Abstract
High comorbidity rates, especially mental–physical comorbidity, constitute an increasing health care burden, with women and men being differentially affected. To gain an overview of comorbidity rates stratified by sex across a range of different conditions, this study examines comorbidity patterns within and between cardiovascular, pulmonary, skin, endocrine, digestive, urogenital, musculoskeletal, neurological diseases, and psychiatric conditions. Self-report data from the LifeGene cohort of 31,825 participants from the general Swedish population (62.5% female, 18–84 years) were analyzed. Pairwise comorbidity rates of 54 self-reported conditions in women and men and adjusted odds ratios (ORs) for their comparison were calculated. Overall, the rate of pairwise disease combinations with significant comorbidity was higher in women than men (14.36% vs. 9.40%). Among psychiatric conditions, this rate was considerably high, with 41.76% in women and 39.01% in men. The highest percentages of elevated mental–physical comorbidity in women were found for musculoskeletal diseases (21.43%), digestive diseases (20.71%), and skin diseases (13.39%); in men, for musculoskeletal diseases (14.29%), neurological diseases (11.22%), and digestive diseases (10%). Implications include the need for integrating mental and physical health care services and a shift from a disease-centered to an individualized, patient-centered focus in clinical care.
Keywords: comorbidity, health, sex, diseases, psychiatric, digestive, musculoskeletal, skin, neurological
1. Introduction
From a public health perspective, comorbidity is understood as the co-occurrence of two or more chronic medical conditions in the same individual [1,2]. Most estimates of comorbidity in primary care exceed 20% but range from 12.9 to 95.1%, depending on measurement methods and sample characteristics [3]. Individuals with comorbid conditions have more hospitalizations, greater functional decline, and increased mortality rates [4,5,6]. Co-/multimorbidity poses many challenges for clinical management, e.g., due to multi-drug therapy and possible drug-disease and drug-drug interactions [1,7,8,9]. Comorbidity is associated with increased health care costs [10] and challenges the organization of (specialized) healthcare delivery [11,12,13]. Moreover, comorbidity rates increase with age [3], and thus the associated health care burden is a growing problem in our aging societies.
For psychiatric conditions, comorbidity rates are known to be substantial [14]: 30% [15] to 40% or more [16,17] of individuals with a mental disorder (12-month prevalence) have two or more diagnoses. In addition, comorbidity and severity of psychiatric conditions are associated [16], and functional impairment and perceived unmet treatment are higher in individuals with comorbid mental disorders [15].
Another increasingly recognized problem is the high comorbidity between psychiatric conditions and physical diseases [18,19,20,21,22,23,24]. The diagnosis of comorbid psychiatric disorders in chronic physical illness can be difficult [25,26,27], and interactions between mental-physical comorbidity can negatively affect the respective treatment outcomes [24,28,29,30]. Excess mortality in people with mental illness across different diagnostic groups [31] is largely related to comorbid medical diseases [32], for which they are less likely to receive standard treatment [19,33].
The identification of frequent comorbidity patterns is important for the planning of health care organization and delivery [3,34,35,36]. Women have generally been found to have higher co-/multimorbidity rates [3,36,37,38,39,40], and sex-specific patterns have been observed [3,37,39,41,42,43]. The leading causes of disability-adjusted life-years also differ by sex [44]. This highlights the importance of investigating sex differences with regard to comorbidity patterns.
This exploratory study aims to investigate pairwise comorbidity rates of 54 self-reported conditions in women and men of the general population to identify sex-specific combinations and patterns of elevated comorbidity across a broad spectrum of conditions: comorbidity within and between cardiovascular diseases, pulmonary diseases, skin diseases, endocrine diseases, digestive diseases, urogenital diseases, musculoskeletal diseases, neurological diseases, and psychiatric conditions. The present analysis investigates pairwise comorbidity (two conditions) instead of multimorbidity to obtain an overview of comorbidity patterns—with a focus on mental–physical comorbidity—and to identify specific comorbidity combinations at the same time. Overall, generally high comorbidity of psychiatric conditions and between psychiatric conditions and physical diseases as well as sex-specific comorbidity patterns are expected.
2. Materials and Methods
2.1. Sample Description
For this study, web-based cross-sectional survey data from the LifeGene cohort collected between 2009 and 2016 in the general Swedish population were used. The recruitment process of LifeGene has been described elsewhere; inclusion criteria were residence in Sweden and recruitment-specific age criteria [45,46]. Information on the past or present occurrence of conditions was selected from the “medical history” module of the LifeGene survey. The tinnitus subsample (N = 7615) has been analyzed by our group in two previous studies [47,48].
From the available data including N = 31,927 participants, 102 participants were excluded from the present study due to being under the age of 18 (N = 68), missing age data (N = 2), or missing data on self-reported diseases (N = 32), leading to the final sample size of N = 31,825 participants.
Descriptive characteristics of the study sample can be found in Table 1. On average, the participants were 35.17 years old (SD = 11.27 years, range = 18–84 years), and 19,876 participants (62.45%) were female. This project was approved by the local ethics committee “Regionala etikprövningsnämnden” in Stockholm (2021-05652-01).
Table 1.
Sample characteristics (N = 31,825).
| Variable | M/N | SD/% |
|---|---|---|
| Age | 35.17 | 11.27 |
| Sex | ||
| Female | 19,876 | 62.45 |
| Male | 11,949 | 37.55 |
| Marital status | ||
| Married | 8047 | 25.29 |
| Cohabiting | 11,098 | 34.87 |
| Single | 7585 | 23.83 |
| Separated/divorced | 1223 | 3.84 |
| Living apart | 3033 | 9.53 |
| Widowed | 111 | 0.35 |
| Same-sex marriage | 14 | 0.04 |
| Missing | 714 | 2.24 |
| Education 1 | ||
| 9-year primary school | 612 | 1.92 |
| Secondary school | 7167 | 22.52 |
| University | 21,087 | 66.26 |
| Missing | 2959 | 9.30 |
| Employment status | ||
| Employed | 18,097 | 56.86 |
| Unemployed | 750 | 2.36 |
| Self-employed 2 | 2325 | 7.31 |
| Age pension | 703 | 2.21 |
| Early retirement 3 | 167 | 0.52 |
| Sick leave | 165 | 0.52 |
| Parental leave | 916 | 2.88 |
| Student | 4626 | 14.54 |
| On leave | 48 | 0.15 |
| Housewife/man | 64 | 0.20 |
| Other | 390 | 1.23 |
| Missing | 3574 | 11.23 |
| Smoking | ||
| Never | 20,600 | 64.73 |
| Ex-smoker | 8350 | 26.24 |
| Current smoker | 2303 | 7.24 |
| Missing | 572 | 1.80 |
| BMI (N = 31,163) | 20.87 | 2.94 |
1 Highest or current education level. 2 Running owned or part-owned company. 3 Early retirement due to illness/disability (activity or sickness benefit). Abbreviations: M = mean; N = number of cases; SD = standard deviation.
