Abstract
Arachnoid cysts are the most common benign cystic abnormalities formed due to congenital splitting of the arachnoid layer. They comprise 1% of intracranial masses, and the orbital location is even more rarely reported in history especially in the pediatric population. They might be discovered as an asymptomatic finding on imaging performed for a concomitant condition or, in most reported cases, as a result of ophthalmic impairment. They can be isolated or associated with gliomas, neurofibromas, empty sella syndrome, and frontotemporal porencephalic cysts. Computed tomography scan shows a non-enhancing liquid cystic lesion, and magnetic resonance imaging remains the best assessment tool confirming the similarity of the fluid to cerebrospinal fluid and evaluating the optic nerves. Herein, we report the case of an incidental discovery of an intraorbital arachnoid cyst on magnetic resonance imaging in a 53-year-old woman with a history of epilepsy. No treatment was performed as the cystic formation was asymptomatic.
Keywords: Arachnoid cyst, optic nerve, magnetic resonance imaging
Introduction
Intraorbital arachnoid cysts are rare entities prevailing mostly in pediatric population. An early diagnosis, especially at the antenatal stage helps preserve the optic functions before the process reaches an advanced stage with irreversible damage. 1
The onset of the disease occurs generally early in childhood and the classic clinical manifestations consist of headaches and progressive loss of visual acuity (VA).
Our case draws attention to the heavy impact that this benign disease can have on the functional prognosis 2 and the importance of considering a range of more serious differential diagnosis and mimics, 3 which raises the need for exclusion criteria notably on magnetic resonance imaging (MRI) as the main imaging modality. MRI confirms the cerebrospinal fluid–like liquid cystic lesion contained in the optic nerve (ON) sheath, non-enhancing after gadolinium administration, which excludes many other pathologies.
In case of deterioration of the optic disk, surgical decompression is indicated. Otherwise, abstention is preferred to prevent further damage. 4
Case representation and imaging findings
A follow-up head multiplanar MRI was performed on a 53-year-old female patient with a history of idiopathic epilepsy and no history of head trauma or infection. The imaging findings show an intraorbital cystic mass following CSF signal in all pulse sequences without diffusion restriction or enhancement after administration of gadolinium without any pre-existing parenchymal lesions or bony or dural defects. The patient reported no visual disorder, and no opthlamologic data were provided.
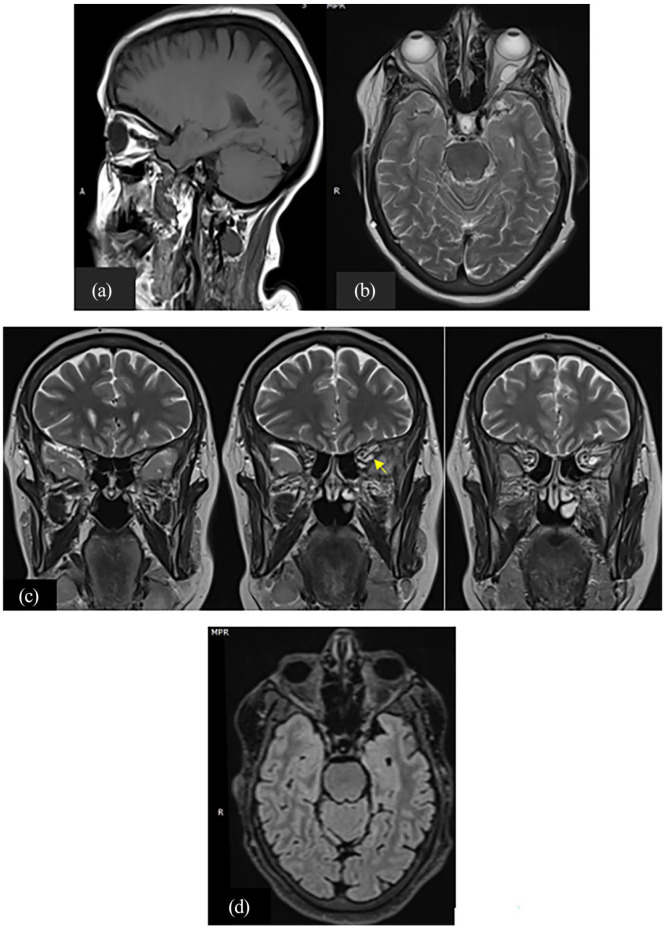
T1-weighted sagittal images show a hypo intense mass compressing the left ON. Weighted axial and coronal images demonstrate a hyper intense regular, lobulated cystic lesion within the left intraconal orbit in the area of the left ON that loses signal on T2 FLAIR sequence and appears to be communicating with the homolateral temporal sub-arachnoidian spaces through the superior orbital fissure (Figure 1).
