Abstract
Purpose
Uric acid (UA) is thought to exert neuroprotective roles. The purpose of this study was to examine the association of serum UA with suicide attempts (SA) in adolescents and young adults with major depressive disorder (MDD).
Patients and Methods
We retrospectively recruited 533 participants with MDD aged 13 to 25 years, of which 168 had a history of SA in the past three months and 365 did not have a history of SA. Serum UA levels were measured using the uricase-peroxidase coupling method. In addition to overall serum UA level comparison in MDD individuals with and without SA, a stratified analysis by biological sex was carried out.
Results
Compared to MDD individuals without a history of SA, serum UA levels were significantly lower in MDD individuals with SA (P < 0.001). Female MDD, but not male MDD individuals, with SA exhibited lower levels of UA than those without SA (P < 0.01). Importantly, serum UA remained significantly associated with SA in MDD individuals (OR = 0.996, 95% CI: 0.993~0.999, P < 0.01) when controlling for possible confounding variables.
Conclusion
This research identifies a relationship between serum UA levels and SA in adolescents and young adults with MDD. UA may represent a biological risk marker for SA, in particular for female MDD individuals.
Keywords: suicide, MDD, uric acid, antioxidant, oxidative stress, biomarker
Introduction
Suicide is an important public health concern,1 accounting for 1.5% of all deaths globally. It is estimated that there are approximately 800,000 suicides worldwide each year, corresponding to 11.4 suicides per 100,000 people.2 Critically, suicide has become the second leading cause of death in adolescents and young adults aged 15–29 years.2 Suicidal behavior is divided into four subtypes: suicidal ideation (SI), suicide plan (SP), suicide attempts (SA), and completed suicide (CS). SI and SA generally peak in adolescence and young adulthood, with a prevalence of SI and SA in adolescents and young adults of 12.1–33% and 4.1–9.3%, respectively.3,4 In China, 63% of suicide victims are found to put up with mental illness prior to death, of which major depressive disorder (MDD) is the most common psychiatric illness.5 It has been estimated that the lifetime prevalence and one-month prevalence rates of SA in MDD are 23.7% and 20.3%, respectively.6 SA has moreover emerged as the most robust clinical predictor for future death by suicide.7,8 Thus, early detection and potential prevention of SA in MDD individuals is critical in the context of suicide prevention research.
Suicide is a complex behavior with heterogeneous traits and is related to many risk factors.1 For instance, previous studies have reported that sleep disturbances, childhood trauma, and psychache are some of the risk factors associated with suicide.9,10 Over the past decade, research has investigated the neurobiological processes underlying suicide, but so far no work has enabled substantial prediction of suicide.11,12 The limited understanding of the pathophysiology of suicide and the lack of effective predictive biomarkers therefore represent urgent medical issues.
Previous studies have shown that oxidative stress damage may be involved in the development of suicidal behavior13,14 and there is evidence that plasma levels of certain oxidative damage markers are increased, while markers of total antioxidant capacity are decreased, in individuals with MDD and SA.13 Another study found that low concentrations of serum antioxidant vitamins and carotenoids were associated with a history of SA.15 These findings suggest that individuals who attempt suicide may have a dysfunctional antioxidant system, which is a defense system counteracting or lessening oxidative damage.16–18 Uric acid (UA) is a final product of purine metabolism and is predominantly excreted by the kidneys. Elevated levels of UA can cause certain physical illnesses, including as gout, metabolic syndrome, or cardiovascular disease.19,20 However, UA is also a potent antioxidant in the central nervous system21 and accounts for more than 50% of the free-radical clearance ability of human blood.22 Many studies have demonstrated that lower levels of serum or plasma UA are associated with an elevated risk for multiple neuropsychiatric diseases, such as Alzheimer’s disease,23 Parkinson’s disease,24 and MDD.25 Moreover, studies have shown that high plasma urate levels are associated with a slower decrease in cognitive functions in individuals with mild cognitive impairment.26 These studies indicate that UA has a potential neuroprotective function which may be related to its antioxidant capacity.
While a small sample study previously explored the association UA serum levels and the severity of SI in individuals with major affective disorders,27 research exploring the association between UA and suicidal behavior is still limited. Hence, we evaluated serum levels of UA retrospectively in adolescent and young adult individuals with MDD and their association with SA. The purpose of this research was to investigate the association between serum UA levels and SA. We also discuss whether UA may be used as a biomarker of suicidal behavior. As previously sex differences in UA levels have been observed,28 we also carried out a stratified analysis by gender.
