Abstract
Antibiotic resistance is increasing worldwide making it necessary to search for alternative antimicrobials. Sodium bituminosulfonate is a long-known substance, whose antimicrobial inhibitory activity has recently been re-evaluated. However, to the best of our knowledge, the bactericidal mode of action of this substance has not been systematically characterized. The aim of this study was to investigate the in vitro bactericidal activity of sodium bituminosulfonate by determining the minimal bactericidal concentrations (MBC), as well as the rapidity of bactericidal effect by time-kill curves. Clinical isolates of methicillin-susceptible (MSSA, n = 20) and methicillin-resistant (mecA/mecC-MRSA, n = 20) Staphylococcus aureus were used to determine MBC by a broth microdilution method. Sodium bituminosulfonate (Ichthyol® light) was tested in double-dilution concentration steps ranging from 0.03 g/L to 256 g/L. For time-kill analysis, two reference and two clinical S. aureus strains were tested with different concentrations of sodium bituminosulfonate (1× minimal inhibitory concentration (MIC), 2× MIC, 4× MIC, 16× MIC and 256× MIC). For MSSA isolates, MBC50, MBC90 and the MBC range were 0.5 g/L, 1.0 g/L and 0.125–1.0 g/L; (MBC/MIC ratio)50, (MBC/MIC ratio)90 and the range of the MBC/MIC ratio were 4, 4 and 1–8, respectively. Among MRSA isolates, MBC50, MBC90 and the MBC range amounted to 0.5 g/L, 1.0 g/L and 0.06–1.0 g/L; (MBC/MIC ratio)50, (MBC/MIC ratio)90 and the range of the MBC/MIC ratio were 2, 4 and 1–8, respectively. Time-kill kinetics revealed a bactericidal effect after 30 min for sodium bituminosulfonate concentrations of 16× MIC and 256× MIC. The bactericidal activity against MSSA and MRSA was demonstrated for sodium bituminosulfonate. The killing was very rapid with the initial population reduced by 99.9% after only short incubation with concentrations of 16× MIC and higher.
Keywords: sodium bituminosulfonate, Staphylococcus aureus, bactericidal activity
1. Introduction
The burden of bacterial resistance against antibiotics is steadily increasing [1,2]. The development of antimicrobial resistance (AMR) is driven by use of antibiotics in humans, animals and the environment, as well as the worldwide spread of resistant bacteria [3]. Although considerable improvements in the control of methicillin-resistant Staphylococcus aureus (MRSA) have been made in certain countries, in the WHO priority list of antibiotic-resistant bacteria, MRSA is still ranked as a high priority pathogen [4]. In 2019, MRSA caused more than 100,000 deaths and 3.5 million disability-adjusted life-years attributable to AMR [5]. Despite some progress achieved in the antibacterial pipeline in recent years, the pipeline outlook remains unfavorable [6,7]. In the context of a scarcity of new antimicrobial treatments, the re-examination of old substances with antimicrobial activity has potential value [8]. Such re-evaluation includes the collection of in vitro susceptibility data as well as consideration of clinical evidence, including pharmacokinetic/pharmacodynamic analyses [9,10]. Sodium bituminosulfonate, a long-known substance derived from sulfur-rich oil shale and commonly known as “Ichthyol®, light” [11], has been used to treat various conditions, particularly in dermatology, including skin infections, for nearly a century [12,13,14]. The in vitro antimicrobial activity of sodium bituminosulfonate has recently been re-evaluated according to current international guidelines on antimicrobial susceptibility testing (AST) [15]. To the best of our knowledge the first time this has been undertaken, we performed a systematic investigation and characterization of the bactericidal activity of sodium bituminosulfonate against S. aureus.
2. Results
2.1. Determination of MIC and MBC
Of 20 clinical MRSA strains, the mecA gene was detected in 19 strains, whereas one strain possessed the mecC gene. All MSSA isolates tested mecA/mecC-negative. For MSSA as well as for MRSA clinical isolates, the MIC50 and MIC90 values were 0.125 g/L and 0.25 g/L, respectively. The MIC range was 0.06–0.5 g/L for MSSA and 0.06–0.25 g/L for MRSA. The MBC50 and MBC90 values were equal for MSSA and MRSA and amounted to 0.5 g/L and 1.0 g/L, respectively (Table 1). MBC ranges were 0.125–1.0 g/L and 0.06–1.0 g/L for MSSA and MRSA, respectively. The (MBC/MIC ratio)50, (MBC/MIC ratio)90 and the range of the MBC/MIC ratio are shown in Table 1.
