on treated occlusal surfaces of molars or premolars
Investigators found a significant difference in favour of the sealant plus fluoride varnish compared with fluoride varnish alone (OR 0.30, 95% CI 0.17 to 0.55; Analysis 3.1; Table 4). There was a caries increment of 5.5% (9 children) in sealed teeth compared to 17.5% (30 children) in teeth that received fluoride varnish only. This study considered both sound occlusal surfaces and surfaces with enamel lesions. Incomplete blinding of outcome measurement caused some uncertainty in the results, although the study was otherwise well conducted. We assessed the certainty of the evidence as very low because of the risk of detection bias, small number of participants, age of the study (conducted in the 1990s) and lack of information on caries incidence among control teeth without treatment.
3.1. Analysis.

Comparison 3: Resin fissure sealant plus fluoride varnish versus fluoride varnish, Outcome 1: Dentinal caries at 24 months (yes/no)
Primary outcome – changes from baseline in decayed, missing and filled figures at surface, tooth and whole‐mouth level
Splieth 2001 reported changes in DMF index at the whole‐mouth level during this study. The mean DMFS score of the whole mouth in the study population increased from 0.2 to 0.6 after one year and to 1.1 after two years. Study authors reported that most caries still occurred on occlusal surfaces of first permanent molars (50.9%).
Primary outcome – progression of dentinal carious lesions into enamel or dentine
The study did not report progression of dentinal carious lesions into enamel or dentine.
Secondary outcome – time taken to apply pit and fissure sealant or fluoride varnish
Splieth 2001 reported a mean treatment time for sealing and fluoride varnish application. Total time needed for sealing and resealing of two teeth was on average 29 minutes during two years, of which most of the time was spent on initial sealants (about 17 minutes). Mean treatment time for each fluoride varnish application was under three minutes (total time during intervention: nine minutes; SDs not presented).
Secondary outcome – number of visits to the dentist for repair of sealant or fluoride varnish application
The study did not measure the number of visits to the dentist for repair of sealant or fluoride varnish application.
Secondary outcome – safety of using sealants and fluoride varnishes assessed by presence or absence of adverse events
Splieth 2001 did not measure adverse events, but five other studies in this review that did evaluate sealants and fluoride varnish reported there were no adverse events for either intervention (see 'Sealant versus fluoride varnish').
Brief economic commentary
To supplement the main systematic review of the effectiveness, we sought to identify trial‐ and decision model‐based economic evaluations of pit and fissure sealants compared to fluoride varnish or fissure sealant plus fluoride varnish compared to fluoride varnish alone for children or adolescents in permanent teeth. Our search identified four relevant economic evaluations.
Two studies conducted Markov decision analysis models to assess the cost‐effectiveness of fissure sealant versus fluoride varnish (Chestnutt 2017 in the UK; Khouja 2018 in the USA). Chestnutt 2017 conducted a within‐trial and model‐based (five‐ and 10‐year time horizon) economic evaluation to assess the cost‐effectiveness (cost per 1% proportion of caries into dentine prevented) and cost‐utility (cost per quality‐adjusted life year (QALY)) of resin‐based fissure sealant (checked and replaced as necessary) compared to fluoride varnish (six‐monthly over 30 months). The study was conducted in children aged six and seven years with at least one fully erupted first permanent molar free of caries into dentine, attending mobile dental clinics at primary schools in Wales. A healthcare payer and partial societal (including costs to families) perspective were considered. The within‐trial analysis found that, over three years of follow‐up, fissure sealants were more costly from both an NHS (2015 data: MD GBP 68.13, 95% CI GBP 5.63 to GBP 130.63; P = 0.033) and partial societal (2015 data: MD GBP 71.96, 95% CI GBP 7.21 to GBP 136.71; P = 0.029) perspective. Given the trial demonstrated no differences in effects, or QALYs, the within‐trial analysis found that fluoride varnish was the most likely cost‐effective strategy, with a probability of cost‐effectiveness of 70% at a threshold willingness to pay for a QALY gain of GBP 20,000. The Markov extrapolation model found that fluoride varnish was also less costly and more effective in the longer term, with a probability of cost‐effectiveness in excess of 95% at the same threshold value. Despite some limitations around the short time horizon of the economic model, which the authors explain was due to a lack of robust long‐term data in dentistry, this appears to be a methodologically robust economic evaluation, in the context of the current data availability. The authors appropriately acknowledge that there is a need for future work to develop and improve on preference‐based utility instruments to aid economic evaluation of dental care interventions.
Khouja 2018 conducted a cost‐effectiveness analysis (cost per first carious lesion averted), using a Markov model with nine‐year time horizon, in a USA general dental practice setting, in children with first permanent molars. The study found that, assuming all fissure sealants would be replaced, fissure sealants were less expensive, with cost savings of USD 324.09 per case (2011 data) and more effective (+0.31 additional first cases of caries avoided) compared to fluoride varnish in preventing occlusal dental caries lesions, and were thus deemed likely to be cost‐effective. It is relevant to note, however, that the study considers only the costs of intervention delivery, and does not consider the potential cost savings associated with avoidance of expensive restorative treatment for carious lesions for the more effective intervention. If the underpinning clinical effectiveness data are robust, and based on sound methodology, then the inclusion of downstream treatment costs would likely improve the cost‐effectiveness case for fissure sealants in this scenario.
Two further studies conducted simple calculations of mean cost‐effectiveness ratios in Australian and US settings (Enno 1982 in Australia; Neidell 2016 in the USA). Enno 1982 found that over two years, the ratio of cost savings in terms of caries treatment avoided to intervention delivery costs for preventive care was 2.1:1 (over three years) for fluoride varnish and 0.77:1 (over two years) for fissure sealants. Mean cost‐effectiveness ratios for fluoride varnish were AUD 3.49 (1982 values over three years) per surface saved for fissure sealants and AUD 18.49 (1982 values over two years) per surface saved for fluoride varnish. It should be noted that these mean cost‐effectiveness ratios were based on a naive comparison of effectiveness between two potentially quite heterogeneous studies, with different follow‐up periods, and should thus be interpreted cautiously. Neidell 2016 conducted a simple calculation of the mean cost per 1% caries reduction for fissure sealants (with possibility of re‐application) and fluoride varnish (every six months) over a 3.5‐year time horizon in a USA school‐based setting. The study included only intervention costs, from the healthcare provider perspective and did not consider longer‐term cost implications. The average cost‐effectiveness ratio (ACER) (year not reported) for fissure sealants was USD 136.63, compared to USD 85 to USD 102 across different percentage reduction in caries explored for fluoride varnish. The study concluded that fluoride varnish may be more cost‐effective because fissure sealants are more costly to deliver. However, the author's conclusions require cautious interpretation. The study excluded any longer‐term cost savings associated with treatment of decay avoided as a result of the more clinically effective intervention. The study was conducted over a short time and may not have captured all the costs and benefits of relevance to decision makers (e.g. the full extent of long‐term benefits).
Discussion
Summary of main results
Resin fissure sealants versus fluoride varnishes
The conclusion of this review has now changed with the addition of one new large, good‐quality study (Chestnutt 2017). We are uncertain whether sealants were superior to fluoride varnish (or vice versa) over 36 months of follow‐up. Four studies with follow‐up times of two to three years contributed to a pooled estimate found no differences in effectiveness. There was substantial heterogeneity and we assessed the certainty of the evidence as very low, in contrast to the last published version of the review, which assessed the certainty as low. One study found a slightly greater reduction in caries increment with sealants (Raadal 1984), but this study was conducted more than 30 years ago when caries incidence was higher and progression more rapid. At four and nine years of follow‐up, results from one small study suggested a benefit for sealant, but we considered this limited evidence to be very low certainty (Bravo 2005). Overall, we interpret the current body of evidence to suggest that there may be no difference in effectiveness between resin fissure sealants and fluoride varnish when applied to occlusal surfaces of permanent molars, with both interventions reducing caries incidence. It should also be stressed that Chestnutt 2017 investigated the sample with apparently the lowest risk of caries among four analysed trials while the effect of sealants is more visible in high‐risk populations. In future studies, grouping of studies by baseline risk might give more clear answers. In addition the results of Tang 2014 on DMFT data and Bravo 2005 on RR data, both point toward significant improvement of outcomes by the use of sealants as intervention; however, in the case of Tang 2014 it is probably not clinically important.
Glass ionomers and resin‐modified glass ionomers versus fluoride varnishes
Three studies – one with traditional glass ionomer (Ji 2007) and two with resin‐modified glass ionomer (Florio 2001; Tagliaferro 2011) – compared glass ionomer versus fluoride varnish. Meta‐analysis was not possible. The small study by Florio 2001 analysed 21 participants and reported no differences between resin‐modified glass ionomer sealant and fluoride varnish at one year. Retention of sealant was 66%. In contrast, Tagliaferro 2011 concluded that over a two‐year period, sealant application in addition to oral health education was the best strategy for children at high risk of caries. The retention rate was high (84% after 24 months). In Ji 2007, numbers of decayed teeth were small in both treatment groups, after two years of follow‐up (at 24 months: 3.4% of sealed surfaces and 4% of fluoride‐varnished surfaces were decayed; at 36 months: 7.1% of sealed surfaces and 7.5% of fluoride‐varnished surfaces were decayed). Rates of caries in control group teeth without intervention were 14% at 24 months and 21% at 36 months. Sealant retention was 60% after three years. Again we are uncertain that glass ionomer and resin modified glass ionomer sealants were superior to fluoride varnish.
Sealant plus fluoride varnish versus fluoride varnish alone
The German split‐mouth study found that sealant given concurrently with fluoride varnish was better than fluoride varnish alone at 24 months' follow‐up (Splieth 2001). Children were examined twice a year for two years; sealants were resealed if necessary and fluoride varnish was applied to all teeth at the time of examination (including the sealed tooth). Study authors reported that the study was conducted in a low‐caries‐risk population and that retention rate of the sealants was high (81%). However, the mean frequency of cariogenic food intake per day was reported to be 15, including a large number of sweetened drinks. Oral hygiene was moderate.
Safety of using sealants and fluoride varnishes assessed by presence or absence of adverse events
Five studies assessed or considered adverse events of sealants and fluoride varnishes (Bravo 2005; Chestnutt 2017; Kalnina 2016; Liu 2012; Tagliaferro 2011). Participants did not detect or report any adverse events during or in the 48 hours after treatment in intervention groups and no adverse event were reported during the follow‐up period.
However, some systematic reports have considered the possible oestrogen‐like effects of resin‐based materials including BPA (Azarpazhooh 2008a; Fleisch 2010). This synthetic chemical resin is widely used in the production of plastic products intended for everyday life but are rarely used as such in dental materials (ADA 2003). Dental resins include primarily BPA derivatives (e.g. bisphenol A‐glycidyl methacrylate, bisphenol A dimethacrylate) rather than pure BPA. These derivatives can hydrolyse to BPA and can be detected transiently in saliva (Arenholt‐Bindslev 1999; Schmalz 1999). BPA has been detected in saliva for up to three hours after application of resin sealants (Fleisch 2010). Evidence suggests that patients are not at risk for oestrogen‐like effects when sealants are used (ADA 2003; Azarpazhooh 2008a; Fleisch 2010). The American Dental Association has concluded that estimated BPA exposure from dental materials is recorded as very low compared with total estimated daily BPA exposure from food and environmental sources (ADA 2003).
Brief economic commentary
We did not subject the identified economic evaluations to a formal critical appraisal and we did not attempt to draw any firm or general conclusions regarding the relative costs or efficiency of different preventive programmes. However, evidence collected from economic evaluations with more rigorous methodological quality (i.e. Chestnutt 2017) indicates that fluoride varnish may achieve similar outcomes to fissure sealants, but at lower costs. However, it is noted that this study was conducted in the UK setting and that the findings may not be transferable to other settings or health systems. The BEC notes that other studies, of generally low quality, draw varying conclusions regarding the most cost‐effective preventive strategy. End users of this review will need to assess the extent to which methods and results of the higher quality Chestnutt 2017 evaluation may be applicable (or transferable) to their own setting or country's health system. It is possible that further context‐specific health economic evaluations may be required.
Overall completeness and applicability of evidence
Date
Two studies were undertaken since the last review update in 2016 (Chestnutt 2017; Kalnina 2016). Eight studies were conducted between 2000 and 2014 (including one added in this update, Tang 2014), and one was in the 1980s.
Setting
Most studies recruited children from schools or public‐oriented dental clinics. One study enrolled children from a private dental practice (Splieth 2001). In general, these studies were conducted in well‐equipped dental settings.
Diagnosis
This review compared sealants versus fluoride varnishes for prevention or control of caries, and we accepted studies with sound occlusal surfaces of molars and premolars or with enamel lesions. Seven of the 11 included studies reported applications only on sound surfaces (Bravo 2005; Chestnutt 2017; Ji 2007; Kalnina 2016; Salem 2014; Tagliaferro 2011; Tang 2014); one study only on surfaces with enamel lesions (Florio 2001); and three studies on sound surfaces or on surfaces with enamel lesions (Liu 2012; Raadal 1984; Splieth 2001). In addition to clinical‐tactile caries diagnostic methods, two studies used other diagnostic methods before applications. Liu 2012 used the DIAGNOdent laser fluorescence device (KaVo Dental Corporation, Lake Zurich, IL, USA) to rule out molars with caries in dentine and fissures with potential dentine caries, and Florio 2001 used digital radiographic and endoscopic examinations to evaluate restricted enamel decay lesions.
Caries diagnosis on occlusal surfaces can, however, be challenging. Conventional visual, tactile and radiographic methods in the diagnosis of occlusal caries have not been accurate enough to identify whether a lesion extends into the dentine (McComb 2001). New technologies such as laser fluorescence methods (e.g. DIAGNOdent device) may be sensitive in detecting occlusal dentinal caries (Bader 2004; Twetman 2013), but the likelihood of false‐positive diagnoses may increase when laser fluorescence is used rather than visual methods (Bader 2004). Regardless of the caries diagnostic method used, the condition of an occlusal surface to be sealed or varnished remains in any case somewhat unclear.
Ongoing studies
There are 10 ongoing trials that may contribute to our next update and help clarify our findings.
Quality of the evidence
Resin‐based sealant versus fluoride varnish
We assessed the certainty of the body of evidence for resin‐based pit and fissure sealants compared with fluoride varnishes as very low according to GRADE assessment criteria (Table 1). The pooled estimate of four studies found no evidence to conclude that resin sealants or fluoride varnishes were superior at two to three years (OR 0.67, 95% CI 0.37 to 1.19); the studies were well conducted (Bravo 2005; Chestnutt 2017; Liu 2012; Raadal 1984), but incomplete blinding of outcome measurements/assessments may have caused bias in the results. At four and nine years, the only study evaluating this comparison (with high dropout rates) found more caries on fluoride‐varnished occlusal surfaces than on resin‐sealed surfaces (Bravo 2005).