Materials and Methods
Study Population
We recruited a total of 533 participants aged 13 to 25 years from the database of the Case-data Management Platform of the University-Town Hospital of Chongqing Medical University between February 2016 and December 2021. For all cases, MDD or recurrent MDD were determined by two experienced clinical psychiatrists according to the 10th Revision of the International Classification of Diseases (ICD-10). In the current study, we included 168 individuals with MDD who attempted suicide over the past three months and 365 individuals with MDD without a history of SA.
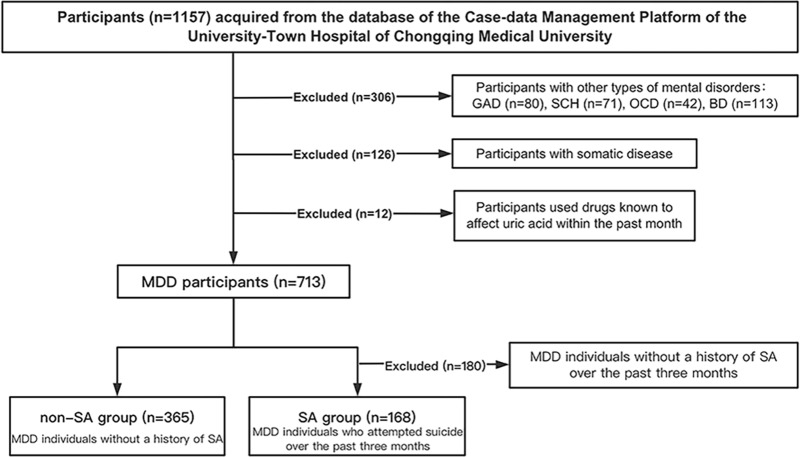
The exclusion criteria were as follows: presence of other types of mental disorders, nervous system diseases, chronic medical conditions (diabetes, hypertension, cardiovascular disease, kidney disease, or similar), allergic diseases, metabolic syndrome, gout, thyroid disease, liver function abnormality, pregnancy or lactation, or use of drugs known to affect uric acid within the past month (Figure 1).
Figure 1.
Flow chart of participant selection.
Abbreviations: MDD, major depressive disorder; GAD, generalized anxiety disorder; SCH, schizophrenia; OCD, obsessive-compulsive disorder; BD, bipolar disorder; SA, suicide attempt.
The study complied with the Declaration of Helsinki, it was approved by the University-Town Hospital of Chongqing Medical University Ethics Committee (LL-202161) and implemented according to relevant ethical requirements. As the retrospective nature of this study, participant informed consent was waived. All the collected data were kept confidential and only used in this study. The personal identity information of all the participants was not disclosed.
Assessment of Suicide Attempt, Depression, and Anxiety
The definition of suicide attempts was referred to the Columbia-Suicide Severity Rating Scale.29 Suicide attempts were characterized as potentially self-injurious behavior accompanied by a conscious intention to end one’s life requiring emergency medical intervention or hospitalization. The Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) scales were used on the day of the participant’s admission, to evaluate their severity of depression and anxiety, respectively.30,31
Data Collection
A custom-made electronic case report questionnaire designed in this research was used to collect demographic (age, sex, education), lifestyle (body mass index (BMI), smoking, alcohol use) and clinical data (age of onset, duration of disease, psychosis family history, antidepressant use, suicide attempts behavior). Alcohol use was classified in three groups according to frequency of alcohol consumption per week: never, occasional (<1 time per week), or frequent (≥1 times per week). The BMI was computed as weight (kg)/height (m2). Data were acquired from the database of the Case-data Management Platform of the University-Town Hospital of Chongqing Medical University by two fully trained researchers and independently confirmed by two independent researchers. The database records the basic information as well as the disease progress and the treatment course of all participants.
Laboratory Assessments
Approximately 3 mL fasted venous blood was obtained from subjects between 6:30 and 7:00 a.m. after overnight fasting. The serum was isolated from blood samples after centrifugation (3500×g for 5 min) and serum uric acid was measured using the uricase-peroxidase coupling method on the Fully Automatic Biochemical Analyzer (BS-800M; Mindray, China).
