Abstract
Silicosis not a disease of the past. It is an irreversible, fibrotic lung disease specifically caused by exposure to respirable crystalline silica (RCS) dust. Over 20,000 incident cases of silicosis were identified in 2017 and millions of workers continue to be exposed to RCS. Identified case numbers are however a substantial underestimation due to deficiencies in reporting systems and occupational respiratory health surveillance programmes in many countries. Insecure workers, immigrants and workers in small businesses are at particular risk of more intense RCS exposure. Much of the focus of research and prevention activities has been on the mining sector. Hazardous RCS exposure however occurs in a wide range of occupational setting which receive less attention, in particular the construction industry. Recent outbreaks of silicosis associated with the fabrication of domestic kitchen benchtops from high‐silica content artificial stone have been particularly notable because of the young age of affected workers, short duration of RCS exposure and often rapid disease progression. Developments in nanotechnology and hydraulic fracking provide further examples of how rapid changes in technology and industrial processes require governments to maintain constant vigilance to identify and control potential sources of RCS exposure. Despite countries around the world dealing with similar issues related to RCS exposure, there is an absence of sustained global public health response including lack of consensus of an occupational exposure limit that would provide protection to workers. Although there are complex challenges, global elimination of silicosis must remain the goal.
Keywords: epidemiology, occupational medicine, prevention, public health, silicosis
Short abstract
See related Editorial
INTRODUCTION
Silicosis is an irreversible, fibrotic lung disease explicitly caused by the inhalation of respirable crystalline silicon dioxide (RCS). It continues to be among the most lethal of occupational diseases and is a major public health challenge internationally. Although the cause of silicosis is undisputed, millions of workers worldwide continue to be exposed to hazardous levels of RCS.
This review provides global and regional perspectives of the epidemiology of silicosis, sources of exposure and barriers that have hampered global elimination. Research and prevention strategies have historically focused on the mining sector. In recent years, there have been significant outbreaks of silicosis related to the use of high‐silica content artificial (engineered) stone material to produce domestic benchtops. 1 , 2 , 3 These outbreaks illustrate the potential for silicosis to rapidly emerge in new occupational settings. This narrative review also provides additional insights from countries that have experienced notable artificial stone silicosis outbreaks including Spain, Australia and Israel.
GLOBAL PICTURE
At the outset, the public health impact and complexities in preventing silicosis at a local and global level make it the most glocal of occupational diseases.
On one hand, the prevalence of silicosis all over the world makes it a global disease. In 2017, the Global Burden of Disease (GBD) study identified 23,695 incident cases of silicosis (age‐standardized incidence rate [ASIR] = 0.30 per 100,000), which represents 39% of the 60,055 incident cases of pneumoconiosis (Figure 1). 4 Silicosis' very name, coined in 1871, only reached medical consensus through the International Labour Organization (ILO) conference in Johannesburg (South Africa) in 1930, 5 which led to an ILO convention in 1934. In 1958, an ILO agreement defined the chest radiograph features of the disease, and in 1995 an ILO/World Health Organization (WHO) Global Programme for the Elimination of Silicosis was established and subsequently reaffirmed. 6 The implementation of global silicosis policies has however generally been disappointing and more limited than what had been envisaged. 7
FIGURE 1.
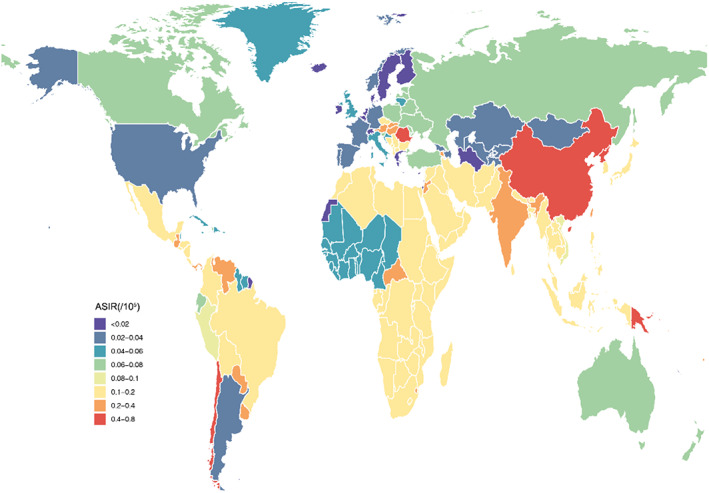
Age‐standardized incidence rates (ASIR) for silicosis in 2017 reported by the Global Burden of Disease Study. Source: Department of Occupational and Environmental Health, Tongji Medical College, Huazhong University of Science and Technology (reproduced with permission)
On the other hand, international law has shaped silicosis as a local disease. Its circular definition in the 1934 ILO convention defined it as a disease occurring in ‘industries or processes recognised by national law or regulations as involving exposure to the risk of silicosis’. By its explicit institutional legal definition, silicosis epitomizes the medicolegal character of ‘occupational disease’, which can vary across countries.
Second, by crystalline silica being the main mineral component in the earth crust, silicosis affects all sectors—not only the traditional industrial ones such as construction and building, but also ancient craftsmanship (stonecutting), modern technologies (dental prostheses), farming or fashionable productions (kitchen benchtop fabricated from artificial stone) and clothes (stone‐washed jeans). 4 The global ubiquity of silica has however never been translated into a universal public health issue. Only in specific contexts have local physicians been aware of the hazard linked to RCS exposure.
The mining industry, on which medical research, prevention and compensation through social welfare have historically focused, provides an obvious exception. However, even in this sector, the visibility of the disease has never been complete nor consistent. For instance, reluctant to acknowledge silicosis in the mining sector, the United Kingdom focused on ‘Coal Workers' Pneumoconiosis’ after World War 2, and the United States built legislation around ‘Black Lung’ in 1969. Currently, the situation is much worse in coal‐producing regions where public debate on pneumoconiosis is actively suppressed (e.g. China, Russia). In the 20th century, trade unions were a primary force advocating for recognition and prevention of silicosis while more recently new actors have emerged including non‐governmental organizations. The use of new information and communication technologies, which drive ‘popular epidemiology’, enables reporting of individual cases, particularly in China. This rapidly changing technology will continue to update and broaden the role that individual whistle‐blowers (including physicians, radiologists, unionists) will play in advocating for the prevention of silicosis, in very diverse national arenas such as political (e.g. parliamentary commissions), administrative (labour ministries, social insurance bureaucracies), judiciary and the media.
More than the national divide between countries, workers' status on the job market has always been key to determining their exposures. Skilled workers (including experienced miners), employed on a stable basis, are submitted to moderate but lifelong silica dust exposures. These workers tend to benefit—even imperfectly—from the implementation of national prevention and compensation schemes. However, workers with insecure jobs, often immigrants, working in small businesses in the ‘informal sector’, are often subjected to more intense exposures, as a result of limited regulatory protections.
The carcinogenic effect of silicon dioxide was recognized by the International Agency for Research on Cancer (IARC) in 1987, re‐evaluated and confirmed in 1997 and 2012. 8 Recently, there has been further interest in other health effects of silica exposure. The ‘sarcoid‐like’ and autoimmune pathologies which have been affecting 9/11 World Trade Center rescuers 9 , 10 , 11 , 12 , 13 , 14 and artificial stone workers 3 , 15 in particular have unexpectedly led to this overdue renewed focus. Furthermore, a recent meta‐analysis of eight studies of silicosis and tuberculosis (TB) yielded a pooled relative risk of 4.01 (95% CI: 2.88, 5.58), providing robust evidence for a strongly elevated risk of TB with radiological silicosis, with a low disease severity threshold. 16 This is the first systematic review of the epidemiological evidence for an association identified at least a century ago.
