Summary
Background
There are widespread concerns that the COVID-19 pandemic may increase suicides. Few studies have analysed effects beyond the pandemic's early months or examined changes in known suicide risk factors.
Methods
Using time series models fit with Poisson regression, we analysed monthly police-reported suicides in Ecuador from January 2015 to June 2021. Treating March 2020 as the start of the pandemic, we calculated rate ratios (RRs) comparing the observed to the expected number of suicides for the total population and by age and sex groups. We investigated changes in risk factors, precipitants, geographic distribution, and suicide methods.
Findings
There was no evidence that suicide rates were higher than expected during the pandemic (RR 0·97 [95% CI 0·92–1·02]). There was some evidence of fewer than expected male suicides (RR 0·95 [95% CI 0·90–1·00]). The proportion of suicides occurring in urban and coastal areas increased but decreased amongst indigenous and other minorities. The proportions of suicides with evidence of alcohol consumption, disability, and amongst married and cohabiting individuals decreased, whereas suicides where mental health problems were considered contributory increased. There were relative increases in the proportion of suicides by hanging but decreases in self-poisoning and other suicide methods.
Interpretation
The pandemic did not appear to adversely impact overall suicide numbers nationwide during the first 16 months of the pandemic. Reduced alcohol consumption may have contributed to the decline in male suicides.
Funding
None.
Keywords: Suicide, COVID-19, Risk factors, Ecuador
Research in context.
Evidence before this study
Most studies of the impact of the COVID-19 pandemic on suicides are based on data from high-income countries and focus on the early months of the pandemic. Few studies from low- and middle-income countries (LMIC) have examined age and sex-specific effects of the pandemic or changes in the characteristics of people dying by suicide. A previous analysis of overall suicides (both sexes and all ages combined) in Ecuador for the first seven months of the pandemic reported fewer than expected suicides (RR 0·68 [95% CI 0·63−0·73]). On Feb 20, 2022, we searched for studies in PubMed that included data on nationwide suicide mortality in LMIC countries during the pandemic and updated with at least some data for 2021, and which presented data by age groups and sex, as well as risk factors. The terms used were: “suicide mortality”, “suicide*” “COVID-19” and “pandemic”. No restriction of language was applied. Only one study from a LMIC analysed suicide trends beyond 2020. That study analysed national suicide data for Nepal and found rises in male and female suicides but did not use models to account for underlying time trends. Data from other LMICs for the early months of the pandemic are mixed with rises reported in India, Mexico, and Thailand but no changes or falls reported in other settings.
Added value of this study
Our study used a time-series design to analyse monthly suicide data for Ecuador from 1 January 2015 to 30 June 2021, a period including the first 16 months of the pandemic (from March 2020). Findings show that pandemic trends were consistent with pre-pandemic trends with no additional suicides beyond the expected number of suicides. There was some evidence of fewer than expected male suicides. Compared to the pre-pandemic period a lower proportion of suicides during the pandemic were from rural areas, were married or cohabiting, were from minority ethnic groups, had a disability, or had evidence of alcohol consumption at the time of death. There was an increase in the proportion of suicides where mental health problems were identified as a trigger. There were increases in the proportion of suicides using hanging as a method of suicide and falls in overdose deaths.
Implications of all the available evidence
Despite high levels of COVID-19-related mortality, suicide numbers have remained stable over the first 16 months of the pandemic in Ecuador. Factors contributing to the lower than expected numbers of male suicides, including measures to restrict alcohol consumption (e.g. sales restrictions, bar closures, and limiting social gatherings), require further investigation.
