Abstract
Introduction:
Post-stroke physical activity (PA) has widespread health benefits. Environmental exposures may shape post-stroke PA behavior. This study investigates relationships between environmental exposures and post-stroke PA.
Methods:
Stroke survivors (N=374) from a cohort of Black and White adults, with post-stroke accelerometer data (2009-2013) were eligible for the current study. Participants’ home addresses were linked with secondary data to capture environmental characteristics, including annual density of neighborhood resources (e.g. parks, PA facilities, and intellectual stimulation destinations), 2010 neighborhood socioeconomic status (nSES), 2010 neighborhood crime, and daily information on extreme cold days. Post-stroke light PA (LPA) and moderate to vigorous PA (MVPA) were captured using accelerometers over a 7-day period. Linear regression and two-part/hurdle models were used to estimate the relationship between density of neighborhood resources with LPA and MVPA, respectively. Analyses were conducted in 2021.
Results:
A 10% increase in the number of extreme cold days was associated with 6.37 fewer minutes of daily LPA (95% CI:−11.37, −1.37). A one-standard deviation increase in nSES was associated with greater odds (OR=1.10; 95% CI:1.02, 1.19) of doing any MVPA. Among participants obtaining any MVPA, a one-unit (count/km2) increase in destinations for intellectual stimulation was associated with 0.99 (95% CI:0.02, 1.97) more minutes of daily MVPA. All other environmental exposures were not associated with post-stroke LPA or MVPA.
Conclusions:
Environmental exposures may facilitate PA participation among stroke survivors. This study found that weather, nSES, and proximity to destinations for intellectual stimulation were associated with PA over and above individual factors.
Introduction
PA is an important component of rehabilitation after stroke due to the widespread benefits including physical,1-4 cognitive,5 and emotional health.6-8 Previous research suggests that exercise and PA post-stroke is protective of bone health,1 walking ability,2 fatigue,3 and muscle strength.4 Furthermore, low levels of PA post-stroke are associated with risk for recurrent stroke and cardiovascular disease.9-11 Stroke survivors have previously indicated that neighborhood resources are important for PA post-stroke.12-14 PA facility access is associated with a greater number of steps taken post-stroke14 and traveling far distances to PA facilities serves as a primary barrier to exercise post-stroke.13 Additionally, retail and service destinations within the neighborhood environment can serve as motivating factors for active transportation (e.g. walking or biking).15-17 Walking long distances, including to public transportation, has been reported as a challenge for community mobility post-stroke.18-23 Thus, access to transportation is an important feature to encourage mobility and participation post-stroke.12, 24
Environmental characteristics are important determinants of population health.25 However, very little is known of the role of environmental exposures for community-dwelling stroke survivors, estimated to represent 7.0 million Americans over the age of 20.26 Previous research found that neighborhood walkability was not associated with post-stroke daily stepping.27 However, this study was limited in geographic variability, did not account for the role of weather, and it is unclear if the assessment of neighborhood walkability preceded measurement of post-stroke walking.27 Targeting physical and social resources intervenes on structural factors associated with health and provides the context through which post-stroke physical activity takes place.28 Additional research is needed to examine the role of physical and social resources on objectively measured post-stroke PA behavior.
This study cross-sectionally examined the relationship between density of neighborhood resources with post-stroke PA. Neighborhood resources selected within this study overlap with the American Heart Association’s recommendation of built environment strategies to increase physical activity in the general population.28 It was hypothesized that greater density of neighborhood resources would be associated with more post-stroke PA. In a sample of stroke survivors with wide geographic variability, this project overcomes many limitations of previous research by integrating objectively measured community characteristics, data on outdoor climate, and objectively measured PA.
Methods
Study Population
The REasons for Geographic and Racial Differences in Stroke (REGARDS) is a national, population-based study which began in January 2003.29 REGARDS is a prospective cohort of 30,239 Black and White participants who continue to be followed for incident stroke.29 Participants were randomly sampled from commercially available lists and oversampled from the south-eastern United States.29 At baseline, participants self-reported previous stroke events. Prospectively, suspected stroke events were obtained through self-report or proxy report during six-month, follow-up phone calls. Medical records were retrieved for all suspected stroke cases and adjudicated by a physician panel. A total of 3,047 stroke survivors (1,921 self-reported stroke events, 1,126 physician adjudicated stroke events) were within the study cohort at the time of accelerometer data collection.
Accelerometer Data Collection
20,557 REGARDS participants were screened for eligibility in an ancillary study to objectively capture PA using accelerometers from May 2009 to January 2013. Participants were eligible for the accelerometer ancillary study if they answered “yes” to the question “on a typical day, are you physically able to go outside where you live and walk, whether or not you actually do?” The majority of REGARDS participants were eligible and invited to participate (n=20,076, 97.7%).30 Among participants invited, 60.5% agreed to participate, 36.4% declined, and 3.1% deferred enrollment.30 Most demographic characteristics did not meaningfully differ between participants who agreed versus declined participation.30 Among participants agreeing to the ancillary study, 407 post-stroke participants had usable accelerometer data collected after their stroke event (Figure 1). Additional details on study design, sampling strategy, recruitment, and study procedures have been previously described.30, 31
Figure 1. Analytic study sample flowchart.
