Abstract
Objective
We aimed to explore the factors that influence medical students’ intention to integrate dHealth technologies in their practice and analyze the influence of the COVID-19 pandemic on their perceptions and intention.
Methods
We conducted a two-phased survey study at the University of Montreal's medical school in Canada. The study population consisted of 1367 medical students. The survey questionnaire was administered in two phases, that is, an initial survey (t0) in February 2020, before the Covid-19 pandemic, and a replication survey (t1) in January 2021, during the pandemic. Component-based structural equation modeling (SEM) was used to test seven research hypotheses.
Results
A total of 184 students responded to the survey at t0 (13%), whereas 138 responded to the survey at t1 (10%). Findings reveal that students, especially those who are in their preclinical years, had little occasion to experiment with dHealth technologies during their degree. This lack of exposure may explain why a vast majority felt that dHealth should be integrated into medical education. Most respondents declared an intention to integrate dHealth, including AI-based tools, into their future medical practice. One of the most salient differences observed between t0 and t1 brings telemedicine to the forefront of medical education. SEM results confirm the explanatory power of the proposed research model.
Conclusions
The present study unveils the specific dHealth technologies that could be integrated into existing medical curricula. Formal training would increase students’ competencies with these technologies which, in turn, could ease their adoption and effective use in their practice.
Keywords: Digital health, eHealth, medical education, medical practice, artificial intelligence, COVID-19, survey
Introduction
Digital health (dHealth), which is defined by Fatehi et al. 1 as “the proper use of technology for improving the health and wellbeing of people at individual and population levels, as well as enhancing the care of patients through intelligent processing of clinical and genetic data” (p.71), has attracted lots of attention in the past decade worldwide. Every day, hundreds of dHealth innovations, technologies, and smart devices are released at lightning speeds, 2 which has amplified into a US $84 billion world industry with a projected increase to over US $220 billion by 2026. 1 Health Canada and the Food and Drug Administration (FDA) consider a broad spectrum of technologies under the concept of digital health; including mobile health applications, wireless medical devices, telehealth and telemedicine, clinical information systems, big data and artificial intelligence (AI), and robotics, to name a few. 2
The effective use of dHealth technologies by clinicians, managers, policy makers and patients has never been more relevant than it is today. Previous research has shown that dHealth has the potential to prevent disease3,4 and lower healthcare costs,5,6 while helping patients monitor and self-manage chronic conditions7,8 or optimizing the identification and use of available community resources by frail and isolated older adults.9,10 It has also been shown that dHealth technologies can improve the quality, continuity, and availability of care,11–13 tailor medical treatments for individual patients14,15 and facilitate remote patient assessment and follow-up during pandemics.16,17
For the practice of medicine to continue transforming itself and producing better outcomes for patients, future generations of physicians must be able to navigate with ease in an ever-changing digital environment. 18 To this end, the literature teaches us that the training of medical students is an important factor in the adoption of dHealth technologies and that the interaction of future physicians with such technologies during their training allows the development of basic patient care competencies as well as dHealth knowledge, self-efficacy, and diagnostic accuracy.19–23 Yet, it is recognized that too many medical schools integrate dHealth little or not at all into the formal training of future physicians, which poorly prepares them for the changing reality of clinical practice.24–26 This underexposure causes medical students to have limited understanding of dHealth 27 and is prone to lead to bad behaviors in medical students (eg, violation of patient confidentiality), which can ultimately lead to severe legal consequences. 28
While several studies have identified important barriers and facilitators to the development of dHealth education in the medical curriculum29,30 and it appears important to accelerate this integration, 31 we know very little about the perspectives of medical students on this issue. Indeed, very few studies investigated medical students’ beliefs about, familiarity with, and intention to integrate dHealth. Moreover, most existing studies focus on a particular type of dHealth technologies, leaving a more comprehensive picture unaccounted for. For instance, Sit et al. 32 explored the attitudes of 484 United Kingdom (UK) medical students regarding training in AI technologies, their understanding of AI, and career intention towards radiology. Findings reveal that medical students do not feel adequately prepared to work alongside AI but understand the increasing importance of AI in healthcare and would like to receive more training on the subject. As another example, Yaghobian et al. 33 conducted a national study on telemedicine training by 3312 medical students and residents in France. Positive attitudes towards telemedicine, particularly in relation to improving patients’ access to care, were observed. However, the majority of respondents felt they were not trained enough and would like to see training in telemedicine increase. Similar results were found in another study published in the United States, where medical students acknowledged the relevance of and need for telemedicine education in the curriculum. 34
In light of the above, little empirical knowledge is available on medical students’ views on, experimentation with, and intention to integrate dHealth technologies. Further, prior studies either focused on a specific dHealth technology [eg, 35 ] or provided a vague definition of dHealth. 36 Importantly, prior studies soliciting medical students’ opinions were conducted prior to the COVID-19 pandemic. In order to explore the factors that influence medical students’ intention to integrate dHealth technologies in their medical practice and analyze the influence of the COVID-19 pandemic on their perceptions and intention related to dHealth, we conducted a two-phased survey of medical students in Canada. Precisely, our study aims to answer the following research questions: Do medical students intend to integrate dHealth into their future medical practice? What factors influence medical students’ intention? Did COVID-19 influence medical students’ perceptions and intention related to dHealth? Given the present dearth of knowledge on these questions and their increased relevance in the context of the ongoing pandemic, 37 the present study's intended contribution to research and practice lies in a clear and concise characterization and explanation of the role of dHealth in medical education.
Theoretical model
To address the above-mentioned research questions, we first developed a theoretical model. One of the main theoretical foundations of this study is Triandis’ theory of interpersonal behavior 38 which posits that individuals’ behavioral intention is influenced by their beliefs toward the behavior. Triandis defines beliefs as assessments of what an individual thinks about the object of interest There is no implied goodness or badness in beliefs, but only an assessment of what one thinks exists or does not exist For instance, an individual may hold a belief that computers in general contribute to the improvement of society. In this study, medical students’ beliefs were operationalized regarding AI-related technologies specifically rather than dHealth technologies generally, as AI-based tools have the most potential to fundamentally alter and significantly improve the practice of medicine.23,39,40 We posit that the stronger the medical students’ beliefs that AI can positively impact the medical profession as well as their own medical practice, the greater their intention to integrate dHealth technologies (including AI tools) into their future practice.
Second, we postulate that perceived facilitating conditions are another critical determinant of medical students’ behavioral intention related to dHealth adoption. Originating in the technology acceptance model (TAM), a theory that models how users come to adopt a new technology, 41 facilitating conditions are external factors that influence an individual's perceptions of the difficulty with which a task (eg, use of dHealth technologies) may be performed.42–46 In the present study, facilitating conditions are operationalized as students’ level of exposure to or experimentation with dHealth technologies during their medical education. We posit that the more medical students experiment with dHealth technologies during their degree, the higher their intention to integrate dHealth in their medical practice.
Third, our theoretical model includes perceived usefulness, another TAM variable, which is defined as the degree to which a person believes that using a particular technology or information system would enhance their job performance. 41 Adapted to the present study context, perceived usefulness refers to medical students’ perceptions of the importance and relevance of integrating dHealth into the medical curriculum. We posit that the more one thinks that all students should receive training in dHealth as part of their medical degree, the more their intention to integrate dHealth in their own medical practice.