Figure 1.
(a) T1-weighted sagittal, (b) T2 axial, (c) T2 coronal, and (d) T2 FLAIR–weighted axial images showing a regular, lobulated lesion adjacent to the left optic nerve, isointense to CSF and presenting a communication with left optic nerve sheaths (c) (arrow).
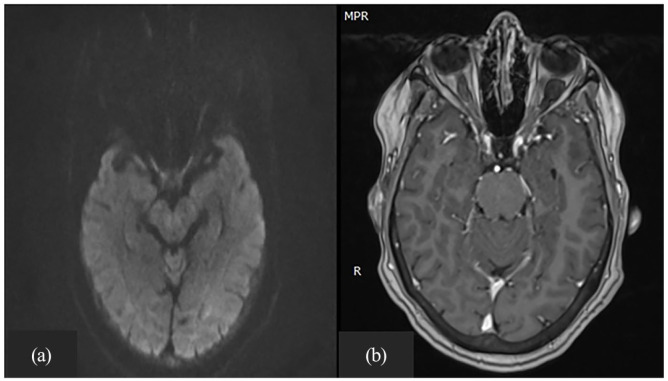
Diffusion-weighted images (DWIs) show no restriction of diffusion in the cystic mass (Figure 2(a)). There is no enhancement on post-contrast T1-weighted images (Figure 2(b)).
Figure 2.
(a) DWI showed no restriction of diffusion in the cystic mass (b) with no enhancement on post-contrast T1-weighted images.
These findings were characteristic of an intraorbital arachnoid cyst, and no further investigation was necessary.
Therapeutic abstention was the right option for this patient.
Discussion
Orbital and periorbital arachnoid cysts represent a benign condition that is due to distention and proliferation of normal fibrovascular tissue comprising the leptomeninges that surround the ON. This may result in globe proptosis and significant decrease in VA subsequent to orbital walls remodeling. 5 Patients with ON sheath arachnoid cysts have been reported in history with or without concomitant abnormalities (Table 1).
Table 1.
| Authors | Patient age/sex | Visual acuity | Optic disk | CT/MRI | Other findings | Treatment and outcome |
|---|---|---|---|---|---|---|
| Nemati et al. 5 | 19 a /F | 20/400 | Atrophic | Right ON cyst extending from optic chiasm | Absence of sphenoid bone right wing | Surgical decompression with VA improvement |
| Wolter and McKenny 6 | 4 a /M | 20/30 | Normal | Left orbital cyst | ON glioma | NA |
| Holt 7 | Case 1: 33
a
/M Case 2: 55 a /F |
20/20 20/20 |
Normal Edema |
Right ON cystic lesion Left ON cystic lesion |
None None |
NA |
| Smith et al. 8 | 45 a /f | 20/20 | Normal | Left ON cyst | Empty sella syndrome | NA |
| Spencer 9 | 3 a /m | Not reported 4/200 |
Not reported Edema |
Orbital cyst | NF | NA |
| Miller and Green 10 | Case 1: 33
a
/F Case 2: 56 a /F |
20/100 | Atrophic | Right ON cyst Left ON cyst |
None Porencephalic cyst |
NA NA |
| Saari et al. 11 | 29 a /F Left | 20/15 | Normal | orbital cyst | None | NA |
| Hupp et al. 12 | 69 a /M | 20/50 | Edema | Right ON enlarged | Trauma | NA |
| Wojno et al. 13 | 43 a /M | 20/200 | Atrophic | Right/left ON enlarged | None | NA |
| Akor et al. 14 | Case 1: 44
a
/M Case 2: 59 a /M |
NLP 1 FTCF |
Not seen Atrophic |
Right ON cyst Left ON cyst |
None None |
Excision biopsy: With VA improvement Excision biopsy With VA improvement |
| Wijngaarde et al. 15 | 2 a /F | 5/15 on right Light perception on left | Not reported | Bilateral intraorbital arachnoid cysts | Coloboma of the ON ends | Surgical decompression of left eye and abstention for the right eye with vision stability |
| Shankar et al. 16 | 2 months/M | Incapacity to follow light | Thin rim of neural tissue surrounding optic disc | Bilateral intraorbital arachnoid cysts | Coloboma of optic disc | Abstention for the cyst and vision stimulation exercises for coloboma with VA improvement |
| Wegener et al. 17 | 9 a /F | 20/200 | Not reported | Left ON cyst extending from optic chiasm | NF1 | Decompression surgery without VA improvement |
| Moschos et al. 18 | 17 a /F | Not reported | Not reported | Left ON arachnoid cyst | None | Patient refused treatment and VA remained unchanged |
CT: computed tomography; MRI: magnetic resonance imaging; ON: optic nerve; VA: visual acuity; NA: not available; NF: neurofibromatosis; NLP: No light perception; FTCF: full to count fingers.
