Abstract
Background
The purpose of this analysis is to evaluate the current evidence with regard to the effectiveness and safety between coiling and clipping in patients with ruptured intracranial aneurysms (RIAs).
Methods
We performed a meta-analysis that compared clipping with coiling between July 2000 and September 2021. PubMed, EMBASE, and the Cochrane Library were searched for related articles systematically. And the treatment efficacy and postoperative complications were analyzed.
Results
We identified three randomized controlled trials and thirty-seven observational studies involving 60,875 patients with ruptured cerebral aneurysms. The summary results showed that coiling was related a better quality of life (mRS0-2; OR=1.327; CI=1.093–1.612; p<0.05), a higher risk of mortality (OR=1.116; CI=1.054–1.180; p<0.05), higher rate of rebleeding (RR=1.410; CI=1.092–1.822; p<0.05), lower incidence of vasospasm (OR=0.787; CI=0.649–0.954; p<0.05), higher risk of hydrocephalous (RR=1.143; CI=1.043–1.252; p<0.05), lower risk of cerebral infarction (RR=0.669; CI=0.596–0.751; p<0.05), lower risk of neuro deficits (RR=0.720; CI=0.582-0.892; p<0.05), and a lower rate of complete occlusion (OR=0.495; CI=0.280-0.876; p<0.05).
Conclusion
Coiling was significantly associated with a better life quality (mRS0-2), a lower incidence of postoperative complications, and a higher rate of mortality, rebleeding, hydrocephalous, and a lower rate of complete occlusion than clipping.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41016-022-00283-3.
Keywords: Ruptured intracranial aneurysms, Coiling, Clipping, Meta-analysis
Background
Aneurysmal subarachnoid hemorrhage (aSAH) is accounted for 80% of cases of nontraumatic subarachnoid hemorrhage (SAH) [1], contributing to significant mortality. There are two procedures for the treatment of aSAH: microsurgical clipping and endovascular coiling [2]. The first clipping operation was published by Walter Dandy in 1937 [3]. In 1991, the Guglielmi detachable coil for coiling was found, putting a platinum coil into a cerebral aneurysm [4]. The goal of treatment was to occlude the aneurysm to reduce the risk of bleeding. Given this purpose, clipping and coiling are both effective, although there remain controversial with regard to which treatment strategies are better for patients with aSAH.
Until 2002, the International Subarachnoid Aneurysm Trial (ISAT) demonstrated that individuals who underwent coiling were associated with a less morbidity and mortality at 1-year follow-up compared with clipping [5]. This finding contributed to endovascular coiling had been widely accepted becoming the preferred strategy of treatment at many centers [6]. However, the results of ISAT also caused some criticism, such as 7416 of the 9559 patients with ruptured intracranial aneurysms (RIAs) were excluded, the location, and type of intracranial aneurysms (IAs) as well as types of recruiting centers were widely different, and the proficiencies of the performer of coiling and clipping were varied [5, 7].
In recent years, some randomized controlled trials (RCTs) and retrospective comparative studies and prospective studies have also been published, and some results of these publications were different from ISAT [8]. As a result, there remains some debate about the choice of coiling and clipping for patients with aSAH, while it is the aim of this meta-analysis and systematic review to evaluate the two treatments’ effectiveness and complications from a great deal of evidence containing RCTs and observational studies to provide a guiding strategy in selecting which treatment methods to perform in patients with aSAH.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [9] was used for this meta-analysis guidelines. And we compared the two treatments by primary outcomes (treatment efficacy) and secondary outcomes (postoperative complications).
Systematic literature search
We searched all literatures with regard to the comparison between coiling and clipping for ruptured intracranial aneurysms (RIAs) through PubMed, MEDLINE, EMBASE, and Cochrane Library databases systematically and comprehensively. The date of these studies was ranged from 2000 to 2021. The search strategies were conducted using “ruptured intracranial aneurysms,” “coiling,” and “clipping,” as our search terms and keywords. A manual search for literatures that was referenced by other publications but met our inclusion criteria was conducted as a supplement. We would use the most current literature, when a study produced multiple papers.
Inclusion and exclusion criteria
Literatures were included if they met the PICOS criteria: (1) population: limited the comparison to the RIAs individuals; (2) intervention: used coiling and clipping; (3) comparison: compared the results after coiling and clipping; (4) outcome measures: the results after treatment and the follow-up; and (5) an official published RCTs or non-RCT.
The exclusion criteria were as follows: (1) Letters to the editor and commentary or conference articles and (2) animal trials; (3) unclear patient outcome data; (4) case reports and case series; (5) systematic reviews or meta-analyses; and (6) other types of IAs, such as trauma.
Selection and data extraction
The data were extracted independently by two observers, C Peng, SF Cai, and YH Diao, containing basic data (author, publication time, age), study characteristics (trial type), and outcomes (rebleeding; mortality; complete occlusion, complications of postoperative) in a table. The senior investigator (YY Yang) would review the data for completeness and accuracy.
Statistical analyses and quality assessment
The results of this study were analyzed by standard software (Stata version 12.0 statistical software). For categorical variable results, risk ration (RR) or odds ratios (ORs) with 95% confidence intervals (CIs) were tested for result assessment. When I2>50%, the data was treated as obvious heterogeneity; therefore, a meta-analysis was performed using random effect model. Otherwise, the fixed effect model was conducted. For continuous variable results, standard mean difference (SMD) or weighted mean difference (WMD) with 95% CIs were calculated for assessment. When I2>50%, the data was treated as obvious heterogeneity, and the data analysis was conducted by a random effect model. Otherwise, the fixed effect model was conducted. The quality of the RCT literatures were assessed by Cochrane Collaboration’s tool, and the Newcastle-Ottawa scale were used to evaluate the quality of the observational studies.
Result
Quality of included studies
The article quality assessment was conducted separately by three reviewers, C Peng, YH Diao, and SF Cai. Thirty-seven observational studies were assessed by the Newcastle-Ottawa scale, and the Cochrane Risk of Bias Tool was used to assess the quality of the 3 RCTs. And the results were showed in Table 1 and Additional file 1.
Table 1.
