Abstract
The COVID-19 pandemic has changed how care is being delivered in Canada. With conventional in-person care being transitioned to virtual care, the approach that patients are able to engage and access their care has dramatically changed. At the University Health Network (UHN), which is Canada's largest academic and teaching hospital network, we expanded the myUHN Patient Portal in 2017 after its early adopter phase to enable patients and family members to view parts of their clinical notes and test results. As the pandemic progressed, we observed high adoption of myUHN to support virtual care and rapid delivery of COVID-19 test results in real time. In this article, we share and reflect on our experience of adapting myUHN to support the demands of the pandemic, including portal adoption outcomes across multiple waves of the pandemic, the impetus for increased patient experience staff dedicated for myUHN support, and patients’ perceptions of the value of the portal and virtual care. Based on these reflections, we outline our perspectives on the future role of patient portals to support patient care and experience in a post-pandemic environment.
Keywords: patient portal, patient education, pandemic, experiences, health informatics
Introduction
Since March 2020, the COVID-19 pandemic has significantly changed on how clinicians are delivering care in Canada (1). With in-person consults and nonessential care reduced to a minimum, this has led to significant changes in how patients are able to interact with their care providers, and receive the necessary treatment for both primary care (2) and specialty care (3,4). As the world continues to manage the unexpected “waves” of the pandemic, these changes are likely to have a lasting impact on the delivery of care during and beyond the pandemic (5).
In this regard, digital health tools such as virtual care and patient portals have been identified to be instrumental tools to support the delivery of health care (6) and have become a staple of medicine moving forward (7). In particular, patient portals have been identified as a critical tool in supporting the continuity and access to care throughout the pandemic (8). For instance, accessing telehealth appointments through the portal, modifying scheduling guidelines to reduce in-person visits, and frequent messaging to increase awareness of new modes of access as COVID-19 regulations change and encourage scheduling appointments (8,9). In the context of COVID-19, patient portals allow patients to view their test and lab results, message their care providers with any concerns, book appointments and seek relevant patient education materials (10,11). Previous studies have purported that patient portals can support patient empowerment and engagement throughout care delivery and encourage shared decision making between patients, families, and clinicians (12). While patient portals continue to be implemented within health systems across North America, the use of these portals for care delivery remains inconsistent, where the level of integration within clinic workflows varies across health organizations and even clinics within a health organization (13). Additionally, reporting on the impact of portals on patient experience and perception of quality of care is limited and predominately qualitative (ie, interview) data (14,–16). Moreover, while these platforms have become a key mechanism for supporting the management of the pandemic, there is a lack of evidence and data about the adoption and use of portals over the last 18 months in the Canadian setting. However, one case (9) in the United States reported that portal activation during the pandemic significantly increased from 18% in February 2020 to 44% in April 2021 at the Nationwide Children's Hospital Primary Care Network in Ohio and another reported an increase from 3,511 in January 2020 to 10,077 in May 2020 at UCHealth in Colorado (17). The forced shift in care models during the pandemic yields unique insights to inform how these solutions can be better positioned to support care delivery and better health outcomes during and beyond the pandemic (18,19).
At the University Health Network (UHN), which is Canada's largest academic and teaching hospital network, myUHN Patient Portal was developed starting in 2012, piloted in 2015, and expanded to all hospital sites in 2017, using a user-centered design approach (20). myUHN enables patients and authorized proxies to see their appointment details, labs, test results, and clinical reports, as well as access to relevant patient education materials (21). myUHN shares many similarities to other patient portals; however, it does not include a messaging feature for two-way secured communication between patient and provider (13). Shortly before the COVID-19 pandemic, the portal was expanded to include all lab results in Ontario from the Ontario Laboratory Information System (OLIS), which is the provincial information repository for lab test information (21). For patients to gain access to myUHN, they are offered a registration code during their visit from their health care team, or can ask for one (ie, codes offered) to create their account (ie, accounts created) (22). Throughout the COVID-19 pandemic, we witnessed an overwhelming and rapid adoption of myUHN. Currently, there is a 71% adoption rate where the total number of registered users (ie, accounts created) is 263,418 out of 368,704 codes offered (as of February 29, 2022). The average number of codes offered daily, and accounts created daily are 230 and 104, respectively. This is a significant increase compared to prior the pandemic where there was a total of 103,986 registered users (as of February 29, 2020), in which the average number of codes offered daily was 9 and accounts created daily was 43. It is evident that the role of myUHN and integrative support model has been instrumental in supporting the delivery of care during the pandemic.