An occupational exposure limit (OEL) is that maximum airborne concentration of a toxic substance that a worker can be exposed to over a period of time (typically 8 h) without suffering any harmful consequences. The limit is determined from the available experimental studies, and toxicological and epidemiological data. Governments can adopt enforceable exposure limits as a tool aid for the protection of workers. Currently, there is no international agreement on a protective and enforceable RCS OEL. OELs for RCS vary significantly between countries, ranging between 0.025 mg/m3 and as high as 0.35 mg/m3 over an 8‐h work shift. 17 , 18 , 19 Most low‐ and middle‐income countries have no legislated exposure limit. A pooled analysis of 10 large silica‐exposed cohorts noted for a worker exposed from age 20 to 65 at an RCS level of 0.1 mg/m3, the excess lifetime risk (through age 75) of lung cancer was 1.1%–1.7%, above the background risk of 3%–6%. 20 A quantitative risk assessment of RCS exposure at a level of 0.05 mg/m3 over a 45‐year period of work indicated that 19 of every 1000 people are at risk of lung cancer mortality, 54 of lung disease other than cancer and 75 of radiographic silicosis. 21 Since 2009, the American Conference of Governmental Industrial Hygienists (ACIGH) has recommended an RCS OEL of 0.025 mg/m3. 19 There are sampling and analytical challenges at that low level; however, it is a protective level that few countries have yet to adopt.
ASIA
The epidemiology of silicosis in Asia is described by the GBS Study. 4 In 2017, the regional incidence of silicosis were East Asia 15,980, Southeast Asia 656, Central Asia 18 and South Asia 2823. Globally, the region of East Asia had the highest overall ASIR of 0.78 per 100,000. The regional incidents in Asia are all higher than those reported in 1990. 4 At a national level, the highest increase in average annual percentage change in ASIR was noted to be in Singapore, and globally the highest number of incident cases were in China (9066) and India (1464). 4
In Asia, there are a wide range of industries associated with exposure to RCS including quarrying, mining, mineral processing, foundry work, brick and tile making, refractory processes and construction (including work with stone, concrete, brick and some insulation boards). 17 A recent review of chest x‐rays of 529 workers in sandstone mines of Rajasthan, India, alarmingly noted 52% had features of silicosis including 7.5% with progressive massive fibrosis. 22 Twelve percent of those with silicosis also had TB.
Although prevention efforts have been taken for many decades, silicosis is still a public health issue in Asia. The rapid economic and industrial development and the large demand for coal energy and metal materials have resulted in more people to be exposed to RCS. From recent reports, more than 23 million workers in China and more than 10 million in India are exposed to RCS. Importantly, more cases of silicosis are emerging in new industries or new technological fields including jewellery and glass production, and use of nanomaterials. 23 , 24
Several strategies have been included in the ‘Healthy China 2030 Action Plan’ to address occupational health issues. The pneumoconiosis prevention and control plan requires that at least 95% of dust‐exposed workers undergo health surveillance. 25 Due to rapid technological changes, more focus is required in identifying and responding to new RCS exposure industries. Additional resources are also required for workers' health education, provision of respiratory protective equipment and increasing awareness of occupational health issues.
AFRICA
In the GBD estimates for Africa, silicosis comprised 32% of all pneumoconiosis, and new cases increased by 124% from 1990 to 2017. 4 While the global ASIR decreased by 0.4% per year, Western sub‐Saharan Africa (SSA) and North Africa showed an increase. The top five countries contributing new cases were Egypt, South Africa, Ethiopia, Democratic Republic of Congo (DRC) and Algeria. It is estimated that 5% of global pneumoconiosis deaths are from Africa, 20% being silicotics. 4 The global pneumoconiosis mortality rate was 0.7%, with the highest (1.3/100,000 persons) found in Southern SSA, which also had the third highest (28.9/100,000 persons) disability‐adjusted life year (DALY) rate.
For South Africa, the epicentre of gold mining in Southern SSA, the silicosis prevalence of 6% remains static, 26 , 27 although the incidence is declining, probably due to the contraction of the mining industry (Figure 2). 28 Earlier studies reported a similar prevalence in older in‐service miners (20%) and ex‐miners (25%), 29 although higher prevalence figures for silicosis (42.5%) and silico‐TB (25.7%) have been reported in Lesotho ex‐miners. 30 In Egypt, reported silicosis prevalence was between 18.5% and 45.8%, 31 while Zambian copper belt miners had lower levels of silicosis (5%–8.8%). 32 Copper and cobalt miners in the DRC are reported to have a 1.1% cumulative silicosis incidence over 25 years. 33 In artisanal and small‐scale gold Zimbabwean miners, 11.2% have silicosis and 4.0% TB. 34 A recent meta‐analysis demonstrated a three‐fold increased risk of TB among silicotics in this region. 16
FIGURE 2.

Rock drill operators in a gold mine. Source: Centre for Environmental and Occupational Health Research, University of Cape Town (reproduced with permission)
The primary source of exposure to silica occurs in formal mining of gold, although platinum, copper, cobalt and phosphate mining also contribute. 26 , 31 , 33 Artisanal gold mining in the informal sector is another source. 34 Non‐mining sectors include construction, manufacturing and agriculture, including well‐digging. 35 High exposures have also been reported in ceramics, foundries, refractories (and brick making) and construction work. 28
South Africa is the only African country with a national programme for silicosis elimination. Barriers to silicosis elimination in formal mining include under‐reporting of routinely collected data and silicosis underdiagnosis especially in ex‐miners. While silica levels are reported to be declining in South Africa, its accuracy remains unclear. 28 In non‐mining sectors, systematic baseline information on silica exposure and silicosis is deficient. 36 Although statutory exposure limits (0.05–0.10 mg/m3) exist, new cases persist due to poor control measures and inadequate enforcement. 28
Future strategies should focus on improved reporting and link with other data sources such as compensation claims. For non‐mining, better baseline exposure and silicosis incidence data are required. Linking of sentinel cases, especially for accelerated silicosis, to workplaces and surveys of long service workers in high‐risk jobs should be pursued. 28 Supportive actions for sustainable dust reduction should be accompanied with improved monitoring using improved RCS exposure standards. For artisanal and small‐scale miners, targeted programmes that include education, indigenous solutions and medical screening services are vital. 34 , 37
EUROPE
The GBD study presents an encouraging decreasing trend in silicosis incidence from 1990 to 2017 (ASIR: 0.33 vs. 0.20 in Central Europe, 0.09 vs. 0.07 in Eastern Europe, 0.12 vs. 0.04 in Western Europe). 4 Despite this decline, the heterogeneity of incidence patterns between countries and the existence of new sources of exposure to crystalline silica has raised concerns and led national health agencies to update medical and epidemiologic knowledge about the RCS risk over the last decade. 38 , 39 , 40
The global history of silicosis illustrates how European welfare systems have contributed to shaping a restricted image of the RCS health hazards. Approaches to silicosis in Western Europe have mainly focused on mining, making silicosis even more invisible elsewhere, despite well‐known hazards in other activities (e.g. foundries, denture production). 7 The disbanding of coal mining and other extractive activities, albeit with notable exceptions, may suggest the disappearance of RCS hazards in Europe. There is a high probability that silicosis is being overlooked given the absence of a comprehensive and sensitive health surveillance system to prevent and detect silicosis (and other possible diseases caused by RCS) in exposed sectors, particularly in construction. 41 , 42
Since the 2000s, the popularity of so‐called ‘artificial’ (engineered) stone has resulted in many workers developing silicosis in several European countries. 1 , 43 , 44 , 45 , 46 Workers diagnosed have tended to be young and healthy males, and the characteristics of artificial stone silicosis indicate that it often rapidly evolves into progressive massive fibrosis. 47 The emergence of artificial stone silicosis has highlighted challenges for occupational preventive measures, epidemiologic surveillance and welfare systems in which the under‐recognition of the occupational origin of chronic diseases is a long‐lasting public issue. 48 Currently, there is advocacy for a complete prohibition of high‐silica content materials. 49
Current guidelines by the French National Authority for Health in relation to health professional related RCS dust exposure may under‐emphasize the hazards of RCS. 50 First, it recommends chest radiography (despite its lower sensitivity to detect early lung lesions) rather than chest HRCT for surveillance of high‐risk groups. 50 , 51 Furthermore, it de‐emphasizes ‘other’ silica diseases by suggesting them as being too rare to constitute a public health priority. 52 In 2017, a Directive of the European Parliament classified ‘work involving exposure to RCS dust’ as carcinogenic, yet it has missed an important opportunity in revising exposure standards, by defining a permissible exposure value for RCS dust to be 0.1 mg/m3 (as an average over 8 h) in occupational settings. 53 This level is considered to be not protective for silicosis according to several studies. 38 , 54 Interestingly, this directive was issued 30 years after the IARC had established the carcinogenicity of crystalline silica for the first time. 8 The current context is characterized by pervasive industrial interests that advocate less constraining exposure standards and hamper compensation of diseased workers. 55 , 56
SOUTH AMERICA
In South America, mineral extraction, manufacturing and construction industries are important as they generate taxes and employment, and provide raw materials. However, when these activities are conducted without proper technology and control measures, they lead to degradation of the physical environment, and increase the risk to worker's health as a result of elevated levels of RCS.