Two of the studies individually showed similar effectiveness between resin sealants and fluoride varnishes. One was conducted in the 2000s; the other was conducted between 2011 and 2013 (Chestnutt 2017). One study did not contribute to the analyses as there was no caries development in either group at 12 months (Kalnina 2016). The two studies favouring sealants were conducted earlier in the 1980s and 1990s. It has been stated that the progression rate of caries in permanent teeth has become slower (Whelton 2004), and varies between populations, making the evidence uncertain, especially when the follow‐up time is fairly short. Effectiveness of resin‐based sealants is strongly related to retention of sealant, and retention also depends on follow‐up time.
Glass ionomer and resin‐modified glass ionomer versus fluoride varnishes
We assessed the certainty of the body of evidence for glass ionomer sealants (one study with original chemically cured material, and two studies with a light curable type modified with resin) compared with fluoride varnishes as very low according to GRADE assessment criteria (Table 2). This rating implies that we are very uncertain about the estimates. Although all three studies comparing glass ionomer versus fluoride varnish reported similar results (no differences between interventions), we downgraded the evidence by three levels because of the small number of trials, with different designs and follow‐up times, which were at high or unclear risk of bias. Further, Tagliaferro 2011 evaluated whether additional benefit was derived from sealants and fluoride varnishes among children receiving regular oral health education.
Sealant plus fluoride varnish versus fluoride varnish alone
We assessed the body of evidence comparing resin‐based sealant plus fluoride varnish versus fluoride varnish alone at very low certainty according to GRADE assessment criteria (Table 3). We downgraded the certainty of the evidence by three levels because the comparison included one study (92 analysed participants) conducted in the 1990s and there was no information on caries incidence of control teeth without treatment, and, although the study was otherwise well conducted, there was no blinding of outcome measurement.
Potential biases in the review process
Study design
In a split‐mouth design, it could be assumed that varnish applied to control teeth might also impact teeth in the intervention group through saliva. However, Sköld‐Larsson 2000 showed that fluoride varnish application elevated fluoride concentrations of dental plaque locally in the treated teeth quadrant but not in the opposite untreated quadrant. Any carry‐over effect of fluoride varnishes would most probably be dose dependent, and we assessed carry‐over effects on sealed occlusal surfaces to be insignificant because they have a fast‐setting base and only a small amount of fluoride varnish was applied to one or two control teeth. Therefore, we decided to accept split‐mouth studies into this review. We grouped the studies based on the used sealants material. Although sealants will work as physical barrier, they still have different properties based on their materials which presumably may influence their performance and longevity.
Reporting bias
We decided to consider only studies with a full‐text report. We excluded studies reported only as abstracts because evidence has shown discrepancies between data reported in the abstract and provided in the final published full report, and has indicated that information on trial quality indicators is often lacking (Chokkalingam 1998; Hopewell 2006). Thus, we judged that the full‐text report was required to ensure reliable data extraction and assessment of risk of bias. To diminish risk of publication bias, we contacted the authors of potential abstracts to ask whether a full‐text report of the study (unpublished or published) was available.
Agreements and disagreements with other studies or reviews
Neusser 2014 considered fissure sealants versus fluoride varnishes and presented conclusions based on the trials of Bravo 2005, Raadal 1984, and Tagliaferro 2011 (which are also included in this review), and on a previous version of this Cochrane systematic review (Hiiri 2010). The review by Neusser 2014 concluded, "The studies and literature reviews have shown protective effects of pit and fissure sealants compared to the professional application of fluorides, particularly in children and adolescents at high caries risk. However, because of methodological flaws, the results of the RCTs should be interpreted with caution."
Another well‐conducted systematic review was undertaken by Wright 2016 and included three studies at two to three years' follow‐up, one of which was Liu 2012. The review concluded that there was beneficial effect of using sealant compared to varnish; however, they emphasised that this was not statistically significant and the studies were of low quality.
A recent systematic review combined slightly different studies in their main meta‐analysis but reached the same conclusion as this review, that the evidence does not suggest either intervention is superior (Li 2020).
Authors' conclusions
Implications for practice.
In this review, we found no evidence suggesting the superiority of resin‐based (or glass‐ionomer based) fissure sealants over fluoride varnish or vice versa, although this was very low certainty evidence. It should be noted that other Cochrane Reviews have shown that both interventions are effective for preventing occlusal caries in the first permanent molars. We did find some very low‐certainty evidence for placing resin‐based sealant and applying fluoride varnish rather than applying fluoride varnish only. Available data are insufficient to reach conclusions about whether it is better to apply sealants or fluoride varnishes on occlusal surfaces of permanent molars, and so either intervention, or both, can be used.
Implications for research.
More high‐quality research is needed to compare the relative effectiveness of sealants versus fluoride varnishes for preventing dental decay on occlusal surfaces. Fourteen studies are currently ongoing and their findings may allow us to draw firmer conclusions. With a split‐mouth study design, the carry‐over effect of fluoride varnish applications on the sealed teeth cannot be totally ruled out. Therefore, a parallel‐group design would provide the most reliable information on differences in effectiveness of sealants and fluoride varnishes. Proper documentation and description of study populations, intervention study designs, follow‐up periods, dropouts and outcomes as described in the CONSORT statement are recommended. In future studies, baseline risk of caries should be recorded and study participants could be grouped based on their baseline caries and caries risk.
What's new
| Date | Event | Description |
|---|---|---|
| 15 December 2020 | Amended | Minor edit |
History
Protocol first published: Issue 2, 2001 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 19 March 2020 | New citation required and conclusions have changed | The evidence available was uncertain, but did not show superiority of either resin‐based fissure sealants over fluoride varnishes or vice versa, to prevent occlusal caries in permanent molars. |
| 19 March 2020 | New search has been performed | This review is an update of one first published in 2006, then updated in 2010 and in 2016. Search strategies were amended and the search updated. This 2020 update contains 11 included studies (three new since the last version: Chestnutt 2017; Kalnina 2016; Tang 2014), involving 3374 participants in total. We identified 14 ongoing studies. The author team has changed from the previous version of this review. |
| 18 February 2009 | Amended | Updated contact details for co‐author |
| 1 August 2008 | Amended | Converted to new review format |
Acknowledgements
We would like to thank Miss Anne Littlewood at Cochrane Oral Health in Manchester, UK, for help with searching the literature, and Miss Laura MacDonald and Mrs Janet Lear, also at Cochrane Oral Health, for the assistance they provided. We thank Information Specialist Jaana Isojärvi at The National Institute for Health and Welfare/THL, Finland, for help with the supplementary search of the literature. We would like to thank Jennifer Hilgart, Prof Chris Deery and Prof Andrew L Sonis for the helpful and constructive feedback they provided. We warmly thank Dr Valeria Marinho, Dr Vasiliy V Vlassov, Dr Joanna M Zakrzewska, Zhao‐Shao‐feng, Prof Shi Zongdao, Prof Hua Chengge, Chunjie Li, Dr Liyuan Ma and Dr Margriet E van Baar for translating reports. We would also like to thank the following investigators who provided additional information about their trials: Dr M Bravo, Dr E Lo, Dr M Raadal, Dr AC Pereira, Dr K Salem, Dr C Splieth, Dr EP Tagliaferro and Dr SR Uma. We gratefully acknowledge the work of the previous authors of this review: Anneli Ahovuo‐Saloranta, Helena Forss, Anne Hiiri, Anne Nordblad and Marjukka Mäkelä.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
Cochrane Oral Health's Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see oralhealth.cochrane.org/trials.
For this update, Cochrane Oral Health's Trials Register was searched via the Cochrane Register of Studies using the search strategy below.
1 (fluoride* or fluor or "PPM F" or PPMF or APF or NAF or "Sodium F" or "Amine F" or SNF2 or "Stannous F" or "phosphat* F" or "acidulat* F" or "acidulat* fluor*" or "phosphat* fluor*" or fluorphosphat* or "amin* fluor*" or "sodium* fluor*" or "stannous* fluor*" or SMFP or MFP or monofluor*):ti,ab 2 (varnish* or lacquer* or laquer* or lacker* or lakk* or polyurethane*):ti,ab 3 #1 and #2 4 ((fissure* and seal*) or (dental and seal*)):ti,ab 5 ((compomer* and seal*) or (composite and seal*)):ti,ab 6 ("glass ionomer*" or glassionomer* or "cermet cement*" or "resin cement*"):ti,ab 7 #4 or #5 or #6 8 (#3 and #7) AND (INREGISTER)
In the previous version of this review, the following search strategy was used via the Procite software.
(((fluoride* AND (varnish* OR lacquer* OR laquer* or lakk* OR verniz* OR silane* OR polyurethane*)) AND ((“pit and fissure sealant*” OR (fissure AND seal*) OR “glass ionomer*” OR “resin cement*” OR enamel or tooth or teeth) AND seal*)))
Appendix 2. Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
#1 [mh "Topical fluorides"] #2 (fluoride* or fluor or "PPM F" or PPMF or APF or NAF or "Sodium F" or "Amine F" or SNF2 or "Stannous F" or "phosphat* F" or "acidulat* F" or "acidulat* fluor*" or "phosphat* fluor*" or fluorphosphat* or "amin* fluor*" or "sodium* fluor*" or "stannous* fluor*" or SMFP or MFP or monofluor*) #3 (varnish* or lacquer* or laquer* or lacker* or lakk* or polyurethane*) #4 #2 and #3 #5 #1 or #4 #6 [mh ^"Pit and fissure sealants"] #7 ((fissure* near/6 seal*) or (dental near/6 seal*)) #8 ((compomer* near/4 seal*) or (composite* near/4 seal*)) #9 [mh "Glass ionomer cements"] #10 [mh "Resin cements"] #11 ("glass ionomer*" or glassionomer* or "cermet cement*" or "resin cement*") #12 {or #6‐#11} #13 #5 and #12
In the previous version of this review, the following search strategy was used.
#1 FLUORIDES TOPICAL (single MeSH term) #2 (topical* NEXT fluoride*) #3 ((fluoride* or fluorine*) AND (varnish* OR lacquer* OR laquer* OR lakk* OR verniz* OR silane* OR polyurethane*)) #4 (#1 OR #2 OR #3) #5 PIT AND FISSURE SEALANTS (Single MeSH term) #6 fissure* NEAR seal* #7 GLASS IONOMER CEMENTS (Explode MeSH term) #8 glass ionomer* #9 cermet cement* #10 RESIN CEMENTS (Single MeSH term) #11 resin cement* #12 (#5 OR #6 OR #7 OR #8 OR #9 OR #10) #13 #4 AND #12
Appendix 3. MEDLINE Ovid search strategy
1. exp Fluorides, topical/
(fluoride$ or fluor or "PPM F" or PPMF or APF or NAF or "Sodium F" or "Amine F" or SNF2 or "Stannous F" or "phosphat$ F" or "acidulat$ F" or "acidulat$ fluor$" or "phosphat$ fluor$" or fluorphosphat$ or "amin$ fluor$" or "sodium$ fluor$" or "stannous$ fluor$" or SMFP or MFP or monofluor$).mp.
(varnish$ or lacquer$ or laquer$ or lacker$ or lakk$ or polyurethane$).mp.
2 and 3
1 or 4
"Pit and fissure sealants"/
(fiss$ adj6 seal$).mp.
(dental adj3 seal$).mp.
(compomer$ adj4 seal$).mp.
(composite$ adj4 seal$).mp.
exp Glass ionomer cements/
exp Resin cements/
("glass ionomer$" or glassionomer$ or "cermet cement$" or "resin cement$").mp.
or/6‐13
5 and 14
This subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity‐maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (Lefebvre 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
In the previous version of this review, the following search strategy was used.
1. exp TOPICAL FLUORIDES 2. topical adj6 fluoride$.mp. 3. ((varnish$ or lacquer$ or laquer$ or lakk$ or verniz$ or silane$ or polyurethane$) adj6 fluor$).mp. 4. 1 or 2 or 3 5. exp PIT AND FISSURE SEALANTS 6. (fiss$ adj6 seal$).mp. 7. exp GLASS IONOMER CEMENTS 8. exp RESIN CEMENTS 9. (“glass ionomer$” or “cermet cement$” or “resin cement$”).mp. 10. 5 or 6 or 7 or 8 or 9 11. 4 and 10
Appendix 4. Embase Ovid search strategy
Fluoride/
(fluoride$ or fluor or "PPM F" or PPMF or APF or NAF or "Sodium F" or "Amine F" or SNF2 or "Stannous F" or "phosphat$ F" or "acidulat$ F" or "acidulat$ fluor$" or "phosphat$ fluor$" or fluorphosphat$ or "amin$ fluor$" or "sodium$ fluor$" or "stannous$ fluor$" or SMFP or MFP or monofluor$).mp.
(varnish$ or lacquer$ or laquer$ or lacker$ or lakk$ or polyurethane$).mp.
1 or 2
3 and 4
"Fissure sealant"/
(fiss$ adj6 seal$).mp.
(dental adj3 seal$).mp.
(compomer$ adj4 seal$).mp.
(composite$ adj4 seal$).mp.
"Glass ionomer"/
Resin cements/
("glass ionomer$" or glassionomer$ or "cermet cement$" or "resin cement$").mp.
or/6‐13
5 and 14
This subject search was linked to Cochrane Oral Health's filter for identifying RCTs in Embase Ovid.
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 16. 14 NOT 15
In the previous version of this review, the following search strategy was used.
1. exp FLUORIDES, TOPICAL 2. topical adj6 fluoride$.mp. 3. ((varnish$ or lacquer$ or laquer$ or lakk$ or verniz$ or silane$ or polyurethane$) adj6 fluor$).mp. 4. 1 or 2 or 3 5. exp PIT AND FISSURE SEALANTS 6. (fiss$ adj6 seal$).mp. 7. exp GLASS IONOMER CEMENTS 8. exp RESIN CEMENTS 9. (“glass ionomer$” or “cermet cement$” or “resin cement$”).mp. 10. 5 or 6 or 7 or 8 or 9 11. 4 and 10
Appendix 5. US National Institutes of Health Trials Register and WHO International Clinical Trials Register Platform search strategy
varnish and sealant
Appendix 6. Search strategies for cost‐effectiveness studies
MEDLINE Ovid search strategy
1. exp Fluorides, topical/ 2. (fluoride$ or fluor or "PPM F" or PPMF or APF or NAF or "Sodium F" or "Amine F" or SNF2 or "Stannous F" or "phosphat$ F" or "acidulat$ F" or "acidulat$ fluor$" or "phosphat$ fluor$" or fluorphosphat$ or "amin$ fluor$" or "sodium$ fluor$" or "stannous$ fluor$" or SMFP or MFP or monofluor$).mp. 3. (varnish$ or lacquer$ or laquer$ or lacker$ or lakk$ or polyurethane$).mp. 4. 2 and 3 5. 1 or 4 6. "Pit and fissure sealants"/ 7. (fiss$ adj6 seal$).mp. 8. (dental adj3 seal$).mp. 9. (compomer$ adj4 seal$).mp. 10. (composite$ adj4 seal$).mp. 11. exp Glass ionomer cements/ 12. exp Resin cements/ 13. ("glass ionomer$" or glassionomer$ or "cermet cement$" or "resin cement$").mp. 14. or/6‐13 15. 5 and 14
This subject search was linked to the Scottish Intercollegiate Guideline Network filter for identifying economic studies in MEDLINE Ovid. Available at: www.sign.ac.uk/search-filters.html.
