Abstract
Amongst the most important conditions in the differential diagnosis of epilepsy is the one that manifests as paroxysms of altered behaviour, awareness, sensation or sense of bodily control in ways that often resemble epileptic seizures, but without the abnormal excessive or synchronous electrical activity in the brain that defines these. Despite this importance, there remains little agreement – and frequent debate – on what to call this condition, known inter alia as psychogenic non-epileptic seizures (PNES), dissociative seizures (DS), functional seizures (FS), non-epileptic attack disorder (NEAD), pseudoseizures, conversion disorder with seizures, and by many other labels besides. This choice of terminology is not merely academic – it affects patients’ response to and understanding of their diagnosis, and their ability to navigate health care systems.This paper summarises two recent discussions hosted by the American Epilepsy Society and Functional Neurological Disorders Society on the naming of this condition. These discussions are conceptualised as the initial step of an exploration of whether it might be possible to build consensus for a new diagnostic label.
Keywords: Non-epileptic seizures, Dissociative seizures, Conversion disorder, Functional neurological disorder
1. Introduction
It has caused me the greatest trouble, and for ever causes me the greatest trouble, to perceive that unspeakably more depends upon what things are called, than on what they are.”
– [1]
When Nietzsche was troubled by the greater attention paid to names than to the things themselves, he was probably not thinking about the nosology of nonepileptic paroxysms associated with alterations of motor and sensory function, perception, and awareness. However, it is certainly the case that the naming of what has mostly been called psychogenic non-epileptic seizures (PNES) in the recent scientific literature,1 but what has also been labelled as dissociative seizures (DS), functional seizures (FS), non-epileptic attack disorder (NEAD), pseudoseizures, and conversion disorder with seizures (to name only the most frequently used labels) has caused vigorous debate. For instance, 10 years ago, the American Epilepsy Society (AES) hosted a discussion of the favoured terminology, with lines being drawn in the pages of Neurology. [2–4] A recent review by Ali Asadi-Pooya and colleagues [5] opened the discussion again, provoking a range of responses. [6–8]
These discussions focus on words – and the words preferred in different cultures, specialties, and fields of practice. But there is more to a name than the words alone; in a 1962 book (to which the title of this piece is owed), the British philosopher J. L. Austin draws attention to the different things we do with words: warning, urging, threatening – or naming. [9] He also draws a distinction between those things we try to do with words, and the things we in fact achieve: the warned person is appropriately cautioned, the urged persuaded, the threatened cowed. What of the named – or diagnosed?
Two recent seminars hosted by the Functional Neurological Disorder Society (FNDS) and the American Epilepsy Society (AES) held at the start of December 2020 sought to address this question – not to debate what to call PNES (the term currently recommended by the International League Against Epilepsy [ILAE]), but to discuss what we are doing – and what we should be aiming to do – when we give certain labels to the condition(s) known inter alia as PNES. An international panel including representatives of the epileptology, neurology, psychology, psychiatry, paediatrics, and patient communities presented their contrasting views of the intended functions and unintended consequences of different names, with subsequent moderated discussion seeking to elucidate what we should want the name for the condition(s) to do. These discussions were conceptualised as the initial step of an exploration, whether it might be possible to build consensus for a new diagnostic label. Here we summarise the key themes emerging from those discussions.
2. Methods
2.1. Data
2.1.1. Seminars
Two 90-minute online seminars were held on the 3rd and 7th December 2020, the first hosted by the FNDS as part of its weekly Zoom® webinar series, the second by the PNES Special Interest Group (SIG) of the AES as part of its 2020 Annual Meeting. The FNDS session was an open-access event, whereas the PNES SIG could only be joined by individuals who had paid to participate in the Annual AES Meeting. The planning committee (under the direction of Barbara Dworetzky, comprising members of AES PNES SIG and FNDS leadership) sought an expert panel aiming to represent each of the following groups of interest: patient advocate; paediatric psychologist; paediatric (child/adolescent) psychiatrist; adult neuropsychiatrist; adult neuropsychologist; epileptologist specialising in FND; and epileptologist not specialising in FND. The panel selection process intentionally sought to ensure a diversity of gender, nationality, and background in the panel. The events were advertised through relevant professional membership organisations (FNDS, AES, ILAE, American Clinical Neurophysiology Society, American Academy of Neurology (AAN), American Psychological Association, American Neuropsychiatric Association, National Association of Epilepsy Centers), patient groups (FND Hope) and on social media (Twitter).
Each event took the form of a series of brief presentations from an expert panel (see Box 1 for panellists in each seminar), followed by a moderated discussion. Participants were able to leave comments and post questions in a ‘chat’ box in writing. Questions were read out and directed at particular experts by the meeting moderators, Dr David Perez (FNDS) and Dr Julia Doss (AES SIG). Spoken and written (chat) content from the sessions is included in this report.
Box 1. Seminar participants and flipped classroom contributors.
FNDS (Functional Neurological Disorder Society)
Coordinator: Barbara A Dworetzky
Presenter: Benjamin Tolchin
Moderator: David L Perez
Discussion participants: Bridget Mildon, W. Curt LaFrance, Jr, Gaston Baslet, Laura Goldstein, Jon Stone, Maria Oto, Julia Doss, Nicole Roberts, Jeffrey Buchhalter, Barbara A Dworetzky
AES (American Epilepsy Society)
Organisers: Julia Doss, Barbara A Dworetzky, Jerzy P Szaflarski
Presenters: Benjamin Tolchin, Julia Doss, Barbara A Dworetzky, Gregory L Barkley, Ellen Riker, Markus Reuber
Discussion participants: Julia Doss, Barbara A Dworetzky, Benjamin Tolchin, Gaston Baslet, W Curt LaFrance, Jr, Markus Reuber
Flipped Classroom material providers
FND Hope, Markus Reuber, Mark Hallett, Kasia Kozlowska, Aileen McGonigal
2.1.2. Flipped classroom materials
We used a ‘flipped classroom’ model, whereby participants are invited to view informational content online prior to the seminar, to provide a shared knowledge base with which to enter the discussion. A series of recorded brief presentations offering different perspectives on the naming of PNES were shared with participants prior to the events (see Box 1 for contributors). These were intended to target known issues of contention in the naming of PNES. Flipped classroom materials are available at https://www.fndsociety.org/fnd-education/dec3-webinar-material.
2.1.3. Survey
Following the seminars, participants were invited to complete two brief surveys: one covering their opinion on the most important issues in the naming of PNES, another inviting open responses to the flipped classroom materials. Sixty-five respondents completed the first survey, but only nine the second. Given very low response rate to the second, we excluded responses from further analysis. References to ‘the survey’ below therefore refer to the first of these.
2.2. Analysis
We used the seminars, flipped classroom material, and survey as data for a thematic analysis conducted within a reflexive and contextualist framework. [10] This involves familiarisation with the data before generating codes that summarise and interpret ideas expressed. Coding supports identification of themes from the data, which are then refined by returning to the data. Our framework acknowledges the influence that theoretical constructs drawn from prior discussions on the naming of PNES are likely to have on our analysis, while allowing for their inductive modification by codes emerging from our interpretations of the data.