Last, following prior research on dHealth training [eg,18,32,47] as well as various studies testing the TAM [eg,42–44] another construct, called individual background, was added to our research model. This construct was operationalized as a composite of three individual characteristics: gender, age, and academic level. Due to the exploratory nature of this study, we simply assert that students’ individual background is likely to influence their views and perceptions on dHealth technologies.
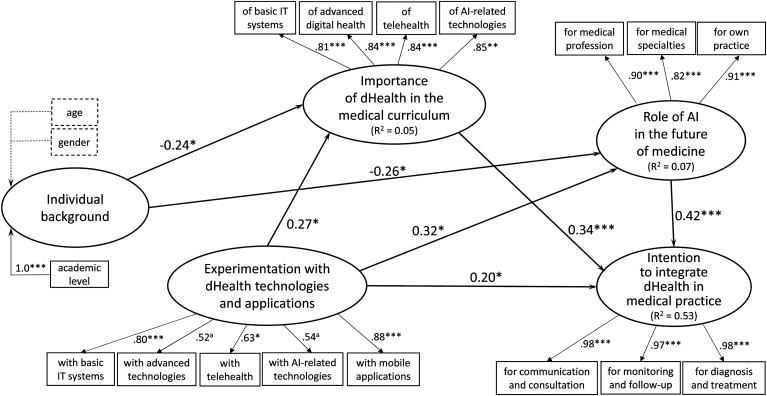
The theoretical model to be empirically tested in this study is shown in Figure 1. Given the relationships postulated by the theoretical lens mobilized above as well as the empirical relationships identified in the extant literature, seven hypotheses were formulated as summarized in Table 1. The first two hypotheses emanate from the TAM wherein medical students’ individual background is deemed to influence their beliefs about the role of dHealth technologies (more particularly AI) in medicine and their perceived dHealth education needs. For their part, hypotheses 3, 4 and 5 also emanate from the TAM wherein external facilitating conditions are deemed to influence beliefs toward a behavior, perceived usefulness, and behavioral intention. Hypothesis 6 is derived from the theory of behavior proposed by Triandis and states that medical students’ beliefs are deemed to positively influence their behavioral intention. The final hypothesis also originates from the TAM and posits a positive relationship between perceived usefulness and behavioral intention.
Figure 1.
Theoretical model.
Table 1.
Research hypotheses.
| # | Hypotheses |
|---|---|
| 1 | Medical students’ individual background will likely influence their beliefs about the role of AI in the future of medicine |
| 2 | Medical students’ individual background will likely influence their perceptions relating to the importance of integrating dHealth into medical education |
| 3 | The greater the students’ experimentation with dHealth during their medical education, the stronger and more positive their beliefs about the role of AI in the future of medicine |
| 4 | The greater the students’ experimentation with dHealth technologies during their medical degree, the greater their perceived dHealth education needs |
| 5 | The greater the students’ experimentation with dHealth technologies during their medical education, the greater their intention to integrate dHealth into their medical practice |
| 6 | The stronger the medical students’ beliefs about the positive impact of AI on medicine, the greater their intention to integrate dHealth into their medical practice |
| 7 | The stronger the medical students’ perceptions related to the inclusion of dHealth into the medical curriculum, the greater their intention to integrate dHealth into their medical practice |
Methods
Setting and data collection
The present study was conducted at the University of Montreal's (UM) medical school in Canada. During the 5-year long undergraduate medical curriculum, no formal dHealth education or training is provided to students. However, students have access to the EDUlib online training platform which offers educational content on a variety of subjects including health and information technologies, as well as to symposia and conferences on different aspects of dHealth. Also, workshops on mobile health and EMR systems are mandatory for students in their clerkship, a stage at which students are called upon to experiment with different dHealth technologies. Finally, issues related to the use of social media, email, and mobile applications by healthcare professionals are also covered in elective seminars.
The study population consisted of 1367 UM medical students. The survey questionnaire was administered in two phases, that is, an initial survey (t0) in February 2020, before the Covid-19 pandemic, and a replication survey (t1) in January 2021, during the pandemic. It was distributed to all students via the medical school's mailing list The study was also promoted via social media groups that are only accessible by UM medical students and the local medical student association sponsored the survey via its newsletter. There was no incentive for students to fill out the online questionnaire and there were no negative consequences if students did not participate.
The invitation contained a hyperlink directing the participants to the questionnaire through a secure Web site. The online questionnaire was developed on the Qualtrics survey platform. Qualtrics complies with applicable data privacy laws in its role as a data processor of customer data, as indicated on the company's website.
Questionnaire development
We were unable to locate any pre-existing questionnaire that assessed the variables included in our research model; hence, we decided to develop our own instrument. The survey design underwent several rounds of iteration, and final validation was performed with a group of 10 UM medical students who were excluded from the sampling population. The final survey instrument consisted of 70 5-point Likert questions and 8 yes/no questions. The four tables located in Appendix I provide essential information on the questionnaire's content and on measurement items and scales.
Statistical analysis
The data were first analyzed through descriptive statistics (mean, standard deviation, percentage) and further examined through analyses of variance and principal component analyses, using the IBM SPSS software v28. Component-based structural equation modeling (SEM) was then used to test the research hypotheses (cf. Figure 1). As implemented in the SmartPLS software, the partial least squares (PLS) technique was chosen for its robustness with regard to the distribution of residuals and its greater affinity for exploratory rather than confirmatory research purposes when compared to covariance-based SEM techniques such as AMOS and EQS. 48
Ethics approvals
The survey questionnaire was approved by the UM's ethics committee on October 29, 2019 (#CERSES-19-108-D). Informed consent was obtained from all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Demographics
A total of 184 students responded to the initial survey at t0 (13%), whereas 138 responded to the replication survey at t1 (10%). As shown in Table 2, most participants were female (65% at t0 and 70% at t1). The mean age was 23 years, which is comparable to the average age of medical students at UM. While our sample was evenly distributed between the first and fifth year of medical studies at t0, there were fewer fourth- and fifth-year medical students at t1.
Table 2.
Profile of the respondents.
| Medical students’ background | Pre-COVID-19 | Peri-COVID-19 | |||
|---|---|---|---|---|---|
| t0 (n = 184) | t1 (n = 138) | ||||
| N | % | N | % | ||
| Academic level | Preparatory year | 40 | 22% | 28 | 20% |
| First year preclinical | 36 | 20% | 32 | 23% | |
| Second year preclinical | 43 | 23% | 55 | 40% | |
| First year clerkship | 33 | 19% | 8 | 6% | |
| Second year clerkship | 32 | 17% | 14 | 10% | |
| Gender | Female | 119 | 65% | 92 | 70% |
| Male | 65 | 35% | 40 | 30% | |
| Age | Mean | 22.9 | 22.6 | ||
| Standard deviation | 3.5 | 2.7 | |||
| Minimum | 18 | 18 | |||
| Maximum | 38 | 35 | |||
Descriptive analysis
For analytical purposes, individual dHealth technologies and applications were grouped under five technology “bundles” that were named basic IT systems (eg, electronic medical records, clinical information systems), advanced dHealth (eg, robotics, virtual reality), telehealth (eg, teleconsultation, tele-expertise), AI-related technologies (eg, artificial intelligence, machine learning) and mobile applications (eg, UpToDate, BMJBestPractice).