In this commentary, we share the experience of our organization in the rapid adoption of myUHN during the pandemic. In particular, by reflecting on the analytics data for the portal and recent survey results with patients and families, we discuss the role that myUHN and the patient experience myUHN support team have played during the pandemic. Based on these reflections, we outline areas of opportunities and recommendations for expanding the value of patient portals in supporting care delivery during and beyond the pandemic.
Portal Usage During the COVID-19 Pandemic
Early Pandemic Portal Adoption and Transformed Staff Support Model
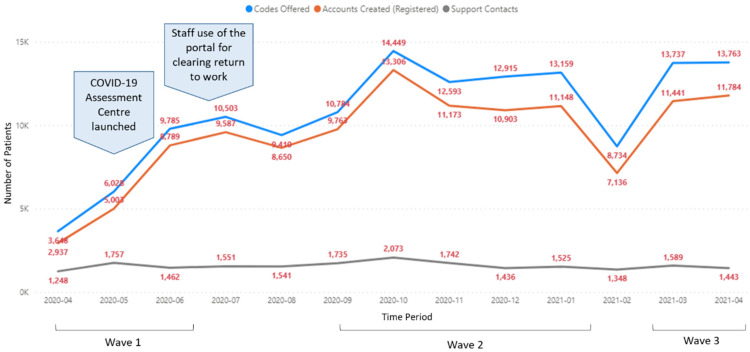
During the pandemic, as outlined in Figure 1, there was a significant increase in levels of adoption of myUHN (ie, trends of the number of codes offered and number of accounts created as a result of the code offering). When the first wave of the pandemic was officially announced on March 11, 2020 by the World Health Organization (23), hospital activities were reduced and nonurgent ambulatory consultations (eg, follow-ups) were transitioned to virtual care. Within the month, a virtual care infrastructure was rapidly set up to support virtual visits using Microsoft Teams and Ontario Telemedicine Network (OTN) (24,25). In terms of the role of myUHN, patients were able to identify if and when they have been provided with a virtual care appointment in real time. As opposed to receiving an updated appointment time in the mail, patients and family members have real-time access to appointment updates and changes without delay. This is particularly useful given the rapid changes in pandemic status over time and a significant increase in virtual visit appointments, as a result. In addition, patients and authorized proxies are able to review their Ontario lab results (both organizational and those available through the OLIS) and UHN clinical reports such as imaging reports, discharge summaries on the portal. This likely contributed to the increased adoption of the portal since March 2020.
Figure 1.
Adoption rates for the myUHN Patient Portal between April 2020 and April 2021. Codes offered (blue) are the number of registration codes provided to patients to sign up for the myUHN Patient Portal. Accounts created (orange) are the number of successfully created accounts. Support contacts (gray) are the number of inquiries about the myUHN Patient Portal.
With these new features and access to COVID-19-related information, as Ontario entered the first wave in March 2020, myUHN inquiries increased. It was recognized that more support staff were needed to help manage the e-mail and call volumes. Prior to the pandemic, myUHN Support was a small team of 3 staff, 1 manager, and 2 coordinators. Patient Experience staff from the patient and family learning centers, patient education, and patient partnerships program volunteered part time to assist myUHN Support with the e-mail and call volumes.
In May 2020, the Toronto Western COVID-19 Assessment Centre was implemented at the organization and the center offered rapid COVID-19 testing to Canadians that met the criteria for screening. As an alternative to receiving a follow-up phone call with a member of the clinical team, individuals being tested were provided the option to get an account for the myUHN to see their COVID-19 results in real time. The availability of this feature was consistent with the sharp increase that was observed from May 2020 to October 2020 (Figure 1).