3. Results
We identified eight salient themes within the different materials summarised (seminars, flipped classroom materials, and survey). These could broadly be categorised into four concerning the intentions of naming – what we might seek to do – and four concerning the consequences – what in fact occurs (see Box 2 for themes and codes within each theme).
Box 2. Themes and sub-themes.
Intentions
- Mechanism
- One mechanism or multiple
- The ‘psychogenic’ question
- Mechanistic vs. mechanism-agnostic naming
- Therapeutic benefit
- Names as treatment
- Defining ‘benefit’
- Communication
- From specialists
- From patients
- Between languages
- Institutional and administrative functions
- Consequences
- Stigma
- Acceptability of names
- Names to address stigma
- Stigmatisation from the health community
Dissonance and disagreement
Barriers to care
Labels shape people
3.1. Intentions
3.1.1. Mechanism
A key focus of debate throughout the texts concerned the relationship between a name for PNES and its mechanism – the causal process (es) by which the clinical phenomena variously labelled as PNES are hypothesised to occur. Comments on mechanism addressed: whether PNES is explained by a single mechanism or multiple mechanisms; the level of explanation at which such mechanisms are situated; and the value (or otherwise) of making reference to the underlying mechanism in the name for PNES.
Despite extensive discussions of the merits and disadvantages of names that make greater or lesser reference to mechanism (for instance terms such as ‘psychogenic’ or ‘dissociative’), more participants felt that other concerns were ultimately of greater terminological importance. In the survey, the three aspects of a name most bound up with mechanism (“connecting the disorder to a broader theoretical category or framework”, “identifying a putative aetiology of the disorder”, or “maintaining agnosticism for mechanisms/etiologies of disorder that remains poorly understood”) were ranked as being the least important (see Fig. 1).
Fig. 1.
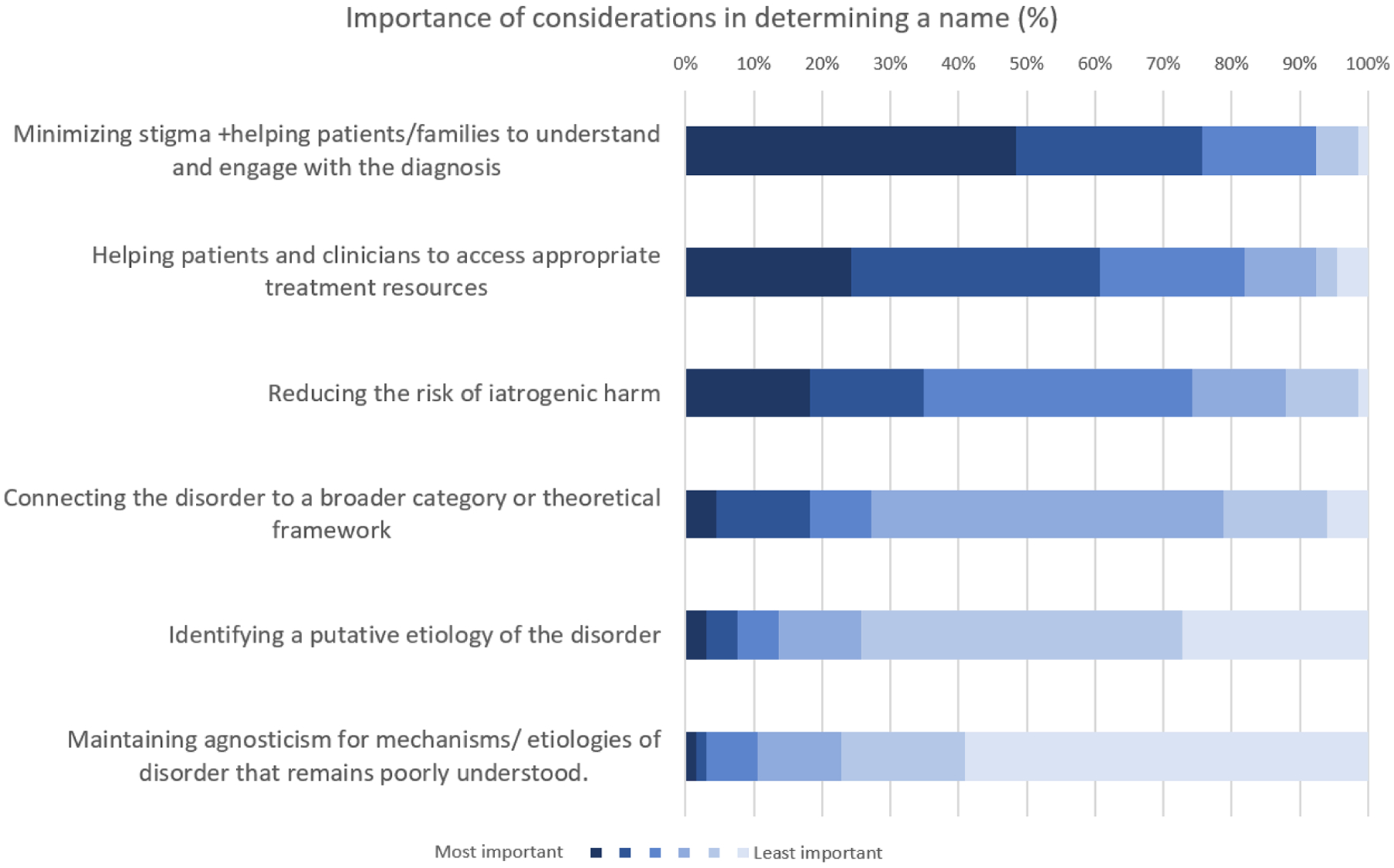
Respondents’ ranking of relative importance of different considerations in determining a name for the disorder (6-point Likert scale from most to least important; bars represent proportion ranking a consideration of given importance, where darker colours are more important, lighter less).
3.1.1.1. One mechanism or multiple.
Considering whether a name for PNES should describe its mechanism invites the question of whether PNES even refers to a sufficiently distinct phenomenon amenable to mechanistic explanation. Contributors to the seminars questioned this in both directions. Reflecting discussions in previous publications, [11, 12] participants asked whether PNES are a particular presentation of a broader disorder (the ‘seizure variant’ of FND or conversion disorder). Mark Hallett, a neurologist and neurophysiologist, made a case for this in his contribution to the flipped classroom materials, highlighting that PNES share overlapping epidemiology, clinical features, putative aetiology and pathophysiology, and treatment approaches with other forms of FND. Or, as one participating neurologist asked in the chat, might it be “mechanistically heterogeneous”, encompassing a syndrome resulting from a range of different processes – in which case, might multiple names in fact be more appropriate?2
Contributors to the FNDS seminar highlighted the context-sensitivity of the degree of specificity required from a name. Resonating with previously published conceptualisations of functional neurological disorder, [13] Nicole Roberts, an experimental clinical psychologist, demonstrated the relevance to PNES of a range of different constructs (emotion processing, agency, attention, interoception, and predictive inference) and underlying neural circuits (e.g. governing salience, multimodal integration, and attention), proposing that these allowed for both ‘cross-cutting’ and ‘sub-typing’ of explanations of PNES. Markus Reuber, an epileptologist, proposed that this may permit a ‘staggered approach’ to nomenclature for clinicians, with more or less specific or mechanism-agnostic terminology being appropriate in different contexts (for instance starting with a term such as “functional seizure” when an episode has been found not to be caused by epileptic activity, and specifying this to “dissociative functional seizure” when a more specific psychological mechanism has been identified).