2.2. Data (LifeGene Survey)
Analyses were performed separately based on the indicated sex of the study participant in the survey (male/female). The investigated variables included the past or present occurrence of 55 different self-reported conditions overall (54 in each sex). All conditions except tinnitus were assessed by the survey question, “Which of the following diseases do you currently have or have you had?”. This question was asked twice with different response options (disease questions 1 and 2).
Disease question 1 included the following options: six ‘heart/vessel’ diseases: hypertension, hyperlipidemia, angina pectoris, myocardial infarction, cardiac arrhythmia, and thrombosis, labeled in the present study as cardiovascular diseases; two ‘pulmonary diseases’: asthma and chronic obstructive pulmonary disease (COPD); four ‘skin’ diseases: herpes, acne, eczema, and psoriasis; two ‘endocrine diseases’: diabetes and thyroid disease; ten ‘stomach’ diseases: Celiac disease, lactose intolerance, gastric acid reflux, stomach ulcer, gastritis, gallbladder problems, irritable bowel syndrome (IBS), Crohn′s disease, ulcerative colitis, and fecal incontinence, labeled in the present study as digestive diseases; and three ‘urology’ diseases: recurring urinary tract infections (UTI), prostate problems, and kidney stones, labeled in the present study as urogenital diseases. No data were missing on disease question 1.
Disease question 2 included the following options: seven ‘musculoskeletal diseases’: sciatica, chronic back pain, chronic shoulder pain, osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus (SLE), and fibromyalgia; six ‘neurology’ diseases, to which bothersome tinnitus was added (see below): dyslexia, migraine, Horton′s syndrome, Meniere′s disease, epilepsy, and multiple sclerosis (MS); two ‘children and youth’ diseases: chickenpox and infectious mononucleosis (IM), which were not included in the present study; and fourteen ‘psychiatry’ diseases: burnout, depression, bipolar disease, generalized anxiety disorder/syndrome (GAD), panic disorder, agoraphobia, social anxiety, obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), schizophrenia, schizoaffective disorder, Asperger′s syndrome, autism, and Tourette’s syndrome, labeled in the present study as psychiatric conditions. On disease question 2, data were missing from 6 participants.
Tinnitus was assessed by the question: “Is there a constant ringing in the ears or do you have any other bothersome sound in the ears (tinnitus)?” No data were missing on this question. Only the response option “all the time, the sound is very bothersome” was included as “bothersome tinnitus” in the analysis (as opposed to “sometimes, but the sound doesn′t bother me”), as only this category was considered to represent individuals with clinically relevant tinnitus (tinnitus disorder) [49]. Bothersome tinnitus was added to the group of neurological diseases.
Age, education, employment, body mass index (BMI), and smoking were included as covariates in the statistical analysis. For education, the response options “don′t know/don′t want to answer” and “other” were set to missing; the variable with the remaining categories of “nine-year primary school”, “secondary school”, and “university” was treated as an ordered factor. Information on education was missing from N = 2959 participants. For employment, the response option “don′t know/don′t want to answer” was set to missing. The remaining options were recoded into the following categories: 1 = employed or self-employed; 2 = unemployed; 3 = on (sick or parental) leave or age pension or early retirement due to illness/disability; 4 = student; 5 = houseman/wife or other. Employment information was missing from N = 3574 participants. The covariate smoking was created with the categories 1 = non-smoker (never or occasionally), 2 = ex-smoker and 3 = current smoker. Information on smoking was missing from N = 572 participants. For the BMI, information was missing for N = 662 participants.
2.3. Statistical Analysis
The data were analyzed using R-4.0.0 [50]. Analyses were performed separately for each sex and included the comparison of pairwise comorbidity rates against the respective prevalence rates of each index condition using odds ratios (OR) obtained from age-, education-, employment-, BMI-, and smoking-adjusted logistic regression models.
Two prevalence rates (%) were calculated (separately for women and men) for each pairwise comorbidity combination, one for each condition as the respective index condition (prevalence rate of condition A given condition B, and prevalence rate of condition B given condition A). ORs with 95% confidence intervals (CIs) were calculated based on age-, education-, employment-, BMI-, and smoking-adjusted logistic regression models (separately for women and men) to determine whether comorbidity rates were elevated in comparison to the index condition prevalence rates. ORs designate the ratio of the odds of condition A among cases with index condition B to the odds of condition A in cases without index condition B. Two ORs were calculated for each pairwise comorbidity combination, one for each condition as the respective index condition.
For female participants, the condition ‘prostate problems’ was not applicable; for male participants, the condition ‘SLE’ was removed due to zero cases, resulting in 54 diseases for both analyses (2862 comorbidity combinations each), which led to 5724 tests in total. Correspondingly, p-values were adjusted for multiple testing (Bonferroni correction) with p < 0.05/5724 as the applied significance level.
3. Results
3.1. Sample Description
Characteristics of the study sample are summarized in Table 1.