In addition, during this month, there was also a reported outbreak that occurred at one of the organization sites (26). This led to the need for a large number of staff COVID-19 testing. Given the ongoing challenges related to staffing, myUHN was a platform for staff members to sign up and get their COVID-19 test results in real time. This reduced uncertainty and the time required for staff to learn their status, ability to return to work, and requirements for isolation and quarantine. The use of myUHN evolved from its original purpose and became a critical facilitator in informing staff about their testing status in the case of an outbreak. The implementation of this functionality was consistent with the steeper increase in portal adoption at that time.
This evolved purpose of myUHN was also crucial for patient and family safety since staff was being redeployed within and outside of the organization to assist with COVID-19 screening, care delivery, and other efforts. For instance, during this time period (May to October 2020), 3 staff from UHN Digital were redeployed to help myUHN Support manage the volume of inquiries. Of all the support queries from patients and families, a significant proportion of the queries (n = 976) were related to COVID-19. In terms of the approach for inquiry, most queries came through email (n = 618), calls (n = 354), and social media (n = 4). Questions to myUHN Support ranged from how to register for myUHN, how to have a virtual visit, patients looking for their COVID-19 results and understanding what they mean, whether patients should come to the hospital, how can a caregiver visit a loved one on an inpatient unit or attend an appointment and beyond. The redeployed staff were able to add their clinical and technology backgrounds to the support team, which was invaluable. For example, they suggested using Microsoft Teams for training and onboarding, setting up three-way calls with families or translators, and long-distance calling. Furthermore, they were able to use their digital education background to teach digital literacy to elderly patients and learn patient experience practices to further support patients and their loved ones. Teamwork was an essential component to the success and positive experience of this redeployment phase for the myUHN Support staff. Thus, the existing support desk for myUHN became a vehicle to support the COVID-19 journey and acted as a point of contact for navigation of the healthcare system. The updated integrative support model that is now in use provides patients with a safe space to seek help remotely and not at the clinic.
Ongoing Adoption Trends
Subsequently, during the second (September 2020 to February 2021) and third waves (March 2021 to Present) of the COVID-19 pandemic, the trends in adoption of myUHN followed the emergence of each pandemic wave. When the Province of Ontario announced restrictions to schools and health care to combat the second wave, we observed another spike in the adoption of myUHN, as well as support calls and emails from patients and families. Similarly, as some clinical operations were being restored in February, the adoption rate of myUHN as well as support calls and emails decreased. This decrease was diminished when a subsequent stay-at-home order was implemented to address the rising COVID-19 cases in the intensive care unit (ICU). Possibly contributing to this decrease was also the provincial long weekend, where typically there is a decrease in portal registrations (22) in addition to the high proportion of frontline staff who would have received their first or second covid vaccination dose in previous months.
Perspectives of Patients and Families on the Use of myUHN During the COVID-19 Pandemic
As part of the organizational priority toward evaluation and improvement of the user experience, over 10% of myUHN users (n = 16,498 out of 143,129) responded to a survey that was sent out by myUHN Support in September 2020 to all myUHN users to better understand how our patients used myUHN during the pandemic. myUHN users can be individuals (patients or caregivers) from any of the 4 UHN care delivery sites: Toronto General Hospital, Toronto Western Hospital (that includes the COVID-19 Assessment Centre), Princess Margaret Cancer Centre, and Toronto Rehabilitation Institute (27). Majority of patients are from the Greater Toronto Area; however, some individuals from other parts of Ontario and other provinces or countries come to UHN to receive specialized or urgent care. Majority of survey respondents self-identified as a UHN patient (n = 14,737), followed by caregiver (n = 868) and both a patient and caregiver (n = 610).