Alt-text: Unlabelled box
Introduction
Since the start of the COVID-19 pandemic, at least 511 million people have been infected with SARS-CoV-2 and over six million have died.1 Alongside the pandemic's impact on physical health and mortality, the disease and the public health measures put in place to prevent its spread have had an adverse effect on population mental health.2 Risk factors for poor mental health and suicidal behaviour have increased during the pandemic, due to factors such as the implementation of social restrictions, economic uncertainty, high levels of bereavement, and the long-term effects of infection with the virus.3,4
The evidence in relation to the effects of the COVID-19 pandemic on suicide mortality comes mainly from high-income countries (HICs) gathered during the early months of the pandemic. There have been few studies from LMICs.5 Most research shows no increase in suicide mortality in the early months of the pandemic. The largest study to date gathered data from 21 countries (16 high-income countries, five middle-income countries) and examined suicide trends up to July 2020. The study showed that the number of suicides was no higher than expected during this initial period, with 12 countries, including Ecuador, reporting fewer than expected suicides. Even when extending the analysis to October 2020, increases in suicides were only observed in three regions – Vienna (Austria), Puerto Rico, and Japan, while Ecuador still reported fewer than expected suicides.5
Data from some LMICs, including Peru6 and China,7 showed initial decreases in deaths by suicide during periods of lockdown. But other LMICs showed an increase in suicides. Borges and colleagues8 reported an increase in suicides in Mexico during the first eight months of the pandemic. In Nepal, there was an increase in males and females when examined up to June 2021.9 Similarly, in India there was a rise in suicides in 2020 compared to 2019, although the rise pre-dated the onset of the pandemic.10
Ecuador, a South American country with a population of 17·5 million in 2020, reported its first SARS-CoV-2 case on February 29, 2020, in the coastal city of Guayaquil. Subsequently, several public health measures were introduced to contain the virus, including national and regional periods of lockdown (strict stay-at-home orders), suspending public events, travel restrictions, banning arrivals at borders, closing schools and universities, working from home, and banning alcohol sales. As of March 13, 2022, there were 843,760 confirmed cases and 35,316 confirmed deaths due to SARS-CoV-2 in Ecuador, and from March 2020 to June 2021, there were approximately 65,000 excess deaths.11 Ecuador's economy fell by 7·8% in 2020, losing more than half a million jobs, and 7% more people were living below the poverty line in 2020 compared to 2019 (32% vs. 25%).12
To investigate the impact of the pandemic and the associated socio-economic changes on suicides in Ecuador, we analysed suicide reports from national police records during the first 16 months of the COVID-19 pandemic (March 1, 2020–June 30, 2021) making a comparison with the January 2015–February 2020 period.
Given the high levels of COVID-19 infections and deaths in Ecuador and the economic impact of the pandemic, we hypothesised that there would be an increase in suicide, particularly among a) the elderly, as some evidence pointed to an increased risk in this population during the 2003 severe acute respiratory syndrome (SARS) epidemic in Hong Kong,13 and b) men, as previous studies indicate that male suicide rates may increase during economic downturns.14
Methods
Study design
We conducted a time series study to examine suicide trends from January 1, 2015 to June 30, 2021, for the total population and stratified analyses by sex and age groups. Subsequent to this, we undertook a case-series study, comparing changes in the characteristics of suicides between the pre-pandemic period and the pandemic period.
Data collection
In Ecuador, suicide is classified as a violent death, which warrants formal investigation by the National Directorate of Crimes against Life, Violent Deaths, Disappearances, Extortion and Kidnapping (DINASED). The procedure for registering a death as a suicide is as follows:
-
•
Once police are notified of a violent death, an investigation team - composed of a minimum of two police officers with training in the investigation of such deaths - attend and secure the scene, identify the victim, examine the incident location, conduct interviews with witnesses and people close to the deceased, and identify information about the likely cause of death. Police officers collect information including methods used, the presence of alcohol on the breath, apparent motivation for the suicide and verify whether the deceased had a recorded disability as registered in identifying documentation from the Ministry of Health. This information is recorded in a single computerised system.
-
•
Based on the police report, DINASED requests the regional forensic centre conduct an autopsy. Findings from the autopsy supplement the police investigation and contribute to DINASED's final classification of cause of death as homicide, suicide, or external death of undetermined intent. Every step is registered in the computerised system and linked using the individual's National identification number with sociodemographic data (marital status, occupation, date of birth, age, sex, ethnicity, disability) from the civil registry. The system records deaths by suicide from 2015 onwards.
Outcomes
Our primary outcome was monthly suicide counts. Suicide was determined from the police investigation and autopsy described above. We adjusted for the population size using official projections from the 2010 Census data of the National Institute of Census and Statistics (for the population aged ≥5 years).
Secondary outcomes included changes in the following characteristics of the deceased as recorded in the linked data: location (urban/rural and region where the death occurred), suicide methods used, civil status, ethnicity, presence of a disability, possible motives/triggers as identified in the police record and possible recent alcohol consumption. The police obtain additional details such as education and occupation from the Civil Registry, but due to high levels of missing data these were not included in our analysis.
Data analysis
We examined the difference in suicides from the pre-COVID-19 period to the COVID-19 period for the population and for six population subgroups. Our modelling strategy was to first identify the baseline trend in suicides in each time series using the pre-COVID-19 data (January 2015 to February 2020). We then used this model to forecast the expected number of suicides in the COVID-19 period (March 2020 to June 2021), comparing it with the observed number of suicides in the same period. To estimate how far the observed suicides differed from the expected suicides, we calculated a rate ratio, defined as the observed divided by the expected number of suicides, as well as its 95% confidence interval. Formulas for these estimates are contained in Lash et al.15
To estimate the baseline trend, we used time-series analysis to identify the best fitting model in each series. We did this using Poisson regressions with a scale term to account for overdispersion and an offset term to account for population size. We considered two possible models: (1) a model with a predictor for linear time trends only; or (2) a model with a predictor for a linear time trend and predictors capturing seasonality trends. (More complex models fitting non-linear time trends were not considered because of the low numbers of suicides in some series.) The linear time trend was fit to the data by including a variable coded 1, 2, …t representing each month and year of the study. Seasonality effects were estimated with Fourier terms (pairs of sine and cosine functions) entered into the models. We chose the best model on the basis of goodness of fit and assessed using the AIC statistic.
