Abstract
Introduction
The general public was discussing racism and potential inequities in COVID-19 vaccinations among African Americans on Twitter before the first COVID-19 vaccine received emergency use authorization, but it is unclear how US state health departments (SHDs) were using Twitter to address the inequities. This study examines the frequency, content and timing of SHD tweets during the US rollout of the first SARS Co-V2 vaccine.
Methods
This was a prospective study of tweets posted from the official Twitter accounts of each of the 50 US SHDs and the DC health department from October 19, 2020 to February 28, 2021. We retrieved the content and metadata of 100% of their tweets; calculated frequencies and proportions of tweets containing key terms related to COVID-19 vaccines, equity and racism; stratified the data by region; and charted longitudinal trends.
Results
Overall, SHDs tweeted infrequently, and rarely tweeted about inequities, mistrust or racism. Though 55.48% of all SHD tweets were about COVID-19, hardly any tweets contained the terms: race/ethnicity (1.20%); equity (1.09); mistrust (.59%); or racism (.06%). Similar patterns existed among vaccination-related tweets, which accounted for 24.38% of all tweets. Only 21.64% of vaccination-related tweets containing any race/ethnicity, equity, mistrust, or racism terms were posted prior to the first Emergency Use Authorization (EUA). Those about African Americans (70.45%) were posted ≥8 weeks after EUA.
Conclusions
Concerns about racism and inequities in COVID-19 vaccination continue on Twitter, but SHDs rarely tweet about them. This strikes a worrisome chord of disconnection from the science linking health inequities to racism.
Keywords: Big Data, Social Media, COVID-19, Vaccine, Health Inequities, Racism
Introduction
Racism-based mistrust of public health messaging among African Americans is well-documented in the literature1-4; its potential to contribute to inequities in COVID-19 vaccinations for African Americans was a common theme in Twitter discussions before and after the US Food and Drug Administration (FDA) granted emergency use authorization (EUA) to Pfizer to make the nation’s first SARS coronavirus-2 vaccine available to the public.5 Racism-based mistrust stems from African Americans’ historical6-10 and present-day experiences with unfair treatment in the health care system (eg, not having their complaints taken seriously by providers) and elsewhere (eg, in social settings).11,12 The intersectional and disproportionate impact of COVID-19 and state-sanctioned violence (eg, policing)13,14 in this population further underscore the need to both promote vaccine equity15 and address racism-based mistrust on Twitter and elsewhere.
State health departments (SHDs), including the District of Columbia (DC) health department, are tasked with coordinating statewide or district-wide COVID-19 vaccination strategies and disseminating accurate information about the vaccine to the public and other stakeholders (eg, local health departments).16 The social media platform Twitter is an increasingly important venue for sharing health information. People use hashtags (#) to embed key terms in the text of a Twitter post (ie, a tweet), which makes it easier to find, track and share information on a specific topic.17 SHDs have increasingly used Twitter to disseminate information about the COVID-19 pandemic,18 but it is unclear how engaged they are in conversations about racism-related mistrust of COVID-19 vaccines.
This prospective study tracked the tweets of all US SHDs over time for four months from baseline (October 19, 2020) to characterize the frequency, key terms and timing of SHD tweets related to COVID-19 vaccination inequities and racism-based mistrust, especially among African Americans. The timing of tweets may offer insights about what motivated SHDs to begin tweeting about inequities and racism during this period; for instance, whether it was focusing on achieving herd immunity for the overall population or, on the other hand, attempting to mitigate the disproportionate burden of COVID-19 that had been documented since nearly the beginning of the pandemic.19
Methods
Design
This was a prospective study of the tweets posted from the official Twitter accounts of the 50 US SHDs and the DC health department from October 19, 2020 to February 28, 2021. This period provides data 54 days prior to FDA EUA of the nation’s first COVID-19 vaccine (ie, Pfizer) and 79 days thereafter. The University of California, Los Angeles (UCLA) institutional review board (IRB) reviewed the protocol and provided a waiver from ethics review.
Data Abstraction
Using Twitter Archiver, we retrieved the content and metadata of 100% of existing tweets, replies and retweets posted from each of the official SHD Twitter accounts during the study period. Twitter Archiver is a Google spreadsheet add-on that identifies tweets in real-time based on queries of Twitter and stores the results continuously (ie, every 15 minutes). Because it is difficult to distinguish quoted retweets from original tweets using Twitter Archiver, we did not count quoted tweets (ie, retweets with comments) as retweets. We linked each tweet to state-level demographic data (eg, racial/ethnic composition) from the 2019 American Community Survey 5-year estimates.
Measures
We generated six categories of key terms, which were words or phrases either with or without hashtags that were contained in the text of a tweet.
Category 1: COVID, pandemic, coronavirus
Category 2: vaccine, vaccination, Pfizer, Moderna, Johnson & Johnson, Janssen
Category 3: race, ethnicity, each racial/ethnic category (eg, Black/African American) specified by US Office of Management and Budget (OMB) Directive 1520,21
Category 4: (in)equity, (in)equality, (in)justice, disparity
Category 5: mistrust, hesitancy, distrust, trust
Category 6: racism, structural racism, institutional racism, systemic racism
We created binary variables coded yes=1/no=0 to indicate whether the text of the tweet contained each key term and excluded those that were irrelevant (eg, @whitehouse). These variables were aggregated by SHD to compute the total number of SHD tweets related to each category.