3.2. Prevalence Rates
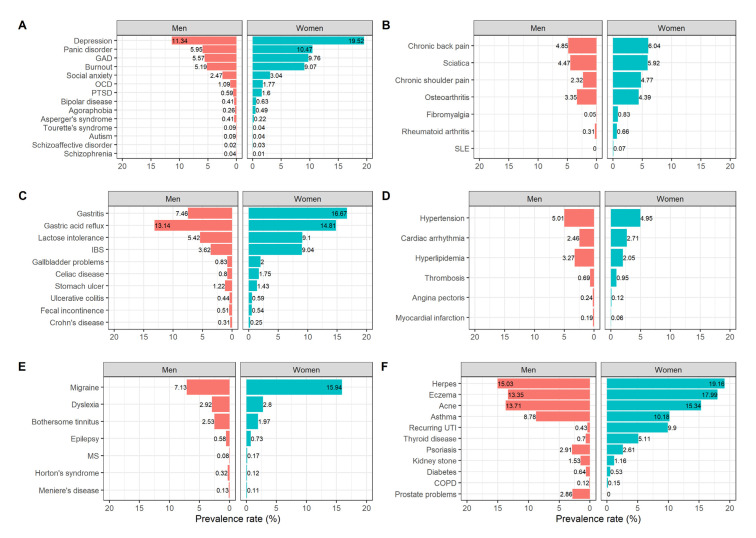
Prevalence rates of psychiatric conditions, musculoskeletal diseases, digestive diseases, cardiovascular diseases, neurological diseases, skin diseases, pulmonary diseases, urogenital diseases, and endocrine diseases in female and male participants are shown in Figure 1. The five conditions with the highest prevalence rates in women were: depression (19.52%), herpes (19.16%), eczema (17.99%), gastritis (16.67%), and migraine (15.94%); in men: herpes (15.03%), acne (13.71%), eczema (13.35%), gastric acid reflux (13.14%), and depression (11.34%).
Figure 1.
Prevalence rates (%) of psychiatric conditions (A), musculoskeletal diseases (B), digestive diseases (C), cardiovascular diseases (D), neurological diseases (E), and skin/pulmonary/urogenital/endocrine diseases (F) in male (N = 11,949) and female (N = 19,876) participants. Abbreviations: COPD = Chronic Obstructive Pulmonary Disease, IBS = Irritable Bowel Syndrome, UTI = Urinary Tract Infections, SLE = Systemic Lupus Erythematosus, MS = Multiple Sclerosis, GAD = Generalized Anxiety Disorder, OCD = Obsessive-Compulsive Disorder, PTSD = Posttraumatic Stress Disorder.
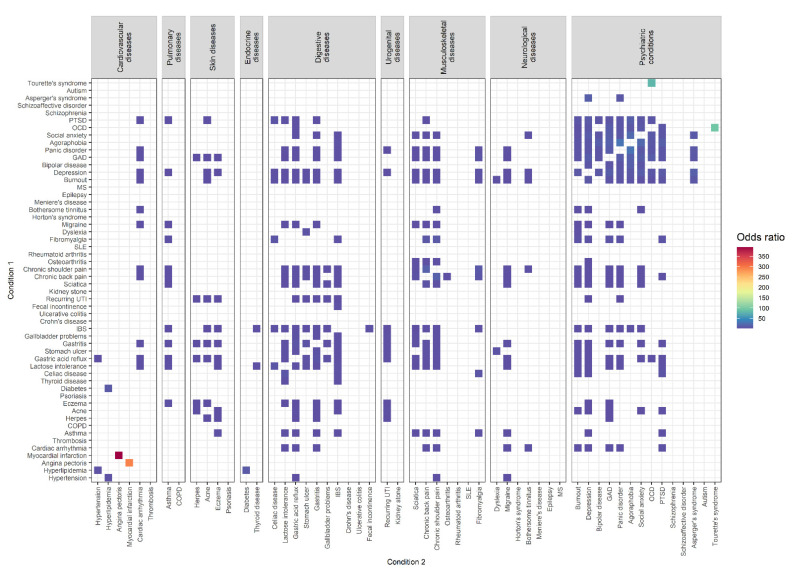
3.3. Comorbidity Combinations in Female Participants
Comorbidity combinations with increased ORs in female participants (N = 19,876) can be found in Figure 2. In total, 411 of the 2862 comorbidity combinations (14.36%) had significantly increased ORs. The results of all significantly increased comorbidity combinations in female participants can be found in Supplementary Table S1.
Figure 2.
Comorbidity combinations of 54 conditions with increased odds ratios (p < 0.05/5724) in female participants (N = 19,876) based on the results of age-, education-, employment-, BMI-, and smoking-adjusted logistic regression analysis.
The three combinations of comorbid conditions with the highest ORs were: angina pectoris among individuals with myocardial infarction (prevalence: 45.45%, OR = 394.14 [65.70, 2717.42])/myocardial infarction among individuals with angina pectoris (prevalence: 20.83%, OR = 293.83 [51.49, 1908.90]), Tourette’s syndrome among individuals with OCD (prevalence: 0.85%, OR = 94.38 [13.27, 658.78])/OCD among individuals with Tourette’s syndrome (prevalence: 42.86%, OR = 79.86 [12.88, 503.13]), and panic disorder among individuals with agoraphobia (prevalence: 82.65%, OR = 29.95 [16.82, 56.91])/agoraphobia among individuals with panic disorder (prevalence: 3.89%, OR = 29.61 [16.69, 56.09]).
Among diseases of the same group, elevated comorbidity combinations were found for skin diseases (50%; 6 of 12), psychiatric conditions (41.76%; 76 of 182), digestive diseases (35.56%; 32 of 90), musculoskeletal diseases (33.33%; 14 of 42), and cardiovascular diseases (13.33%; 4 of 30).
Between diseases of different groups, elevated comorbidity combinations were found for urogenital and skin diseases (37.50%; 6 of 16), musculoskeletal and pulmonary diseases (28.57%; 8 of 28), musculoskeletal and digestive diseases (25.71%, 36 of 140), urogenital and digestive diseases (25%; 10 of 40), digestive and skin diseases (22.50%; 18 of 80), psychiatric conditions and musculoskeletal diseases (21.43%; 42 of 196), psychiatric conditions and digestive diseases (20.71%; 58 of 280), digestive and pulmonary diseases (20%; 8 of 40), psychiatric conditions and skin diseases (13.39%, 15 of 112), skin and pulmonary diseases (12.50%; 2 of 16), digestive and endocrine diseases (10%; 4 of 40), endocrine and cardiovascular diseases (8.33%; 2 of 24), psychiatric conditions and neurological diseases (8.16%; 16 of 196), neurological and musculoskeletal diseases (8.16%; 8 of 98), psychiatric conditions and pulmonary diseases (7.14%, 4 of 56), psychiatric conditions and urogenital diseases (7.14%; 4 of 56), neurological and pulmonary diseases (7.14%, 2 of 28), digestive and cardiovascular diseases (6.67%; 8 of 120), neurological and cardiovascular diseases (5.95%; 5 of 84), musculoskeletal and cardiovascular diseases (5.95%; 5 of 84), psychiatric conditions and cardiovascular diseases (5.95%; 10 of 168), and neurological and digestive diseases (5.71%, 8 of 140).
