Summary
Background
The burden of Alzheimer's disease and related dementias (ADRDs) is expected to grow rapidly with population aging, especially in low- and middle-income countries, in the next few decades. We used a willingness-to-pay approach to project the global, regional, and national economic burden of ADRDs from 2019 to 2050 under status quo.
Methods
We projected age group and country-specific disability-adjusted life years (DALYs) lost to ADRDs in future years based on historical growth in disease burden and available population projections. We used country-specific extrapolations of the value of a statistical life (VSL) year and its future projections based on historical income growth to estimate the economic burden – measured in terms of the value of lost DALYs – of ADRDs. A probabilistic uncertainty analysis was used to calculate point estimates and 95% uncertainty bounds of the economic burden.
Findings
In 2019, the global VSL-based economic burden of ADRDs was an estimated $2.8 trillion. The burden was projected to increase to $4.7 trillion (95% uncertainty bound: $4 trillion–$5.5 trillion) in 2030, $8.5 trillion ($6.8 trillion–$10.8 trillion) in 2040, and $16.9 trillion ($11.3 trillion–$27.3 trillion) in 2050. Low- and middle-income countries (LMICs) would account for 65% of the global VSL-based economic burden in 2050, as compared with only 18% in 2019. Within LMICs, upper-middle income countries would carry the largest VSL-based economic burden by 2050 (92% of LMICs burden and 60% of global burden).
Interpretation
ADRDs have a large and inequitable projected future VSL-based economic burden.
Funding
The Davos Alzheimer's Collaborative.
Keywords: Alzheimer's disease and related dementias, Dementia, ADRD, Value of statistical life, VSL
Research in context.
Evidence before this study
We searched PubMed and Google Scholar databases on April 11, 2022, using search terms that included variations and combinations of the phrases “Alzheimer's”, “dementia”, “ADRD”, “economic cost”, “economic burden”, “VSL”, “projected”, and “projection” without any date, language, or publication type restrictions. Several country, regional, and global studies estimating the cost of care for dementia or Alzheimer's disease and related dementias (ADRDs), along with systematic reviews, were found. Two global studies projected future direct economic cost of dementia care to be $2 trillion by 2030 and $1.6 trillion by 2050, while a third study projected the direct and indirect care cost to be $9.12 trillion by 2050.
Added value of this study
This study is the first to project global, regional, and country level value of statistical life (VSL) based economic burden of ADRDs through 2050. Our findings show substantially large and growing global VSL- based economic burden of ADRDs, and that the burden will shift from high-income countries to low- and middle-income countries over time.
Implications of all the available evidence
More investment is necessary for ADRDs treatment, care, and prevention research and development, which until now has remained underfunded.
Alt-text: Unlabelled box
Introduction
Advances in medicine, public health, and standards of living increased global life expectancy at birth from less than 60 years in the early 1970s to 72.7 years in 2019, and it is projected to rise to 82 years by 2075.1, 2, 3 In tandem, the burden of Alzheimer's disease and related dementias (ADRDs), which begin in mid-life with symptoms but primarily affect older adults as symptoms progress, has been increasing steadily and will continue to increase, and is now a major component—albeit frequently forgotten—of the disease burden affecting mental health. ADRDs have a severely debilitating effect on quality of life, including loss of memory and cognitive and verbal capacity, reduced mobility, and eventual death. ADRDs contributed to 33.1 million disability-adjusted life years (DALYs) lost in 2019, making it the sixth largest cause of mortality and morbidity among older adults globally.4,5 If the age-specific incidence rate of ADRDs were to grow at the same pace as in the last decade, 115.8 million DALYs would be lost annually by 2050.4
ADRDs care is complex and expensive, involving medical care, formal and informal (e.g., provided by a family member) long-term and hospice care, and end-of-life care.6 The World Alzheimer Report (2015) and other studies have projected the global direct cost of dementia care (including ADRDs and other dementias) to be $2 trillion by 2030, while the direct and indirect cost (which includes lost wages of caregivers) of care is estimated to rise to $9.12 trillion by 2050.7, 8, 9, 10 However, these and other estimates often do not capture the broader individual aspects of the burden of ADRDs such as lost market and nonmarket productivity of patients and the value of suffering and loss of dignity.7,11, 12, 13 Failure to account for the economic burden of ADRDs could lead countries to underinvest in the development and delivery of therapeutic drugs for ADRDs and in new approaches to ADRDs’ prevention and care.14,15