3.1.1.2. Should a label reference ‘psychogenicity’?.
As introduced by Aileen McGonigal, an epileptologist, in her pre-seminar video, the alterations of function culminating in PNES can be understood as occurring at the level of neurophysiology, [14–16] but at present psychological models are relatively more developed. [17, 18] While most participants in both seminars eschewed the mind-body dualism that has held these different levels of explanation to be fundamentally different in kind, a number of arguments were made emphasising one or the other. Gaston Baslet, a neuropsychiatrist, as well as several audience members, argued for a name that at least retains a “conceptual link” with the term ‘psychogenic’, with the hope that understanding the condition in such terms will support engagement with the present best-evidenced (psychological) treatments. W. Curt LaFrance Jr (a neurologist and psychiatrist) favoured use of ‘conversion’ on such grounds. In his treatment experience in clinic and extensive research on patient outcomes, making this psychological mechanism explicit supports patients in finding alternative means of managing challenging emotions – and thus breaking the link to their symptomatic episodes. Laura Goldstein, an adult clinical neuropsychologist, gave support for ‘dissociation’ by noting that “it’s a term that conveys a mechanism to work with”; based on her group’s research and related clinical activities she finds that patients can draw from everyday understandings of more familiar dissociative phenomena, to come to understand how similar processes might produce their own experiences.
By contrast, Rebecca Geiger – a person with a diagnosis of FND – suggested that emphasising a psychological aetiology may cause confusion for patients whose own phenomenal experience is over-whelmingly physical, and who may find their events accompanied by an array of other physical symptoms. A putative solution to this impasse was provided by those who advocated an explicitly biopsychosocial approach to naming the condition. Reflecting suggestions made elsewhere, [19] McGonigal highlighted successes in multi-scale modelling of other neurological disorders – where mechanisms operating at different levels of explanation are employed in complementary, rather than competing, fashion. Roberts proposed the use of a name that explicitly describes the mechanisms operating at psychological and neural circuit levels (e.g. “emotion dysregulation and emotional interoception disorder”).
3.1.1.3. Mechanism-specific vs mechanism-agnostic naming.
While the arguments in the previous section highlighted the advantages of referring to a particular mechanism in the name of the condition, other participants stated that uncertainty over underlying mechanisms was a reason to favour an agnostic approach. Jon Stone, a neurologist, observed that many other conditions (e.g. migraine, multiple sclerosis) do not wear their (complex) aetiologies on their sleeves. Using migraine as an example, he suggested that names not making explicit reference to psychological causation may support rather than inhibit engagement with psychological factors (such as stress) contributing to the condition. Bridget Mildon, representing the patient organisation FND Hope, proposed that patients’ preference for the term ‘functional seizures’ may in part stem from its lack of commitment to an underlying mechanism; this “allowed researchers and clinicians to keep an open mind” in approaching the condition. This would contrast to the inference (false, as highlighted by LaFrance) made by some clinicians that patients with PNES all have a history of trauma or abuse; while reported adverse life events are highly prevalent amongst those with PNES, they are not universal. [20] Barbara Dworetzky, a neurologist, also drew attention to the need to avoid premature closure in our hunt for the mechanisms of the disorder. She noted that (as discussed by McGonigal in her pre-seminar material), modelling at various levels (including structural anatomy, neurological networks, and psychological processes) contribute to our understanding of the condition. Opting for a name that emphasises the (presently most-developed) psychological mechanisms risks dismissing the importance of others; or, perhaps of more immediate clinical relevance, “licensing people [who do not treat ‘psychological’ problems] to say ‘I don’t need to know this.’” Open-ended terms like ‘functional’ can be understood as operating across these levels – i.e. in explicitly biopsychosocial fashion – since function and dysfunction are relevant concepts at all levels.
However, open-endedness runs the risk of moving toward meaninglessness. As highlighted in an animated dramatization of the experience of a person with PNES navigating their first hospital assessment (shared with seminar attendees by Dworetzky, courtesy of Bernd Pohl-mann, an epileptologist), contentless names (NEAD arguably being the commonly used term coming closest to this) can allow clinicians to absolve themselves of responsibility for dealing with a real problem, and leave patients in a state of uncertainty, told only that “you have nothing”.
Even when names are not completely empty, open-endedness may fail to capture clinically relevant distinctions. McGonigal highlighted that current use of the term ‘functional’ may cause some confusion since disturbances of brain ‘function’ (as recorded e.g. with EEG) are the hallmarks of other conditions (such as epilepsy) to which functional diagnoses are otherwise contrasted. At worst, the use of ‘functional’/’structural’ dichotomy may simply replicate ‘mind’/’body’ dualism by another name (see box 3).
Box 3. Candidate names for PNES.
| Prefixes | ||
|---|---|---|
| PREFIX | POTENTIAL ADVANTAGES | POTENTIAL DISADVANTAGES |
| Functional |
|
|
| Psychogenic |
|
|
| Non-epileptic |
|
|
| Specific mechanisms (dissociative, conversion) |
|
|
| Suffixes | ||
| SUFFIX | POTENTIAL ADVANTAGES | POTENTIAL DISADVANTAGES |
| Seizures |
|
|
| Attacks |
|
|
| Other (event, episode, spell) |
|
|
3.1.2. Therapeutic benefit
Discussion around the therapeutic role of naming concerned: whether names could prove therapeutic by helping patients and families to understand and engage with the diagnosis (and consequent treatment); and how ‘therapeutic benefit’ should be defined. The function of “Minimizing stigma +helping patients/families to understand and engage with the diagnosis” was ranked as the most important consideration when choosing a name in the survey.
3.1.2.4. Names as treatment.
Some participants reported that, in their experience, different choices of terminology can affect patient outcome and thus names can play a therapeutic role. Reflecting the findings of previous studies, [21] Kasia Kozlowska, a child and adolescent psychiatrist, reported – and Julia Doss, a child psychologist, agreed – that, within the context of child and adolescent care, choice of language could play a therapeutic role by “activat[ing] positive hopes and expectations and [steering] the child towards healthy thinking, healthy actions, and healthy future outcomes.” For this reason, Kozlowska reported that she avoids terms that children and adolescents interpret negatively – for example, “psycho” meaning mad, “pseudo” meaning fake, or “behavioural” meaning naughty – because such terms activate anger and distress, and are therefore countertherapeutic and illness-promoting.