Thus, the three highest percentages of elevated mental–physical comorbidity combinations were found for psychiatric conditions and musculoskeletal diseases (21.43%), psychiatric conditions and digestive diseases (20.71%), and psychiatric conditions and skin diseases (13.39%). The overall mental–physical comorbidity rate in female participants was 13.30% (149 of 1120).
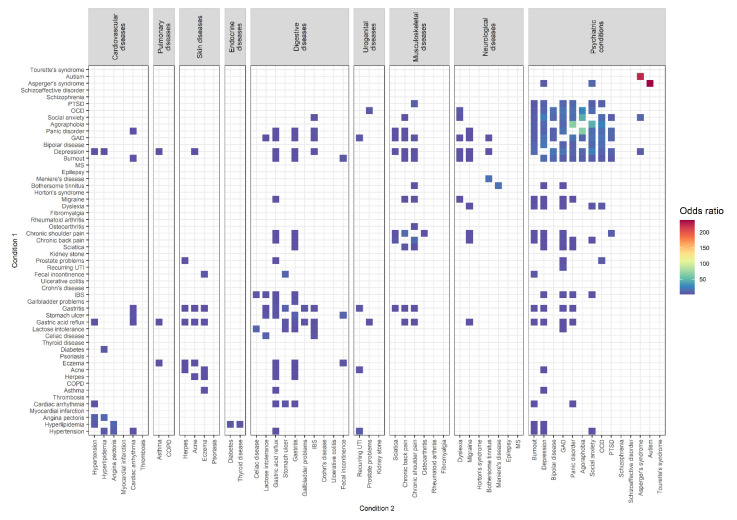
3.4. Comorbidity Combinations in Male Participants
Comorbidity combinations with increased ORs in male participants (N = 11,949) can be found in Figure 3. In total, 269 of the 2862 comorbidity combinations (9.40%) had significantly increased ORs. The results of all significantly-elevated comorbidity combinations in male participants can be found in Supplementary Table S2.
Figure 3.
Comorbidity combinations of 54 conditions with increased odds ratios (p < 0.05/5724) in male participants (N = 11,949) based on the results of age-, education-, employment-, BMI-, and smoking-adjusted logistic regression analysis.
The three combinations of comorbid conditions with the highest ORs were: autism among individuals with Asperger’s syndrome (prevalence: 12.24%, OR = 239.05 [20.33, 2127.42])/Asperger’s syndrome among individuals with autism (prevalence: 54.55%, OR = 224.58 [22.00, 2157.84]), panic disorder among individuals with agoraphobia (prevalence: 80.65%, OR = 66.54 [26.61, 202.10])/agoraphobia among individuals with panic disorder (prevalence: 3.52%, OR = 65.79 [26.38, 199.46]), and social anxiety among individuals with agoraphobia (prevalence: 51.61%, OR = 46.10 [20.46, 104.42])/agoraphobia among individuals with social anxiety (prevalence: 5.42%, OR = 45.43 [20.50, 101.31]).
Among diseases of the same group, elevated comorbidity combinations were found for skin diseases (50%; 6 of 12), psychiatric conditions (39.01%; 71 of 182), digestive diseases (28.89%; 26 of 90), musculoskeletal diseases (26.67%; 8 of 30), cardiovascular diseases (26.67%; 8 of 30), and neurological diseases (9.52%; 4 of 42).
Between diseases of different groups, elevated comorbidity combinations were found for skin diseases and digestive diseases (17.5%; 14 of 80), psychiatric conditions and musculoskeletal diseases (14.29%; 24 of 168), endocrine diseases and cardiovascular diseases (12.50%; 3 of 24), skin diseases and pulmonary diseases (12.5%; 2 of 16), psychiatric conditions and neurological diseases (11.22%; 22 of 196), psychiatric conditions and digestive diseases (10%; 28 of 280), musculoskeletal diseases and digestive diseases (8.33%; 10 of 120), urogenital diseases and skin diseases (8.33%; 2 of 24), digestive diseases and cardiovascular diseases (6.67%; 8 of 120), psychiatric conditions and cardiovascular diseases (6.55%; 11 of 168), psychiatric conditions and urogenital diseases (5.95%; 5 of 84), neurological diseases and musculoskeletal diseases (5.95%; 5 of 84), urogenital diseases and digestive diseases (5%; 3 of 60), digestive diseases and pulmonary diseases (5%; 2 of 40) psychiatric conditions and pulmonary diseases (3.57%; 2 of 56), urogenital diseases and cardiovascular diseases (2.78%; 1 of 36), psychiatric conditions and skin diseases (1.79%; 2 of 112), and neurological diseases and digestive diseases (1.43%; 2 of 140).
Thus, the three highest percentages of elevated mental–physical comorbidity combinations were found for psychiatric conditions and musculoskeletal diseases (14.29%), psychiatric conditions and neurological diseases (11.22%), and psychiatric conditions and digestive diseases (10%). The overall mental–physical comorbidity rate in male participants was 8.39% (94 of 1120).
4. Discussion
The present study investigated pairwise comorbidity rates of 54 self-reported conditions in women and men of the LifeGene cohort from the Swedish general population, including cardiovascular diseases, pulmonary diseases, skin diseases, endocrine diseases, digestive diseases, urogenital diseases, musculoskeletal diseases, neurological diseases, and psychiatric conditions. Overall, a higher percentage of significantly increased pairwise comorbidity combinations were found in women than in men (14.36% vs. 9.40%). The percentage of significantly increased pairwise comorbidity combinations between the studied psychiatric conditions was 41.76% in women and 39.01% in men. For mental–physical comorbidity, this rate was 13.30% in women and 8.39% in men. In women, the three highest percentages of elevated comorbidity with psychiatric conditions were found for musculoskeletal diseases (21.43%), digestive diseases (20.71%), and skin diseases (13.39%). For men, the three highest percentages of elevated psychiatric comorbidity were found for musculoskeletal diseases (14.29%), neurological diseases (11.22%), and digestive diseases (10%).
These findings are difficult to compare with previous studies on co-/multimorbidity [35,36,51]. However, two partially overlapping systematic reviews identified three main comorbidity patterns: comorbidity of cardiovascular and metabolic diseases, comorbidity of mental health problems (with each other or with organic diseases), and comorbidity of musculoskeletal or pain diseases (with each other or with other diseases) [3,22]. While the first pattern was less pronounced in our sample, the two other patterns were present in both sexes. Furthermore, an additional comorbidity pattern was observed here, involving digestive system disorders (with each other or with other diseases).