We examined suicide counts in the whole population and in the following subgroups: men, women, people aged 5 to 14 years (children), 15 to 24 years (youth), 25 to 59 years (adults of working age), and older adults (≥60), per the United Nations definition.16 We chose these categories to distinguish children from young adults and to divide adults into working-aged and retired, as we considered the social and economic impacts of the pandemic might differ in these groups.
For the risk factor data, we calculated risk ratios and risk differences and their 95% confidence intervals and two-sided exact p-values in Stata for the pre-COVID-19 and COVID-19 periods.
We analysed data in Stata, version 16·1. We are unable to provide the dataset as it was provided for exclusive use and not allowed to be shared.
Ethics committee approval
This study reports on anonymised and unidentifiable data available to the public upon request from the National Police. Following the Helsinki Declaration, international and national guidelines of good practice, we used this anonymous database to report on suicide trends ensuring that no harm was caused, or confidentiality breached. At the time this study was conducted, ethical approval was not required, given that we used an anonymous de-identified database.
Role of the funding source
There was no specific funding for this study. All authors had full access to all the data in the study and all had responsibility for the decision to submit for publication.
Results
Between January 1, 2015, and June 30, 2021, the police recorded 7 525 deaths by suicide. Records of 38 of these deaths were excluded after consultation with the police: 10 did not record the age of the deceased, two did not record sex and a further 26 cases were misclassified, stating motives that matched with homicide and not suicide. In total, 7 487 cases remained for the final analyses, 5 894 occurred before the pandemic and 1 593 occurred during the COVID-19 period. The suicide rate was 6·7 (per 100,000 person-years) in the pre-COVID-19 period and 7·0 (per 100,000 person-years) in the COVID-19 period (Table 1).
Table 1.
Number of suicides and rate (per 100,000 person-years) overall and by sex and age-group in the 62-month pre-pandemic period (January 2015–February 2020) vs. the first 16 months of the pandemic (March 2020–June 2021) with estimated rate ratios during the pandemic based on pre-pandemic trends from time-series analyses.
| No. deaths /rates per 100,000 before COVID-19 pandemic January 1, 2015–February 29, 2020 | No. deaths/ rates per 100,000 during COVID-19 pandemic March 1, 2020–June 30, 2021 | Rate ratio* (95%CI) | p-value | |
|---|---|---|---|---|
| All ages and sexes | 5894 6·7 |
1593 7·0 |
0·97 (0·92–1·02) | 0·1858 |
| Males | 4633 10·4 |
1261 11·0 |
0·95 (0·90–1·00) | 0·0479 |
| Females | 1261 2·9 |
332 3·0 |
1·05 (0·95–1·17) | 0·3357 |
| 5–14 years | 383 2·2 |
109 2·4 |
1·11 (0·92–1·34) | 0·2873 |
| 15–24 years | 1799 11·4 |
414 10·1 |
0·92 (0·83–1·01) | 0·0787 |
| 25–59 years | 2944 8·0 |
828 8·7 |
0·95 (0·88–1·01) | 0.1059 |
| ≥60 years | 768 8·4 |
242 10·2 |
1·08 (0·95–1·22) | 0·2598 |
*Note: Note the differences in rates per 100,000 person-years do not correspond with the rate ratios as the latter are derived from time series models which compare observed vs. predicted rates based on trends in rates between January 2015 and February 2020, rather than a crude comparison of rates over this period.
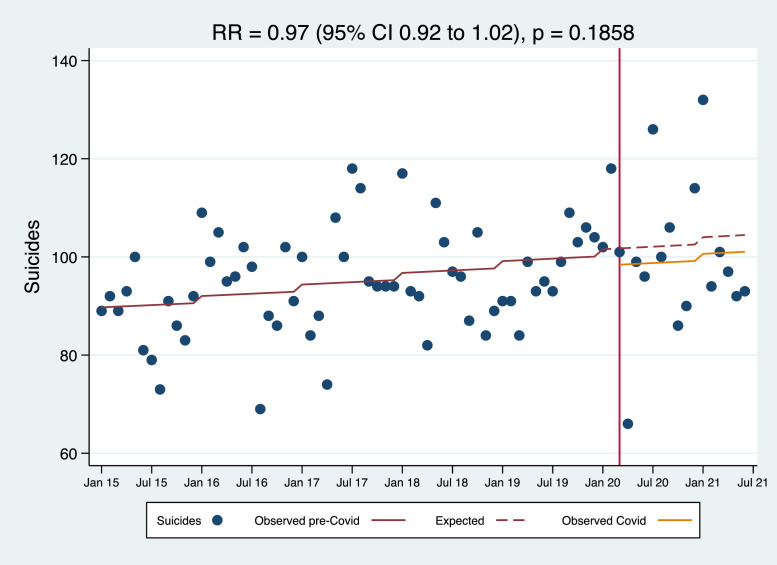
Our best-fitting model (a model with a linear time trend and no seasonality terms) indicated a non-significant (p = 0·255) upward linear trend in total suicides during the pre-COVID-19 period. There was no evidence that the observed number of suicides during the COVID-19 period differed from this pattern (RR 0·97, 95% CI 0·92–1·02; p=0·1858) (Figure 1, Table 1). In the population subgroups, there was some evidence that the number of male suicides was lower than predicted (RR 0·95, 95% CI 0·90–1·00; p=0·0479) but no differences were observed in any of the other groups we studied (see supplement for figures of trends over time for subgroups).