In Brazil, about 500,000 workers are employed in mining, 2,300,000 in manufacturing and 3,800,000 in construction. According to Fundacentro (Jorge Duprat Figueiredo Foundation for Occupational Safety and Medicine), there are numerous occupational activities associated with increased risk of silicosis. These include foundry of iron, steel or other metals using sand moulds; extractive industries (mining, quarrying and processing of mineral‐bearing stones); rock drilling in construction (tunnels, dams and roads); and sandblasting (shipping and metallurgical industry). 57 Brazil is also one of the world's largest producers of gemstones. A 2017 study of workers in the Minas Gerais region identified 48.3% of semi‐precious stone craftsmen with silicosis and RCS exposure levels to be up to 29 times greater than the Brazilian 8‐h OEL of 0.1 mg/m3. 58
A study of silicosis‐associated mortality in Brazil between 1980 and 2017 indicated an increasing slope until 2006, with a decline thereafter. Mortality trends varied according to age groups, with a sharper decline observed in individuals aged 20–49 years from 2011 onwards while the decline in individuals aged 50–69 years occurred from 2005 onwards. However, individuals at 70 years or older displayed increasing mortality rates throughout the entire period. The decrease in deaths mostly occurred in municipalities that regulated economic activities. 57
Silicosis is the most common diffuse interstitial lung disease associated with occupational dust inhalation in Brazil and also the most important fibrogenic pneumoconiosis. Silicosis has a high prevalence especially in those over 60 years, followed by the age group between 40 and 59 years. It most commonly affects men (95.4%). 59 In this study, the risk factors for silicosis included inadequate ventilation in the underground galleries combined with dry drilling and duration of RCS exposure, while it was inversely associated with education.
In Latin America, especially in countries with significant mineral extraction, silicosis has become a serious public health problem. Silicosis represents 30.3% of newly diagnosed cases of all pneumoconiosis. 4
In Argentina, according to the database of Occupational Risk Superintendence (April 2015–March 2017) of 1502 cases of respiratory diseases, 34 workers were registered with silicosis, which represented 2.3% of the total. 60
In 2005, the Chilean Institute of Public Health found that the main industries with exposure to RCS were mining and construction, followed by manufacturing. It is estimated that 5.4% of formal and informal workers in Chile are likely to be exposed to RCS. 61
Working in enclosed and poorly ventilated spaces is particularly hazardous. The use of crushers and other processes that produce high dust levels increases the risk. In cities with mining and other RCS exposure activities, these occur at altitudes above 3000 m. In Peru, Bolivia, Chile and other countries in the region, it is important to consider altitude and its adverse clinical impact on exposed workers. In 2007, the number of miners in Peru who worked at altitudes above 2500 m represented 84.5% of the total miner population. In 2008, 26% (n = 840) of workers studied had silicosis. 62
In Brazil, the development of the National Program to eliminate silicosis began in 2002, but significant numbers of new cases continue to be reported through surveillance systems. Formal workers are covered by the Brazilian Social Security system, unlike informal workers. As a result of a legal decision by the Ministry of Labour and the Ministry of Health, workers exposed to particulate dust must undergo annual chest radiograph examination and spirometry every 2 years. The National Program for the Elimination of Silicosis aims to eliminate silicosis in Brazil by 2030.
NORTH AMERICA
Silicosis remains an important occupational lung disease in North America. There are data on exposures and cases in the United States and Canada, but little surveillance has been reported from Mexico. There are an estimated 2.3 million workers in the United States exposed to RCS, including 1.85 million construction workers and 320,000 general industry and maritime workers. 63 The reporting system for occupational injuries and illnesses in the United States fails to capture many cases, leading to a poor understanding of silicosis incidence and prevalence. 64 The only existing surveillance system for silicosis is based on data from two states, whose data demonstrate that manufacturing and construction are associated with the greatest number of silicosis cases. Estimates extrapolating data from these states using capture–recapture analysis determined that there were likely 3600–7300 cases of silicosis per year between 1987 and 1996 in the United States. 65 Using a broad case definition of silicosis, health insurance claims data derived from a population of adults aged 65 years or greater revealed a 16‐year prevalence of silicosis of 20.1–39.5 per 100,000 beneficiaries. 66 Mortality data revealed 2163 decedents with silicosis listed as the underlying or contributing cause of death between 1999 and 2014, 66 although it is likely that these data represent under‐reporting.
In Canada, there are no national data on the incidence or prevalence of silicosis. In the province of Alberta, 67 where silicosis is a notifiable disease, health insurance data revealed 861 cases with at least one reported diagnosis of ‘silicosis’ during a period of 10 years from 2000. These results were based on raw data and not a secondary review of primary imaging and clinical information. Data from 2000 through 2009 showed that only 29 workers' compensation claims were accepted for silicosis in Alberta. Data from Quebec's compensation system revealed 351 compensated cases of silicosis between 1988 and 1998. 68 Of note, workers who participated in regular surveillance had milder disease at the time of compensation.