In line with our result, women have often been found to have higher rates of co-/multimorbidity than men [1,3,36,37,38,39,40]. A strong sex-specific finding observed here was the greatly increased comorbidity between angina and myocardial infarction in female participants (OR > 290), which was not present in men. Some findings report an increased risk for women to develop angina pectoris after myocardial infarction [52,53]. However, this relationship appears to be confounded by medical factors [53,54], which might also be possible for our observation.
The analyses were corrected for age, education, employment, BMI, and smoking. However, other factors such as environmental or socioeconomic characteristics which can increase the risk for co-/multimorbidity [1] might have influenced the results. Other limiting factors for the present analysis include the lack of temporal information and the use of self-report data as opposed to confirmed medical diagnoses, which may have introduced bias. Thus, the results need to be interpreted with caution.
4.1. Comorbidity between Psychiatric Conditions
As expected, the degree of comorbidity among psychiatric conditions was high, in line with the literature [14,15,16], particularly regarding the high comorbidity between depression/mood disorders and anxiety disorders [3,22,36]. In women, comorbidity between OCD and Tourette’s syndrome and between agoraphobia and panic disorder was among the three most highly elevated comorbidity combinations. In men, comorbidity between Asperger’s syndrome and autism, panic disorder and agoraphobia, and social anxiety and agoraphobia were the three most highly elevated comorbidity combinations. However, the precision of OR estimates of conditions with low prevalence rates—such as Tourette’s syndrome, agoraphobia, Asperger’s syndrome, and autism—need to be interpreted with caution.
Tourette syndrome is known to be frequently associated with obsessive-compulsive behavior or OCD [55,56], and consistent with our results, higher rates of comorbid OCD were found in females with Tourette syndrome [55]. By the newest classifications, autism and Asperger’s syndrome are not considered separate diagnoses but are conceptualized to belong to the broader group of autism spectrum disorder (ASD) [57]. In children, the prevalence of ASD is markedly higher in boys than in girls [58]. Thus, the highly increased comorbidity between Asperger’s syndrome and autism observed here in men is not surprising. The comorbidity of agoraphobia and panic disorder was high in both women and men. There is disagreement in the literature as to whether agoraphobia is indeed a frequent comorbidity of panic disorder or whether it should be conceptualized as a consequence of it [59]. However, there are indications that panic disorder can be primarily characterized as distress disorder and agoraphobia as a fear disorder [59].
4.2. Comorbidity between Psychiatric and Physical Conditions
4.2.1. Psychiatric-Musculoskeletal Comorbidity
Comorbidity between psychiatric conditions and musculoskeletal diseases was the most common type of mental–physical comorbidity in both sexes, but with higher rates in women than men (21.43% vs. 14.29%). Respective combinations were mostly found for sciatica, chronic shoulder or back pain (both sexes), and in women, additionally for fibromyalgia (chronic, widespread musculoskeletal pain) with mood and anxiety disorders (burnout, depression, GAD, panic disorder, social anxiety, and PTSD).
In the literature, anxiety and depression have been identified as risk factors for sciatica [60,61]. Moreover, associations of fibromyalgia [62,63,64,65,66] and chronic back/shoulder pain [62,67,68,69,70,71] with mood and anxiety disorders are well-known, and interacting biopsychosocial influences appear important for their co-occurrence [72,73]. The relationship between mood/anxiety disorders and musculoskeletal pain is thought to be bidirectional [66,72,73,74,75], with both groups of conditions constituting a risk factor for the other. For the association between depression and chronic pain, predisposing genetic factors and different neurobiological mechanisms [66,72,76,77], including neuroplasticity changes [78] or neuroinflammation [79], as well as overlapping psychosocial factors [72] are assumed.
4.2.2. Psychiatric-Digestive Comorbidity
The high comorbidity observed here between psychiatric conditions and diseases of the digestive system is consistent with the literature [80,81]. In men, psychiatric–digestive comorbidity (10%) was mainly present between gastric acid reflux, gastritis, and IBS with mood and anxiety disorders (burnout, depression, GAD, panic disorder, social anxiety). In women, on the other hand, more associations were present in total (20.71%). In addition to associations shared with men (of gastric acid reflux, gastritis, and IBS), they included associations of Celiac disease, lactose intolerance, and stomach ulcer with mood and anxiety disorders.
Concerning the temporal relationships of psychiatric–digestive comorbidity, affective disorders were found to precede the onset of certain digestive system diseases [80]. In contrast, in a population-based study, anxiety and depression were only found to precede the onset of functional gastrointestinal disorders in one-third of the cases, while for two-thirds, functional gastrointestinal disorders preceded the mental conditions [82]. Overall, the temporal association seems clear for some specific disease combinations, e.g., mood/anxiety disorders increase the risk for stomach ulcers [23,83,84], but for others, particularly functional gastrointestinal disorders, the relationship appears to be bidirectional. Not surprisingly, complex interactions between psychosocial factors and gastrointestinal symptoms are known for functional gastrointestinal disorders such as IBS [85,86]. Possible explanations for psychiatric-digestive comorbidity might lie in the microbiota–gut–brain axis, the bidirectional communication between the gut microbiota and the central nervous system [81]. Research on the microbiota–gut–brain axis suggests a link between gut microbiota and functional gastrointestinal disorders, such as IBS [81,86], as well as psychiatric conditions, such as depression [81,87].
4.2.3. Psychiatric-Dermatological Comorbidity
In women, the comorbidity of psychiatric conditions and skin diseases (13.39%) was markedly higher than in men (1.79%). In men, the only significantly increased psychiatric-dermatological comorbidity association was found for acne and depression. In women, acne was additionally associated with burnout, GAD, and PTSD, and additional associations were found for herpes (with GAD) and eczema (with depression and GAD).
A recent meta-analysis showed significant associations of acne with depression and anxiety [88]. The influence of sex was not investigated in this meta-analysis, but there are some indications that women with acne tend to have more psychological difficulties than men [89]. High comorbidity of psychiatric conditions in patients with atopic eczema has been observed previously [90,91]. While Kauppi et al. [90] observed a higher risk for anxiety disorders in women with atopic eczema than men, but not for other psychiatric conditions, Schmitt et al. [91] found psychiatric comorbidity in atopic eczema to be independent of sex.
