Abstract
In the time of the COVID-19 pandemic, where clinical environments are plagued by both uncertainty and complexity, the importance of the informal and social aspects of learning among health care teams cannot be exaggerated. While there have been attempts to better understand the nuances of informal learning in the clinical environment through descriptions of the tacit or hidden curriculum, incidental learning in medical education has only been partially captured in the research. Understood through concepts borrowed from the Cynefin conceptual framework for sensemaking, the early stages of the pandemic immersed clinical teams in complex and chaotic situations where there was no immediately apparent relationship between cause and effect. Health care teams had to act quickly amidst the chaos: they had to first act, make sense of, and respond with intentionality. Informal and incidental learning (IIL) emerged as a byproduct of acting with the tools and knowledge available in the moment. To integrate the informal, sometimes haphazard nature of emergence among health care teams, educators require an understanding of IIL. This understanding can help medical educators prepare health professions learners for the cognitive dissonance that accompanies uncertainty in clinical practice. The authors introduce IIL as an explanatory framework to describe how teams navigate complexity in the clinical learning environment and to better inform curricular development for health professions training that prepares learners for uncertainty. While further research in IIL is needed to illuminate tacit knowledge that makes learning explicit for all audiences in the health professions, there are opportunities to cultivate learners’ skills in formal curricula through various learning interventions to prime them for IIL when they enter complex clinical learning environments.
The clinical learning environment (CLE) is a complex system consisting of interacting and intertwined components—personal, social, organizational, physical, and virtual—that magnify uncertainty in everyday clinical practice. 1,2 The dynamic nature of clinical teams, multiple learners in the workplace, pressing sociocultural influences, and the built environment further add to this complexity. 3 Clinical environments embody the characteristics of complex systems, 4 including large numbers of elements interacting in nonlinear ways. Elements adapt to one another, but they also constrain adaptation; in many instances, it is virtually impossible for a team to predict the results of its actions.
The COVID-19 pandemic has only amplified the impact of this complexity on clinical practice. Given the dynamic nature of the CLE, solutions cannot be imposed; rather, teams work together to develop their own solutions, taking into account context and systems’ historical “propensities” or “tendencies to act in a particular way.” 5 Emergence, when it occurs, can lead to modifications and new solutions 4 when “small-scale, simple interactions among the diverse individual parts lead to more complex behavioral changes to the social systems themselves.” 5 Movement starts with “low-level rules” and moves to “higher-level sophistication”—essentially, a shift from a top-down to a bottom-up means of problem solving, where smaller-scale actions create contexts for larger interventions to take place. 5 Clinical environments do not exist in a vacuum; instead, the lived experiences of patients, practitioners, and teams dynamically change throughout care along with the changing compositions of clinical teams, to emerge in a complex health system.
Focus on Sensemaking: Lessons from COVID-19 Using a Complexity Framework
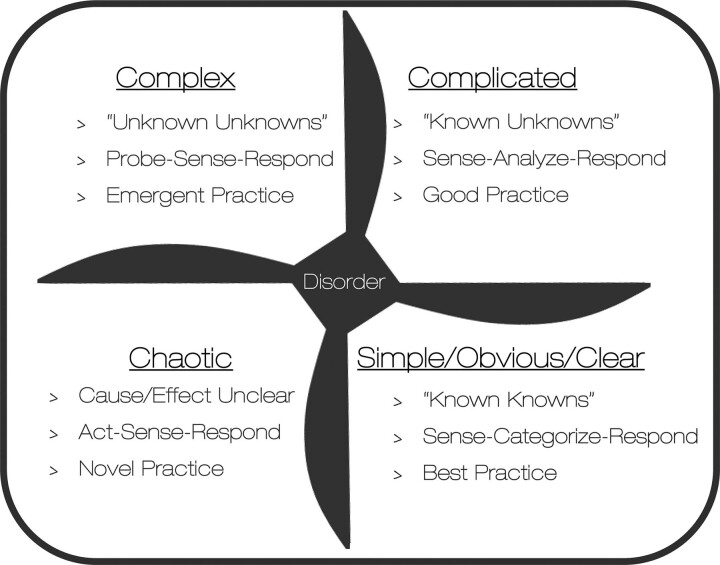
The COVID-19 pandemic has magnified awareness that the CLE is replete with uncertainty—so much so, that there is an opportunity to provide agents in the clinical workplace with a framework to both make sense and to act within a complex health system. The Cynefin framework, as adapted by Snowden and Boone, can be used as a sensemaking tool for understanding the “habitat” of a specific situation as a starting point to grapple with the issue at hand. 4 We chose the Cynefin framework over other sensemaking approaches, such as Weick’s theory on making sense of uncertain and ambiguous environments, because of the framework’s dynamic nature of describing stages of simple, complicated, complex, chaotic, and disordered environments. 6 Borrowing terminology from the Cynefin framework, the early stages of the pandemic immersed clinical teams in complex and chaotic situations, where there was no immediately apparent relationship between cause and effect (Figure 1).