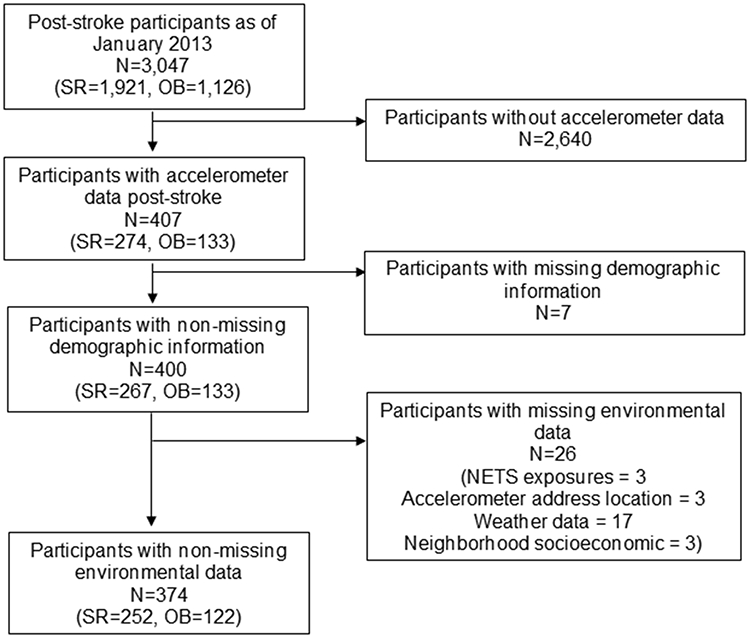
Analytic sample from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study, United States, May 2009 to January 2013. SR = Self-reported a stroke at baseline REGARDS; OB = Stroke was observed during the REGARDS study period prior to accelerometer data collection
Objective light PA (LPA) and moderate to vigorous PA (MVPA) were captured using Actical accelerometers. Participants wore the accelerometer over their right hip and completed a daily wear log over a seven-day period. Hip-worn Actical accelerometers have excellent retest reliability among post-stroke populations in a community setting.32,33 Actical devices were initialized to collect data in 60s epochs. Activity counts of 50-1,064 counts per minute (cpm) and >1,065 cpm distinguished LPA and MVPA, respectively. Cut-points were informed by a laboratory-based validation study among older adult34 with transferability to stroke survivors.35 Daily minutes of LPA and MVPA were summed across valid wear days (≥four days with ≥ten waking hours) and divided by the number of valid days to calculate average daily minutes of LPA and MVPA.36,37
Individual Characteristics
Information collected on individual participant characteristics was obtained from the REGARDS baseline data collection. A computer-assisted telephone interview was completed to obtain demographic (i.e. age, sex, race, region) and socioeconomic characteristics (i.e. education, income) of participants. Time since stroke was calculated from self-reported year of stroke at baseline (n=274) or from the date of observed stroke within the REGARDS study (n=133).
Geospatial Procedures
Participants’ home addresses were identified during initial enrollment, follow-up phone calls, and/or annual mailings. Addresses were updated through regular mailings, a public record database (i.e. LexisNexis)38,39, and ancillary study contacts. Participants’ home addresses were geocoded using Environmental Systems Research Institute (Esri) ArcGIS® Business Analyst Desktop 10.5.1 with Esri 2016 Business Analyst Data. The address at the time of accelerometer wear was utilized, and participants missing a geocoded address were excluded (n=3; Figure 1).
Environmental Characteristics
Population Density
Using block-level 2010 Decennial Census population data and block geographies from the US Census Bureau, a weighted population count was generated within a 1 km radial buffer surrounding each participant’s home address.40 Population density was estimated using areal weighting interpolation to assign population data to geographies.41 Using block geographies, the population in proportion to the land area (units: 100 people/km2) was calculated within the buffer (range: 0.02 to 187.07).
Park Area
Local, state, and national park area was calculated by triangulating three sources of data: Esri StreetMap Premium, Esri Living Atlas, and ParkServe®. After excluding water, each park layer was dissolved into one combined layer to account for overlapping parks across the data sources. Proportion of park area in 2016 was calculated within a 1 km radial buffer (range: 0 to 0.77).
Neighborhood Retail Environments
The annual number of neighborhood retail establishments was obtained from the National Establishment Time Series (NETS) database. To capture buildings set back from the street, research staff calculated a 1 km sausage buffer using a 0.85 km network distance with a 150 m radius from the street centerline.42 Counts of NETS establishments geocoded at the address point or street address range level were included in exposure calculation. The year of NETS exposures was determined by the year of participant accelerometry data collection.
Previous research has defined categories of NETS retail establishments that potentially impact PA behavior.43 Using Standard Industrial Classification (SIC) codes and name-based algorithms, NETS retail establishments theorized to impact PA behavior were combined into six categories of environmental exposures43 including: food stores (e.g. farmers markets; range: 0 to 61.64), restaurants and eating places (e.g. coffee shops; range: 0 to 79.12), PA facilities (e.g. gyms/fitness centers; range: 0 to 5.41), department stores (e.g. retail apparel; range: 0 to 1.66), general mass merchandisers (i.e. high volume merchandisers; range: 0 to 0.75), destinations for intellectual stimulation (e.g. libraries; range: 0 to 23.03). Additional details on classification, integration, and quality control of NETS based data have been previously described.43
Public Rail
Subway, light rail, and commuter rail station information was obtained from the Center for Transit-Oriented Development database.44 Information from municipal transit agencies was used to code the year of station service.45 Counts of public rail stations within a 1 km sausage buffer in 2010 were included (range: 0 to 12.67).
Rural-Urban Commuting Area (RUCA) Codes
RUCA codes capture measures of population density, urbanization, and daily commuting to code census tracts into levels of urbanicity.46 Using 2010 RUCA 4, primary and secondary RUCA codes were aggregated into four categories (i.e. urban, large, rural, small rural, isolated).46 Due to small cell size, “small rural” and “isolated” categories were collapsed into one category.
Neighborhood Socioeconomic Status (nSES)
nSES was measured using previously defined methods.47 Briefly, the nSES index variable is the sum of six census variables representing income, occupation, and education from the 2010 American Communities Survey.47 Higher values of this index indicate higher nSES within the census tract (range: −10.10 to 14.61).
Crime
Using 2010 Esri CrimeRisk Indexes data, crime was separated into personal crime (e.g. murder; range: 2.60 to 692.58) and property crime (e.g. motor vehicle theft; range: 1.52 to 624.65). An index of 100 is considered the national average, with higher index scores representing greater amounts of crime. Using a 1 km modified sausage buffer, crime risk was estimated using areal weighting interpolation to assign CrimeRisk Indexes to geographies.41 The modified sausage buffer differs from the sausage buffer, in that all space fully enclosed by the buffered area is included.42
Extreme Cold Days
Data on extreme cold days were derived from the Global Historical Climatology Network-Daily dataset integrating daily climate observations from multiple sources.48 Weather station geocodes were downloaded and spatially joined to 2010 US County shapefiles. Extreme cold temperatures were defined as county temperatures below the 5th percentile of all days over the past year within the county. The variable of “extreme cold days” captures the 10 percent change of days, during the accelerometer wear days with extremely cold temperatures (range: 0 to 10). This study examined extreme cold temperatures because of the established relationship between cold climate and post-stroke spasticity.49
Statistical Analysis
Minutes per day spent in LPA was approximately normally distributed within the study sample. Therefore, LPA was treated as a continuous outcome within a linear regression model. MVPA was right skewed within the study population with a large proportion (20.1%) obtaining 0 minutes of MVPA. Therefore, a two-part/hurdle model was used to examine the association (1) between individual and environmental characteristics with obtaining any MVPA using logistic regression and (2) between individual and environmental characteristics with the number of minutes of MVPA using linear regression among participants accumulating any MVPA. Analyses were completed for (1) LPA and (2) MVPA; with MVPA having two parts (2.1) logistic regression and (2.2) linear regression.