Psychosocial factors may be involved in the development of skin diseases [92]. Anxiety disorders have been found to precede the onset of certain skin diseases [34]. On the other hand, skin diseases can lead to psychological problems [89,92,93]. Therefore, the relationship between psychiatric conditions and skin diseases seems to be bidirectional [92]. Overall, sex differences regarding psychiatric-dermatological comorbidity require further research.
4.2.4. Psychiatric-Neurological Comorbidity
In men, neurological diseases were the third most common group with increased psychiatric comorbidity (11.22%). In women, they were the fourth most common group (8.16%). In both sexes, significantly increased comorbidity associations were found for migraine, dyslexia, and bothersome tinnitus with mood and anxiety disorders.
The biggest sex difference was present for dyslexia. In women, it was only associated with burnout, while in men, it was additionally associated with depression, GAD, social anxiety, and OCD. Sex differences in dyslexia include higher rates in boys than girls [94], as well as potential differences in behavior, neuroanatomy, and genetics [95]. Dyslexia and emotional problems frequently co-occur [96,97]. In contrast to our results, some studies observed higher anxiety levels in dyslexic females [98,99], but further research on this topic is needed.
4.3. Biopsychosocial Causes for Mental–Physical Comorbidity
Overall, the observed elevated comorbidity between psychiatric conditions (mood/anxiety disorders) and physical diseases (digestive, musculoskeletal, skin, and neurological) is likely related to shared and interacting biopsychosocial influences. For example, shared predisposing genetic and environmental factors, chronic stress, immune abnormalities, and psychosocial factors seem related to fibromyalgia, IBS, and depression [77]. Overall, the effects of biological, psychological, behavioral, and social factors on mental–physical comorbidity are often interrelated [26]. Examples of shared and interacting biopsychosocial risk factors for mental-physical comorbidity, especially for functional somatic syndromes, include early life stress/chronic stress, somatization, and health-compromising behaviors.
The biological and mental consequences of early life stress and/or chronic stress experiences seem implicated in many of the identified comorbidity patterns. Stress can be associated with the onset or exacerbation of functional somatic syndromes such as IBS [86,100,101] and fibromyalgia [66,102]. For some psychiatric conditions such as PTSD and depression, stress has a central pathogenic role [103,104], but early life stress, such as childhood maltreatment, appears relevant for psychopathology in general [105,106]. Multiple adverse experiences in childhood are associated with an increased risk of developing mental health problems and major physical diseases later in life and also show associations with health-compromising behavior, e.g., problematic alcohol or drug use [107,108]. Moreover, chronic stress leads to widespread biological changes, such as persistent neuroendocrine or immune dysregulation, which increase the susceptibility to a range of physical diseases [109].
Following traumatic events, stress reactions and somatization symptoms are interlinked [110]. Somatization is a risk factor for functional somatic syndromes [111,112] and is related to higher anxiety or depression levels in these patients [113]. In addition, somatization is related to increased functional disability in primary care patients independent of psychiatric and medical comorbidity [114].
Moreover, psychiatric conditions are associated with lifestyle factors that have detrimental effects on physical health, such as smoking, heavy drinking, reduced activity, poor diet, and obesity [21,26,29,33]. In addition, socioeconomic factors, namely low education levels and living in a deprived area, have been identified as risk factors for multimorbidity [115]. Next to more direct effects such as access to medical care, lower socioeconomic status seems to negatively affect health through greater stress and more health-compromising behaviors [116]. Consequently, influences of stress, somatization, and social and behavioral factors on mental and physical health are highly interrelated.
4.4. Limitations
This study has some limitations. First, the cross-sectional design provides neither causal nor temporal information regarding the identified comorbidity patterns. Moreover, it is important to note that the assessed comorbidity does not necessarily mean that the conditions were present in an individual at the same time, as the survey question did not differentiate between past and present occurrences. A second limitation concerns the data source. The use of self-report disease data without medical verification of the diagnoses by health care professionals can question their reliability. However, even though the correspondence between self-report data and health administrative data is generally low, it also varies strongly and is high for some diseases, e.g., for diabetes and hypertension [117,118]. Comorbidity or multimorbidity estimates derived from self-report are often higher than those from health administrative data [117,119], but self-report data might be more sensitive for the detection of symptoms-based conditions [119]. Third, a recall bias or a bias caused by psychological influences on response tendencies could be present, e.g., due to somatization. Fourth, a selection bias regarding the sample or the included conditions cannot be excluded. Information on other diseases, such as different cancer types, was not available for the analysis but would have constituted important variables of interest [120,121]. Fifth, the analyses were performed separately based on the indicated sex, but information on sexual orientation was missing. However, multimorbidity was found to be increased among sexual minorities [122,123], and respective effects could not be considered in the present study. Finally, this study focused on the comorbidity of two conditions, although multimorbidity is a common phenomenon for many patients. Therefore, the observed bivariate associations between conditions do not necessarily reflect direct associations, as they could be caused by shared comorbidity with other conditions. However, the bivariate approach allowed us to quantify the comorbidity rates of specific disease combinations, which would not have been possible with broader multimorbidity clusters.
4.5. Implications
Research into shared and modifiable risk factors of frequent (sex-specific) comorbidity patterns is important for prevention and improving clinical care. Based on the high observed mental–physical comorbidity, the need for better integration of mental and physical health care services is apparent, as discussed by others [28,29,33]. Interacting effects between comorbid conditions on the respective treatment and prognosis can render the clinical management of patients with co-/multimorbidity more complex [2,33,124]. Therefore, clinical guidelines are often not applicable to patients with multiple comorbid conditions [2,125,126]. Consequently, for the clinical assessment and management of these patients, a shift from the current disease-oriented approach to a more patient-centered, individualized approach is needed [2,125,126,127]. A patient-centered approach for co-/multimorbidity management should take a holistic, biopsychosocial perspective [126], integrate and coordinate the delivery of health care across disciplines [125,127], and involve shared decision making in tailoring treatment to the individual [125,127]. Different initiatives to increase patient-centredness in co-/multimorbidity care are currently being applied, which could reflect a possible beginning in this needed transition [127].