Table 1.
Bactericidal activity of sodium bituminosulfonate against methicillin-susceptible (MSSA, n = 20) and methicillin-resistant (MRSA, n = 20) Staphylococcus aureus isolates.
| Strains | MIC50 (g/L) | MIC90 (g/L) | MIC Range (g/L) | MBC50 (g/L) | MBC90 (g/L) | MBC Range (g/L) | (MBC/MIC Ratio)50 | (MBC/MIC Ratio)90 | (MBC/MIC Ratio) Range |
|---|---|---|---|---|---|---|---|---|---|
| MSSA | 0.125 | 0.25 | 0.06–0.5 | 0.5 | 1.0 | 0.125–1.0 | 4 | 4 | 1–8 |
| MRSA | 0.125 | 0.25 | 0.06–0.25 | 0.5 | 1.0 | 0.06–1.0 | 2 | 4 | 1–8 |
The MICs of vancomycin determined for S. aureus ATCC 29213 by general QC testing were within the ranges recommended by EUCAST and CLSI [15,16].
2.2. Time-Kill Curves
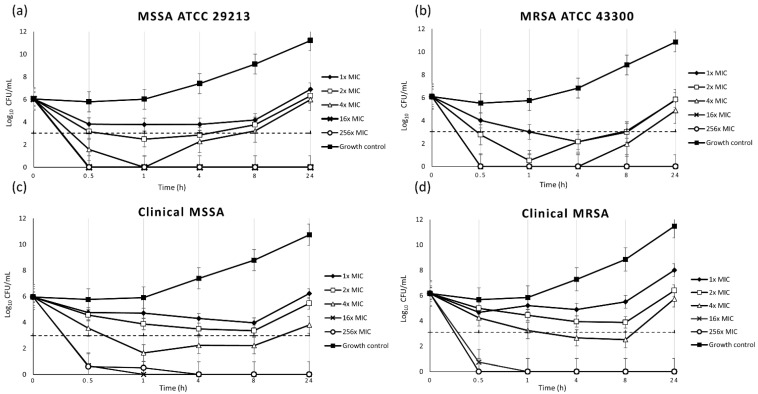
Time-kill kinetic investigations demonstrated a rapid bactericidal effect of sodium bituminosulfonate against MSSA and MRSA. Confirmation of the initial inoculum revealed a mean real bacterial density of 1.1 × 106 CFU/mL and 1.3 × 106 CFU/mL for the reference strains MSSA ATCC 29213 and MRSA ATCC 43300, respectively, 1 × 106 for clinical MSSA and 1.5 × 106 for clinical MRSA strains. At concentrations of 16 × MIC and 256 × MIC, a bactericidal efficacy of 99.9% inoculum reduction by sodium bituminosulfonate was already achieved after 30 min of incubation. Regrowth was observed at 1 × MIC, 2 × MIC and 4 × MIC within 4 to 24 h, whereas killing without regrowth was documented at 16 × MIC and 256 × MIC (Figure 1).
Figure 1.
Time-kill curves for sodium bituminosulfonate against two reference strains (a,b) and two clinical strains (c,d) of Staphylococcus aureus. The threshold (dashed line) denotes 99.9% decreases in CFU/mL. MSSA, methicillin-susceptible S. aureus; MRSA, methicillin-resistant S. aureus; MIC, minimal inhibitory concentration.