Years old.
The congenital origin of arachnoid cysts is admitted by most authors. 19 It results from aberrant development of arachnoid tissue.
The histological and ultramicroscopic studies find cellular layers identical to the arachnoid tissue and cerebrospinal fluid secretion capacities revealing the morphological and functional similarities that arachnoid cysts share with arachnoid granulations.
The pathogenesis of primary ON sheath arachnoid cyst remains unknown, but the theory of an eventual congenital process is supported by the association with other congenital anomalies. However, secondary arachnoid cysts might develop following trauma; the resulting intraorbital hemorrhage leads to cyst formation. It might as well be a response to the increasing intracranial and intra-cyst pressure transmitted along the vaginal sheaths of the ON subsequent to porencephalic cyst for example.
Most of the reported cases of intraorbital arachnoid cysts, if not all of them, presented with a decrease of VA or a globe proptosis predominantly during childhood.
On computed tomography (CT), the typical appearance is an extra-axial space-occupying cystic lesion with a Hounsfield attenuation around 10–20 IU compatible with CSF density, non-enhanced, or belatedly enhanced following iodinated contrast administration.
CT scan is the most available firsthand neuroimaging exam whose major role is to identify complications, especially, cystic internal hemorrhage.
MRI is the key tool for evaluating ON abnormalities due its superior spatial resolution identifying different tissue characteristics. However, interpretation must be careful because of chemical shift artifacts in an enlarged ON. In most cases, only have arachnoid cysts been confirmed by histological studies. It shows an intraorbital homogeneous cystic lesion adjacent to the ON hypo intense in T1- and hyper intense in T2-weighted images, attenuated on FLAIR sequence proving the similarity of cyst fluid to CSF. Arachnoid cysts have a very thin wall, frequently not seen; therefore, their presence can only be implied by the displacement of the ON. And as their wall have no solid component, it does not enhance after gadolinium administration, hence, ruling out eventual malignant lesions. Meningoceles carry the same characteristic signals but can be differentiated from arachnoid cyst by the evident herniation of the meninges through a bone defect, and they are most commonly associated with cerebral malformations.
Moreover, MRI sequences, such as DWI, enable to identify epidermoid cysts, as a differential diagnosis, by displaying diffusion restriction.
Some centers report using MRI modalities such as intrathecal contrast-enhanced MRI cisternography and non-contrast techniques like constructive interference in steady state (CISS) and fast imaging employing steady-state acquisition (FIESTA) to demonstrate the cyst wall and the surrounding structures. And finally, three-dimensional (3D)-spin echo T2 highlights the connection of the arachnoid cyst with the surrounding CSF space, by demonstrating signal loss in areas of CSF flow. 20
These studies can be helpful in planning ON sheath decompression.
Excisional biopsies, potentially diagnostic and therapeutic, indicate a wall predominantly composed of few meningothelial cells, arachnoid with thickened dura mater and leptomeninges consistent with an arachnoid cyst. There has also been found within arachnoid cysts fibrous tissue with a simple epithelial lining and non-arachnoid luminal epithelia with plentiful microvilli and/or cilia.
Arachnoid cysts have similar clinicopathologic features with numerous orbital conditions, mainly neoplasms, making it very difficult sometimes to be able to distinguish between these different entities. We might cite the epidermoid cysts, ON sheath meningioma, glioma, tuberculoma, or intraneural hematoma. Peri optic spaces dilatation in idiopathic intracranial hypertension in its unilateral presentation is also to be mentioned.