1 Economics/ 2 "costs and cost analysis"/ 3 Cost allocation/ 4 Cost‐benefit analysis/ 5 Cost control/ 6 Cost savings/ 7 Cost of illness/ 8 Cost sharing/ 9 "deductibles and coinsurance"/ 10 Medical savings accounts/ 11 Health care costs/ 12 Direct service costs/ 13 Drug costs/ 14 Employer health costs/ 15 Hospital costs/ 16 Health expenditures/ 17 Capital expenditures/ 18 Value of life/ 19 Exp economics, hospital/ 20 Exp economics, medical/ 21 Economics, nursing/ 22 Economics, pharmaceutical/ 23 Exp "fees and charges"/ 24 Exp budgets/ 25 (low adj cost).mp. 26 (high adj cost).mp. 27 (health?care adj cost$).mp. 28 (fiscal or funding or financial or finance).tw. 29 (cost adj estimate$).mp. 30 (cost adj variable).mp. 31 (unit adj cost$).mp. 32 (economic$ or pharmacoeconomic$ or price$ or pricing).tw. 33 Or/1‐32
Embase Ovid search strategy
1. Fluoride/ 2. (fluoride$ or fluor or "PPM F" or PPMF or APF or NAF or "Sodium F" or "Amine F" or SNF2 or "Stannous F" or "phosphat$ F" or "acidulat$ F" or "acidulat$ fluor$" or "phosphat$ fluor$" or fluorphosphat$ or "amin$ fluor$" or "sodium$ fluor$" or "stannous$ fluor$" or SMFP or MFP or monofluor$).mp. 3. (varnish$ or lacquer$ or laquer$ or lacker$ or lakk$ or polyurethane$).mp. 4. 1 or 2 5. 3 and 4 6. "Fissure sealant"/ 7. (fiss$ adj6 seal$).mp. 8. (dental adj3 seal$).mp. 9. (compomer$ adj4 seal$).mp. 10. (composite$ adj4 seal$).mp. 11. "Glass ionomer"/ 12. Resin cements/ 13. ("glass ionomer$" or glassionomer$ or "cermet cement$" or "resin cement$").mp. 14. or/6‐13 15. 5 and 14
This subject search was linked to the Scottish Intercollegiate Guideline Network filter for identifying economic studies in Embase Ovid. Available at: www.sign.ac.uk/search-filters.html.
1 Socioeconomics/ 2 Cost benefit analysis/ 3 Cost effectiveness analysis/ 4 Cost of illness/ 5 Cost control/ 6 Economic aspect/ 7 Financial management/ 8 Health care cost/ 9 Health care financing/ 10 Health economics/ 11 Hospital cost/ 12 (fiscal or financial or finance or funding).tw. 13 Cost minimization analysis/ 14 (cost adj estimate$).mp. 15 (cost adj variable$).mp. 16 (unit adj cost$).mp. 17 Or/1‐16
Appendix 7. Search strategies for the other electronic databases searched in the previous versions of the review
OpenSIGLE (from 1980 to 2005)
((fluor*) AND (silane* OR polyurethane* OR lack* OR laquer* OR lacquer* OR varnish* OR verniz* OR vernis*))
SCISEARCH, CAplus, INSPEC, JICST‐EPLUS, NTIS, PASCAL searched via STN Easy (to November 2009)
fluor* AND ( varnish OR lacquer* OR laquer* OR lack* OR vernis* OR verniz* OR silane* OR polyurethane*) AND ( dental OR
tooth OR teeth OR enamel*)
DARE, HTA searched via the CAIRS web interface (to November 2009)
fluor* AND silane* or polyurethane* or varnish* or lacquer* or laquer* or verniz* or vernis* or lack* or laka* AND “fissure sealant*”
or ionomer* AND dental or tooth or teeth or enamel*
Data and analyses
Comparison 1. Resin fissure sealant versus fluoride varnish.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Dentinal caries at 2–3 years (yes/no) | 4 | Odds Ratio (IV, Random, 95% CI) | 0.67 [0.37, 1.19] | |
| 1.1.1 Split‐mouth studies with paired data | 1 | Odds Ratio (IV, Random, 95% CI) | 0.67 [0.48, 0.93] | |
| 1.1.2 Parallel‐group studies | 3 | Odds Ratio (IV, Random, 95% CI) | 0.66 [0.26, 1.73] | |
| 1.2 Dentinal caries at 4 years (yes/no) | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.42 [0.21, 0.84] | |
| 1.3 Dentinal caries at 9 years (yes/no) | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.48 [0.29, 0.79] | |
| 1.4 Increment in decayed, missing and filled permanent teeth at 2 years | 1 | 542 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.14, ‐0.02] |
| 1.5 Increment in decayed, missing and filled permanent surfaces at 2 years | 1 | 542 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.15, ‐0.03] |
1.5. Analysis.

Comparison 1: Resin fissure sealant versus fluoride varnish, Outcome 5: Increment in decayed, missing and filled permanent surfaces at 2 years
Comparison 2. Resin‐modified glass ionomer fissure sealant versus fluoride varnish.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Dentinal caries at 12 months (yes/no) | 1 | 21 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 4.27] |
Comparison 3. Resin fissure sealant plus fluoride varnish versus fluoride varnish.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Dentinal caries at 24 months (yes/no) | 1 | Odds Ratio (IV, Fixed, 95% CI) | 0.30 [0.17, 0.55] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bravo 2005.
| Study characteristics | ||
| Methods |
Trial design: cluster‐randomised trial. 15 school classes randomly assigned to 3 treatment arms. School classes conducted at 5 primary schools, which were selected at random from a group of 21 schools. Mean number of studied teeth per child was 3.5 (a child was an additional cluster) Follow‐up period: 9 years: 4‐year caries preventive programme, plus 5 years after active programme Started: 1990 |
|
| Participants |
Location: Spain, in a non‐fluoridated city (0.07 ppm fluoride ion in tap water) Inclusion criteria: children with sound permanent first molars. Children were from middle or lower‐middle socioeconomic status families Age at baseline: 6–8 years (mean 7 years) Sex: girls: 68% in FS group, 47% in FV group Baseline caries: FS group: mean dft 2.24 (SD 2.59); FV group: 2.42 (SD 3.26) Number randomly assigned: 362 (112 in FS group; 115 in FV group; 135 in control group) Number evaluated: 75 (37 in FS group; 38 in FV group; 45 in control group). Only children who had ≥ 1 completely erupted and sound permanent molar at any period during the active programme, and were examined at 4‐year follow‐up were included in the analysis at 9 years. |
|
| Interventions |
Comparison: resin‐based FS vs FV Group 1: visible‐light‐polymerised opaque Delton FS applied to completely erupted occlusal surfaces of permanent first molars by 1 dentist plus an assistant, who used portable equipment. After 6, 12, 18, 24 and 36 months, FS was applied to molars that had not previously erupted and was replaced if partial or total loss had occurred since the previous examination Group 2: FV (Duraphat, sodium fluoride) Varnish applied to partially or fully erupted occlusal surfaces of permanent first molars by 1 dentist plus an assistant, who used portable equipment. After 6, 12, 18, 24, 30, 36 and 42 months, varnish was applied to newly erupted molars and was reapplied to all those that were still sound. Group 3: control group without treatment (Only FS (group 1) and FV (group 2) were used in this review) Co‐interventions: none reported |
|
| Outcomes |
Primary outcome Dental caries: sound or carious occlusal surface of molar Assessed by a dentist. Examinations were made with an exploration probe and a flat mirror Secondary outcomes Number of visits to the dentist for repair of FS or FV application Adverse events |
|
| Notes |
Inter‐rater agreement: Kappa coefficients for intra‐examiner and inter‐examiner reliability > 0.68 for all measurements Sealant retention: complete sealant retention 63% at 4‐year follow‐up and 39% at 9‐year follow‐up Funding source: Spain Ministry of Education and Science. Study authors were from the university |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote from author correspondence: "Each school‐class was numbered. By using a list of random numbers from a statistical book each school‐class was assigned to the 3 groups. When 1 group was full of children (i.e. the sum of the children in the assigned school‐classes was above the sample size needed for a group), then that group was excluded for new random assignations. The school classes allocation was not completely random, since it had some restrictions: for example, the total number of children should be at last more or less equilibrated between the three groups (thus, after the first random assignment, the following were conditional)." Comment: randomisation procedure was not completely random. |
| Allocation concealment (selection bias) | High risk | Comment: the non‐random method used for sequence generation would likely not allow for allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | Assessor was not informed of intervention, but presence or absence of the sealant would reveal the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Missing data: 18% for all 3 groups combined at 4 years (dropout rates by group not detailed). Comment: the information on dropouts was not provided by group at 4 years of follow‐up. At 9 years of follow‐up, we graded the study as having high risk of attrition bias because the proportion of participants assessed and included in the analysis was 33% (only children who had ≥ 1 completely erupted and sound permanent molar at any time period during the active programme, and were examined at 4‐year follow‐up, were included in the analysis at 9 years). No information about dropout/missing data from 2‐ to 3‐year timepoint. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response and sealant retention. Comment: prespecified outcomes (in methods) were reported in the prespecified way. |
| Other bias | Low risk |
Comparability of groups: Comment: detailed description of demographic characteristics and caries risk level at baseline was given for groups available at 4 and 9 years, and groups were assessed as comparable. Baseline mean dmft in FS group was 2.24 (SD 2.59) and in FV group 2.42 (SD 3.26). Mean age in FS group was 7.3 years, and in FV group 7.6 years. Proportion of girls was 68% in FS group and 47% in FV group. Although proportion of girls was bigger in FS group than in FV group, groups were in balance at baseline. Co‐interventions: Quote: "The children received no toothbrushing, fluoride rinse, or fluoride tablet programs." Comment: no co‐interventions were included in the protocol. |
Chestnutt 2017.
| Study characteristics | ||
| Methods |
Trial design: 2‐arm parallel‐group RCT Follow‐up period: 36 months: resin‐based FS was applied to caries‐free FPMs and maintained at 6‐month intervals. FV was applied at baseline and at 6‐month intervals for 3 years. Started: 2011: participants recruited in 2 cohorts between October and January in the 2011–2012 and 2012–2013 school years Assessment: at baseline and 36 months |
|
| Participants |
Location: UK, children attending 66 primary schools in Communities First areas Inclusion criteria: children aged 6 or 7 years, attended the schools participating in the Cardiff and Vale University Health Board Designed to Smile programme, written informed consent of the person with parental responsibility, and had ≥ 1 fully erupted FPM free of caries into dentine Exclusion criteria: medical history precluded inclusion; any abnormality of the lips, face or soft tissues of the mouth that would cause discomfort in the provision of fluoride seal/varnish; current participation in another clinical trial involving an investigational medicinal product, obvious signs of systemic illness Age: 6–7 years Sex: 472 boys, 543 girls (FS: 237:277; FV 235:266) Baseline caries: dentine caries in first molar D4-6MFT = FV; 31 (6.2%), FS; 27 (5.3%) Number randomly assigned: 1015 (1 participant from FV group did not permit use of data) (FS 514; FV 502) Number evaluated: 835 (FS 418; FV 417) Pretreatment: group 1 pit and fissure FS, Group 2 FV |
|
| Interventions |
Comparison: resin‐based FS vs FV Group 1: sealant used was the Delton Light Curing Opaque Pit FS (CE0086; Dentsply Ltd). FS was reapplied if the existing sealant had become detached or if occlusal coverage was considered insufficient, either due to further eruption of the tooth or due to part of the sealant becoming loose. Group 2: varnish used was Duraphat 50 mg/mL dental suspension (PL 00049/0042; Colgate‐Palmolive Ltd), equivalent to 22,600 ppm fluoride. Dosage per single application did not exceed 0.4 mL Re‐application: study protocol dictated that reapplication should occur within a 4‐week interval on either side of the 6‐month anniversary of the previous application Co‐interventions: none reported |
|
| Outcomes |
Primary outcome: development of dental caries on FPMs at 36 months Outcome type: dichotomous Reporting: fully reported Unit of measure: present or absent Direction: lower is better Data value: endpoint |
|
| Notes |
Inter‐rater agreement: based on Landis and Koch (Landis 1977), examiners showed substantial agreement (0.69–0.8) or excellent agreement (0.81–1) throughout the study. Calibration was at the d/D0–3:d/D4–6 level. Sealant retention: at the 30‐month treatment visit, only a small proportion of previously sealed teeth were reported as being 'lost', with 74% of upper teeth and 88–91% of lower teeth reported as 'partial', i.e. sealant did not cover the whole of the occlusal surface. Funding source: National Institute for Health Research UK (NIHR) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was carried out in the South East Wales Trials Unit (SEWTU) using lists of pupil sex and caries chart data collected by the CDS [community dental service] from each school they visited for the screening examination. Eligible children were randomised using the minimisation algorithm. Allocation lists were produced and provided to the CDS, with a 2‐week window before the CDS returned to the school for the baseline treatments." |
| Allocation concealment (selection bias) | Low risk | Quote: "...All randomisation and allocation lists were produced by SEWTU independently of the recruiting and examining personnel in the CDS." Quote: "allocation‐blinded." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | Assessor was not informed of the intervention, but the presence or absence of the sealant would have revealed the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate was insignificant. In both trial arms, the number of children completing was in excess of the numbers required to satisfy the power calculation (page 110 of the full report). |
| Selective reporting (reporting bias) | Low risk | All intended outcomes were reported. |
| Other bias | Low risk | Trial was conducted according to the protocol, with the exception of some minor changes to improve the return rate of follow‐up questionnaires. Comparability of groups: dentine caries in first molar D4-6MFT = FV; 31 (6.2 % ), FS; 27 (5.3%). Comment: detailed descriptions of participants characteristics including baseline caries and cariology scores were reported and there were no differences between groups. Co‐interventions: none reported. Comment: however, the article mentioned that parents reported an improvement in children's diet and toothbrushing routine during the trial. |
Florio 2001.
