Abstract
Background
Gout is of unknown reason associated with cardiovascular disease. Ultrasound is sensitive for detecting crystal deposition and plasma calprotectin is a sensitive inflammatory marker. This study explores the associations between crystal deposition, inflammation and carotid artery pathology.
Method
A cross-sectional analysis of baseline assessments from the NOR-Gout study was undertaken. Crystal deposition was assessed by ultrasound (double contour, tophi, aggregates) and dual-energy CT (DECT) and laboratory assessments included plasma calprotectin. The carotid arteries were bilaterally examined for carotid intima–media thickness (cIMT) and presence of plaques. Spearman correlations, Mann-Whitney tests and linear regression analyses were used to explore associations between crystal deposition, inflammatory markers, and carotid pathology.
Results
202 patients with intercritical gout (95.5% men, mean (SD) age 56.5 (13.8) years, disease duration 7.9 (7.7) years) were included. Calprotectin was correlated with all scores of crystal deposition by ultrasound (r=0.26–0.32, p<0.001) and DECT (r=0.15, p<0.05). cIMT was correlated with sum score aggregates (r=0.18–0.22, p<0.05). Patients with large tophi had higher levels of calprotectin as well as more frequent carotid plaque (p<0.05).
Conclusions
Study findings point towards crystal deposition contributing to subclinical inflammation with subsequent vascular implications. However, future longitudinal studies are needed to confirm such causal relationships.
Keywords: Gout, Ultrasonography, Cardiovascular Diseases, Inflammation
WHAT IS ALREADY KNOWN ON THIS TOPIC
Monosodium urate (MSU) crystal deposition in gout may be detected and quantified by use of established ultrasound scores of double contour, tophi and aggregates. Calprotectin is a major granulocyte protein being a sensitive marker of inflammation.
WHAT THIS STUDY ADDS
The present findings of associations between MSU crystal deposition, calprotectin levels and carotid pathologies may suggest that crystal deposition contributes to subclinical inflammation with subsequent vascular implications.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Elimination of MSU crystal deposits by prolonged use of urate lowering therapy in patients with gout may reduce subclinical inflammation and the development of vascular pathology as well as gout flares and tophi.
Introduction
Gout is caused by deposition of monosodium urate (MSU) crystals in joints and/or extra-articular tissues and gout has increased in incidence the last decades.1 Evidence describes associations between gout and cardiovascular disease.2–4 High urate levels and presence of subcutaneous tophi have both been associated with an increased risk of mortality in patients with gout, and it was suggested that total body urate load could be a plausible pathophysiological link between gout and cardiovascular disease.5 The volume of crystal deposition measured with dual-energy CT (DECT) has been found to be a biomarker for the risk of developing new cardiometabolic diseases.6 Ultrasound of the carotids detected atheroma plaques in about half of the gout patients7 and silent deposition of MSU crystals in patients with asymptomatic hyperuricaemia have been associated with more severe coronary calcification, suggesting more severe cardiovascular disease.8
Calprotectin (S100A8/A9, MRP8/MRP14) is a major granulocyte and monocyte protein released during cell activation and turnover, and is a sensitive marker of inflammation.9 Calprotectin was released by MSU crystal-stimulated neutrophils10 and calprotectin levels were elevated in the synovium, tophi and serum of patients with gout and correlated with disease activity.11 Increased levels of calprotectin have been suggested to be a link between chronic inflammation and the risk of cardiovascular disease in gout patients.12 This is supported by studies where the calprotectin level was identified as a biomarker for prediction of mortality in patients with heart failure and associated with systemic inflammation in stable coronary atherosclerosis.13
DECT and ultrasound are both included in the classification criteria for gout.14 Ultrasound detects crystal deposition in patients with gout, and the OMERACT ultrasound group has defined the following typical gout lesions caused by crystal deposition; double contour (DC), tophi and aggregates,15 and a scoring system has been developed.16
MSU crystal deposition can be assessed by ultrasound, MSU crystals may induce release of calprotectin and raised levels of calprotectin may be associated with cardiovascular disease. Thus, the aim of this study was to explore the relationship between a comprehensive ultrasound examination of MSU crystal deposition, inflammatory markers including calprotectin and carotid artery pathologies.
Methods
We used baseline data from the Norwegian gout study (NOR-Gout), a prospective observational study of patients with crystal-proven intercritical gout with increased serum urate (SUA) levels (>360 µmol/L) to undertake a cross-sectional analysis.17 18 Patient representatives with gout participated in the project planning.