The Newcastle-Ottawa scale for quality assessment observational studies
| Trials | Representativeness cohort | Exposure Ascertainment | Comparability | Outcome Assessment | Sufficient Duration | Adequacy of follow up of cohorts |
|---|---|---|---|---|---|---|
| Kelly et al. | Yes | database | No restricton, Matched in 1,2,5,6 | record linkage | Yes | Yes |
| Choi et al. | Yes | database | Restricted to MCA, Matched in 1,2,5,6 | record linkage | Yes | Yes |
| Ayling et al. | Yes | database | No restricton, Matched in 1,2,4,5,6 | record linkage | No | Yes |
| Berro et al. | Yes | medical record | Restricted to MCA, Matched in 1,2,4 | record linkage | No | Yes |
| Darsaut et al. | Yes | database | No restricton | record linkage | Yes | Yes |
| Zanaty et al. | Yes | database | No restricton, Matched in 1,2,4,5,6 | record linkage | No | Yes |
| Heit et al. | Yes | medical record | Restricted to ACOA, Matched in 1,2,3 | record linkage | No | Yes |
| Scheller et al. | Yes | medical record | No restricton, Matched in 1,2,3, 6 | record linkage | Yes | Yes |
| Koh et al. | Yes | medical record | No restricton, Matched in 1,2,6 | record linkage | No | Yes |
| Shen et al. | Yes | medical record | Restricted to Anterior Circulation, Matched in 1,2,4,5 | record linkage | No | Yes |
| Zhao et al. | Yes | medical record | No restricton, Matched in 1,2,4,5,6 | record linkage | Yes | Yes |
| McDonald et al. | Yes | database | No restricton, Matched in 1,2 | record linkage | unclear | unclear |
| Li et al. | Ysa | medical record | No restricton, Matched in 1,2,4,5,6 | record linkage | Yes | Yes |
| Yu et al. | Yes | medical record | No restricton, Matched in 1,2,5 | record linkage | Yes | Yes |
| Bekelis et al. | Yes | database | No restricton, Matched in 1,2 | record linkage | Yes | Yes |
| Li et al. | Yes | medical record | No restricton, Matched in 1,2,3,5,6 | record linkage | Yes | Yes |
| Deutsch et al. | Yes | database | No restricton, Matched in 1,2 | record linkage | Yes | Yes |
| Ryttlefors et al. | Yes | medical record | Restricted to ≥65 years, Matched in 1,2,4,5,6 | record linkage | Yes | NO |
| Wadd et al. | Yes | medical record | Restricted to ACOA, Matched in 1,2,4 | record linkage | Yes | Yes |
| Hoh et al. | Yes | database | Restricted to ≥18 years, Matched in 1,2 | record linkage | unclear | unclear |
| Brunken et al. | Yes | medical record | No restricton, Matched in 1,2,3,6 | record linkage | NO | Yes |
| Taweesomboonyat et al. | Yes | medical record | Restricted to PCOA, Matched in 1,2,3,4,5,6 | record linkage | Yes | Yes |
| Zhao et al. | Yes | medical record | Restricted to ACOA, Matched in 1,2,4,5 | record linkage | Yes | Yes |
| Klompenhouwer et al | Yes | medical record | No restricton, Matched in 1,2,3,5,6 | record linkage | Yes | Yes |
| Liao et al. | Yes | medical record | Restricted to Anterior Circulation, Matched in 1,2,3,4 | record linkage | Yes | Yes |
| Zhang et al. | Yes | medical record | Restricted to 60 years, Matched in 1,2,3,6 | record linkage | Yes | Yes |
| Lusseveld et al. | Yes | medical record | Restricted to basilar tip aneurysm, Matched in 1,2,4,5 | record linkage | No | Yes |
| Varelas et al. | Yes | medical record | No restricton, Matched in 1,2,3,6 | record linkage | Yes | Yes |
| Hoh et al. | Yes | medical record | Restricted to age older than 18 | record linkage | Unclear | Unclear |
| Li et al. | Yes | medical record | No restricton | record linkage | Yes | Yes |
| Liu et al. | Yes | medical record | No restricton, Matched in 1,2,3,5 | record linkage | Yes | Yes |
| Gross et al. | Yes | medical record | No restricton, Matched in 1,2,3,6 | record linkage | Unclear | Unclear |
| Suzuki et al. | Yes | medical record | No restricton, Matched in 1,2,4,5,6 | record linkage | Yes | Unclear |
| Zaidat et al. | Yes | medical record | No restricton, Matched in 1,2,3,6 | record linkage | Unclear | Unclear |
| Niskanen et al. | Yes | medical record | No restricton, Matched in 1,2,3,5,6 | record linkage | Yes | Yes |
| Rabinstein et al. | Yes | medical record | No restricton, Matched in 1,2,4,6 | record linkage | Yes | Yes |
| Kim et al. | Yes | medical record | Restricted to anterior choroidal artery aneurysms, Matched in 1,2,3,5 | record linkage | Yes | Yes |
Note: 1 = Age; 2 = Sex; 3 = Hunt and Hess Grade; 4 = World Federation of Neurological Societies Scale; 5 = Aneurism size; 6 =Aneurism location
Search results and study characteristics
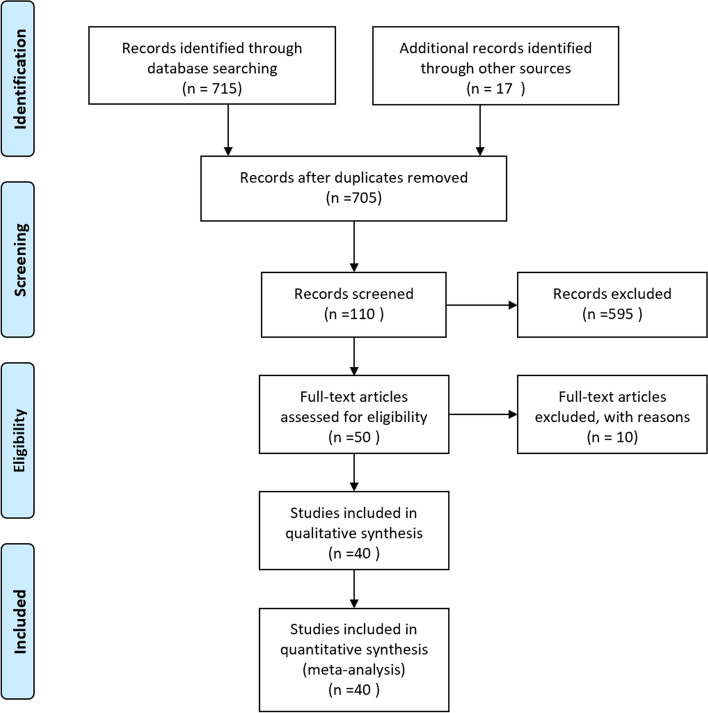
Initially, 715 literatures were found by searching an electronic database, and 17 articles were identified by manual search. And there were 705 articles after duplicates were removed. 595 publications were deleted by preliminary screening, ultimately, 40 articles met the inclusion criteria and were included in this meta-analysis. The details were shown in the flow chart (Fig. 1). There were 3 RCTs and 37 observational studies [7, 10-43]. A total of 60,875 patients were included and the size of the sample ranged from 32 to 21,905, 31,791 patients were treated by coiling, 29,084 individuals performed by clipping, and other information was shown in Table 2. And synthesis of the results in Table 3.
Fig. 1.
Forty articles met the inclusion criteria and were included in this meta-analysis
Table 2.