Statistical Analyses
Measurement data is shown as mean ± standard deviation (SD) or median (interquartile range, IQR). To assess differences between the SA and non-SA groups, independent t-tests or Mann–Whitney U-tests were used. To compare count data between groups, chi-square or Fisher’s exact tests (when the expected frequency was <5) were used. According to the history of antidepressant use, we used the Mann–Whitney U-test in SA and non-SA groups separately, to compare the difference of serum UA levels in different antidepressant use groups. We applied logistic regression analyses to analyze the relationship between UA and attempted suicide, with variables associated with SA in univariable analysis included as potential confounding factors and computed odds ratios (OR) and 95% confidence intervals (CI). All statistical data analyses were conducted using SPSS software (version 25.0). P < 0.05 (two-tailed) was considered statistically significant.
Results
Participant Characteristics
We identified 1157 potentially eligible participants. We excluded 306 participants with other types of mental disorders, 126 participants with somatic disease, 12 participants using medication known to influence uric acid within the past month, and 180 participants without SAs in the past three months. We ultimately included 533 participants with MDD, 73.5% of whom were female. Among all participants, 168 had a history of suicide attempts (SA group) while the remaining 365 did not (non-SA group) (Figure 1). The demographic, lifestyle, and clinical characteristics of the included subjects are displayed in Table 1. Participants had an average age of 17.63 ± 2.97 years and an average of 11.33 ± 2.34 years of education.
Table 1.
Demographic, Lifestyle, and Clinical Characteristics of Included Participants
| History of Suicide Attempts (N = 168) | No History of Suicide Attempts (N = 365) | t/χ2/ Z | P-value | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Median (IQR) | Median (IQR) | |||
| Demographics | ||||
| Age (years) | 17.19 ± 2.83 | 17.83 ± 3.02 | −2.313 | <0.05 |
| Sex, female, n (%) | 130 (77.4%) | 262 (71.8%) | 1.854 | 0.173 |
| Education (years) | 11.11 ± 2.29 | 11.43 ± 2.37 | −1.464 | 0.144 |
| Lifestyle | ||||
| BMI (kg/m2) | 19.82 ± 2.18 | 20.12 ± 2.30 | −1.417 | 0.157 |
| Smoking, yes, n (%) | 27 (16.1%) | 31 (8.5%) | 6.813 | <0.01 |
| Alcohol use, n (%) | <0.01 a | |||
| Never | 138 (82.1%) | 331 (90.7%) | ||
| Occasionally | 26 (15.5%) | 34 (9.3%) | ||
| Frequently | 4 (2.4%) | 0 (0%) | ||
| Clinical features | ||||
| Age of onset (years) | 14.96 ± 3.16 | 15.85 ± 3.40 | −2.840 | <0.01 |
| Duration of disease (months) |
15.00 (6.00~36.00) | 12.00 (6.00~36.00) | −1.216 | 0.224 |
| Psychosis family history, yes, n (%) | 26 (15.5%) | 53 (14.5%) | 0.083 | 0.773 |
| Antidepressant use, n (%) | 7.827 | <0.01 | ||
| None | 72 (42.8%) | 204 (55.9%) | ||
| SSRIs | 68 (40.5%) | 113 (30.9%) | ||
| SNRIs | 7 (4.2%) | 20 (5.5%) | ||
| Other | 21 (12.5%) | 28 (7.7%) | ||
| PHQ-9 | 19.83 ± 5.64 | 17.34 ± 5.88 | 4.600 | <0.001 |
| GAD-7 | 13.60 ± 5.84 | 12.43 ± 5.44 | 2.247 | <0.05 |
Notes: a Fisher’s exact test. Bold and italics P-values indicate significance (P < 0.05).
Abbreviations: SD, standard deviation; IQR, inter quartile range; BMI, Body mass index; SSRIs, selective serotonin re uptake inhibitors; SNRIs, serotonin-norepinephrine reuptake inhibitors; other, including bupropion, tandospirone, buspirone, quetiapine, agomelatine, mirtazapine, alprazolam; PHQ-9, Patient Health Questionnaire-9; GAD-7, Generalized Anxiety Disorder-7.
Participants in the SA group were younger, more likely to be smokers, had a younger age of MDD onset, and more severe depression and anxiety compared to participants the non-SA group. Moreover, there was statistical difference in alcohol use and antidepressant drug use (57.2% in SA versus 44.1% in non-SA) between the two groups. Gender, years of education, BMI, disease duration and psychosis family history were not significantly different between the groups (p > 0.05).