First, with regard to the questions relating to experimentation with dHealth technologies, a large majority of the medical students had little occasion to experiment with advanced dHealth, telehealth, and AI-related technologies in the course of their medical curriculum (see Table A1 in Appendix I). A minority of the participants reported having been somewhat or very exposed to basic IT systems (i.e. EMR, CIS, and iEHR systems) and two specific mobile apps, namely, UpToDate and the Quebec Health Technology Assessment (HTA) Institute's mobile app. 3
Second, a vast majority of respondents agreed that all students should receive formal dHealth education as part of their medical degree. As shown in Table A2 in Appendix I, medical students believe that the most important dHealth education needs concern, by order of importance, basic IT systems, telehealth, AI-related technologies, and robotics. A majority of respondents, however, perceive lesser need concerning other advanced dHealth technologies including blockchain, internet of things, virtual reality, and augmented reality.
Third, a large majority of the sampled students at both t0 and t1 are observed to have strong beliefs toward AI-related technologies, be it in terms of these technologies’ impact on the medical profession, in general, as well as on many medical specialties such as radiology and anatomopathology (see Table A3 in Appendix I). Moreover, most students indicate that they expect to use AI-based tools in support of one or more of their future medical activities including image and data analysis, diagnosis and, to a lesser extent, prognosis.
Fourth, a large majority of students declared an intention to integrate dHealth into their medical practice. As shown in Table A4 in Appendix I, this intention is most important with regard to disease prevention, diagnosis, and treatment, followed by patient communication and consultation, and patient monitoring and follow-up activities.
Last, when comparing the variable means between the two samples (t0 and t1), as presented in Table 3, t-test analyses confirm statistically significant differences (P < 0.001) on a few research variables. For one thing, medical students in the replication study (t1), on average, experimented more with telehealth technologies and, conversely, experimented less with basic IT systems and mobile applications than those in the initial survey (t0). This last result may be due to the fewer proportion of fourth- and fifth-year students who participated at t1 in comparison to t0. Further, medical students surveyed at t1 expressed a greater need for education on telehealth technologies than those surveyed at t0. This specific need was ranked first by students in the replication study, whereas it was ranked second by participants in the initial study. Here, one may tentatively explain these differences by the advent of the COVID-19 pandemic, which has brought telemedicine to the forefront of medical training and medical practice. 49
Table 3.
Comparison of medical students’ views and intention between t0 and t1.
| Research construct | Pre-COVID-19 | Peri-COVID-19 | T-test |
|---|---|---|---|
| Research variable | (n = 184) | (n = 138) | (two-tailed) |
| mean | mean | ||
| Individual Background | |||
| Age | 22.9 | 22.6 | 1 |
| Gender | 0.65 | 0.7 | -0.9 |
| Academic level | 2.9 | 2.6 | 1.9 |
| Experimentation with dHealth technologies | |||
| Basic IT systems | 1.8 | 1.4 | 4.2*** |
| Advanced dHealth | 1.2 | 1.1 | 2.4** |
| Telehealth | 1.2 | 1.5 | −4.6*** |
| AI-related technologies | 1.3 | 1.2 | 2 |
| Mobile applications | 1.5 | 1.3 | 3.6*** |
| Importance of dHealth in medical curriculum | |||
| Basic IT systems | 4.1 | 4.1 | 0.3 |
| Advanced dHealth | 3.4 | 3.4 | -0.1 |
| Telehealth | 3.7 | 4.1 | −5.0*** |
| AI-related technologies | 3.5 | 3.5 | 0.3 |
| Beliefs about impact of AI-related technologies | |||
| On the medical profession | 3.6 | 3.5 | 1.2 |
| On various medical specialties | 3.4 | 3.3 | 0.8 |
| On one's own medical practice | 3.9 | 3.6 | 0.8 |
| Intent to integrate dHealth in medical practice | |||
| Patient communication and consultation | 3.4 | 3.3 | 0.6 |
| Patient monitoring and follow-up | 3.3 | 3.1 | 1.5 |
| Disease prevention, diagnosis and treatment | 3.6 | 3.3 | 2.1** |
** P < 0.05; *** P < 0.001.
Measurement model
Component-based SEM was used to empirically test our set of research hypotheses. The PLS technique was selected because it is suited to measurement models such as ours that include both exogenous (reflective) and endogenous (formative) constructs. 50 Precisely, whereas the research construct “individual background” is modeled as being “formative” given its composite and multidimensional nature, the four other constructs are modeled as being “reflective”. 51
The initial step consisted of estimating the measurement model at t0 and t1 using the SmartPLS software. We started by assessing the internal consistency of the measures (manifest variables) as well as the unidimensionality, reliability, predictive validity, and discriminant validity of the four reflective research constructs (latent variables). As shown in Table 4, all the Cronbach α values (except one at t1) were above the .70 threshold, thus confirming the internal consistency of the research variables. The unidimensionality of a reflective construct is assessed by looking at each of its indicators’ loading (λ), the threshold being 0.40 for newly developed scales. 52
Table 4.
Psychometric properties of the research variables and constructs.
| Pre-COVID-19 (t0) | Peri-COVID-19 (t1) | |||||||
|---|---|---|---|---|---|---|---|---|
| Research construct | CR b | AVE c | CR b | AVE c | ||||
| Research variable | α a | VIF d | α a | VIF d | ||||
| Individual background | - | - | - | - | ||||
| Age (yrs.) | - | 1.11 | - | 1.23 | ||||
| Gender (0: male, 1: female) | - | 1.02 | - | 1.08 | ||||
| Academic level (1 to 5) | - | 1.12 | - | 1.2 | ||||
| Experimentation with dHealth technologies | 0,81 | 0.47 | 0,81 | 0.48 | ||||
| With basic IT systems | 0.86 | - | 0.87 | - | ||||
| With advanced dHealth | 0.88 | - | 0.81 | - | ||||
| With telehealth | 0.78 | - | 0.69 | - | ||||
| With AI-related technologies | 0.84 | - | 0.84 | - | ||||
| With mobile applications | 0.88 | - | 0.86 | - | ||||
| Importance of dHealth in the curriculum | 0.90 | 0.70 | 0.93 | 0.76 | ||||
| On basic IT systems | 0.93 | - | 0.97 | - | ||||
| On advanced dHealth technologies | 0.93 | - | 0.93 | - | ||||
| On telehealth | 0.86 | - | 0.87 | - | ||||
| On AI-related technologies | 0.84 | - | 0.84 | - | ||||
| Role of AI in the future of medicine | 0.91 | 0.76 | 0.92 | 0.80 | ||||
| For the medical profession | 0.82 | - | 0.78 | - | - | |||
| For the medical specialties | 0.82 | - | 0.79 | - | ||||
| For their medical practice | - | - | - | - | ||||
| Intention to integrate dHealth in future practice | 0.98 | 0.95 | 0.99 | 0.98 | ||||
| For patient communication and consultation | 0.94 | - | 0.97 | - | ||||
| For patient monitoring and follow-up | 0.91 | - | 0.95 | - | ||||
| For disease prevention, diagnosis and treatment | 0.95 | - | 0.97 | - | ||||
Cronbach alpha coefficient of reliability.
CR: composite reliability. [CR = (Σλi)2/((Σλi)2 + Σ(1-λi2))] .