In general, 83% of respondents (n = 13,657) reported that myUHN was very helpful (n = 9,655) or helpful (n = 4,002) during the pandemic. Of those who starting using myUHN during the COVID-19 pandemic (March to September 2020; n = 3,098, 19%), about 55% of respondents (n = 1,697) used the portal to view their COVID-19 PCR results, 43% (n = 1,324) looked at lab results and reports for their care and 42% (n = 1,296) looked at the appointments tab. In addition, 16% (n = 491) used the portal to help or refer to when speaking with their health care providers, and 6% (n = 194) looked at patient education resources. Of the respondents that used the portal to view their COVID-19 results, 97% (n = 1,632) reported that it was very useful (n = 1,421, 85%) or useful (n = 211, 13%) to do so through the portal.
Since the start of the pandemic, 66% (n = 10,907) of respondents reported through the survey that they had a telephone and/or video visit at UHN. Of these respondents, they reported that using myUHN helped them prepare for or referred to it during the virtual care appointments, where over 70% of respondents used the portal to view their appointments tab (n = 8,495) or results and reports (n = 8,191).
Timely access to labs and results, tracking appointments, and being able to view and share UHN clinician input with other clinicians within their circle of care were the primary reasons that respondents felt that myUHN was useful, particularly during the pandemic (Table 1). Some respondents further noted that with this kind of access to their own or a loved ones’ health information, they were able to gather their thoughts in advance, put together questions, and prepare for discussions with clinicians in their circle of care.
Table 1.
Direct quotes from patients and families in response to “How Helpful is the myUHN Patient Portal During the COVID-19 Pandemic (March 2020-Now), and Why?”.
| Category | Quotes |
|---|---|
| Timely access | “I am in another city. My appointments with Dr. E are extremely important. With
myUHN I have direct access to my results, reports, appointments, and
correspondence. It helps the patient feel more in control of their
health.” “I am not allowed into the hospital with patient, this allows me to see his tests and results.” “Allows me to stay informed about my care without having to come into contact with too many people.” “Adding the Ontario labs to the portal allows for quick review of labs etc and to be sure results available and easily accessible by MDs as well as myself” “The portal is helpful at any time but during this pandemic, I think we are all more anxious about our health. Being able to check or results assures us that we are fine without having to leave home.” |
| Tracking appointments | “I am notified of any appointment changes immediately so I can reschedule my
time. I can read my test results and doctors’ evaluations and recommendations
online very quickly after the test is done.” “I don't need to spend a long time over telephone to get and change appointment date. And also, I can see my lab results on my computer and can make as many copies as I need. I can see the referral letters and report back to my family physician. It is important for transparency.” “We received information about a new appointment made for us and instructions for restrictions set up for then because of COVID-19.” |
| Preparing for conversations with clinicians | “Keeps me informed about appointments, results of tests, and input from the
doctor. Let's me prepare for discussions with the doctor and gather my thoughts in
advance.” “I can now check relevant medical reports prior to having telephone conversation with treating specialist as only telephone contacts during COVID-19 Pandemic.” “Ability to review physician's report following consultation confirms the discussion. It is not always easy to remember what has been said so i appreciate the written report.” |
From the survey, there is a strong indication of the important role that myUHN had in communication and continuity of care. The ability to stay engaged with their care providers at home or in the community closes the gap that was created due to the impact of care during the pandemic.
Areas of Opportunities and Recommendations for Improving Patient Experience With Patient Portals
The COVID-19 pandemic has greatly accelerated the use of digital technologies including the patient portal (28,–30). In our experience with myUHN, we found that the platform was instrumental in addressing and mitigating patient access and experience challenges created by the COVID-19 pandemic. In particular, myUHN has become an essential platform in supporting the needs of patients and families during these unprecedented times. From this experience, we have identified several lessons learned and future directions of how the value of the patient portal can be maximized during and beyond the pandemic.
The implementation of the features of myUHN was conducted in close collaboration and co-design with patients, caregivers, and staff (31). While these efforts required additional time and resources throughout the design, implementation, and optimization of the platform, we consider it a hallmark of the large adoption rate and integrative use of myUHN across all domains of care (22). Future digital models of care should position patients and caregivers front and center throughout all stages of the health IT development lifecycle (32,33). This includes having a dedicated patient experience team to manage patient experience evaluations and also ensures that the portal is promoted and integrated into the patient journey. The close collaboration with key stakeholders and end users such as patients, families, and clinicians, allows for the early identification of challenges and bottlenecks that can jeopardize the success of the patient portal.