Figure 1.
Monthly suicide counts from January 1, 2015, to June 30, 2021, before and during the COVID-19 pandemic in Ecuador.
There was some evidence of differences in the distribution of risk factors before vs. during the pandemic (Table 2). During the pandemic, there were declines in the proportion of people dying by suicide who lived in rural areas (RR 0·88, 95% CI 0·81–0·96), were married or co-habiting (RR 0·90, 95% CI 0·82–1·00), were of indigenous ethnicity (RR 0·70, 95% CI 0·52–0·92), had a disability (RR 0·77, 95% CI 0·61–0·98), had school problems as motives/triggers (RR 0·62, 95% CI 0·42–0·92) and had alcohol detected on the breath (RR 0·73, 95% CI 0·61–0·86). In contrast, there were increases in the proportion of deaths amongst people of mestizos (mixed) ethnicity (RR 1·03, 95% CI 1·01–1·05) and for mental health problems as the motive for suicide (RR 1·21, 95% CI 1·01–1·45) There was no evidence of other changes in the motives thought to underlie a suicide. There was evidence that the methods used for suicide changed in the pandemic period, with increases in the use of hanging (RR 1·10, 95% CI 1·07–1·14) and falls in the use of poisoning (RR 0·73, 95% CI 0·63–0·86) and other methods (RR 0·83, 95% CI 0·71–0·98) (Table 3).
Table 2.
Proportion of suicides by risk factors in the 62-month pre-pandemic period (January 2015–February 2020) vs. the first 16 months of the pandemic (March 2020–June 2021).
| Suicide cases |
Risk |
|||||||
|---|---|---|---|---|---|---|---|---|
| Category | Variables | Pre-COVID -19 January 1, 2015, - February 29, 2020 | COVID -19 March 1, 2020 - June 30, 2021 | Pre-COVID-19 January 1, 2015, - February 29, 2020 | COVID-19 March 1, 2020 - June 30, 2021 | Risk difference (95% CI) | Risk ratio (95% CI) | p value |
| Urban/Rural | Rural | 1869/5894 | 445/1593 | 0·32 | 0·28 | -0·04(-0·06–-0·01) | 0·88(0·81–0·96) | <0·01 |
| Natural regions++ | Amazon | 360/5894 | 75/1593 | 0·06 | 0·05 | -0·01(-0·03–-0·00) | 0·77(0·60–0·98) | 0·03 |
| Coast | 2295/5894 | 667/1593 | 0·39 | 0·42 | 0·03(0·00–0·06) | 1·08(1·00–1·15) | 0·04 | |
| Highland | 3232/5894 | 850/1593 | 0·55 | 0·53 | -0·01(-0·04–0·01) | 0·97(0·92–1·02) | 0·29 | |
| Civil status | Married or living together | 1536/5894 | 375/1593 | 0·26 | 0·24 | -0·03(-0·00 -0·05) | 0·90(0·82–1·00) | 0·04 |
| Ethnicity | Mixed race/ ethnicity (Mestizos) | 5256/5894 | 1459/1593 | 0·89 | 0·92 | 0·02(0·01-0·04) | 1·03(1·01–1·05) | <0·01 |
| Indigenous | 299/5894 | 56/1593 | 0·05 | 0·04 | -0·02(-0·03–-0·00) | 0·70(0·52–0·92) | <0·01 | |
| Afro-ecuadorians | 108/5894 | 31/1593 | 0·02 | 0·02 | 0·00(-0·01–-0·01) | 1·06(0·72–1·58) | 0·75 | |
| Others (Mulatos, Montubios, Asians, White and Others) | 231/5894 | 47/1593 | 0·04 | 0·03 | -0·01(-0·02-0·00) | 0·75(0·55–1·03) | 0·07 | |
| Disability status | Disability | 370/5894 | 77/1593 | 0·06 | 0·05 | 0·01(-0·03–-0·00) | 0·77(0·61–0·98) | 0·03 |
| Motives or triggers++ | Economic problems | 659/5891 | 179/1593 | 0·11 | 0·11 | 0.01(-0·02-0·02) | 1·00(0·86–1·17) | 0·96 |
| Emotional problems | 2198/5891 | 608/1593 | 0·37 | 0·38 | 0·01(-0·02-0·04) | 1·02(0·95–1·10) | 0·54 | |
| Mental health | 430/5891 | 141/1593 | 0·07 | 0·09 | 0·02(0·00-0·03) | 1·21(1·01–1·45) | 0·04 | |
| School problems | 167/5891 | 28/1593 | 0·03 | 0·02 | -0·01(-002–0·00) | 0·62(0·42–0·92) | 0·02 | |
| Terminal disease | 442/5891 | 108/1593 | 0·08 | 0·07 | -0·01(-0·02–0·01) | 0·90(0·74–1·11) | 0·36 | |
| Family problems | 1985/5891 | 523/1593 | 0·34 | 0·33 | -0·01(-0·03–0·02) | 0·97(0·90–1·05) | 0·53 | |
| Alcohol | Alcohol smell on breath | 708/5894 | 139/1593 | 0·12 | 0·09 | -0·03(-0·05–0·02) | 0·73(0·61–0·86) | <0·01 |
*Two-sided Fisher's exact p value.