3.1.2.5. Defining benefit.
Reuber highlighted that this purported function is more complex than it perhaps sometimes appears in debates surrounding naming: not only do we lack solid evidence of whether choice of name promotes better or worse outcomes; we have failed to specify what a good outcome is. Existing research studies on the ‘number needed to offend’ of particular choices of nomenclature [22, 23] do not actually cover clinical outcomes: do particular names affect rates of seizure freedom, engagement with treatment, or patient and family acceptance? Such questions are amenable to empirical study, but the evidence does not yet exist.
3.1.3. Communication
The communicative function of names was addressed with respect to different speakers and audiences: from specialist to patient; from patient or specialist to other clinicians; and from patients to their friends, families, and communities. The texts also addressed issues of communicating between different languages.
3.1.3.6. Communication from specialists.
Exchanges around the use of the term ‘seizure’ and its alternatives (attack, event, episode) serve as microcosm for the broader questions around communication raised by choice of terminology. Maria Oto, a psychiatrist and epileptologist, drew attention to the implications of this choice in her presentation, arguing that the close semantic association between ‘seizure’ and ‘epilepsy’ could often cause confusion when the former was used to refer to something other than epilepsy, this being amplified for the many people with PNES who may either have been previously misdiagnosed with epilepsy or else experience comorbid epileptic seizures. Benjamin Tolchin, an epileptologist, highlighted that Oto’s concern was a common one amongst US neurologists at least, following his recent informal survey of AAN members responding to discussion of a draft guideline. Reuber observed that this confusion may not just arise in communication with patients or families, but also other professionals. Non-expert clinicians, especially those needing to make time-sensitive decisions in high-pressure environments on the basis of limited information, hearing ‘seizure’ may be inclined to treat as epilepsy – with potentially dangerous, even fatal, consequences for people with PNES. [24] However, despite its drawbacks the term ‘seizure’ came out as preferred by most respondents to the post-seminar survey (Fig. 3).
Fig. 3.
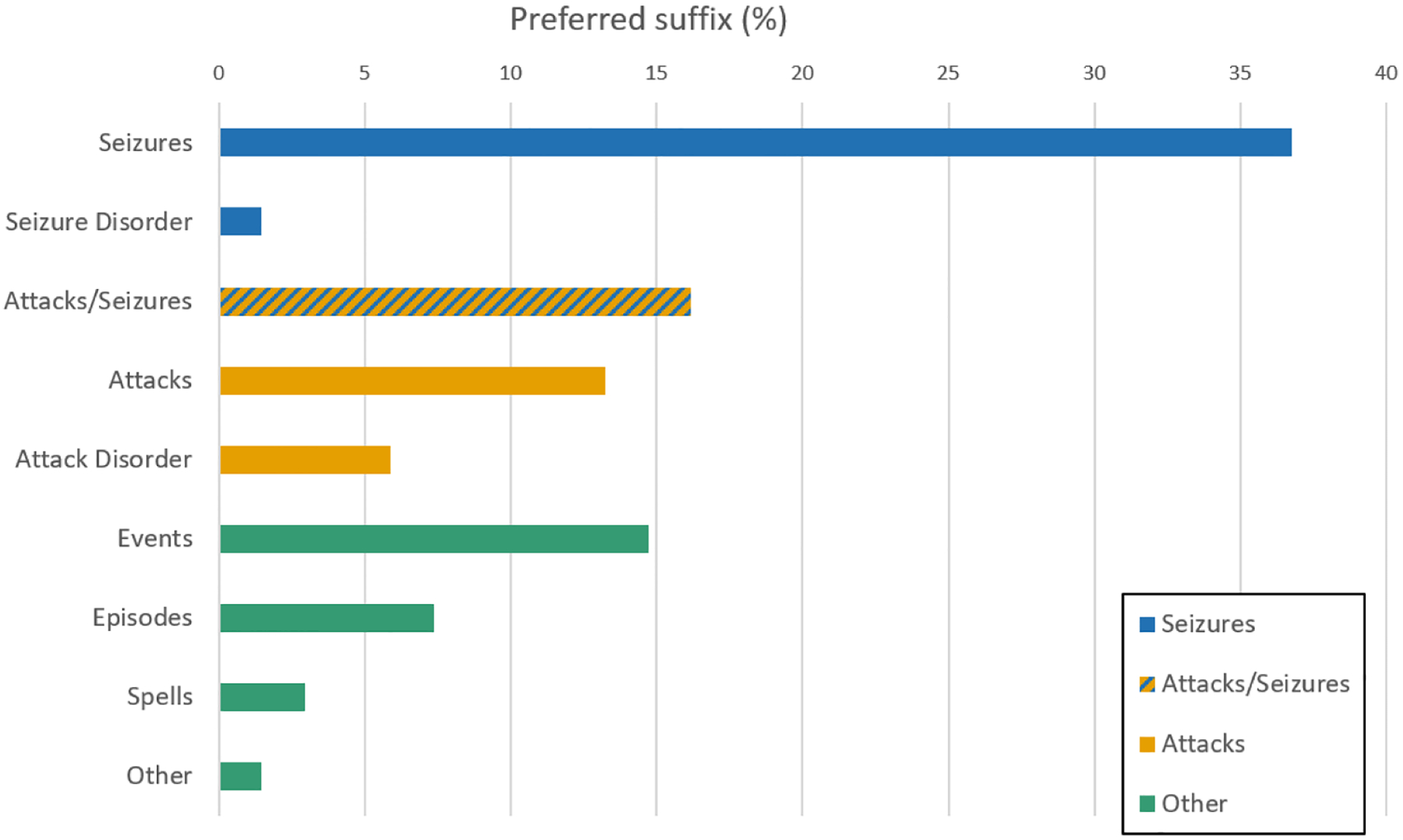
Preferred suffix.
3.1.3.7. Communication from patients.
Mildon observed that communication is also a concern for patients – “how do [patients] convey to other people in the outside world what is wrong with them?” For this purpose, she proposed that ‘seizure’ “very clearly explains what is happening”, whereas more neutral terms like ‘event’ “leave the patient having to go on further” in their explanation. In contrast, Reuber referred to his previous research demonstrating that some people with PNES show resistance to the ‘seizure’ label [25].
3.1.3.8. Communication between languages.
Discussions around naming should account for its use in different languages and cultures, as well as by and for different audiences. In some cases, terms will have different connotations in different languages. For instance, as observed by McGonigal, the term ‘dissociation’ has a strong historical association with schizophrenia in Francophone psychiatry. In others, the semantic nuances are lost altogether in translation. Christian Hoppe, a psychologist, demonstrated the most extreme version of this when he noted that, in German, the different words ‘seizure’, ‘fit’, and ‘attack’ are simply not used in the medical context – all would be translated as the single term “Anfall”.