We linked each SHD’s official Twitter account to its state (n=51) and census region (n=4). Region was a categorical variable denoting the SHD’s US Census Designated Region. The US Census Bureau defines four census regions:22
Midwest (12 states: Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota and South Dakota);
Northeast (9 states: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York and Pennsylvania);
South (17 states: Delaware, District of Columbia, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, and Texas); and
West (13 states: Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, Alaska, California, Hawaii, Oregon, and Washington).
Population size and racial/ethnic composition were continuous, state-level measures of the number of residents and percentage of adults reporting Black race alone or in combination with some other race in the state based on the 2019 American Community Survey 5-year estimates.
Time was a continuous measure generated automatically by Twitter to indicate the date and time when tweets were posted. We retrieved it from the metadata of each tweet.
FDA EUA timing was a dichotomized variable indicating whether tweets occurred before (no=0) December 11, 2020 or not (yes=1).
Retweet was a binary variable coded yes=1/no=0 to indicate whether Twitter Archiver automatically coded it a retweet with text, “RT.”
Statistical Analysis
All analyses were completed using STATA version 15.23 We calculated the state-level frequencies and proportions of tweets containing each key term, stratified the data by region, and charted trends by region and state racial/ethnic composition. We also computed Spearman correlations between the number of tweets containing each key term and state racial/ethnic composition and performed unadjusted chi-square tests to compare the percentage of tweets posted before and after FDA EUA.
Results
Overall Tweets
Every official SHD Twitter account posted at least one tweet between October 19, 2020 and February 28, 2021, except for the Wyoming SHD’s account, which has been inactive since November 2019. Overall, there were N= 36,554 tweets, 22.73% of all tweets were retweets. How often SHDs tweeted ranged from n=1 (ME) to n=2,462 (MA); tweet frequency was unrelated to state population size. Of the posts tweeted during this period, 49 of the SHDs posted any tweets about COVID-19, 48 about vaccines, 43 about race, 38 about equity, 36 about mistrust and 10 about racism.
Relatively few tweets included the key terms (Table 1 and Table 2); therefore, we pooled the data across states to examine geographical trends by region. With respect to the total number of tweets, SHDs located in the South posted a greater overall percentage of all tweets (33.97%), tweets about COVID-19 (35.40%), vaccines (34.70%), inequities (39.20%) and racism (38.10%) than did SHDs in other regions. However, the number of states in a region varies, ranging from 17 (South) to 9 (Northeast). When we calculated averages to account for the number of states per region, the Northeast had the highest average number of tweets per SHD overall and for each key term category except for race/ethnicity.
Table 1. Tweets generated from state health department Twitter accounts by region - midwest and northeast, October 19, 2020 - February 28, 2021, n (%).