+The police did not report data from the Insular region (Galapagos).
For motives, in the pre-COVID-19 period three cases were not classified. The motive of religious beliefs was excluded because there were only 16 cases in total.
Table 3.
Methods used for suicide in the 62-month pre-pandemic period (January 2015–February 2020) vs. the first 16 months of the pandemic (March 2020–June 2021).
| Suicide cases |
Risk |
|||||||
|---|---|---|---|---|---|---|---|---|
| Category | Variables | Pre-COVID-19 January 1, 2015, - February 29, 2020 | COVID-19 March 1, 2020 - June 30, 2021 | Pre-COVID-19 January 1, 2015, - February 29, 2020 | COVID-19 March 1, 2020 - June 30, 2021 | Risk difference (95% CI) | Risk ratio (95% CI) | p value |
| Methods used | Firearms | 322/5894 | 72/1593 | 0·05 | 0·05 | -0·01 (-0·02–0·00) | 0·83 (0·64–1·06) | 0·15 |
| Hanging | 3952/5894 | 1179/1593 | 0·67 | 0·74 | 0·07 (0·04–0·09) | 1·10 (1·07–1·14) | <0·01 | |
| Knives and cutting blades | 110/5894 | 24/1593 | 0·02 | 0·02 | -0·00 (-0·01–0·00) | 0·81 (0·52–1·25) | 0·39 | |
| Poisoning | 816/5894 | 162/1593 | 0·14 | 0·10 | -0·04 (-0·05–-0·02) | 0·73 (0·63–·86) | <0·01 | |
| Others | 694/5894 | 156/1593 | 0·12 | 0·10 | -0·02 (-0·04–0·00) | 0·83 (0·71–0·98) | 0·03 | |
*Two-sided Fisher's exact p value.
Discussion
The findings from our study suggest there was no evidence of an overall change in suicide rates nationwide in Ecuador in the first 16 months of the COVID-19 pandemic from March 2020 to June 2021, compared to predicted levels based on pre-pandemic trends. There was, however, some evidence of fewer than expected male suicides.
Mental health researchers warned of the potential impact of the pandemic on individuals’ mental health, due to public health restrictions, economic difficulties, access to healthcare, and education (including the closure of schools),17 especially in vulnerable groups such as children and adolescents. In Ecuador, education shifted online between March 2020 and June 2021 with very few schools delivering face-to-face teaching. Furthermore, families with children may have been particularly affected by decreases in income, crowded housing conditions, and domestic violence.18
For adults aged 60 and over, loneliness is an important risk factor for suicide,19 and because of physical distancing measures and the fear of COVID-19, many older adults were confined to their homes, losing social connections and having limited access to online support.17 Data from the SARS outbreak in 2003 in Hong Kong indicated that older people were at a greater risk of suicide during that epidemic,13 however our study found no evidence of this in people aged over 60 years.
There were fewer than expected suicides amongst males, despite the fact that they may have been particularly vulnerable to the economic consequences of the pandemic. Many Ecuadorians live in close-knit family groups, where the permanent presence of others could have helped prevent suicide.
Our study found that the proportion of suicides in rural areas decreased during the COVID-19 pandemic, while there was a shift between the Coastal and Amazon regions, with an increased proportion occurring in the Coastal region, and a decreased proportion in the Amazon region. This is surprising, as historically the Coast has had considerably lower suicide rates than the Highland and Amazon regions.20 As for the impact of the pandemic across Ecuador's regions, evidence shows the Coast was the worst affected area, with the highest excess mortality of all regions21; patients with diagnosed or suspected COVID-19 from the Coast also had higher levels of anxiety and depression than in other regions.22 It could be hypothesised that the impact of the COVID-19 pandemic on the inhabitants of coastal areas may have influenced the increase in the proportion of suicides. However, studies that address this issue in greater depth are needed.