Jeffrey Buchhalter, an epileptologist, suggested incorporation of whatever terms are decided upon to be included in the Systematized Nomenclature of Medicine – Clinical Terms (SNOMED CT). This is an international clinical vocabulary/taxonomy that would allow research across languages facilitated by a common coding system. SNOMED CT’s structured “ontology of medical knowledge” could facilitate understanding the relationships between symptoms and functional neurological disorders.
3.1.4. Institutional and administrative functions
Several participants drew attention to the institutional functions played by names. A 2019 FND Hope patient survey reported that 65% felt that their current diagnostic label had adversely affected their care. Some labels may erect obstacles to receiving appropriate care, while – as Dworetzky put it – if nothing else, “‘seizure’ gets you into the seizure specialist’s office.” Of course, this is only of value to the extent that said specialist acknowledges their role (and perhaps more importantly, those of other disciplines) in the diagnosis and treatment of PNES.
Some terms (such as ‘conversion’ and ‘dissociation’) already exist within standard diagnostic classifications such as the ICD and DSM. Goldstein observed that this has practical utility, even if only in obeying Ockham’s admonition to avoid the unnecessary multiplication of entities. However, this issue is complicated by the use of such classifications for administrative as well as clinical functions. Gregory L Barkley, an epileptologist, described how the intimate relationship between ICD codes and payment for services in the US can erect barriers to care. Such payments vary with patterns of healthcare consumption associated with different groups of conditions, which has historically constrained the kinds of terminology that could be used for PNES. While making reference to the psychological components of PNES may be preferable for other reasons, in billing terms, PNES does not behave like other conditions coded as ‘psychiatric’ – addressing it within the ‘seizure’ category more accurately reflects how patients interact with healthcare services. Other terms like ‘events’ or ‘spells’, meanwhile, have no place in ICD codes at all. Such coding is also used in retrospective research, and the lack of consistent coding – and the possibility of the condition falling between ‘neurological’ and ‘psychiatric’ codings – may contribute to some of the research lacunae in PNES. The significance for research does not only look backwards, however; classifications may shape future research directions and funding opportunities, potentially emphasising different aspects of the condition.
3.2. Consequences
3.2.1. Stigma
Stigma was one of the most prevalent themes in the data, and considered highly important by participants. Survey participants ranked “Minimizing stigma +helping patients/families to understand and engage with the diagnosis” as the most important function of a name for PNES. Discussions on the theme of stigma concerned: the potential of a name to reduce or perpetuate stigma; the influence of stigma on the acceptability of names for patients; and the role of the healthcare community in perpetuating stigmatisation of PNES.
3.2.1.9. Stigma and acceptability.
Acceptability of a label to those who bear it ranked highly amongst many participants’ objectives. Several referred to previous research on the perceived offensiveness of different names for PNES. [22, 23] As argued by Stone, such offensiveness is usually bound closely with associated stigma – “and stigma tends to change and move with the term.” This point was used by several participants to argue that choosing a name was of secondary importance until the processes driving the stigma attached to those labels were addressed. However, as Dworetzky highlighted, utopian visions of a future free of stigma do not help patients in the here and now; and until we reach that future “patients need something to say” to their family, friends, and colleagues – using a name that does not harm them and helps them engage in treatment remains important.
3.2.1.10. Names addressing stigma.
Elsewhere, however, comments addressed the potential of names as a tool to reduce stigma. Roberts, by drawing an analogy with attention deficit hyperactivity disorder (ADHD), raised hopes that a diagnostic label could “legitimise […] in a biological way that may be helpful.” Other participants suggested that specifically incorporating the physical or biological components of the condition into the name would be important for this process, whereas emphasising the psychosocial aspects “does a disservice to patients who are trying to find treatments [for physical symptoms]” (Geiger, FNDS webinar) – especially when, without a diagnosis, insurers will not cover such treatment.
The distinction between biological and psychological and its relation to stigma also manifested in comments addressing mind-body dualism in medicine. Some suggested this dualism as a source of stigma, being particularly attached to the ‘mind’ side. Lorna Myers, an adult psychologist, proposed that resisting this stigma requires a name and practice that helps patients and families to understand “there is no shame in having a psychological condition.” By contrast, avoidance of terminology to make something more palatable in the short term may exacerbate its stigmatisation. David Perez, a neurologist and psychiatrist, proposed that an understanding of PNES and FND more broadly as biopsychosocial conditions could serve to mitigate this: “We know that mental illness in society is stigmatised, and there is a divide between physical health and mental health. I have oftentimes wondered if FND – at the intersection […] is an avenue frankly to tackle that stigma, that mental health and physical health are not (inherently) separate.”
3.2.1.11. Stigmatisation by healthcare institutions.
Several participants discussed the tendency for stigmatising associations to be transferred between terms. Some questioned the individuals and institutions driving this process. Mildon proposed that healthcare workers and institutions must be responsible, because the lay public does not know what technical terms such as ‘functional’ mean in medical contexts, so “it’s important that we look at how the medical community perpetuates this bias.” She suggested a “hidden curriculum” (as described elsewhere) [26] socialises health workers into this bias; the differing ‘prestige’ afforded to different conditions amongst health workers – and the stability of these ratings across time – does suggest that negative attitudes toward some conditions persist in the health community. [27] Others also argued for a need for change in healthcare education to address this: Baslet commented that PNES and other conditions need to be acknowledged in medical training “as early as possible” to prevent this process.
3.2.2. Dissonance and disagreement
One important emerging theme was that of dissonance within and between different stakeholder groups as to the best choice of terminology and the most important factors in shaping that terminology. This was evident in the survey, which displayed a wide spread of terminological preferences (see Figs. 2 and 3 ). Within this theme, there also emerged reference to how this dissonance itself can be a cause of difficulty. The disagreement on name – and its implications of disagreement regarding the nature of the condition itself – could cause confusion for patients and families, impeding understanding and acceptance of the diagnosis. As Mildon commented: “When the medical community can’t even agree on a name and terminology, it really discredits the diagnosis in general.” This does perhaps underestimate just how common an occurrence the proliferation of names is throughout medicine, however – multiple names for the same condition is perhaps the rule and not the exception.
Fig. 2.