Using a sequential model building strategy, this study examined the association of individual characteristics, environmental characteristics, and these models combined. All models controlled for participant wear time. To estimate the severity of multicollinearity of independent variables, variance inflation factor was calculated and reported for all models. All analyses were conducted using Stata 16.1. Participants provided written informed consent to be a part of REGARDS, and this study was approved by all participating Institutional Review Boards.
Results
A total of 374 participants met inclusion criteria (Figure 1). On average, participants accumulated 142.02 minutes of LPA per day and 5.75 minutes of MVPA per day. Participants were on average 73 years (range: 53-94) of age, with 52% male and 37% self-identified as Black. PA measurement was on average 10 years (SD: 8.99) after a participant experienced a stroke. Participants were distributed across socioeconomic measures of education and income. Environmental characteristics were highly variable across the study sample, with 82% of participants living within urban areas. Additional details on descriptive statistics of individual and environmental characteristics can be found in Table 1.
Table 1.
Sample characteristics are reported for the analytic sample (n=374).
| Analytic Samplea (n = 374) |
||
|---|---|---|
| Sample characteristics | Mean | SD |
| Light physical activity (minutes/day) | 142.02 | 74.74 |
| Moderate to vigorous physical activity (minutes/day) | 5.75 | 11.62 |
| Individual characteristics | ||
| Wear Time | 868.54 | 120.27 |
| Age | 72.63 | 8.16 |
| Gender (n, % Male participants) | 195 | 52.14% |
| Race (n, % Black participants) | 139 | 37.17% |
| Time since stroke (years) | 10.04 | 8.99 |
| Education (n, %) | ||
| College graduate or more | 125 | 33.42% |
| Some college | 120 | 32.09% |
| High school graduate | 90 | 24.06% |
| Less than high school | 39 | 10.43% |
| Income | ||
| > $75,000 | 47 | 12.57% |
| $35,000 - $74,999 | 118 | 31.55% |
| $20,000 - $34,999 | 112 | 29.95% |
| < $20,000 | 65 | 17.38% |
| Refused | 32 | 8.56% |
| Environmental characteristics | ||
| Population density (n/km2)b | 12.40 | 16.42 |
| Park area (proportion) | 0.04 | 0.08 |
| Food stores (count/km2) | 2.61 | 4.28 |
| Restaurants and eating places (count/km2) | 2.56 | 5.29 |
| Physical activity facilities (count/km2) | 0.28 | 0.68 |
| Department stores (count/km2) | 0.04 | 0.19 |
| General mass merchandise (count/km2) | 0.01 | 0.07 |
| Intellectual stimulation (count/km2) | 0.93 | 1.94 |
| Public rail (count/km2) | 0.09 | 0.76 |
| RUCA codes (n, %) | ||
| Urban | 306 | 81.82% |
| Large rural | 42 | 11.23% |
| Small rural & isolated | 26 | 6.95% |
| Region (n, %) | ||
| Non-stroke belt/buckle | 185 | 49.47% |
| Stroke belt | 116 | 31.02% |
| Stroke buckle | 73 | 19.52% |
| Neighborhood socioeconomic status | −0.81 | 5.11 |
| Personal crime | 183.85 | 155.16 |
| Property crime | 159.84 | 123.59 |
| Extreme cold daysc | 0.36 | 1.40 |
Note. SD=standard deviation; km=kilometer; RUCA=rural-urban community area
Post-stroke participants from the REasons for Geographic and Racial Differences in Stroke (REGARDS) cohort, who have valid accelerometry data and no missing covariate data.
Summarized in units of 100 people per square kilometer
Summarized in units of 10 percent of days with extremely cold temperatures
Within the individual characteristics model, a one-year increase in age was associated with 3.94 (95% CI:−4.82, −3.05) fewer minutes of LPA per day (Table 2). Black participants accumulated on average 18.58 (95% CI:−33.51, −3.65) fewer minutes of LPA in comparison to White participants. Within the environmental characteristics model, a one-unit increase in the percentage of extreme cold days was associated with 8.33 (95% CI:−13.75, −2.90) fewer minutes of LPA per day. Within the joint individual and environmental characteristics model, age (β=−3.82; 95% CI:−4.73, −2.92), race (β=−21.33; 95% CI:−39.65, −3.02), and extreme cold weather (β=−6.37; 95% CI:−11.37, −1.37) were all significantly associated with lower minutes of LPA. Other environmental exposures examined were not significantly associated with post-stroke LPA behavior.
Table 2.
Individual and environmental characteristics associated with minutes of post-stroke light physical activity (n=374).