In terms of suicide methods, our findings that the proportion of suicides by hanging increased contrasts with the decreases recorded in hanging in a study from Romania23 and in suffocation (largely hanging) in the US.24 However, our findings that suicide by poisoning declined are consistent with US findings.24 It is possible that self-poisoning may be more difficult to implement if others are at home due to stay-at-home orders; likewise, the suicide attempt may be discovered earlier, leading to prompt hospital treatment saving the life of the person who attempted to take his own life.
The drop in the proportion of suicides in indigenous and other minorities is surprising, as these groups historically accounted for a disproportionate number of suicides relative to their population size25 and these groups had higher overall mortality during the pandemic.21 Ethnic disparities in the impact of the pandemic on suicide rates have been reported in studies from the United States.24 Our finding of a decrease in the proportion of suicides by indigenous people is consistent with the decreases observed in the suicide rates of Native Hawaiian people in the US.24 However, Ehlman et al.24 also reported nonsignificant increases in American Indian or Alaska Native suicides and, in keeping with our study, increases in people of mixed race. It is possible that associations may depend on whether a specific ethnic group is a minority or a majority population in the geographical region they inhabit. The lower proportion of deaths by suicide among indigenous people in Ecuador could be related to social factors, such as community union in face of adversity. However, given that indigenous suicide is an extremely complex and under-researched issue, further research is needed to understand contributing factors as these may be informative for future suicide prevention initiatives.
Alcohol consumption has been linked to increases in mental health problems and suicide.26 Our study indicates that in the year since the pandemic began, lower proportions of suicide victims were reported by police to smell of alcohol. Banning the sale of alcohol, closure of bars and pubs, and the physical distancing measures to prevent the spread of the virus (e.g., restrictions on social gatherings and stay-at-home orders) may have contributed towards reducing alcohol consumption in vulnerable people and the fall in male suicides (see above). There is, to our knowledge, no representative study on alcohol use in Ecuador, however, a survey conducted by the Pan-American Health Organization in several Andean countries, including Ecuador, showed that the prevalence of self-reported episodic heavy episodic alcohol consumption decreased from 51% in 2019 to 24% in 2020,27 suggesting that restrictive policies may have reduced harmful alcohol consumption. The Internal Revenue Service reported a 25% reduction in sales of alcoholic beverages between 2019 and 2020.28 This could possibly have led to a reduction of men psychologically vulnerable to suicide exposed to harmful alcohol use in Ecuador. Our findings are consistent with other data showing alcohol regulations are associated with falls in suicide.29 Therefore (re)-implementation of laws and regulations, such as taxation, and sales restrictions on certain hours or days may be a cost-effective public health policy to reduce suicide as well as other alcohol-related mortality.30
The pandemic does not appear to have changed the order of importance of the reported motives/triggers for suicide, with the most common reason reported by the police being emotional and family problems. Despite national economic hardship and a rise in unemployment rates during the pandemic, economic problems as an apparent motivation for suicide did not increase during the pandemic period. The reduction in school problems could be explained by the fact that until June 2021 students were largely taught in online classes, and this may have resulted in reduced bullying and other school-related stress. The increase in the proportion of suicides where mental health problems were identified as a motive may reflect the impact of the pandemic not only on population mental health,2,22 but also on the availability of health services support for mental illness – health services were already understaffed before the pandemic and suffered significant human losses during the pandemic.12
The lack of an increase in the proportion of suicides amongst those with disabilities is surprising as disabled people may have experienced increased difficulties with their health, worries about their vulnerability to infection, and difficulties in accessing care during the pandemic.
It is possible that the physical distancing measures to prevent the spread of the virus, like stay-at-home orders may have increased family and community unity.31 Adversities shared by whole communities may foster a sense of togetherness, as was observed in the aftermath of the 2016 Ecuadorian earthquake. While adolescents who had stayed in shelters for over nine months after the disaster showed higher levels of anxiety and depression than those who were less affected, their suicide ideation was lower.32
Strengths and limitations
To our knowledge, our study is one of the first national studies of suicide rates by age group and sex in a LMIC, which compares the contribution of different suicide risk factors before and during the pandemic. The police database includes several variables such as possible motives for the suicide, presence of a disability, and the possible contribution of alcohol to the suicide. This information provides important insights into changes in patterns of risk factors for suicide.