Figure 1.
The Cynefin framework for sensemaking. Source: Papanagnou D, Jaffe R, Ziring D. Highlighting a curricular need: Uncertainty, COVID-19, and health systems science. Health Sci Rep. 2021;4:e363. Open access permission granted from Creative Commons. https://creativecommons.org/licenses/by/4.0/legalcode. Accessed April 21, 2022.
In most instances, teams were expected to emerge through the chaos amidst conflicting evidence and guidelines, limitations, shortages, and reconfiguration requirements. Solutions were not readily available. Teams had to act quickly amidst the chaos: they had to first act to establish order and stability, make sense of their actions, and respond with intentionality to move to a more ordered state. Murugan and colleagues describe the events of the pandemic through the lens of the volatility, uncertainty, complexity, and ambiguity (VUCA) framework of leadership action, identifying instances in which those 4 attributes characterized the health care setting. 7 Shortages of health care professionals, adequate access to personal protective equipment, and the heightened need for training health care workers on infection prevention and control measures exemplified instances in which VUCA challenged the complex system of the CLE. Teams had to experiment, adopt new evidence, and learn in the moment to tackle the challenges the pandemic posed. 7
The uncertainty surrounding clinical practice during the pandemic has had substantial repercussions on both individual practitioners and clinical care teams. Herzog notes there was no correct answer for teams, nor was there a curriculum teams could rely on to address clinical challenges. 8 Teams had to reconcile moral uncertainty as they rationed care for patients. 9 Practitioners had to navigate metaphysical uncertainty as they had to balance their personal and professional lives. 9 Providers even confronted the epistemic uncertainty that came with simply not knowing how to care for their patients at the bedside. 9 In hindsight, teams literally moved clockwise within the Cynefin framework: teams moved from the chaotic into the complex. The elements of VUCA surrounding COVID-19 continue to significantly alter the training environment and mental health of providers and learners in the CLE, 10 even as we are now moving toward the complicated domain of this framework. The pandemic has illustrated that teams will need to develop the capacity to productively learn together amidst complicated and complex circumstances. Complexity science offers the opportunity to better understand the informal and incidental learning (IIL) that takes place in the CLE.
Clinical teams working through complexity require a worldview that creates space for team members to adapt their mental models and be open to new perspectives, approaches, and techniques, particularly when traditional practices are no longer effective for achieving specific goals. 11 With regard to learning through complexity, Pendleton-Jullian and colleagues contend that individuals must be able to hold a range of possible responses in mind for problem solving. 12 The dynamics of both creativity and combinatorial activity can provide new and interesting responses to this complexity. In this regard, sensemaking is not necessarily the acquisition of new knowledge; rather, sensemaking is the reconfiguration of knowledge such that it means something personal to those working through the uncertainty. 12 In the face of uncertainty, teams must work together to create meaning and make sense of competing challenges. According to Pendleton-Jullian, “we need to poke at the corners of a problem, remain at the periphery, and allow [ourselves] to imagine, ‘What if I did this? What if I tried that out?’ Peripheral thinking holds solutions in abeyance so that a novel idea may emerge.” 12 This kind of unbound design liberates the practitioner to explore multiple pathways to solving a problem. 5
During the pandemic, patients presented with multiple confounding comorbidities that interacted with one another to obscure the effects of COVID-19; treatment plans that only addressed one diagnosis were simply not sufficient. Constraints such as these enable possibility by driving the dynamics within which solutions must be found. Relaxing constraints to free the imagination allows for a new coherence—or meaning—to emerge. In the face of uncertainty, this kind of learning, through freeing imagination, is only possible if we remain aware of the constraints at hand (e.g., time, resources, space, personnel). 12