These affections should be rapidly identified and correctly treated to obtain a prompt vision recovery (Table 2).
Table 2.
Most common differential diagnosis along with their characteristic features as an exclusion criteria.
| Characteristic features | ||||
|---|---|---|---|---|
| T1 | T2/T2 FLAIR (Fluid attenuated inversion recovery) | DWI | Post contrast | |
| Epidermoid cyst | Isointense to CSF | Heterogeneous signal from isointense to intensity higher than CSF | Restriction on DWI: hyperintense, similar ADC (Apparent diffusion coefficient) values compared to adjacent brain parenchyma | Peripheral enhancement |
| Lymphangioma | Isointense to brain parenchyma | Hyper intense with occasional multiple fluid: fluid levels and internal septations | Focal areas of restricted diffusion | Marginal and septal enhancement and a variable solid component enhancement |
| Meningioma | Isointense to hypointense compared to the optic nerve | Mildly hyperintense compared to the optic nerve | Restriction and ADC value vary according to the histological form | Homogeneous enhancement |
| Glioma | Hypointense heterogeneous with cystic and solid components. | hyperintense centrally with a thin low-signal at the periphery representing the dura. | Variable intensity and ADC values | Variable enhancement |
| Tuberculoma | Isointense to grey matter ± central hyperintensity representing caseation. | Isointense to grey matter ± a central hypointensity representing gliosis and abundant monocytes infiltration, surrounded by hyperintense T2/T2 FLAIR vasogenic edema. | Central low signal but if liquid necrosis is present centrally, may be high signal. | Usually appears as ring-enhancement. |
| Hematoma | Intermediate signal at hyperacute period. | Hyperintense at hyperacute period. Hypointense at chronic period. | Might be bright at hyperacute period. | Peripheral enhancement around the non-enhancing clot may be visible. |
| Orbital varix | Hypointense | Hypointense | None | Matches other veinous structures. |
DWI: diffusion-weighted imaging; CSF: cerebro-spinal fluid.
Therapeutic abstention might be considered if the arachnoid cyst is asymptomatic or if vision acuity is not significantly altered, considering that the brutal decompression might cause more harm to the ON. However, if clinical and radiological findings suggest a deterioration of optic disk, endangering the functional prognosis, surgical decompression is then proposed with positive outcome in most cases. 1
A CT-guided aspiration is a less-invasive procedure improving visual function with a lower risk of reccurence. 21
Different surgical approaches might be adopted then, whether a trans frontal craniotomy, orbitotomy or a simple percutaneous puncture. Add to that, the excisional biopsy as a double-interest technique in providing histological proof and decompressing the injured nerve. 14
Conclusion
Orbital arachnoid cysts are not commonly reported in history. Although benign, are nonetheless still dangerous since they might mimic more malignant orbital lesions or silently increase in volume causing progressively an irreversible damage to the ON if surgical decompression is not performed early.
Acknowledgments
The authors thank the professors and all the colleagues who participated in the completion of this work.