| Study characteristics | ||
| Methods |
Trial design: parallel group, where individuals were randomly assigned to 3 treatment arms Follow‐up: 12 months Started: 1998 |
|
| Participants |
Location: 4 public day nursery schools (families at low economic level), Brazil Inclusion criteria: children with FPMs with restricted enamel decay on occlusal surfaces Age at baseline: 6 years Sex: not reported Baseline caries: FS group: mean dmfs 3.8 (SD 2.5); FV group: 4.5 (SD 2.7) Number randomly assigned: 34 (FS group 12, FV group 11, control group 11 (with total 108 teeth; mean number of teeth 3.2 per child) Number evaluated: 31 (10 in FS group; 11 in FV group; 10 in control group) |
|
| Interventions |
Comparison: resin‐modified glass ionomer FS vs FV 3 treatment arms Group 1: FS group (resin‐modified glass ionomer Vitremer), applied on occlusal surfaces of FPMs with restricted enamel decay. No resealing Group 2: FV group (Duraphat, sodium fluoride), applied every 6 months on occlusal surfaces of FPMs with restricted enamel decay Group 3: control group (Only FS (group 1) and FV (group 2) were used in this review) Co‐interventions: fluorinated tap water. Children received professional prophylaxis during dental examination visits |
|
| Outcomes |
Primary outcome Arrestment of enamel caries lesion or progression into dentine was noted at 12 months of follow‐up. To evaluate the caries progression rate, used digital radiograph + endoscopic examination. Examinations were carried out by the same dentist who administered the interventions |
|
| Notes |
Inter‐rater agreement: not applicable Sealant retention: complete sealant retention was 66% at 12 months Funding source: FAPESP/Brazil (São Paulo Research Foundation is an independent public foundation) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers was used. Comment: information was obtained from study authors. |
| Allocation concealment (selection bias) | Unclear risk | No information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants can be seen. |
| Blinding of outcome assessor (detection bias) | High risk | No blinding of outcome assessor was performed. Comment: additional information was obtained from study authors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing data: 2/12 (17%) children in FS group and 0/11 (0%) children in FV group Reasons for dropouts no given. Comment: imbalanced groups |
| Selective reporting (reporting bias) | Low risk | Outcome reported: arrestment of enamel caries lesion or progression into dentine at 12 months of follow‐up. Comment: prespecified caries outcome (in methods) was reported in the prespecified way. |
| Other bias | High risk |
Comparability of groups: baseline mean dmfs was 3.8 (SD 2.5) in FS group and 4.5 (SD 2.7) in FV group Comment: imbalanced groups. Co‐interventions: co‐interventions in FS and FV groups: water supply fluorination; professional prophylaxis during follow‐up consultations; children individually informed about concepts of oral health. Additional information was obtained from study authors. Comment: similar co‐interventions in both groups. |
Ji 2007.
| Study characteristics | ||
| Methods |
Trial design: parallel group, where children were randomly assigned to 3 treatment arms Follow‐up: 36 months |
|
| Participants |
Location: community dental clinic, and children selected from 13 primary schools in Yangpu district of Shanghai, China Inclusion criteria: children with sound permanent first molars (caries status determined by WHO criteria) Age at baseline: 6–8 years Sex: not reported Baseline caries: not reported but 21% of control teeth without treatment were decayed after 3 years Number randomly assigned: 622 children (1016 molars, on average 1.6 teeth per child) in 3 groups: 205 children in FS group, 207 in FV group, 210 in control group Number evaluated: at 24 months: 641 teeth (321 teeth in FS group; 320 teeth in FV group); at 36 months: 631 teeth (311 teeth in FS group; 320 teeth in FV group) (no information on dropout rates) |
|
| Interventions |
Comparison: glass ionomer FS vs FV 3 treatment arms Group 1: FS (Fuji II glass ionomer cement), applied by dentist with help of assistant. No resealing Group 2: silane FV (Fluor Protector 0.1% fluoride), applied by dentist with help of assistant, applied every 6 months for 3 years Group 3: control (Only FS (group 1) and FV (group 2) were considered in this review) Co‐interventions: none reported |
|
| Outcomes |
Primary outcome Dental caries – sound or carious occlusal surface of molar No information was given on outcome measurement procedure. |
|
| Notes |
Inter‐rater agreement: not considered Sealant retention: after 24 months: retained 65%, partial retained 22%, total loss 13% after 36 months: retained 61%, partial retained 25%, total loss 14% Funding source: no information |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "622 participants were selected from 13 primary schools, and were randomly divided into 3 groups." Comment: no information on randomisation procedure provided. |
| Allocation concealment (selection bias) | Unclear risk | No information was provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | No information was provided; however, the presence or absence of the sealant would have revealed the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data by teeth: at 24 months, 6/327 (1.8%) in FS group and 15/335 (4.5%) in FV group; and at 36 months 16/327 (4.9%) in FS group and 15/335 (4.5%) in FV group. Comment: although no information on dropout rates of participants was provided, we graded this domain at low risk of bias because the dropout rate of teeth was < 5% |
| Selective reporting (reporting bias) | Low risk | Comment: outcomes, caries status and sealant retention reported in prespecified way. |
| Other bias | Unclear risk |
Comparability of groups: Comment: no information was provided on demographic characteristics and on caries risk level at baseline. Co‐interventions: Comment: no information was provided on co‐interventions, such as frequency and methods of toothbrushing, or application of fluoride toothpaste. |
Kalnina 2016.
| Study characteristics | ||
| Methods |
Trial design: 4‐arm parallel‐group RCT Follow‐up period: 12 months Sample size: power estimation done to have a power > 80% |
|
| Participants |
Location: Latvia Inclusion criteria: children aged 10 years with ≥ 1 healthy and fully erupted premolar Exclusion criteria: not mentioned Age at baseline: 10 years Sex: 56 boys, 51 girls Baseline caries: none Number randomly assigned: 122 children, 540 premolars Number evaluated: 107 children with 457 premolars Group 1 control: 50 children/173 premolars Group 2 FV: 21 children/103 premolars Group 3 FS: 17 children/78 premolars Group 4 ozone: 19 children/103 premolars Recall: evaluated for occlusal caries at baseline, 6 and 12 months. Dental status for all teeth and OHI‐S were recorded after 6 and 12 months. Unit of analysis: each tooth was considered as the unit of the analysis. Data were analysed using t‐test and the Chi2 test. |
|
| Interventions |
Comparison: resin‐based FS vs FV Group 1: control Group 2: FV
Group 3: FS
Group 4: ozone (Only FV (group 2) and FS (group 3) were used in this review.) |
|
| Outcomes |
Primary outcome New caries reported at 12 months |
|
| Notes |
Inter‐rater agreement: not considered Sealant retention: not reported; however, at 12 months, 0 caries was developed in FS group Funding source: Riga Stradin (Lativa) University, Institute of Stomatology and Oral Health |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of randomisation unclear. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no mention of allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | Comment: not possible to blind the assessor as sealant and varnish could be detected (provided the sealant had not failed). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 15 participants dropped out (5 sealant and 1 varnish). |
| Selective reporting (reporting bias) | Low risk | Comment: intended outcomes were fully reported (apart from dropouts). |
| Other bias | Unclear risk |
Comparability of groups: Comment: comparable in terms of age, sex and baseline caries. No significant differences in caries risk factors (child's toothbrushing habits, snacking habits, family‐related factors) Co‐interventions: Comment: not mentioned |
Liu 2012.
| Study characteristics | ||
| Methods |
Trial design: parallel‐group, 4 treatment arms (sealant, sodium fluoride varnish, silver diamine fluoride solution, placebo) Follow‐up: 24 months Study started in 2008 |
|
| Participants |
Location: children were chosen from primary schools, China Inclusion criteria: ≥ 1 sound permanent first molar with deep fissures or fissures with signs of early (enamel) caries viewed as wet, with opacities and discolouration, similar to ICDAS code 2 (proportion of early caries 35% of tooth sites) (clinical examinations included DIAGNOdent readings and were done by a dentist) Age at baseline: mean 9.1 years (range 8–10 years) Sex: 248 boys, 253 girls Baseline caries: baseline mean dmft scores: FS 3.19 (SD 2.68), FV 3.58 (SD 2.25) (information obtained from study author) Number randomly assigned: 501 children (1539 molars, on average 3 teeth per child) in 4 groups: 124 children in FS, 124 in FV, 125 in silver diamine fluoride solution, 128 in placebo Number evaluated: 482 at 2‐year follow‐up (121 children in FS, 116 in FV, 121 in silver diamine fluoride solution, 124 in placebo) |
|
| Interventions |
Comparison: resin‐based FS vs FV 4 treatment arms Group 1: light‐cured, fluoride‐releasing resin‐based sealant Clinpro Sealant (3M ESPE, St Paul, MN, USA) (applied by a dentist). No resealing Group 2: semi‐annual application of 5% sodium fluoride varnish (Duraphat) (applied by a dentist) Group 3: annual application of 38% silver diamine fluoride solution (applied by a dentist) Group 4: placebo control – annual application of water (applied by a dentist) (Only FS (group 1) and FV (group 2) were considered in this review) Co‐interventions: 90% of toothpastes on sale contained fluoride (no systemic fluoridation in the study area) |
|
| Outcomes |
Primary outcome Dental caries – sound or carious occlusal surface of molar (caries in dentine ICDAS codes 4–6). Each molar was assessed at 2 sites (upper molar – mesial pit/fossa and distal‐palatal groove; lower molar – occlusal fissure and buccal pit/groove). Caries incidence was reported as child level, tooth level and fissure site level Outcomes assessed by the same blinded examiner using disposable mouth‐mirrors attached to an intra‐oral LED light and CPI probes Secondary outcome Adverse events |
|
| Notes |
Intra‐examiner reliability: Kappa statistic > 0.9 Sealant retention: 46% Funding source: Hong Kong Research Grants Council (study authors were from the university) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An assistant, using computer‐generated random numbers, allocated the children individually among four groups." Comment: adequate random sequence generation provided. |
| Allocation concealment (selection bias) | Low risk | Additional information obtained from study author as computer‐generated random number table (consisting only of numbers 1, 2, 3 and 4) was printed out and kept by a research assistant. Group allocation of participants, i.e. group 1 to group 4, followed random numbers in the random number table. Treatment was performed immediately on‐site by a dentist not involved in examination of children according to group allocation while research assistant was present. Comment: adequate allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | Comment: presence or absence of the sealant would reveal the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data: 3/124 (2.4%) in FS group, 7/124 (5.6%) in FV group. Comment: marginal dropout rates. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response, sealant retention. Comment: prespecified outcomes (in methods) were reported in prespecified way. |
| Other bias | Low risk |
Comparability of groups: Quote: "Proportionately more children in the sealant group than in other groups had visited a dentist or consumed snacks once a day or less (P < 0.05)". (13% of children in sealant group and 31% in FV group consumed snacks twice or more often a day)." Additional information obtained from study author revealed no statistically significant differences between groups in baseline caries risk of children. Mean baseline dmft scores: FS 3.19 (SD 2.68); FV 3.58 (SD 2.25). Comment: although we noted differences in dental visit history and consumption of snacks between groups at baseline, baseline caries risk scores of children were similar. Co‐interventions: Quote: "No systemic fluoridation in the study area. 90% of the toothpastes on sale contained fluoride." Comment: no co‐interventions other than fluoridated toothpaste were included in the protocol. |
Raadal 1984.
| Study characteristics | ||
| Methods |
Trial design: split‐mouth, sealant tooth randomly assigned Follow‐up: mean 23 months |
|
| Participants |
Location: study setting was a public dental clinic in a small town in Norway Inclusion criteria: children had to have 1 recently erupted homomaxillary pair of permanent first molars. Occlusal surface was sound or had initial caries in enamel Age at baseline: 6–9 years Sex: 62 girls, 59 boys Baseline caries: mean dmft 4.7 (SD 3.3) Number randomly assigned: 121 children with 210 tooth site pairs (110 in maxilla and 100 in mandible; in maxilla, mesial and distal portions of occlusal surface were treated separately) Number evaluated: no description of dropouts regarding children provided, but information provided indicated that 208/210 sealed sites were evaluated (meaning that 1 child or 2 children had dropped out) |
|
| Interventions |
Comparison: resin‐based FS vs FV Tooth pair: occlusal surface of 1 tooth sealed with autopolymerised resin‐based Concise; on occlusal surface of the other tooth of the tooth pair, FV (Duraphat, sodium fluoride) was applied No information was provided on proportions of sound surfaces and teeth with enamel lesions. Surfaces with initial caries in enamel were opened mechanically and caries removed before sealant application (quote from the article: "In those cases where caries had progressed to the dentin, conventional cavities for amalgam fillings were prepared, and these cases were excluded from the study") No resealing Surfaces to be painted with FV were treated every 6 months Co‐interventions: annual information and motivation about dental care; fluoride tablets recommended; fluoride rinsing with 0.5% sodium fluoride solution at school |
|
| Outcomes |
Primary outcome Dental caries – sound or carious occlusal surface of molar Caries status was recorded using visual‐tactile method and bitewings |
|
| Notes |
Inter‐rater agreement: not considered Complete sealant retention: 63% at 23 months Funding source: no information |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin tossing. Additional information was obtained from study author. Comment: random sequence generation was adequate. |
| Allocation concealment (selection bias) | Low risk | Comment: random sequence was adequately concealed up until the moment of allocation by flipping a coin to allocate a particular tooth, within a tooth pair, to be sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding not possible as sealants could be seen; however, we judged it to be unlikely to be a significant source of bias in a study with a split‐mouth design. |
| Blinding of outcome assessor (detection bias) | High risk | No blinding of the outcome assessor performed. Comment: additional information obtained from study author. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropout rate 1% for tooth site pairs after 23 months (no description of dropouts was provided regarding children, but information indicated that 208/210 sealed sites were evaluated, meaning that 1 child or 2 children dropped out). No reasons for dropouts described. Comment: marginal dropout rate. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: incidence of dentinal carious lesion on treated occlusal surfaces of molars (yes or no) at 23 months of follow‐up, retention. Comment: prespecified caries outcomes (in methods) were reported in the prespecified way. |
| Other bias | Low risk |
Comparability of groups: Comment: split‐mouth design, which included sound surfaces or surfaces with enamel lesions. With split‐mouth designs, we considered that both surfaces within a tooth pair in any case will eventually be at equal risk for caries because of the long follow‐up (regardless of whether the diagnosis consisted of a sound surface or a surface with an enamel lesion). Co‐interventions: Annual information and motivation about dental care; fluoride tablets recommended; fluoride rinsing with 0.5% sodium fluoride solution at school. Comment: split‐mouth design. Conditions are the same for both teeth within a tooth pair. |
Salem 2014.