3. Discussion
S. aureus is one of the most common and important pathogens that can cause infections of skin and soft tissues, which are particularly difficult to treat when originating from methicillin-resistant strains [17]. Methicillin resistance in S. aureus is mediated by the mecA, mecB or mecC genes and leads to resistance to almost all β-lactam antibiotics [18,19,20,21]. Alternative antimicrobial substances may be important for the successful treatment of such infections or for the eradication of cutaneous colonization by S. aureus. Bituminosulfonate compounds have been known for over 100 years [22,23]. Data obtained from older studies—performed with various derivatives and formulations—showed good antimicrobial effects against Gram-positive bacteria, such as staphylococci and streptococci [24,25,26]. The activity of sodium bituminosulfonate against Gram-positive bacteria has recently been confirmed in an in vitro study [27]. Notably, another very recent study found only a low potential for resistance development in S. aureus after exposure to this derivate [28]. For comparison purposes, the antimicrobial inhibitory effect of sodium bituminosulfonate against S. aureus was also demonstrated in our study (Table 1). Its MIC values against 40 clinical and two reference S. aureus strains were found to be below the concentrations contained in commercially available preparations and the results were comparable to previous results [25,26,27,28]. The bactericidal efficacy of sodium bituminosulfonate was demonstrated by MBC determination. In agreement with international guidelines, a 99.9% killing of bacteria was considered as the criterion for a bactericidal effect [29]. To the best of our knowledge, no data are available on the rapidity of the bactericidal effect of sodium bituminosulfonate. Therefore, we characterized the bactericidal effect of sodium bituminosulfonate using a time-kill methodology [29,30]. In this first study of sodium bituminosulfonate’s bactericidity, a very rapid bactericidal effect against MSSA and MRSA was observed, with 99.9% of the inoculum already killed after a short incubation time of 30 min by concentrations corresponding to 16× MIC and 256× MIC (Figure 1). Regrowth—a phenomenon occasionally observed with the time-kill methodology [31,32]—was noted at lower concentrations of 1× MIC, 2× MIC and 4× MIC, while the higher concentrations of 16× MIC and 256× MIC caused irreversible killing. In conclusion, a bactericidal effect was demonstrated for sodium bituminosulfonate by MBC determination on a clinical collection of MSSA and MRSA strains. Detailed analyses of time-kill kinetics revealed very rapid bactericidal activity. This study contributes to the deeper in vitro characterization of the antimicrobial effects of sodium bituminosulfonate by investigating MBCs and time-kill curves under standardized conditions and has confirmed sodium bituminosulfonate as a promising alternative to commonly used topical antibiotics.
4. Materials and Methods
4.1. Bacterial Strains and Antimicrobial Substance
For the determination of minimal inhibitory concentrations (MICs) and minimal bactericidal concentrations (MBCs), 40 clinical isolates of S. aureus from routine diagnostics of the Friedrich Loeffler-Institute of Medical Microbiology, University Medicine Greifswald, in 2019–2021 were used, including 20 consecutive MSSA isolates and 20 consecutive MRSA isolates. The isolates were recovered from blood, urine, wounds, aspirates and respiratory samples. Only one isolate per patient was eligible. For time-kill experiments, two of these clinical strains (one MSSA and one MRSA) were used, as well as two reference strains (MSSA ATCC 29213 and MRSA ATCC 43300). The presence of mec genes in MRSA strains was confirmed using a loop-mediated isothermal amplification assay (eazyplex® MRSAplus, Amplex Diagnostics, Gars-Bahnhof, Germany) according to the user’s manual [33].
Sodium bituminosulfonate (Ichthyol® light) was provided by the Ichthyol-Gesellschaft Cordes, Hermanni & Co. (Hamburg, Germany).
4.2. Determination of MIC and MBC
For MIC determination, a broth microdilution method was used according to the recommendations of the Clinical and Laboratory Standards Institute (CLSI) and the International Organization for Standardization (ISO) [15,34,35]. The strains were cultivated overnight on Columbia blood agar plates at 35 °C. Afterwards, colony material from the overnight culture was adjusted to the turbidity standard of McFarland 0.5 in 0.9% saline. The cultures were diluted in cation-adjusted Mueller–Hinton broth (CA-MHB, BD Diagnostics, Heidelberg, Germany) to obtain a final test inoculum of 5 × 105 CFU/mL. The testing was performed in sterile U-bottom microtiter plates (Brand, Wertheim, Germany) with an incubation time of 18 ± 2 h at 35 °C in ambient air. Sodium bituminosulfonate was tested in double-dilution concentration steps ranging from 0.03 g/L to 256 g/L. As no quality control (QC) ranges exist for the susceptibility testing of sodium bituminosulfonate, MIC determination was additionally performed for S. aureus ATCC 29213 with vancomycin to control for the overall performance of the testing procedures.
