Study Design:
Retrospective radiologic analysis.
Objective:
The aim was to investigate if lateral flexion-extension radiographs identify additional cases of degenerative cervical spondylolisthesis (DCS) that would be missed by obtaining solely neutral upright radiographs, and determine the reliability of magnetic resonance imaging (MRI) in diagnosis.
Summary of Background Data:
DCS and instability can be a cause of neck pain, radiculopathy, and even myelopathy. Standard anteroposterior and lateral radiographs and MRI of the cervical spine will identify most cervical spine pathology, but spondylolisthesis and instability are dynamic issues. Standard imaging may also miss DCS in some cases.
Methods:
We compared the number of patients who demonstrated cervical spondylolisthesis on lateral neutral and flexion-extension radiographs in addition to MRI. We used established criteria to define instability as ≥2 mm of listhesis on neutral imaging, and ≥1 mm of motion between flexion-extension radiographs.
Results:
A total of 111 patients (555 cervical levels) were analyzed. In all, 41 patients (36.9%) demonstrated cervical spondylolisthesis on neutral and/or flexion-extension radiographs. Of the 77 levels of spondylolisthesis, 17 (22.1%) were missed on neutral radiographs (P,0.05). Twenty levels (26.0%) were missed when flexion-extension radiographs were used alone (P=0.02). Twenty-nine levels (37.7%) of DCS identified on radiograph were missed by MRI (P=0.004).
Conclusions:
Lateral flexion-extension views can be useful in the diagnosis of DCS. These views provide value by identifying a significant cohort of patients that would be undiagnosed based on neutral radiographs alone. Moreover, MRI missed 38% of DCS cases identified by radiographs. Therefore, lateral radiographs can be a useful adjunct to neutral radiographs and MRI when instability is suspected or if these imaging modalities are unable to identify the source of a patient’s neck or arm pain.
Key Words: degenerative cervical spondylolisthesis, flexion-extension radiographs, neutral upright radiographs, MRI
Degenerative cervical spondylolisthesis (DCS) is characterized by vertebral body translation with respect to the caudal vertebral body.1,2 The etiology of DCS is multifactorial and includes facet instability or fracture, cervical disc degeneration, and hypertrophic arthropathy of facet joints.1–3 Patients with DCS typically present with neck pain and symptoms relating to radiculopathy or myelopathy. The prevalence of DCS may be as high as 5.2% in asymptomatic patients and 20% in symptomatic patients reporting neck pain or radiculopathy with or without neurological symptoms.2,4–6
DCS has increasingly been noted in the literature as a source of neck pain and radiculopathy. In a study by Dean and colleagues, the authors performed a retrospective review on 58 patients who underwent surgery specifically for cervical spondylolisthesis.5 The authors noted an average Nurick grade improvement of 1.5. In another study by Woiciechowsky and colleagues, the authors perfomed a retrospective review on 16 patients with cervical spondylolisthesis. The authors noted severe myelopathy in 8 patients, myeloradiculopathy in 5 paitents, and neck pain in 3 patients.6 The authors noted that neck pain was the initial complaint in all the patients. After surgery, neurological improvement was seen in 6 of 8 patients with myelopathy and 4 of 5 patients with radiculomyelopathy. Hence, cervical spondylolisthesis can be a significant source of pain and disability.
Given the recent findings of these studies, we set out to perform a study to determine if flexion-extension radiographs held value in radiographic evaluation of DCS. We hypothesized that flexion-extension radiographs would not identify additional cases of instability, and their use may be discontinued in routine evaluation of DCS. Secondarily, we hypothesized as the Segebarth group found for DLS, MRI would not identify all cases of cervical spondylolisthesis as compared with those detected on neutral or dynamic radiographs.
METHODS
After institutional IRB approval, we used billing codes to identify all patients who presented to our outpatient spine clinic from 2015 to 2018 who underwent cervical spine magnetic resonance imaging (MRI) and complete cervical spine radiograph series including, at minimum, upright anteroposterior, lateral neutral, flexion, and extension views. Exclusion criteria included MRI and radiographs completed >1 year of each other and patients with radiographic evidence or electronic medical record documentation of acute trauma or prior cervical spine surgery.
Horizontal translation of the posterior vertebral body of one level compared with the posterior vertebral body of the caudad cervical level was measured as previously described.6 This was completed on 5 levels for each patient, including C2-C3, C3-C4, C4-C5, C5-C6, and C6-C7, on each radiograph (neutral, flexion, extension), and midline sagittal T1 reconstruction of cervical spine MRI. Anterolisthesis was recorded as a positive value, and retrolisthesis recorded as a negative value. The value of flexion listhesis minus extension listhesis was recorded at each level to determine the magnitude of dynamic instability. Final magnitudes of listheses were converted to absolute values when determining instability thresholds. All measurements were recorded to 0.1 mm. A positive case of spondylolisthesis was defined as displacement of the posterior vertebral body relative to the caudad vertebral body of at least 2 or 1 mm of adjacent cervical vertebral body motion between upright lateral flexion and extension radiographs.7
After measurements were recorded, all computations performed in SPSS version 22.0 (IBM, Armonk, NY). Analyses were performed to identify levels in which spondylolisthesis were present as per above radiographic thresholds on lateral neutral listhesis magnitude, flexion minus extension listhesis (dynamic instability) magnitude, and MRI listhesis magnitude. We then used computational analyses to determine the number of levels with spondylolisthesis based on lateral neutral and flexion-extension radiographs, as well as on MRI. We compared these values to identify the total number of cases of spondylolisthesis and determine the number of cases that were missed on either neutral or flexion-extension radiographs, as well as on MRI. We also used this data to characterize spondylolisthesis at each level. χ2 testing was used to identify if there were any statistically significant differences.