The sources of exposure in North America do not vary greatly between countries. Excessive exposure to RCS has been well documented in the US construction industry with median exposures to RCS ranging from 0.75 to 3.2 mg/m3 among painters, laborers, bricklayers and operating engineers. The probability for overexposure to RCS in the industry was estimated to be 64.5%–100%. 69 Significant exposures are also found in general industry and maritime occupations. 70 In Alberta, industries with the highest potential for overexposure were sand and mineral processing; commercial building construction; aggregate mining and crushing; and abrasive blasting and demolition. 67
Hydraulic fracturing is prevalent in both the United States and Canada, but not in Mexico despite significant gas reserves in the Burgos Basin. 71 In an exposure monitoring study with full‐shift personal breathing zone samples collected from 11 hydraulic fracture sites in five US states, more than 50% of samples exceeded the permissible exposure limit (PEL), with some RCS concentrations 10–20 times higher than the PEL, mainly in jobs with close proximity to sand‐moving machinery. 72
In the United States, mining has long been associated with excessive exposures to RCS. More recently, there has been an increase in severe and rapidly progressive pneumoconiosis in Central Appalachian coal miners. 73 Rapidly progressive pneumoconiosis has been linked to silica exposure based on lung pathology showing features of accelerated silicosis along with classic silicotic nodules. Mining coal from thinner seams is associated with more rock cutting above and below the coal seam, likely leading to increased RCS exposure and more virulent disease. 74 , 75 , 76
The fabrication of artificial stone has been a source of many new cases of silicosis throughout the world, but only a handful of cases have been reported thus far in North America. The populations involved tend to be vulnerable and less likely to be engaged in compensation claims and surveillance. 77
Throughout North America, as in the rest of the world, the barriers to the elimination of silicosis have been the lack of enforcement of dust exposure limits coupled with inadequate medical surveillance and compensation programmes. The United States recently began a programme aimed at inspecting target industries to ensure compliance with regulatory standards. 78 This is intended to improve enforcement of updated silica standards, including a PEL of 0.05 mg/m3 time‐weighted average which went into effect in 2016–2018. Canada has an OEL for RCS of 0.025 mg/m3 2009; previously, the OEL was 0.1 mg/m3 for quartz and 0.05 mg/m3 for cristobalite.
AUSTRALASIA
The GBD study indicated the silicosis ASIR in Australia to be 0.06 in 2017, and 0.07 in New Zealand. 4 New Zealand was however noted to have second highest average annual percentage increase in ASIR between 1990 and 2017. 4 Although the number of workers diagnosed with silicosis had been relatively low for several decades in the Australasian region, since 2017, there has been an alarming increase in cases occurring in the stone benchtop industry. 39 , 79
Between the 1970s and mid‐2010s, industries most frequently associated with silicosis were foundries, brickworks/furnace construction, mining/quarries and excavation/tunnelling. 80 , 81 A 2003 review of 1467 compensated silicosis cases in the state of New South Wales (NSW) indicated a significant decline in incidence. 81 While 63% of the cases were compensated before the end of the 1960s, only 9% were compensated between 1979 and 2000. 81 Retrospective analysis of national mortality data between 1979 and 2002 noted that the crude mortality rates for silicosis showed a sustained decline, from 1.8 per million in 1982–1984 to 0.5 per million in 1997–1999. 80 An accurate understanding of the epidemiology of silicosis in Australia has however been limited, due to reliance on worker's compensation and mortality statistics. 82
Despite the small number of identified cases of silicosis, a cross‐sectional survey of the Australian working population in 2013 noted a significant prevalence of RCS exposure, with 6.6% deemed to be exposed, including 3.7% at a high level. 83 Miners and construction workers were most likely to be highly exposed when performing tasks with concrete and cement or working near crushers. 83 A study of construction industry workers in New Zealand noted 56% of samples exceeded 0.025 mg/m3. 84
In recent years, there has been a major increase in the number of workers diagnosed with silicosis. 3 , 85 , 86 , 87 In NSW, the annual number of certified silicosis cases increased from nine in 2015–2016 to 107 in 2019–2020. 88 This surge has primarily been related to the stone benchtop industry and handling of artificial stone. 39 Artificial stone was introduced to Australia in the early 2000s and has rapidly grown in popularity, to the point that it now accounts for almost half of the Australian benchtop market. 89 The stone benchtop industry in Australia is characterized by small and micro businesses, with 75% operating with five or fewer employees. 39 Processing of artificial stone without water dust suppression (dry cutting) has been noted to have been a widespread practice. 3 , 87
Following recognition of the initial cases of artificial stone silicosis, Australian governments have offered enhanced screening for workers. As of September 2021, 236 (22.4%) out of 1053 stonemasons assessed in Queensland were diagnosed with silicosis, including 32 with progressive massive fibrosis. 90 Similar results have been noted in Victoria with 108 workers confirmed to have silicosis during the first year of screening. 91 All Victorian workers diagnosed were male with a mean age of 42 years and 62% had been born in a country other than Australia. 3 Twenty‐six percent had worked in the stone benchtop industry for less than 10 years, consistent with the accelerated form of silicosis. 3
These enhanced assessments have demonstrated poor chest radiograph and spirometry sensitivity for screening silica‐exposed stone benchtop workers. In Victoria, initial results indicated 23 of 65 (35%) workers with simple silicosis had ‘normal’ chest radiographs (ILO category 0) but had consistent chest computed tomography features. 3 Interestingly, mean forced expiratory volume in 1 s and forced vital capacity percentage predicted values were noted to be over 80% for both simple and complicated silicosis. 3
Similar to international experience, follow‐up of patients with artificial stone silicosis has suggested rapid progression of disease and some have required lung transplantation. 85 , 87 , 92 These patients with progressive silicosis have highlighted inadequacies in treatments available for this disease. 93
As a response to the emergence of silicosis, an investigation by an Australian Government Taskforce noted that there has been inadequate dust control measures, ineffective health monitoring and insufficient enforcement of existing occupational health and safety laws applied to the stone benchtop industry. 39 The Taskforce recommended restriction of artificial stone fabrication to businesses licenced by government. The Taskforce also recommended a total importation ban on artificial stone products by July 2024 should there has been no measurable improvement in regulatory compliance or if preventive measures have been deemed inadequate to protect workers. 39
ISRAEL
Since the early 2010s, Israel has been one of the main countries which has experienced a dramatic outbreak of silicosis associated with the use of artificial stone material. The experience in Israel provides an example of a failure to identify and control a new source of RCS exposure and how that can rapidly lead to an outbreak of silicosis.
In Israel, kitchen and bathroom benchtops are mainly manufactured from artificial stone, with approximately 3500 workers currently involved in cutting and processing activities. In 2012, Kramer et al. first reported 25 workers with artificial stone‐associated silicosis. 2 These patients had a shared history of exposure to the same commercial brand of decorative, artificial stone and performed a similar work task of dry cutting the stone in the production of domestic benchtops. This 2012 report was a major warning due to the worldwide use of this material; however, to what extent this warning has been headed is unclear. 2
The Israeli Institute for Occupational Safety and Hygiene requires that the maximum exposure limit to silica dust is 0.1 mg/m3 for respirable dust (≤7 μm) and 0.3 mg/m3 for floating dust. Importantly, these standards refer to current exposure and ignore cumulative exposure. Investigation of induced sputum from 116 individuals exposed mainly to artificial stone dust from small workshops nationwide found that over one‐third (36.8%) of exposed workers had no previous diagnosis of silicosis, and 63.2% of these had confirmed silicosis. 94
In 2015, the US National Institute of Occupational Safety and Health (NIOSH) issued a Hazard Alert for the stone benchtop manufacturing and installation industry, which highlighted the need for monitoring RCS exposure levels and use of engineering controls such as water dust suppression, automated cutting tools and local exhaust ventilation. 95 In Israel, and elsewhere, in recent years, 96 computer numeric‐controlled stone cutting machinery, with some utilizing high‐pressure water for cutting, has become more commonly used to reduce aerosolized dust particles. The effectiveness of this process in reducing dust levels, however, remains untested.
Analysis of survival post lung transplantation for artificial stone silicosis in Israel has not been demonstrated to be reduced compared to similar patients undergoing transplantation for idiopathic pulmonary fibrosis. 97 Extremely high levels of silica content were noted in workers' explanted lungs. 97 , 98
CONCLUSION
Despite silicosis being one of the oldest described lung diseases, the occurrence of over 20,000 new cases per year indicates that the disease remains very present. The high incidence of silicosis in regions of Asia, Africa and South America is particularly concerning and the recent emergence of silicosis in the benchtop production industry has clearly demonstrated that even high‐income countries are not immune from this preventable occupational disease.