| Study characteristics | ||
| Methods |
Trial design: cluster‐randomised, 12 primary schools; 2 classes from each grade were randomly assigned to 2 treatment arms Follow‐up: 24 months Started: 2009 The study was not considered in analyses of this review because results and data – complex multi‐level model with teeth nested in a child nested in a school class nested in a school – were not in useable form (unit of analysis was chosen to be a tooth surface, but clustering of data was not taken into account in the analyses. Study author gave the following additional information on analyses of the trial: "During study period we found that the arrangement of pupils in each class is undergoing substantial changes every year. Hence there was a combination of both groups in each class at the second year and we decided to analyse the study population at surface level.") |
|
| Participants |
Location: university clinic, Iran Inclusion criteria: children had to have ≥ 1 sound (by Nyvad criteria) and newly and completely erupted FPM with deep occlusal fissure Age at baseline: 6–7 years Sex: girls 38%, boys 62% Baseline caries: FS group: mean dmft index 4.41 (SD 0.92); FV group: 4.76 (SD 2.75) (additional information was obtained from study authors) Number randomly assigned: 400 children (FS 200, FV 200) with 1579 occlusal surfaces (mean number of teeth 3.9 per child) Number evaluated: 352 at 2 years (173 in FS group, 179 in FV group) |
|
| Interventions |
Comparison: resin‐based FS vs FV 2 treatment arms Group 1: resin‐based FS (Eco Seal), applied by dentist without assistant (additional information obtained from study authors). Partially and completely lost sealants were repaired/reapplied once if needed after 6 months Group 2: sodium FV (Durafluor, 5%), applied biannually by dentist without assistant (additional information obtained from study authors) Co‐interventions: all children participated in oral hygiene education sessions including restriction of sugary snacks, regular toothbrushing and toothbrush and 1450 ppm fluoride toothpaste given at every visit Fluoride concentration of water during the years 2009–2012 at study area was in the range of 0.45–0.8 ppm, on the basis of seasonal changes |
|
| Outcomes |
Primary outcome Dental caries – sound or carious occlusal surface of first molar: caries numbers for occlusal surfaces scored by Nyvad criteria. DMFT and DMFS scores reported for whole tooth surfaces 1 calibrated dentist carried out all examinations. Caries status was determined by 2 visual‐tactile measures: WHO criteria (DMF) and Nyvad criteria applied |
|
| Notes |
Intra‐examiner reliability: Kappa co‐efficient for Nyvad was 0.79 and WHO criteria was 0.81. Sealant retention: after 24 months: completely retained 43%, partial retention 46%, total loss 11% Funding source: granted by Institutional Review Board and Ethical Committee of Guilan University of Medical Sciences, Iran. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In each school, one class from each grade was assigned to sealant and the other to varnish by coin tossing." Comment: random sequence generation was adequate. |
| Allocation concealment (selection bias) | Low risk | Quote from author correspondence: "The records were kept by dental nurses at dental clinic files. The nurses were the staff of university dental clinic and did not know the children or their dental history." Comment: independent staff combined with cluster‐randomised study design gave the impression of adequate randomisation procedure. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | Quote from author correspondence: "The examiner was not involved in the study design and had no access to records." Comment: the presence or absence of the sealant would have revealed the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data: 27/200 (13.5%) in FS group, and 21/200 (10.5%) in FV group. Reason for dropouts in both groups: children moved away from the area. Comment: missing data were < 25%, and groups were balanced in numbers and reasons for missing data. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response, sealant retention. Comment: prespecified outcomes (in methods) were reported in prespecified way. |
| Other bias | Low risk |
Comparability of groups: Information on groups was available at 2 years (additional information was obtained from study authors): baseline mean dmft in FS group was 4.41 (SD 0.92) and in FV group 4.76 (SD 2.75). Proportion of girls was 46% in FS group and 31% in FV group. Quote: "The majority of children reported brushing their teeth once daily and sugary snacks 1–2 times per day without significant difference between the groups." Comment: detailed description of demographic characteristics and caries risk level was provided at baseline. Although the proportion of girls was greater in FS group than in FV group, we assessed that groups were balanced at baseline. Co‐interventions: all children participated in oral hygiene education sessions including restriction of sugary snacks and regular tooth brushing, and received toothbrush and 1450 ppm fluoride toothpaste at every visit. Comment: in both groups, the same co‐interventions were allowed. |
Splieth 2001.
| Study characteristics | ||
| Methods |
Trial design: split‐mouth, sealant tooth randomly assigned Follow‐up: 2 years Started: 1995 |
|
| Participants |
Location: a private dental practice, Germany Inclusion criteria: children had to have ≥ 1 pair of equivalent FPMs without carious defects (occlusal surface sound or with initial lesion in enamel) Age at baseline: 5–8 years Sex: no information about boy to girl ratio Baseline caries: mean DMFS 0.2 Number randomly assigned: 98 children with 181 tooth pairs (on average 1.8 tooth pairs per child) Number evaluated: 92 at 2‐year follow‐up |
|
| Interventions |
Comparison:resin‐based FS plus FV vs FV alone Tooth pair: occlusal surface of 1 tooth sealed with visible‐light activated Fissurit Transparent (VOCO GmbH, Cuxhaven, Germany); occlusal surface of the other tooth of the tooth pair applied with FV (Duraphat, sodium fluoride) FV was applied to all teeth including the sealed tooth Children were examined semi‐annually for 2 years – sealants were resealed if necessary and FV was applied to all teeth at examinations Co‐interventions: children were instructed about better oral hygiene and brushed their teeth under supervision (mean frequency of cariogenic food intake per day was 15, including a large number of sweetened drinks. Oral hygiene was moderate). 5% of the children used fluoride tablets during the study. (Fluoride concentration of public water supply was 0.1 ppm.) |
|
| Outcomes |
Primary outcome Status of sound/caries in enamel/caries in dentine on occlusal surfaces Changes in DMF scores on whole‐mouth level Caries status was recorded by 1 experienced dentist according to WHO criteria, but without applying pressure to the explorer. Secondary outcome Mean treatment time for sealing and varnish application |
|
| Notes |
Inter‐rater agreement: not considered Complete sealant retention: 81% at 24 months Funding source: no information |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin tossing. Additional information was obtained from study authors. Comment: random sequence generation was adequate. |
| Allocation concealment (selection bias) | Low risk | Comment: random sequence was adequately concealed up until the moment of allocation by flipping a coin to allocate a particular tooth, within a tooth pair, to be sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding not possible as sealants could be seen; however, we judged it to be unlikely to be a significant source of bias in a study with a split‐mouth design. |
| Blinding of outcome assessor (detection bias) | High risk | No blinding of outcome assessor was performed. Comment: additional information was obtained from study author. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data: 6/98 (6%) after 2 years. No description of reasons for dropouts. Comment: missing data rate < 25%. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: status of sound/caries in enamel/caries in dentine on occlusal surfaces; changes in DMF scores on whole‐mouth level; treatment time; sealant retention; costs. Comment: prespecified outcomes (in methods) were reported in the prespecified way. |
| Other bias | Low risk |
Comparability of groups: Comment: split‐mouth design, which included sound surfaces or surfaces with initial lesions in enamel. With split‐mouth designs, we considered that both surfaces within a tooth pair would eventually be at equal risk for caries because of the long follow‐up (regardless of whether the diagnosis was sound surface or surface with enamel lesion). Co‐interventions: The fluoride concentration of the public water supply was 0.1 ppm. 5% of children used fluoride tablets during the study. Mean frequency of cariogenic food intake per day was 15, including a large number of sweetened drinks. Oral hygiene was moderate. Comment: split‐mouth design. Conditions were the same for both teeth within a tooth pair. |
Tagliaferro 2011.
| Study characteristics | ||
| Methods |
Trial design: parallel‐group study, 6 randomly assigned treatment arms Follow‐up: 24 months |
|
| Participants |
Location: children were from 2 public schools and lived in a low‐caries‐prevalence city, Brazil Inclusion criteria: children had to have: dmft ≥ 3 or ≥ 1 active cavitated lesion or dmft + DMFT = 0, or a combination of these, and ≥ 2 sound permanent first molars Age at baseline: mean age 7 years Sex: 52% girls, 48% boys Baseline caries: mean dmft index: 4.51 (SD 2.81) for HRS group and 4.28 (SD 2.54) for HRV group. In low‐caries‐risk groups (LRS, LRV groups), dmft + DMFT was 0 Number randomly assigned: 327 children with mean number of occlusal surfaces treated 3.47 (SD 0.80) Numbers of children per group: 57 in HRC group; 57 in HRV group; 55 in HRS group; 53 in LRC group; 52 in LRV group; 53 in LRS group Number evaluated: 268 at 24 months (44 children in HRC group; 48 in HRV group; 47 in HRS group; 42 in LRC group; 43 in LRV group; 44 in LRS group) |
|
| Interventions |
Comparison: resin‐modified glass ionomer FS vs FV 6 treatment arms Groups 1, 2 and 3 included only high‐caries‐risk children Group 1 (HRC): control group with high‐caries‐risk children receiving OHE Group 2 (HRV): OHE and FV application biannually Group 3 (HRS): OHE and single FS application (resin‐modified glass ionomer cement) Groups 4, 5 and 6 included only low‐caries‐risk children Group 4 (LRC): control group receiving OHE Group 5 (LRV): OHE and FV application biannually Group 6 (LRS): OHE and single FS application (resin‐modified glass ionomer cement) (Only FS and FV groups were considered in this review: groups 2, 3, 5 and 6) Sealants were applied by dentist assisted by dental hygienist in dental clinic (sealants were applied to healthy permanent first molars). Procedure consisted of 4 stages: etching tooth surfaces with 37% phosphoric acid, primer application, ionomer application and finishing gloss application No resealing FV (Duraphat, sodium fluoride) was applied by dentist assisted by dental hygienist, at schools in well‐lit areas, under natural light. Duraphat was applied to occlusal surfaces of sound FPMs. Participants were informed to not brush their teeth or chew food for ≥ 2 hours after treatment, and to consume only soft foods and liquids for 24 hours OHE was carried out by dentist assisted by dental hygienist. Sessions lasting 1 hour were held every 3 months, with talks covering themes such as dental caries, dental plaque and fluoride. Oral hygiene instructions, supervised tooth brushing and dietary counselling were presented to children by means of lectures, videos, educational games and oral quizzes Co‐interventions: 93% of children used fluoridated dentifrice. Mean fluoride concentration in tap water was 0.7 ppm |
|
| Outcomes |
Primary outcome Sound or carious occlusal surface of FPM: caries increment was stated as mean DMF scores 1 calibrated dentist carried out all examinations. Diagnosis was based on clinical examination, and no radiographs were taken at baseline or at final examinations Secondary outcome Adverse events |
|
| Notes |
Intra‐examiner reliability: Kappa coefficients 0.95 (caries as cavitated lesions) and 0.90 (caries as cavitated and non‐cavitated lesions) Sealant retention: total sealant loss 16% at 24 months Funding source: FAPESP (São Paulo Research Foundation is an independent public foundation) Caries prevalence of population at study area: mean DMFT 1.32 for 12‐year‐old children |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Additional information was obtained from study authors. Children were systematically allocated to each treatment group as follows: approximately 10 children were taken from each classroom at random by a dental hygienist. The hygienist did not know the caries risk of each child. The hygienist organised the 10 children in a queue at random. (In the queue were also those children not included in the study because they did not fulfil the inclusion criteria of the study; those children were excluded after baseline examination by a dentist.) The examiner (Pardi V) performed the examination of the first child in the queue, and the main researcher (Tagliaferro EP) recorded data on a specific form and classified the child as having high‐ or low‐caries risk, according to pre‐established criteria. After each examination day, record forms were organised according to caries risk (low or high) and sequence of examination. After this, for example, the first examined child of that day classified as having high risk of caries was systematically allocated to the control group, the second to the FV group and the third to the FS group, and successively. Each child was given an ID code to be used over the whole study period. Comment: we graded this domain as low risk of bias because we considered that the randomisation procedure as a whole was unsystematic when noting to which treatment group each child was finally allocated. |
| Allocation concealment (selection bias) | Low risk | Additional information was obtained from study authors. The main researcher (Tagliaferro) called children for treatments as follows: children allocated to FS groups were brought to a clinical setting, their names and treatment group were checked and Tagliaferro applied sealants, with the help of a dental hygienist. Then, at another time, Tagliaferro went to the school, called the children allocated to FV groups and performed varnish applications. The process of calling only children allocated to FS or FV groups, when sealant applications or varnish applications were performed, respectively, ensured that each child received the intended treatment. Comment: despite incomplete allocation concealment (the same main researcher kept the records and made the applications), the large number of children in each allotted group and the fact that implementation of each treatment was centralised gave the impression that concealment was real. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | The presence or absence of the sealant would have revealed the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data: 8/55 (14.5%) in HRS group, 9/57 (15.8%) in HRV group, 9/53 (17%) in LRS group, 9/52 (17.3%) in LRV group. Quote: "Many individuals had moved out of the schools where the research was conducted, and some refused to take part in the final examination." Comment: although no information was provided to explain reasons for dropouts by group, groups (HRS vs HRV; LRS vs LRV) were assessed as balanced with each other. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response. Comment: prespecified outcomes (in methods) were reported in the prespecified way. |
| Other bias | Low risk |
Comparability of groups: Quote: "At baseline, gender, age, use of fluoridated dentifrice, family income, father's and mother's education were not statistically different among the six groups." With regard to clinical variables (dmfs, dmft, DMFS, DMFT, number of occlusal surfaces being treated) at baseline, groups were reported to be balanced. Quote: "Baseline caries experience (dmft + DMFT) was not significantly different between full participants and those lost to follow‐up for HRC, HRV, and HRS groups (in the low caries risk groups, dmft + DMFT was zero)." Comment: detailed description was given on demographic characteristics (sex, age and social class), on baseline caries risk level and on baseline condition of tooth surfaces to be treated, to assess comparability of groups also at 24 months. Groups were assessed as balanced with each other Co‐interventions: All children participated in an oral education programme. 93% of children used fluoridated dentifrice. Comment: in all groups, the same co‐interventions were allowed. |
Tang 2014.