After a stratification by gender, there was a significant difference in female participants with SA and without SA for smoking, alcohol use, age of onset, antidepressant use, and depression and anxiety severity (Table S1). In male participants, the severity of depression was different between the SA and non-SA group (Table S2).
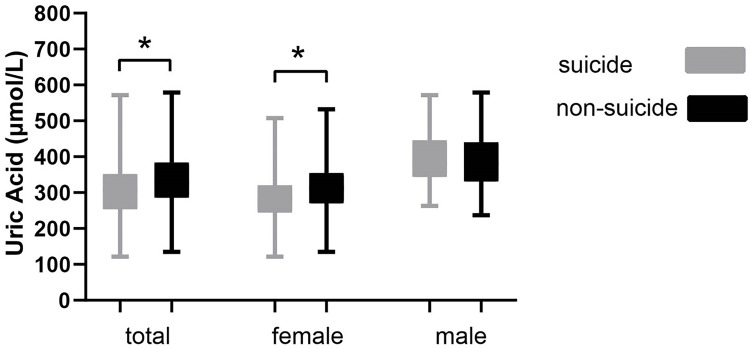
Serum Levels of UA
Serum levels of UA in each group are displayed in Figure 2 and Table S3. Serum UA levels were significantly lower in the SA group than non-SA group looking at the participants overall or female participants only (P < 0.001 and P < 0.001), but not when assessing differences in the SA and non-SA group in males only (P > 0.05), suggesting the effect was largely driven by differences in female participants.
Figure 2.
Comparison of serum UA levels in the SA and non-SA group in all participants, or female and male participants, respectively.
Note: *P < 0.001.
Abbreviations: UA, uric acid; SA, suicide attempt.
Association of Serum UA with SA
After controlling for all potential influencing factors, binary logical regression analysis revealed that serum UA levels were significantly associated with SA in both overall and female participants (OR = 0.996, 95% CI: 0.993~0.999, P < 0.01 and OR = 0.993, 95% CI: 0.989~0.996, P < 0.001, respectively) (see Table 2).
Table 2.
Logistic Regression Analysis of Attempted Suicide and UA Levels
| Item | Independent Variable | B | OR | 95% CI | P-value |
|---|---|---|---|---|---|
| Overalla | Uric acid | −0.004 | 0.996 | 0.993~0.999 | <0.01 |
| Femaleb | Uric acid | −0.007 | 0.993 | 0.989~0.996 | <0.001 |
| Malec | Uric acid | 0.001 | 1.001 | 0.996~1.007 | 0.609 |
Notes: aControl age, smoking, alcohol use, age of onset, antidepressant use, depression and anxiety symptoms severity, bcontrol smoking, alcohol use, age of onset, antidepressant use, depression and anxiety symptoms severity, ccontrol depression symptoms severity. Bold and italics P-values indicate significance (P < 0.05).
Analysis of the Effects of Antidepressant Use on UA
We also tested the effects of antidepressant drug use on serum UA. We found no significant difference in serum UA levels between subjects with and without antidepressant use comparing the SA and non-SA group (P > 0.05) (Figure S1).
Discussion
In the present study, we examined the levels of serum UA in 533 adolescent and young adult with MDD, including 168 with a history of SA and 365 without, and explored the relationship between serum UA levels and SA. Our results suggest that UA levels are significantly lower in participants with SA than in those without SA when looking at overall participants of female individuals only. Moreover, controlling for possible confounding variables, regression analysis demonstrated that serum UA levels were significantly associated with SA. Serum UA levels were not markedly affected by the antidepressant. Our results are in line with two previous studies which demonstrated reduced levels of antioxidant markers in individuals with a history of SA.13,15 Together with our study, these findings indicate that SA in individuals with MDD may be associated with an impaired antioxidant defense system. Our research is also consistent with a similar study reporting that serum UA levels were negatively associated with the severity of SI in a small sample study of individuals with major affective disorders.27 However, another study found no difference in serum UA levels between 69 MDD individuals with SA and 202 MDD individuals without a history of SA in China.32 The discrepancy in results may potentially be explained by differences in sample size. Moreover, the previous study also included significantly older participants (average age is about 36 years compared to 17 years in our study) and did not specifically investigate adolescents and young adults. Serum UA levels have been reported to be influenced by age,33 hence we speculate that the difference in participant ages may be one of the key factors contributing to the diverging results in these two studies.