Ultrasound and DECT assessment of crystal depositions
As described previously,17 all patients had an extensive ultrasound assessment (GE Logic E9 machine) to assess the elementary lesions of deposition (DC, tophi and aggregates) with bilateral assessment of joints (radiocarpal, MCP 2, MTP 1) cartilage (distal femur (maximal flexed knee) and talus) and tendons (insertion of triceps and quadriceps, proximal/distal patellar and Achilles) scored according to the OMERACT scoring system.16 A sum score was made for each lesion as well as for all three lesions together. In addition, patients were explored for the presence of a large tophus (either clinically visible or the largest tophus (length ≥2 mm) detected by ultrasound) in the regions of elbow, hand, knee, ankle or foot.17 Ankles and feet were examined bilaterally by DECT and scored as described previously.19
Laboratory examinations
Plasma calprotectin was assessed by ELISA (Calpro, normal levels <910 µg/L). Kidney function tests and C reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were assessed as a routine at our hospital laboratory (normal levels; CRP ≤4 mg/L and ESR ≤12 men/≤17 women).
Assessments of the carotid artery
Bilateral B‐mode ultrasound examinations20 were performed to assess the carotid intima–media thickness (cIMT) (increased thickness defined as >0.9 mm). Atherosclerotic plaques were identified as protrusions of ≥1.5 mm or ≥2 times the adjacent IMT.
Statistics
Correlations were performed by use of Spearman’s rank and differences between groups examined by Mann-Whitney test. Linear regression explored each of the crystal deposition parameters separately as independent variable and each of the laboratory markers or carotid assessments separately as dependent variable, all with adjustments for sex, age and disease duration.
Results
From the NOR-Gout study, 202 patients with baseline calprotectin and ultrasound assessments were included (95.5% men, mean (SD) age 56.5 (13.8) years, disease duration 7.9 (7.7) years). The mean (SD) body mass index (BMI) was 28.8 (4.6), 43.4% had never smoked, 44.5% had smoked previously and 9.8% smoked ≤10 cigarettes per day. Calprotectin levels had no significant correlation with BMI or smoking.
Imaging results
The mean (SD) sum sore of DC was 4.4 (3.5), tophi 6.6 (6.6), aggregates 9.3 (5.6). A large tophus was detected in 50 patients (24.8%) (mean (SD) length 18 (22) mm).17 DECT was performed in 179 patients (88.6%) with mean (SD) sum score of 4.6 (6.3) (range 0–24).
Laboratory results
Mean (SD) of calprotectin was 801 (525) µg/L, CRP 7 (14) mg/L, ESR 14 (14) mm/hour, SUA 499 (77) μmol/L, creatinine 96 (19) μmol/L and estimated glomerular filtration rate 78 (19) mL/min/1.73 m2.
Carotid artery examinations
A total of 122 (60.4%) of the patients had assessments of cIMT and for presence of carotid artery plaques. Of these patients, 22 (18.0%) had increased cIMT and 67 (54.9%) had carotid artery plaque. cIMT at right or left side and sum both sides were substantially associated with age (correlation coefficient (r)=0.52–0.63, p<0.001), presence of plaque was higher with age (p<0.001), but carotid pathologies (cIMT and plaques) were not associated with sex or gout disease duration.
Correlations between crystal deposition, laboratory and carotid examinations
Table 1 shows the correlations between the ultrasound scores of crystal deposition and the inflammatory markers, showing highest correlations with calprotectin (table 1). In addition, DECT was correlated with calprotectin (r=0.15, p=0.039), but not with CRP or ESR.
Table 1.
Spearman’s rank correlations at baseline of 202 patients with gout
| Calprotectin | CRP | ESR | SUA | Creatinine | eGFR | |
| CRP | 0.63* | |||||
| ESR | 0.49* | 0.66* | ||||
| S-urate | 0.23† | 0.14† | 0.06 | |||
| Creatinine | 0.23† | 0.18† | 0.22† | 0.31* | ||
| eGFR | −0.26* | −0.23† | −0.35* | −0.17† | −0.89* | |
| Sum score double contour | 0.26* | 0.20† | 0.20† | 0.32* | 0.27* | −0.26* |
| Sum score tophi | 0.32* | 0.25* | 0.28* | 0.15† | 0.30* | −0.40* |
| Sum score aggregates | 0.28* | 0.18† | 0.22† | 0.09 | 0.27* | −0.40* |
| Sum scores double contour, tophi and aggregates | 0.31* | 0.24† | 0.27* | 0.20† | 0.33* | −0.43* |
*P<0.001.
†P<0.05.
CRP, C reactive protein; eGFR, estimated glomerular filtration rate; ESR, erythrocyte sedimentation rate; S-urate, serum urate.