| Study characteristics | ||
| Methods | Trial design: single‐blind, parallel‐group RCT | |
| Participants |
Location: China Inclusion criteria: children aged 7–8 years living in Shanghai Jingán District of China for > 2.5 years, from 4 primary schools Age: 7–8 years Sex: 486 boys, 530 girls randomised Baseline caries: baseline mean DMFT index 0.08 (SD 0.37) Number randomised: 1016 pupils from 33 classes Number evaluated: 977 participants received final examination after 2 years. 39 dropouts attributed to moving away. |
|
| Interventions |
Group 1: FV (243 children) 0.1% Fluor Protector by Ivoclar Vivadent + OHE The tooth surface was cleaned and dried, smeared with FV for 30 seconds then dried it again with chip blower. Smearing of the FV was repeated twice. The children were instructed not to gargle, drink or eat for 45 minutes after the procedure. This procedure was repeated after 6 months, 4 times in total in 2 years. Group 2: fluoride foam (242 children) 0.6% (6000 µg/mL of fluorion) with pH 3.0 to 3.8 by Laikeli + OHE The tooth surface was cleaned using cotton ball. Fluoride foam was poured into a disposable dental tray and the children were asked to bite the tray firmly for 4 minutes, with their heads leaning forward and the saliva drooling into a plastic bag to avoid nausea, vomiting or swallowing the agent. The children were instructed not to gargle or eat for 30 minutes after applying fluoride foam. This procedure was repeated every 6 months for 2 years (4 times). Group 3: resin FS (321 children) Clinpro and LED dental curing lights by 3M + OHE The FS were applied according to a textbook "Oral Preventive Medicine" (4th edition, in Chinese). The procedure was done with the child sitting in a dental chair, tooth surfaces cleaned and acid etched, saliva suctioned and isolated, sealant coated on the pits and fissures and light cured; attention was paid to avoid producing air bubbles when coating the sealant. The children were advised to not bite hard or eat sticky food for 24 hours. Group 4: control group (210 children) OHE only (Only FV (group 1) and FS (group 3) were used in this review) |
|
| Outcomes |
Primary outcomes Prevalence of caries in FPMs at baseline and after 2 years Clinical diagnosis by 2 dentists with mouth mirror and CPI probe under artificial light as per criteria recommended by the 5th edition of WHO Oral Health Survey: Basic Methods (WHO 2013) OHEs were conducted by 4 dentists at baseline and after 2 years, and the results recorded. Diagnosis agreement between dentists was measured by Kappa test (Kappa = 0.84). Caries increment (DMFT and DMFS) was recorded from baseline to 2 years. Factors that affect caries increment were explored. Secondary outcome Retention of sealants |
|
| Notes | It is likely the study was a government programme but the authors did not mention this. This study was not detected by Cochrane search as the spelling of varnish was not correct in the title. Translation was completed by Dr Liyuan Ma, checked and revised by Prof Zongdao Shi and Prof Chengge Hua, Department of Evidence‐based Stomatology, West China School and Hospital of Stomatology, Sichuan University, Chengdu, P.R. China on 31 July 2016 Inter‐rater agreement: not considered Sealant retention: complete retention 1067 teeth (90.12%) from 1184 teeth, partial retention 79 teeth and no retention 38 teeth Funding source: Shangahai Jiaotong University |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was applied to divide participants into 4 groups (from translation). |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible as sealants could be seen. |
| Blinding of outcome assessor (detection bias) | High risk | The presence or absence of the sealant would have revealed the intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were data at baseline and after 2‐year follow‐up. Follow‐up rates were 95.5% for group 1 (FV), 95.9% for group 2 (fluoride foam), 96.6% for group 3 (FS) and 96.7% for control group. |
| Selective reporting (reporting bias) | Low risk | Primary outcomes (sealants' retention and incidence of caries) and secondary outcome (factors effect on caries incidence) were reported. |
| Other bias | Low risk | Comparability of the groups: baseline data were comparable. |
CPI: Community Periodontal Index; dft: decayed, filled deciduous teeth; dmfs: decayed, missing and filled deciduous surfaces; dmft: decayed, missing and filled deciduous teeth; DMF: decayed, missing and filled; DMFS: decayed, missing and filled permanent surfaces; DMFT: decayed, missing and filled permanent teeth; FPM: first permanent molar; FS: fissure sealant; FV: fluoride varnish; HRC: high‐risk control; HRS: high‐risk sealant; HRV: high‐risk varnish; ICDAS: International Caries Detection and Assessment System; LED: light‐emitting diode; LRC: low‐risk control; LRS: low‐risk sealant; LRV: low‐risk varnish; OHE: oral health education; OHI‐S: Simplified Oral Hygiene Index; ppm: part per million; RCT: randomised controlled trial; SD: standard deviation; WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Atkins 2016 | Not an RCT. |
| Fischman 1977 | Not an RCT. Random allocation not stated. Not comparing sealant vs fluoride varnish. |
| Herndon 2015 | Not an RCT. |
| Himida 2017 | Wrong intervention. |
| Honkala 2015 | Wrong participant population – kindergartens. |
| Humphreys 2017 | Duplicate |
| Jaworska 1984 | Not an RCT. Random allocation not stated. Study design not clear. No contact details of study author provided for further information. |
| Li 2020 | Not an RCT. |
| Liu 2009 | Abstract; no full report was found. |
| Liu 2014 | Not an RCT. |
| Muller‐Bolla 2018 | Wrong intervention. |
| Neidell 2016 | Ineligible study design. |
| Petterson 1983 | Not an RCT. Commune study where children born in odd month received sealant and fluoride varnish applications on first permanent molars, and children born in even month were given only fluoride varnish applications. Clustered data (several teeth per child) but no information on number of children at baseline or at follow‐up (follow‐up times varied between children). Description of characteristics of children was missing. |
| Riethe 1977 | Not an RCT. Random allocation not stated. No contact details of study authors were given for further information. |
| Ruff 2018 | Wrong intervention. |
| Saifullina 1990 | Not an RCT. Random allocation not stated. No reply to letter requesting information on the issue of randomisation. |
| Templeton 2016 | Wrong study design. |
| Uma 2011 | Caries data remained unreliable despite additional information from study author. |
| Vermaire 2015 | Wrong study design. |
| Wolff 2016 | Wrong study design. |
RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12615000693527.
| Study name | Preventing tooth decay in children in a remote community in Australia |
| Methods | RCT |
| Participants | All children (approximately 600–650) attending the 2 primary and 1 secondary school campuses will be invited to participate in the intervention study. Age 4–17 years |
| Interventions | Fissure sealant, fluoride varnish and povidone iodine |
| Outcomes | Caries |
| Starting date | 10 August 2015 |
| Contact information | Prof Newell W Johnson Building G40, Room 9.16, Gold Coast Campus, Griffith University, Queensland 4222, Australia Telephone: +61 07 56789306 Email: n.johnson@griffith.edu.au |
| Notes | End date 10 October 2017, no publication found |
ACTRN12616001537448.
| Study name | Management of dental decay in young Aboriginal children |
| Methods | RCT |
| Participants | Children < 72 months of age with early childhood dental decay within an Aboriginal community |
| Interventions | Unclear |
| Outcomes | Caries |
| Starting date | 8 November 2016 |
| Contact information | Primary sponsor: government body; National Health and Medical Research Council Dental Health Services, Locked Bag 15, Bentley Delivery Centre 6983, Perth, Western Australia Contact person for information and recruitment: Dr Peter Arrow, address as above, +61 8 93130 600, parrow@ozemail.com.au |
| Notes |
CTRI201805013564.
| Study name | Effectiveness of glass ionomer sealant and fluoride varnish in preventing dental caries on newly erupted permanent molars: a randomized clinical trial |
| Methods | Interventional |
| Participants | Children aged 6–8 years with newly erupted non‐carious first permanent molars. Operculum covering 1/4th of the occlusal surface and presence of ≥ 1 interproximal lesions on other teeth |
| Interventions | Resin sealant vs fluoride varnish |
| Outcomes | Caries |
| Starting date | 2018 |
| Contact information | Manipal College of Dental Sciences, Mangalore, Karnataka |
| Notes |
CTRI201805013799.
| Study name | Evaluation of relative effectiveness of fissure sealants and fluoride varnish in prevention of occlusal caries in children a randomized control trial |
| Methods | Interventional trial |
| Participants | Deep retentive pit and fissures in permanent molar in children |
| Interventions | Resin sealant vs varnish |
| Outcomes | Caries |
| Starting date | 2018 |
| Contact information | Vishnu Dental College, Andhira Pradesh |
| Notes |
ISRCTN81071356.
| Study name | The effectiveness of fluoride varnish versus pit and fissure sealant for the prevention of caries in children of primary health care |
| Methods | Single‐blind multi‐centre RCT |
| Participants | Children 6 years old (on average) having ≥ 1 of the first permanent molars compatible with the application of materials, and free of clinically detectable caries (with exposed dentine) or fillings at the beginning of the study |
| Interventions | Resin pit and fissure sealant vs sodium fluoride varnish |
| Outcomes | Occlusal caries, sealant retention |
| Starting date | 1 May 2009 |
| Contact information | Dr Hector Rossi, Universidad de Chile, Facultad de Medicina, Santiago |
| Notes | 1 May 2011 study end date; no publication found |
NCT01438866.
| Study name | The effectiveness of sealants in prevention of occlusal caries on primary molars |
| Methods | RCT |
| Participants | 148 children aged 42–52 months |
| Interventions | Fissure sealants vs fluoride varnish |
| Outcomes | Caries |
| Starting date | October 2011 |
| Contact information | Sisko Honkala, Associate Professor, Kuwait University |
| Notes | End date March 2014. Data submitted pending quality control review |
NCT01829334.
| Study name | A comparative study on the cost‐effectiveness of four methods in preventing fissure caries in permanent teeth |
| Methods | RCT |
| Participants | 329 children aged 6–9 years |
| Interventions | Sealant vs varnish |
| Outcomes | Caries |
| Starting date | April 2013 |
| Contact information | LO, Edward Chin Man, Professor, The University of Hong Kong |
| Notes |
NCT03189797.
| Study name | Effect of tailored preventive program on caries incidence using international caries classification and management system (ICCMS): a randomized clinical trial |
| Methods | RCT |
| Participants | 40 |
| Interventions | Fissure sealant vs fluoride varnish |
| Outcomes | Incidence of dental caries |
| Starting date | 30 June 2017 |
| Contact information | Ahmed Refaat, Cairo University, 12345, Egypt |
| Notes |
NCT03315312.
| Study name | Occlusal caries management in first permanent molars in child dental care |
| Methods | RCT |
| Participants | 400 children aged 6–9 years |
| Interventions | Fissure sealant vs fluoride varnish |
| Outcomes | Caries |
| Starting date | 1 February 2017 |
| Contact information | Oral Health Centre of Expertise in Eastern Norway |
| Notes |
NCT03448107.
| Study name | Comparative effectiveness of treatments to prevent dental caries |
| Methods | Interventional RCT |
| Participants | Rural children in school‐based settings |
| Interventions | Silver diamine fluoride and fluoride varnish vs fluoride varnish and glass ionomer sealants |
| Outcomes | Caries |
| Starting date | 20 September 2017 |
| Contact information | Principal Investigator: Richard Niederman, DMD, New York University School of Medicine |
| Notes |
NCT03685058.
| Study name | Effect of light curable resin modified glass ionomer varnish on non‐cavitated proximal carious lesions' progression |
| Methods | RCT |
| Participants | 88 |
| Interventions | Light curable resin modified glass ionomer varnish vs standard‐of‐care preventive measures |
| Outcomes | Caries |
| Starting date | January 2018 |
| Contact information | Najlaa M Alamoudi, BDS, MSc, DSc Jihan A Khan, BDS, MSc |
| Notes |
NCT04163354.
| Study name | Glass ionomer sealant versus fluoride varnish on occlusal caries prevention |
| Methods | RCT |
| Participants | 348 children aged 3–5 years |
| Interventions | GI sealant vs fluoride varnish |
| Outcomes | Caries |
| Starting date | 14 November 2019 |
| Contact information | Principal investigator: Cynthia Kar Yung Yiu, FHKAM, FCDSHK, The University of Hong Kong |
| Notes | Completion date: 31 December 2022 |
SLCTR/2019/009.
| Study name | Comparison of the cost effectiveness of fluoride varnish versus pit sealants and fissures in reducing the incidence of caries in children – a randomized controlled clinical trial |
| Methods | RCT |
| Participants | 288 |
| Interventions | Fluoride varnish vs fissure sealant |
| Outcomes | Cost and caries |
| Starting date | 25 March 2019 |
| Contact information | Circuito Ex Hacienda La Concepcion S/N Carretera Tlaxiaca, Hidalgo. Mexico. C.P 421. piccolo@uaeh.edu.mx |
| Notes |
TCTR20180124001.
| Study name | Prevention of early childhood caries (ECC) through high risk approach |
| Methods | RCT |
| Participants | 120 |
| Interventions | Apply fluoride varnish every 6 months vs sealant on first and second primary molar teeth vs apply silver diamine fluoride every 6 months |
| Outcomes | Caries |
| Starting date | 2 September 2017 |
| Contact information | Palinee N/A, Detsomboonrat, palinee_kung@hotmail.com |
| Notes |
RCT: randomised controlled trial.
Differences between protocol and review
We added a cost effectiveness objective and an economic commentary. New Cochrane methods were applied for inclusion of 'Summary of findings' tables and GRADE assessment of the certainty. In the previous version, we had not downgraded for detection bias because it is inevitable with an intervention like sealants, which are visible; however, we considered this time that detection bias is a potential problem and should be factored into the assessment of the certainty of the evidence.
Contributions of authors
This update: Study selection: WK, PG, HW. Data extraction: WK, PG. Data analysis: WK, HW. Writing of the review: WK, HW, PG, DB.
Previous versions: Writing of the protocol: Anne Hiiri (AH), Anneli Ahovuo‐Saloranta (AAS), Anne Nordblad (AN), Marjukka Mäkelä (MM). Study selection: AAS, Helena Forss (HF) and AH. Data extraction: AAS, HF and AH. Data analysis: WK, HW. Writing of the review: AAS, HF, AH, AN, MM.
Sources of support
Internal sources
Finnish Office for Health Technology Assessment/Finohta, National Institute for Health and Welfare/THL, Finland
School of Dentistry, The University of Manchester, UK
External sources
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Evidence Synthesis Programme, the NIHR, the NHS or the Department of Health and Social Care.
-
Cochrane Oral Health Group Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships-alliances). Contributors in the last two years have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Swiss Society of Endodontology, Switzerland.
Declarations of interest
WK: none. PG: none. HW: none. I was Co‐ordinating Editor with Cochrane Oral Health until earlier this year. DB: none.