5. Conclusions
The present study investigated pairwise comorbidity rates of 54 self-reported conditions in women and men of the LifeGene cohort from the Swedish general population adjusted for age, education, employment, BMI, and smoking. Overall, a higher percentage of significantly increased pairwise comorbidity combinations were found in women than in men (14.36% vs. 9.40%). The comorbidity between psychiatric conditions was considerably high in both women and men (41.76% vs. 39.01%), and highest between OCD and Tourette’s syndrome (women only), Asperger’s syndrome and autism (men only), agoraphobia and panic disorder (both), social anxiety and agoraphobia (both). For mental–physical comorbidity (women: 13.30%; men: 8.39%), the three groups with the highest elevated psychiatric comorbidity in women were musculoskeletal (21.43%), digestive (20.71%), and skin diseases (13.39%); in men, musculoskeletal (14.29%), neurological (11.22%), and digestive diseases (10%). Overlap and interactions between biopsychosocial risk factors appear relevant for the identified mental–physical comorbidity patterns, including, but not limited to, influences of chronic or early life stress, somatization, and health-compromising behavior. Limitations of the present study included the absence of any temporal information and the use of self-report data. The results implicate the need for a more integrated mental–physical health care approach and improved patient-centered treatment.
Acknowledgments
The authors thank Nancy Pedersen, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden, for sharing the LifeGene data.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biom12070949/s1, Table S1: Significantly elevated comorbidity combinations (p < 0.05/5724) in female participants (N = 19,876) sorted by odds ratio; Table S2: Significantly elevated comorbidity combinations (p < 0.05/5724) in male participants (N = 11,960) sorted by odds ratio.
Author Contributions
Conceptualization, B.B., B.M., and C.R.C.; formal analysis, L.B.; funding acquisition, B.M.; methodology, L.B., P.N.; project administration, B.M., C.R.C., L.B.; supervision, B.B., B.M., P.N., C.R.C.; visualization, L.B.; writing—original draft preparation, L.B.; writing—review and editing, B.B., P.B., B.M., M.R., P.N., and C.R.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee (“Regionala etikprövningsnämnden”) of Karolinska Institute, Stockholm, Sweden (2021-05652-01; date of approval: 15 November 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available from Nancy Pedersen (nancy.pedersen@ki.se), Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden, but restrictions apply to the availability of these data: restrictions are based on the Swedish Act (2013:794) requiring that a valid ethical approval is obtained in Sweden.
Conflicts of Interest
C.R.C. is supported by the UK National Institute for Health Research (NIHR) Biomedical Research Centre but the views expressed herein are his own and do not represent those of NIHR nor the UK Department of Health and Social Care. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Funding Statement
This research was funded by the European Union′s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No. 764604, the European Union’s Horizon 2020 Research and Innovation Programme, grant agreement No. 848261 as well as by the GENDER-Net Co-Plus Fund (GNP-182).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Xu X., Mishra G.D., Jones M. Evidence on Multimorbidity from Definition to Intervention: An Overview of Systematic Reviews. Ageing Res. Rev. 2017;37:53–68. doi: 10.1016/j.arr.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Zulman D.M., Asch S.M., Martins S.B., Kerr E.A., Hoffman B.B., Goldstein M.K. Quality of Care for Patients with Multiple Chronic Conditions: The Role of Comorbidity Interrelatedness. J. Gen. Intern. Med. 2014;29:529–537. doi: 10.1007/s11606-013-2616-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Violan C., Foguet-Boreu Q., Flores-Mateo G., Salisbury C., Blom J., Freitag M., Glynn L., Muth C., Valderas J.M. Prevalence, Determinants and Patterns of Multimorbidity in Primary Care: A Systematic Review of Observational Studies. PLoS ONE. 2014;9:e102149. doi: 10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.France E.F., Wyke S., Gunn J.M., Mair F.S., McLean G., Mercer S.W. Multimorbidity in Primary Care: A Systematic Review of Prospective Cohort Studies. Br. J. Gen. Pract. 2012;62:e297–e307. doi: 10.3399/bjgp12X636146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nunes B.P., Flores T.R., Mielke G.I., Thumé E., Facchini L.A. Multimorbidity and Mortality in Older Adults: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2016;67:130–138. doi: 10.1016/j.archger.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Ryan A., Wallace E., O’Hara P., Smith S.M. Multimorbidity and Functional Decline in Community-Dwelling Adults: A Systematic Review. Health Qual. Life Outcomes. 2015;13:168. doi: 10.1186/s12955-015-0355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grandt D., Gamstätter T., Fölsch U.R. Entwicklung von Empfehlungen zum Management von Arzneimitteltherapie bei Multimorbidität. Dtsch. Med. Wochenschr. 2020;145:1504–1508. doi: 10.1055/a-1234-9684. [DOI] [PubMed] [Google Scholar]
- 8.Muth C., Blom J.W., Smith S.M., Johnell K., Gonzalez-Gonzalez A.I., Nguyen T.S., Brueckle M.-S., Cesari M., Tinetti M.E., Valderas J.M. Evidence Supporting the Best Clinical Management of Patients with Multimorbidity and Polypharmacy: A Systematic Guideline Review and Expert Consensus. J. Intern. Med. 2018;285:272–288. doi: 10.1111/joim.12842. [DOI] [PubMed] [Google Scholar]
- 9.Boyd C.M., Darer J., Boult C., Fried L.P., Boult L., Wu A.W. Clinical Practice Guidelines and Quality of Care for Older Patients With Multiple Comorbid Diseases: Implications for Pay for Performance. JAMA. 2005;294:716. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 10.McDaid D., Park A.-L. Counting All the Costs: The Economic Impact of Comorbidity. In: Sartorius N., Holt R.I.G., Maj M., editors. Key Issues in Mental Health. Volume 179. S. Karger AG; Basel, Switzerland: 2014. pp. 23–32. [Google Scholar]