AVE: average variance extracted by a construct from its associated variables. [AVE = ∑λi2 / n] .
VIF: variance inflation factor. VIF = 1 / (1 – Ri2), where Ri2 is the unadjusted R2 obtained when variable i is regressed against all other variables forming a construct.
Moreover, the reflective constructs’ composite reliability (CR) must be above the 0.7 threshold, which is the case for all four reflective constructs. There is also evidence of the convergent validity of these constructs because their average variance extracted (AVE) is above the 0.50 threshold, except for the “Experimentation with dHealth” construct which is just below this threshold (0.47). Despite this, it was decided not to remove any of this last construct's indicators from its measure, given that it demonstrated adequate reliability and unidimensionality. Finally, there is evidence of discriminant validity, that is, of the extent to which a research construct differs from other constructs. In the case of the four reflective constructs, the shared variance between each construct and the other constructs was found to be less than the AVE from its indicators. 52 In the case of the sole formative construct, individual background, the fact that it shared less than 70% variance with the other construct in the measurement model, and thus correlated less than perfectly with these constructs, was again indicative of strong discriminant validity. 51
Next, as the usual validity criteria for reflective constructs are inapplicable to a formative construct, one must instead verify that there is no multicollinearity among the formative construct's indicators. One uses the variance inflation factor (VIF) statistic to do so, a common rule being that a variable's VIF value be less than 3.3, or in other words, that less than 70% of the variance in the variable be jointly explained by the other variables. 53 As shown in Table 4, the outer VIF values estimated by PLS for the three formative indicators of the individual background construct varied from 1.02 to 1.12 at t0 and from 1.08 to 1.23 at t1, well below the 3.3 threshold, thus indicating the absence of multicollinearity.
Measuring the research variables through a self-administered questionnaire with a single respondent poses a risk of common method bias (CMB). 54 As precautionary measures, we chose different question formats and scale types. Further, we examined the correlation matrix of the five research constructs to determine if any two constructs correlated above 0.90, as this could signal the presence of CMB in the data. 55 In our case, all construct correlations (not shown here) were well-below this threshold. We also employed Harman's single-factor test to check for CMB, examining the unrotated factor solution for all variables in the measurement model. As multiple factors emerged from the factor analysis and as no single factor accounted for 50% or more of the covariance among the variables, this further suggests the absence of CMB. 56
Causal analysis at t0
Next, the causal paths inferred from the conceptual framework were tested by assessing the path coefficients (β) estimated by the SEM procedure as executed by the SmartPLS software. As shown in Figure 2, the performance of the theoretical model at t0 that interrelates the five research constructs is indicated by the strength and significance of the βs and the proportion of explained variance (R2 = 0.53), as befits PLS's focus on prediction and concern with generalization. 57
Hypothesis 1 (partly confirmed). Given the results of the initial causal analysis (t0) provided by the SEM procedure, an initial finding lies in the negative and highly significant path coefficient that links the medical students’ characteristics to their beliefs about the role of AI in the future of medicine (β = −0.26, P < 0.05). As shown in Figure 2, the primary explanatory characteristic is the academic level, as students who are in their preparatory and preclinical years have stronger beliefs about the positive impact of AI on the medical profession, various medical specialities, and their own medical practice. Age and gender were not significantly associated with students’ beliefs about AI technologies.
Figure 2.
Causal analysis results at t0.
Hypothesis 2 (partly confirmed). Another related finding is that medical students’ characteristics are negatively and significantly associated to their perceived dHealth education needs (β = −0.24, P < 0.05). Here again, the primary explanatory characteristic is the academic level, as students in their preparatory or preclinical years express more important needs than those in their clerkship years. One may surmise that the more advanced students, having experimented more with various dHealth technologies and applications during rotations, are more realistic as to the place of dHealth in the curriculum and thus have less expectations in this regard. Age and gender were not associated with perceived dHealth education needs.
Hypothesis 3 (confirmed). As expected, we found a positive and significant relationship between medical students’ experimentation with dHealth and their beliefs about the role of AI technologies in the future of medicine and their own medical practice (β = 0.32, P < .05).
Hypothesis 4 (confirmed). Another finding concerns the positive influence of the medical students’ experimentation with dHealth technologies on their dHealth education needs (β = 0.27, P < 0.05). In other words, greater exposure to and practical experience with dHealth technologies lead students to understand and appreciate the pivotal role of these technologies in healthcare and the necessity of integrating dHealth into medical education.
Hypothesis 5 (confirmed). We also found a positive and significant relationship between students’ level of experimentation with dHealth technologies and their intention to integrate dHealth into their practice (β = 0.20, P < 0.05). In other words, experimenting with dHealth technologies during their medical degree spurs students’ intention to integrate these systems and tools in their future practice. Now, given that the indirect effects of experimenting with dHealth on the students’ intention (through their dHealth education needs and beliefs about AI) are greater than the direct effects, this finding is rather tentative and calls for further empirical validation.
Hypothesis 6 (confirmed). The next finding lies in the positive and highly significant path coefficient (β = 0.42, P < 0.001) that links medical students’ beliefs about the impact of AI on medicine to their behavioral intention. This result is in line with Triandis’ interpersonal behavior theory 36 which postulates that individuals’ behavioral intention is influenced by their beliefs toward the behavior.
Hypothesis 7 (confirmed). The study's final finding lies in the positive and significant path coefficient (β = 0.34, P < 0.001) that confirms the influence of medical students’ dHealth education needs on their intention to integrate dHealth in their practice. This finding is in line with prior TAM 41 and UTAUT (unified theory of acceptance and use of technology) research. 58
Causal analysis at t1
As depicted in Figure 3, the causal paths inferred from the research model were tested anew at t1 by assessing the path coefficients (β) estimated by the SEM procedure. As indicated by the strength and significance of the βs and the proportion of explained variance, the performance of the theoretical model was found in the replication study to be superior to that of the initial study (R2t0 = 0.53 vs. R2t1 = 0.69). These results provide further confirmation of the validity and predictive ability of our theoretical model. Moreover, the advent of the COVID-19 pandemic appears to have had no impact on the theorized relationships between the research constructs, as replicating the causal analysis produced results similar to those observed at t0, that is, in terms of the strength and significance of these relationships. The reader may thus essentially refer to the above presentation of the causal analysis at t0 for further analysis of the t1 results.
Figure 3.
Causal analysis results at t1.
Discussion
Principal findings
The present study provides a clear and concise explanation of medical students’ intention to integrate dHealth technologies into their practice. We found the sampled students, especially those who are in their preparatory or preclinical years, to have had little occasion to experiment with dHealth technologies during their medical studies. A plausible explanation might be that during their preclinical years, students do not have direct access to EMRs and other clinical information systems available in hospital settings. The lower scores at t1 might be related to the pandemic where students were even less exposed to hospital practice (and hospital IT systems), with many parts of the curriculum being offered virtually.
This lack of exposure may explain why a vast majority of respondents felt that all medical students should receive dHealth training as part of their formal education. Further, most had strong beliefs about the positive impact of AI-related technologies in the future of medicine, in general, and the progress of various medical disciplines. Importantly, a majority of students declared an intention to integrate dHealth technologies, including AI-based tools, into their medical practice.