Overview of Included Studies
| Author | Country | Years | Type of Study | Recruitment period | Participants (n) | Gender (FM) | Age (mean ± standard) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Coil | Clip | Coil(%) | Clip(%) | Coil | Clip | |||||
| Kelly et al. | Canada | 2010 | RCS | 1995-2004 | 778 | 2342 | 67 | 65.5 | 54.4 | 53.7 |
| Choi et al. | Korea | 2016 | RCS | 2008-2012 | 8 | 30 | 62.5 | 60 | 64.75±11.47 | 53.17±11.96 |
| Ayling et al. | Canada | 2015 | RCS | 2005-2006 | 212 | 181 | NA | NA | NA | NA |
| Berro et al. | France | 2019 | RCS | 2012-2015 | 48 | 42 | 68.8 | 81 | 52 ± 10.8 | 52.6 ± 11.7 |
| Darsaut et al. | Canada | 2019 | RCS | 2012-2017 | 48 | 55 | 65 | 67 | 56.5 | 58.5 |
| Zanaty et al. | USA | 2016 | RCS | 2010-2015 | 182 | 70 | 73.6 | 67.1 | 56.6±12.4 | 55.9±12.7 |
| Heit et al. | USA | 2017 | RCS | 2010-2014 | 50 | 50 | 62 | 52 | 55±11.67 | 50±12.59 |
| Scheller et al. | Germany | 2018 | RCS | 2010-2015 | 45 | 54 | 55.8 | 75.9 | 60±13.75 | 57±13.75 |
| Koh et al. | Singapore | 2013 | RCS | 2005-2009 | 23 | 33 | 65.2 | 54.5 | 52.8 ± 11.6 | 54.1 ± 13.9 |
| Shen et al. | China | 2019 | RCS | 2013-2018 | 29 | 65 | 62 | 69 | 65.86±11.597 | 59.92±10.603 |
| Zhao et al. | China | 2016 | prospective | 2010-2012 | 133 | 129 | 46.6 | 53.5 | 54.5 ±11.8 | 54.4±10.9 |
| McDonald et al. | USA | 2014 | RCS | 2006-2011 | 1227 | 1227 | 65 | 66 | 53±13.33 | 53±12.59 |
| Yu et al. | China | 2007 | RCS | 1995-2001 | 80 | 89 | 60 | 62.9 | 56±13 | 57±13 |
| Bekelis et al. | Lebanon | 2016 | RCS | 2007-2012 | 2004 | 1206 | 73.4 | 77.2 | 75.3±6.8 | 73.5±6.2 |
| Li et al. | China | 2017 | RCS | 2002-2010 | 77 | 85 | 59.7 | 54.1 | 47.5±10.3 | 48.1±11.6 |
| Deutsch et al. | USA | 2018 | RCS | 2013-2014 | 15350 | 6555 | 65.9 | 69..0 | 55.3±33.45 | 54.1±31.58 |
| Ryttlefors et al. | UK | 2008 | RCS | NA | 138 | 140 | 68.8 | 74.3 | NA | NA |
| Wadd et al. | Pakistan | 2015 | RCS | 2010-2013 | 70 | 70 | 60 | 60 | 52.5±10 | 51±10 |
| Hoh et al. | USA | 2010 | RCS | 2002-2016 | 3564 | 5783 | 68 | 69 | 55.0±14.0 | 53.1±13.0 |
| Brunken et al. | Germany | 2009 | RCS | 1990-2004 | 145 | 370 | NA | NA | 53.7±15.5 | 50.7±16 |
| Taweesomboonyat et al. | Thailand | 2019 | RCS | 2002-2018 | 84 | 105 | 81 | 74.3 | 64.3±13.9 | 56.5±11.4 |
| Zhao et al. | China | 2019 | RCS | 2008-2015 | 46 | 65 | 52.2 | 55.4 | 54.5±11.2 | 55.5±11.1 |
| Klompenhouwer et al. | Netherlands | 2011 | RCS | 2000-2008 | 230 | 173 | 70.4 | 69.9 | 53.6 | 53.1 |
| Liao et al. | China | 2013 | RCS | 2008-2009 | 56 | 44 | 68 | 61 | 57.91±11.89 | 56.93±13.75 |
| Zhang et al. | China | 2012 | RCS | 2005-2009 | 76 | 122 | 64.5 | 72.95 | 51.7±13.0 | 52.8±10.4 |
| Lusseveld et al. | Netherlands | 2002 | RCS | 1983-1999 | 44 | 44 | 66 | 59 | 47.0 | 44.2 |
| Varelas et al. | USA | 2006 | RCS | 2000-2004 | 48 | 135 | 45 | 66 | 51±15 | 53±14 |
| Hoh et al. | USA | 2011 | RCS | 2002-2007 | 4306 | 6593 | NA | NA | NA | NA |
| Li et al. | China | 2012 | RCS | 2005-2009 | 94 | 92 | 27.7 | 32.6 | 54.7±14.2 | 53.7±13.8 |
| Liu et al. | China | 2013 | RCS | 2001-2005 | 281 | 361 | 60.5 | 66.8 | 55.6±15.21 | 56.90±13.36 |
| Gross et al. | USA | 2014 | RCS | 2007-2013 | 52 | 203 | 75 | 75 | NA | NA |
| Suzuki et al. | Japan | 2013 | Prospective | 2006-2007 | 297 | 282 | 65.7 | 69.9 | 62.4 ± 14.6 | 60.2 ± 12.5 |
| Zaidat et al. | USA | 2009 | RCS | 1999-2005 | 98 | 118 | 72 | 72 | 58 ±1.5 | 52 ±1.25 |
| McDougall et al. | USA | 2012 | RCT | 2003-2007 | 233 | 238 | 71 | 70 | 54.3 ± 12.0 | 53.1 ± 12.8 |
| Molyneux et al | Europe | 2005 | RCT | 1994-2002 | 1073 | 1070 | 63 | 63 | 52 | 52 |
| Koivisto et al. | Finland | 2000 | RCT | 1995-1997 | 52 | 57 | 46.1 | 59.6 | 49±14.25 | 50±15.25 |
| Niskanen et al. | Finland | 2004 | RCS | 1997-2000 | 68 | 103 | 52.9 | 57.3 | 54 ±13 | 54±13 |
| Rabinstein et al. | USA | 2003 | RCS | 1990-2000 | 76 | 339 | 62 | 65 | 56 | 53 |
| Li et al. | China | 2021 | RCS | 2015-2020 | 329 | 329 | NA | NA | NA | NA |
| Kim et al. | Korea | 2008 | RCS | 1999-2006 | 37 | 35 | 62.2 | 57.1 | 54±13 | 45±12 |
Note: NA = not available; RCT = randomized controlled trial; RCS = Retrospective comparative study; FM = female
Table 3.
Meta-analysis results
| Outcomes | Overall effect | Heterogeneity | ||||
|---|---|---|---|---|---|---|
| Effect estimate | 95% CI | p-Value | I2(%) | p-Value | ||
| Efficacy | mRS(0-2) | 1.327 | 1.093-1.612 | <0.05 | 38.8 | 0.091 |
| Rebleeding rate | 1.410 | 1.092-1.822 | <0.05 | 10.6 | 0.337 | |
| Mortality | 1.116 | 1.054-1.180 | <0.05 | 36.9 | 0.047 | |
| Complete occlusion | 0.375 | 0.308-0.456 | <0.05 | 0.0 | 0.424 | |
| Complications | Vasospasm | 0.787 | 0.649-0.954 | <0.05 | 41.1 | 0.060 |
| Hydrocephaly | 1.143 | 1.043-1.252 | <0.05 | 30.7 | 0.173 | |
| Cerebral infarction | 0.669 | 0.596-0.751 | <0.05 | 18.9 | 0.238 | |
| Neuro deficits | 0.720 | 0.582-0.892 | <0.05 | 15.6 | 0.315 | |
Note: mRS = Modified Rankin Scale; GOS = Glasgow Outcome Scale
Effectiveness of treatment
Modified Rankin Scale (MRS)
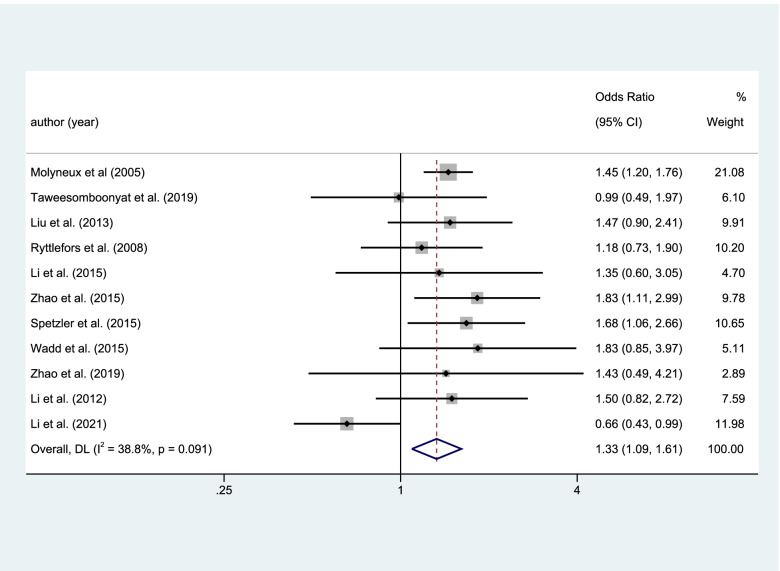
The mRS were used in this article to assess the quality of life. There were 11 articles, 4106 patients, including the result of mRS. 65.2% of the patients in the coiling group and 59.9% of patients in the clipping group had a good quality of life defined as mRS0-2. And there was a statistical significance in the results of mRS0-2 (coiling 1523 of 2336 (65.2%) VS clipping1454 of 2428 (59.9%); OR=1.327; CI=1.093–1.612; p<0.05; I2=38.8%; Fig. 2).