We estimated the decadal global, regional, and national economic burden of ADRDs through 2050 using a willingness-to-pay (value of statistical life, or VSL) approach. VSL is a widely used concept in health economics research and policy for quantifying the trade-off between income and the risk of death.16, 17, 18, 19,19,20 It measures the marginal rate of substitution between wealth and the probability of dying, i.e., the aggregated willingness to pay for a small reduction in mortality risk. For example, if the average individual were willing to pay $100 for a 1 in 100,000 reduction in the probability of own death, it would require 100,000 such individuals to make such a payment to reduce to expected number of deaths by one “statistical life”, corresponding to a collective willingness to pay—or statistical value of life—of $10 million.16, 17, 18 The VSL concept—when generalized for mortality and morbidity—can be interpreted as the monetized equivalent of all measurable (e.g., being economically productive or avoiding medical care cost) and intangible (e.g., happiness or leisure) aspects of a healthy life that an individual might consider. VSL estimates play an important role in benefit-cost analysis of regulatory policies in the United States and other countries, by allowing policymakers to examine the cost of a policy relative to the value of the resulting lives saved.16,21, 22, 23 It is also commonly used to measure the economic burden of diseases or the economic benefits of health interventions but has yet to be applied in the context of ADRDs’ economic burden.24, 25, 26, 27, 28, 29, 30, 31, 32 To the best of our knowledge, only one study has examined the value of healthy longevity (increase in life expectancy) using the VSL approach in the United States.33
Methods
Future burden of disease projections
We projected future year DALYs lost to ADRDs based on data from the Institute for Health Metrics and Evaluation's (IHME) Global Burden of Diseases (GBD) study and the U.S. Aging, Demographics, and Memory Study (ADAMS).5 IHME DALY estimates of Alzheimer's disease and other dementias are available annually until 2019 but do not include data on vascular dementia, a major contributor to the burden of ADRDs. ADAMS offers standardized, in-person neuropsychological assessments of 856 participants aged 70 years and older to determine the etiology of dementia.6 We estimated the relative prevalence of Alzheimer's disease and related dementias from ADAMS and adjusted IHME estimates upward to include the additional dementias not captured in the IHME data.4
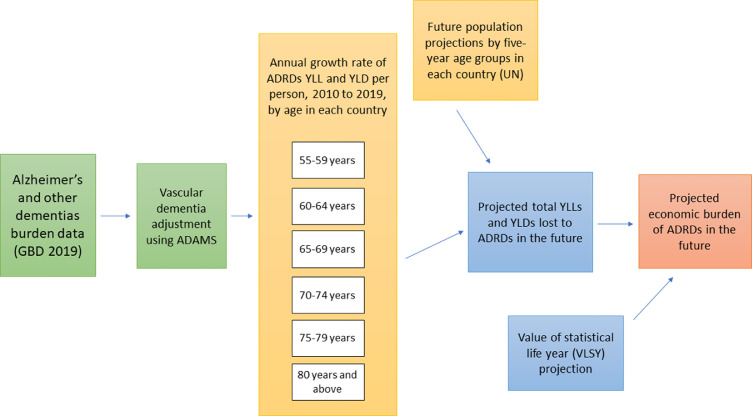
IHME also projects the future burden of Alzheimer's disease and other dementias through 2040 but the estimates are only available for deaths and years of life lost (YLLs).34 Other studies have used baseline dementia prevalence rates with dynamic population projections to estimate future disease burden.10,35 We employed a more detailed approach, incorporating both recent growth in ADRDs prevalence rates and future age- and sex-specific population projections in each country (Model 1). For each country, we first used GBD data (with vascular dementia adjustment) to calculate the average annual growth rate of per person YLLs and years of life lived with disability (YLDs) from ADRDs during 2010–2019 by five year age groups.4 We assumed that these growth rates and the relative share of Alzheimer's vis-à-vis other dementias (i.e., the vascular dementia adjustment factor) would remain the same into the future, and projected per person YLL and YLD rates of ADRDs by country and age groups in 2030, 2040, and 2050. These per person rates were then combined with population projection data from the United Nations (World Population Prospects, medium variant) to estimate the absolute number of YLLs and YLDs lost to ADRDs for each country and age group for the future years.2,4 Figure 1 presents a visual interpretation of the model and further details of uncertainty incorporated in the model are discussed later.
Figure 1.
Methodological summary for projecting future VSL-based economic burden of ADRDs (Model 1).
As a sensitivity analysis, we also modeled future disease burden based on the aforementioned IHME projections of YLLs (Model 2).34 We assumed that the 2019 ratio of YLLs and YLDs lost to Alzheimer's disease and other dementias would continue to be the same into the future. We combined this ratio with 2030 and 2040 IHME projections of YLLs to extrapolate the YLDs lost to Alzheimer's disease and other dementias in those years respectively. We then assumed that YLLs and YLDs after 2040 would grow at the same rate as during 2019–2040 and projected their quantities for 2050. These estimates were adjusted upward using the ADAMS-based adjustment factor for capturing additional dementias. The projections from both models were varied in a probabilistic uncertainty analysis as discussed later.