In terms of features, the need for real-time access to data and information has been instrumental in the success of the patient portal (34). As consistent with our previous survey evaluations (35), delivering COVID-19 results in real-time to patients and families without significant delay was found to be useful. The immediate notification of the results can reduce anxiety caused by waiting time as well as allow patients and families to resume normal activities if the COVID-19 test was negative. Additionally, access to patient results and care notes has been reported to support patient safety and experience (36,37). Patients who have questions could call the support line for assistance. For staff, this means that they would be able to receive notification and return to work faster and likely a reduction in administrative tasks (eg, calling each staff member to inform them of their results). While previous studies have hinted at concerns regarding the interpretation of results without clinical guidance (38,39), our experience demonstrates that delivering basic tests such as the COVID-19 results without clinical guidance is sufficient in most cases. Moreover, timely access to lab results, beyond those COVID-19-related could support virtual visits and care, enhancing patient-centered communication and engagement (40,41). Additional information could potentially be followed up by email or phone calls.
Throughout the pandemic, digital tools including virtual care and myUHN, were implemented at speeds never seen before (42,43). While these tools each have their own objectives as part of clinical care delivery, interoperability is essential and the service should be delivered collaboratively in order to maximize its value (32). For example, the patient portal can act as a mode of transparency and communication (eg, appointment reminders) that enables easy access to virtual care. Judson and colleagues had integrated a COVID-19 self-triage and scheduling tool within the UCSF patient portal to reduce burden and unnecessary messaging to patients (10). However, in order to realize the full value of these tools, developing seamless digital models of care is critical to ensuring a smooth and sensible user experience for patients and families (44,45). While these tools are often identified to be conducive to patient care, the lack of a synthesized and evidence-driven approach can lead to lukewarm adoption and success in real-world environments (46).
Lastly, upon reflecting on our experience with expanding myUHN to meet the needs of patients and families, issues related to digital literacy and health equity must not be forgotten (47). With real-time COVID-19 results and appointment bookings now accessible on the platform, it is important that we do not exclude disadvantaged and marginalized populations that may not have the technology requirements and knowledge to use the portal and reap its benefits (48,–50). For example, some older populations who are not familiar with the internet may not be comfortable with using myUHN for their lab and test results. In this regard, providing alternative approaches for those who choose or may not be able to use the patient portal is critical. In our case, providing a dedicated support line to extend assistance was useful in supporting patients and families to navigate the healthcare system and use the portal to their full potential. Recurring questions that the dedicated support line has received also yielded important insight into further patient education opportunities. For example, this has led to the development of patient education resources on COVID-19 testing and strategic directions on how to better support care delivery through education (51). Patients and families must be better equipped to use the virtual solutions being delivered as part of digital models of care (52).
Moreover, organizations should perform their due diligence and continuously evaluate what are the current barriers to portal use, what are the gaps in resources and navigation or support systems in place to mitigate these barriers, and how effective are the current resources and navigation or support systems in terms of meeting patient needs and preferences. Future directions include exploring digital health inequities, identifying if the patient portal population is a representative sample of the larger health organization population, and understanding why patients and families did not complete portal registration after being offered a code. In addition, it would be useful to look at data use cases and specific associations between portal usage and indicators of patient experience, (eg, retention in care, appointment no-shows/cancelations).
Conclusion
As the COVID-19 pandemic accelerates the adoption of digital tools (53), myUHN continues to play a critical role in supporting the delivery. From our reflection and experience with expanding the portal to meet the rapidly changing demands of the environment, we highlight the need for a comprehensive service model in order to maximize the value of the patient portal. These models should be developed in close collaboration with patients and families, and should consider emerging concepts (eg, health equity and digital health literacy) that ensure inclusivity and access as we continue to expand the digital health care environment.
Acknowledgments
The authors would like to acknowledge the UHN Digital Team as well as the UHN patients and patient partners for their support with this work.