Fig. 2.
Statistical significance in the results of mRS0-2
Rebleeding
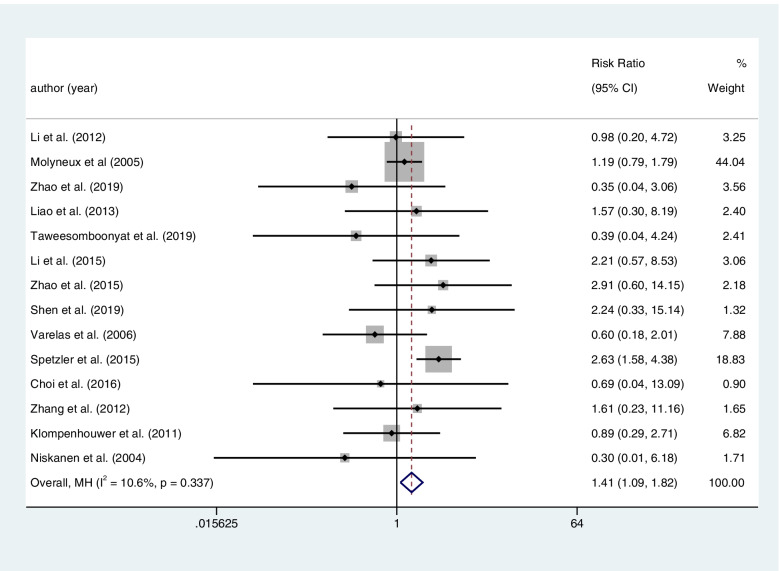
Fourteen articles included a total of 4659 patients with RIAs provided the rate of rebleeding after clipping or coiling. There was higher postoperative rebleeding in the coiling group than in the clipping group. And it was associated with a statistical significance (coiling 128 of 2232 (5.7%) VS clipping103 of 2427 (4.2%); RR=1.410; CI=1.092–1.822; p<0.05; I2=10.6%; Fig. 3).
Fig. 3.
Fourteen articles included a total of 4659 patients with RIAs provided the rate of rebleeding after clipping or coiling. There was higher postoperative rebleeding in the coiling group than the clipping group. And it was associated with a statistical significance
Mortality
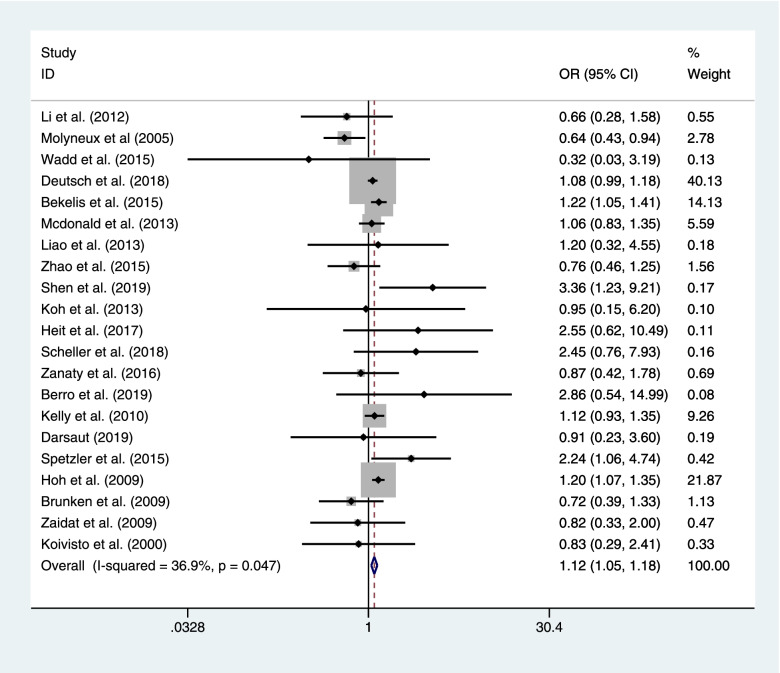
Twenty-one literatures encompassing the rate of mortality after coiling or clipping among 44,909 patients with RIAs. Coiling had a significant effect on the risk of mortality compared with clipping (coiling 3847 of 25,268 (15.2%) VS clipping 2955 of 19,641 (15.0%); OR=1.116; CI=1.054–1.180; p<0.05; I2=36.9%; Fig. 4).
Fig. 4.
Twenty-one literatures encompassing the rate of mortality after coiling or clipping among 44,909 patients with RIAs
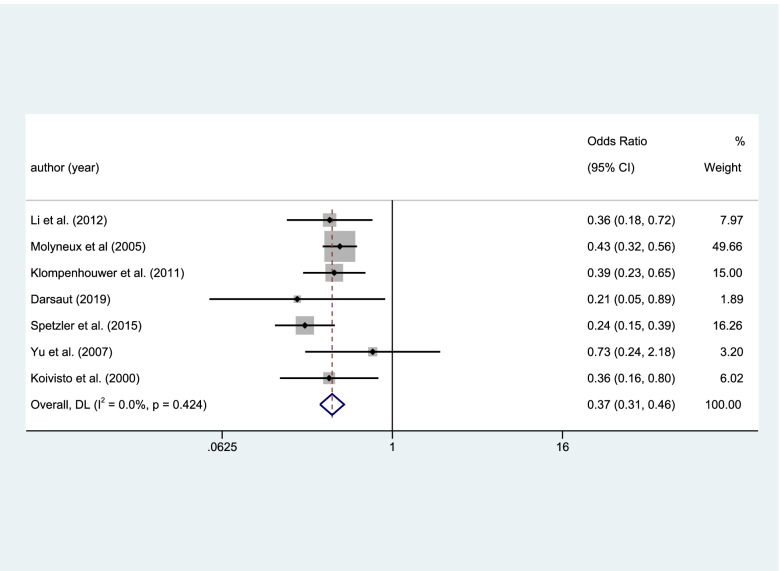
Complete occlusion
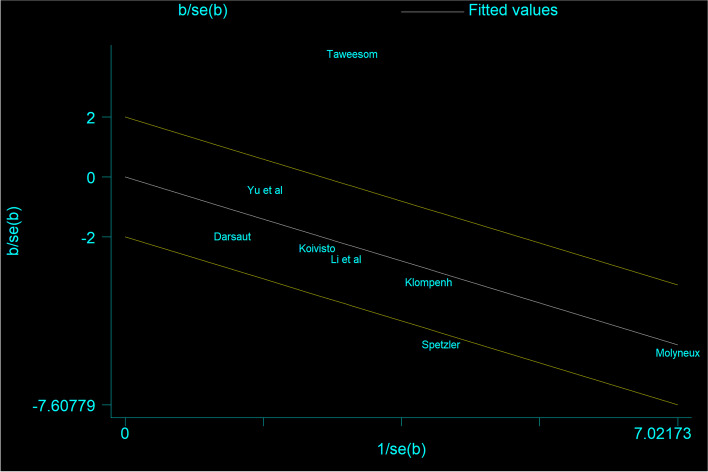
Eight studies included the result of complete occlusion, and the result was high heterogeneity. This study deleted a publication by heterogeneity analysis (Fig. 5). Seven studies included the result of complete occlusion among 2545 patients with RIAs. There was a higher rate of occlusion in the clipping group than the coiling group with a statistical significance (coiling 956 of 1480 (64.6%) VS clipping 881 of 1065 (82.7%); OR=0.375; CI=0.308–0.456; p<0.05; I2=0.0%; Fig. 6).
Fig. 5.