U.S. and global estimates of the VSL
There is a large economic literature devoted to estimating the VSL in the US and other high-income countries. A 2018 meta-analysis surveyed 1025 VSL estimates from 68 studies to find a median VSL ranging from $9.7 million to $10.1 million (2015 US$), depending upon the methodology of the underlying studies.36 The authors separately considered only studies that used data from the US Census of Fatal Occupational Injuries (CFOI) – a source known to have the lowest measurement errors in estimated mortality risk by occupation – and adjusted for publication bias. The bias-corrected CFOI based estimate was around $10 million in 2015 US$.36
Major US government agencies such as the Federal Aviation Administration, Department of Transportation, and the National Highway Traffic Safety Administration have estimated VSLs related to occupational safety policies in the US. The most of recent of these estimates – developed in the last decade – range from $9.4–$9.7 million.36 In particular, the U.S. Department of Health and Human Services (HHS) 2015 VSL estimate of $9.4 million is used widely by researchers and policymakers.17,21
Notable estimates from other countries are the United Kingdom Treasury's estimate of $2.29 million (2015 US$) and the Organisation for Economic Co-operation and Development's (OECD) estimate of $3 million (2005 US$).36 For most other countries of the world, there are no reliable government estimates of the VSL.21
To produce global estimates of the VSL and use it to project the economic burden of ADRDs, we applied the methodology developed in 2019 by a global expert group of benefit-cost researchers.16,17,21,37 The starting point of this model is the U.S. VSL estimate of $10.6 million (2019 US$, inflation-adjusted from the 2015 U.S. Department of Health and Human Services estimate of $9.4 million).
The statistical value of a life is positively associated with income. Intuitively, the willingness to pay to avoid a 1 in 100,000 risk of death is not the same in the United States, which has a gross national income (GNI) per capita of $63,690 (2018 US$, purchasing power parity or PPP) and a low-income country such as Chad, which has a GNI per capita of $1,930 (2018 US$, PPP).1 Furthermore, differences in the VSL across countries may also be due to differences in the type of policies considered for mortality risk reduction. We used the following formula to compute the VSL of all non-U.S. countries:21
where is the unknown VSL of country x, is the VSL of the United States ($10.6 million), and GNIPC is the 2019 gross national income per capita (PPP) of country x or the United States, as applicable. GNIPC data were obtained from the World Bank.1
E denotes the income elasticity of VSL, i.e., the percentage change in VSL associated with a 1% change in real income. Previous studies have used a wide range of income elasticity of VSL values—from less than 1 to as high as 3.17,19 The elasticity is generally considered to be higher for low- and middle-income countries (LMICs) than for high-income countries (HICs), which reflects greater substitution between willingness to pay for mortality risk reduction and other goods and services in LMICs. We used an elasticity value of 1 for HICs and 1.5 for LMICs following a previous meta-analysis study.21 However, benefit-cost researchers recommend also reporting results from alternative values of the income elasticity.16,17,21,37 We analyzed two additional scenarios in which E=1 and E=1.5 were assumed for all countries of the world. A lower bound of 20 times the GNI per capita (PPP, 2019 US$) of country x was considered for VSLs that were otherwise too low in all scenarios.21 World Bank 2020 definitions of country income group classifications were used throughout our analysis, including for future years.1
Economic valuation of DALYs using value of a statistical life year
We applied the concept of value of a statistical life year (VSLY) to estimate the value of a year of life lost to ADRDs. VSLY is typically calculated by distributing the total VSL over the remaining life years of the target population group for a policy or intervention that can reduce mortality risk. For example, the economic benefit analysis of a health intervention that reduces the risk of neonatal death should consider life expectancy at birth to estimate the VSLY. For policies targeted toward adults or the working-age population, it is recommended that the VSLY be calculated at the average age of the population in a country.21 We obtained median age and the remaining life expectancy at median age data from the World Population Prospects and World Health Organization life tables and divided the VSL equally among the remaining life years at the median age, without any discounting.2,21,38 For example, the estimated 2019 VSL of Bangladesh was $234,383. Considering a median age of 27.6 years and the remaining life expectancy of 52.5 years at this age, the VSLY for Bangladesh was $4,464.
We projected the future values of VSLY of a country by adjusting its 2019 VSLY—as previously calculated—upward for income growth. We calculated the average annual growth rate of GNI per capita (PPP, current international $) in 2010–2019 for each country using World Bank data.1 We assumed that VSLY would grow annually at this same rate into the future and projected country-specific VSLY values for the years 2030, 2040, and 2050.
We equated each DALY lost with a VSLY lost which is commonly done in heath economic evaluations such as in studies of neonatal sepsis, childhood vaccines, air pollution, and surgery.24, 25, 26, 27, 28, 29, 30, 31, 32 The aggregate economic burden of ADRDs is the sum of all VSLYs lost. The risk of ADRDs includes both mortality (as measured by YLLs) and morbidity (as measured by YLDs). Mortality accounts for the majority of the ADRDs disease burden – during 2010–2019, the proportion of YLLs to DALYs lost have remained consistently around 71%.5 Because willingness-to-pay approach studies are typically conducted for fatal risks, it is appropriate to value one YLL at the rate of one VSLY.17,21,37 In comparison, estimating the economic value of morbidity separately requires VSL estimates based on nonfatal risk reduction. As benefit-cost experts note, willingness-to-pay estimates for nonfatal risks are rarely available even for high-income countries, and they recommend valuing nonfatal risks using averted costs when possible.17,21,37 While a few modeling studies have estimated dementia care costs, such estimates are not available at the per capita level necessary for our analysis.7, 8, 9, 10 Therefore, we valued YLLs and YLDs equally at the rate of one VSLY following previous studies that have used this approach.24, 25, 26, 27, 28, 29, 30, 31, 32
Uncertainty analysis
We captured the uncertainty of future estimates through a probabilistic sensitivity analysis. We varied the age-group-specific population projections, annual YLL and YLD growth rates (projected values of YLLs and YLDs for Model 2), and the growth rate of GNI per capita of each country within a range of 50%–150% of the initial value. We drew 1000 random samples from uniform distributions of these parameters within the 50%–150% value range and simulated the economic burden of ADRDs. Simulations were done separately for each country and five-year age groups for the 55 years and older population. Those older than 80 years were considered as one group due to lack of age-disaggregated data in many countries. In Model 2, all ages were considered as one group due to lack of age-disaggregated data. Results were aggregated to compute global, regional, and country mean values with 95% uncertainty bounds. All future year estimates were discounted using an annual discount rate of 3%.