The main differences observed between t0 and t1 brings telehealth, and teleconsultation in particular, to the forefront of medical education. Indeed, the pandemic's advent appears to have shifted medical students’ view of telemedicine, now considered to be an important aspect of their dHealth education and future medical practice. Moreover, this shift is made at the expense of another component, basic IT systems (eg, EMRs), that could be now considered as a ‘given’, 59 that is, as being fully and seamlessly integrated within medical education and medical practice.
Last, as predicted by our theoretical model, the combination of three factors (experimentation with dHealth, perceived importance of integrating dHealth into medical curriculum, and beliefs about AI in medicine) explains, in both phases of the study, medical students’ intention to integrate dHealth into their practice.
Study contributions and implications
The factors included in the theoretical model constitute important descriptive, predictive, and explanatory keys upon which to reflect on the issue of dHealth education in medical schools. The proposed model may thus constitute an initial conceptual framework for researchers and practitioners concerned with informing, motivating, and preparing medical students to make effective use of dHealth technologies, in general, and of AI tools, in particular. In this regard, it appears that the emphasis on basic IT systems such as EMRs still remains, whereas telehealth appears to have taken on added importance with the advent of the COVID-19 pandemic. Furthermore, as the students’ future use of dHealth technologies is determined above all by their beliefs about the positive impact of AI on modern medicine, it ensues that the introduction of AI training in medical curricula should be further considered and investigated. 60
This study has several practical implications. For one thing, our study provides medical schools with a conceptual template with which to make a strategic assessment of their dHealth situation and thus obtain actionable insights as to the technologies to be included in the medical curriculum. Our findings also allow us to make a few recommendations to medical schools in Canada and elsewhere wishing to better serve their students through the mindful integration of dHealth within the curriculum: (1) integrate dHealth training as part of the doctorate in medicine; (2) create one or several specialized diplomas in dHealth (eg, telehealth, AI in health); (3) set-up a working group within each faculty of medicine, comprised of professors and students of all levels, to periodically review dHealth training needs in light of existing and emerging technologies; (4) periodically assess students’ satisfaction with their dHealth training, and make the necessary adjustments; and (5) foster collaboration and exchange between medical students and those from other faculties (eg, computer science, software engineering) interested in dHealth technologies through the organization of “hacking health” type of events.
Importantly, our results have implications for key institutional actors in the development and deployment of dHealth technologies in Canada, as they seek to guide and support medical schools in their integration of these technologies within the medical curriculum. For instance, the Association of Faculties of Medicine of Canada (AFMC) and the Canadian Medical Association (CMA) could collaborate on developing and implementing an evidence standards framework for dHealth technologies, like the one developed in the United Kingdom by the National Institute for Health and Care Excellence. 61 This framework would enable a more agile evaluation of these technologies in medical school settings, as well as render them more meaningful to students and add value to dHealth education.
Study limitations and suggestions for future research
The results of this study must be interpreted with caution due to its inherent limitations. Given the nature of the sample, its representativeness in relation to all Canadian medical students limits the scope of these results. Future research could investigate the nature and scope of dHealth education offered in medical schools located elsewhere in Canada as well as in other countries and compare students’ level of proficiency in dHealth as well as their intention to integrate dHealth technologies in their medical practice. It would also be important to conduct a follow-up survey once the COVID-19 pandemic is behind us. Moreover, the rather low response rate may have induced a non-response bias that is hard to evaluate. 62 Notwithstanding our aim for parsimony, the theoretical model could also be extended in future research by including other variables such as social influence and effort expectancy to be more comparable to the previously cited behavioral studies. Further, one could include, in addition to dHealth technologies and applications, the IT-enabled medical knowledge management capabilities such as e-healthcare intelligence and e-collaboration that students must develop to practice modern medicine and, hence, be both innovative and productive.63,64
Conclusions
This study provides a better understanding of the factors predicting medical students’ intention to integrate dHealth into their medical practice. Based upon a multi-theory behavioral model, it reveals the specific dHealth technologies and applications that could be inserted in the medical curriculum to encourage and facilitate students’ adoption of these technologies. Medical schools and faculties are asked to do more and better about preparing their students for the effective use of dHealth in their medical practice. It thus behooves them to develop their dHealth education resources and capabilities in coherence with this imperative.
Acknowledgements
We would like to thank Jean-François Echelard, François Méthot, Hue-Anh Nguyen, and David Lord for their assistance with the pre-test of the survey questionnaire. Our thanks are also extended to the UM medical student association for its valuable assistance with data collection.
Appendix I. Questionnaire content and descriptive statistics.
Table A1.
Level of experimentation with dHealth technologies.
| dHealth technology bundle | dHealth technologies and applications | Pre-COVID-19 (t0) | Peri-COVID-19 (t1) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 or 3 | 4 or 5 | Mean | 1 | 2 or 3 | 4 or 5 | Mean | ||
| Basic IT systems a | Interoperable electronic health record (iEHR) system c | 48% | 33% | 19% | 2.2 | 62% | 31% | 7% | 1.6 |
| Electronic medical record (EMR) systems | 57% | 23% | 23% | 2 | 72% | 20% | 8% | 1.5 | |
| Clinical information systems (CIS) | 56% | 23% | 29% | 1.9 | 75% | 21% | 4% | 1.4 | |
| Interoperable personal health record (iPHR) system d | 71% | 26% | 26% | 1.4 | 79% | 20% | 1% | 1.3 | |
| Interoperable medical appointment system (iMAS) e | 78% | 19% | 19% | 1.3 | 83% | 16% | 1% | 1.2 | |
| TeleHealth a | Teleconsultation | 83% | 17% | 0% | 1.2 | 54% | 43% | 3% | 1.7 |
| Tele-expertise | 90% | 9% | 1% | 1.1 | 80% | 18% | 2% | 1.3 | |
| AI-related technologies a | Artificial intelligence | 71% | 27% | 2% | 1.4 | 80% | 18% | 2% | 1.3 |
| Machine learning | 86% | 13% | 1% | 1.2 | 90% | 9% | 1% | 1.1 | |
| Big data in healthcare | 86% | 13% | 1% | 1.2 | 93% | 7% | 0% | 1.1 | |
| Advanced dHealth a | Robotics in healthcare | 69% | 30% | 1% | 1.4 | 81% | 18% | 1% | 1.2 |
| Virtual reality | 84% | 13% | 3% | 1.3 | 88% | 12% | 0% | 1.1 | |
| Nanotechnology | 86% | 13% | 1% | 1.2 | 91% | 9% | 0% | 1.1 | |
| Augmented reality | 87% | 11% | 2% | 1.2 | 91% | 9% | 0% | 1.1 | |
| 3D printing | 83% | 16% | 1% | 1.2 | 88% | 12% | 0% | 1.1 | |
| Internet of things | 90% | 9% | 1% | 1.1 | 94% | 5% | 1% | 1.1 | |
| Blockchain | 91% | 8% | 1% | 1.1 | 96% | 4% | 0% | 1 | |
| Mobile applications b | UpToDate | 48% | 20% | 32% | 2.5 | 57% | 27% | 16% | 1.9 |
| INESSS (Quebec HTA Institute's mobile app) | 42% | 36% | 22% | 2.3 | 51% | 35% | 14% | 2 | |
| Medscape | 52% | 36% | 12% | 1.9 | 67% | 27% | 6% | 1.6 | |
| Lanthier | 70% | 15% | 15% | 1.7 | 86% | 8% | 6% | 1.3 | |
| MedCalc | 73% | 19% | 8% | 1.6 | 84% | 14% | 2% | 1.2 | |
| BMJBestPractice | 75% | 19% | 6% | 1.5 | 83% | 15% | 2% | 1.3 | |
5-point scales [1 = never exposed to the technology, 2, 3 = somewhat exposed, 4, 5 = very exposed].