Eight studies included the result of complete occlusion, the result was high heterogeneity
Fig. 6.
Eight studies included the result of complete occlusion, the result was high heterogeneity
Postoperative complications
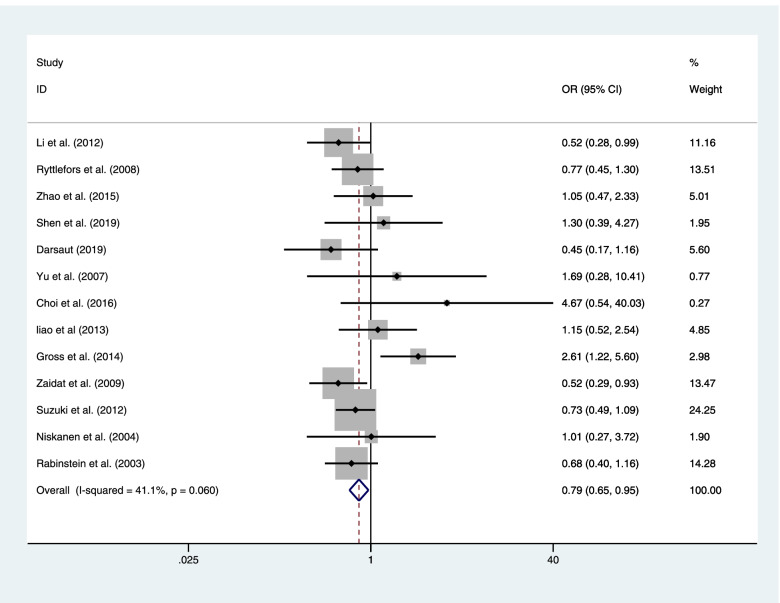
Vasospasm
Thirteen publications included a total of 2857 patients with RIAs who provided the result of vasospasm after clipping or coiling. There was a less postoperative vasospasm in the coiling group than in the clipping group with a statistical significance (coiling 241 of 1177 (20.5%) VS clipping 416 of 1680 (24.8%); OR=0.787; CI=0.649–0.954; p<0.05; I2=41.1%; Fig. 7).
Fig. 7.
Thirteen publications included a total of 2857 patients with RIAs provided the result of vasospasm after clipping or coiling
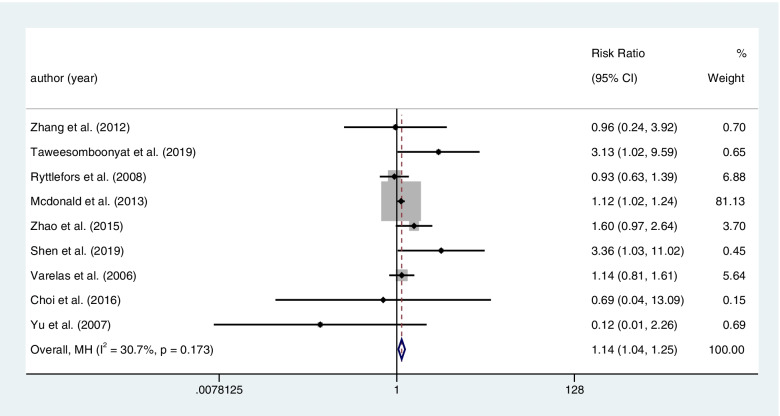
Hydrocephalous
Nine literatures contained the result of hydrocephalous after treatment among 3856 patients with RIAs. Coiling had a significant effect on the postoperative hydrocephalous compared with clipping (coiling 611 of 1819 (50.6%) VS clipping 581 of 2037 (39.9%); RR=1.143; CI=1.043–1.252; p<0.05; I2=30.7%; Fig. 8).
Fig. 8.
Nine literatures contained the result of hydrocephalous after treatment among 3856 patients with RIAs
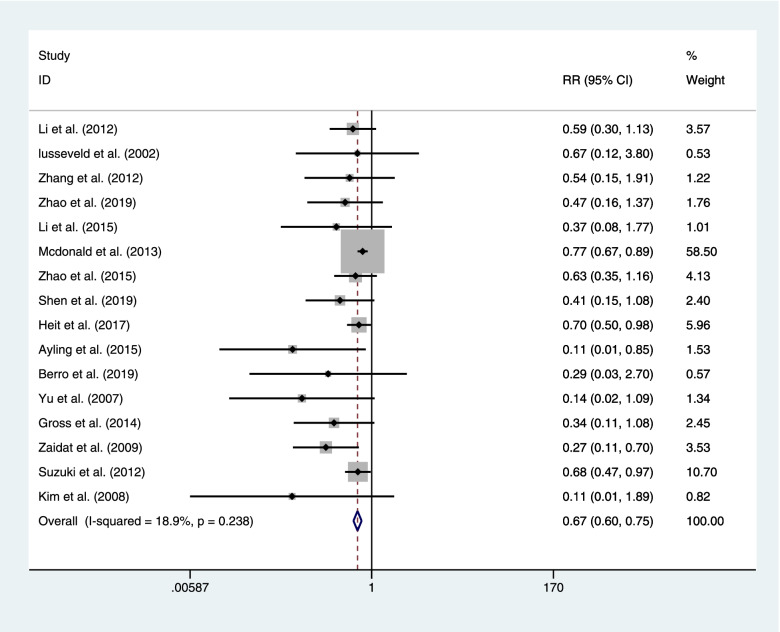
Cerebral infarction
There sixteen articles concluded the result of ischemic infarct after coiling or clipping among 5423 patients. Coiling had a lower postoperative ischemic infarct than clipping with a statistical significance (coiling 375 of 2598 (14.4%) VS clipping 597 of 2825 (21.1%); RR=0.669; CI=0.596–0.751; p<0.05; I2=18.9%; Fig. 9).
Fig. 9.
There sixteen articles concluded the result of ischemic infarct after coiling or clipping among 5423 patients
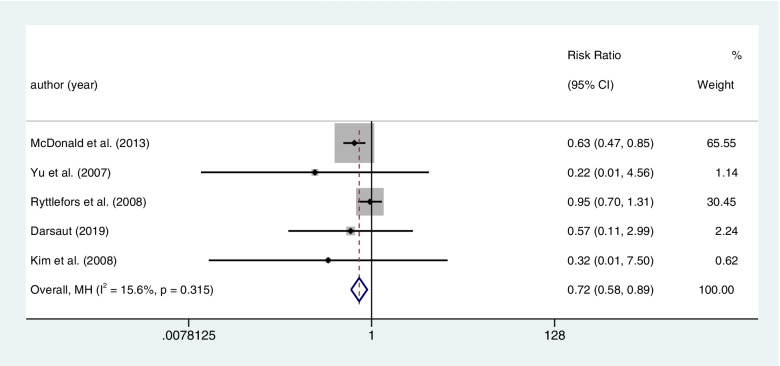
Postoperative neuro deficits
The five articles concluded the result of neuro complications (defined as any new weakness, decreased level of consciousness, paresthesia, or cranial nerve deficit), after coiling or clipping among 3076 patients. Clipping had a higher rate of postoperative neuro deficits than coiling with a statistical significance (coiling 119 of 1530 (7.8%) VS clipping 167 of 1546 (10.8%); RR=0.720; CI=0.582–0.892; p<0.05; I2=15.6%; Fig. 10).
Fig. 10.
There five articles concluded the result of neuro complications (defined as any new weakness, decreased level of consciousness, paresthesia or cranial nerve deficit), after coiling or clipping among 3076 patients
Discussion
This meta-analysis summarized the available data with regard to outcomes of patients with RIAs who underwent clipping or coiling procedures systematically. Our meta-analysis included 40 articles involving 60,875 patients with RIAs. And we compared eight outcomes between coiling and clipping including the effectiveness of treatment (mRS, postoperative rebleeding, postoperative mortality, the rate of complete occlusion) and the postoperative complications (vasospasm, hydrocephalous, cerebral infarction, postoperative neuro deficits).