| State health department | Total tweets | Number of tweets containing a term related to: | |||||
| N=36,554a | COVID-19 | Vaccines | Race/ethnicity | Equity | Mistrust | Racism | |
| n=20,278a | n=8,913a | n=439a | n=398a | n=217a | n=21a | ||
| Midwest, n=12 | |||||||
| OH | 1,104 (3.02) | 621 (3.06) | 200 (2.24) | 10 (2.28) | 2 (.50) | 32 (14.75) | 0 (0) |
| MN | 763 (2.09) | 480 (2.37) | 104 (1.17) | 24 (5.47) | 6 (1.51) | 2 (.92) | 0 (0) |
| IN | 651 (1.78) | 432 (2.13) | 147 (1.65) | 8 (1.82) | 5 (1.26) | 1 (.46) | 0 (0) |
| WI | 617 (1.69) | 352 (1.74) | 101 (1.13) | 9 (2.05) | 11 (2.76) | 1 (.46) | 0 (0) |
| IL | 608 (1.66) | 454 (2.24) | 145 (1.63) | 6 (1.37) | 4 (1.01) | 2 (.92) | 0 (0) |
| SD | 563 (1.54) | 330 (1.63) | 131 (1.47) | 1 (0.23) | 0 (0) | 2 (.92) | 1 (4.76) |
| MI | 545 (1.49) | 351 (1.73) | 147 (1.65) | 14 (3.19) | 15 (3.77) | 3 (1.38) | 2 (9.52) |
| KS | 500 (1.37) | 148 (.73) | 72 (.81) | 11 (2.51) | 7 (1.76) | 0 (0) | 0 (0) |
| MO | 402 (1.10) | 165 (.81) | 143 (1.60) | 5 (1.14) | 5 (1.26) | 3 (1.38) | 0 (0) |
| ND | 375 (1.03) | 286 (1.41) | 41 (.46) | 3 (.68) | 1 (.25) | 3 (1.38) | 0 (0) |
| NE | 245 (.67) | 97 (.48) | 59 (.66) | 4 (.91) | 2 (.50) | 0 (0) | 0 (0) |
| IA | 138 (.38) | 41 (.2) | 17 (.19) | 3 (.68) | 0 (0) | 1 (.46) | 0 (0) |
| Northeast, n=9 | |||||||
| MA | 2,462 (6.74) | 1,520 (7.50) | 460 (5.16) | 17 (3.87) | 17 (4.27) | 45 (20.74) | 0 (0) |
| NY | 2,246 (6.14) | 974 (4.80) | 477 (5.35) | 25 (5.69) | 37 (9.30) | 8 (3.69) | 1 (4.76) |
| RI | 1,648 (4.51) | 714 (3.52) | 367 (4.12) | 7 (1.59) | 20 (5.03) | 7 (3.23) | 1 (4.76) |
| NJ | 1,115 (3.05) | 545 (2.69) | 330 (3.70) | 21 (4.78) | 18 (4.52) | 6 (2.76) | 0 (0) |
| VT | 1,049 (2.87) | 451 (2.22) | 281 (3.15) | 11 (2.51) | 12 (3.02) | 11 (5.07) | 2 (9.52) |
| PA | 926 (2.53) | 519 (2.56) | 232 (2.60) | 3 (.68) | 0 (0) | 4 (1.84) | 0 (0) |
| NH | 274 (0.75) | 191 (.94) | 57 (.64) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| CT | 130 (.36) | 33 (.16) | 57 (.64) | 2 (.46) | 2 (0.50) | 0 (0) | 0 (0) |
| ME | 1 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
a. N or n is for all four regions (across Tables 1 and 2)
Source: Authors’ analysis of state health department tweets posted between October 19, 2020 – February 28, 2021. Notes: State health departments include the Twitter accounts of the District of Columbia health department and all US state health departments. COVID-19 terms: COVID, coronavirus, pandemic; Vaccine terms: vaccine, vaccination, Pfizer, Moderna, Johnson & Johnson, Janssen; Race terms: race, ethnicity, racial/ethnic categories specified by US Office of Management and Budget; Equity terms: (in)equity, (in)equality, (in)justice, disparity; Mistrust terms: trust, mistrust, distrust, hesitancy; Racism terms: racism, racist. Derivatives of terms are included.
Table 2. Tweets generated from state health department Twitter accounts by region - south and west, October 19, 2020 - February 28, 2021, n (%).
| State health department | Total tweets | Number of tweets containing a term related to: | |||||
| N=36,554a | COVID-19 | Vaccines | Race/ethnicity | Equity | Mistrust | Racism | |