Edited (no change to conclusions)
References
References to studies included in this review
Bravo 2005 {published and unpublished data}
- Bravo M, Baca P, Llodra JC, Osorio E. A 24-month study comparing sealant and fluoride varnish in caries reduction on different permanent first molar surfaces. Journal of Public Health Dentistry 1997;57(3):184-6. [DOI] [PubMed] [Google Scholar]
- Bravo M, Garcia-Anllo I, Baca P, Llodra JC, Junco P. Effectiveness of fissure sealant and fluoride varnish on different tooth surfaces: a 48-month study [Estudio comparativo sobre la efectividad de sellador de fisuras y bariz de fluor en distintas superficies dentarias: Ensayo comunitario a 48 meses]. Archivos de Odontoestomatologia Preventiva y Comunitaria 1996;12:717-23. [Google Scholar]
- Bravo M, Garcia-Anllo I, Baca P, Llodra JC. A 48-month survival analysis comparing sealant (Delton) with fluoride varnish (Duraphat) in 6- to 8-year-old children. Community Dentistry and Oral Epidemiology 1997;25(3):247-50. [DOI] [PubMed] [Google Scholar]
- Bravo M, Llodra JC, Baca P, Osorio E. Effectiveness of visible light fissure sealant (Delton) versus fluoride varnish (Duraphat): 24-month clinical trial. Community Dentistry and Oral Epidemiology 1996;24(1):42-6. [DOI] [PubMed] [Google Scholar]
- Bravo M, Montero J, Bravo JJ, Baca P, Llodra JC. Sealant and fluoride varnish in caries: a randomized trial. Journal of Dental Research 2005;84(12):1138-43. [DOI] [PubMed] [Google Scholar]
Chestnutt 2017 {published data only}
- Chestnutt IG, Hutchings S, Playle R, Morgan-Trimmer S, Fitzsimmons D, Aawar N, et al. Seal or varnish? A randomised controlled trial to determine the relative cost and effectiveness of pit and fissure sealant and fluoride varnish in preventing dental decay. Health Technology Assessment 2017;21(21):1-256. [DOI: 10.3310/hta21210] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys I, Chestnutt I, Fitzsimmons D. Seal or varnish? Cost-effectiveness of fissure sealants versus fluoride varnish in preventing dental decay in children. Value in Health 2017;20(9):A867. [DOI: 10.1016/j.jval.2017.08.2530] [DOI] [Google Scholar]
Florio 2001 {published and unpublished data}
- Florio FM, Pereira AC, Meneghim Mde C, Ramacciato JC. Evaluation of non-invasive treatment applied to occlusal surfaces. ASDC Journal of Dentistry for Children 2001;68(5-6):326-31, 301. [PubMed] [Google Scholar]
Ji 2007 {published data only}
- Ji PH, Xu QL, Ba Y. Clinical evaluation of fluor protector and glass-ionomer cement used as pit and fissure sealant for preventing pit and fissure caries in children. Shanghai Kou Qiang Yi Xue 2007;16(4):374-6. [PubMed] [Google Scholar]
Kalnina 2016 {published data only}
- Kalnina J, Care R. Prevention of occlusal caries using a ozone, sealant and fluoride varnish in children. Stomatologija 2016;18(1):26-31. [PubMed] [Google Scholar]
Liu 2012 {published and unpublished data}
- Liu BY, Lo EC, Chu CH, Lin HC. Randomized trial on fluorides and sealants for fissure caries prevention. Journal of Dental Research 2012;91(8):753-8. [DOI] [PubMed] [Google Scholar]
Raadal 1984 {published and unpublished data}
- Raadal M, Laegreid O, Laegreid KV, Hveem H, Korsgaard EK, Wangen K. Fissure sealing of permanent first molars in children receiving a high standard of prophylactic care. Community Dentistry and Oral Epidemiology 1984;12(2):65-8. [DOI] [PubMed] [Google Scholar]
Salem 2014 {published and unpublished data}
- Salem K, Shahsavari F, Kazemnejad E, Poorhabibi Z. Pit and fissure sealant versus fluoride varnish in prevention of occlusal caries. Journal of Dentomaxillofacial Radiology, Pathology and Surgery 2014;2(4):37-47. [Google Scholar]
Splieth 2001 {published and unpublished data}
- Splieth C, Förster M, Meyer G. Additional caries protection by sealing permanent first molars compared to fluoride varnish applications in children with low caries prevalence: 2-year results. European Journal of Paediatric Dentistry 2001;2(3):133-8. [Google Scholar]
Tagliaferro 2011 {published and unpublished data}
- Tagliaferro EP, Pardi V, Ambrosano GM, Meneghim Mde C, da Silva SR, Pereira AC. Occlusal caries prevention in high and low risk schoolchildren. A clinical trial. American Journal of Dentistry 2011;24(2):109-14. [PubMed] [Google Scholar]
Tang 2014 {published data only}
- Tang LH, Shi L, Yuan S, Lv J, Lu H-X. Effectiveness of 3 different methods in prevention of dental caries in permanent teeth among children. Shanghai Journal of Stomatology 2014;23(6):736-9. [PubMed] [Google Scholar]
References to studies excluded from this review
Atkins 2016 {published data only}
- Atkins CY, Thomas TK, Lenaker D, Day GM, Hennessy TW, Meltzer MI. Cost-effectiveness of preventing dental caries and full mouth dental reconstructions among Alaska Native children in the Yukon-Kuskokwim delta region of Alaska. Journal of Public Health Dentistry 2016;76(3):228-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fischman 1977 {published data only}
- Fischman SL, English JA, Albino JE, Bissell GD, Greenberg JS, Juliano DB, et al. A comprehensive caries control program-design and evaluation of the clinical trial. Journal of Dental Research 1977;56 Spec No:C99-103. [DOI] [PubMed] [Google Scholar]
Herndon 2015 {published data only}
- Herndon JB, Tomar SL, Catalanotto FA, Rudner N, Huang IC, Aravamudhan K, et al. Measuring quality of dental care: caries prevention services for children. Journal of the American Dental Association 2015;146(8):581-91. [DOI] [PubMed] [Google Scholar]
Himida 2017 {published data only}
- Himida T, Promise U. School-based dental sealant programmes may be effective in caries prevention. Evidence-based Dentistry 2017;18(1):13-4. [DOI] [PubMed] [Google Scholar]
Honkala 2015 {published data only}
- Honkala S, ElSalhy M, Shyama M, Al-Mutawa SA, Boodai H, Honkala E. Sealant versus fluoride in primary molars of kindergarten children regularly receiving fluoride varnish: one-year randomized clinical trial follow-up. Caries Research 2015;49(4):458-66. [DOI] [PubMed] [Google Scholar]
Humphreys 2017 {published data only}
- Humphreys I, Chestnut I, Fitzsimmons D. Seal or varnish? Cost-effectiveness of fissure sealants versus fluoride varnish in preventing dental decay in children. Value in Health 2017;20(9):A867. [Google Scholar]
Jaworska 1984 {published data only}
- Jaworska D. Possibilities of preventing fissure caries of first molars in children 6 to 7 years of age. Annales Academiae Medicae Stetinensis 1984;30:281-93. [PubMed] [Google Scholar]
Li 2020 {published data only}
- Li F, Jiang P, Yu F, Li C, Wu S, Zou J, et al. Comparison between fissure sealant and fluoride varnish on caries prevention for first permanent molars: a systematic review and meta-analysis. Scientific Reports 2020;10(1):2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2009 {published data only}
- Liu BY, Lo EC, Lin HC. Preventing fissure caries by sealant and fluorides: 12-month results. Journal of Dental Research 2009;(Special issue B):Abstract 272. [Google Scholar]
Liu 2014 {published data only}
- Liu Y, Rong W, Zhao X, Wang M. Caries prevention effect of resin based sealants and glass ionomor sealants. Zhonghua Kou Qiang Yi Xue za Zhi [Chinese Journal of Stomatology] 2014;49(4):199-203. [PubMed] [Google Scholar]
Muller‐Bolla 2018 {published data only}
- Muller-Bolla M, Courson F, Lupi-Pegurier L, Tardieu C, Mohit S, Staccini P, et al. Effectiveness of resin-based sealants with and without fluoride placed in a high caries risk population: multicentric 2-year randomized clinical trial. Caries Research 2018;52(4):312-22. [DOI] [PubMed] [Google Scholar]
Neidell 2016 {published data only}
- Neidell M, Shearer B, Lamster IB. Cost-effectiveness analysis of dental sealants versus fluoride varnish in a school-based setting. Caries Research 2016;50(Suppl 1):78-82. [DOI] [PubMed] [Google Scholar]
Petterson 1983 {published data only}
- Petterson E, Pettersson M, Olofsson IL, Ogeman B. Does fissure sealing of the 6th year molars add to the preventive measures of fluoride application? [Har fissurförsegling på 6-ärsmolarer en försvarbar tilläggseffect utöver fluorlackning?]. Tandlakartidningen 1983;75(9):497-9. [PubMed] [Google Scholar]
Riethe 1977 {published data only}
- Riethe P, Streib W, Schubring G. Clinical studies of Nuva Seal, Epoxylite 9070 and Fluor-Protector [Klinische Untersuchungen mit Nuva Seal, Epoxylite 9070 und Fluor-Protector]. Deutsche Zahnarztliche Zeitschrift 1977;32(11):853-5. [PubMed] [Google Scholar]
Ruff 2018 {published data only}
- Ruff RR, Niederman R. Comparative effectiveness of treatments to prevent dental caries given to rural children in school-based settings: protocol for a cluster randomised controlled trial. BMJ Open 2018;8(4):e022646. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saifullina 1990 {published data only}
- Saifullina KhM, El'darusheva ZA. The effectiveness of preventing caries in the first permanent molars [Effektivnost' profilaktiki kariesa pervykh postoiannykh moliarov]. Stomatologiia 1990;69(6):67-9. [PubMed] [Google Scholar]
Templeton 2016 {published data only}
- Templeton AR, Young L, Bish A, Gnich W, Cassie H, Treweek S, et al. Patient-, organization-, and system-level barriers and facilitators to preventive oral health care: a convergent mixed-methods study in primary dental care. Implementation Science 2016;11:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Uma 2011 {published and unpublished data}
- Uma SR, Shankar AM, Arunadevi M, Naganandini S. Comparison of caries preventive effectiveness of fissure sealant and fluoride varnish. Archives of Oral Sciences and Research 2011;1(4):198-204. [Google Scholar]
Vermaire 2015 {published data only}
- Vermaire JH, Loveren C. Caries prevention strategies for 6-year-olds. A randomized controlled study, Dutch study. Nederlands Tijdschrift voor Tandheelkunde 2015;122(4):200-8. [DOI] [PubMed] [Google Scholar]
Wolff 2016 {published data only}
- Wolff MS, Hill R, Wilson-Genderson M, Hirsch S, Dasanayake AP. Nationwide 2.5-year school-based public health intervention program designed to reduce the incidence of caries in children of Grenada. Caries Research 2016;50 Suppl 1:68-77. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12615000693527 {published data only}
- ACTRN12615000693527. Preventing tooth decay in children in a remote community in Australia. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368750 (first received 3 July 2015).
ACTRN12616001537448 {published data only}
- ACTRN12616001537448. Management of dental decay in young Aboriginal children [Minimally invasive approach to manage early childhood caries in Aboriginal preschoolers]. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=371735 (first received 8 November 2016). [ACTRN12616001537448]
CTRI201805013564 {published data only}
- CTRI/2018/05/013564. Effectiveness of glass ionomer sealant and fluoride varnish in preventing dental caries on newly erupted permanent molars: a randomized clinical trial. ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=24732 (first received 1 May 2018).
CTRI201805013799 {published data only}
- CTRI/2018/05/013799. Evaluation of relative effectiveness of fissure sealants and fluoride varnish in prevention of occlusal caries in children a randomized control trial. ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=24795 (first received 9 May 2018).
ISRCTN81071356 {published data only}
- ISRCTN81071356. The effectiveness of fluoride varnish versus pit and fissure sealant for the prevention of caries in children of primary health care. isrctn.com/ISRCTN81071356 (first received 15 June 2009). [DOI: 10.1186/ISRCTN81071356] [DOI]
NCT01438866 {published data only}
- NCT01438866. Use of fissure sealants on primary molars. clinicaltrials.gov/ct2/show/NCT01438866 (first received 22 September 2011).
NCT01829334 {published data only}
- NCT01829334. Cost-effectiveness of four methods in preventing fissure caries in permanent teeth. clinicaltrials.gov/ct2/show/NCT01829334 (first received 11 April 2013).
NCT03189797 {published data only}
- NCT03189797. Effect of tailored preventive program on caires [sic] incidence using International Caries Classification and Management System (ICCMS) a randomized clinical trial. clinicaltrials.gov/show/NCT03189797 (first received 16 June 2017).
NCT03315312 {published data only}
- NCT03315312. Occlusal caries management in first permanent molars in child dental care. clinicaltrials.gov/show/NCT03315312 (first received 20 October 2017).
NCT03448107 {published data only}
- NCT03448107. Comparative effectiveness of treatments to prevent dental caries. clinicaltrials.gov/show/NCT03448107 (first received 27 February 2018).
NCT03685058 {published data only}
- NCT03685058. Effect of light curable resin modified glass ionomer varnish on non-cavitated proximal carious lesions' progression. clinicaltrials.gov/show/NCT03685058 (first received 26 September 2018).
NCT04163354 {published data only}
- NCT04163354. Glass ionomer sealant versus fluoride varnish on occlusal caries prevention. clinicaltrials.gov/ct2/show/NCT04163354 (first received 14 November 2019).
SLCTR/2019/009 {published data only}
- SLCTR/2019/009. Comparison of the cost effectiveness of fluoride varnish versus pit sealants and fissures in reducing the incidence of caries in children - a randomized controlled clinical trial. slctr.lk/trials/slctr-2019-009 (first received 10 March 2019).
TCTR20180124001 {published data only}
- TCTR20180124001. Prevention of early childhood caries (ECC) through high risk approach. clinicaltrials.in.th/index.php?tp=regtrials&menu=trialsearch&smenu=fulltext&task=search&task2=view1&id=3179 (first received 2 September 2017).
Additional references
ADA 2003
- American Dental Association. Bisphenol A and dental materials. ada.org/1766.aspx (accessed December 2014).
ADA 2016
- American Dental Association. Statement on bisphenol A and dental materials. ada.org/en/member-center/oral-health-topics/bisphenol-a (accessed 10 February 2019).