The cIMT was correlated with sum score aggregates; right cIMT: r=0.18 (p=0.045), left cIMT: r=0.21 (p=0.019) and sum bilateral cIMT: r=0.22 (p=0.013). However, there were no significant correlations between cIMT and sum scores of DC, tophi or DECT.
Associations between presence of inflammation/carotid artery pathologies and crystal load
Twenty-seven per cent of the patients had elevated calprotectin levels and they had the highest sum scores of each of, and sum of, the three elementary lesions (p≤0.001) (figure 1), as well as the highest DECT scores (p=0.044). Thirty-four per cent of patients had elevated CRP levels and they had the highest sum scores for tophi and aggregates as well as sum scores for all three elementary lesions (p≤0.03). Thirty-seven per cent of patients had elevated ESR and they had higher levels of sum scores for tophi as well as sum scores for all the three elementary lesions (p≤0.02). However, patients with elevated CRP or ESR did not have higher DECT scores.
Figure 1.
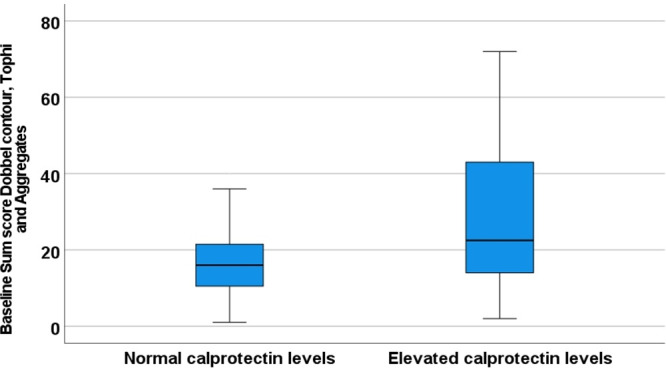
With elevated calprotectin levels had significantly higher crystal load (p<0.001) than patients with normal calprotectin levels.
Eighteen per cent of patients with pathological cIMT (at one or both sides) and the 54.9% of patients with presence of carotid plaque had higher levels of aggregate sum score (p=0.003 and p=0.037, respectively).
Associations between presence of tophus and inflammation/carotid artery pathologies
Patients with a large tophus had higher levels of calprotectin (p=0.03), presence of carotid plaque (p=0.049) and higher sum scores for each of the three ultrasound elementary lesions (p<0.001). However, CRP, ESR or cIMT showed no differences between patients with or without a large tophus.
Regression analyses between crystal deposition and laboratory/carotid artery examinations
In the linear regression analyses, calprotectin and ESR were both associated with each elementary lesion sum score and with the three elementary lesions sum score (p<0.001) and calprotectin was associated with DECT (p=0.003). CRP was associated with sum scores for DC and tophi as well as the sum score for all three elementary lesions (p≤0.02). However, neither CRP nor ESR was associated with DECT. In addition, neither cIMT nor presence of plaque was associated with sum score for any of the ultrasound lesions separately or together nor DECT score.
Discussion
To the best of our knowledge, this is the first large study examining intercritical gout patients with assessments of MSU crystal deposits by both ultrasound and DECT to explore associations with inflammation and carotid pathology. We found calprotectin levels to be associated with the crystal deposits assessed by both ultrasound and DECT. In addition, both cIMT and carotid plaques were associated with aggregates of MSU crystals detected by ultrasound. Thus, this study suggests that MSU crystal deposition is associated with inflammation and carotid pathology in gout patients.
Metabolic syndrome is associated with inflammation. However, calprotectin was presently not correlated with BMI. The associations between inflammatory markers, especially calprotectin levels, and crystal depositions were robust and observed for all forms of depositions. Calprotectin reflects the degree of leucocyte activation, and even if there may be several causes for increased levels, the present findings may indicate that MSU crystal depositions initiate a local inflammation causing release of calprotectin.
We found cIMT to be associated with ultrasound aggregates, but not to DC or tophi. Aggregates may be the form of deposition that is generated first in gout and is the slowest to disappear during urate lowering treatment.17 In addition, presence of large tophus was associated with presence of carotid plaque, which may reflect a long-time deposition of crystals being associated with the gradual development of carotid plaques.
Strengths of this study are the high number of patients assessed by comprehensive assessments of MSU crystal deposition as well as sensitive examinations for inflammatory markers and carotid pathology. Limitations includes the one centre design, no control group and that not all patients had carotid and DECT assessments as well as a cross-sectional design that prevents evaluation of causalities.