Role of the funding source
The Davos Alzheimer's Collaborative provided financial support, through a contract with Data for Decisions, LLC, for the conduct of the research on which this manuscript is based. The funder had no role in study design, analysis, preparation of the manuscript, or the decision to submit for publication. All authors had full access to the data and accepted responsibility to submit for publication.
Results
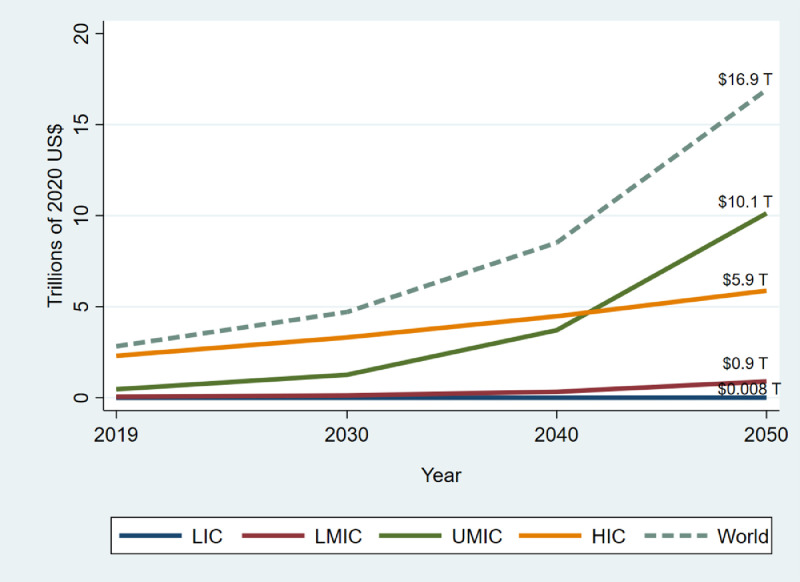
Figure 2 presents regional results in 2020 constant US$ (also see Supplementary Appendix Table 1). Figure 3 shows the distribution of the VSL-based aggregate economic burden of ADRDs across countries, and Supplementary Figure 4 presents per capita burden. In 2019, the estimated global VSL-based economic burden of ADRDs (Model 1, E=1 for HICs and E=1.5 for LMICs) was $2.8 trillion. Considering constant growth rates of per person DALYs and VSLYs into the future, the present value (with 3% annual discounting) of the global VSL-based economic burden is projected to increase to $4.7 trillion (95% uncertainty bound: $4 trillion–$5.5 trillion) in 2030, $8.5 trillion ($6.8 trillion–$10.8 trillion) in 2040, and $16.9 trillion ($11.3 trillion–$27.3 trillion) in 2050. The largest proportional increases are expected in low-, lower-middle-, and upper-middle-income countries, with respective 12.8-, 16.5-, and 21.7-fold increases in the VSL-based economic burden of ADRDs. In high-income countries this is expected to be a 2.6-fold increase. The largest absolute increase, of $9.7 trillion 2020 US$, is similarly expected in upper-middle-income countries, followed by high-income countries, lower-middle-income countries, and low-income countries at $3.6 trillion, $841 billion, and $7.7 billion respectively.
Figure 2.
Estimated economic burden of ADRDs by country groups through 2050, trillions of 2020 constant US$ (Model 1).
Note: Data were available for 168 countries covering more than 99% of the world population. Country income group classifications are from the World Bank (2020 definition). Disease burden was projected based on constant 2010-2019 growth rate (Model 1). Estimates were based on income elasticity values of E=1 for HICs and E=1.5 for LMICs, and adjusted to 2020 constant US$ using consumer price index data from the U.S. Bureau of Labor Statistics. All future year estimates were discounted at a 3% annual discount rate. LIC: Low-income countries; LMIC: Lower-middle income countries; UMIC: Upper-middle income countries; HIC: High-income countries; T: Trillion.
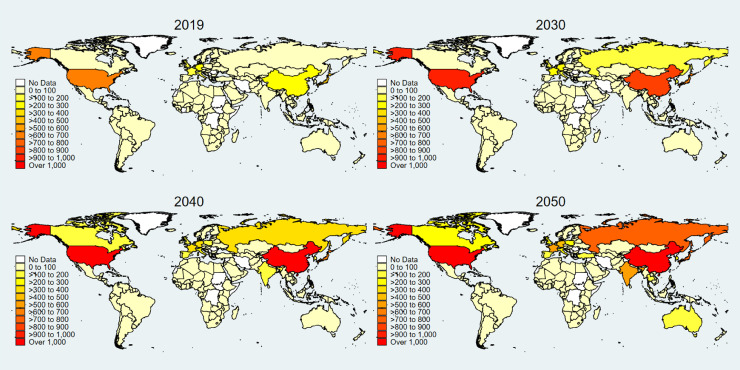
Figure 3.