Progress towards elimination of silicosis seems to have stagnated over the last 20 years. Ongoing failures by governments, industries and employers to tackle the health risks of silica dust, with sufficient and sustained determination, have resulted in millions of workers continuing to be exposed to dusty conditions. Undoubtably, there have been and continue to be major obstacles to achieve elimination of silicosis. This is particularly the case in developing countries where there are other major health issues to be tackled, a situation that has been significantly exacerbated by the COVID‐19 pandemic. 99
The abundance of silicon dioxide in the earth's crust and its presence in an extremely wide range of industrial settings make silicosis a global health issue that requires a collaborative global response. Unquestionably, silicosis can be eliminated through the prevention of occupational dust exposure. Low levels of impetus to control occupational dust is contributed by there being a lack of immediate adverse health effect from exposure and perceived difficulty in the implementation of preventative practices, especially in small businesses. At the most fundamental level, there needs to be increased awareness and surveillance of the risks associated with silica dust exposures and more effective methods of control. To contribute towards global silicosis elimination strategies, there is an urgent need for countries worldwide to adopt more protective RCS OELs exposure standards, specifically of 0.025 mg/m3. However, any limit is only protective if it is enforced in all industrial sectors where RCS exposure may occur.
CONFLICT OF INTEREST
None declared.
The peer‐review of this invited review was handled by Philip Bardin (Editor‐in‐chief).
ACKNOWLEDGEMENTS
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Biographies
Dr. Ryan F. Hoy is a respiratory physician and senior research fellow at the Monash University Centre for Occupational and Environmental Health in Melbourne, Australia. He is the lead physician at the Occupational Respiratory Clinic at the Alfred Hospital, Melbourne. He holds a Master's degree in Occupational and Environmental Health. His research interests have included the areas of work‐related asthma, laryngeal dysfunction and artificial stone‐associated silicosis. He was a member of the National Dust Diseases Taskforce which published recommendations for the prevention, early identification, control and management of occupational dust diseases in Australia.
Professor Mohamed F. Jeebhay is an occupational medicine specialist and Head of Occupational Medicine in the School of Public Health & Family Medicine and the Department of Medicine at the University of Cape Town in South Africa. He is a fellow of the Collegium Ramazzini and serves on the editorial boards of Current Allergy & Clinical Immunology Journal and the African Journal of Thoracic & Critical Care Medicine. His major research focus is on the epidemiology of occupational lung diseases in Southern Africa with a focus on environmental risk factors and medical surveillance for the prevention of work‐related asthma and pneumoconiosis.
Catherine Cavalin is a permanent CNRS fellow researcher in sociology at IRISSO (Interdisciplinary Research Institute in the Social Sciences, Paris‐Dauphine University, PSL). She works on the diversity of health statuses and social health inequalities, which includes gender, labour and exposure to toxicants at work, as well as interpersonal violence. She particularly investigates the categories on which statistics are based, the nosological categories that frame medical knowledge, the borders between occupational and environmental health and associated public health policies. She was one of the contributors of the report published in 2019 by the French health agency (ANSES) on silica hazards.
Dr. Weihong Chen is chief and professor at Department of Occupational Health and Environmental Health in School of Public Health, University of Science & Technology in Wuhan, China. Major research interests include the epidemiology study on adverse health effects and preventive strategy of particulate matter including ambient PM2.5, industrial crystalline silica and coal mine dust; the pathogenic mechanism of ambient pollutants to cause cardiopulmonary diseases; and also the evaluation on protective effects of personal respiratory protection equipment.
Dr. Robert A. Cohen is Professor of Medicine at Northwestern University and is Clinical Professor of Environmental and Occupational Health Sciences at the University of Illinois Chicago, School of Public Health. His research interests include respiratory disease in mineral dust‐exposed workers. He has served as a consultant to the Respiratory Health Division of the US National Institute of Occupational Safety and Health and the Mine Safety and Health Administration. He has worked internationally in the area of medical surveillance for coal mine dust and silica‐exposed workers on projects in Ukraine, Colombia, Argentina and Australia.
Dr. Elizabeth Fireman is head of the Occupational/Environmental Lung Diseases Research Laboratory at the Tel Aviv Medical Center, Israel, and head of the Israeli National Laboratory Service for Interstitial Lung Diseases. She is Associate Professor of Occupational Environmental Health, Sackler School of Public Health, Tel Aviv University, Israel. She identified the first Israeli case of chronic beryllium disease (CBD) masked as sarcoidosis, followed by nationwide identification of all exposed workers with CBD misdiagnosed as having sarcoidosis. She is actively involved in research and laboratory workup of workers who sustained artificial stone‐induced silicosis from 2010 to the present.
Dr. Leonard H. T. Go is a research assistant professor at the University of Illinois Chicago (UIC) School of Public Health and a respiratory physician at Northwestern University Feinberg School of Medicine. He is the Project Director of the Black Lung Clinic programme at UIC, and his research interests centre on mineral dust‐related lung diseases.
Dr. Antonio León‐Jiménez is head of Pulmonology, Allergy and Thoracic Surgery Department at the Puerta del Mar University Hospital in Cádiz, Spain. He leads the artificial stone (AS) silicosis outpatient clinic and is a member of the research group of the Andalusian Comprehensive AS Silicosis Plan. His research has focused since 2016 on AS silicosis and he is the principal investigator of the clinical trial ‘Efficiency of Pirfenidone for the Reduction of Pulmonary Metabolic, Inflammatory and Fibrogenic Activity in Patients with Silicosis due to Artificial Stone and Progressive Massive Fibrosis’.
Professor Alfredo Menéndez‐Navarro is Professor of the History of Science at the University of Granada, Spain. His main research field is the history of occupational health and particularly focuses on the medical and social framing of occupational diseases in contemporary Spain. He investigates the emergence of medical and social concerns on asbestos‐related diseases and silica hazards, as well as the processes of under‐recognition of these risks. He is member and has served as Secretary of the ICOH Scientific Committee on the History of Prevention of Occupational and Environmental Diseases.
Dr. Marcos Ribeiro is an Associate Professor of the Pulmonology Department and is responsible for the Environmental and Occupational Health Sciences Section at Londrina State University Parana Brazil. His research interests include respiratory disease in mineral dust‐exposed workers.
Professor Paul‐André Rosental is a Professor in modern history at Sciences Po in Paris. He has directed an ERC Advanced Grant program at the crossroads between history, social sciences and medicine, devoted to the pathogenic effects of inorganic dusts. He has edited Silicosis. A World History, Johns Hopkins U.P. 2017, and co‐edited From Silicosis to Silica Hazards: An Experiment in Medicine, History, and the Social Sciences. American Journal of Industrial Medicine, 2015, https://onlinelibrary.wiley.com/toc/10970274/2015/58/S1. His last books include A Human Garden: French Policy and the Transatlantic Legacies of Eugenic Experimentation, NY, Berghahn Books (2020); and Population, the State, and National Grandeur. Demography as a political science in modern France, Peter Lang (2018).