This meta-analysis showed that patients who underwent coiling had a significantly better quality of life (mRS 0-2) than those who underwent clipping at 1 year after treatment. Liu et al. [36] also reported that coiling patients had more good quality of life outcomes than clipping patients at 1 year after treatment. And this result was consistent with ISAT data [5, 7]. Additionally, some articles [23, 28] showed the trend that coiling was related to a higher rate of good outcomes (mRS 0-2) than the clipping group. Yu et al. [21] reported that the result of Glasgow Outcome Score (GOS) (1–3) was lower in endovascular coiling (12/80, 15%) than in microsurgical clipping (30/89, 34%; p<0.05). Zhang et al. [19] had the opposite result about the rate of GOS (4–5). Because the admission grade (Hunt-Hess 4–5; p<0.01) [27] was associated with poor outcomes, it could explain why there were different results.
250 (23.5%) of 1063 individuals who underwent coiling treatment were dependent or dead at 1 year, compared with 326 (30.9%) of 1055 patients with clipping, an absolute risk reduction of 7.4% (95% CI 3.6–11.2, p<0.05) reported by Molyneux et al. [7]. Spetzler et al. [43] also showed coiling was related with a lower rate of mortality. While Shen et al. [18] had the opposite point, their result showed coiling was associated with a higher mortality rate than clipping, this result was similar with our meta-analysis. Our result of mortality was different from published studies, and the difference in categorical data may be one of the reasons [18]. Additionally, this study found that the coiling group has a higher incidence rate of rebleeding rate and a lower complete occlusion rate. It may be associated with higher mortality in the coiling group.
Several articles [18, 19, 31, 32] demonstrated that a trend toward postoperative rebleeding in the coiling group, while other literatures [17, 33] showed the clipping group had a higher rate of rebleeding than the coiling group, and there was no significant difference in their results. In the present article, we find a significantly higher risk of rebleeding in the endovascular coiling group (p<0.05). Varelas et al. [33] reported that rebleeding was significantly associated with the ventriculoperitoneal shunt (p<0.05), and some published articles suggested that rebleeding also depended on the follow-up period and on the rate of occlusion after endovascular coiling or microsurgical clipping [5, 7] and this meta-analysis also found that clipping was significantly associated with a higher rate of complete occlusion (p<0.05), this result was consistent with published studies [28, 31, 35]. Murayama et al. [44] also reported that the rate of complete occlusion was found in 55% of aneurysms, and the lesion neck remnant was identified in 35.4% of aneurysms and the rate of recanalization was up to 20.9%, which was associated with the neck of the aneurysm and size of the dome. And coil compaction and/or loosening and a high rate of the remnant of the neck could also cause recanalization [5, 45].
Our articles showed endovascular coiling was associated with a significantly lower risk of vasospasm, cerebral infarction, post neuro deficits, but with a significantly higher postoperative hydrocephalous than microsurgical clipping.
Li et al. [35, 46] also showed the lower incidence of vasospasm and cerebral infarction in the coiling group. Some other publications [46, 47] were similar to ours about the infarction. One of the vasospasm reasons is that blood degradation products, accumulating in subarachnoid space and reserve as triggers to cause intramural inflammation and endothelial dysfunction [48]. However, there was an argument about vasospasm, someone thought that remove the cisternal blood during clipping would reduce the risk of vasospasm [45]. But this effect could be offset by other effects related with clipping [49], such as surgical operations of the vessels and craniotomy with brain retraction would aggravate the preexisting cerebral vasospasm. And some previous publications suggested that cerebral vasospasm was associated with the incidence of cerebral infarction [50, 51]. There were some other reasons of cerebral infarction: microsurgical clipping blocked some microvascular during surgery, leading to ischemia event. The compression of the small vessels that around the lesion clip may lead to local ischemia [18]. These factors may cause a higher risk of infarction in the clipping group. Additionally, vasospasm-related cerebral infarction significantly influences the rate of mortality following aSAH and cause poor clinical outcomes [52].
The result of postoperative neuro complications was consistent with some published studies [49, 53], and Dumont et al. also analyzed the risk factor of neuro deficits, such as clipping, ventriculostomy, thick clot size, history of hypertension, and intracerebral hemorrhage [49].
So far, some publications had reviewed the morbidity of hydrocephalus after endovascular coiling and microsurgical clipping systematically, while there was no uniform conclusion [21, 54]. While the result of Shen et al. [18] was consistent with this article that coiling was related with a higher risk of hydrocephalous. As is known to all, arachnoid granules absorbed cerebrospinal fluid (CSF), and some CSF was absorbed through the cerebral capillaries. Blood clots may lead to impairment of CSF absorption by disturbing cerebral capillaries and arachnoid villi, causing cerebral hydrocephalous [54]. While clipping could remove the blood clots, improving circulation of CSF, decreasing the risk of hydrocephalous [18]. And the controversy with regard to the result of hydrocephalous may be the different diagnosis criteria of cerebral hydrocephalus [19].
This study has several potential limitations: (1) The included literatures were only 3 RCTs, and this article was limited to the evaluation of short-term results. (2) The sample of some comparative indicators was relatively small.
Conclusion
Coiling was significantly associated with a better quality of life (mRS0-2), a lower incidence of postoperative complications (vasospasm, cerebral infarction, neuro deficits), and a higher rate of mortality, rebleeding and hydrocephalous than clipping. Additionally, coiling was associated with a lower rate of complete occlusion.
Supplementary Information
Additional file 1. Cochrane Collaboration’s tool for quality assessment RCTs
Acknowledgements
None.
Abbreviations
- RIAs
Ruptured intracranial aneurysms
- aSAH
Aneurysmal subarachnoid hemorrhage
- SAH
Subarachnoid hemorrhage
- ISAT
the International Subarachnoid Aneurysm Trial
- IAs
Intracranial aneurysms
- RCTs
Randomized controlled trials
- mRS
Modified Rankin Scale
- GOS
Glasgow outcome score
- CSF
Cerebrospinal fluid
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
Authors’ contributions
Chao Peng: writing the draft, editing, data election, quality evaluation of included studies, and data analysis. Yu-hang Diao: quality evaluation of included studies, data election, and data analysis. Shi-fei Cai: data election, quality evaluation of included studies, and data analysis. Xin-yu Yang: writing - review & editing, supervision, and project administration. The authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Chao Peng, Email: pengchao3892@163.com.
Yu-hang Diao, Email: aerod0328@163.com.
Shi-fei Cai, Email: caishifeiXM@163.com.
Xin-yu Yang, Email: yangxinyu@tmu.edu.cn.