Estimated economic burden of ADRDs by country through 2050, billions of 2020 US$ (Model 1).
Note: Data were available for 168 countries covering more than 99% of the world population. Disease burden was projected based on constant 2010-2019 growth rate (Model 1). Estimates were based on income elasticity values of E=1 for HICs and E=1.5 for LMICs, and adjusted to 2020 constant US$ using consumer price index data from the U.S. Bureau of Labor Statistics. All future year estimates were discounted at a 3% annual discount rate. Countries without data are marked with white color.
In 2019, the five countries with the largest VSL-based economic burden of ADRDs were the United States ($618.4 billion), China ($495.1 billion), Japan ($475 billion), Germany ($226.5 billion), and Italy ($160.2 billion). By 2050, the countries with the highest VSL-based economic burden of ADRDs would be China with $8.7 trillion ($3.3 trillion–$18.8 trillion), United States with $1.4 trillion ($0.8 trillion–$2.5 trillion), Russian Federation with $758.6 billion ($321.8 billion–$1.6 trillion), Japan with $757.9 billion ($367.7 billion–$1.4 trillion), and India with $578.2 billion ($246.4 billion–$1.3 trillion).
Considering an alternative value of E=1 for all countries (Model 1), the estimated global VSL-based economic burden of ADRDs would be $3.3 trillion in 2019 and going up to $28.3 trillion ($17.2 trillion - $48.9 trillion) by 2050. If we assumed that E=1.5 for all countries (Model 1), the VSL-based economic burden of ADRDs would be $2.6 trillion in 2019 and it would increase to $16.3 trillion ($10.6 trillion - $26.7 trillion) in 2050. The distribution of the burden across world regions would be similar to the base case, although with varying rates of growth over time (Supplementary Appendix Table 2).
Using the alternative YLL-extrapolated projections of future disease burden (Model 2, E=1 for HICs and E=1.5 for LMICs), the estimated global VSL-based economic burden of ADRDs would be $6 trillion ($4.4 trillion–$7.9 trillion) in 2030, $10.5 trillion ($6.7 trillion–$17.4 trillion) in 2040, and $19.4 trillion ($10.7 trillion–$47.5 trillion) in 2050 (Supplementary Appendix Table 3). In low-, lower-middle-, and upper-middle-income countries, the economic burden from 2019 to 2050 would grow 11.3, 12.8, and 24.7 times respectively, as compared with 3.1-fold growth in HICs
The full set of country level estimates of economic burden from Model 1 and presented in Supplementary Appendix Table 4.
Discussion
The United Nations declared 2021–2030 as the “decade of healthy aging,” with the goals that older adults would be able to meet their basic needs, be mobile, learn, grow and decide, foster relationships, and contribute to society. The looming health and economic burden of ADRDs seriously threatens the wellbeing of older adults in this decade and beyond. If the current status quo is maintained, the global economic burden of ADRDs as measured by the value of statistical life years lost would be $17 trillion by 2050. The VSL-based burden would increase approximately two- to three-fold every decade in low-income, lower-middle-income, and upper-middle-income countries. In comparison, the growth rate will be slower in high-income countries, equivalent to about a two-fold increase during the entire period 2019–2050. High-income countries would continue to have the largest VSL-based economic burden of ADRDs in the world through 2040, and by 2050, upper-middle-income countries would become the largest contributor to the global burden. While high-income countries accounted for 83% of the global VSL-based economic burden of ADRDs in 2019, low- and middle-income countries would account for 66% of the burden by 2050. In particular, the burden share of upper-middle-income countries would rise from 27% in 2019 to 60% in 2050. The results were similar under two different disease burden projection models, with slightly higher YLL-extrapolated economic burden estimates.
Underlying country-level demographic and economic conditions and future projections explain these estimates. The populations in low-income, lower-middle-income, and upper-middle-income countries are projected to grow at much higher rates those of high-income countries, leading to substantially larger cohorts of people suffering from ADRDs. Especially in upper-middle-income countries, life expectancy is also projected to grow at a high rate. Finally, the future income growth rates (i.e., GNI per capita growth) of many LMICs are assumed to be higher than the rest of the world in our analysis. Therefore, the VSL-based economic burden of ADRDs in LMICs is projected to grow rapidly.