| Individual characteristics |
Environmental characteristics |
Individual + Environmental Characteristics |
||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Variables | β | 95% CI | β | 95% CI | β | 95% CI |
| Individual characteristics | ||||||
| Wear Time | 0.06 | (0.005, 0.12) | 0.06 | (0.002, 0.12) | ||
| Age | −3.94 | (−4.82, −3.05) | −3.82 | (−4.73, −2.92) | ||
| Gender (Male participants) | −1.11 | (−15.19, 12.98) | −1.04 | (−15.57, 13.48) | ||
| Race (Black participants) | −18.58 | (−33.51, −3.65) | −21.33 | (−39.65, −3.02) | ||
| Time since stroke (years) | 0.20 | (−0.57, 0.98) | 0.21 | (−0.59, 1.01) | ||
| Education | ||||||
| College graduate or more | - | - | - | - | ||
| Some college | 15.65 | (−1.90, 33.19) | 15.71 | (−2.66, 34.07) | ||
| High school graduate | 14.05 | (−5.37, 33.48) | 16.64 | (−3.90, 37.17) | ||
| Less than high School | 3.90 | (−21.68, 29.48) | 7.85 | (−18.79, 34.48) | ||
| Income | ||||||
| >$75,000 | - | - | - | - | ||
| $35,000 - $74,999 | 5.65 | (−17.96, 29.25) | 9.17 | (−15.01, 33.34) | ||
| $20,000 - $34,999 | −4.13 | (−28.82, 20.55) | 4.10 | (−22.10, 30.31) | ||
| < $20,000 | −17.67 | (−45.33, 10.00) | −10.86 | (−39.69, 17.97) | ||
| Refused | −3.10 | (−35.34, 29.14) | 1.94 | (−30.94, 34.82) | ||
| Environmental characteristics | ||||||
| Population density (n/km2)a | 0.70 | (−0.18, 1.58) | 0.34 | (−0.50, 1.17) | ||
| Park area (proportion) | −25.83 | (−128.19, 76.54) | −8.48 | (−103.40, 86.45) | ||
| Public rail (count/km2) | −1.37 | (−12.36, 9.62) | 0.08 | (−10.04, 10.19) | ||
| Food stores (count/km2) | −2.99 | (−6.58, 0.61) | −1.03 | (−4.37, 2.30) | ||
| Restaurants and eating places (count/km2) | −0.91 | (−3.54, 1.71) | −1.58 | (−3.99, 0.82) | ||
| Physical activity facilities (count/km2) | −2.76 | (−15.94, 10.42) | −0.89 | (−13.02, 11.24) | ||
| Department stores (count/km2) | −1.05 | (−46.48, 44.37) | −0.25 | (−42.09, 41.60) | ||
| General mass merchandise (count/km2) | −36.62 | (−150.41, 77.17) | 25.88 | (−79.18, 130.93) | ||
| Intellectual stimulation (count/km2) | 1.73 | (−3.89, 7.35) | 3.48 | (−1.70, 8.67) | ||
| RUCA codes | ||||||
| Urban | - | - | - | - | ||
| Large rural | 11.68 | (−13.33, 36.70) | 8.62 | (−14.33, 31.56) | ||
| Small rural & isolated | −13.25 | (−45.24, 18.73) | −18.74 | (−48.12, 10.64) | ||
| Region | ||||||
| Non-stroke belt/buckle | - | - | - | - | ||
| Stroke belt | 15.90 | (−4.30, 36.10) | 7.48 | (−11.30, 26.26) | ||
| Stroke buckle | 9.30 | (−13.58, 32.18) | 8.62 | (−13.12, 30.36) | ||
| Neighborhood socioeconomic status | 1.39 | (−0.37, 3.14) | 1.00 | (−0.79, 2.79) | ||
| Personal crime | −0.02 | (−0.09, 0.06) | 0.02 | (−0.05, 0.09) | ||
| Property crime | 0.005 | (−0.09, 0.10) | −0.01 | (−0.10, 0.07) | ||
| Extreme cold daysb | −8.33 | (−13.75, −2.90) | −6.37 | (−11.37, −1.37) | ||
| Mean Variance Inflation Factor | 1.60 | 1.88 | 1.90 | |||
| R-squared | 0.22 | 0.07 | 0.26 | |||
Note. CI=confidence interval; km=kilometer; RUCA=rural-urban community area
Units of 100 people per square kilometer
Units of 10 percent of days with extremely cold temperatures
Table 3 displays results of the two-step/hurdle model estimating associations with MVPA. Within the individual and environmental characteristics model, a one-year increase in age (OR=0.90; 95% CI:0.87, 0.94) and one-standard deviation increase in nSES (OR=1.10; 95% CI:1.02, 1.19) were associated with the likelihood of accumulating any minutes of MVPA. In addition, the odds of males accumulating any minutes of MVPA were 2.36 (95% CI:1.26, 4.41) times the odds of any MVPA among women. Other environmental exposures examined were not significantly associated with the likelihood of participating in post-stroke MVPA. Among participants accumulating any amount of MVPA (n=299), age (β=−0.52; 95% CI:−0.70, −0.34) and Black race (β=−4.05; 95% CI:−7.60, −0.50) were associated with fewer minutes of MVPA per day. Additionally, annual income categories of less than $20,000 (β=−6.46; 95% CI:−12.07, −0.86) and Refused (β=−7.70; 95% CI:−13.96, −1.44) were associated with fewer minutes of MVPA per day in comparison to those earning >$75,000 a year. A one-unit increase in destinations for intellectual stimulation (β=0.99; 95% CI:0.02, 1.97) was associated with more minutes of MVPA, conditional on participating in any MVPA. All other environmental exposure examined were not significantly associated with minutes of post-stroke MVPA.
Table 3.
Individual and environmental characteristics associated with post-stroke moderate to vigorous physical activity (nLogit=374; nLinear=299).