Hoy RF, Jeebhay MF, Cavalin C, Chen W, Cohen RA, Fireman E, et al. Current global perspectives on silicosis—Convergence of old and newly emergent hazards. Respirology. 2022;27:387–398. 10.1111/resp.14242
Series Editor: Ryan Hoy
Handling Editor: Philip Bardin
See related Editorial
REFERENCES
- 1. Martinez C, Prieto A, Garcia L, Quero A, Gonzalez S, Casan P. Silicosis: a disease with an active present. Arch Bronconeumol. 2010;46:97–100. [DOI] [PubMed] [Google Scholar]
- 2. Kramer MR, Blanc PD, Fireman E, Amital A, Guber A, Rhahman NA, et al. Artificial stone silicosis [corrected]: disease resurgence among artificial stone workers. Chest. 2012;142:419–24. [DOI] [PubMed] [Google Scholar]
- 3. Hoy RF, Glass DC, Dimitriadis C, Hansen J, Hore‐Lacy F, Sim MR. Identification of early‐stage silicosis through health screening of stone benchtop industry workers in Victoria, Australia. Occup Environ Med. 2021;78:296–302. [DOI] [PubMed] [Google Scholar]
- 4. Shi P, Xing X, Xi S, Jing H, Yuan J, Fu Z, et al. Trends in global, regional and national incidence of pneumoconiosis caused by different aetiologies: an analysis from the Global Burden of Disease Study 2017. Occup Environ Med. 2020;77:407–14. [DOI] [PubMed] [Google Scholar]
- 5. Rosental P‐A, Rosner D, Blanc PD. From silicosis to silica hazards: an experiment in medicine, history, and the social sciences. Am J Ind Med. 2015;58(Suppl 1):S3–5. [DOI] [PubMed] [Google Scholar]
- 6. Fedotov I. The ILO/WHO global programme for the elimination of silicosis. Occup Health South Afr. 2006;12:4–7. [Google Scholar]
- 7. Rosental P‐A. Silicosis. A world history. Baltimore: Johns Hopkins University Press; 2017. [Google Scholar]
- 8. International Agency for Research on Cancer . Silica dust, crystalline, in the form of quartz or cristobalite. IARC Monogr. 2018;100C:355–405. [Google Scholar]
- 9. Perlman SE, Friedman S, Galea S, Nair HP, Eros‐Sarnyai M, Stellman SD, et al. Short‐term and medium‐term health effects of 9/11. Lancet. 2011;378:925–34. [DOI] [PubMed] [Google Scholar]
- 10. Crowley LE, Herbert R, Moline JM, Wallenstein S, Shukla G, Schechter C, et al. "Sarcoid like" granulomatous pulmonary disease in World Trade Center disaster responders. Am J Ind Med. 2011;54:175–84. [DOI] [PubMed] [Google Scholar]
- 11. Izbicki G, Chavko R, Banauch GI, Weiden MD, Berger KI, Aldrich TK, et al. World Trade Center "sarcoid‐like" granulomatous pulmonary disease in New York City Fire Department rescue workers. Chest. 2007;131:1414–23. [DOI] [PubMed] [Google Scholar]
- 12. Webber MP, Moir W, Crowson CS, Cohen HW, Zeig‐Owens R, Hall CB, et al. Post‐September 11, 2001, incidence of systemic autoimmune diseases in World Trade Center‐exposed firefighters and emergency medical service workers. Mayo Clin Proc. 2016;91:23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Azofeifa A, Martin GR, Howard J. World Trade Center Health Program, 2012‐2020: implications for clinicians and health care systems. JAMA. 2021;326:1147–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abbasi J. Twenty years after 9/11, responders are still healing. JAMA. 2021;326:995–8. [DOI] [PubMed] [Google Scholar]
- 15. Shtraichman O, Blanc PD, Ollech JE, Fridel L, Fuks L, Fireman E, et al. Outbreak of autoimmune disease in silicosis linked to artificial stone. Occup Med (Lond). 2015;65:444–50. [DOI] [PubMed] [Google Scholar]
- 16. Ehrlich R, Akugizibwe P, Siegfried N, Rees D. The association between silica exposure, silicosis and tuberculosis: a systematic review and meta‐analysis. BMC Public Health. 2021;21:953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Leung CC, Yu IT, Chen W. Silicosis. Lancet. 2012;379:2008–18. [DOI] [PubMed] [Google Scholar]
- 18. Centres for Disease Control and Prevention . Health effects of occupational exposure to respirable crystalline silica. NIOSH hazard review. Cincinnati: National Institute for Occupational Safety and Health; 2002.
- 19. American Conference of Government Industrial Hygienists Threshold limit values for chemical substances and physical agents and biological exposure indices. Cincinnati, OH: ACGIH; 2021.
- 20. Steenland K, Mannetje A, Boffetta P, Stayner L, Attfield M, Chen J, et al. Pooled exposure‐response analyses and risk assessment for lung cancer in 10 cohorts of silica‐exposed workers: an IARC multicentre study. Cancer Causes Control. 2001;12:773–84. [DOI] [PubMed] [Google Scholar]
- 21. Rice F, Park R & Stayner L Silica, lung cancer, and respiratory disease quantitative risk. Washington, D.C.: National Institute for Occupational Safety and Health; 2011.
- 22. Nandi SS, Dhatrak SV, Sarkar K. Silicosis, progressive massive fibrosis and silico‐tuberculosis among workers with occupational exposure to silica dusts in sandstone mines of Rajasthan state: an urgent need for initiating national silicosis control programme in India. J Family Med Prim Care. 2021;10:686–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ahmad I, Khan MI, Patil G, Chauhan LK. Evaluation of cytotoxic, genotoxic and inflammatory responses of micro‐ and nano‐particles of granite on human lung fibroblast cell IMR‐90. Toxicol Lett. 2012;208:300–7. [DOI] [PubMed] [Google Scholar]
- 24. Zhang R, Liu S, Zheng S. Characterization of nano‐to‐micron sized respirable coal dust: particle surface alteration and the health impact. J Hazard Mater. 2021;413:125447. [DOI] [PubMed] [Google Scholar]
- 25. The L. Improving occupational health in China. Lancet. 2019;394:443. [DOI] [PubMed] [Google Scholar]
- 26. Nelson G, Girdler‐Brown B, Ndlovu N, Murray J. Three decades of silicosis: disease trends at autopsy in South African gold miners. Environ Health Perspect. 2010;118:421–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Knight D, Ehrlich R, Fielding K, Jeffery H, Grant A, Churchyard G. Trends in silicosis prevalence and the healthy worker effect among gold miners in South Africa: a prevalence study with follow up of employment status. BMC Public Health. 2015;15:1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brouwer DH, Rees D. Can the South African milestones for reducing exposure to respirable crystalline silica and silicosis be achieved and reliably monitored? Front Public Health. 2020;8:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Churchyard GJ, Ehrlich R, teWaterNaude JM, Pemba L, Dekker K, Vermeijs M, et al. Silicosis prevalence and exposure‐response relations in South African goldminers. Occup Environ Med. 2004;61:811–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maboso BM, Moyo DM, Muteba KM, Govender VG, Barnes DF, Maama‐Maime LBM, et al. Occupational lung disease among Basotho ex‐miners in a large outreach medical assessment programme. Occup Health South Afr. 2020;18:145–52. [Google Scholar]
- 31. Kalliny MS, Bassyouni MI. Immune response due to silica exposure in Egyptian phosphate mines. J Health Care Poor Underserved. 2011;22:91–109. [DOI] [PubMed] [Google Scholar]
- 32. Mwaanga P, Silondwa M, Kasali G, Banda PM. Preliminary review of mine air pollution in Zambia. Heliyon. 2019;5:e02485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kabamba Ngombe L, Nlandu Ngatu R, Nyembo Mukena C, Kabyla Ilunga B, Wembonyama Okitotsho S, Kakoma Sakatolo JB, et al. Silicosis in underground miners in Lubumbashi, Democratic Republic of the Congo: 27 cases. Med Sante Trop. 2018;28:395–8. [DOI] [PubMed] [Google Scholar]
- 34. Moyo D, Zishiri C, Ncube R, Madziva G, Sandy C, Mhene R, et al. Tuberculosis and silicosis burden in artisanal and small‐scale gold miners in a large occupational health outreach programme in Zimbabwe. Int J Environ Res Public Health. 2021;18:11031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Elidrissi AM, Zaghba N, Benjelloun H, Yassine N. Well‐digger's lung. Pan Afr Med J. 2016;25:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Khoza NN, Grové T, Schutte PC. Worker exposure to silica dust in South African non‐mining industries in Gauteng: an exploratory study. Occup Health South Afr. 2012;18:18–26. [Google Scholar]
- 37. Tsang VWL, Lockhart K, Spiegel SJ, Yassi A. Occupational health programs for artisanal and small‐scale gold mining: a systematic review for the WHO Global Plan of Action for Workers' Health. Ann Glob Health. 2019;85:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Occupational Safety and Health Administration editor. Workers' exposure to respirable crystalline silica: final rule overview. More than 2 million workers gain protections from deadly dust. Washington, D.C.: OSHA Fact Sheet; 2016. p. 1–2.