Ahovuo‐Saloranta 2017
- Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No: CD001830. [DOI: 10.1002/14651858.CD001830.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Alves 2014
- Alves LS, Zenkner JE, Wagner MB, Damé-Teixeira N, Susin C, Maltz M. Eruption stage of permanent molars and occlusal caries activity/arrest. Journal of Dental Research 2014;93((7 Suppl 1)):114-9S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arenholt‐Bindslev 1999
- Arenholt-Bindslev D, Breinholt V, Preiss A, Schmalz G. Time-related bisphenol-A content and estrogenic activity in saliva samples collected in relation to placement of fissure sealants. Clinical Oral Investigations 1999;3:120-5. [DOI] [PubMed] [Google Scholar]
Azarpazhooh 2008a
- Azarpazhooh A, Main PA. Is there a risk of harm or toxicity in the placement of pit and fissure sealant materials? A systematic review. Journal of the Canadian Dental Association 2008;74(2):179-83. [PubMed] [Google Scholar]
Azarpazhooh 2008b
- Azarpazhooh A, Main PA. Fluoride varnish in the prevention of dental caries in children and adolescents: a systematic review. Journal of the Canadian Dental Association 2008;74:73-9. [PubMed] [Google Scholar]
Bader 2004
- Bader JD, Shugars DA. A systematic review of the performance of a laser fluorescence device for detecting caries. Journal of the American Dental Association 2004;135(10):1413-26. [DOI] [PubMed] [Google Scholar]
Batchelor 2004
- Batchelor PA, Sheiham A. Grouping of tooth surfaces by susceptibility to caries: a study in 5–16 year-old children. BMC Oral Health 2004;4:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bawden 1998
- Bawden JW. Fluoride varnish: a useful new tool for public health dentistry. Journal of Public Health Dentistry 1998;58(4):266-9. [DOI] [PubMed] [Google Scholar]
Brown 1995
- Brown LJ, Selwitz RH. The impact of recent changes in the epidemiology of dental caries on guidelines for the use of dental sealants. Journal of Public Health Dentistry 1995;55(5 Spec No):274-91. [DOI] [PubMed] [Google Scholar]
Carvalho 2014
- Carvalho JC. Caries process on occlusal surfaces: evolving evidence and understanding. Caries Research 2014;48(4):339-46. [DOI] [PubMed] [Google Scholar]
Chokkalingam 1998
- Chokkalingam A, Scherer R, Dickersin K. Agreement of data in abstracts compared to full publications. Controlled Clinical Trials 1998;19:S61-2. [Google Scholar]
Chu 2006
- Chu CH, Lo EC. A review of sodium fluoride varnish. General Dentistry 2006;54(4):247-53. [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation Covidence. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Curtin 2002
- Curtin F, Elbourne D, Altman DG. Meta-analysis combining parallel and cross-over clinical trials. II: binary outcomes. Statistics in Medicine 2002;21(15):2145-59. [DOI] [PubMed] [Google Scholar]
Dorri 2015
- Dorri M, Dunne SM, Walsh T, Schwendicke F. Micro-invasive interventions for managing proximal dental decay in primary and permanent teeth. Cochrane Database of Systematic Reviews 2015, Issue 11. Art. No: CD010431. [DOI: 10.1002/14651858.CD010431.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekstrand 2012
- Ekstrand K, Martignon S, Bakhshandeh A, Ricketts DN. The non-operative resin treatment of proximal caries lesions. Dental Update 2012;39:614-22. [DOI] [PubMed] [Google Scholar]
Enno 1982
- Enno A, Craig GG. Economic aspects of the prolonged fluoride application method. Australian Dental Journal 1982;27(2):91-3. [DOI] [PubMed] [Google Scholar]
Fleisch 2010
- Fleisch AF, Sheffield PE, Chinn C, Edelstein BL, Landrigan PJ. Bisphenol A and related compounds in dental materials. Pediatrics 2010;126(4):760-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frencken 2017
- Frencken JE, Sharma P, Stenhouse L, Green D, Laverty D, Dietrich T. Global epidemiology of dental caries and severe periodontitis–a comprehensive review. Journal of Clinical Periodontology 2017;44:S94-105. [DOI] [PubMed] [Google Scholar]
GRADE 2004
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 1 April 2020. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Griffin 2008
- Griffin SO, Oong E, Kohn W, Vidakovic B, Gooch BF, CDC Dental Sealant Systematic Review Work Group, et al. The effectiveness of sealants in managing caries lesions. Journal of Dental Research 2008;87:169-74. [DOI] [PubMed] [Google Scholar]
Hallstrom 1993
- Hallstrom U. Adverse reaction to a fissure sealant. Report of a case. ASDC Journal of Dentistry for Children 1993;60(2):143-6. [PubMed] [Google Scholar]
Helfenstein 1994
- Helfenstein U, Steiner M. Fluoride varnishes (Duraphat): a meta-analysis. Community Dentistry and Oral Epidemiology 1994;22(1):1-5. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. In: Higgins JP, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hopewell 2006
- Hopewell S, Clarke M, Askie L. Reporting of trials presented in conference abstracts needs to be improved. Journal of Clinical Epidemiology 2006;59(7):681-4. [DOI] [PubMed] [Google Scholar]
ICDAS 2008
- International Caries Detection and Assessment System (ICDAS) Coordinating Committee. ICDAS International Caries Assessment and Detection System. www.icdas.org/assets/downloads/Appendix.pdf (no longer available) (accessed August 2015).
Isaksson 1993
- Isaksson M, Bruze M, Björkner B, Niklasson B. Contact allergy to Duraphat. Scandinavian Journal of Dental Research 1993;101:49-51. [DOI] [PubMed] [Google Scholar]
Joskow 2006
- Joskow R, Boyd Barr D, Barr JR, Calafat AM, Needham LL, Rubin C. Exposure to bisphenol A from bis-glycidyl dimethacrylate-based dental sealants. Journal of the American Dental Association 2006;137:353-62. [DOI] [PubMed] [Google Scholar]
Khouja 2018
- Khouja T, Smith KJ. Cost-effectiveness analysis of two caries prevention methods in the first permanent molar in children. Journal of Public Health Dentistry 2018;78(2):118-26. [DOI] [PubMed] [Google Scholar]
Landis 1977
- Landis JR, Koch GG. The measurement of observer agreement for categorial data. Biometrics 1977;33:159-74. [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Llodra 1993
- Llodra J, Bravo M, Delgado-Rodriquez M, Baca P, Galvez R. Factors influencing the effectiveness of sealants: a meta-analysis. Community Dentistry and Oral Epidemiology 1993;21(5):261-8. [DOI] [PubMed] [Google Scholar]
Marinho 2013
- Marinho VC, Worthington HV, Walsh T, Clarkson JE. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD002279. [DOI: 10.1002/14651858.CD002279.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McComb 2001
- McComb D, Tam LE. Diagnosis of occlusal caries. Part I. Conventional methods. Journal of Canadian Dental Association 2001;67(8):454-7. [PubMed] [Google Scholar]
McDonald 1992
- McDonald SP, Sheiham A. The distribution of caries on different tooth surfaces at varying levels of caries – a compilation of data from 18 previous studies. Community Dental Health 1992;9(1):39-48. [PubMed] [Google Scholar]
Mejàre 2003
- Mejàre I, Lingström P, Petersson LG, Holm AK, Twetman S, Källestål C, et al. Caries-preventive effect of fissure sealants: a systematic review. Acta Odontologica Scandinavica 2003;61:321-30. [DOI] [PubMed] [Google Scholar]
Mejàre 2014
- Mejàre I, Axelsson S, Dahlén G, Espelid I, Norlund A, Tranaeus S, et al. Caries risk assessment: a systematic review. Acta Odontologica Scandinavica 2014;72(2):81-91. [DOI] [PubMed] [Google Scholar]
Neusser 2014
- Neusser S, Krauth C, Hussein R, Bitzer EM. Clinical effectiveness and cost-effectiveness of fissure sealants in children and adolescents with a high caries risk [Molarenversiegelung als Kariesprophylaxe bei Kindern und Jugendlichen mit hohem Kariesrisiko]. GMS Health Technology Assessment 2014;10(Doc2):0. [DOI: 10.3205/hta000118, URN:urn:nbn:de:0183-hta0001180] [DOI] [PMC free article] [PubMed] [Google Scholar]
NHS England
- NHS England. National cost collection for the NHS. improvement.nhs.uk/resources/national-cost-collection/ (accessed prior to 19 September 2020).
Nicholson 2007
- Nicholson JW. Polyacid-modified composite resins ("compomers") and their use in clinical dentistry. Dental Materials 2007;23(5):615-22. [DOI] [PubMed] [Google Scholar]
Nyvad 1999
- Nyvad B, V Machiulskiene V, Bælum V. Reliability of a new caries diagnostic system differentiating between active and inactive caries lesions. Caries Research 1999;33(4):252-60. [DOI] [PubMed] [Google Scholar]
Petersen 2005
- Petersen PE. Sociobehavioural risk factors in dental caries – international perspectives. Community Dentistry and Oral Epidemiology 2005;33:274-9. [DOI] [PubMed] [Google Scholar]
Petersson 1993
- Petersson LG. Fluoride mouthrinses and fluoride varnishes. Caries Research 1993;27 Suppl 1:35-42. [DOI] [PubMed] [Google Scholar]
Petersson 2004
- Petersson LG, Twetman S, Dahlgren H, Norlund A, Holm AK, Nordenram G, et al. Professional fluoride varnish treatment for caries control: a systematic review of clinical trials. Acta Odontologica Scandinavica 2004;62:170-6. [DOI] [PubMed] [Google Scholar]
Public Health England 2019
- Public Health England. Press release: almost 9 out of 10 child hospital tooth extractions due to decay. www.gov.uk/government/news/almost-9-out-of-10-child-hospital-tooth-extractions-due-to-decay (accessed prior to 19 September 2020.
Public Health Scotland 2019
- Public Health Scotland. General dental service: treatments provided by dentists. www.isdscotland.org/Health-Topics/Dental-Care/General-Dental-Service/treatments-provided-by-dentists.asp (access prior to 19 September 2020).
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Righolt 2018
- Righolt AJ, Jevdjevic M, Marcenes W, Listl S. Global-, regional-, and country-level economic impacts of dental diseases in 2015. Journal of Dental Research 2018;97(5):501-7. [DOI] [PubMed] [Google Scholar]
Ripa 1993
- Ripa LW. Sealants revised: an update of the effectiveness of pit-and-fissure sealants. Caries Research 1993;27 Suppl 1:77-82. [DOI] [PubMed] [Google Scholar]
Ruse 1999
- Ruse ND. What is a "compomer"? Journal of Canadian Dental Association 1999;65(9):500-4. [PubMed] [Google Scholar]
Schmalz 1999
- Schmalz G, Preiss A, Arenholt-Bindslev D. Bisphenol-A content of resin monomers and related degradation products. Clinical Oral Investigations 1999;3(3):144-9. [DOI] [PubMed] [Google Scholar]
Seppä 1999
- Seppä L. Efficacy and safety of fluoride varnishes. Compendium of Continuing Education in Dentistry 1999;20(1 Suppl):18-26. [PubMed] [Google Scholar]
Shellis 1994
- Shellis RP, Duckworth RM. Studies on the cariostatic mechanisms of fluoride. International Dental Journal 1994;44:263-73. [PubMed] [Google Scholar]
Shemilt 2019
- Shemilt I, Aluko P, Graybill E, Craig D, Henderson C, Drummond M, et al, on behalf of the Campbell and Cochrane Economics Methods Group. Chapter 20: Economic evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated August 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Sköld‐Larsson 2000
- Sköld-Larsson K, Modeer T, Twetman S. Fluoride concentration in plaque in adolescents after topical application of different fluoride varnishes. Clinical Oral Investigations 2000;4(1):31-4. [DOI] [PubMed] [Google Scholar]
Splieth 2010
- Splieth CH, Ekstrand KR, Alkilzy M, Clarkson J, Meyer-Lueckel H, Martignon S, et al. Sealants in dentistry: outcomes of the ORCA Saturday Afternoon Symposium 2007. Caries Research 2010;44(1):3-13. [DOI] [PubMed] [Google Scholar]
Splieth 2016
- Splieth CH, Christiansen J, Foster Page LA. Caries epidemiology and community dentistry: changes for future improvements in caries risk groups. Outcomes of the ORCA Saturday Afternoon Symposium, Greifswald, 2014. Part 1. Caries Research 2016;50:9-16. [DOI] [PubMed] [Google Scholar]
Stedman 2011
- Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2011;40(6):1732-4. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JA, Egger M, Moher D. Chapter 10: Addressing reporting biases. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Tellez 2013
- Tellez M, Gomez J, Pretty I, Ellwood R, Ismail AI. Evidence on existing caries risk assessment systems: are they predictive of future caries? Community Dentistry and Oral Epidemiology 2013;41(1):67-78. [DOI] [PubMed] [Google Scholar]
Ten Cate 1997
- Ten Cate JM. Review on fluoride, with special emphasis on calcium fluoride mechanisms in caries prevention. European Journal of Oral Sciences 1997;105:461-5. [DOI] [PubMed] [Google Scholar]
Twetman 2013
- Twetman S, Axelsson S, Dahlen G, Espelid I, Mejàre I, Norlund A, et al. Adjunct methods for caries detection: a systematic review of literature. Acta Odontologica Scandinavica 2013;71:388-97. [DOI] [PubMed] [Google Scholar]
Twetman 2016
- Twetman S. Caries risk assessment in children: how accurate are we? European Archives of Paediatric Dentistry 2016;17:27-32. [DOI] [PubMed] [Google Scholar]
Whelton 2004
- Whelton H. Overview of the impact of changing global patterns of dental caries experience on caries clinical trials. Journal of Dental Research 2004;83(Spec Iss No C):C29-34. [DOI] [PubMed] [Google Scholar]
WHO 1997
- World Health Organization. Oral Health Survey: Basic Methods. 4th edition. Geneva: WHO, 1997. [Google Scholar]
WHO 2013
- World Health Organization. Oral Health Surveys: Basic Methods. 5th edition. Geneva: WHO, 2013. [Google Scholar]
WHO 2014
- WHO (World Health Organization). Global caries map for 12 year olds (based on the most recent data in CAPP in 2014 according-to-WHO-Regions). Figure: Dental caries levels (DMFT) among 12-years-olds, December 2014. mah.se/CAPP/Country-Oral-Health-Profiles/According-to-WHO-Regions/Global-caries-map-2013--2014/ (accessed 10 February 2019).
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision-making. Evidence-based Dentistry 2015;16(3):69-71. [DOI] [PubMed] [Google Scholar]
Wright 2016
- Wright JT, Tampi MP, Graham L, Estrich C, Crall JJ, Fontana M, et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: a systematic review of randomized controlled trials – a report of the American Dental Association and the American Academy of Pediatric Dentistry. Journal of American Dental Association 2016;147(8):631-45. [DOI] [PubMed] [Google Scholar]
Zenkner 2013
- Zenkner JE, Alves LS, Oliveira RS, Bica RH, Wagner MB, Maltz M. Influence of eruption stage and biofilm accumulation on occlusal caries in permanent molars: a generalized estimating equations logistic approach. Caries Research 2013;47(3):177-82. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Ahovuo‐Saloranta 2016
- Ahovuo-Saloranta A, Forss H, Hiiri A, Nordblad A, Mäkelä M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No: CD003067. [DOI: 10.1002/14651858.CD003067.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hiiri 2006
- Hiiri A, Ahovuo-Saloranta A, Nordblad A, Mäkelä M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD003067. [DOI: 10.1002/14651858.CD003067.pub2] [DOI] [PubMed] [Google Scholar]
Hiiri 2010
- Hiiri A, Ahovuo-Saloranta A, Nordblad A, Mäkelä M. Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No: CD003067. [DOI: 10.1002/14651858.CD003067.pub3] [DOI] [PubMed] [Google Scholar]