| Individual characteristics | Environmental characteristics | Individual + Environmental Characteristics |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Logit Modela
(n = 374) |
Linear Modelb
(n = 299) |
Logit Modela
(n = 374) |
Linear Modelb
(n = 299) |
Logit Modela
(n = 374) |
Linear Modelb
(n = 299) |
|||||||
|
|
|
|
||||||||||
| Variables | OR | 95% CI | β | 95% CI | OR | 95% CI | β | 95% CI | OR | 95% CI | β | 95% CI |
| Individual characteristics | ||||||||||||
| Wear Time | 1.002 | (0.999, 1.004) | 0.004 | (−0.01, 0.01) | 1.002 | (0.999, 1.004) | 0.004 | (−0.01, 0.02) | ||||
| Age | 0.90 | (0.87, 0.94) | −0.50 | (−0.68, −0.33) | 0.90 | (0.87, 0.94) | −0.52 | (−0.70, −0.34) | ||||
| Gender (Male participants) | 2.49 | (1.40, 4.44) | 1.60 | (−1.13, 4.33) | 2.36 | (1.26, 4.41) | 1.84 | (−1.00, 4.67) | ||||
| Race (Black participants) | 0.70 | (0.39, 1.26) | −3.40 | (−6.31, −0.49) | 0.94 | (0.45, 1.97) | −4.05 | (−7.60, −0.50) | ||||
| Time since stroke (years) | 0.996 | (0.97, 1.03) | −0.02 | (−0.17, 0.13) | 0.99 | (0.96, 1.03) | −0.02 | (−0.18, 0.13) | ||||
| Education | ||||||||||||
| College graduate or more | ref | ref | ref | ref | ||||||||
| Some college | 0.80 | (0.39, 1.63) | 0.51 | (−2.88, 3.90) | 0.77 | (0.35, 1.66) | 0.67 | (−2.96, 4.29) | ||||
| High school graduate | 0.72 | (0.33, 1.56) | −3.19 | (−6.99, 0.62) | 0.86 | (0.37, 2.00) | −2.15 | (−6.17, 1.86) | ||||
| Less than high School | 0.94 | (0.35, 2.50) | −3.26 | (−8.30, 1.78) | 1.16 | (0.40, 3.43) | −2.95 | (−8.25, 2.35) | ||||
| Income | ||||||||||||
| >$75,000 | ref | ref | ref | ref | ||||||||
| $35,000 - $74,999 | 1.46 | (0.53, 4.06) | −4.48 | (−8.92, −0.04) | 2.16 | (0.73, 6.39) | −4.39 | (−8.99, 0.21) | ||||
| $20,000 - $34,999 | 1.07 | (0.38, 2.97) | −4.08 | (−8.80, 0.64) | 1.56 | (0.52, 4.73) | −3.78 | (−8.85, 1.27) | ||||
| < $20,000 | 1.54 | (0.48, 4.89) | −6.02 | (−11.37, −0.66) | 2.54 | (0.72, 9.01) | −6.46 | (−12.07, −0.86) | ||||
| Refused | 2.15 | (0.55, 8.42) | −7.76 | (−13.81, −1.72) | 2.98 | (0.69, 12.75) | −7.70 | (−13.96, −1.44) | ||||
| Environmental characteristics | ||||||||||||
| Population density (n/km2)c | 1.01 | (0.98, 1.04) | 0.08 | (−0.09, 0.24) | 1.003 | (0.97, 1.04) | 0.05 | (−0.11, 0.21) | ||||
| Park area (proportion) | 0.36 | (0.01, 15.02) | −2.15 | (−21.31, 17.02) | 0.49 | (0.007, 35.80) | 5.30 | (−12.97, 23.58) | ||||
| Public rail (count/km2) | 7.57 | (0.40, 143.72) | 0.08 | (−1.83, 1.99) | 4.69 | (0.32, 69.62) | 0.21 | (−1.58, 2.00) | ||||
| Food stores (count/km2) | 0.91 | (0.79, 1.05) | −0.01 | (−0.71, 0.70) | 0.93 | (0.81, 1.09) | 0.14 | (−0.53, 0.81) | ||||
| Restaurants and eating places (count/km2) | 0.97 | (0.88, 1.07) | −0.57 | (−1.29, 0.15) | 0.95 | (0.87, 1.04) | −0.43 | (−1.12, 0.26) | ||||
| Physical activity facilities (count/km2) | 1.03 | (0.60, 1.77) | −0.47 | (−2.93, 1.99) | 0.96 | (0.57, 1.62) | −1.02 | (−3.32, 1.29) | ||||
| Department stores (count/km2) | 1.24 | (0.22, 6.98) | 0.52 | (−7.97, 9.02) | 2.19 | (0.30, 15.80) | 0.73 | (−7.20, 8.66) | ||||
| General mass merchandise (count/km2) | 1.25 | (0.02, 85.43) | 15.79 | (−5.51, 37.08) | 2.37 | (0.03, 221.61) | 19.24 | (−0.73, 39.22) | ||||
| Intellectual stimulation (count/km2) | 0.996 | (0.82, 1.22) | 0.84 | (−0.19, 1.87) | 1.05 | (0.86, 1.29) | 0.99 | (0.02, 1.97) | ||||
| RUCA codes | ||||||||||||
| Urban | ref | ref | ref | ref | ||||||||
| Large rural | 1.68 | (0.30, 4.37) | −0.93 | (−5.66, 3.81) | 1.42 | (0.51, 3.92) | −2.20 | (−6.62, 2.22) | ||||
| Small rural & isolated | 3.26 | (0.87, 12.23) | −1.72 | (−7.64, 4.19) | 2.83 | (0.70, 11.40) | −2.92 | (−8.44, 2.60) | ||||
| Region | ||||||||||||
| Non-stroke belt/buckle | ref | Ref | Ref | ref | ||||||||
| Stroke belt | 0.61 | (0.30, 1.25) | 0.99 | (−2.90, 4.89) | 0.52 | (0.24, 1.14) | 0.97 | (−2.75, 4.68) | ||||
| Stroke buckle | 0.74 | (0.33, 1.69) | 1.07 | (−3.31, 5.45) | 0.70 | (0.27, 1.79) | 1.00 | (−3.29, 5.29) | ||||
| Neighborhood SES | 1.09 | (1.02, 1.16) | 0.28 | (−0.05, 0.61) | 1.10 | (1.02, 1.19) | 0.03 | (−0.31, 0.38) | ||||
| Personal crime | 0.999 | (0.997, 1.001) | −0.01 | (−0.02, 0.01) | 0.999 | (0.996, 1.002) | −0.01 | (−0.02, 0.01) | ||||
| Property crime | 1.002 | (0.999, 1.01) | 0.004 | (−0.01, 0.02) | 1.002 | (0.998, 1.01) | 0.001 | (−0.02, 0.02) | ||||
| Extreme cold daysd | 0.82 | (0.70, 0.96) | −0.78 | (−1.98, 0.42) | 0.87 | (0.73, 1.03) | −0.57 | (−1.69, 0.56) | ||||
| Mean Variance Inflation Factor | 8.70 | 1.57 | 2.54 | 1.89 | 5.63 | 1.92 | ||||||
| Pseudo R-squared | 0.12 | 0.08 | 0.18 | |||||||||
| R-squared | 0.19 | 0.05 | 0.23 | |||||||||
Note. OR=odds ratio; CI=confidence interval; km=kilometer; RUCA=rural-urban community area; SES=socioeconomic status
The logit model (n=374) presents effect estimates between individual and environmental characteristics with obtaining any moderate to vigorous physical activity using logistic regression.