- 39. Australian Government . National Dust Disease Taskforce. Final Report. Canberra, ACT: Australian Government; 2021.
- 40. Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement et du travail . Dangers, expositions et risques relatifs à la silice cristalline. Maisons‐Alfort: ANSES; 2019.
- 41. Boudigaard SH, Schlünssen V, Vestergaard JM, Søndergaard K, Torén K, Peters S, et al. Occupational exposure to respirable crystalline silica and risk of autoimmune rheumatic diseases: a nationwide cohort study. Int J Epidemiol. 2021;50:1213–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Blanc PD, Järvholm B, Torén K. Prospective risk of rheumatologic disease associated with occupational exposure in a cohort of male construction workers. Am J Med. 2015;128:1094–101. [DOI] [PubMed] [Google Scholar]
- 43. Martinez Gonzalez C, Prieto Gonzalez A, Garcia Alfonso L, Fernandez Fernandez L, Moreda Bernardo A, Fernandez Alvarez R, et al. Silicosis in artificial quartz conglomerate workers. Arch Bronconeumol. 2019;55:459–64. [DOI] [PubMed] [Google Scholar]
- 44. Perez‐Alonso A, Cordoba‐Dona JA, Millares‐Lorenzo JL, Figueroa‐Murillo E, Garcia‐Vadillo C, Romero‐Morillos J. Outbreak of silicosis in Spanish quartz conglomerate workers. Int J Occup Environ Health. 2014;20:26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Paolucci V, Romeo R, Sisinni AG, Bartoli D, Mazzei MA, Sartorelli P. Silicosis in workers exposed to artificial quartz conglomerates: does it differ from chronic simple silicosis? Arch Bronconeumol. 2015;51:e57–60. [DOI] [PubMed] [Google Scholar]
- 46. Menéndez‐Navarro A, Cavalin C, García‐Gómez M, Gherasim A. The re‐emergence of silicosis as an occupational disease in Spain, 1990‐2019. Rev Esp Salud Publica. 2021;95:e202108106. [PubMed] [Google Scholar]
- 47. León‐Jiménez A, Hidalgo‐Molina A, Conde‐Sánchez M, Pérez‐Alonso A, Morales‐Morales JM, García‐Gámez EM, et al. Artificial stone silicosis: rapid progression following exposure cessation. Chest. 2020;158:1060–8. [DOI] [PubMed] [Google Scholar]
- 48. Cavalin C, Henry E, Jouzel J‐N. One hundred years of under‐recognition of occupational diseases. Paris: Presses des Mines; 2020. [Google Scholar]
- 49. Cohen RA, Go LHT. Artificial stone silicosis: removal from exposure is not enough. Chest. 2020;158:862–3. [DOI] [PubMed] [Google Scholar]
- 50. Haute Autorité de santé. Recommandations de bonne pratique. Surveillance médico‐professionnelle des travailleurs exposés ou ayant été exposés à la silice cristalline. Paris: Haute Autorité de santé; 2021.
- 51. Perret JL, Miles S, Brims F, Newbigin K, Davidson M, Jersmann H, et al. Respiratory surveillance for coal mine dust and artificial stone exposed workers in Australia and New Zealand: a position statement from the Thoracic Society of Australia and New Zealand. Respirology. 2020;25:1193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lescoat A, Cavalin C, Ehrlich R, Cazalets C, Ballerie A, Belhomme N, et al. The nosology of systemic sclerosis: how lessons from the past offer new challenges in reframing an idiopathic rheumatological disorder. Lancet Rheumatol. 2019;1:e257–e64. [DOI] [PubMed] [Google Scholar]
- 53. The European Parliament and of the Council . Directive (EU) 2017/2398 of the European Parliament and of the Council: amending Directive 2004/37/EC on the protection of workers from the risks related to exposure to carcinogens or mutagens at work. Luxembourg: Official Journal of the European Union; 2017.
- 54. Occupational Safety and Health Administration . Occupational exposure to respirable crystalline silica – review of health effects literature and preliminary quantitative risk assessment. Washington, D.C.: Occupational Safety and Health Administration; 2013.
- 55. Musu T. Revision of the carcinogens directive: anything happening? HesaMag. 2013;8:21–4. [Google Scholar]
- 56. Vogel L. Is health and safety policy being hijacked in the drive for competitiveness? Social developments in the European Union 2006. Brussels: European Trade Union Institute; 2007.
- 57. Algranti E, Saito CA, Carneiro APS, Bussacos MA. Mortality from silicosis in Brazil: temporal trends in the period 1980‐2017. Am J Ind Med. 2021;64:178–84. [DOI] [PubMed] [Google Scholar]
- 58. Carneiro AP, Braz NF, Algranti E, Bezerra OM, Araujo NP, Amaral Eng Hyg LS, et al. Silica exposure and disease in semi‐precious stone craftsmen, Minas Gerais, Brazil. Am J Ind Med. 2017;60:239–47. [DOI] [PubMed] [Google Scholar]
- 59. Souza TP, Watte G, Gusso AM, Souza R, Moreira JDS, Knorst MM. Silicosis prevalence and risk factors in semi‐precious stone mining in Brazil. Am J Ind Med. 2017;60:529–36. [DOI] [PubMed] [Google Scholar]
- 60. Beaucham CC, Lentz TJ, Rice FL. Expanding control banding for workplace silica exposures throughout the Americas. Int J Occup Environ Health. 2012;18:344–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Vergara A. The recognition of silicosis: labor unions and physicians in the Chilean copper industry, 1930s‐1960s. Bull Hist Med. 2005;79:723–48. [DOI] [PubMed] [Google Scholar]
- 62. Donroe JA, Maurtua‐Neumann PJ, Gilman RH, Acosta AT, Cain G, Parker JE, et al. Surveillance for early silicosis in high altitude miners using pulse oximetry. Int J Occup Environ Health. 2008;14:187–92. [DOI] [PubMed] [Google Scholar]
- 63. Occupational Safety and Health Administration . Silica, crystalline – overview. [cited 2021 Dec 1]. Available from: https://www.osha.gov/silica-crystalline
- 64. Rosenman KD, Kalush A, Reilly MJ, Gardiner JC, Reeves M, Luo Z. How much work‐related injury and illness is missed by the current national surveillance system? J Occup Environ Med. 2006;48:357–65. [DOI] [PubMed] [Google Scholar]
- 65. Rosenman KD, Reilly MJ, Henneberger PK. Estimating the total number of newly‐recognized silicosis cases in the United States. Am J Ind Med. 2003;44:141–7. [DOI] [PubMed] [Google Scholar]
- 66. Casey ML, Mazurek JM. Silicosis prevalence and incidence among Medicare beneficiaries. Am J Ind Med. 2019;62:183–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lappi VG, Radnoff DL, Karpluk PF. Silica exposure and silicosis in Alberta, Canada. J Occup Environ Med. 2014;56(Suppl 10):S35–9. [DOI] [PubMed] [Google Scholar]
- 68. Infante‐Rivard C. Severity of silicosis at compensation between medically screened and unscreened workers. J Occup Environ Med. 2005;47:265–71. [DOI] [PubMed] [Google Scholar]
- 69. Rappaport SM, Goldberg M, Susi P, Herrick RF. Excessive exposure to silica in the US construction industry. Ann Occup Hyg. 2003;47:111–22. [DOI] [PubMed] [Google Scholar]
- 70. Occupational Safety and Health Administration . Small entity compliance guide for the respirable crystalline silica standard for general industry and maritime. Washington, D.C.: Occupational Safety and Health; 2017.
