As of December 2021, although half of the global population had already been fully vaccinated,1 a new variant gave new contours to the pandemic. Preliminary data suggest that the Omicron variant is far more infectious than the previous ones but is associated with reduced risk of severity. Recently, Cochran et al2 reported a 2% lethality rate among transplant recipients from a single US center during the Omicron wave, which was much attenuated compared with their historical rate of 19.6%. It is unknown whether this information is consistent in other regions of the globe.
Here, we report the behavior of coronavirus disease 2019 (COVID-19) in 10 497 kidney transplant recipients, followed-up in our transplant center, compared with the city of Ipaussu in the state of São Paulo with 14 506 inhabitants. This municipality was selected as a comparator group based on equivalent surveillance, diagnostic and monitoring strategies, accurate electronic database,3 similar sample size, and high vaccination coverage. We compared the number of COVID-19 diagnoses and deaths among kidney transplant recipients versus the general population of Ipaussu, before (era 1: March 20, 2020–December 16, 2021) and after (era 2: December 17, 2021–March 25, 2022) the predominance of the Omicron variant in Brazil.4
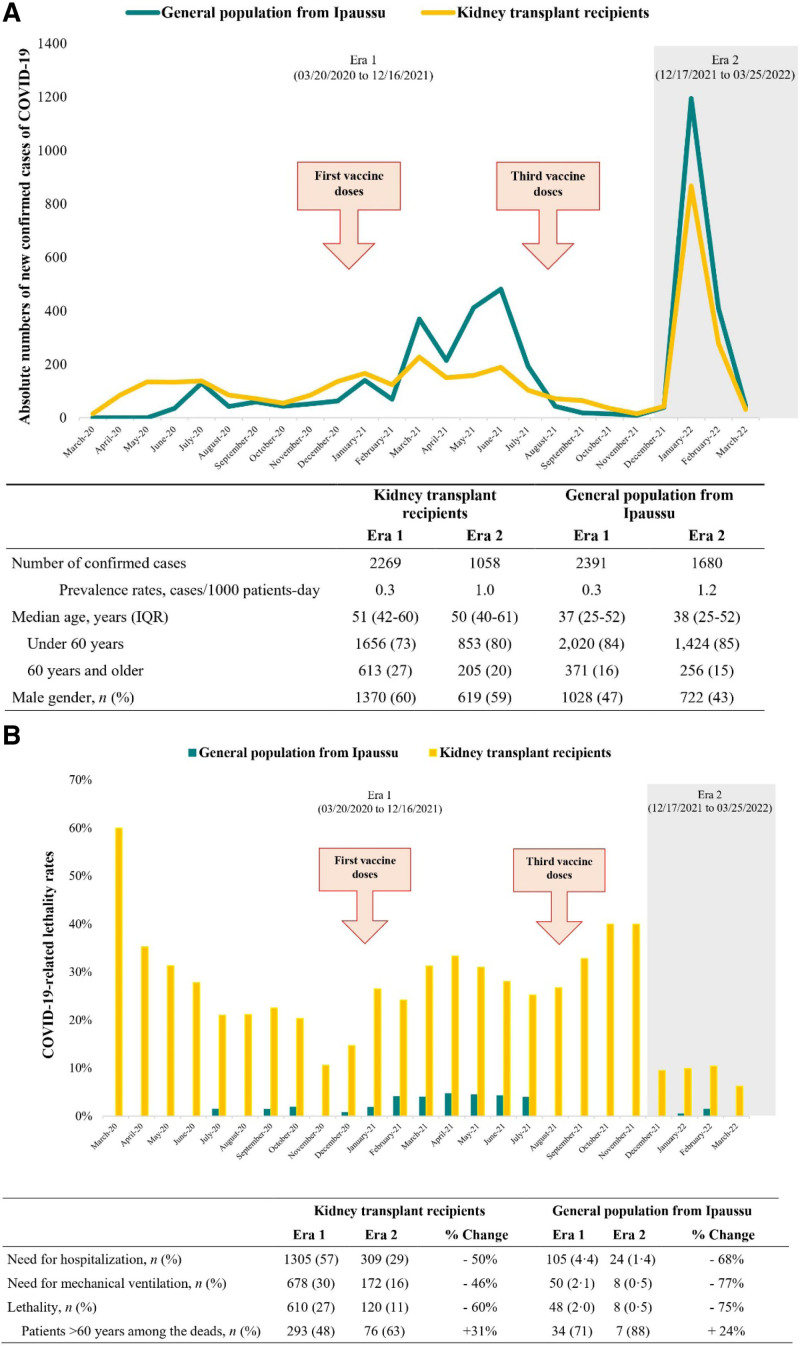
The pandemic showed similar dynamics in the 2 populations, with 3327 confirmed cases of COVID-19 among kidney transplant recipients and 4071 in Ipaussu. The absolute number of cases was >3 times higher during era 2 versus era 1, with no detectable changes in the demography of the affected patients (Figure 1A).