| n=20,278a | n=8,913a | n=439a | n=398a | n=217a | n=21a | ||
| South, n=17 | |||||||
| WV | 2,430 (6.65) | 1,906 (9.40) | 100 (1.12) | 3 (.68) | 56 (14.07) | 13 (5.99) | 0 (0) |
| SC | 1,223 (3.35) | 661 (3.26) | 441 (4.95) | 9 (2.05) | 9 (2.26) | 4 (1.84) | 0 (0) |
| NC | 1,212 (3.32) | 635 (3.13) | 314 (3.52) | 24 (5.47) | 36 (9.05) | 9 (4.15) | 3 (14.29) |
| AL | 1,060 (2.9) | 478 (2.36) | 316 (3.55) | 14 (3.19) | 1 (.25) | 6 (2.76) | 0 (0) |
| LA | 932 (2.55) | 315 (1.55) | 123 (1.38) | 0 (0) | 8 (2.01) | 5 (2.30) | 1 (4.76) |
| DC | 866 (2.37) | 425 (2.10) | 268 (3.01) | 2 (.46) | 19 (4.77) | 0 (0) | 2 (9.52) |
| TN | 719 (1.97) | 405 (2.00) | 148 (1.66) | 7 (1.59) | 4 (1.01) | 2 (.92) | 2 (9.52) |
| MD | 663 (1.81) | 448 (2.21) | 196 (2.20) | 4 (.91) | 8 (2.01) | 1 (.46) | 0 (0) |
| DE | 642 (1.76) | 367 (1.81) | 157 (1.76) | 5 (1.14) | 5 (1.26) | 3 (1.38) | 0 (0) |
| VA | 513 (1.40) | 231 (1.14) | 218 (2.45) | 7 (1.59) | 2 (.50) | 2 (.92) | 0 (0) |
| AR | 489 (1.34) | 394 (1.94) | 147 (1.65) | 1 (.23) | 1 (.25) | 1 (.46) | 0 (0) |
| TX | 473 (1.29) | 255 (1.26) | 172 (1.93) | 6 (1.37) | 5 (1.26) | 4 (1.84) | 0 (0) |
| FL | 330 (.90) | 83 (.41) | 146 (1.64) | 1 (.23) | 1 (.25) | 0 (0) | 0 (0) |
| OK | 303 (.83) | 141 (.70) | 155 (1.74) | 1 (.23) | 0 (0) | 1 (.46) | 0 (0) |
| GA | 290 (.79) | 238 (1.17) | 142 (1.59) | 2 (.46) | 1 (.25) | 3 (1.38) | 0 (0) |
| MS | 241 (.66) | 189 (.93) | 44 (.49) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| KY | 30 (.08) | 7 (.03) | 6 (.07) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| West, n=13 | |||||||
| AZ | 1,459 (3.99) | 586 (2.89) | 497 (5.58) | 5 (1.14) | 4 (1.01) | 4 (1.84) | 0 (0) |
| OR | 1,403 (3.84) | 692 (3.41) | 545 (6.11) | 40 (9.11) | 26 (6.53) | 6 (2.76) | 6 (28.57) |
| WA | 1,364 (3.73) | 995 (4.91) | 416 (4.67) | 12 (2.73) | 27 (6.78) | 6 (2.76) | 0 (0) |
| CO | 888 (2.43) | 633 (3.12) | 244 (2.74) | 10 (2.28) | 2 (.50) | 7 (3.23) | 0 (0) |
| NM | 701 (1.92) | 329 (1.62) | 93 (1.04) | 85 (19.36) | 3 (.75) | 0 (0) | 0 (0) |
| AK | 606 (1.66) | 252 (1.24) | 66 (.74) | 2 (.46) | 2 (.50) | 0 (0) | 0 (0) |
| ID | 602 (1.65) | 443 (2.18) | 243 (2.73) | 3 (.68) | 1 (.25) | 3 (1.38) | 0 (0) |
| CA | 539 (1.47) | 379 (1.87) | 69 (.77) | 9 (2.05) | 13 (3.27) | 5 (2.3) | 0 (0) |
| UT | 115 (.31) | 43 (.21) | 50 (.56) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| NV | 58 (.16) | 23 (.11) | 9 (.10) | 2 (.46) | 0 (0) | 0 (0) | 0 (0) |
| MT | 36 (.10) | 18 (.09) | 20 (.22) | 1 (.23) | 0 (0) | 1 (.46) | 0 (0) |
| HI | 5 (.01) | 3 (.01) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| WY | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
a. N or n is for all four regions (across Tables 1 and 2)
Source: Authors’ analysis of state health department tweets posted between October 19, 2020 – February 28, 2021. Notes: State health departments include the Twitter accounts of the District of Columbia health department and all US state health departments. COVID-19 terms: COVID, coronavirus, pandemic; Vaccine terms: vaccine, vaccination, Pfizer, Moderna, Johnson & Johnson, Janssen; Race terms: race, ethnicity, racial/ethnic categories specified by US Office of Management and Budget; Equity terms: (in)equity, (in)equality, (in)justice, disparity; Mistrust terms: trust, mistrust, distrust, hesitancy; Racism terms: racism, racist. Derivatives of terms are included.