Complexity science acknowledges the messiness and recognizes the interplay of contextual characteristics of clinical care, patient histories and presentations, team dynamics and interactions, and available knowledge and understanding, as well as emerging perception to take action. “Learning in the moment” is likely to occur in complex and/or chaotic contexts and yields emergent and novel responses. 13 This complexity viewpoint generates distinctions and assists individuals with “seeing the invisible,” so they may act from within learning—whether it be formal, informal, incidental, or novel. 13
Complexity science also focuses on interrelatedness. How experiences in the CLE are understood, in turn, affects the medical actions taken and practices pursued by care teams. One person’s sensemaking affects those around them. The networks teams form eventually become a source of knowledge for team members to draw on. Naturally, teams rely on these networks to manage uncertainty. To integrate the informal, sometimes haphazard nature of emergence among teams in the CLE, however, will require a better understanding of the processes that take place on the ground, in the moment, and at the point of care. The Marsick and Watkins model of IIL in the workplace is one way to describe this process of meaning making. 14
Focus on IIL: Learning in the Clinical Environment Amidst Complexity
Learning in the clinical environment, long described as informal, represents a process for learning that is “implicit, unintended, opportunistic, and unstructured” and not facilitated by a teacher. 15 Marsick and Watkins characterize this type of informal learning as learning that is integrated with work and daily routines, and triggered by an internal or external jolt—an impetus for learning that is not highly conscious, often haphazard, and influenced by chance and an inductive process of reflection and action. 16 Informal learning can be intentional even though unplanned, but it can also be incidental, or a semiconscious byproduct of tasks team members in the CLE undertake; for example, adopting practices of a hidden curriculum that may include specific workflows, procedures, and team roles for a designated clinical context. 17 Marsick and Watkins note that informal learning occurs in the moment, as gaps that need to be addressed arise; and often when doing something for which the primary purpose is not learning, such as solving a problem in the CLE. 11 In essence, IIL describes how clinical teams learn every day as they face challenges and circumstances calling for new ways to solve problems, make decisions, innovate, and develop. 11 Marsick and Watkins have argued that IIL is typically facilitated by individuals who are proactive, creative, and critically reflective. 18,19 When faced with uncertainty and disruptions in routine, IIL is required to “learn [a] way out” of novel circumstances. 11
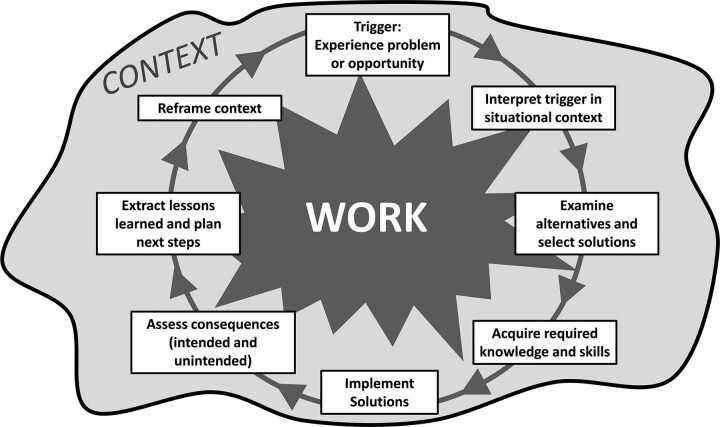
The IIL model (Figure 2) typically begins with a “trigger” or catalyst, which is often prompted by a gap between what individuals know and can do, and what they are expected to do. Members of the clinical team enter uncertain situations by accessing previous experiences, frames of reference, and/or mental models of previous similar situations, which immediately begin to influence developing mental models and actions during new and unfamiliar situations. Typically, members of the team will begin to survey the external environment, as well as their own internal meaning-making, to make sense of the situation they are experiencing. If members too strongly cling to previous frames of reference, they will likely be blind to other options for action and miss potential learning opportunities. If members remain open to creative and alternative ways of thinking, they can more readily explore and experiment with different ways of reacting, and in the process, reinterpret and reframe how they think about the problem. Members can maximize the benefit of IIL by remaining receptive to new ideas, as well as checking in and reflecting on feelings and biases that normally impede imagination and experimentation. 11 As team members experiment with responses to a specific situation, their understanding expands, and they eventually become aware of assumptions that may get in their way. Reflection is needed to assess lessons learned, examine mistakes, forestall unintended consequences, unearth assumptions, and/or transform views. 19
Figure 2.