Nevertheless, there are several potential limitations to our findings. First, police investigations into suicides may have been hampered because of COVID-19 restrictions and concerns about their own risk of becoming infected. Second, the quality and completeness of the suicide data may vary from region to region and across time, depending on the degree of disruption caused by the pandemic and variations in the quality of police data collection due to staff capacity and training. For example, during the period when the most deaths occurred in the city of Guayaquil (April–May 2020), the police force investigating deaths by suicide was also responsible for collecting the bodies of people who died from COVID-19 and other causes in this area. With a large increase in deaths during the early months of the pandemic, fewer resources would have been available for investigating suicides, which could lead to lower data quality and underreporting.
Third, some risk factor variables (e.g., motivation for suicide, presence of alcohol) are potentially difficult to record reliably. Data on motives for suicide were collected by police officers, but not using the more rigorous psychological autopsy-based approaches used in many studies of suicide. Furthermore, the smell of alcohol on the breath is a subjective measure that may depend on when this is assessed. Blood alcohol levels would provide a more reliable assessment but are not currently included in the police dataset. Other data, such as disability and marital status, which the police obtain from social registers and the Ministry of Health may have been out of date due to recording delays during the first year of the pandemic. Lastly, we did not have data on key areas of concern such as domestic violence or difficulty accessing mental health services, both of which may have influenced suicide rates during the pandemic.
Conclusion
Our findings show that in the first year of the pandemic in Ecuador, with the exception of somewhat fewer than expected male suicides, there were no marked changes in suicide mortality trends. Nevertheless, the long-term impact of the economic, health, and social consequences of the pandemic on suicide remains uncertain, meaning there is a need for continued monitoring in order to respond to any increases in suicide. More data are required from other LMICs to better understand the impact of the pandemic on suicide trends and determine which features of national responses may have resulted in rises in suicide rates in some countries9,10 but not others. The possibility that alcohol sales restrictions may have contributed to the decline in male suicides requires further investigation.
Contributors
RG, MIT, and PAA conducted the literature review and prepared the manuscript. RG and FN conducted data cleaning and risk data analysis with statistical overview from SL. MJS advised about the data analysis framework and conducted the time-series analysis. DG, MJS and SL interpreted data and made critical intellectual revisions to the manuscript. All authors interpreted data and made critical intellectual revisions to the manuscript.
Data sharing statement
Data used in this study was shared exclusively to study authors. Data may be obtained from a third party (National Police of Ecuador) and are not publicly available. Any data requests can be made to the National Police of Ecuador.
Declaration of interests
Matthew Spittal is a recipient of an Australian Research Council Future Fellowship (project number FT180100075) funded by the Australian Government. David Gunnell receives funding support from the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust. Stuart Leske is a recipient of a grant from Queensland Health. The other authors declare no competing interests.
Acknowledgments
We acknowledge the National Police of Ecuador, specifically the National Directorate of Crimes Against Life, Violent Deaths, Disappearances, Extortion and Kidnapping (DINASED) for sharing requested information about suicides in police reports and providing relevant information relating to the methodology of the data collection. DG is supported by the NIHR Biomedical Research Centre at University Hospitals Bristol and Weston NHS Foundation Trust and the University of Bristol, England. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Footnotes
Supplementary material associated with this article can be found, in the online version at doi:10.1016/j.lana.2022.100324.
Appendix. Supplementary materials
References
- 1.World Health Organization (WHO) [cited 9 May 2022]. COVID-19 weekly epidemiological update. Situation Report (04 May 2022), Washington, DC, 2022. https://reliefweb.int/report/world/weekly-operational-update-covid-19-4-may-2022