Footnotes
Author’s Contribution: DW, BL, RC, and LW conceived the idea for this article; BL and RC led the writing of the first draft of the paper with support from VB, SL; all authors reviewed and provided substantial edits to the manuscript. All authors reviewed and approved the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Not applicable.
Consent to Participate: Not applicable.
Consent for Publication: Not applicable.
Availability of Data and Material: Not applicable.
Code Availability: Not applicable.
ORCID iD: David Wiljer https://orcid.org/0000-0002-2748-2658
References
- 1.Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193:E200-10. DOI: 10.1503/cmaj.202303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Majeed A, Maile EJ, Bindman AB. The primary care response to COVID-19 in England’s National Health Service. J R Soc Med. 2020;113:208-10. DOI: 10.1177/0141076820931452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schrag D, Hershman DL, Basch E. Oncology practice during the COVID-19 pandemic. JAMA. 2020;323:2005-6. DOI: 10.1001/jama.2020.6236. [DOI] [PubMed] [Google Scholar]
- 4.Feijt M, de Kort Y, Bongers I, Bierbooms J, Westerink J, IJsselsteijn W. Mental health care goes online: practitioners’ experiences of providing mental health care during the COVID-19 pandemic. Cyberpsychol Behav Soc Netw. 2020;23:860-4. DOI: 10.1089/cyber.2020.0370. [DOI] [PubMed] [Google Scholar]
- 5.Vogel L. Canada has long way to go on virtual care. CMAJ. 2020;192:E227-8. DOI: 10.1503/cmaj.1095851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957-62. DOI: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glauser W. Virtual care is here to stay, but major challenges remain. CMAJ. 2020;192:E868-9. DOI: 10.1503/cmaj.1095884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA. Rapidly converting to “virtual practices”: outpatient care in the era of COVID-19. NEJM Catal Innov Care Deliv. 2020. DOI: 10.1056/CAT.20.0091. [DOI] [Google Scholar]
- 9.Snyder DA, Schuller J, Ameen Z, Toth C, Kemper AR. Improving patient-provider continuity in a large urban academic primary care network. Acad Pediatr. 2022;22:305-12. DOI: 10.1016/j.acap.2021.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Judson TJ, Odisho AY, Neinstein AB, Chao J, Williams A, Miller C, et al. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J Am Med Inform Assoc. 2020;27:860-6. DOI: 10.1093/jamia/ocaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Power K, McCrea Z, White M, Breen A, Dunleavy B, O'Donoghue S, et al. The development of an epilepsy electronic patient portal: facilitating both patient empowerment and remote clinician-patient interaction in a post-COVID-19 world. Epilepsia. 2020;61:1894-905. DOI: 10.1111/epi.16627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antonio MG, Petrovskaya O, Lau F. The state of evidence in patient portals: umbrella review. J Med Internet Res. 2020;22:e23851. DOI: 10.2196/23851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alturkistani A, Greenfield G, Greaves F, Aliabadi S, Jenkins RH, Costelloe C. Patient portal functionalities and uptake: systematic review protocol. JMIR Res Protoc. 2020;9:e14975. DOI: 10.2196/14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McAlearney AS, Sieck CJ, Gaughan A, Fareed N, Volney J, Huerta TR. Patients’ perceptions of portal use across care settings: qualitative study. J Med Internet Res. 2019;21:e13126. DOI: 10.2196/13126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kooij L, Groen WG, van Harten WH. Barriers and facilitators affecting patient portal implementation from an organizational perspective: qualitative study. J Med Internet Res. 2018;20:e183. DOI: 10.2196/jmir.8989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nost TH, Faxvaag A, Steinsbekk A. Participants’ views and experiences from setting up a shared patient portal for primary and specialist health services- a qualitative study. BMC Health Serv Res. 2021;21:171. DOI: 10.1186/s12913-021-06188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Portz JD, Brungardt A, Shanbhag P, Staton EW, Bose-Brill S, Lin CT, et al. Advance care planning among users of a patient portal during the COVID-19 pandemic: retrospective observational study. J Med Internet Res. 2020;22:e21385. DOI: 10.2196/21385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hollander JE, Sites FD. The Transition from Reimagining to Recreating Health Care Is Now. 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0093.