Marsick and Watkins’ informal and incidental learning model.
While the model suggests a linear approach to IIL, in most cases, the application to real-life circumstances is nonlinear. In our work with studying critical incidents involving frontline clinicians working in acute care settings, IIL has served as an explanatory framework to better understand how physicians navigated uncertainty during the nascent stages of the pandemic. In several of these narratives, emergency medicine physicians commented on managing respiratory distress in COVID-positive patients (trigger). Specifically, it was disorienting to encounter younger, previously healthy patients present with uncharacteristically abnormal vital signs, such as significantly low oxygen saturation on pulse oximetry (trigger in a situational context). The concomitant presence of other disease processes in these patients, such as pneumonia and pulmonary embolism, further added to the complexity in the treating physicians’ ability to identify optimal treatment interventions (examining alternatives and selecting solutions). Unfortunately, however, conventional interventions for managing respiratory distress (e.g., mechanical ventilation) came with specific consequences for COVID-positive patients (assess consequences). As evidence-based strategies were not readily available, many turned to just-in-time social media outlets for management guidance from national and international peers (acquire required knowledge and skills), prompting clinicians to quickly test and adopt alternative, unconventional solutions (implement solutions). This illustrated that invasive measures that would normally support patients with respiratory distress must be reconsidered for this subset of patients (reframe context) and that much of their management of the disease would be situated around trial and error, with frequent communication with their interdisciplinary peers (extract lessons learners and plan next steps).
Complexity adds the need to learn while sensing and responding, as the Cynefin framework suggests, because of its inherent unpredictability. In the CLE, complexity and dynamic connections within and between actors in the CLE that are nondeterministic call for an openness to tensions, an embrace of paradox and contradictions, and readiness for testing an intervention that emerges in the situation itself. 20 Essentially, IIL describes the learning that needs to occur in unpredictable settings, when tools and/or experts are not readily available, and when learning is a by-product of working through issues amidst uncertainty. Understood through concepts borrowed from the Cynefin framework, the enabling constraints of complexity allow novel solutions to emerge, as teams become aware of possibilities that exist at the periphery. In the context of the pandemic, team culture, team structure, and team practices in the clinical environment have and continue to change, as teams transgress boundaries that were formerly impermeable to make space for emergence of new forms of work and learning within the dynamic context of the health system.
IIL is not easy to assess in action; however, informal learning relationships and networks that affect and support informal learning have been described. 15 Networks provide opportunity for clinicians to structure learning and increase homophily, a sociological theory whereby similar individuals will move toward each other and act similarly. Paradoxically, to optimize informal learning in team members across the health professions, heterophily is more desirable. The CLE offers the opportunity for team members from various health professions to come together to take best advantage of their diverse knowledge and specializations. 15 Social role-modeling, as well as the social hierarchy of the clinical team, also plays a role in the informal learning relationships developed. 15 For example, the roles of educators in the health professions are coconstructed within their respective clinical teams, as they “model, but rarely articulate, the implicit curriculum of norms, standards and expectations.” 21 In response to this, learners present themselves as capable members of the team by recognizing, interpreting, and reproducing their instructors’ implicit curricula. 21
Engaging in IIL is social and involves collaboration with others within the context of the organization or institution in which individuals are learning. 11 Learning in clinical environments relies on “social participation,” and is best theorized using a situated learning model of communities of practice (CoP). 22 Approaches to social learning offer a useful alternative to describing learning in terms of individualistic and social constructivist models, which have long held a privileged position in medical education. 22 Several studies of IIL in clinical environments reference Bandura’s social cognitive theory 23; Vygotsky’s socio-cultural theory 24; Wenger’s CoP theory 25; and Billet’s practice-based theory of guidance, participation, and engagement. 26,27 These theories describe tacit, socialized learning when solutions are known and conditions are predictable. Interprofessional teams learning in dynamic, complex environments, however, need to encourage fresh thinking by diverse members to create novel solutions to new challenges, as witnessed during the pandemic.