While slightly more than half (55.47%) of all SHD tweets posted during this period included COVID-19 terms and nearly a quarter (24.38%) included vaccine terms, few included any race/ethnicity (1.20%) or equity (1.09%) terms. Hardly any included mistrust (.59%) or racism (.06%) terms (Table 1 and Table 2).
Vaccination-related Tweets
Similar patterns of key term inclusion existed among the vaccination-related tweets (n=8,913), though the frequencies were greater than they were with the overall tweets: 2.41% (n=215) of them included equity-related key terms, 1.96% (n=175) race/ethnicity terms and 1.82% (n=162) mistrust terms. Less than 1% (in two states: OR, NY) of all vaccination-related tweets included any racism term. No correlation existed between the frequency of vaccination-related tweets about race, racism, equity or mistrust and the percentage of Black residents in a state (Figure 1).
Figure 1. Number and percent of state health department vaccine tweets posted October 19, 2020 – February 28, 2021 that contained one of the key terms race, racism, equity, or mistrust by state percentage of non-Hispanic Black residents.
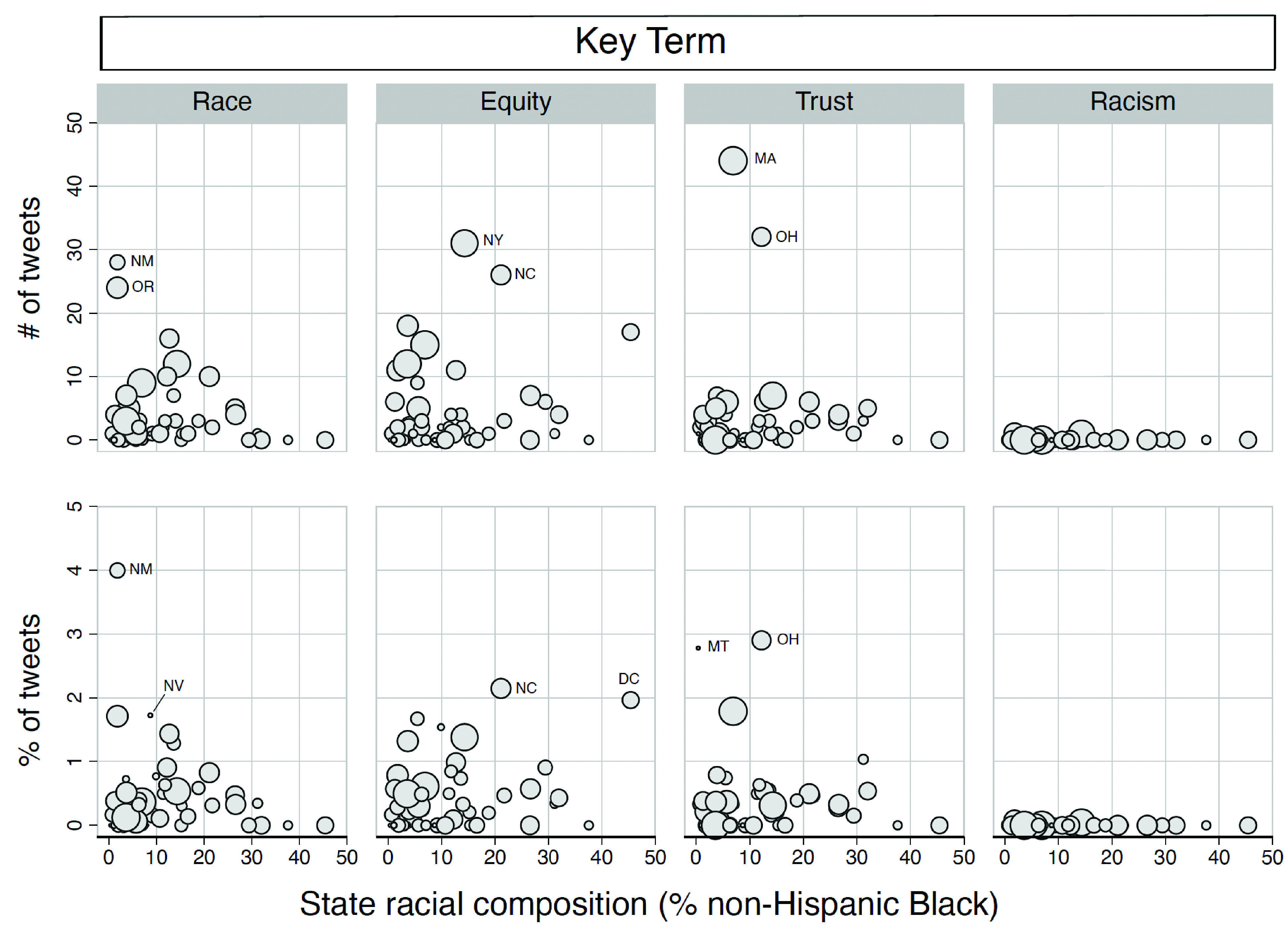
Source: % non-Hispanic Black data are from the 2019 American Community Survey 5-Year Estimates. Notes: Markers are weighted by the total number of tweets the state health department posted during the study period. The two states with the highest number/percentage of vaccine tweets that mention the key term are labeled. State health departments include the Twitter accounts of the District of Columbia health department and all US state health departments, except for the Wyoming state health department. Vaccine terms: vaccine, vaccination, Pfizer, Moderna, Johnson & Johnson, Janssen; Race terms: race, ethnicity, racial/ethnic categories specified by US Office of Management and Budget; Equity terms: (in)equity, (in)equality, (in)justice, disparity; Mistrust terms: trust, mistrust, distrust, hesitancy; Racism terms: racism, racist. Derivatives of terms are included.
With respect to the timing of all tweets and vaccination-related tweets, several trends were apparent (Figure 2). The majority of all tweets (62.58%) and tweets mentioning any race/ethnicity, equity, mistrust, or racism term (79.44%) were posted on or after the first EUA. Only 21.64% of tweets containing any race/ethnicity term (n=439) were posted prior to EUA of the first vaccine. Similarly, 87.92% of all tweets and 90.91% of all vaccination-related tweets about Black/African Americans were posted 8 or more weeks after EUA. Some 70.47% of all tweets and 70.45% of all vaccination-related tweets about African Americans were posted then. During the 30-day window on either side of EUA, a greater proportion of tweets containing race/ethnicity, equity, mistrust, or racism terms were posted on or after the first EUA, not before it (χ2=20.93, P<.001).
Figure 2. Daily number of state health department vaccine tweets by US Census designated region relative to the daily number of COVID-19 vaccine doses administered in the US, October 19, 2020 - February 28, 2021.