As conclusion, in gout patients studied during an intercritical period, higher loads of MSU crystal deposition as assessed by ultrasound and DECT were associated with increased levels of inflammatory markers as well as cIMT and presence of atherosclerotic plaques in the carotid arteries. These findings may have several explanations. However, they may indicate that MSU crystal depositions could contribute to subclinical inflammation with subsequent vascular implications. This study has a cross-sectional design, and future longitudinal and targeted studies are needed to confirm a causal relationship.
Acknowledgments
We want to thank Gina Stenberg, Anita Reinhard, Heidi Lunøe and Ingerid Müller who contributed as trained study nurses in the NOR-GOUT study, and research secretary Mona Thorkildsen for organisation.
Footnotes
Collaborators: Not applicable.
Contributors: HBH has made a substantial contributions to the conception and design of the work; the acquisition of data, the statistical analysis, interpretation of data for the work; and drafted the manuscript as well as revising it critically for important intellectual content; and given a final approval of the version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SR has given substantial contributions to the design of the manuscript, the acquisition of data, as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. GJ has given substantial contributions to the design of the manuscript, the acquisition of data, as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. LFK has given substantial contributions to the design of the manuscript, the acquisition of data, as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. LT has given substantial contributions to the design of the manuscript as well as the analysis and interpretation of data for the manuscript; and revising the manuscript critically for important intellectual content; and given final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. EAH has given substantial contributions to the design of the manuscript as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. TKK has given substantial contributions to the design of the manuscript as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AGS has given substantial contributions to the design of the manuscript, the acquisition of data, as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. TU has given substantial contributions to the design of the manuscript, the acquisition of data, as well as the interpretation of data for the work; and revised the manuscript critically for important intellectual content; and given a final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: Dr. Hammer reports personal fees from AbbVie, Lilly, UCB and Novartis, outside the submitted work. Dr. Rollefstad has no disclosures. Msc Jensen has no disclosures.Dr. Karoliussen has no disclosures.Dr. Terslev reports personal fees from Novartis, Roche, BMS and Pfizer outside the submitted work.Dr. Haavardsholm reports personal fees from Pfizer, UCB, Eli Lilly, Celgene, Janssen-Cilag, AbbVie and Gilead outside the submitted work.Dr. Kvien reports grants and personal fees from AbbVie, MSD, UCB, Hospira/Pfizer, Eli-Lilly, grants from BMS, personal fees from Roche, Hikma, Orion, Sanofi, Celltrion, Sandoz, Biogen, Amgen, Egis, Ewopharma and Mylan, outside the submitted work.Dr. Semb has received speaker honoraria and/or consulting fee from Novartis, AbbVie, Sanofi, KPMG, Bayer and Lilly and a collaborative agreement for independent research from Eli Lilly outside the submitted work.Dr. Uhlig reports personal fees from Galapagos, Grünenthal, Novartis, Pfizer, SOBI and UCB outside the submitted work.
Patient and public involvement statement: Two patient research partners participated in the project and took part in the discussion of the research questions and outcome measures.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
The data will be shared if there is a reasonable request for it.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the Norwegian Regional Committee for Medical and Health Research Ethics approved the study. Reference number 2015/990. Participants gave informed consent to participate in the study before taking part.