- 2.Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheridan Rains L, Johnson S, Barnett P, et al. Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Soc Psychiatry Psychiatr Epidemiol. 2021;56:13–24. doi: 10.1007/s00127-020-01924-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pirkis J, John A, Shin S, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8:579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calderon-Anyosa RJC, Bilal U, Kaufman JS. Variation in non-external and external causes of death in Peru in relation to the COVID-19 lockdown. Yale J Biol Med. 2021;94:23–40. [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng X-Y, Tang S-L, Ma S-L, et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-045317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borges G, Garcia JA, Pirkis J, et al. A state level analyses of suicide and the COVID-19 pandemic in Mexico. BMC Psychiatry. 2022;22 doi: 10.1186/s12888-022-04095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acharya B, Subedi K, Acharya P, Ghimire S. Association between COVID-19 pandemic and the suicide rates in Nepal. PLoS One. 2022;17 doi: 10.1371/journal.pone.0262958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arya V, Page A, Spittal MJ, et al. Suicide in India during the first year of the COVID-19 pandemic. J Affect Disord. 2022;307:215–220. doi: 10.1016/j.jad.2022.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ritchie H, Ortiz-Ospina E, Beltekian D, et al. [cited 14 March 2022]. Estimated excess mortality from The Economist. https://ourworldindata.org/excess-mortality-covid
- 12.Secretaría Planifica Ecuador (SPE) [cited 20 March 2022]. Evaluación socioeconómica PDNA Covid-19 Ecuador. Quito, Ecuador, 2020. https://www.planificacion.gob.ec/wp-content/uploads/downloads/2021/06/INFORME_PDNA_COVID-19_ECUADOR_WEB.pdf
- 13.Cheung YT, Chau PH, Yip PSF. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int J Geriatr Psychiatry. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- 14.Haw C, Hawton K, Gunnell D, Platt S. Economic recession and suicidal behaviour: possible mechanisms and ameliorating factors. Int J Soc Psychiatry. 2014;61:73–81. doi: 10.1177/0020764014536545. [DOI] [PubMed] [Google Scholar]
- 15.Lash T, VanderWeele T, Haneuse S, Rothman K. 4th edn. Lippincott Williams and Wilkins; 2021. Modern Epidemiology. [Google Scholar]
- 16.UNHCR . 2022. Older Persons - UNHCR|Emergency Handbook.https://emergency.unhcr.org/entry/43935/older-persons Accessed 3 March 2022. [Google Scholar]
- 17.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United Nations Children's Fund (UNICEF) 2021. Ecuador Humanitarian Situation Report.https://www.humanitarianresponse.info/en/operations/ecuador/wash/documents Accessed 4 March 2022. [Google Scholar]
- 19.Conejero I, Olié E, Courtet P, Calati R. Suicide in older adults: current perspectives. Clin Intervent Aging. 2018;13:691–699. doi: 10.2147/CIA.S130670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ortiz-Prado E, Simbaña K, Gómez L, et al. The disease burden of suicide in Ecuador, a 15 years’ geodemographic cross-sectional study (2001–2015) BMC Psychiatry. 2017;17:342. doi: 10.1186/s12888-017-1502-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cuéllar L, Torres I, Romero-Severson E, et al. Excess deaths reveal the true spatial, temporal and demographic impact of COVID-19 on mortality in Ecuador. Int J Epidemiol. 2022;51:54–62. doi: 10.1093/ije/dyab163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paz C, Mascialino G, Adana-Díaz L, et al. Behavioral and sociodemographic predictors of anxiety and depression in patients under epidemiological surveillance for COVID-19 in Ecuador. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vuscan ME, Buciuta A, Vica ML, et al. Impact of the COVID-19 pandemic on the suicidal behavior in Romania. Arch Suicide Res. 2022:1–11. doi: 10.1080/13811118.2021.2022052. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 24.Ehlman D, Yard E, Stone D, Jones C, Mack K. Changes in suicide rates—United States, 2019 and 2020. Morb Mort Wkly Rep. 2022;71(8):306–312. doi: 10.15585/mmwr.mm7108a5. [DOI] [PubMed] [Google Scholar]
- 25.Troya MI, Gerstner RM, Narvaez F, Arensman E. Sociodemographic analysis of suicide rates among older adults living in Ecuador: 1997-2019. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.726424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol Med. 2017;47:949–957. doi: 10.1017/S0033291716002841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garcia-Cerde R, Valente JY, Sohi I, Falade R, Sanchez ZM, Monteiro MG. Alcohol use during the COVID-19 pandemic in Latin America and the Caribbean. Rev Panam Salud Publica 2021;45:e52. 10.26633/RPSP.2021.52. [cited 2022 March 20]. Available from: https://iris.paho.org/handle/10665.2/53908. [DOI] [PMC free article] [PubMed]
- 28.Servicio de Rentas Internas. Sistema de identificación, marcación, autentificación, rastreo y trazabilidad fiscal de bebidas alcohólicas, cervezas y cigarrillos de producción nacional. https://www.sri.gob.ec/simar. [cited 25 March 2022]
- 29.Kõlves K, Chitty KM, Wardhani R, Värnik A, de Leo D, Witt K. Impact of alcohol policies on suicidal behavior: a systematic literature review. Int J Environ Res Public Health. 2020;17(19) doi: 10.3390/ijerph17197030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ortiz-Prado E, Mascialino G, Paz C, et al. A nationwide study of incidence and mortality due to traumatic brain injury in Ecuador (2004–2016) Neuroepidemiology. 2020;54(1):33–44. doi: 10.1159/000502580. [DOI] [PubMed] [Google Scholar]
- 31.Sinyor M, Knipe D, Borges G, et al. Suicide risk and prevention during the COVID-19 pandemic: one year on. Arch Suicide Res. 2021:1–6. doi: 10.1080/13811118.2021.1955784. Ahead of print. [DOI] [PubMed] [Google Scholar]
- 32.Gerstner RMF, Lara-Lara F, Vasconez E, Viscor G, Jarrin JD, Ortiz-Prado E. Earthquake-related stressors associated with suicidality, depression, anxiety and post-traumatic stress in adolescents from Muisne after the earthquake 2016 in Ecuador. BMC Psychiatry. 2020;20:347. doi: 10.1186/s12888-020-02759-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.