Implications for Health Professions Education
Fundamentally, training in health professions education should highlight the uncertainty that is intrinsic to clinical practice and “openly embrace it,” rather than trying to eliminate it in curricula. 8 It is possible to weave reflections on clinical uncertainty early in the classroom, together with evidence-based strategies, to better prepare learners to face the unknown. 8 Teams in the CLE require new models to address the complexities of the workplace that have emerged as a result of the pandemic. 10
The Cynefin framework may serve as a sensemaking tool to help practitioners better understand clinical complexity, better identify appropriate strategies, and avoid using reductionist approaches to complex situations. 28 The medical workforce needs to be equipped with the skills to manage change and emotional challenges, as well as the ability to build resilience. 29 Strategies to build these skills include leveraging coaching for self-directed learning and designing person-centered conversations with peers and patients. 29 There is a need to formally include innovative problem solving, such as rapid design thinking, in formal curricula to better address the complexities of the CLE.
Similarly, educators should leverage opportunities to prepare learners for the IIL they will likely participate in when working in the clinical environment over the course of their careers. Curriculum design must focus on the development of abilities that will support the exploration of creativity in the context of IIL. 11 To support decision making in the face of ambiguous, nonroutine situations, students in the health professions will require the power of intelligence (i.e., the ability to seek all available knowledge for a given situation), the power of design (i.e., the ability to craft innovative solutions and possibilities), and the power of choice (i.e., the ability to take intuitive leaps to select best possible options). Equally important, students will require the power of abductive reasoning—the ability to move from sensemaking (i.e., the ability to make observations and deductively and inductively reason) to sense-breaking (i.e., the ability to apply imagination and experiment in practice). 11
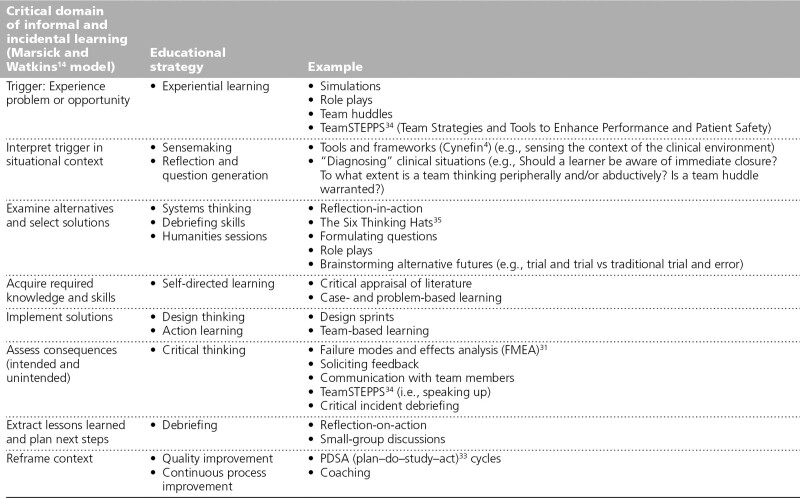
A curriculum for uncertainty in clinical practice should aim to build trainees’ curiosity, self-awareness, and flexibility. Such a curriculum should strategically concentrate on the development of skills that will prepare trainees to fully engage in the process of IIL with their interprofessional colleagues when they enter the clinical environment. Trainees should have the opportunity to deliberately practice skills such as asking open-ended questions, experimentation, and environmental scanning, as well as perspective taking, collecting data, and predicting and reacting to multiple alternative scenarios for uncertain situations. While we specifically target opportunities in undergraduate medical education, this approach also applies to ongoing curriculum development across the continuum of medical education, including learners involved in graduate medical education programs. Similarly, fostering IIL presents opportunities for skills development and training that may be achieved through continuing medical education and faculty development programming. Table 1 summarizes the implications for health professions education drawn from an integration of IIL in educating for uncertainty and complexity. Instructional modalities can be strategically integrated into a formal curriculum that aligns with the critical domains of the Marsick and Watkins model of IIL (Table 1).
Table 1.