For the determination of MBCs, 10 µL samples from the clear wells were sub-cultured on tryptic soy agar plates (TSA, BD Diagnostics, Heidelberg, Germany) and colonies were counted after overnight incubation at 35 °C. The minimal concentration needed to kill at least 99.9% of the initial inoculum was considered as the MBC, according to CLSI [29]. All MIC and MBC determinations were performed in triplicate and median values were calculated for analysis.
4.3. Time-Kill Curves
To determine the rapidity of the bactericidal effect of sodium bituminosulfonate against S. aureus, a time-kill kinetic methodology was used. The initial liquid culture prepared in 10 mL tryptic soy broth (TSB) from overnight growth on Columbia blood agar was incubated for 3 h at 35 °C and 160 rpm. After adjusting to the 0.5 McFarland turbidity standard and dilution, 5 mL of a suspension containing approximately 106 CFU/mL was transferred into glass flasks with different concentrations of sodium bituminosulfonate (1 × MIC, 2 × MIC, 4 × MIC, 16 × MIC and 256 × MIC for the respective isolate). The suspensions were incubated at 35 °C and 160 rpm for 0.5 h, 1 h, 4 h, 8 h and 24 h. After incubation, 200-µL samples were collected and serially diluted, followed by plating of 10 µL in triplicate on TSA plates. After overnight incubation at 35 °C, the colonies were counted, and average values were calculated. A growth control without antimicrobial substance, as well as a sterile control, were used in each experiment. The time-kill curves were performed in triplicate.
Acknowledgments
The authors are thankful to Katrin Darm, Betty Nedow, Annemarie Mawick and Claudia Wiede for their technical assistance. Parts of the study were presented as a poster at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) in 2021, online, (2977), and as an oral presentation at the Annual Meeting of the German Society for Hygiene and Microbiology (DGHM) in 2021, online (069/DKMV).
Author Contributions
Conceptualization, E.A.I. and K.B.; methodology, E.A.I. and E.H.; investigation, E.H.; data curation, E.H.; writing—original draft preparation, E.H.; writing—review and editing, E.A.I. and K.B.; project administration, E.A.I. and K.B.; funding acquisition, K.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data for the study are available in the article.
Conflicts of Interest
K.B. received a speaker fee from Ichthyol-Gesellschaft. E.H. and E.A.I. declare no conflict of interest.
Funding Statement
This research was funded by the Ichthyol-Gesellschaft Cordes, Hermanni & Co. (GmbH & Co. KG); Hamburg, Germany.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roca I., Akova M., Baquero F., Carlet J., Cavaleri M., Coenen S., Cohen J., Findlay D., Gyssens I., Heure O.E., et al. The global threat of antimicrobial resistance: Science for intervention. New Microbes New Infect. 2015;6:22–29. doi: 10.1016/j.nmni.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassini A., Högberg L.D., Plachouras D., Quattrocchi A., Hoxha A., Simonsen G.S., Colomb-Cotinat M., Kretzschmar M.E., Devleesschauwer B., Cecchini M., et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019;19:56–66. doi: 10.1016/S1473-3099(18)30605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McEwen S.A., Collignon P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018;6 doi: 10.1128/microbiolspec.ARBA-0009-2017. [DOI] [PubMed] [Google Scholar]
- 4.Tacconelli E., Carrara E., Savoldi A., Harbarth S., Mendelson M., Monnet D.L., Pulcini C., Kahlmeter G., Kluytmans J., Carmeli Y., et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018;18:318–327. doi: 10.1016/S1473-3099(17)30753-3. [DOI] [PubMed] [Google Scholar]