FIGURE 1.
Behaviour of COVID-19 across the two populations over the months of the pandemic. A, Absolute numbers of new cases of COVID-19, prevalence rates, and major demographic characteristics. B, COVID-19–related lethality rates in kidney transplant recipients (orange lines/columns) and in the comparator group of the general population of Ipaussu (dark green lines/columns). The study period was arbitrarily split into era 1, “pre-Omicron,” and era 2, “post-Omicron.” According to the National Immunization Program, the first dose of vaccines that were anti–SARS-CoV-2 were made available since January 2021 and the third dose of vaccine from August 2021. COVID-19, coronavirus disease 2019; IQR, interquartile range; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
In era 1, the clinical efficacy of the vaccines could be clearly noticed in Ipaussu, where no deaths were recorded between August and November 2021. This was not evident among transplant patients, perhaps because of their poor response to vaccines5 (Figure 1B).
Era 2 was associated with a 50%–70% reduction in the need for hospitalization, mechanical ventilation, and deaths in both groups. There was also no change in key demographic characteristics associated with poor prognosis, with 63% of deaths among transplant recipients and 88% among the general population occurring in persons >60 y (Figure 1B).
These equivalent results in both populations support the initial hypothesis of immune evasion (higher infection rate) and reduced pathogenicity (lower fatality rate) of Omicron compared with previous variants. Yet, lethality among kidney transplant recipients remains prohibitive, because 1 in 10 still die from COVID-19. Compared with the general population, this residual risk may result from the intermingling of variant immune escape with the lower vaccine response and the accumulation of comorbidities inherent to the transplant patient. Until more effective pharmacological strategies are developed, it is crucial to maintain the highly effective nonpharmacological preventive measures in this high-risk population, such as the immunosuppressed patients.
REFERENCES
- 1.Mathieu E, Ritchie H, Ortiz-Ospina E, et al. A global database of COVID-19 vaccinations. Nat Hum Behav. 2021;5:947–953. [DOI] [PubMed] [Google Scholar]
- 2.Cochran W, Shah P, Barker L, et al. COVID-19 clinical outcomes in solid organ transplant recipients during the Omicron surge. Transplantation. 2022;106:e346–e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rissoni RAP, Foresto RD, Oliveira FR, et al. Abordagem da pandemia por COVID-19 na cidade de Ipaussu com 14 mil habitantes no interior do Estado de São Paulo. An Acad Bras Cienc. 2020;19:84–92. [Google Scholar]
- 4.Fundação Oswaldo Cruz, Ministério da Saúde do Brasil. Rede Genomica Fiocruz. Available at http://www.genomahcov.fiocruz.br. Accessed March 29, 2022.
- 5.Carr EJ, Kronbichler A, Graham-Brown M, et al. Review of early immune response to SARS-CoV-2 vaccination among patients with CKD. Kidney Int Rep. 2021;6:2292–2304. [DOI] [PMC free article] [PubMed] [Google Scholar]