Oxidative stress refers to the excessive production of reactive oxygen species (ROS) and reactive nitrogen species (RNS) or a reduction in the antioxidant defense system, that is, an imbalance of the pro- and antioxidant system.34,35 The accumulation of ROS in vivo or in cells has been shown to lead to oxidative damage of DNA, proteins, and lipids, which may result in apoptosis and cell death.35,36 A post-mortem study found that suicide victims who died of asphyxiation had higher expression levels of NADPH oxidase 2 (NOX2) in the cerebral cortex than controls or non-suicide subjects who died of asphyxiation.14 ROS are predominantly produced by NOX2.37 Cells typically prevent oxidative damage by using the antioxidant defense system, including enzymatic and non-enzymatic antioxidants, to limit ROS.38,39 UA is a powerful endogenous, hydrophilic non-enzymatic antioxidant which plays a pivotal role in the antioxidant system. It possesses more than half of antioxidant capacity in plasma, which is enabled by scavenging of free radicals and preventing the oxidation of ascorbic acid, another well-known non-enzymatic antioxidant.21,22 Importantly, UA levels can indirectly reflect the state of the antioxidant system in the body. There is evidence that individuals with a history of suicide attempts exhibit higher levels of oxidative stress than those without.13,14
We speculate that low UA levels may be caused by resistance to excessive oxidative stress damage. However, there is another possible theory: individuals with low UA levels may exhibit a lower antioxidant defense capacity. The antioxidant capacity of UA has been suspected to convey neuroprotective functions and as the brain consumes high levels of oxygens, lower antioxidant levels may render the brain vulnerable to oxidative damage.40
Additionally, indirect evidence indicates that the purinergic system contributes to neurobiological mechanisms for suicidal behavior in mental illness.41 Purinergic signaling may influence depression-related suicidal behaviors via adenosine A2A receptor.42 A previous epidemiological study reported that caffeine, an adenosine receptor antagonist, is correlated with a lower risk of suicide.43,44 Presumably, there could be activation of adenosine A2A receptors in individuals with depression-related suicidal ideation. A decrease in the activity of adenosine deaminase, a key enzyme in the adenosine metabolic pathway, has been shown to result in elevated adenosine levels45 which may be related to the activation of adenosine receptors. Importantly, a decline of adenosine deaminase activity is also accompanied by a decrease in uric acid, the end metabolite of adenosine.42 Our results provide novel clinical evidence which supports an association between the purinergic system and suicidal behavior.
Stratified analysis by gender showed that serum UA levels were significantly lower in female MDD individuals with a history of SA than those without. Interestingly, we did not observe any differences in UA levels in male MDD individuals without SA. A possible reason for this discrepancy is a relatively small proportion of male participants in our study. On the other hand, this discrepancy may also be related to differences in sex hormones between men and women. The sex hormone testosterone has been shown to increase UA levels by enhancing renal reabsorption of UA,46 while estrogen reduces UA level by both decreasing its production and increasing its excretion.47 Thus, the UA levels are generally lower in females than in males. Individuals with low UA levels may have lost part of the antioxidant protection of UA. Epidemiological data from 17 countries showed a higher prevalence of SA in females.48 Additionally, a double-blind, randomized, clinical research for Acute Ischemic Stroke has confirmed UA treatment could enhance clinical outcomes in female stroke individuals.49 These data indicate that UA may be a unique and important clinical indicator of antioxidant stress in the female population.
Levels of UA in neuropsychiatric diseases may be of clinical importance. A series of studies have shown that UA may exhibit therapeutic value in the treatment of acute ischemic stroke.50 Moreover, serum UA levels on admission may be predictive of development of post-stroke depression.51 In addition, a meta-analysis revealed that individuals with bipolar disorder had increased UA levels, in particular during a manic episode.52 Allopurinol is a treatment for gout which reduces UA levels. Studies have demonstrated that allopurinol may be an adjuvant treatment for mania.53 However, more clinical research is needed to identify whether UA may represent a potential target for intervention in suicidal behavior. While increased levels of UA may improve the antioxidant capacity of the body, they may also increase the risk of other somatic diseases. Moreover, antioxidant therapies are not always strictly beneficial for human health. The functions of UA in vivo are diverse, depending on its cellular environment: intracellular, UA exerts pro-oxidant functions while it acts as an antioxidant in the extracellular milieu.54 If UA is used as a means of intervention for suicidal behavior, based on our results we recommend its use restricted to female individuals.