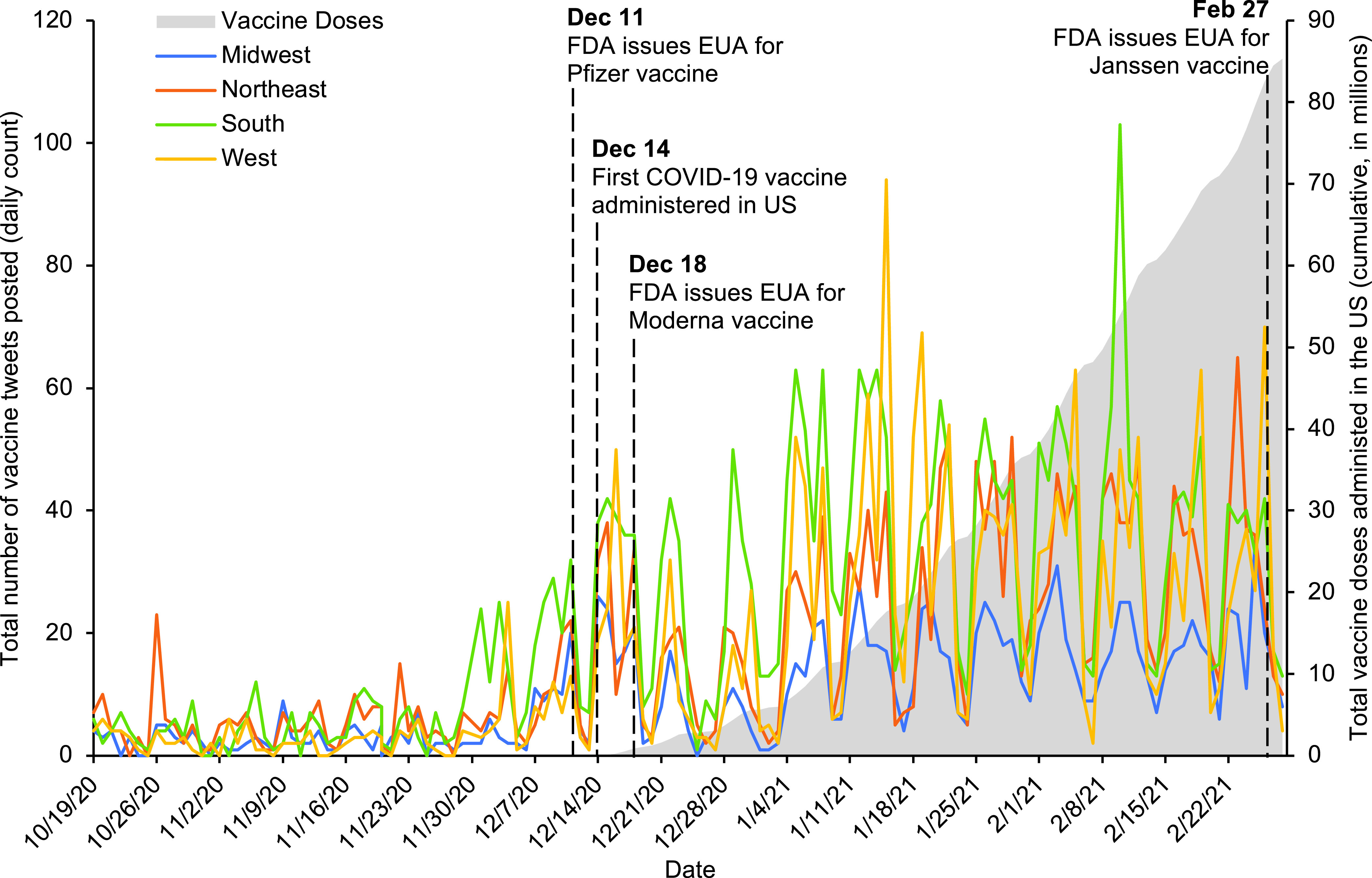
Sources: Authors’ analysis of state health department tweets posted between October 19, 2020 – February 28, 2021 and vaccine distribution data from the CDC COVID Data Tracker available at: https://covid.cdc.gov/covid-data-tracker/#vaccination-trends
Notes: Vaccine terms: vaccine, vaccination, Pfizer, Moderna, Johnson & Johnson, and Janssen. Derivatives of vaccine terms are included.
Discussion
Twitter is a potentially useful platform for addressing racism-based mistrust and the possibility of COVID-19 vaccination inequities; however, SHDs rarely used their Twitter accounts during the critical period when the vaccine was being rolled out to do so. This is notable given COVID-19 deaths were surging and concerns were already being raised that racism-based mistrust of COVID-19 vaccines among African Americans might contribute to inequities and, importantly, impede attainment of herd immunity for the overall US population.
On Twitter, to tweet often and use salient key terms (ie, hashtags) increases the likelihood that tweets reach the intended audiences as well as others who are interested in a topic. Since October 2020, however, most SHDs tweeted infrequently, and the tweets rarely included key terms related to COVID-19 vaccinations, COVID-19 inequities or racism, highlighting opportunities for them to expand the reach of SHD tweets.
With respect to timing, SHDs were slow to tweet using any of the key terms. Nearly 3/4ths of all inequity, mistrust and racism tweets occurred at least eight weeks after FDA EUA of the first vaccine. This delayed engagement contrasts starkly with on-the-ground vaccination efforts (Figure 2) that were ramping up rapidly during this period.24 Most SHD vaccination-related tweets on equity were posted nearly two months after FDA EUA; by this stage of the pandemic, COVID-19 rates among African Americans exceeded those of any other US racial/ethnic group.25 The delay leaves unresolved questions about what motivated SHDs to post the few tweets that did begin to include the key terms weeks after the vaccine had become widely available. Racial trends in a wide range of COVID outcomes had already been documented by mid-October 2020.25 Thus, the paucity of tweets in the pre-EUA period provides clear evidence that SHDs were not using Twitter then either to mitigate the disproportionate burden of disease already impacting African Americans or to prevent the emergence of racism-related inequities in vaccinations.
Why SHDs tweet so infrequently is not known. Access to Twitter does not appear to be a barrier. All SHDs and the District of Columbia have official Twitter accounts, and only one of them was inactive. Other potential explanations include time or resource constraints, inadequate training in social media use and agency policies that discourage social media use. It is also possible that SHDs were focused on other COVID-19 prevention activities and had little time to engage in social media.