Our VSL-based economic burden estimates are substantially higher than previous studies of dementia care cost due to differences in methodology. The World Alzheimer Report (2015) estimated the direct medical and social care cost, along with indirect (opportunity cost) cost, to be $893 billion in 2015 and $2.2 trillion in 2030 (2020 US$).7 Pedroza and colleagues estimated the global healthcare spending for dementia to be $263 billion in 2019, and projected that it would increase to $1.6 trillion by 2050.10 Jia and colleagues9 estimated the combined direct medical cost (e.g., inpatient and outpatient), direct nonmedical cost (e.g., social sector costs and long-term care fees), and indirect cost (e.g., opportunity cost and comorbidities) to be $2.54 trillion in 2030, $4.83 trillion in 2040, and $9.12 trillion in 2050. Our estimates of economic burden as the monetized value of DALYs lost to ADRDs are not directly comparable to these estimates. The only study with a VSL-based analysis of healthy aging estimated the economic value of 1- and 10-year increases in life expectancy in the United States to be $38 and $367 trillion respectively.33 Our estimates could also be compared with VSL-based economic burden estimates of other diseases and conditions which affect older adults. For example, a recent study estimated the global economic burden of PM2.5 air pollution induced deaths among older adults (at least 60 years old) to be $2.4 trillion in 2016.27 Similarly, the global economic burden of epilepsy – which primarily affects children and adults over the age of 65 years – was estimated to be $647.4 billion in 2016, while the global economic burden of COVID-19 deaths in 2020 was estimated to be $10.1 trillion.39,40
Our findings have important policy implications. If the health burden of ADRDs continued to grow at its current pace, it would not only impose a large formal and informal care cost burden, but also a large economic burden when measured in terms of the value of DALYs lost. The VSL-based economic burden will shift over time from HICs to LMICs, potentially exacerbating global inequalities in ADRDs care and associated costs.14,15 LMICs are already at a disadvantage when it comes to factors such as air pollution, lower education levels, and poor diet which are linked with higher rates of dementia.41, 42, 43, 44 Substantial inequities also exist regarding those countries that are best equipped to invest now and where the greatest value of averted ADRDs will be in the coming decades. International collaboration is necessary to invest to diminish this looming health, economic, and social threat and advance global equity.
Our analysis has some limitations. We considered a status quo scenario in which the prevalence of ADRDs is assumed to grow at the same rate as in the past decade. To the best of our knowledge, only one study has projected the global and national prevalence of dementia through 2050.45 However, the estimates are available only for dementia prevalence in 2050 and not for other metrics or years. We used two different modeling approaches for projecting future DALYs lost to ADRDs. In addition, we conducted a probabilistic sensitivity analysis that systematically varied the growth rate. Second, we extrapolated country level VSL values for the rest of the world from US-based VSL estimates, and assumed that VSLY would grow at the rate at which GNI per capita of each country grew during the past decade. The VSL literature does not provide guidelines for projecting future VSL in the US or other countries. While willingness to pay for mortality risk reduction will likely increase with income growth, whether it would grow at the same rate as per capita GNI is unknown. The 95% uncertainty bounds of our estimates represent these assumptions, and they should be interpreted accordingly. Third, due to lack of data on the willingness to pay for nonfatal risk reduction, we considered a simple framework in which YLLs lost and YLDs lost are equally valued at the rate of one VSLY. The literature on cost-benefit analysis also recommends valuing quality-adjusted life years (QALYs) with dollar weights instead of DALYs.17,22,46,47 However, DALYs are commonly used in economic evaluation studies when QALY data are not available, such as in our case.25,26,28 Also, we calculated VSLY by distributing VSL over remaining life years at median age without discounting. Alternative approaches that recommend discounting would result in lower estimates of the economic burden of ADRDs.48 Further research is necessary to understand the individual value of healthy longevity in the context of ADRDs. Fourth, the VSL concept incorporates monetary and nonmonetary burdens of ADRDs that an individual might consider. It does not capture opportunity costs or social costs such as loss in caregiver wages or welfare, health system costs, or macroeconomic burden. This is particularly important to note as ADRDs have an especially large economic cost due to informal caregiving.9,12 Finally, we used the 2020 definition of country income groups from the World Bank. As income levels grow, some countries may move across income groups, and our analysis does not capture such future changes.
Despite these limitations, our findings show that ADRDs have a potentially large and inequitable future VSL-based economic burden that necessitates strong mitigation strategies, including public policy and research and development investments.
Contributors
DEB and AN designed the study. AN and SC collected the data, and AN conducted the analysis and wrote the first version of the manuscript. All authors had full access to the data and AN and DEB take responsibility for the integrity of the findings. AN, NC, SC, BS, DT, DV, and DEB critically evaluated the methodology and results, and reviewed and edited the manuscript. All authors accepted the responsibility to submit for publication.
Data sharing statement
All data are available upon request to the corresponding author.
Declaration of interests
AN, DT, and DEB consult for, and NC's employer has received financial support from Data for Decisions, LLC whose clients include GSK, Merck, and Pfizer. These entities did not fund the research in this manuscript. BS has done pro bono advisory work for Ceresti Health which did not fund the research in this manuscript. All other authors declare no conflict of interest. This publication does not represent the views of the Department of Veterans Affairs or the US government.
Acknowledgement
AN, DT, DEB, and NC acknowledge financial support from Data for Decisions for research presented in this manuscript. The authors are grateful to George Vradenburg, Drew Holzapfel, Arnaud Bernaert, Megan Jackson, Alissa Kurzman, James K. Hammitt, Lisa A. Robinson, and participants in a series of webinars for helpful comments, and to Sabrina Malik and Jessica Klusty for their research assistance.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101580.