Footnotes
Author contributions: F.T. contributed to the conception of the work, design of the work, and acquisition of data. I.E.O. contributed in acquisition of data. N.E. and M.F. contributed by drafting the work. M.J. contributed by revising the work critically for important intellectual content and final approval of the version to be published.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Ibtissam El Ouali  https://orcid.org/0000-0001-6501-6888
https://orcid.org/0000-0001-6501-6888
References
- 1. Momtchilova M, Moussaoui K, Laroche L, et al. Kystes arachnoïdiens et manifestations ophtalmologiques chez l’enfant: à propos de deux cas. J Fr Ophtalmol 2013; 36(9): 775–778. [DOI] [PubMed] [Google Scholar]
- 2. Edgar LC, Milena BTA, Vanessa LT. Quiste aracnoideo de la vaina del nervio óptico simulando defecto glaucomatoso en el campo visual. CES Med 2021; 35(1): 44–50. [Google Scholar]
- 3. Vegunta S, Patel BC. Optic nerve cysts. Treasure Island, FL: StatPearls Publishing, https://www.ncbi.nlm.nih.gov/books/NBK534104/ (2022, accessed January 2022) [PubMed] [Google Scholar]
- 4. Menon RK. Arachnoid cyst and visual function. In: Wester KG. (ed.) Arachnoid cysts: clinical and surgical management. Amsterdam: Elsevier, 2018, pp. 29–43. [Google Scholar]
- 5. Nemati A, Rashid M, Nazari S, et al. Progressive proptosis due to arachnoid cyst: a case report and review. Neurosurg Quart 2011; 21: 1–3. [Google Scholar]
- 6. Wolter JR, McKenney MJ. Collateral hyperplasia and cyst formation of orbital leptomeninx and cyst formation of orbital leptomeninx. Am J Ophthlamol 1964; 57: 1037–1042. [DOI] [PubMed] [Google Scholar]
- 7. Holt H. Cysts of the intracranial portion of the optic nerve. Am J Ophthalmol 1966; 61(5 Pt 2): 1166–1170. [DOI] [PubMed] [Google Scholar]
- 8. Smith JL, Hoyt WF, Newton TH. Optic nerve sheath decompression for relief of chronic monocular choked disc. Am J Ophthalmol 1969; 68(4): 633–639. [DOI] [PubMed] [Google Scholar]
- 9. Spencer WH. Primary neoplasms of the optic nerve and its sheaths: clinical features and current concepts in pathogenic mechanisms. Trans Am Ophthalmol Soc 1972; 70: 490–528. [PMC free article] [PubMed] [Google Scholar]
- 10. Miller NR, Green WR. Arachnoid cysts involving a portion of the intraorbital optic nerve. Arch Ophthalmol 1975; 93(11): 1117–1121. [DOI] [PubMed] [Google Scholar]
- 11. Saari M, Mustonen E, Palva A, et al. Arachnoid cyst of the intraorbital portion of the optic nerve with unilateral disc oedema and transient shallowing of the anterior chamber. Acta Ophthalmol 1977; 55(6): 959–964. [DOI] [PubMed] [Google Scholar]
- 12. Hupp SL, Buckley EG, Byrne SF, et al. Post traumatic venous obstructive retinopathy associated with enlarged optic nerve sheath. Arch Ophthalmol 1984; 102: 254–256. [DOI] [PubMed] [Google Scholar]
- 13. Wojno T, Beck RW, Grosserode R. Bilateral optic nerve sheath enlargement. Ophthalmic Surg 1986; 17(9): 584–588. [PubMed] [Google Scholar]
- 14. Akor C, Wojno TH, Newman NJ, et al. Arachnoid cyst of the optic nerve: report of two cases and review of the literature. Ophthalmic Plast Reconstr Surg 2003; 19(6): 466–469. [DOI] [PubMed] [Google Scholar]
- 15. Wijngaardel R, Blaauw G, Van Balen A. Bilateral intraorbital arachnoid cysts of the optic nerves and coloboma of the optic nerve ends. Neuro-Ophthalmology 2009; 4(3): 165–168. [Google Scholar]
- 16. Shankar LG, Khadia A, Gayam K, et al. An eye behind an eye: a rare association of bilateral optic disc coloboma with retrobulbar cyst. Indian J Ophthalmol 2020; 68(8): 1656–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wegener M, Prause JU, Thygesen J, et al. Arachnoid cyst causing an optic neuropathy in neurofibromatosis 1. Acta Ophthalmol 2010; 88(4): 497–499. [DOI] [PubMed] [Google Scholar]
- 18. Moschos MM, Lymberopoulos C, Moschos M. Arachnoid cyst of the optic nerve: a case report. Klin Monbl Augenheilkd 2004; 221(5): 408–409. [DOI] [PubMed] [Google Scholar]
- 19. Rengachary SS, Watanabe I. Ultrastructure and pathogenesis of intracranial arachnoïd cysts. J Neuropathol Exp Neurol 1981; 40: 61–83. [PubMed] [Google Scholar]
- 20. White ML, Das JM. Arachnoid cysts. Treasure Island, FL: StatPearls Publishing, https://www.ncbi.nlm.nih.gov/books/NBK563272/ (2021, accessed January 2022). [PubMed] [Google Scholar]
- 21. Das D, Deka P, Deka AC, et al. An unusual case of retrobulbar arachnoid cyst and its management. Orbit 2009; 28(2–3): 169–171. [DOI] [PubMed] [Google Scholar]