5-point scales [1 = application never used, 2, 3 = used rarely or regularly, 4, 5 = used often or very often] – Only the top-6 apps are shown here.
Named « Dossier Santé Québec » in French.
Named « Carnet Santé Québec » in French.
Named « Rendez-vous Santé Québec » in French.
Table A2.
Perceived importance of dHealth in the medical curriculum.
| dHealth technology bundle | dHealth technologies | Pre-COVID-19 (t0) | Peri-COVID-19 (t1) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 or 3 | 4 or 5 | Mean | 1 | 2 or 3 | 4 or 5 | Mean | ||
| Basic IT systems a | Interoperable electronic health record (iEHR) system b | 0% | 24% | 76% | 4.2 | 0% | 33% | 67% | 4.1 |
| Electronic medical record (EMR) systems | 0% | 24% | 76% | 4.2 | 0% | 31% | 69% | 4.1 | |
| Clinical information systems (CIS) | 1% | 27% | 72% | 4.1 | 0% | 37% | 63% | 4 | |
| Interoperable personal health record (iPHR) system b | 1% | 32% | 67% | 3.9 | 0% | 36% | 64% | 4 | |
| Interoperable medical appointment system (iMAS) d | 0% | 27% | 73% | 4 | 0% | 35% | 65% | 4 | |
| TeleHealth a | Teleconsultation | 2% | 43% | 55% | 3.7 | 0% | 29% | 71% | 4.2 |
| Tele-expertise | 2% | 51% | 47% | 3.6 | 0% | 35% | 65% | 4 | |
| AI-related technologies a | Artificial intelligence | 1% | 43% | 56% | 3.7 | 1% | 48% | 51% | 3.6 |
| Machine learning | 2% | 57% | 41% | 3.5 | 1% | 59% | 40% | 3.5 | |
| Big data in healthcare | 3% | 65% | 32% | 3.4 | 1% | 68% | 31% | 3.4 | |
| Advanced technologies a | Robotics | 1% | 45% | 54% | 3.7 | 1% | 43% | 56% | 3.8 |
| virtual reality | 1% | 63% | 36% | 3.4 | 2% | 67% | 31% | 3.3 | |
| Nanotechnology | 3% | 60% | 37% | 3.4 | 3% | 64% | 33% | 3.4 | |
| Augmented reality | 2% | 65% | 33% | 3.3 | 2% | 67% | 31% | 3.3 | |
| 3D printing | 4% | 62% | 34% | 3.3 | 1% | 63% | 36% | 3.4 | |
| Internet of things | 2% | 70% | 28% | 3.3 | 2% | 73% | 25% | 3.1 | |
| Blockchain | 5% | 73% | 22% | 3.1 | 4% | 76% | 20% | 3.1 | |
5-point Likert scales [1 = totally disagree, 2, 3 = neither disagree nor agree, 4, 5 = totally agree].
Named « Dossier Santé Québec » in French.
Named « Carnet Santé Québec » in French.
Named « Rendez-vous Santé Québec » in French.
Table A3.
Beliefs about the impact of AI on medicine.
| Pre-COVID-19 (t0) | Peri-COVID-19 (t1) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 or 3 | 4 or 5 | Mean | 1 | 2 or 3 | 4 or 5 | Mean | ||
| On the medical profession a | Prevention of diseases | 0% | 42% | 58% | 3.7 | 0% | 47% | 53% | 3.6 |
| Diagnosis of diseases | 1% | 29% | 70% | 3.9 | 0% | 41% | 59% | 3.7 | |
| Treatment of diseases | 0% | 39% | 61% | 3.8 | 0% | 45% | 55% | 3.7 | |
| Prognosis of diseases | 0% | 45% | 55% | 3.7 | 0% | 51% | 49% | 3.6 | |
| Doctor-patient relationship | 8% | 80% | 12% | 2.7 | 2% | 85% | 13% | 2.8 | |
| On the medical specialties b | Anatomopathology | 1% | 46% | 53% | 3.7 | 0% | 54% | 46% | 3.7 |
| Radiology | 0% | 32% | 68% | 4.2 | 0% | 41% | 59% | 4 | |
| Dermatology | 2% | 59% | 39% | 3.4 | 0% | 70% | 30% | 3.3 | |
| Ophthalmology | 1% | 49% | 50% | 3.6 | 1% | 58% | 41% | 3.5 | |
| Urgent care and critical care | 1% | 67% | 32% | 3.3 | 1% | 68% | 31% | 3.2 | |
| Family medicine | 2% | 67% | 31% | 3.2 | 1% | 75% | 24% | 3.2 | |
| Internal medicine | 1% | 59% | 40% | 3.4 | 0% | 66% | 34% | 3.3 | |
| Psychiatry | 13% | 78% | 9% | 2.5 | 7% | 30% | 63% | 2.6 | |
| Surgery | 0% | 54% | 46% | 3.6 | 1% | 56% | 43% | 3.6 | |
| 1 | 2 | 1 | 2 | ||||||
| On medical students’ future practice c | Analyze radiological images | 89% | 11% | 97% | 3% | ||||
| Analyze photographical images | 87% | 13% | 91% | 9% | |||||
| Analyze pathological images | 84% | 16% | 86% | 14% | |||||
| Make diagnoses with regard to patients | 59% | 41% | 67% | 33% | |||||
| Make prognoses with regards to patients | 70% | 30% | 87% | 13% | |||||
| Determine patient care protocols | 74% | 26% | 76% | 24% | |||||
| Analyze anamnesis data and form a medical opinion | 55% | 45% | 57% | 43% | |||||
| Supervise and evaluate exchanges with patients | 29% | 71% | 34% | 66% | |||||
5-point scales [1 = very negative effect of AI and ML, 2, 3 = slight negative or no effect, 4, 5 = positive or very positive effect].
5-point scales [1 = unaffected by AI and ML, 2, 3 = uncertain, 4, 5 = affected or very affected by AI and ML].
2-point-scales [1 = yes, 2 = no].
Table A4.