Appendix. Supplementary materials
References
- 1.World Bank. DataBank | The World Bank. 2021. https://databank.worldbank.org/home.aspx. Accessed 23 September 2021.
- 2.United Nations, Department of Economic and Social Affairs, Population Division. World population prospects. 2019. https://population.un.org/wpp/Publications/. Accessed 6 April 2022.
- 3.United Nations. UNdata. 2022. https://data.un.org/Default.aspx. Accessed 17 March 2022.
- 4.Bloom D, Chen S, Counts N, et al. Addressing Alzheimer's disease and related dementias to realise the promise of the UN's ‘Decade of Healthy Ageing’. VoxEU. 2021. https://voxeu.org/article/alzheimer-s-and-un-s-decade-healthy-ageing. Accessed 14 May 2021.
- 5.Institute for Health Metrics and Evaluation . GBD Results Tool. 2019. Global burden of diseases results tool.http://ghdx.healthdata.org/gbd-results-tool [Google Scholar]
- 6.Langa KM, Plassman BL, Wallace RB, et al. The aging, demographics, and memory study: study design and methods. Neuroepidemiology. 2005;25:181–191. doi: 10.1159/000087448. [DOI] [PubMed] [Google Scholar]
- 7.Prince M, Wimo A, Guerchet MM, Ali GC, Wu Y-T, Prina M. Alzheimer's Disease International; London: 2015. World Alzheimer Report 2015 - The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends.http://www.alz.co.uk/research/world-report-2015 [Google Scholar]
- 8.Wimo A, Guerchet M, Ali G-C, et al. The worldwide costs of dementia 2015 and comparisons with 2010. Alzheimers Dement. 2017;13:1–7. doi: 10.1016/j.jalz.2016.07.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jia J, Wei C, Chen S, et al. The cost of Alzheimer's disease in China and re-estimation of costs worldwide. Alzheimers Dement. 2018;14:483–491. doi: 10.1016/j.jalz.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Pedroza P, Miller-Petrie MK, Chen C, et al. Global and regional spending on dementia care from 2000–2019 and expected future health spending scenarios from 2020–2050: an economic modelling exercise. eClinicalMedicine. 2022;45:1–13. doi: 10.1016/j.eclinm.2022.101337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Hayek YH, Wiley RE, Khoury CP, et al. Tip of the iceberg: assessing the global socioeconomic costs of Alzheimer's disease and related dementias and strategic implications for stakeholders. J Alzheimers Dis. 2019;70:323–341. doi: 10.3233/JAD-190426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368:1326–1334. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bloom D, Khoury A, Algur E, Sevilla J. Valuing productive non-market activities of older adults in Europe and the US. De economist. 2020;168:153–181. [Google Scholar]
- 14.Bloom DE, Counts N, Nandi A, Tortorice D, Vigo D. World Economic Forum. 2022. How to address Alzheimer's disease and support healthier ageing.https://www.weforum.org/agenda/2022/02/this-is-how-to-address-a-global-alzheimers-disease/ Accessed 25 March 2022. [Google Scholar]
- 15.Counts N, Nandi A, Seligman B, Tortorice D. Dementia storm on the horizon: the rising incidence of dementia around the world calls for global collaboration and decisive financing. Financ Develop. 2021;58:54–57. [Google Scholar]
- 16.U.S. Department of Health and Human Services; Washington, DC: 2017. Guidelines for Regulatory Impact Analysis. [Google Scholar]
- 17.Robinson LA, Hammitt JK, Cecchini M, et al. Reference case guidelines for benefit-cost analysis in global health and development. 2019. https://sites.sph.harvard.edu/bcaguidelines/guidelines/. Accessed 4 January 2021.