It is worth noting that this study also has certain limitations. Firstly, the proportion of male participants in our study was relatively small and we lacked data from a normal control population. Therefore, care is needed in interpreting for the findings of our study. Secondly, this was a retrospective study with some uncontrollable factors and there was selection bias caused by the small sample size. Thirdly, while we excluded the effects of lifestyle, diseases, and drug use on uric acid, we ignored other metabolic parameters, such as fasting blood glucose, high-density Lipoprotein (HDL), low-density Lipoprotein (LDL), cholesterol, triglycerides,55 which may influence the uric acid levels. Some of these metabolic parameters, in particular the cholesterol,56 may also influence suicide attempts. Fourthly, we did not assess other antioxidant markers; while UA represents a large part of the antioxidant system in the blood, other factors may also contribute.
Conclusion
Our study describes that serum UA levels are correlated with SA in adolescents and young adults with MDD. We found that the serum UA levels of SA group were significantly lower than that of non-SA group looking at the overall participants, and this difference was significant in female but not in male participants. Decreases in serum UA were associated with the increased suicide risk. This reveals a possible involvement of a dysfunctional antioxidant defense system in the pathophysiology of suicide. Based on our findings, UA may represent a potential biomarker for risk of suicide in female individuals with MDD. We propose that UA levels should be more frequently assessed in clinical psychiatry, and drugs reducing UA levels should be used with caution in individuals with MDD. However, further work is required to confirm our finding in larger-scale studies, including controlled longitudinal studies.
Acknowledgments
This research was supported by the National Natural Science Foundation of China (Grant NO. 81671360, 81971286, 81901373).
Disclosure
All authors declare no conflicts of interest.
References
- 1.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387(10024):1227–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Mental health: suicide prevention; 2014. Available from: http://www.who.int/mental_health/suicide-prevention/en. Accessed 5 November, 2014.
- 3.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA psychiatry. 2013;70(3):300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brezo J, Paris J, Barker ED, et al. Natural history of suicidal behaviors in a population-based sample of young adults. Psychol Med. 2007;37(11):1563–1574. [DOI] [PubMed] [Google Scholar]
- 5.Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet. 2002;360(9347):1728–1736. [DOI] [PubMed] [Google Scholar]
- 6.Dong M, Bin WS, Li Y, et al. Prevalence of suicidal behaviors in patients with major depressive disorder in China: a comprehensive meta-analysis. J Affect Disord. 2018;225:32–39. [DOI] [PubMed] [Google Scholar]
- 7.Suominen K, Isometsä E, Suokas J, Haukka J, Achte K, Lönnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161(3):562–563. [DOI] [PubMed] [Google Scholar]
- 8.Suokas J, Suominen K, Isometsaè E, Ostamo A, Loènnqvist J. Long-term risk factors for suicide mortality after attempted suicide–findings of a 14-year follow-up study. Acta Psychiatr Scand. 2001;104(2):117–121. [DOI] [PubMed] [Google Scholar]
- 9.Uğur K, Demirkol ME, Tamam L. The mediating roles of psychological pain and dream anxiety in the relationship between sleep disturbance and suicide. Arch Suicide Res. 2021;25(3):512–528. [DOI] [PubMed] [Google Scholar]
- 10.Demirkol ME, Uğur K, Tamam L. The mediating effects of psychache and dissociation in the relationship between childhood trauma and suicide attempts. Anadolu Psikiyatr Derg. 2020;21(5):453–460. [Google Scholar]
- 11.Sokolowski M, Wasserman J, Wasserman D. An overview of the neurobiology of suicidal behaviors as one meta-system. Mol Psychiatry. 2015;20(1):56–71. [DOI] [PubMed] [Google Scholar]
- 12.Lutz PE, Mechawar N, Turecki G. Neuropathology of suicide: recent findings and future directions. Mol Psychiatry. 2017;22(10):1395–1412. [DOI] [PubMed] [Google Scholar]