The linear model (n=299) presents effect estimates between individual and environmental characteristics with the number of minutes of moderate to vigorous physical activity using linear regression among participants accumulating any moderate to vigorous physical activity.
Units of 100 people per square kilometer
Units of 10 percent of days with extremely cold temperatures
Discussion
To date, few studies have comprehensively examined the role of individual characteristics and environmental exposures on post-stroke PA participation. In a geographically diverse, bi-racial cohort, this study found that individual and environmental characteristics were associated with PA participation post-stroke. Age, race, and extreme cold weather were all significantly associated with minutes of LPA post-stroke. Age, sex, and nSES were associated with the likelihood of participating in any MVPA. Among participants who accumulated any MVPA, age, race, income, and greater density of destinations for intellectual stimulation was associated with more minutes of MVPA. Caution interpreting the clinical significance of these changes is warranted. The observed associations between environmental characteristics and PA were modest in size (range: 1-6 min/day). Without established minimal important differences in post-stroke physical activity behavior we cannot place these results into clinical context. However, epidemiologic evidence suggests that even small increases in physical activity have clinically-relevant health benefits.50
Of the environmental characteristics examined, this study found that extreme cold weather, nSES and destinations for intellectual stimulation were associated with PA. Extreme cold weather can influence PA by changing individual motivation to participate and also elicit concerns of safety in the outdoor environment.51 Stroke survivors might have greater awareness of the effect cold weather has on function (e.g. spasticity),49 built environment experiences (e.g. icy surfaces), and the combined effects on safe mobility (e.g. loss of balance). Higher nSES was associated with the likelihood of participating in any MVPA. It is possible that nSES captured the underlying quality/investment in infrastructure of the built environment (e.g. sidewalk maintenance), providing greater accessibility of the neighborhood environment for PA participation. Accessible sidewalks are critical for independent mobility and might allow for post-stroke active travel benefits.52 Lastly, a one-unit increase in destinations for intellectual stimulation was associated with 0.99 (95% CI:0.02, 1.97) more daily minutes of MVPA. This sample of older stroke survivors might have high motivation to travel to these destinations (e.g. libraries) for social interaction, community integration, and lifelong learning.53
Many neighborhood destinations were not associated with post-stroke PA. Among the destinations examined in this project, many were privately owned businesses and establishments (e.g. restaurants, food stores), while few were publicly owned (e.g. destinations for intellectual stimulation). One potential explanation might be the physical accessibility of these destinations. After traveling to an establishment, upon arrival, stroke survivors may find the physical building/infrastructure to be inaccessible, thereby discouraging future travel to the destination. While both private and public destinations have federal regulations for accessible infrastructure, laws regulating private destinations (1990) were put into place 17 years after public destinations (1973).54,55 Destinations may have been inaccessible during data collection given the time needed to implement accessibility standards. Unfortunately, national data measuring the extent to which establishments complied with accessibility standards is not available.
Future Research
Additional research is needed to understand the potential role that quality of built environment infrastructure has on post-stroke PA participation. Many environmental destinations examined in this study were not associated with post-stroke PA as hypothesized. Future research should evaluate if the quality of the built environment moderates the association between neighborhood destinations and PA, or if these destinations are not associated with PA participation post-stroke regardless of quality of the built environment.
Strengths and Limitations
This study has many strengths. The REGARDS study is a national cohort, and post-stroke participants had geographic variability across the US to allow for comparisons across heterogeneous environments. This study measured environmental destinations using comprehensive, longitudinal data sources which allowed for linking of the year of environmental characteristics with the year that PA measures were obtained. PA was objectively measured using accelerometers, which are less prone to measurement bias compared to self-reported PA.56 Lastly, information about weather data during the week of accelerometer data collection was integrated into the analysis, an important predictor of PA participation.
This study is not without limitations. There was large variability in the time from stroke to the date of accelerometer data collection, limiting our ability to make specific recommendations for specific post-stroke patients. Post-stroke REGARDS participants had different probabilities of inclusion into the study (Appendix Table 1), potentially subjecting this study to selection bias. Post-stroke participants who were included in this study sample were generally healthier than those who were excluded from the study and lived in environments with fewer destinations, higher nSES, and less crime. This study excluded cases with missing data, possibly biasing our study findings. This study did not control for stroke severity, a characteristic associated with physical activity levels post stroke.57 While the integration of weather was a strength of this study, only one dimension of weather (extreme cold days) was examined.
Conclusions
While many environmental characteristics were not associated with post-stroke PA, extreme cold weather, nSES, and destinations for intellectual stimulation appear important for PA participation post-stroke. Future research is needed to understand if the quality and accessibility of outdoor spaces are modifying the relationship between neighborhood establishments and post-stroke PA.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the Center For Statistical Consultation and Research at the University of Michigan for their assistance with data analysis. This research was supported in part through computational resources and services provided by Advanced Research Computing at the University of Michigan, Ann Arbor.
FUNDING DISCLOSURE
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health (NIH), Department of Health and Human Service. Additional funding was provided by the NINDS of NIH under award numbers 1R01NS092706 and 1R01NS061846, the NIA of the NIH under award numbers 1R01AG049970 and 3R01AG049970-04S1, the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) of NIH under award number 5F31HD098870, the Commonwealth Universal Research Enhancement (C.U.R.E) program funded by the Pennsylvania Department of Health -- 2015 Formula award --SAP #4100072543, the Urban Health Collaborative at Drexel University, the Built Environment and Health Research Group at Columbia University, and by an unrestricted research grant from The Coca-Cola Company. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS, NIA, or the NICHD. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy/.