Educational Strategies and Domains of Informal and Incidental Learning
For example, medical simulations and student role plays can be designed to trigger learners to “experience” a problem or an opportunity for action. Discussing complexity theory (i.e., the Cynefin framework) and linking concepts to clinical events can assist learners with the sensemaking needed to interpret triggers in situational contexts. Including pedagogies that foster participatory learning, such as case- and problem-based learning, can equip students with the skills to search for new knowledge and build self-directed learning. 30 Offering students the opportunity to participate in design sprints can build skills in design thinking and action learning, and can support the implementation and testing of solutions. 10 Immersing students in patient safety initiatives, such as failure modes and effects analyses 31 and critical incident debriefing in the CLE, 32 can help students assess both intended and unintended consequences. Additionally, active involvement in continuous quality and process improvement discussions can expose students to plan–do–study–act cycles, which can make reframing one’s context a habit. 33
Concluding Remarks
The study of IIL in the CLE is underdeveloped in health professions education. IIL offers the opportunity to describe the nuances of how teams navigate complexity and uncertainty in clinical practice, and take practical steps to integrate these observations into formal curricula to better prepare learners for their transition into the clinical workplace. While further research on IIL is needed to surface and reflect on tacit knowledge to make learning both more explicit and challengeable for all audiences in the health professions, 19 there are opportunities to cultivate learner skills in formal curricula to prime them for IIL when they enter the complexity of different CLEs.
Acknowledgments:
The authors would like to acknowledge medical students Nicholas MacDonald and Jacob Garcia, at the Sidney Kimmel Medical College at Thomas Jefferson University, for their assistance with developing Figure 1.
Footnotes
Funding/Support: At the time of writing, Dr. Papanagnou was a Macy Faculty Scholar through the Josiah Macy Jr. Foundation.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Contributor Information
Karen E. Watkins, Email: kwatkins@uga.edu.
Henriette Lundgren, Email: henriette.lundgren@gmail.com.
Grace A. Alcid, Email: gaa2128@tc.columbia.edu.
Deborah Ziring, Email: deborah.ziring@jefferson.edu.
Victoria J. Marsick, Email: marsick@tc.columbia.edu.
References
- 1.Gruppen LD, Irby DM, Durning SJ, Maggio LA. Conceptualizing learning environments in the health professions. Acad Med. 2019;94:969–974. [DOI] [PubMed] [Google Scholar]
- 2.Gheihman G, Johnson M, Simpkin AL. Twelve tips for thriving in the face of clinical uncertainty. Med Teach. 2020;42:493–499. [DOI] [PubMed] [Google Scholar]
- 3.Jaffe RC, Bergin CR, Loo LK, et al. Nested domains: A global conceptual model for optimizing the clinical learning environment. Am J Med. 2019;132:886–891. [DOI] [PubMed] [Google Scholar]
- 4.Snowden DJ, Boone ME. A leader’s framework for decision making. Harv Bus Rev. 2007;85:68–76. [PubMed] [Google Scholar]
- 5.Pendleton-Jullian AM, Brown JS. Design unbound. In: Design Unbound: Designing for Emergence in a White Water World. Cambridge, MA: MIT Press; 2018. [Google Scholar]
- 6.Weick K. Sensemaking in Organizations. Thousand Oaks, CA: Sage Publications; 1995. [Google Scholar]
- 7.Murugan S, Rajavel S, Aggarwal A, Singh A. Volatility, uncertainty, complexity and ambiguity (VUCA) in context of the COVID-19 pandemic: Challenges and way forward. Int J Health Systems Implement Res. 2020;4:10–16. [Google Scholar]
- 8.Herzog L. COVID-19: Unveiling the role of uncertainty in medical education. MedEdPublish. 2020;9:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tonelli MR, Upshur REG. A philosophical approach to addressing uncertainty in medical education. Acad Med. 2019;94:507–511. [DOI] [PubMed] [Google Scholar]
- 10.Thakur A, Soklaridis S, Crawford A, Mulsant B, Sockalingam S. Using rapid design thinking to overcome COVID-19 challenges in medical education. Acad Med. 2021;96:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watkins KE, Marsick VJ. Informal and incidental learning in the time of COVID-19. Adv Dev Hum Resour. 2021;23:88–96. [Google Scholar]