- 13.Vargas HO, Nunes SOV, De Castro MP, et al. Oxidative stress and lowered total antioxidant status are associated with a history of suicide attempts. J Affect Disord. 2013;150(3):923–930. [DOI] [PubMed] [Google Scholar]
- 14.Schiavone S, Neri M, Mhillaj E, et al. The NADPH oxidase NOX2 as a novel biomarker for suicidality: evidence from human post mortem brain samples. Transl Psychiatry. 2016;6(5):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Zhang J. Serum concentrations of antioxidant vitamins and carotenoids are low in individuals with a history of attempted suicide. Nutr Neurosci. 2007;10(1–2):51–58. [DOI] [PubMed] [Google Scholar]
- 16.Gutiérrez-Uzquiza Á, Arechederra M, Bragado P, Aguirre-Ghiso JA, Porras A. p38α mediates cell survival in response to oxidative stress via induction of antioxidant genes: effect on the p70S6K pathway. J Biol Chem. 2012;287(4):2632–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dreger H, Westphal K, Weller A, et al. Nrf2-dependent upregulation of antioxidative enzymes: a novel pathway for proteasome inhibitor-mediated cardioprotection. Cardiovasc Res. 2009;83(2):354–361. [DOI] [PubMed] [Google Scholar]
- 18.Ozcan ME, Gulec M, Ozerol E, Polat R, Akyol O. Antioxidant enzyme activities and oxidative stress in affective disorders. Int Clin Psychopharmacol. 2004;19(2):89–95. [DOI] [PubMed] [Google Scholar]
- 19.Yuan H, Yu C, Li X, et al. Serum uric acid levels and risk of metabolic syndrome: a dose-response meta-analysis of prospective studies. J Clin Endocrinol Metab. 2015;100(11):4198–207. [DOI] [PubMed] [Google Scholar]
- 20.Fang J, Alderman MH. Serum uric acid and cardiovascular mortality: the NHANES I Epidemiologic Follow-up Study, 1971-1992. J Am Med Assoc. 2000;283(18):2404–2410. [DOI] [PubMed] [Google Scholar]
- 21.Bowman GL, Shannon J, Frei B, Kaye JA, Quinn JF. Uric acid as a CNS antioxidant. J Alzheimers Dis. 2010;19(4):1331–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ames BN, Cathcart R, Schwiers E, Hochstein P. Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: a hypothesis. Proc Natl Acad Sci U S A. 1981;78(11):6858–6862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Du N, Xu D, Hou X, et al. Inverse association between serum uric acid levels and alzheimer’s disease risk. Mol Neurobiol. 2016;53(4):2594–2599. [DOI] [PubMed] [Google Scholar]
- 24.Pan M, Gao H, Long L, et al. Serum uric acid in patients with Parkinson’s disease and vascular parkinsonism: a cross-sectional study. Neuroimmunomodulation. 2013;20(1):19–28. [DOI] [PubMed] [Google Scholar]
- 25.Black CN, Bot M, Scheffer PG, Snieder H, Penninx BWJH. Uric acid in major depressive and anxiety disorders. J Affect Disord. 2018;225:684–690. doi: 10.1016/J.JAD.2017.09.003 [DOI] [PubMed] [Google Scholar]
- 26.Irizarry MC, Raman R, Schwarzschild MA, et al. Plasma urate and progression of mild cognitive impairment. Neurodegener Dis. 2009;6(1–2):23–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bartoli F, Crocamo C, Trotta G, et al. Testing the role of the antioxidant uric acid as a biomarker of suicidal ideation in subjects with major affective disorders: an exploratory study. Gen Hosp Psychiatry. 2018;51:128–129. [DOI] [PubMed] [Google Scholar]
- 28.Barbieri L, Verdoia M, Schaffer A, Marino P, Suryapranata H, De Luca G. Impact of sex on uric acid levels and its relationship with the extent of coronary artery disease: a single-centre study. Atherosclerosis. 2015;241(1):241–248. [DOI] [PubMed] [Google Scholar]
- 29.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang W, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–544. [DOI] [PubMed] [Google Scholar]
- 31.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 32.Peng R, Dai W, Li Y. Low serum free thyroxine level is correlated with lipid profile in depressive patients with suicide attempt. Psychiatry Res. 2018;266:111–115. [DOI] [PubMed] [Google Scholar]
- 33.Moulin-Mares SRA, Zaniqueli D, Oliosa PR, Alvim RO, Bottoni JP, Mill JG. Uric acid reference values: report on 1750 healthy Brazilian children and adolescents. Pediatr Res. 2021;89(7):1855–1860. [DOI] [PubMed] [Google Scholar]
- 34.Sies H. Oxidative stress: from basic research to clinical application. Am J Med. 1991;91:3C. [DOI] [PubMed] [Google Scholar]