Footnotes
FINANCIAL DISCLOSURE
No financial disclosures were reported by the authors of this paper
REFERENCES
- 1.Pang MY, Lau RW. The effects of treadmill exercise training on hip bone density and tibial bone geometry in stroke survivors: a pilot study. Neurorehabil Neural Repair 2010;24(4):368–376. [DOI] [PubMed] [Google Scholar]
- 2.Mehta S, Pereira S, Janzen S, Mays R, Viana R, Lobo L, et al. Cardiovascular conditioning for comfortable gait speed and total distance walked during the chronic stage of stroke: a meta-analysis. Top Stroke Rehabil 2012;19(6):463–470. [DOI] [PubMed] [Google Scholar]
- 3.Zedlitz AM, Rietveld TC, Geurts AC, Fasotti L. Cognitive and graded activity training can alleviate persistent fatigue after stroke: a randomized, controlled trial. Stroke 2012;43(4):1046–1051. [DOI] [PubMed] [Google Scholar]
- 4.Harris JE, Eng JJ. Strength training improves upper-limb function in individuals with stroke: a meta-analysis. Stroke 2010;41(1):136–140. [DOI] [PubMed] [Google Scholar]
- 5.Oberlin LE, Waiwood AM, Cumming TB, Marsland AL, Bernhardt J, Erickson KI. Effects of physical activity on poststroke cognitive function: a meta-analysis of randomized controlled trials. Stroke 2017;48(11):3093–3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartman-Maeir A, Soroker N, Ring H, Avni N, Katz N. Activities, participation and satisfaction one-year post stroke. Disabil Rehabil 2007;29(7):559–566. [DOI] [PubMed] [Google Scholar]
- 7.Graven C, Brock K, Hill K, Joubert L. Are rehabilitation and/or care co-ordination interventions delivered in the community effective in reducing depression, facilitating participation and improving quality of life after stroke? Disabil Rehabil 2011;33(17-18):1501–1520. [DOI] [PubMed] [Google Scholar]
- 8.Lai SM, Studenski S, Richards L, Perera S, Reker D, Rigler S, et al. Therapeutic exercise and depressive symptoms after stroke. J Am Geriatr Soc 2006;54(2):240–247. [DOI] [PubMed] [Google Scholar]
- 9.Bell EJ, Lutsey PL, Windham BG, Folsom AR. Physical activity and cardiovascular disease in African Americans in ARIC. Medicine and science in sports and exercise 2013;45(5):901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willey JZ, Moon YP, Sacco RL, Greenlee H, Diaz KM, Wright CB, et al. Physical inactivity is a strong risk factor for stroke in the oldest old: Findings from a multi-ethnic population (the Northern Manhattan Study). Int J Stroke 2017;12(2):197–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blomstrand A, Blomstrand C, Ariai N, Bengtsson C, Björkelund C. Stroke incidence and association with risk factors in women: a 32-year follow-up of the Prospective Population Study of Women in Gothenburg. BMJ Open 2014;4(10):e005173–e005173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hammel J, Jones R, Gossett A, Morgan E. Examining barriers and supports to community living and participation after a stroke from a participatory action research approach. Top Stroke Rehabil 2006;13(3):43–58. [DOI] [PubMed] [Google Scholar]
- 13.Débora Pacheco B, Guimarães Caetano LC, Amorim Samora G, Sant'Ana R, Fuscaldi Teixeira-Salmela L, Scianni AA. Perceived barriers to exercise reported by individuals with stroke, who are able to walk in the community. Disabil Rehabil 2021;43(3):331–337. [DOI] [PubMed] [Google Scholar]
- 14.Kanai M, Izawa KP, Kubo H, Nozoe M, Mase K, Koohsari MJ, et al. Association of Perceived Built Environment Attributes with Objectively Measured Physical Activity in Community-Dwelling Ambulatory Patients with Stroke. Int J Environ Res Public Health 2019;16(20):3908–3916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 2012;125(5):729–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Twardzik E, Judd S, Bennett A, Hooker S, Howard V, Hutto B, et al. Walk Score and objectively measured physical activity within a national cohort. J Epidemiol Community Health 2019;73(6):549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirsch JA, Moore KA, Evenson KR, Rodriguez DA, Roux AVD. Walk Score® and Transit Score® and walking in the multi-ethnic study of atherosclerosis. Am J Prev Med 2013;45(2):158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pound P, Gompertz P, Ebrahim S. A patient-centred study of the consequences of stroke. Clin Rehabil 1998;12(4):338–47. [DOI] [PubMed] [Google Scholar]
- 19.Corrigan R, McBurney H. Community ambulation: perceptions of rehabilitation physiotherapists in rural and regional communities. Physiother Theory Pract 2012;28(1):10–17. [DOI] [PubMed] [Google Scholar]
- 20.Barnsley L, McCluskey A, Middleton S. What people say about travelling outdoors after their stroke: a qualitative study. Aust Occup Ther J 2012;59(1):71–78. [DOI] [PubMed] [Google Scholar]
- 21.Risser R, Iwarsson S, Ståhl A. How do people with cognitive functional limitations post-stroke manage the use of buses in local public transport? Transp Res Part F Traffic Psychol Behav 2012;15(2):111–118. [Google Scholar]
- 22.White JH, Miller B, Magin P, Attia J, Sturm J, Pollack M. Access and participation in the community: a prospective qualitative study of driving post-stroke. Disabil Rehabil 2012;34(10):831–838. [DOI] [PubMed] [Google Scholar]
- 23.Jellema S, van Hees S, Zajec J, van der Sande R, Nijhuis-van der Sanden MW, Steultjens EM. What environmental factors influence resumption of valued activities post stroke: A systematic review of qualitative and quantitative findings. Clin Rehabil 2016;31(7):936–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griffen JA, Rapport LJ, Coleman Bryer R, Scott CA. Driving status and community integration after stroke. Top Stroke Rehabil 2009;16(3):212–221. [DOI] [PubMed] [Google Scholar]
- 25.Roux AVD. Neighborhoods and health: what do we know? What should we do? Am J Public Health 2016;106(3):430–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 2020;141(9):e139–e596. [DOI] [PubMed] [Google Scholar]
- 27.Miller A, Pohlig RT, Reisman DS. Social and physical environmental factors in daily stepping activity in those with chronic stroke. Top Stroke Rehabil 2021;28(3):161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Omura JD, Carlson SA, Brown DR, Hopkins DP, Kraus WE, Staffileno BA, et al. Built environment approaches to increase physical activity: a science advisory from the American Heart Association. Circulation 2020;142(11):e160–e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 2005;25(3):135–143. [DOI] [PubMed] [Google Scholar]