- 71. Pskowski M. Mexico's Fracking Impasse. 2020. [cited by 2021 Nov 25]. Available from: https://nacla.org/news/2020/10/22/mexico-fracking-impasse
- 72. Esswein EJ, Breitenstein M, Snawder J, Kiefer M, Sieber WK. Occupational exposures to respirable crystalline silica during hydraulic fracturing. J Occup Environ Hyg. 2013;10:347–56. [DOI] [PubMed] [Google Scholar]
- 73. Antao VC, Petsonk EL, Sokolow LZ, Wolfe AL, Pinheiro GA, Hale JM, et al. Rapidly progressive coal workers' pneumoconiosis in the United States: geographic clustering and other factors. Occup Environ Med. 2005;62:670–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Laney AS, Blackley DJ, Halldin CN. Radiographic disease progression in contemporary US coal miners with progressive massive fibrosis. Occup Environ Med. 2017;74:517–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Almberg KS, Halldin CN, Blackley DJ, Laney AS, Storey E, Rose CS, et al. Progressive massive fibrosis resurgence identified in U.S. coal miners filing for black lung benefits, 1970–2016. Ann Am Thorac Soc. 2018;15:1420–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Blackley DJ, Reynolds LE, Short C, Carson R, Storey E, Halldin CN, et al. Progressive massive fibrosis in coal miners from 3 clinics in Virginia. JAMA. 2018;319:500–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Rose C, Heinzerling A, Patel K, Sack C, Wolff J, Zell‐Baran L, et al. Severe silicosis in engineered stone fabrication workers – California, Colorado, Texas, and Washington, 2017‐2019. MMWR Morb Mortal Wkly Rep. 2019;68:813–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Occupational Safety and Health Administration . U.S. Department of Labor revises National Emphasis Program to reduce or eliminate worker exposure to silica. Washington, D.C.: Occupational Safety and Health; 2020.
- 79. Australian Safety and Compensation Council . Occupational respiratory diseases in Australia. Canberra: Australian Government; 2006.
- 80. Smith DR, Leggat PA. 24 years of pneumoconiosis mortality surveillance in Australia. J Occup Health. 2006;48:309–13. [DOI] [PubMed] [Google Scholar]
- 81. Berry G, Rogers A, Yeung P. Silicosis and lung cancer: a mortality study of compensated men with silicosis in New South Wales, Australia. Occup Med (Lond). 2004;54:387–94. [DOI] [PubMed] [Google Scholar]
- 82. Alif SM, Glass DC, Abramson M, Hoy RF, Sim MR. Occupational lung diseases in Australia 2006–2019. Melbourne, Victoria: Monash University; 2020. p. 1–86.
- 83. Si S, Carey RN, Reid A, Driscoll T, Glass DC, Peters S, et al. The Australian work exposures study: prevalence of occupational exposure to respirable crystalline silica. Ann Occup Hyg. 2016;60:631–7. [DOI] [PubMed] [Google Scholar]
- 84. McLean D, Glass B, 't Mannetje A, Douwes J. Exposure to respirable crystalline silica in the construction industry‐do we have a problem? N Z Med J. 2017;130:78–82. [PubMed] [Google Scholar]
- 85. Matar E, Frankel A, Blake LKM, Silverstone EJ, Johnson AR, Yates DH. Complicated silicosis resulting from occupational exposure to engineered stone products. Med J Aust. 2017;206:385–6. [DOI] [PubMed] [Google Scholar]
- 86. Frankel A, Blake L, Yates D. LATE‐BREAKING ABSTRACT: complicated silicosis in an Australian worker from cutting engineered stone countertops: an embarrassing first for Australia. Eur Respir J. 2015;46:PA1144. [Google Scholar]
- 87. Hoy RF, Baird T, Hammerschlag G, Hart D, Johnson AR, King P, et al. Artificial stone‐associated silicosis: a rapidly emerging occupational lung disease. Occup Environ Med. 2018;75:3–5. [DOI] [PubMed] [Google Scholar]
- 88. Insurance and Care NSW . Annual Report 2019–20. NSW Government; 2020.
- 89. Caesarstone® Investor Presentation Caesarstone. Sdot Yam, Israel; 2020.
- 90. Workplace Health and Safety Queensland . Silicosis – WorkCover screening outcomes [cited 2021 Nov 1]. Available from:https://www.worksafe.qld.gov.au/claims-and-insurance/work-related-injuries/types-of-injury-or-illness/work-related-respiratory-diseases/silicosis
- 91. Monash Centre for Occupational and Environmental Health. Silica associated lung disease health screening research project: phase 1. Melbourne, Victoria: Monash University; 2020.
- 92. Levin K, McLean C, Hoy R. Artificial stone‐associated silicosis: clinical‐pathological‐radiological correlates of disease. Respirol Case Rep. 2019;7:e00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Hoy R, Chambers DC. Silicosis: an ancient disease in need of a dose of modern medicine. Respirology. 2020;25:464–5. [DOI] [PubMed] [Google Scholar]
- 94. Ophir N, Shai AB, Alkalay Y, Israeli S, Korenstein R, Kramer MR, et al. Artificial stone dust‐induced functional and inflammatory abnormalities in exposed workers monitored quantitatively by biometrics. ERJ Open Res. 2016;2:00086‐2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Occupational Safety and Health Administration . OSHA/NIOSH Hazard Alert: worker exposure to silica during countertop manufacturing, finishing and installation. 2015 [cited 2021 Nov 20]. Available from: https://www.cdc.gov/niosh/docs/2015-106/default.html
- 96. Glass DC, Dimitriadis C, Hansen J, Hoy RF, Hore‐Lacy F, Sim MR. Silica exposure estimates in artificial stone benchtop fabrication and adverse respiratory outcomes. Ann Work Expo Health. 2021;66:5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Rosengarten D, Fox BD, Fireman E, Blanc PD, Rusanov V, Fruchter O, et al. Survival following lung transplantation for artificial stone silicosis relative to idiopathic pulmonary fibrosis. Am J Ind Med. 2017;60:248–54. [DOI] [PubMed] [Google Scholar]
- 98. Fireman E, Mahamed AE, Rosengarten D, Ophir NN, Kramer MR. Quantitation of silica contents in lung explants of transplanted patients: artificial stone‐induced silicosis vs. idiopathic pulmonary fibrosis. Int J Environ Res Public Health. 2021;18:7237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Naidoo RN, Jeebhay MF. COVID‐19: a new burden of respiratory disease among South African miners? Curr Opin Pulm Med. 2021;27:79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]