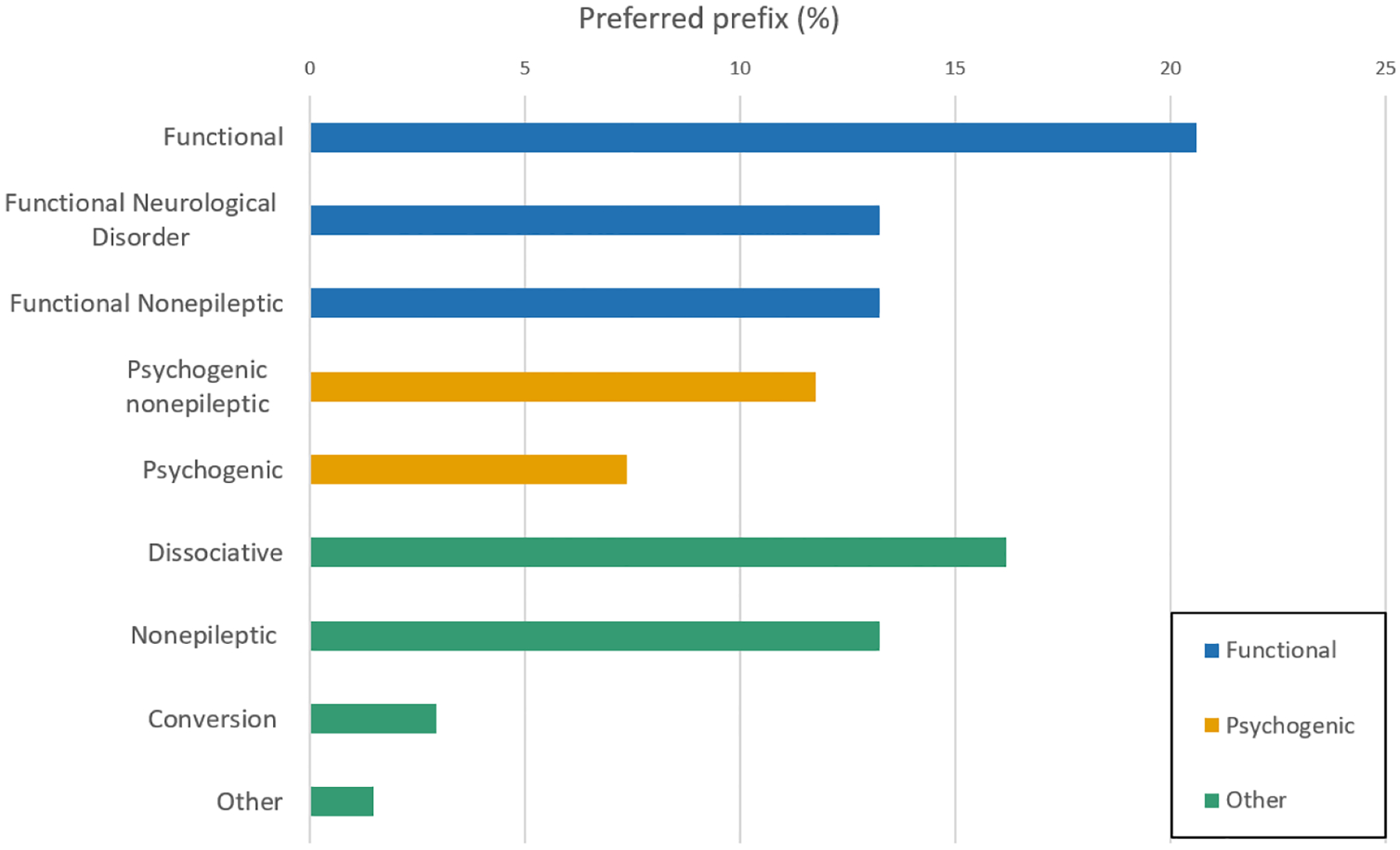
Preferred prefix.
3.2.3. Barriers to care
Related to, but distinct from, the administrative theme identified above, another emerging theme was of the choice of name as a potential barrier to care. The 2019 FND Hope patient survey suggested that nearly two thirds of respondents experienced their diagnostic label as adversely affecting their ability to access appropriate healthcare. [28]
This theme involved discussion of how different terminology may influence referral pathways – for instance the term ‘seizures’ (but not necessarily ‘events’ or ‘attacks’) facilitating the referral to a seizure specialist. They may also influence available treatments. The repur-posing of clinical terminology for administrative purposes – e.g. by insurance companies or other payers – may inhibit access. Mildon suggested that: “It’s really difficult for patients with a psychological definition and coding to access physical therapy when they need it, or sometimes [occupational therapy] … It literally can change whether a patient can access appropriate treatment.” This highlights the multimodal treatments that can affect this disorder and the need for the name to not limit this access.
Of course, patients with PNES do not just present to neurologists with epileptic-seizure-like events, they also present to specialists in internal medicine or cardiologists with syncope-like (atonic/unresponsive) events (sometimes called “pseudosyncope”), or to movement disorder specialists with abnormal involuntary movements. As Reuber said, given that both types of presentation are thought to be underpinned by the same pathological process, an ideal label would need to work for the latter type of presentation as well.
3.2.4. Labels shape people
Several contributors expressed ideas reflecting the views of the philosopher Ian Hacking, who observed that the engines of scientific discovery have an unusual effect when directed at human categories: rather than presenting fixed targets, human experiences are modified by scientific attempts to classify them. The very fact of being described in a certain way can shape those classified, how they perceive themselves and their position in the world. [29, 30] At several points participants addressed how the classification of PNES might do more than just name – for some who internalise the name, it might create a particular way of being. In contrast, patients who externalise their diagnosis have said, “I have seizures, but my seizures don’t have me.” [31] While patients may approach their diagnosis differently, the burden of illness remains: in Mildon’s words, patients “take their diagnoses home […they] live with them every day.”
Roberts expressed a concern that “biology in a name can be constraining”, suggesting that certain ways of naming the condition may shape people’s self-perception in a way that impedes their recovery. She cited the example of ‘mild traumatic brain injury’, a name from which patients can infer permanent brain damage and thus an expectation of permanent cognitive deficit. [32, 33] Reuber suggested that the ways in which different labels make up people may differ in where they attribute agency and the locus of control. He referenced recent research on the different language used by people with diagnoses of “FND” compared with “conversion disorder”, describing how those with the FND diagnosis are more likely to describe their minds or selves as passive, in relation to a body or brain that is ‘out of control’; those with a conversion diagnosis are more likely to view the mind as active agent, and the self as a resilient entity, able to find ways to reinstate control. [34]
There remains an open question whether any terminology for or model of the disorder could capture all that is most relevant to those experiencing it. Many people with the condition have lived through and been unable to prevent experiences that are irreconcilable with their core moral beliefs, morally injurious “soul wounds.” [35] The experience can leave the person “sitting uncomfortably in [their] physical and metaphysical chair.” [36] If nothing else, this serves as reminder that the nosological map is not the territory of all human experience, [37] and what is most relevant from the medical perspective may not./’ be what is most important for the person labelled.
4. Discussion
The discussions arising in these two seminars were not intended to provide a consensus on naming for PNES – indeed, they highlighted persisting dissonance over terminology. However, they showed a significant development from preceding debates in the inclusion of the voices of those who experience the condition, and the weight placed by participating clinicians on their perspective. However, in the absence of broader consultation with other professional and patient groups and the arguments put forward against these particular terms, the findings of the survey should only be regarded as a preliminary step along the journey of negotiating an optimal name for PNES.
There was general support for a unifying name – for the sake of the patients who bear the label, and communication within and outside medicine. This support was tempered by acknowledgement that potential heterogeneity of mechanism or different therapeutic objectives may merit use of different terminology in different contexts, or a nested approach incorporating both broader and more specific names. Potential advantages and disadvantages suggested for different names are summarised in Box 3.