- 19.Herrera V, Finkler N, Vincent J. Innovation and Transformation in the Response to Covid-19: Seven Areas Where Clinicians Need to Lead. 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0087.
- 20.Bakas V. A portal codesigned by patients that promotes a caring safely culture. 2019. https://www.healthpromotioncanada.ca/wp-content/uploads/2019/01/myUHN-patient-portal_S.-Laberge.pdf.
- 21.University Health Network. About myUHN Patient Portal. https://www.uhn.ca/PatientsFamilies/myUHN/Pages/default.aspx.
- 22.Bola J, Charow R, Hope J, Bakas V, Bishop L, Brudnicki S, et al. Adoption strategies for electronic patient portals: employing advanced data mining and analytics. Stud Health Technol Inform. 2019;257:36-41. [PubMed] [Google Scholar]
- 23.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. Geneva2020.
- 24.Brown EM. The Ontario telemedicine network: a case report. Telemed J E Health. 2013;19:373-6. DOI: 10.1089/tmj.2012.0299. [DOI] [PubMed] [Google Scholar]
- 25.Jiang DM, Berlin A, Moody L, Kumar R, Hannon B, Krzyzanowska MK, et al. Transitioning to a new normal in the post-COVID era. Curr Oncol Rep. 2020;22:73. DOI: 10.1007/s11912-020-00956-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.University Health Network. COVID-19 Outbreak Information at UHN. https://www.uhn.ca/Covid19/Pages/Outbreak_Information.aspx.
- 27.University Health Network. About University Health Network. 2020. https://www.uhn.ca/corporate/AboutUHN/Pages/uhn_at_a_glance.aspx.
- 28.Patel PD, Cobb J, Wright D, Turer RW, Jordan T, Humphrey A, et al. Rapid development of telehealth capabilities within pediatric patient portal infrastructure for COVID-19 care: barriers, solutions, results. J Am Med Inform Assoc. 2020;27:1116-20. DOI: 10.1093/jamia/ocaa065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.March CA, Flint A, DeArment D, Gilliland A, Kelly K, Rizzitano E, et al. Paediatric diabetes care during the COVID-19 pandemic: lessons learned in scaling up telemedicine services. Endocrinol Diabetes Metab. 2020:e00202. DOI: 10.1002/edm2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hsu H, Greenwald PW, Laghezza MR, Steel P, Trepp R, Sharma R. Clinical informatics during the COVID-19 pandemic: lessons learned and implications for emergency department and inpatient operations. J Am Med Inform Assoc. 2021;28:879-89. DOI: 10.1093/jamia/ocaa311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCurdie T, Taneva S, Casselman M, Yeung M, McDaniel C, Ho W, et al. Mhealth consumer apps: the case for user-centered design. Biomed Instrum Technol. 2012;(Suppl):49-56. DOI: 10.2345/0899-8205-46.s2.49. [DOI] [PubMed] [Google Scholar]
- 32.Strudwick G, Leung K, McLean D, Booth R, Borycki E, Rossetti S, et al. Patient and Family Engagement in Health Information Technology Initiatives: Findings of a Literature Review, Focus Groups and Symposium. Toronto: Centre for Addiction and Mental Health; 2019. [Google Scholar]
- 33.Kildea J, Battista J, Cabral B, Hendren L, Herrera D, Hijal T, et al. Design and development of a person-centered patient portal using participatory stakeholder co-design. J Med Internet Res. 2019;21:e11371. DOI: 10.2196/11371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Armstrong S. Patient access to health records: striving for the Swedish ideal. Br Med J. 2017;357:j2069. DOI: 10.1136/bmj.j2069. [DOI] [PubMed] [Google Scholar]
- 35.University Health Network. How myUHN Patient Portal can improve care in your clinic. 2015. uhn.ca/corporate/News/Documents/myUHN_infographic.pdf.