References
- 1.Lawton MT, Vates GE. Subarachnoid hemorrhage. N Engl J Med. 2017;377(3):257–266. doi: 10.1056/NEJMcp1605827. [DOI] [PubMed] [Google Scholar]
- 2.Solheim O, Eloqayli H, Muller TB, Unsgaard G. Quality of life after treatment for incidental, unruptured intracranial aneurysms. Acta Neurochir (Wien) 2006;148(8):821–830. doi: 10.1007/s00701-006-0804-7. [DOI] [PubMed] [Google Scholar]
- 3.Dandy WE. Intracranial aneurysm of the internal carotid artery: cured by operation. Ann Surg. 1938;107(5):654–659. doi: 10.1097/00000658-193805000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dovey Z, Misra M, Thornton J, Charbel FT, Debrun GM, Ausman JI. Guglielmi detachable coiling for intracranial aneurysms: the story so far. Arch Neurol. 2001;58(4):559–564. doi: 10.1001/archneur.58.4.559. [DOI] [PubMed] [Google Scholar]
- 5.Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002;360(9342):1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 6.Lin N, Cahill KS, Frerichs KU, Friedlander RM, Claus EB. Treatment of ruptured and unruptured cerebral aneurysms in the USA: a paradigm shift. J Neurointerv Surg. 2018;10(Suppl 1):i69–i76. doi: 10.1136/jnis.2011.004978.rep. [DOI] [PubMed] [Google Scholar]
- 7.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366(9488):809–817. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 8.Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. 2013;44(1):29–37. doi: 10.1161/STROKEAHA.112.663559. [DOI] [PubMed] [Google Scholar]
- 9.Akhigbe T, Zolnourian A, Bulters D. Compliance of systematic reviews articles in brain arteriovenous malformation with PRISMA statement guidelines: Review of literature. J Clin Neurosci. 2017;39:45–48. doi: 10.1016/j.jocn.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 10.O'Kelly CJ, Kulkarni AV, Austin PC, Wallace MC, Urbach D. The impact of therapeutic modality on outcomes following repair of ruptured intracranial aneurysms: an administrative data analysis. Clinical article. J Neurosurg. 2010;113(4):795–801. doi: 10.3171/2009.9.JNS081645. [DOI] [PubMed] [Google Scholar]
- 11.Choi JH, Park JE, Kim MJ, Kim BS, Shin YS. Aneurysmal neck clipping as the primary treatment option for both ruptured and unruptured middle cerebral artery aneurysms. J Korean Neurosurg Soc. 2016;59(3):269–275. doi: 10.3340/jkns.2016.59.3.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ayling OG, Ibrahim GM, Drake B, Torner JC, Macdonald RL. Operative complications and differences in outcome after clipping and coiling of ruptured intracranial aneurysms. J Neurosurg. 2015;123(3):621–628. doi: 10.3171/2014.11.JNS141607. [DOI] [PubMed] [Google Scholar]
- 13.Berro DH, L'Allinec V, Pasco-Papon A, Emery E, Berro M, Barbier C, et al. Clip-first policy versus coil-first policy for the exclusion of middle cerebral artery aneurysms. J Neurosurg. 2019:1–8. 10.3171/2019.5.JNS19373. [DOI] [PubMed]
- 14.Darsaut TE, Roy D, Weill A, Bojanowski MW, Chaalala C, Bilocq A, et al. A randomized trial of endovascular versus surgical management of ruptured intracranial aneurysms: interim results from ISAT2. Neurochirurgie. 2019;65(6):370–376. doi: 10.1016/j.neuchi.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Heit JJ, Ball RL, Telischak NA, Do HM, Dodd RL, Steinberg GK, et al. Patient outcomes and cerebral infarction after ruptured anterior communicating artery aneurysm treatment. AJNR Am J Neuroradiol. 2017;38(11):2119–2125. doi: 10.3174/ajnr.A5355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scheller C, Strauss C, Prell J, Simmermacher S, Brandt S. Increased rate of ventriculostomy-related hemorrhage following endovascular treatment of ruptured aneurysms compared to clipping. Acta Neurochir (Wien) 2018;160(3):545–550. doi: 10.1007/s00701-018-3471-6. [DOI] [PubMed] [Google Scholar]
- 17.Koh KM, Ng Z, Low SY, Chua HZ, Chou N, Low SW, et al. Management of ruptured intracranial aneurysms in the post-ISAT era: outcome of surgical clipping versus endovascular coiling in a Singapore tertiary institution. Singapore Med J. 2013;54(6):332–338. doi: 10.11622/smedj.2013127. [DOI] [PubMed] [Google Scholar]
- 18.Shen J, Huang K, Shen J, Zhu Y, Jiang H, Pan J, et al. Clinical efficacy between microsurgical clipping and endovascular coiling in the treatment of ruptured poor-grade anterior circulation aneurysms. World Neurosurg. 2019:127 e321-e329. 10.1016/j.wneu.2019.02.248. [DOI] [PubMed]
- 19.Zhao B, Tan X, Yang H, Li Z, Zheng K, Xiong Y, et al. Endovascular coiling versus surgical clipping for poor-grade ruptured intracranial aneurysms: postoperative complications and clinical outcome in a multicenter poor-grade aneurysm study. AJNR Am J Neuroradiol. 2016;37(5):873–878. doi: 10.3174/ajnr.A4649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDonald JS, McDonald RJ, Fan J, Kallmes DF, Lanzino G, Cloft HJ. Comparative effectiveness of ruptured cerebral aneurysm therapies: propensity score analysis of clipping versus coiling. AJNR Am J Neuroradiol. 2014;35(1):164–169. doi: 10.3174/ajnr.A3642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu SC, Wong GK, Wong JK, Poon WS. Endovascular coiling versus neurosurgical clipping for ruptured intracranial aneurysms: significant benefits in clinical outcome and reduced consumption of hospital resources in Hong Kong Chinese patients. Hong Kong Med J. 2007;13(4):271–278. [PubMed] [Google Scholar]
- 22.Bekelis K, Gottlieb D, Su Y, O'Malley AJ, Labropoulos N, Goodney P, et al. Surgical clipping versus endovascular coiling for elderly patients presenting with subarachnoid hemorrhage. J Neurointerv Surg. 2016;8(9):913–918. doi: 10.1136/neurintsurg-2015-011890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li J, Su L, Ma J, Kang P, Ma L, Ma L. Endovascular coiling versus microsurgical clipping for patients with ruptured very small intracranial aneurysms: management strategies and clinical outcomes of 162 cases. World Neurosurg. 2017;99:763–769. doi: 10.1016/j.wneu.2015.11.079. [DOI] [PubMed] [Google Scholar]
- 24.Deutsch BC, Neifert SN, Caridi JM. No disparity in outcomes between surgical clipping and endovascular coiling after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2018:120 e318-e325. 10.1016/j.wneu.2018.08.060. [DOI] [PubMed]
- 25.Ryttlefors M, Enblad P, Kerr RS, Molyneux AJ. International subarachnoid aneurysm trial of neurosurgical clipping versus endovascular coiling: subgroup analysis of 278 elderly patients. Stroke. 2008;39(10):2720–2726. doi: 10.1161/STROKEAHA.107.506030. [DOI] [PubMed] [Google Scholar]
- 26.Hoh BL, Chi YY, Lawson MF, Mocco J, Barker FG., 2nd Length of stay and total hospital charges of clipping versus coiling for ruptured and unruptured adult cerebral aneurysms in the Nationwide Inpatient Sample database 2002 to 2006. Stroke. 2010;41(2):337–342. doi: 10.1161/STROKEAHA.109.569269. [DOI] [PubMed] [Google Scholar]
- 27.Brunken M, Kehler U, Fiehler J, Leppien A, Eckert B. Coiling vs. clipping: hospital stay and procedure time in intracranial aneurysm treatment. Rofo. 2009;181(10):989–995. doi: 10.1055/s-0028-1109344. [DOI] [PubMed] [Google Scholar]
- 28.Taweesomboonyat C, Tunthanathip T, Kaewborisutsakul A, Saeheng S, Oearsakul T, Riabroi K, et al. Outcome of ruptured posterior communicating artery aneurysm treatment comparing between clipping and coiling techniques. World Neurosurg. 2019:125 e183–8. 10.1016/j.wneu.2019.01.037. [DOI] [PubMed]