- 5.Murray C.J., Ikuta K.S., Sharara F., Swetschinski L., Aguilar G.R., Gray A., Han C., Bisignano C., Rao P., Wool E., et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler M.S., Gigante V., Sati H., Paulin S., Al-Sulaiman L., Rex J.H., Fernandes P., Arias C.A., Paul M., Thwaites G.E., et al. Analysis of the clinical pipeline of treatments for drug resistant bacterial infections: Despite progress, more action is needed. Antimicrob. Agents Chemother. 2022;63:e01991-21. doi: 10.1128/aac.01991-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization, editor. 2020 Antibacterial Agents in Clinical and Preclinical Development: An Overview and Analysis. WHO; Geneva, Switzerland: 2020. [Google Scholar]
- 8.Zayyad H., Eliakim-Raz N., Leibovici L., Paul M. Revival of old antibiotics: Needs, the state of evidence and expectations. Int. J. Antimicrob. Agents. 2017;49:536–541. doi: 10.1016/j.ijantimicag.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Theuretzbacher U., Paul M. Revival of old antibiotics: Structuring the re-development process to optimize usage. Clin. Microbiol. Infect. 2015;21:878–880. doi: 10.1016/j.cmi.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 10.Muller A.E., Theuretzbacher U., Mouton J.W. Use of old antibiotics now and in the future from a pharmacokinetic/pharmacodynamic perspective. Clin. Microbiol. Infect. 2015;21:881–885. doi: 10.1016/j.cmi.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Wernicke E.A. Schieferöl-Präparate. Münchener Med. Wochenzeitschr. 1936;13:522. (In German) [Google Scholar]
- 12.Korting H.C., Schöllmann C., Cholcha W., Wolff L. Efficacy and tolerability of pale sulfonated shale oil cream 4% in the treatment of mild to moderate atopic eczema in children: A multicentre, randomized vehicle-controlled trial. J. Eur. Acad. Dermatol. Venereol. 2010;24:1176–1182. doi: 10.1111/j.1468-3083.2010.03616.x. [DOI] [PubMed] [Google Scholar]
- 13.Beckert S., Warnecke J., Zelenkova H., Kovnerystyy O., Stege H., Cholcha W., Königsrainer A., Coerper S. Efficacy of topical pale sulfonated shale oil in the treatment of venous leg ulcers: A randomized, controlled, multicenter study. J. Vasc. Surg. 2006;43:94–100. doi: 10.1016/j.jvs.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 14.Weber G. Klinische Erfahrungen mit Ichtholan T; therapeutische Mitteilung. Arztl. Wochensch. 1954;9:521–522. [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute (CLSI) Performance Standards for Antimicrobial Susceptibility Testing. 31st ed. CLSI; Wayne, PA, USA: 2021. M100-S31. [Google Scholar]
- 16.The European Committee on Antimicrobial Susceptibility Testing . Routine and Extended Internal Quality Control for MIC Determination and Disk Diffusion as Recommended by EUCAST. EUCAST; Växjö, Sweden: 2021. [(accessed on 1 September 2021)]. Version 11.0. Available online: http://www.eucast.org. [Google Scholar]
- 17.Sunderkötter C., Becker K. Frequent bacterial skin and soft tissue infections: Diagnostic signs and treatment. J. Dtsch. Dermatol. Ges. 2015;13:501–524. doi: 10.1111/ddg.12721. [DOI] [PubMed] [Google Scholar]
- 18.Becker K., van Alen S., Idelevich E.A., Schleimer N., Seggewiß J., Mellmann A., Kaspar U., Peters G. Plasmid-Encoded Transferable mecB-Mediated Methicillin Resistance in Staphylococcus aureus. Emerg. Infect. Dis. 2018;24:242–248. doi: 10.3201/eid2402.171074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ubukata K., Nonoguchi R., Matsuhashi M., Konno M. Expression and inducibility in Staphylococcus aureus of the mecA gene, which encodes a methicillin-resistant S. aureus-specific penicillin-binding protein. J. Bacteriol. 1989;171:2882–2885. doi: 10.1128/jb.171.5.2882-2885.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcí a-Álvarez L., Holden M.T., Lindsay H., Webb C.R., Brown D.F., Curran M.D., Walpole E., Brooks K., Pickard D.J., Teale C., et al. Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: A descriptive study. Lancet Infect. Dis. 2011;11:595–603. doi: 10.1016/S1473-3099(11)70126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shore A.C., Deasy E.C., Slickers P., Brennan G., O’Connell B., Monecke S., Ehricht R., Coleman D.C. Detection of staphylococcal cassette chromosome mec type XI carrying highly divergent mecA, mecI, mecR1, blaZ, and ccr genes in human clinical isolates of clonal complex 130 methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2011;55:3765–3773. doi: 10.1128/AAC.00187-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baumann E., Schotten C. Über das “Ichthyol”. Mon. Prakt. Dermatol. 1883;2:257–262. (In German) [Google Scholar]