The lack of SHD tweets mentioning racism raises questions about why and how some government agencies treat racism as a public health issue while others do not. For example, by October 2020 – the month our study began – most policies declaring racism a public health issue were from local rather than state government entities.26 It is possible that compared to other state and local government actors (eg, governors, mayors, and city councils), SHDs lack the political interest, will or pressure to publicly acknowledge and address racism as a public health issue.
Implications for Research
Research implications include the need for future studies to identify barriers to and facilitators of Twitter engagement among SHDs. The work should consider agency policies, limited resources, competing priorities (eg, testing), and training in social media use and health communications. Research is also needed to clarify the best allocation of prevention efforts between social media engagement and other prevention efforts. Finally, future research should determine if SHD tweeting about racism-related mistrust influences COVID-19 vaccination behaviors. Prior evidence on HIV inequities suggests racism-based mistrust is not necessarily a barrier to African Americans engaging in preventive behaviors.27,28
Implications for Practice
Hashtags function as key terms on Twitter helping individuals identify conversations to follow. The frequency and content of tweets can influence the number and types of people who follow an account. People may not follow SHD Twitter accounts that post infrequently, SHDs must optimize the timing and content of their tweets in order to reach their intended audiences.29 SHDs can improve the relevance and reach of their messages by using the same key terms as those used by the public.30
Limitations and Strengths
The study was limited to SHD tweets, therefore, our findings may not be generalizable to SHD social media posts on other platforms (eg, Facebook). While Twitter is not the most used social media platform, especially among vulnerable and socially marginalized populations (eg, African Americans, adults aged ≥50 years, and adults with low incomes),31 previous research indicates that discussions about racism-based mistrust of the COVID-19 vaccine among African Americans were common on Twitter before and after a COVID-19 vaccine became available.5 The findings do not explain the determinants of tweet frequency, timing and content. We determined the set of key terms to track and excluded misspelled words and tweets not written in English, which may have produced undercounts of potentially relevant tweets.
Study strengths include its longitudinal design and objective assessments of tweets, which provide valid, reliable indicators of SHD Twitter behavior. Furthermore, whereas most studies are based on a 1% sample of all specified tweets, this study is based on 100% of the tweets posted from the population of all US SHD official Twitter accounts, including the DC health department.
Conclusions
Despite the low cost, convenience, and popularity of Twitter, SHDs rarely use it to publicly discuss inequities in COVID-19 vaccination rates among diverse racial and ethnic populations. The near dearth of SHD tweets on this issue strikes a worrisome chord of disconnection from the science linking health and health care inequities to racism.
Acknowledgments
Bradford and Sharif were supported by the Ralph J. Bunche Center for African American Studies at UCLA. Work foundational to this publication was supported in part by the APA SAMHSA Minority Fellowship (Grant 1H79SM080388-01) awarded to Nicolás E Barceló who assisted in acquiring social media expertise. Opinions expressed are those of the authors.
We would also like to thank the staff at the Center for the Study of Racism, Social Justice & Health and UCLA FSPH Department of Community Health Sciences for administrative and technical support; and members of the COVID-19 Task Force on Racism & Equity for feedback on earlier versions of this work.
References
- 1.Corbie-Smith G, Ford CL. Distrust and poor self-reported health. Canaries in the coal mine? J Gen Intern Med. 2006;21(4):395-397. 10.1007/s11606-006-0138-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freimuth VS, Quinn SC, Thomas SB, Cole G, Zook E, Duncan T. African Americans’ views on research and the Tuskegee Syphilis Study. Soc Sci Med. 2001;52(5):797-808. 10.1016/S0277-9536(00)00178-7 [DOI] [PubMed] [Google Scholar]
- 3.Gamble VN. A legacy of distrust: African Americans and medical research. Am J Prev Med. 1993 Nov-Dec 1993;9(6 Suppl):35-8. [PubMed]
- 4.Gamble VN. Under the shadow of Tuskegee: african Americans and health care. Am J Public Health. 1997;87(11):1773-1778. 10.2105/AJPH.87.11.1773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Criss S, Nguyen TT, Norton S, et al. Advocacy, hesitancy, and equity: exploring U.S. race-related discussions of the COVID-19 vaccine on Twitter. Int J Environ Res Public Health. 2021;18(11):5693. 10.3390/ijerph18115693 10.3390/ijerph18115693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey ZD, Moon JR. Racism and the political economy of COVID-19: will we continue to resurrect the past? J Health Polit Policy Law. 2020;45(6):937-950. 10.1215/03616878-8641481 [DOI] [PubMed] [Google Scholar]
- 7.Bailey Z, Barber S, Robinson W, Slaughter- Acey J, Ford C, Sealy-Jefferson S. Racism in the Time of COVID-19. January, 2021. Interdisciplinary Association of Public Health Sciences. Last accessed May 12, 2022 from https://iaphs.org/racism-in-the-time-of-covid-19/