- 29.Zhao B, Xing H, Fan L, Tan X, Zhong M, Pan Y, et al. Endovascular coiling versus surgical clipping of very small ruptured anterior communicating artery aneurysms. World Neurosurg. 2019:126 e1246–50. 10.1016/j.wneu.2019.03.074. [DOI] [PubMed]
- 30.Klompenhouwer EG, Dings JT, van Oostenbrugge RJ, Oei S, Wilmink JT, van Zwam WH. Single-center experience of surgical and endovascular treatment of ruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2011;32(3):570–575. doi: 10.3174/ajnr.A2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liao CC, Huang YH, Fang PH, Lee TC. Surgical and endovascular treatment for ruptured anterior circulation cerebral aneurysms: a comparison of outcomes--a single centre study from Taiwan. Int J Surg. 2013;11(9):998–1001. doi: 10.1016/j.ijsu.2013.05.038. [DOI] [PubMed] [Google Scholar]
- 32.Zhang QR, Zhang X, Wu Q, Shi JX, Wang HD, Hang CH, et al. The impact of microsurgical clipping and endovascular coiling on the outcome of cerebral aneurysms in patients over 60 years of age. J Clin Neurosci. 2012;19(8):1115–1118. doi: 10.1016/j.jocn.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 33.Varelas P, Helms A, Sinson G, Spanaki M, Hacein-Bey L. Clipping or coiling of ruptured cerebral aneurysms and shunt-dependent hydrocephalus. Neurocrit Care. 2006;4(3):223–228. doi: 10.1385/NCC:4:3:223. [DOI] [PubMed] [Google Scholar]
- 34.Lusseveld E, Brilstra EH, Nijssen PC, van Rooij WJ, Sluzewski M, Tulleken CA, et al. Endovascular coiling versus neurosurgical clipping in patients with a ruptured basilar tip aneurysm. J Neurol Neurosurg Psychiatry. 2002;73(5):591–593. doi: 10.1136/jnnp.73.5.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li ZQ, Wang QH, Chen G, Quan Z. Outcomes of endovascular coiling versus surgical clipping in the treatment of ruptured intracranial aneurysms. J Int Med Res. 2012;40(6):2145–2151. doi: 10.1177/030006051204000612. [DOI] [PubMed] [Google Scholar]
- 36.Liu HM, Wong HF, Lee KW, Tu YK, Yeh YS, Chou CW, et al. Taiwan aneurysm registry: multivariate analysis of two-month, one-year, and two-year outcomes after endovascular and microsurgical treatment of ruptured aneurysms. Interv Neuroradiol. 2013;19(1):35–42. doi: 10.1177/159101991301900105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoh BL, Nathoo S, Chi YY, Mocco J, Barker FG., 2nd Incidence of seizures or epilepsy after clipping or coiling of ruptured and unruptured cerebral aneurysms in the nationwide inpatient sample database: 2002-2007. Neurosurgery. 2011;69(3):644–650. doi: 10.1227/NEU.0b013e31821bc46d. [DOI] [PubMed] [Google Scholar]
- 38.Gross BA, Rosalind Lai PM, Frerichs KU, Du R. Treatment modality and vasospasm after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2014;82(6):e725–e730. doi: 10.1016/j.wneu.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 39.Suzuki H, Taki W. Prospective Registry of Subarachnoid Aneurysms Treatment G. Effect of aneurysm treatment modalities on cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Acta Neurochir Suppl. 2013:115 99-105. 10.1007/978-3-7091-1192-5_22. [DOI] [PubMed]
- 40.Zaidat OO, Ionita CC, Hussain SI, Alexander MJ, Friedman AH, Graffagnino C. Impact of ruptured cerebral aneurysm coiling and clipping on the incidence of cerebral vasospasm and clinical outcome. J Neuroimaging. 2009;19(2):144–149. doi: 10.1111/j.1552-6569.2008.00285.x. [DOI] [PubMed] [Google Scholar]
- 41.Koivisto T, Vanninen R, Hurskainen H, Saari T, Hernesniemi J, Vapalahti M. Outcomes of early endovascular versus surgical treatment of ruptured cerebral aneurysms. A prospective randomized study. Stroke. 2000;31(10):2369–2377. doi: 10.1161/01.str.31.10.2369. [DOI] [PubMed] [Google Scholar]
- 42.Niskanen M, Koivisto T, Ronkainen A, Rinne J, Ruokonen E. Resource use after subarachnoid hemorrhage: comparison between endovascular and surgical treatment. Neurosurgery. 2004;54(5):1081–1086. doi: 10.1227/01.neu.0000119350.80122.43. [DOI] [PubMed] [Google Scholar]
- 43.Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ, et al. The barrow ruptured aneurysm trial: 6-year results. J Neurosurg. 2015;123(3):609–617. doi: 10.3171/2014.9.JNS141749. [DOI] [PubMed] [Google Scholar]
- 44.Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg. 2003;98(5):959–966. doi: 10.3171/jns.2003.98.5.0959. [DOI] [PubMed] [Google Scholar]
- 45.Inagawa T, Yamamoto M, Kamiya K. Effect of clot removal on cerebral vasospasm. J Neurosurg. 1990;72(2):224–230. doi: 10.3171/jns.1990.72.2.0224. [DOI] [PubMed] [Google Scholar]
- 46.de Oliveira JG, Beck J, Ulrich C, Rathert J, Raabe A, Seifert V. Comparison between clipping and coiling on the incidence of cerebral vasospasm after aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurosurg Rev. 2007;30(1):22–30. doi: 10.1007/s10143-006-0045-5. [DOI] [PubMed] [Google Scholar]
- 47.Kim BM, Kim DI, Shin YS, Chung EC, Kim DJ, Suh SH, et al. Clinical outcome and ischemic complication after treatment of anterior choroidal artery aneurysm: comparison between surgical clipping and endovascular coiling. AJNR Am J Neuroradiol. 2008;29(2):286–290. doi: 10.3174/ajnr.A0806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Budohoski KP, Guilfoyle M, Helmy A, Huuskonen T, Czosnyka M, Kirollos R, et al. The pathophysiology and treatment of delayed cerebral ischaemia following subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 2014;85(12):1343–1353. doi: 10.1136/jnnp-2014-307711. [DOI] [PubMed] [Google Scholar]
- 49.Dumont AS, Crowley RW, Monteith SJ, Ilodigwe D, Kassell NF, Mayer S, et al. Endovascular treatment or neurosurgical clipping of ruptured intracranial aneurysms: effect on angiographic vasospasm, delayed ischemic neurological deficit, cerebral infarction, and clinical outcome. Stroke. 2010;41(11):2519–2524. doi: 10.1161/STROKEAHA.110.579383. [DOI] [PubMed] [Google Scholar]
- 50.Leclerc JL, Blackburn S, Neal D, Mendez NV, Wharton JA, Waters MF, et al. Haptoglobin phenotype predicts the development of focal and global cerebral vasospasm and may influence outcomes after aneurysmal subarachnoid hemorrhage. Proc Natl Acad Sci U S A. 2015;112(4):1155–1160. doi: 10.1073/pnas.1412833112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kumar G, Shahripour RB, Harrigan MR. Vasospasm on transcranial Doppler is predictive of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurosurg. 2016;124(5):1257–1264. doi: 10.3171/2015.4.JNS15428. [DOI] [PubMed] [Google Scholar]
- 52.Dorsch NW, King MT. A review of cerebral vasospasm in aneurysmal subarachnoid haemorrhage part I: incidence and effects. J Clin Neurosci. 1994;1(1):19–26. doi: 10.1016/0967-5868(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 53.Kassell NF, Torner JC, Jane JA, Haley EC, Jr, Adams HP. The international cooperative study on the timing of aneurysm surgery. Part 2: Surgical results. J Neurosurg. 1990;73(1):37–47. doi: 10.3171/jns.1990.73.1.0037. [DOI] [PubMed] [Google Scholar]
- 54.Xie Z, Hu X, Zan X, Lin S, Li H, You C. Predictors of shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage? A Systematic Review and Meta-Analysis. World Neurosurg. 2017;106(844-860):e846. doi: 10.1016/j.wneu.2017.06.119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Cochrane Collaboration’s tool for quality assessment RCTs
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.