- 36.Bell SK, Delbanco T, Elmore JG, Fitzgerald PS, Fossa A, Harcourt K, et al. Frequency and types of patient-reported errors in electronic health record ambulatory care notes. JAMA Netw Open. 2020;3:e205867. DOI: 10.1001/jamanetworkopen.2020.5867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lam BD, Bourgeois F, Dong ZJ, Bell SK. Speaking up about patient-perceived serious visit note errors: patient and family experiences and recommendations. J Am Med Inform Assoc. 2021;28:685-94. DOI: 10.1093/jamia/ocaa293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blease CR, O’Neill SF, Torous J, DesRoches CM, Hagglund M. Patient access to mental health notes: motivating evidence-informed ethical guidelines. J Nerv Ment Dis. 2021;209:265-9. DOI: 10.1097/NMD.0000000000001303. [DOI] [PubMed] [Google Scholar]
- 39.Dendere R, Slade C, Burton-Jones A, Sullivan C, Staib A, Janda M. Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J Med Internet Res. 2019;21:e12779. DOI: 10.2196/12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Avdagovska M, Menon D, Stafinski T. Capturing the impact of patient portals based on the quadruple aim and benefits evaluation frameworks: scoping review. J Med Internet Res. 2020;22:e24568. DOI: 10.2196/24568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jung C, Padman R. Disruptive digital innovation in healthcare delivery: the case for patient portals and online clinical consultations. In: Agarwal R, Selen W, Roos G, Green R. (eds) The Handbook of Service Innovation. London: Springer; 2015:297-318. [Google Scholar]
- 42.Annis T, Pleasants S, Hultman G, Lindemann E, Thompson JA, Billecke S, et al. Rapid implementation of a COVID-19 remote patient monitoring program. J Am Med Inform Assoc. 2020;27:1326-30. DOI: 10.1093/jamia/ocaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gilbert AW, Billany JCT, Adam R, Martin L, Tobin R, Bagdai S, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9. DOI: 10.1136/bmjoq-2020-000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Davenport TA, Cheng VWS, Iorfino F, Hamilton B, Castaldi E, Burton A, et al. Flip the clinic: a digital health approach to youth mental health service delivery during the COVID-19 pandemic and beyond. JMIR Ment Health. 2020;7:e24578. DOI: 10.2196/24578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodriguez-Villa E, Rauseo-Ricupero N, Camacho E, Wisniewski H, Keshavan M, Torous J. The digital clinic: implementing technology and augmenting care for mental health. Gen Hosp Psychiatry. 2020;66:59-66. DOI: 10.1016/j.genhosppsych.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Connolly SL, Kuhn E, Possemato K, Torous J. Digital clinics and mobile technology implementation for mental health care. Curr Psychiatry Rep. 2021;23:38. DOI: 10.1007/s11920-021-01254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020;22:e19361. DOI: 10.2196/19361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rodriguez JA, Clark CR, Bates DW. Digital health equity as a necessity in the 21st century cures act era. JAMA. 2020;323:2381-2. DOI: 10.1001/jama.2020.7858. [DOI] [PubMed] [Google Scholar]
- 49.Ganguli I, Orav EJ, Lupo C, Metlay JP, Sequist TD. Patient and visit characteristics associated with use of direct scheduling in primary care practices. JAMA Netw Open. 2020;3:e209637. DOI: 10.1001/jamanetworkopen.2020.9637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drake C, Lian T, Cameron B, Medynskaya K, Bosworth HB, Shah K. Understanding telemedicine’s “new normal”: variations in telemedicine use by specialty line and patient demographics. Telemed J E Health. 2022;28:51-9. DOI: 10.1089/tmj.2021.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.University Health Network. What Does My COVID-19 Test Result Mean? 2019. https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Documents/Next_Steps_for_Patients_Tested_for_COVID19.pdf.
- 52.Wisniewski H, Torous J. Digital navigators to implement smartphone and digital tools in care. Acta Psychiatr Scand. 2020;141:350-5. DOI: 10.1111/acps.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Torous J, Jan Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Ment Health. 2020;7:e18848. DOI: 10.2196/18848. [DOI] [PMC free article] [PubMed] [Google Scholar]