RESULTS
A total of 111 patients were identified as having appropriate imaging for study inclusion, totaling 555 cervical levels. Forty-one of these patients demonstrated cervical spondylolisthesis (36.9%) for a total of 77 of the examined levels (13.9%) based on neutral and/or flexion-extension radiographs. Of these 77 levels, 60 levels (77.9%) of spondylolisthesis were demonstrated on neutral radiographs and 57 levels (74.0%) were identified using flexion-extension radiographs. Seventeen levels (22.1%) were missed by using solely neutral radiographs. This difference was noted to be statistically significant (P<0.05). Twenty levels (26.0%) were missed by using solely flexion-extension radiographs. This difference was also noted to be statistically significant (P=0.02). Fifty-two levels (67.5%) demonstrated corresponding spondylolisthesis on MRI, leaving 29 levels (37.7%) missed by MRI. This difference was noted to be statistically significant (P=0.004). These results are listed in Table 1.
TABLE 1.
Quantification of Cases of Spondylolisthesis Identified on Various Imaging Modalities
| Spondylolisthesis Identified On | n (%) |
|---|---|
| Neutral or flexion-extension radiograph | 77 (100.00) |
| Neutral radiograph | 60 (77.92) |
| Flexion-extension radiograph | 57 (74.03) |
| Neutral and flexion-extension radiograph | 40 (51.90) |
| MRI | 52 (67.53) |
| Radiograph but not MRI | 29 (37.66) |
| Neutral radiograph but not flexion-extension radiograph | 20 (25.97) |
| Flexion-extension radiograph but not neutral radiograph | 17 (22.08) |
MRI indicates magnetic resonance imaging.
The most common location of spondylolisthesis was at the C4-5 level with 29 cases identified (35.8%). The least frequent location of spondylolisthesis was demonstrated at the C6-7 level with 1 case identified (1.2%). Characteristics of spondylolisthesis per level are represented in Table 2 and Figure 1.
TABLE 2.
Characterization of Spondylolisthesis Per Cervical Level on Neutral or Flexion-extension Radiographs
| Level | n (%) | Mean (mm) | SD | Range (mm) | Minimum (mm) | Maximum (mm) |
|---|---|---|---|---|---|---|
| C2-3 | 9 (11.1) | 0.9889 | 2.2784 | 7.4 | −3.5 | 3.9 |
| C3-4 | 19 (23.5) | 1.1632 | 2.13 | 8.6 | −4.3 | 4.3 |
| C4-5 | 29 (35.8) | 0.0931 | 2.50798 | 8.7 | −3.9 | 4.8 |
| C5-6 | 19 (23.5) | −1.4421 | 1.91204 | 5.7 | −3.2 | 2.5 |
| C6-7 | 1 (1.2) | −2.3 | NA | NA | −2.3 | −2.3 |
FIGURE 1.
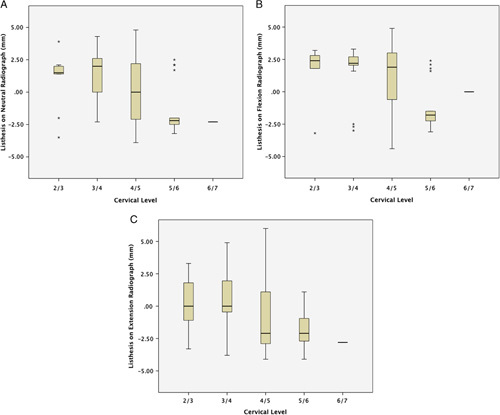
Graphical representation of spondylolisthesis per cervical level on neutral (A), flexion (B), and extension (C) radiographs.
DISCUSSION
Flexion and extension radiographs provide important information in the diagnosis and characterization of DCS. In this study, 17 levels (22.1%) were missed by using solely neutral radiographs. This was statistically significant (P<0.05). However, it is important to note that cases of spondylolisthesis were not identified on flexion-extension views alone. Twenty levels (26.0%) were missed by using solely flexion-extension radiographs (P=0.02). Also, 29 levels (37.7%) were missed by MRI alone (P=0.004). So, flexion and extension radiographs should not be used in place of standard anteroposterior (AP) and lateral radiographs. But they can be a useful adjunct in identifying cervical spondylolisthesis when standard AP and lateral imaging and MRI are not able to identify the source of a patient’s complaint of neck and radicular pain. To our knowledge, this is a field of study that has not received attention in current literature.