A plurality of respondents to the post-seminar survey favoured the terms ‘functional’ and ‘seizures’. This contrast with the results of recent discussions amongst AAN members (who sought to move away from use of these terms) perhaps reflects the involvement of participants living with the condition, and the relative priorities of survey respondents: while the arguments for avoiding the term ‘seizure’ chiefly concern mechanism and communication between specialists, Mildon suggested using it might help people with the condition communicate within their communities while avoiding stigmatisation.
There was, however, a diversity of opinion regarding what we should aim to be doing with a name. The themes explored above cover many of these – contrasting, and even potentially conflicting – objectives. That naming should support (or at least not impede) access to treatment and successful outcomes was understandably a priority both for those working with and those experiencing the condition. A name should also function across contexts (clinical, social, and cultural or linguistic), and minimise dissonance and disagreement regarding the nature or legitimacy of the underlying condition.
There was also recognition that diagnostic labels do not exist purely within the clinic; those with the condition carry their labels with them throughout their lives. The potentially stigmatising consequences of names were a recurrent concern throughout the seminars. Link and Phelan’s influential model of the process of stigmatisation begins with identification and labelling of difference [38] – thus names are indeed closely bound up with stigmatisation. The means of preventing stigmatisation are less clear. New labels can quickly come to bear the same associations. Several patients and some clinicians suggest that emphasising the biological aspects of the condition would be a “legitimising” manoeuvre in addressing stigma. The example of psychiatric conditions such as schizophrenia, however, may prove cautionary here – in general the promise of biological explanations has not reduced, and may even have increased, negative associations attached to these conditions. [39–41]
Having thus drawn some preliminary perspectives on what the clinical community should be seeking to do with its words, there remains the question of how best to do it. The results of these seminars will inform further work on this subject by the FNDS. Additionally, the ILAE PNES Task Force is proposing a plan to create a consensus diagnostic label for the condition currently termed PNES. A multi-stage, mixed-method process involving an international, multi-lingual survey of relevant patient and professional groups (ideally not only representing those with an interest in epileptology and psychiatry but also psychosomatic medicine, psychotherapy and syncope) regarding the most commonly used terminology and stakeholders’ perspectives on these terms could be subjected to qualitative and quantitative analysis. The results of this analysis could then inform a second-round survey on respondents’ conclusions regarding the acceptability of different terms.
Nietzsche notwithstanding, the question of what things are called may not be more important than what they are. In the case of PNES, these two questions may not be readily separable. Clinicians treat people – with complex personal narratives, values, and systems of meaning – not diagnoses; but diagnoses can facilitate or obstruct that process. For those living with the condition, finding a common consensus name for (what is currently called) PNES (or at least a commonly agreed, least worst option) may be an important step in sharing with their community and their clinicians what the condition is.
Acknowledgements
This paper represents independent research part-funded (LHG) by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed in this publication are those of the author and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. LHG is a Director of the FND Society and a member of the Medical Advisory Board for FND Action. She receives royalties from Wiley and from Taylor & Francis.
(DLP) Funding:
None.
Disclosures:
D.L.P. has received honoraria for continuing medical education lectures on functional neurological disorder and is on the editorial board of Epilepsy & Behaviour.
(BT) Funding:
None.
Disclosures:
BT has received honoraria from Columbia University Medical Centre, the International League against Epilepsy, and the American Academy of Neurology.
(BAD) Supported in part from the A.J. Trustey Research Fund. B.A.D. receives royalties from Oxford University Press.
(MH) Funding:
NINDS Intramural Program
Disclosures:
G.B. has received honoraria for continuing medical education lectures on functional neurological disorder and royalties from Oxford University Press.
Footnotes
Use of the term PNES in this article reflects this convention only, and should not be inferred to reflect that this is necessarily the preferred label moving forward.
We thank an anonymous reviewer for highlighting the need to emphasise this point.
References
- [1].Nietzsche F The Joyful Wisdom (La Gaya Scienza). T.N. Foulis; 1910. https://www.gutenberg.org/files/52124/52124-h/52124-h.htm. [Google Scholar]
- [2].Benbadis SR. Psychogenic nonepileptic “seizures” or “attacks”? It’s not just semantics: attacks. Neurology 2010;75(1):84–6. 10.1212/WNL.0b013e3181e6216f. [DOI] [PubMed] [Google Scholar]
- [3].LaFrance WC. Psychogenic nonepileptic “seizures” or “attacks”? Neurology 2010; 75(1):87–8. 10.1212/WNL.0b013e3181e62181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Langfitt J, Watson W. Seizures” or “attacks”: a follow-up. Neurology 2010;75(23): 2056–7. 10.1212/WNL.0b013e3182015290. [DOI] [PubMed] [Google Scholar]
- [5].Asadi-Pooya AA, Brigo F, Mildon B, Nicholson TR. Terminology for psychogenic nonepileptic seizures: making the case for “functional seizures. Epilepsy & Behavior 2020;104:106895. 10.1016/j.yebeh.2019.106895. [DOI] [PubMed] [Google Scholar]
- [6].Duncan R Perspectives on a name. Epilepsy & Behavior 2020;105:106986. 10.1016/j.yebeh.2020.106986. [DOI] [PubMed] [Google Scholar]
- [7].Kerr WT, Stern JM. We need a functioning name for PNES: consider dissociative seizures. Epilepsy & Behavior 2020;105:107002. 10.1016/j.yebeh.2020.107002. [DOI] [PubMed] [Google Scholar]
- [8].Tolchin B, Perez DL, Szaflarski JP, et al. What’s in a name? Epilepsy & Behavior 2020;112:107364. 10.1016/j.yebeh.2020.107364. [DOI] [PubMed] [Google Scholar]
- [9].Austin JL. How to do things with words. Harvard University Press; 1975. 2nd edition. [Google Scholar]
- [10].Terry G, Hayfield N, Clarke V, Braun V. Thematic analysis. In: the Sage Handbook of Qualitative Research in Psychology. SAGE; 2017:17–37. [Google Scholar]