References
- 1.Lim SY, Lu N, Oza A, et al. Trends in gout and rheumatoid arthritis hospitalizations in the United States, 1993-2011. JAMA 2016;315:2345–7. 10.1001/jama.2016.3517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cox P, Gupta S, Zhao SS, et al. The incidence and prevalence of cardiovascular diseases in gout: a systematic review and meta-analysis. Rheumatol Int 2021;41:1209–19. 10.1007/s00296-021-04876-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clarson LE, Chandratre P, Hider SL, et al. Increased cardiovascular mortality associated with gout: a systematic review and meta-analysis. Eur J Prev Cardiol 2015;22:335–43. 10.1177/2047487313514895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calabuig I, Martínez-Sanchis A, Andrés M. Sonographic tophi and inflammation are associated with carotid atheroma plaques in gout. Front Med 2021;8:795984. 10.3389/fmed.2021.795984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perez-Ruiz F, Martínez-Indart L, Carmona L, et al. Tophaceous gout and high level of hyperuricaemia are both associated with increased risk of mortality in patients with gout. Ann Rheum Dis 2014;73:177–82. 10.1136/annrheumdis-2012-202421 [DOI] [PubMed] [Google Scholar]
- 6.Marty-Ané A, Norberciak L, Andrès M, et al. Crystal deposition measured with dual-energy computed tomography: association with mortality and cardiovascular risks in gout. Rheumatology 2021;60:4855–60. 10.1093/rheumatology/keaa920 [DOI] [PubMed] [Google Scholar]
- 7.Andrés M, Bernal JA, Sivera F, et al. Cardiovascular risk of patients with gout seen at rheumatology clinics following a structured assessment. Ann Rheum Dis 2017;76:1263–8. 10.1136/annrheumdis-2016-210357 [DOI] [PubMed] [Google Scholar]
- 8.Andrés M, Quintanilla M-A, Sivera F, et al. Silent monosodium urate crystal deposits are associated with severe coronary calcification in asymptomatic hyperuricemia: an exploratory study. Arthritis Rheumatol 2016;68:1531–9. 10.1002/art.39581 [DOI] [PubMed] [Google Scholar]
- 9.Romand X, Bernardy C, Nguyen MVC, et al. Systemic calprotectin and chronic inflammatory rheumatic diseases. Joint Bone Spine 2019;86:691–8. 10.1016/j.jbspin.2019.01.003 [DOI] [PubMed] [Google Scholar]
- 10.Ryckman C, Gilbert C, de Médicis R, et al. Monosodium urate monohydrate crystals induce the release of the proinflammatory protein S100A8/A9 from neutrophils. J Leukoc Biol 2004;76:433–40. 10.1189/jlb.0603294 [DOI] [PubMed] [Google Scholar]
- 11.Holzinger D, Nippe N, Vogl T, et al. Myeloid-Related proteins 8 and 14 contribute to monosodium urate monohydrate crystal-induced inflammation in gout. Arthritis Rheumatol 2014;66:1327–39. 10.1002/art.38369 [DOI] [PubMed] [Google Scholar]
- 12.Kienhorst LBE, van Lochem E, Kievit W, et al. Gout is a chronic inflammatory disease in which high levels of interleukin-8 (CXCL8), myeloid-related protein 8/Myeloid-Related protein 14 complex, and an altered proteome are associated with diabetes mellitus and cardiovascular disease. Arthritis Rheumatol 2015;67:3303–13. 10.1002/art.39318 [DOI] [PubMed] [Google Scholar]
- 13.Baumann M, Schmaderer C, Burkhardt K, et al. MRP8/14 is associated with systemic inflammation in stable coronary atherosclerosis in men. Eur J Clin Invest 2011;41:1261–7. 10.1111/j.1365-2362.2011.02530.x [DOI] [PubMed] [Google Scholar]
- 14.Neogi T, Jansen TLTA, Dalbeth N, et al. 2015 gout classification criteria: an American College of Rheumatology/European League against rheumatism collaborative initiative. Ann Rheum Dis 2015;74:1789–98. 10.1136/annrheumdis-2015-208237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Terslev L, Gutierrez M, Christensen R, et al. Assessing elementary lesions in gout by ultrasound: results of an OMERACT patient-based agreement and reliability exercise. J Rheumatol 2015;42:2149–54. 10.3899/jrheum.150366 [DOI] [PubMed] [Google Scholar]
- 16.Christiansen SN, Filippou G, Scirè CA, et al. Consensus-Based semi-quantitative ultrasound scoring system for gout lesions: results of an OMERACT Delphi process and web-reliability exercise. Semin Arthritis Rheum 2021;51:644–9. 10.1016/j.semarthrit.2020.11.011 [DOI] [PubMed] [Google Scholar]
- 17.Hammer HB, Karoliussen L, Terslev L, et al. Ultrasound shows rapid reduction of crystal depositions during a treat-to-target approach in gout patients: 12-month results from the NOR-Gout study. Ann Rheum Dis 2020;79:1500–5. 10.1136/annrheumdis-2020-217392 [DOI] [PubMed] [Google Scholar]
- 18.Uhlig T, Karoliussen LF, Sexton J, et al. 12-Month results from the real-life observational treat-to-target and tight-control therapy NOR-Gout study: achievements of the urate target levels and predictors of obtaining this target. RMD Open 2021;7:e001628. 10.1136/rmdopen-2021-001628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uhlig T, Eskild T, Karoliussen LF. Two-Year reduction of dual-energy CT urate depositions during a treat-to-target strategy in gout in the NOR-Gout longitudinal study.. Rheumatology (Oxford). 2021. 10.1093/rheumatology/keab533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Semb AG, Rollefstad S, Provan SA, et al. Carotid plaque characteristics and disease activity in rheumatoid arthritis. J Rheumatol 2013;40:359–68. 10.3899/jrheum.120621 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data will be shared if there is a reasonable request for it.