In the cervical spine, unique force vectors and the kinematics involved in flexion and extension which may contribute to the findings obtained in this study. High-speed cineradiography has previously demonstrated the complexities of cervical flexion and extension. Flexion is initiated at the lower cervical spine levels (C4-C7), followed by motion sequentially from the occiput through C4. Continuing this motion, C6 through C7 exhibit a transient extension moment, with subsequent reversal of motion at the occiput through C2, with C6 and C7 contributing to terminal flexion.8,9 Similarly, extension begins at the lower cervical spine levels (C4-C7), followed by motion at the occiput through C2, with the mid-cervical region contributing to intermediate range of motion and lower cervical spine contributing to terminal extension.9,10 Initiation of flexion and extension at C4 correlates with C4-5 being the most frequent level of spondylolisthesis in our study, which may be related to this principle and an interesting further avenue of study.
This study is the first published to our knowledge with regard to the topic of flexion and extension radiographs in DCS. While it may bring up some curious findings that open up further research topics, our study does have the weaknesses of being limited to a single clinical setting. We also used all patients presenting to clinic with available imaging, and did not limit inclusion criteria to patients with delineated symptoms. Whether this would have statistical or clinical significance is unclear. There is also no clinical correlation as to whether each patient went on to subsequent surgery, which we could not completely identify, given some patients were visiting for second opinions or may have eventually had surgery at another institution. What is clear is that our knowledge of the pathology and factors associated with DCS is not complete and should be further studied to continue improving patient care. It has been reported that unfamiliarity with DCS has resulted in patients being unnecessarily placed in cervical traction and hospitalized, underpinning the importance of appropriate radiographic characterization of this pathologic process.11
CONCLUSION
Lateral flexion-extension can be a useful adjunct to standard AP and lateral radiographs in the diagnosis and characterization of DCS. Recent studies have shown that cervical spondylolisthesis can be a source of cervical spine pain and nerve injury. This is the first study to show how lateral flexion-extension radiographs can be useful in identifying cases of cervical spondylolisthesis that standard AP and lateral radiographs, and MRI may miss.
Footnotes
The authors declare no conflict of interest.
Contributor Information
Andrew P. Alvarez, Email: andrewpa@hs.uci.edu.
Amanda Anderson, Email: amandma1@uci.edu.
Saifal-Deen Farhan, Email: saifaldeen81@yahoo.com.
Young Lu, Email: yxl2185@miami.edu.
Yu-Po Lee, Email: yupol1@hs.uci.edu.
Michael Oh, Email: ohm2@hs.uci.edu.
Charles Rosen, Email: crosen@hs.uci.edu.
Douglas Kiester, Email: pkiester@protonmail.com.
Nitin Bhatia, Email: bhatian@hs.uci.edu.
REFERENCES
- 1.Kopacz KJ, Connolly PJ. The prevalence of cervical spondylolisthesis. Orthopedics. 1999;22:677–679. [PubMed] [Google Scholar]
- 2.Suzuki A, Daubs MD, Inoue H, et al. Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine (Phila Pa 1976). 2013;38:E1115–E1120. [DOI] [PubMed] [Google Scholar]
- 3.Boulos AS, Lovely TJ. Degenerative cervical spondylolisthesis: diagnosis and management in five cases. J Spinal Disord. 1996;9:241–245. [PubMed] [Google Scholar]
- 4.Dean CL, Gabriel JP, Cassinelli EH, et al. Degenerative spondylolisthesis of the cervical spine: analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J. 2009;9:439–446. [DOI] [PubMed] [Google Scholar]
- 5.Jiang SD, Jiang LS, Dai LY. Degenerative cervical spondylolisthesis: a systematic review. Int Orthop. 2011;35:869–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woiciechowsky C, Thomale UW, Kroppenstedt SN. Degenerative spondylolisthesis of the cervical spine—symptoms and surgical strategies depending on disease progress. Eur Spine J. 2004;13:680–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aoyama R, Shiraishi T, Kato M, et al. Characteristic findings on imaging of cervical spondylolisthesis: analysis of computed tomography and X-ray photography in 101 spondylolisthesis patients. Spine Surg Relat Res. 2018;2:30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Mameren H, Drukker J, Sanches H, et al. Cervical spine motion in the sagittal plane (I) range of motion of actually performed movements, an X-ray cinematographic study. Eur J Morphol. 1990;28:47–68. [PubMed] [Google Scholar]
- 9.Swartz EE, Floyd RT, Cendoma M. Cervical spine functional anatomy and the biomechanics of injury due to compressive loading. J Athl Train. 2005;40:155–161. [PMC free article] [PubMed] [Google Scholar]
- 10.van Mameren H, Sanches H, Beursgens J, et al. Cervical spine motion in the sagittal plane. II. Position of segmental averaged instantaneous centers of rotation—a cineradiographic study. Spine (Phila Pa 1976). 1992;17:467–474. [DOI] [PubMed] [Google Scholar]
- 11.Lee C, Woodring JH, Rogers LF, et al. The radiographic distinction of degenerative slippage (spondylolisthesis and retrolisthesis) from traumatic slippage of the cervical spine. Skeletal Radiol. 1986;15:439–443. [DOI] [PubMed] [Google Scholar]