- 23.Unna P.G. Über Ichthyol. Mon. Prakt. Dermatol. 1897;25:533–539. (In German) [Google Scholar]
- 24.Latteux P. Bakteriologische Untersuchungen, die antiseptischen Eigenschaften des Ichthyols betreffend. Mon. Prakt. Dermatol. 1892;14:389–397. [Google Scholar]
- 25.Pantke R. Zur Kenntnis der Wirkung von Seefelder Schieferölprodukten auf Staphylococcen und Streptococcen (Action of Seefeld slate oil products on staphylococci and streptococci) Arzneim. Forsch. Drug Res. 1951;1:415–416. (In German) [PubMed] [Google Scholar]
- 26.Pantke R. Bakteriologische Untersuchung von Arzneimitteln aus Schieferöl (Bacteriological studies of drugs from shale oil) Arzneim. Forsch. Drug. Res. 1965;15:570–573. [PubMed] [Google Scholar]
- 27.Idelevich E.A., Becker K. In vitro activity of sodium bituminosulfonate: Susceptibility data for the revival of an old antimicrobial. Microb. Drug Resist. 2020;26:1405–1409. doi: 10.1089/mdr.2019.0390. [DOI] [PubMed] [Google Scholar]
- 28.Blisse M., Idelevich E., Becker K. Investigation of In-Vitro Adaptation toward Sodium Bituminosulfonate in Staphylococcus aureus. Microorganisms. 2020;8:1962. doi: 10.3390/microorganisms8121962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clinical and Laboratory Standards Institute (CLSI) Methods for Determining Bactericidal Activity of Antimicrobial Agents. CLSI; Wayne, PA, USA: 1999. Approved Guideline, CLSI Document M26-A. [Google Scholar]
- 30.Schleimer N., Kaspar U., Knaack D., von Eiff C., Molinaro S., Grallert H., Idelevich E.A., Becker K. In Vitro Activity of the Bacteriophage Endolysin HY-133 against Staphylococcus aureus Small-Colony Variants and Their Corresponding Wild Types. Int. J. Mol. Sci. 2019;20:716. doi: 10.3390/ijms20030716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tängdén T., Lundberg C.V., Friberg L.E., Huttner A. How preclinical infection models help define antibiotic doses in the clinic. Int. J. Antimicrob. Agents. 2020;56:106008. doi: 10.1016/j.ijantimicag.2020.106008. [DOI] [PubMed] [Google Scholar]
- 32.Kaspar U., Schleimer N., Idelevich E.A., Molinaro S., Becker K. Exploration of Bacterial Re-Growth as In Vitro Phenomenon Affecting Methods for Analysis of the Antimicrobial Activity of Chimeric Bacteriophage Endolysins. Microorganisms. 2022;10:445. doi: 10.3390/microorganisms10020445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leikeim R.S.M., Kesselmeier M., Löffler B., Rödel J., Höring S. Diagnostic accuracy and clinical impact of loop-mediated isothermal amplification for rapid detection of Staphylococcus aureus bacteremia: A retrospective observational study. Eur. J. Clin. Microbiol. Infect. Dis. 2020;39:679–688. doi: 10.1007/s10096-019-03773-y. [DOI] [PubMed] [Google Scholar]
- 34.Clinical and Laboratory Standards Institute (CLSI) Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically, Approved Standard. 11th ed. CLSI; Wayne, PA, USA: 2018. M07-A11. [Google Scholar]
- 35.Clinical Laboratory Testing and In Vitro Diagnostic Test Systems—Susceptibility Testing of Infectious Agents and Evaluation of Performance of Antimicrobial Susceptibility Test Devices—Part 1: Reference Method for Testing the In Vitro Activity of Antimicrobial Agents Against Rapidly Growing Aerobic Bacteria Involved in Infectious Diseases. ISO International Standard; Geneva, Switzerland: 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for the study are available in the article.