- 12.Watkins K, Nicolaides A, Herr N, Juarrero A, Pendleton-Jullian A, Siemens G. Learning through complexity: Exploring the intersection of complexity science and informal and incidental learning. Webinar, Mary Frances Early College of Education, The University of Georgia; January 29, 2021. https://www.youtube.com/watch?v=USmWilo-Hnc. Accessed March 30, 2022. [Google Scholar]
- 13.Marsick VJ, Watkins KE, Scully-Russ E, Nicolaides A. Rethinking informal and incidental learning in terms of complexity and the social context. J Adult Learn Knowl Innov. 2017;1:27–34. [Google Scholar]
- 14.Watkins KE, Marsick VJ. Re-cognizing informal learning in the workplace. Chapman D, ed. In: Proceedings of the Academy of Human Resource Development: Conference in the Americas. Houston, TX: Academy of Human Resource Development; 2014. [Google Scholar]
- 15.Wagter JM, van de Bunt G, Honing M, Eckenhausen M, Scherpbier A. Informal interprofessional learning: Visualizing the clinical workplace. J Interprof Care. 2012;26:173–182. [DOI] [PubMed] [Google Scholar]
- 16.Marsick VJ, Watkins KE. Informal and incidental learning. New Direct Adult Continuing Educ. 2001;2001:25. [Google Scholar]
- 17.Hafler JP, Ownby AR, Thompson BM, et al. Decoding the learning environment of medical education: A hidden curriculum perspective for faculty development. Acad Med. 2011;86:440–444. [DOI] [PubMed] [Google Scholar]
- 18.Marsick VJ, Watkins KE. Introduction to the special issue: An update on informal and incidental learning theory. New Direct Adult Continuing Educ. 2018;2018:9–19. [Google Scholar]
- 19.Watkins KE, Marsick VJ, Wofford MG, Ellinger AD. The evolving Marsick and Watkins (1990) theory of informal and incidental learning. New Direct Adult Continuing Educ. 2018;2018:21–36. [Google Scholar]
- 20.Nicolaides A, Scully-Russ E. Connections, questions, controversies, and the potential paths forward. New Direct Adult Continuing Educ. 2018;2018:103–124. [Google Scholar]
- 21.Cantillon P, De Grave W, Dornan T. Uncovering the ecology of clinical education: A dramaturgical study of informal learning in clinical teams. Adv Health Sci Educ Theory Pract. 2021;26:417–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egan T, Jaye C. Communities of clinical practice: The social organization of clinical learning. Health (London). 2009;13:107–125. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 24.Daniels H. Applications of sociocultural and activity theory to education. Daniels H. In: Vygotsky and Pedagogy. New York, NY: Routledge; 2002:106–140. [Google Scholar]
- 25.Wenger E. Communities of practice and social learning systems: The career of a concept. Blackmore C, ed. In: Social Learning Systems and Communities of Practice. London, UK: Springer London; 2010:179–198. [Google Scholar]
- 26.Billett S. Toward a workplace pedagogy: Guidance, participation, and engagement. Adult Educ Quarterly. 2002;53:27–43. [Google Scholar]
- 27.Billett S. Critiquing workplace learning discourses: Participation and continuity at work. Studies Educ Adults. 2002;34:56–67. [Google Scholar]
- 28.Van Beurden EK, Kia AM, Zask A, Dietrich U, Rose L. Making sense in a complex landscape: How the Cynefin framework from complex adaptive systems theory can inform health promotion practice. Health Promot Int. 2013;28:73–83. [DOI] [PubMed] [Google Scholar]
- 29.Maini A, Saravanan Y, Singh TA, Fyfe M. Coaching skills for medical education in a VUCA world. Med Teach. 2020;42:1308‐1309. [DOI] [PubMed] [Google Scholar]
- 30.Loyens SMM, Magda J, Rikers RMJP. Self-directed learning in problem-based learning and its relationships with self-regulated learning. Educ Psychol Rev. 2008;20:411–427. [Google Scholar]
- 31.Chiozza ML, Ponzetti C. FMEA: A model for reducing medical errors. Clin Chim Acta. 2009;404:75–78. [DOI] [PubMed] [Google Scholar]
- 32.Nadir NA, Bentley S, Papanagnou D, Bajaj K, Rinnert S, Sinert R. Characteristics of real-time, non-critical incident debriefing practices in the emergency department. West J Emerg Med. 2017;18:146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leis JA, Shojania KG. A primer on PDSA: Executing plan-do-study-act cycles in practice, not just in name. BMJ Qual Saf. 2017;26:572–577. [DOI] [PubMed] [Google Scholar]
References cited only in Table 1
- 34.Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS). Agency for Healthcare Research and Quality. https://www.ahrq.gov/teamstepps/index.html. Accessed April 20, 2022. [PubMed]
- 35.de Bono E. Six Thinking Hats. Boston, MA: Back Bay Books; 1999. [Google Scholar]