Intention to integrate dHealth in one's own medical practice.
| Pre-COVID-19 (t0) | Peri-COVID-19 (t1) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 or 3 | 4 or 5 | Mean | 1 | 2 or 3 | 4 or 5 | Mean | ||
| For patient communication and consultation a | Use an online medical appointment platform | 20% | 10% | 70% | 3.7 | 32% | 9% | 59% | 3.4 |
| Do virtual consultations with patients | 22% | 52% | 26% | 2.7 | 32% | 9% | 59% | 3.2 | |
| Communicate by email or SMS with patients | 22% | 36% | 42% | 3 | 34% | 20% | 46% | 2.9 | |
| Communicate by email or SMS with other physicians | 17% | 3% | 78% | 4 | 32% | 1% | 67% | 3.6 | |
| For patient monitoring and follow-up a | Prescribe mobile applications to patients | 20% | 28% | 52% | 3.2 | 33% | 21% | 46% | 2.9 |
| Recommend reliable and secure websites to patients | 20% | 7% | 73% | 3.8 | 32% | 22% | 46% | 3.5 | |
| Prescribe connected medical devices (objects) to patients | 21% | 41% | 38% | 3.8 | 34% | 27% | 39% | 2.8 | |
| Use smart medical devices to assess patients’ health | 21% | 28% | 51% | 3.3 | 33% | 13% | 54% | 3.1 | |
| For disease prevention, diagnosis and treatment a | Solicit second opinions via a tele-expertise platform | 19% | 18% | 63% | 3.5 | 32% | 9% | 59% | 3.3 |
| Consult medical websites to assist me in my practice | 17% | 1% | 80% | 4.1 | 32% | 1% | 67% | 3.6 | |
| Use mobile applications to assist me in my practice | 19% | 3% | 78% | 4 | 31% | 20% | 49% | 3.5 | |
| Use systems based on AI algorithms to assist me in my practice | 20% | 33% | 47% | 3.2 | 33% | 23% | 44% | 2.9 | |
5-point scales [1 = very improbable, 2 = improbable, 3 = uncertain, 4 = probable, 5 = very probable].
Facts and Factors (2021). Available at: https://www.globenewswire.com/en/news-release/2021/09/02/2290548/0/en/Global-Report-on-Digital-Health-Market-Size-Valuation-Will-Reach-to-USD-220-94-Billion-by-2026-According-to-Facts-Factors.html.
See https://www.canada.ca/en/health-canada/services/drugs-health-products/medical-devices/activities/announcements/notice-digital-health-technologies.html and https://www.fda.gov/medical-devices/digital-health.
Called INESSS.
Footnotes
Conflict of interest: The authors have no conflicts of interest to declare.
Contributorship: GP and MPP contributed equally to the conception and design of the study. The literature review was performed by LR, AC, and AGO. Data collection was under the responsibility of GP, MPP, and GG. Data analyses were performed by LR and GP. All authors contributed to the writing of the manuscript.
Ethical approval: The ethics committee of the University of Montreal approved this study (REC number: CERSES-19-108-D).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: GP.
ORCID iDs: Guy Paré https://orcid.org/0000-0001-7425-1994
Louis Raymond https://orcid.org/0000-0003-1631-8171
Peer review: XXXXXXXXXXXXXXXX.
References
- 1.Fatehi F, Samadbeik M, Kazemi A. What is digital health? Review of definitions. Stud Health Technol Inf 2020; 275: 67–71. [DOI] [PubMed] [Google Scholar]
- 2.Brewer LC, Fortuna KL, Jones Cet al. et al. Back to the future: achieving health equity through health informatics and digital health. JMIR Mhealth Uhealth 2020; 8: e14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leatherdale ST, Lee J. Artificial intelligence (AI) and cancer prevention: the potential application of AI in cancer control programming needs to be explored in population laboratories such as COMPASS. Cancer Causes Control 2019; 30: 671–675. [DOI] [PubMed] [Google Scholar]
- 4.Islam SMS, Maddison R. Digital health approaches for cardiovascular diseases prevention and management: lessons from preliminary studies. Mhealth 2021; 7: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paré G, Poba-Nzaou P, Sicotte Cet al. et al. Comparing the costs of home telemonitoring and usual care of chronic obstructive pulmonary disease patients: a randomized controlled trial. Eur Res Telemed 2013; 2: 35–47. [Google Scholar]
- 6.Lemelin A, Paré G, Bernard Set al. et al. Demonstrated cost-effectiveness of a telehomecare program for gestational diabetes mellitus management. Diabetes Tech Ther 2020; 22: 195–202. [DOI] [PubMed] [Google Scholar]
- 7.Jaana M, Paré G, Sicotte C. Home telemonitoring for respiratory conditions: a systematic review. Am J Manage Care 2009; 15: 313–320. [PubMed] [Google Scholar]
- 8.Kitsiou S, Vatani H, Paré Get al. Effectiveness of mobile health technology interventions for patients with heart failure: systematic review and meta-analysis. Can J Cardiol 2021; 37: 1248–1259. [DOI] [PubMed] [Google Scholar]
- 9.Lussier M, Aboujaoudé A, Couture Met al. Using ambient assisted living to monitor older adults with Alzheimer disease: single-case study to validate the monitoring report. JMIR Med Inform 2020; 8: e20215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bier N, Couture M, Tannou T, et al. Smart environments in support of fragile and isolated older adults: protocol for the city of Côte-Saint-Luc's living lab. In: Biostec 2022, virtual conference, paper #3, February 9–11, 2022.
- 11.Paré G, Sicotte C, Moreault M Pet al. et al. Mobile computing and the quality of home care nursing practice. J Telemed Telecare 2011; 17: 313–317. [DOI] [PubMed] [Google Scholar]
- 12.Raymond L, Maillet É, Trudel M Cet al. et al. Advancing laboratory medicine in hospitals through health information exchange: a survey of specialist physicians in Canada. BMC Med Inform Decis Mak 2020; 20: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paré G, Raymond L, Castonguay Aet al. et al. Assimilation of medical appointment scheduling systems and their impact on the accessibility of primary care: mixed methods study. JMIR Med Inform 2021; 9: e30485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panahiazar M, Taslimitehrani V, Jadhav A, et al. Empowering personalized medicine with big data and semantic web technology: promises, challenges, and use cases. In: 2014 IEEE Int Conf Big Data (Big Data), 790–795. [DOI] [PMC free article] [PubMed]
- 15.Hoeyer K. Data as promise: reconfiguring danish public health through personalized medicine. Soc Stud Sci 2019; 49: 531–555. [DOI] [PubMed] [Google Scholar]
- 16.Wong A, Bhyat R, Srivastava Set al. et al. Patient care during the COVID-19 pandemic: use of virtual care. J Med Internet Res 2021; 23: e20621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mihalj M, Carrel T, Gregoric IDet al. Telemedicine for preoperative assessment during a COVID-19 pandemic: recommendations for clinical care. Best Pract Res Clin Anaesthesiology 2020; 34: 345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vossen K, Rethans JJ, van Kuijk SMet al. et al. Understanding medical students’ attitudes toward learning eHealth: questionnaire study. JMIR Med Educ 2020; 6: e17030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ 2019; 5: e12515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng DR, Scodellaro T, Uahwatanasakul Wet al. et al. An electronic medical record in pediatric medical education: survey of medical students' expectations and experiences. Appl Clin Inform 2018; 9: 809–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herrmann-Werner A, Holderried M, Loda Tet al. et al. Navigating through electronic health records: survey study on medical students’ perspectives in general and with regard to a specific training. JMIR Med Inform 2019; 7: e12648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walker C, Echternacht H, Brophy PD. Model for medical student introductory telemedicine education. Telemed e-Health 2019; 25: 717–723. [DOI] [PubMed] [Google Scholar]
- 23.Cheng CT, Chen CC, Fu CYet al. Artificial intelligence-based education assists medical students’ interpretation of hip fracture. Insights Imaging 2020; 11: 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chandrashekar P. A digital health preclinical requirement for medical students. Acad Med 2019; 94: 749. [DOI] [PubMed] [Google Scholar]