- [11].Kanaan RAA, Duncan R, Goldstein LH, Jankovic J, Cavanna AE. Are psychogenic non-epileptic seizures just another symptom of conversion disorder? J Neurol Neurosurg Psychiatry 2017;88(5):425–9. 10.1136/jnnp-2017-315639. [DOI] [PubMed] [Google Scholar]
- [12].Rather MA, Cavanna AE. Nonepileptic attack disorder and functional movement disorder: a clinical continuum? Epilepsy & Behavior 2020;106:107028. 10.1016/j.yebeh.2020.107028. [DOI] [PubMed] [Google Scholar]
- [13].Drane DL, Fani N, Hallett M, Khalsa SS, Perez DL, Roberts NA. A framework for understanding the pathophysiology of functional neurological disorder. CNS Spectr September 4, 2020:1–7. 10.1017/S1092852920001789. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ding J-R, An D, Liao W, et al. Altered Functional and Structural Connectivity Networks in Psychogenic Non-Epileptic Seizures. PLoS ONE 2013;8(5):e63850. 10.1371/journal.pone.0063850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Gallucci-Neto J, Brunoni AR, Ono CR, Fiore LA, Martins Castro LH, Marchetti RL. Ictal spect in psychogenic nonepileptic and epileptic seizures. Psychosomatics; 2020. 10.1016/j.psym.2020.05.016. Published online May 27. [DOI] [PubMed] [Google Scholar]
- [16].Madec T, Lagarde S, McGonigal A, Arthuis M, Benar C-G, Bartolomei F. Transient cortico-cortical disconnection during psychogenic nonepileptic seizures (PNES). Epilepsia 2020;61(8):e101–6. 10.1111/epi.16623. [DOI] [PubMed] [Google Scholar]
- [17].Reuber M, Brown RJ. Understanding psychogenic nonepileptic seizures-Phenomenology, semiology and the Integrative Cognitive Model. Seizure 2017;44: 199–205. 10.1016/j.seizure.2016.10.029. [DOI] [PubMed] [Google Scholar]
- [18].Brown RJ, Reuber M. Psychological and psychiatric aspects of psychogenic non-epileptic seizures (PNES): a systematic review. Clin Psychol Rev 2016;45:157–82. 10.1016/j.cpr.2016.01.003. [DOI] [PubMed] [Google Scholar]
- [19].Lytton WW, Arle J, Bobashev G, et al. Multiscale modeling in the clinic: diseases of the brain and nervous system. Brain Inform 2017;4(4):219–30. 10.1007/s40708-017-0067-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ludwig L, Pasman JA, Nicholson T, et al. Stressful life events and maltreatment in conversion (functional neurological) disorder: systematic review and meta-analysis of case-control studies. The Lancet Psychiatry 2018;5(4):307–20. 10.1016/S2215-0366(18)30051-8. [DOI] [PubMed] [Google Scholar]
- [21].Karterud HN, Risør MB, Haavet OR. The impact of conveying the diagnosis when using a biopsychosocial approach: a qualitative study among adolescents and young adults with NES (non-epileptic seizures). Seizure 2015;24:107–13. 10.1016/j.seizure.2014.09.006. [DOI] [PubMed] [Google Scholar]
- [22].Stone J, Campbell K, Sharma N, Carson A, Warlow CP, Sharpe M. What should we call pseudoseizures?: the patient’s perspective. Seizure 2003;12(8):568–72. 10.1016/S1059-1311(03)00055-4. [DOI] [PubMed] [Google Scholar]
- [23].Stone J, Wojcik W, Durrance D, et al. What should we say to patients with symptoms unexplained by disease? The “number needed to offend. BMJ 2002;325 (7378):1449–50. 10.1136/bmj.325.7378.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Reuber M, Baker GA, Gill R, Smith DF, Chadwick DW. Failure to recognize psychogenic nonepileptic seizures may cause death. Neurology 2004;62(5):834–5. [DOI] [PubMed] [Google Scholar]
- [25].Plug L, Sharrack B, Reuber M. Seizure, Fit or Attack? The Use of Diagnostic Labels by Patients with Epileptic or Non-epileptic Seizures. Applied Linguistics 2010;31 (1):94–114. 10.1093/applin/amp012. [DOI] [Google Scholar]
- [26].Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med 1998;73(4):403–7. 10.1097/00001888-199804000-00013. [DOI] [PubMed] [Google Scholar]
- [27].Album D, Johannessen LEF, Rasmussen EB. Stability and change in disease prestige: a comparative analysis of three surveys spanning a quarter of a century. Soc Sci Med 2017;180:45–51. 10.1016/j.socscimed.2017.03.020. [DOI] [PubMed] [Google Scholar]
- [28].FND Hope Research.. FND hope international. 2021. Accessed February 14, https://fndhope.org/fnd-hope-research/.
- [29].Hacking I The looping effects of human kinds. In: Sperber D, Premack D, Premack AJ, editors. Causal cognition: a multidisciplinary debate. Oxford University Press; 1996. Accessed January 9, 2021, https://oxford.universitypressscholarship.com/view/10.1093/acprof:oso/9780198524021.001.0001/acprof-9780198524021-chapter-12. [Google Scholar]
- [30].Hacking I Kinds of people: moving targets. Proc Br Acad 2021;151. VolBritish Academy; 2007. Accessed January 9, https://britishacademy.universitypressscholarship.com/view/10.5871/bacad/9780197264249.001.0001/upso-9780197264249-chapter-10. [Google Scholar]
- [31].White M, Epston D. Narrative means to therapeutic ends. 1990. First Edition. W. W. Norton & Company. [Google Scholar]
- [32].Suhr JA, Gunstad J. Diagnosis Threat”: the Effect of Negative Expectations on Cognitive Performance in Head Injury. J Clin Exp Neuropsychol 2002;24(4): 448–57. 10.1076/jcen.24.4.448.1039. [DOI] [PubMed] [Google Scholar]
- [33].Roberts NA, Burleson MH, Burmeister LB, et al. Brain boosters: evaluating a pilot program for memory complaints in veterans. Psychol Serv 2020;17(1):33–45. 10.1037/ser0000279. [DOI] [PubMed] [Google Scholar]
- [34].Brenninkmeijer J Conversion disorder and/or functional neurological disorder: how neurological explanations affect ideas of self, agency, and accountability. Hist Human Sci 2020;33(5):64–84. 10.1177/0952695120963913. [DOI] [Google Scholar]
- [35].LaFrance WC, Vo P, Baird G, East R, Stein NR. Moral injury in Veterans with nonepileptic seizures. Epilepsy & Behavior 2020;102:106681. 10.1016/j.yebeh.2019.106681. [DOI] [PubMed] [Google Scholar]
- [36].Reuber M, Rawlings G, Schachter SC. Our words: personal accounts of living with non-epileptic seizures. Oxford University Press; 2018. [Google Scholar]
- [37].Wardrope A Mistaking the Map for the Territory: what Society Does With Medicine. Int J Health Policy Manag 2017;6(10):605–7. 10.15171/ijhpm.2017.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Link BG, Phelan JC. Stigma and its public health implications. Lancet 2006;367 (9509):528–9. 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- [39].Phelan JC. Geneticization of deviant behavior and consequences for stigma: the case of mental illness. J Health Soc Behav 2005;46(4):307–22. 10.1177/002214650504600401. [DOI] [PubMed] [Google Scholar]
- [40].Bennett L, Thirlaway K, Murray AJ. The stigmatising implications of presenting schizophrenia as a genetic disease. J Genet Couns 2008;17(6):550–9. 10.1007/s10897-008-9178-8. [DOI] [PubMed] [Google Scholar]
- [41].Corrigan PW, Rowan D, Green A, et al. Challenging two mental illness stigmas: personal responsibility and dangerousness. Schizophr Bull 2002;28(2):293–309. 10.1093/oxfordjournals.schbul.a006939. [DOI] [PubMed] [Google Scholar]