- 35.Siwek M, Sowa-Kuaema M, Dudek D, et al. Oxidative stress markers in affective disorders. Pharmacol Rep. 2013;65(6):1558–1571. [DOI] [PubMed] [Google Scholar]
- 36.Maes M, Galecki P, Chang YS, Berk M. A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro)degenerative processes in that illness. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(3):676–692. [DOI] [PubMed] [Google Scholar]
- 37.Sorce S, Krause KH. NOX enzymes in the central nervous system: from signaling to disease. Antioxid Redox Signal. 2009;11(10):2481–2504. [DOI] [PubMed] [Google Scholar]
- 38.Radermacher KA, Wingler K, Langhauser F, et al. Neuroprotection after stroke by targeting NOX4 as a source of oxidative stress. Antioxid Redox Signal. 2013;18(12):1418–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matés JM. Effects of antioxidant enzymes in the molecular control of reactive oxygen species toxicology. Toxicology. 2000;153(1–3):83–104. [DOI] [PubMed] [Google Scholar]
- 40.Finkel T, Holbrook NJ. Oxidants, oxidative stress and the biology of ageing. Nature. 2000;408(6809):239–247. [DOI] [PubMed] [Google Scholar]
- 41.Gonçalves MCB, Corrêa-Velloso J, Naaldijk Y, Cheffer A, Ulrich H. Purinergic modulation of pathways associated to suicidal behavior. Mol Psychiatry. 2020;25(3):514–516. [DOI] [PubMed] [Google Scholar]
- 42.Bartoli F, Clerici M, Carrà G. Purinergic system and suicidal behavior: exploring the link between adenosine A2A receptors and depressive/impulsive features. Mol Psychiatry. 2020;25(3):512–513. [DOI] [PubMed] [Google Scholar]
- 43.Lucas M, O’reilly EJ, Pan A, et al. Coffee, caffeine, and risk of completed suicide: results from three prospective cohorts of American adults. World J Biol Psychiatry. 2014;15(5):377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaster MP, Machado NJ, Silva HB, et al. Caffeine acts through neuronal adenosine A2A receptors to prevent mood and memory dysfunction triggered by chronic stress. Proc Natl Acad Sci U S A. 2015;112(25):7833–7838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Elgün S, Keskinege A, Kumbasar H. Dipeptidyl peptidase IV and adenosine deaminase activity. Decrease in depression. Psychoneuroendocrinology. 1999;24(8):823–832. [DOI] [PubMed] [Google Scholar]
- 46.Li T, Walsh JR, Ghishan FK, Bai L. Molecular cloning and characterization of a human urate transporter (hURAT1) gene promoter. Biochim Biophys Acta. 2004;1681(1):53–58. [DOI] [PubMed] [Google Scholar]
- 47.Xiao-Tian C, Yun Z, Cheng-Yan D, et al. Estrogen and hyperuricemia. Chin J Allergy Clin Immunol. 2019;13(5):400–405. [Google Scholar]
- 48.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Llull L, Amaro S, Chamorro Á. Response to letter regarding article, ‘Uric Acid Therapy Improves Clinical Outcome in Women With Acute Ischemic Stroke’. Stroke. 2015;46(11):e242. [DOI] [PubMed] [Google Scholar]
- 50.Amaro S, Jiménez-Altayó F, Chamorro Á. Uric acid therapy for vasculoprotection in acute ischemic stroke. Brain Circ. 2019;5(2):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gu Y, Han B, Wang L, et al. Low serum levels of uric acid are associated with development of poststroke depression. Medicine. 2015;94(45):e1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bartoli F, Crocamo C, Mazza MG, Clerici M, Carrà G. Uric acid levels in subjects with bipolar disorder: a comparative meta-analysis. J Psychiatr Res. 2016;81:133–139. [DOI] [PubMed] [Google Scholar]
- 53.Bartoli F, Crocamo C, Clerici M, Carra G. Allopurinol as add-on treatment for mania symptoms in bipolar disorder: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry. 2017;210(1):10–15. [DOI] [PubMed] [Google Scholar]
- 54.So A, Thorens B. Uric acid transport and disease. J Clin Invest. 2010;120(6):1791–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bartoli F, Crocamo C, Gennaro GM, et al. Exploring the association between bipolar disorder and uric acid: a mediation analysis. J Psychosom Res. 2016;84:56–59. [DOI] [PubMed] [Google Scholar]
- 56.Bartoli F, Crocamo C, Dakanalis A, et al. Association between total serum cholesterol and suicide attempts in subjects with major depressive disorder: exploring the role of clinical and biochemical confounding factors. Clin Biochem. 2017;50(6):274–278. [DOI] [PubMed] [Google Scholar]