- 25.Gaglani SM, Topol EJ. Imeded: the role of mobile health technologies in medical education. Acad Med 2014; 89: 1207–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forman TM, Armor DA, Miller AS. A review of clinical informatics competencies in nursing to inform best practices in education and nurse faculty development. Nurs Educ Perspect 2019; 41: e3–e7. [DOI] [PubMed] [Google Scholar]
- 27.Lam MK, Hines M, Lowe Ret al. et al. Preparedness for eHealth: health sciences students’ knowledge, skills, and confidence. J Inf Technol Educ: Res 2016; 15: 305–334. [Google Scholar]
- 28.Mostaghimi A, Olszewski AE, Bell SKet al. et al. Erosion of digital professionalism during medical students’ core clinical clerkships. JMIR Med Educ 2017; 3: e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edirippulige S, Gong S, Hathurusinghe Met al. Medical students’ perceptions and expectations regarding digital health education and training: a qualitative study. J Telemed Telecare 2022; 28: 258–265. [DOI] [PubMed] [Google Scholar]
- 30.Echelard JF, Méthot F, Nguyen HAet al. et al. Medical student training in eHealth: scoping review. JMIR Med Educ 2020; 6: e20027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Car LT, Kyaw BM, Panday RSNet al. et al. Digital health training programs for medical students: scoping review. JMIR Med Educ 2021; 7: e28275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sit C, Srinivasan R, Amlani Aet al. et al. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: a multicentre survey. Insights Imaging 2020; 11: 7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yaghobian S, Ohannessian R, Iampetro Tet al. Knowledge, attitudes and practices of telemedicine education and training of French medical students and residents. J Telemed Telecare 2022; 28: 248–257. [DOI] [PubMed] [Google Scholar]
- 34.Pathipati AS, Azad TD, Jethwani K. Telemedical education: training digital natives in telemedicine. J Med Internet Res 2016; 18: e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Machleid F, Kaczmarczyk R, Johann Det al. Perceptions of digital health education among European medical students: mixed methods study. J Med Internet Res 2020; 22: e19827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Almohtadi A, Van M, Seyedzenouzi G. Medical students respond: question precision and gender differentiation. Comment on “understanding medical students’ attitudes toward learning eHealth: questionnaire study”. JMIR Med Educ 2021; 7: e24993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health Care Inf 2020; 27: e100166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Triandis HC. Values, attitudes, and interpersonal behavior. In: Nebraska symposium on motivation 1979: beliefs, attitudes and values, Lincoln, Nebraska: University of Nebraska Press, 1980, pp.195–259. [PubMed] [Google Scholar]
- 39.Banerjee R, George P, Priebe Cet al. et al. Medical student awareness of and interest in clinical informatics. J Am Med Inform Assoc 2015; 22: e42–e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aungst TD, Patel R. Integrating digital health into the curriculum – considerations on the current landscape and future developments. J Med Educ Curricular Dev 2020; 7: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 1989; 13: 319–340. [Google Scholar]
- 42.Venkatesh V. Determinants of perceived ease of use: integrating control, intrinsic motivation, and emotion into the technology acceptance model. Inf Syst Res 2000; 11: 342–365. [Google Scholar]
- 43.Ngai EWT, Poon JKJ, Chan YHC. Empirical examination of the adoption of WebCT using TAM. Comput Educ 2007; 48: 250–267. [Google Scholar]
- 44.Teo T. Examining the influence of subjective norm and facilitating conditions on the intention to use technology among pre-service teachers: a structural equation modeling of an extended technology acceptance model. Asia Pac Educ Rev 2010; 11: 253–262. [Google Scholar]
- 45.Paré G, Elam JJ. Discretionary use of personal computers by knowledge workers: testing of a social psychology theoretical model. Behav Inf Technol 1995; 14: 215–228. [Google Scholar]
- 46.Bergeron F, Raymond L, Rivard Set al. et al. Determinants of EIS use: testing a behavioral model. Decis Support Syst 1995; 14: 131–146. [Google Scholar]
- 47.Haluza D, Wernhart A. Does gender matter? Exploring perceptions regarding health technologies among employees and students at a medical university. Int J Med Inf 2019; 130: 103948. [DOI] [PubMed] [Google Scholar]
- 48.Gefen D, Ringdon EE, Straub D. An update and extension to SEM guidelines for administrative and social science research. MIS Q 2011; 35: iii–xiv. [Google Scholar]
- 49.Ouimet A G, Wagner G, Raymond Let al. et al. Investigating patient continuance of teleconsultation to anticipate post-crisis momentum: survey study. J Med Internet Res 2020; 22: e22081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roberts N, Thatcher J. Conceptualizing and testing formative constructs: tutorial and annotated example. SIGMIS Database 2009; 40: 9–39. [Google Scholar]
- 51.Diamantopoulos A, Siguaw J. Formative vs. Reflective indicators in organizational measure development: a comparison and empirical illustration. Br J Manage 2006; 17: 263–282. [Google Scholar]
- 52.Hair JF, Hult GTM, Ringle CMet al. et al. A primer on partial least squares structural equation modeling (PLS-SEM). Second Edition. Thousand Oaks, California: Sage Publications, 2017. [Google Scholar]
- 53.Powers P. Québec’s e-health journey – assessing the path forward. Electron Healthcare 2012; 10: e30–e44. [Google Scholar]
- 54.Podsakoff PM, MacKenzie SB, Lee JYet al. et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol 2003; 88: 879–903. [DOI] [PubMed] [Google Scholar]
- 55.Pavlou PA, Liang H, Xue Y. Understanding and mitigating uncertainty in online exchange relationships: a principal–agent perspective. MIS Q 2007; 31: 105–136. [Google Scholar]
- 56.Lowry PB, Gaskin J. Partial least squares (PLS) structural equation modeling (SEM) for building and testing behavioral causal theory: when to choose it and how to use it. IEEE Trans Prof Commun 2014; 57: 123–146. [Google Scholar]
- 57.Ringle CM, Sarstedt M, Straub D. A critical look at the use of PLS-SEM in MIS quarterly. MIS Q 2012; 36: iii–xiv. [Google Scholar]
- 58.Venkatesh V, Thong JYL, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Q 2012; 36: 157–178. [Google Scholar]
- 59.Carr NG. IT Doesn’t matter. Harv Bus Rev 2003; 81: 41–49. [PubMed] [Google Scholar]
- 60.Dos Santos D P, Giese D, Brodehl Set al. et al. Medical students' attitude towards artificial intelligence: a multicentre survey. Eur Radiol 2019; 29: 1640–1646. [DOI] [PubMed] [Google Scholar]
- 61. NICE . Evidence standards framework for digital health technologies. London, UK: National Institute for Health and Care Excellence. www.nice.org.uk/Media/Default/About/what-we-do/our-programmes/evidence-standards-framework/digital-evidence-standards-framework.pdf (2019, accessed 14 January 2022). [Google Scholar]
- 62.Phillips AW, Friedman BT, Utrankar Aet al. et al. Surveys of health professions trainees: prevalence, response rates, and predictive factors to guide researchers. Acad Med 2017; 92: 222–228. [DOI] [PubMed] [Google Scholar]
- 63.Brunner M, McGregor D, Keep Met al. An eHealth capabilities framework for graduates and health professionals: mixed-methods study. J Med Internet Res 2018; 20: e10229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Raymond L, Paré G, Maillet E. IT-based clinical knowledge management in primary health care: a conceptual framework. Knowl Process Manage 2017; 24: 247–256. [Google Scholar]