- 8.Bailey ZD, Feldman JM, Bassett MT. How structural racism works - racist policies as a root cause of US racial health inequities. N Engl J Med. 2021;384(8):768-773. 10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Academies of Sciences Engineering and Medicine . Communities in Action: Pathways to Health Equity. Washington, DC: National Academies Press; 2017. [PubMed] [Google Scholar]
- 10.Gee GC, Ford CL. Structural racism and health inequities: old issues, new directions. Du Bois Rev. 2011;8(1):115-132. 10.1017/S1742058X11000130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care . Unequal Treatment: What healthcare providers need to know about racial and ethnic disparities in healthcare. Washington, DC: Institute of Medicine; 2002. [Google Scholar]
- 12.Shavers VL, Fagan P, Jones D, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953-966. 10.2105/AJPH.2012.300773 10.2105/AJPH.2012.300773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Representative Ayanna Pressley Press Releases. Pressley, Warren, Lee Reintroduce Bold Legislation to Confront Structural Racism as a Public Health Crisis. February 1, 2021. Last accessed March 18, 2022 from https://pressley.house.gov/media/press-releases/pressley-warren-lee-reintroduce-bold-legislation-confront-structural-racism
- 14.COVID-19 Task Force on Racism & Equity . Statement on Policing and the Pandemic. Last accessed March 4, 2021, 2021. https://www.racialhealthequity.org/blog/policingandpandemic
- 15.Jones CP. Systems of power, axes of inequity: parallels, intersections, braiding the strands. Med Care. 2014;52(10)(suppl 3):S71-S75. 10.1097/MLR.0000000000000216 10.1097/MLR.0000000000000216 [DOI] [PubMed] [Google Scholar]
- 16.Tsao SF, Chen H, Tisseverasinghe T, Yang Y, Li L, Butt ZA. What social media told us in the time of COVID-19: a scoping review. Lancet Digit Health. 03 2021;3(3):e175-e194. https://doi.org/ 10.1016/S2589-7500(20)30315-0 [DOI] [PMC free article] [PubMed]
- 17.Neiger BL, Thackeray R, Burton SH, Thackeray CR, Reese JH. Use of twitter among local health departments: an analysis of information sharing, engagement, and action. J Med Internet Res. 2013;15(8):e177. 10.2196/jmir.2775 10.2196/jmir.2775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y, Hao H, Platt LS. Examining risk and crisis communications of government agencies and stakeholders during early-stages of COVID-19 on Twitter. Comput Human Behav. 2021;114:106568. https://doi.org/ 10.1016/j. chb.2020.106568 PMID:32982038 [DOI] [PMC free article] [PubMed]
- 19.United States Food and Drug Administration . Comirnaty and Pfizer-BioNTech COVID-19 Vaccine. Updated January 25, 2022. Last accessed January 31, 2022 from https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/comirnaty-and-pfizer-biontech-covid-19-vaccine
- 20.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Fed Regist. 1997;62(210):58782-58790. [Google Scholar]
- 21.Friedman DJ, Cohen BB, Averbach AR, Norton JM. Race/ethnicity and OMB Directive 15: implications for state public health practice. Am J Public Health. 2000;90(11):1714-1719. 10.2105/AJPH.90.11.1714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Census Bureau . Geographic Levels. Last accessed March 24, 2022 from https://www.census.gov/programs-surveys/economic-census/guidance-geographies/levels.html#par_textimage_34
- 23.StataCorp . Stata Statistical Software: Release 15. College Station, TX: StataCorp LP; 2017. [Google Scholar]
- 24.McClung N, Chamberland M, Kinlaw K, et al. The Advisory Committee on Immunization Practices’ Ethical Principles for Allocating Initial Supplies of COVID-19 Vaccine-United States, 2020. Am J Transplant. 2021;21(1):420-425. 10.1111/ajt.16437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID Tracking Project . The COVID Racial Data Tracker. Updated March 7, 2021. Last accessed January 31, 2022 from https://covidtracking.com/race
- 26.Mendez DD, Scott J, Adodoadji L, Toval C, McNeil M, Sindhu M. Racism as public health crisis: assessment and review of municipal declarations and resolutions across the United States. Front Public Health. 2021;9:686807. 10.3389/fpubh.2021.686807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bohnert AS, Latkin CA. HIV testing and conspiracy beliefs regarding the origins of HIV among African Americans. AIDS Patient Care STDS. 2009;23(9):759-763. 10.1089/apc.2009.0061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ford CL, Daniel M, Earp JL, Kaufman JS, Golin CE, Miller WC. Perceived everyday racism, residential segregation and HIV testing in an STD clinic sample. Am J Public Health. 2009;99(suppl 1):S137-S143. 10.2105/AJPH.2007.120865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ortega P, Shin TM, Pérez-Cordón C, Martínez GA. Incorporate language in medical education to address structural barriers to care during the COVID-19 pandemic and beyond. Acad Med. 2021;96(2):e10-e11. 10.1097/ACM.0000000000003845 10.1097/ACM.0000000000003845 [DOI] [PubMed] [Google Scholar]
- 30.Renshaw SL, Mai S, Dubois E, Sutton J, Butts CT. Cutting through the noise: predictors of successful online message retransmission in the first 8 months of the COVID-19 pandemic. Health Secur. 2021;19(1):31-43. 10.1089/hs.2020.0200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Auxier B, Anderson M. Social media use in 2021. Pew Research Center. Last accessed April 4, 2022 from https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/