- 30.Howard VJ, Rhodes JD, Mosher A, Hutto B, Stewart MS, Colabianchi N, et al. Obtaining accelerometer data in a national cohort of black and white adults. Med Sci Sports Exerc 2015;47(7):1531–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hooker SP, Hutto B, Zhu W, Blair SN, Colabianchi N, Vena JE, et al. Accelerometer measured sedentary behavior and physical activity in white and black adults: the REGARDS study. J Sci Med Sport 2016;19(4):336–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rand D, Eng JJ, Tang P-F, Jeng J-S, Hung C. How active are people with stroke? Use of accelerometers to assess physical activity. Stroke 2009;40(1):163–168. [DOI] [PubMed] [Google Scholar]
- 33.Gebruers N, Vanroy C, Truijen S, Engelborghs S, De Deyn PP. Monitoring of physical activity after stroke: a systematic review of accelerometry-based measures. Arch Phys Med Rehabil 2010;91(2):288–297. [DOI] [PubMed] [Google Scholar]
- 34.Hooker SP, Feeney A, Hutto B, Pfeiffer KA, McIver K, Heil DP, et al. Validation of the actical activity monitor in middle-aged and older adults. J Phys Act Health 2011;8(3):372–381. [DOI] [PubMed] [Google Scholar]
- 35.Serra MC, Balraj E, DiSanzo BL, Ivey FM, Hafer-Macko CE, Treuth MS, et al. Validating accelerometry as a measure of physical activity and energy expenditure in chronic stroke. Top Stroke Rehabil 2017;24(1):18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Safford MM, et al. Patterns of sedentary behavior and mortality in US middle-aged and older adults: a national cohort study. Ann Intern Med 2017;167(7):465–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hutto B, Howard VJ, Blair SN, Colabianchi N, Vena JE, Rhodes D, et al. Identifying accelerometer nonwear and wear time in older adults. Int J Behav Nutr Phys Act 2013;10(1):120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hurley S, Hertz A, Nelson DO, Layefsky M, Von Behren J, Bernstein L, et al. Tracing a path to the past: exploring the use of commercial credit reporting data to construct residential histories for epidemiologic studies of environmental exposures. Am J Epidemiol 2017;185(3):238–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacquez GM, Slotnick MJ, Meliker JR, AvRuskin G, Copeland G, Nriagu J. Accuracy of commercially available residential histories for epidemiologic studies. Am J Epidemiol 2011;173(2):236–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ruggles S, Flood S, Goeken R, Grover J, Meyer E, Pacas J, et al. Integrated Public Use Microdata Series: Version 9.0 [dataset]. In. Minneapolis: University of Minnesota; 2019. [Google Scholar]
- 41.Lam NS-N. Spatial interpolation methods: a review. The American Cartographer 1983;10(2):129–150. [Google Scholar]
- 42.Forsyth A, Van Riper D, Larson N, Wall M, Neumark-Sztainer D. Creating a replicable, valid cross-platform buffering technique: the sausage network buffer for measuring food and physical activity built environments. Int J Health Geogr 2012;11(1):14–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hirsch JA, Moore KA, Cahill J, Quinn J, Zhao Y, Bayer FJ, et al. Business Data Categorization and Refinement for Application in Longitudinal Neighborhood Health Research: a Methodology. J Urban Health 2020;98(2):271–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Center for Transit-Oriented Development. National TOD Database. In: Center for Neighborhood Technology, editor. https://toddata.cnt.org; 2012. [Google Scholar]
- 45.Rundle AG, Chen Y, Quinn JW, Rahai N, Bartley K, Mooney SJ, et al. Development of a neighborhood walkability index for studying neighborhood physical activity contexts in communities across the US over the past three decades. J Urban Health 2019;96(4):583–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rural Health Research Center. RUCA Data Version 2.0. 2010 March 4, 2021]; Available from: https://depts.washington.edu/uwruca/ruca-data.php
- 47.Roux AD, Kiefe CI, Jacobs DR Jr, Haan M, Jackson SA, Nieto FJ, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol 2001;11(6):395–405. [DOI] [PubMed] [Google Scholar]
- 48.Menne MJ, Durre I, Korzeniewski B, McNeal S, Thomas K, Yin X, et al. Global historical climatology network-daily (GHCN-Daily), Version 3. NOAA National Climatic Data Center 2012;10:V5D21VHZ. [Google Scholar]
- 49.Phadke CP, Balasubramanian CK, Ismail F, Boulias C. Revisiting physiologic and psychologic triggers that increase spasticity. Am J Phys Med Rehabil 2013;92(4):357–369. [DOI] [PubMed] [Google Scholar]
- 50.Warburton DE, Bredin SS. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol 2017;32(5):541–556. [DOI] [PubMed] [Google Scholar]
- 51.Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. Average temperature, diurnal temperature variation, and stroke hospitalizations. J Stroke Cerebrovasc Dis 2016;25(6):1489–1494. [DOI] [PubMed] [Google Scholar]
- 52.Twardzik E, Clarke P, Judd S, Colabianchi N. Neighborhood participation is less likely among older adults with sidewalk problems. J Aging Health 2021;33(1-2):101–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Finlay J, Esposito M, Kim MH, Gomez-Lopez I, Clarke P. Closure of ‘third places’? Exploring potential consequences for collective health and wellbeing. Health Place 2019;60(1):102225–102230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Section 504 Of the Rehabilitation Act of 1973. In: 93–112. Public Law; 1973. [Google Scholar]
- 55.Americans with Disabilities Act of 1990. In: 101–336. Public Law; 1990. [Google Scholar]
- 56.Resnick B, Michael K, Shaughnessy M, Nahm ES, Kopunek S, Sorkin J, et al. Inflated perceptions of physical activity after stroke: pairing self-report with physiologic measures. J Phys Act Health 2008;5(2):308–318. [DOI] [PubMed] [Google Scholar]
- 57.Thilarajah S, Mentiplay BF, Bower KJ, Tan D, Pua YH, Williams G, et al. Factors associated with post-stroke physical activity: a systematic review and meta-analysis. Arch Phys Med Rehabil 2018;99(9):1876–1889. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