- 18.Viscusi WKK, Aldy JEJ. The value of a statistical life: a critical review of market estimates throughout the world. J Risk Uncertainty. 2003;27:5–76. [Google Scholar]
- 19.Viscusi WK, Masterman CJ. Income elasticities and global values of a statistical life. J Benefit Cost Anal. 2017;8:226–250. [Google Scholar]
- 20.Aldy JE, Viscusi WK. Adjusting the value of a statistical life for age and cohort effects. Rev Econ Stat. 2008;90:573–581. [Google Scholar]
- 21.Robinson LA, Hammitt JK, O'Keeffe L. Valuing mortality risk reductions in global benefit-cost analysis. J Benefit-Cost Ana. 2019;10:15–50. doi: 10.1017/bca.2018.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson LA, Hammitt JK. Valuing reductions in fatal illness risks: implications of recent research. Health Econ. 2016;25:1039–1052. doi: 10.1002/hec.3214. [DOI] [PubMed] [Google Scholar]
- 23.Hammitt JK. Valuing mortality risk: theory and practice. Environ Sci Technol. 2000;34:1396–1400. [Google Scholar]
- 24.Brent RJ. A CBA of corrective lenses, including the benefits for reducing the symptoms of dementia. App Econ. 2020;52:5218–5229. [Google Scholar]
- 25.Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Global Health. 2018;3 doi: 10.1136/bmjgh-2017-000347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watts E, Sim SY, Constenla D, Sriudomporn S, Brenzel L, Patenaude B. Economic benefits of immunization for 10 pathogens in 94 low- and middle-income countries from 2011 to 2030 using cost-of-illness and value-of-statistical-life approaches. Value Health. 2021;24:78–85. doi: 10.1016/j.jval.2020.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Yin H, Brauer M, Zhang J, et al. Population ageing and deaths attributable to ambient PM2·5 pollution: a global analysis of economic cost. Lancet Planetary Health. 2021;5:e356–e367. doi: 10.1016/S2542-5196(21)00131-5. [DOI] [PubMed] [Google Scholar]
- 28.Corlew DS, Alkire BC, Poenaru D, Meara JG, Shrime MG. Economic valuation of the impact of a large surgical charity using the value of lost welfare approach. BMJ Glob Health. 2016;1 doi: 10.1136/bmjgh-2016-000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Watts E, Mak J, Patenaude B. Benefit-cost ratios of continuing routine immunization during the COVID-19 pandemic in Africa. J Benefit-Cost Anal. 2022;13:91–106. [Google Scholar]
- 30.Morgan A, Hartmanis S, Tsochatzis E, et al. Disease burden and economic impact of diagnosed non-alcoholic steatohepatitis (NASH) in the United Kingdom (UK) in 2018. Eur J Health Econ. 2021;22:505–518. doi: 10.1007/s10198-020-01256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Florence C, Luo F, Rice K. The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. 2021;218 doi: 10.1016/j.drugalcdep.2020.108350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alkire B, Hughes CD, Nash K, Vincent JR, Meara JG. Potential economic benefit of cleft lip and palate repair in sub-Saharan Africa. World J Surg. 2011;35:1194–1201. doi: 10.1007/s00268-011-1055-1. [DOI] [PubMed] [Google Scholar]
- 33.Scott AJ, Ellison M, Sinclair DA. The economic value of targeting aging. Nat Aging. 2021;1:616–623. doi: 10.1038/s43587-021-00080-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Institute for Health Metrics and Evaluation . 2022. Global Burden of Diseases Foresight.http://vizhub.healthdata.org/gbd-foresight/forecasting Accessed 27 May 2022. [Google Scholar]
- 35.Hurd MD, Martorell P, Langa K. Future monetary costs of dementia in the United States under alternative dementia prevalence scenarios. J Popul Ageing. 2015;8:101–112. doi: 10.1007/s12062-015-9112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Viscusi WK. Best estimate selection bias in the value of a statistical life. J Benefit-Cost Anal. 2018;9:205–246. [Google Scholar]
- 37.Robinson LA, Hammitt JK, Jamison DT, Walker DG. Conducting benefit-cost analysis in low- and middle-income countries: introduction to the special issue. J Benefit-Cost Anal. 2019;10:1–14. doi: 10.1017/bca.2019.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.WHO . 2020. World Health Organization Life Tables.https://apps.who.int/gho/data/node.main.LIFECOUNTRY?lang=en Accessed 4 January 2021. [Google Scholar]
- 39.O'Donohoe TJ, Choudhury A, Callander E. Global macroeconomic burden of epilepsy and the role for neurosurgery: a modelling study based upon the 2016 Global Burden of Disease data. Eur J Neurol. 2020;27:360–368. doi: 10.1111/ene.14085. [DOI] [PubMed] [Google Scholar]
- 40.Viscusi WK. Economic lessons for COVID-19 pandemic policies. Southern Econ J. 2021;87:1064–1089. doi: 10.1002/soej.12492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scarmeas N, Stern Y, Tang M-X, Mayeux R, Luchsinger JA. Mediterranean diet and risk for Alzheimer's disease. Ann Neurol. 2006;59:912–921. doi: 10.1002/ana.20854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ballarini T, Lent DM van, Brunner J, et al. Mediterranean diet, alzheimer disease biomarkers, and brain atrophy in old age. Neurology. 2021;96:e2920–e2932. doi: 10.1212/WNL.0000000000012067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sharp ES, Gatz M. The relationship between education and dementia an updated systematic review. Alzheimer Dis Assoc Disord. 2011;25:289–304. doi: 10.1097/WAD.0b013e318211c83c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alzheimer's Association. Improving air quality reduces dementia risk, multiple studies suggest | AAIC 2021. 2021. //aaic.alz.org/releases_2021/air-pollution-dementia-risk.asp. Accessed 28 May 2022.
- 45.Nichols E, Steinmetz JD, Vollset SE, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of disease study 2019. Lancet Public Health. 2022;7:e105–e125. doi: 10.1016/S2468-2667(21)00249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hammitt JK. Valuing mortality risk in the time of COVID-19. J Risk Uncertain. 2020;61:129–154. doi: 10.1007/s11166-020-09338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haagsma JA, Polinder S, Cassini A, Colzani E, Havelaar AH. Review of disability weight studies: comparison of methodological choices and values. Popul Health Metrics. 2014;12:20. doi: 10.1186/s12963-014-0020-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murphy KM, Topel RH. The value of health and longevity. J Polit Econ. 2006;114:871–904. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.