- 11.Fortin M., Soubhi H., Hudon C., Bayliss E.A., van den Akker M. Multimorbidity’s Many Challenges. BMJ. 2007;334:1016–1017. doi: 10.1136/bmj.39201.463819.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sartorius N. Comorbidity of Mental and Physical Disorders: A Key Problem for Medicine in the 21st Century. Acta Psychiatr. Scand. 2018;137:369–370. doi: 10.1111/acps.12888. [DOI] [PubMed] [Google Scholar]
- 13.Starfield B. Global Health, Equity, and Primary Care. J. Am. Board Fam. Med. 2007;20:511–513. doi: 10.3122/jabfm.2007.06.070176. [DOI] [PubMed] [Google Scholar]
- 14.Plana-Ripoll O., Pedersen C.B., Holtz Y., Benros M.E., Dalsgaard S., de Jonge P., Fan C.C., Degenhardt L., Ganna A., Greve A.N., et al. Exploring Comorbidity Within Mental Disorders Among a Danish National Population. JAMA Psychiatry. 2019;76:259–270. doi: 10.1001/jamapsychiatry.2018.3658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forman–Hoffman V.L., Batts K.R., Hedden S.L., Spagnola K., Bose J. Comorbid Mental Disorders among Adults in the Mental Health Surveillance Survey. Ann. Epidemiol. 2018;28:468–474. doi: 10.1016/j.annepidem.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Kessler R.C., Chiu W.T., Demler O., Walters E.E. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:617. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobi F., Wittchen H.-U., Hölting C., Höfler M., Pfister H., Müller N., Lieb R. Prevalence, Co-Morbidity and Correlates of Mental Disorders in the General Population: Results from the German Health Interview and Examination Survey (GHS) Psychol. Med. 2004;34:597–611. doi: 10.1017/S0033291703001399. [DOI] [PubMed] [Google Scholar]
- 18.Daré L.O., Bruand P.-E., Gérard D., Marin B., Lameyre V., Boumédiène F., Preux P.-M. Co-Morbidities of Mental Disorders and Chronic Physical Diseases in Developing and Emerging Countries: A Meta-Analysis. BMC Public Health. 2019;19:304. doi: 10.1186/s12889-019-6623-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Hert M., Correll C.U., Bobes J., Cetkovich-Bakmas M., Cohen D., Asai I., Detraux J., Gautam S., Möller H.-J., Ndetei D.M., et al. Physical Illness in Patients with Severe Mental Disorders. I. Prevalence, Impact of Medications and Disparities in Health Care. World Psychiatry. 2011;10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iacovides A., Siamouli M. Comorbid Mental and Somatic Disorders: An Epidemiological Perspective. Curr. Opin. Psychiatry. 2008;21:417–421. doi: 10.1097/YCO.0b013e328303ba42. [DOI] [PubMed] [Google Scholar]
- 21.Kim J.-H., Chang S.M., Bae J.N., Cho S.-J., Lee J.-Y., Kim B.-S., Cho M.J. Mental-Physical Comorbidity in Korean Adults: Results from a Nationwide General Population Survey in Korea. Psychiatry Investig. 2016;13:496. doi: 10.4306/pi.2016.13.5.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prados-Torres A., Calderón-Larrañaga A., Hancco-Saavedra J., Poblador-Plou B., van den Akker M. Multimorbidity Patterns: A Systematic Review. J. Clin. Epidemiol. 2014;67:254–266. doi: 10.1016/j.jclinepi.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 23.Scott K.M., Lim C., Al-Hamzawi A., Alonso J., Bruffaerts R., Caldas-de-Almeida J.M., Florescu S., de Girolamo G., Hu C., de Jonge P., et al. Association of Mental Disorders With Subsequent Chronic Physical Conditions: World Mental Health Surveys From 17 Countries. JAMA Psychiatry. 2016;73:150. doi: 10.1001/jamapsychiatry.2015.2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Šprah L., Dernovšek M.Z., Wahlbeck K., Haaramo P. Psychiatric Readmissions and Their Association with Physical Comorbidity: A Systematic Literature Review. BMC Psychiatry. 2017;17:2. doi: 10.1186/s12888-016-1172-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans D.L., Charney D.S., Lewis L., Golden R.N., Gorman J.M., Krishnan K.R.R., Nemeroff C.B., Bremner J.D., Carney R.M., Coyne J.C., et al. Mood Disorders in the Medically Ill: Scientific Review and Recommendations. Biol. Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Gold S.M., Köhler-Forsberg O., Moss-Morris R., Mehnert A., Miranda J.J., Bullinger M., Steptoe A., Whooley M.A., Otte C. Comorbid Depression in Medical Diseases. Nat. Rev. Dis. Primers. 2020;6:69. doi: 10.1038/s41572-020-0200-2. [DOI] [PubMed] [Google Scholar]
- 27.Turner J., Kelly B. Emotional Dimensions of Chronic Disease. West. J. Med. 2000;172:124–128. doi: 10.1136/ewjm.172.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Šimunović Filipčić I., Bajić Ž., Filipčić I. The Onset and Accumulation of Physical Multimorbidity in Severe and Common Mental Disorders. Curr. Opin. Psychiatry. 2020;ahead of print doi: 10.1097/YCO.0000000000000635. [DOI] [PubMed] [Google Scholar]
- 29.Prince M., Patel V., Saxena S., Maj M., Maselko J., Phillips M.R., Rahman A. No Health without Mental Health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 30.Stein M.B., Cox B.J., Afifi T.O., Belik S.-L., Sareen J. Does Co-Morbid Depressive Illness Magnify the Impact of Chronic Physical Illness? A Population-Based Perspective. Psychol. Med. 2006;36:587. doi: 10.1017/S0033291706007239. [DOI] [PubMed] [Google Scholar]
- 31.Starace F., Mungai F., Baccari F., Galeazzi G.M. Excess Mortality in People with Mental Illness: Findings from a Northern Italy Psychiatric Case Register. Soc. Psychiatry Psychiatr. Epidemiol. 2018;53:249–257. doi: 10.1007/s00127-017-1468-8. [DOI] [PubMed] [Google Scholar]
- 32.Lawrence D., Kisely S., Pais J. The Epidemiology of Excess Mortality in People with Mental Illness. Can. J. Psychiatry. 2010;55:752–760. doi: 10.1177/070674371005501202. [DOI] [PubMed] [Google Scholar]
- 33.Firth J., Siddiqi N., Koyanagi A., Siskind D., Rosenbaum S., Galletly C., Allan S., Caneo C., Carney R., Carvalho A.F., et al. The Lancet Psychiatry Commission: A Blueprint for Protecting Physical Health in People with Mental Illness. Lancet Psychiatry. 2019;6:675–712. doi: 10.1016/S2215-0366(19)30132-4. [DOI] [PubMed] [Google Scholar]
- 34.Britt H.C., Harrison C.M., Miller G.C., Knox S.A. Prevalence and Patterns of Multimorbidity in Australia. Med. J. Aust. 2008;189:72–77. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]
- 35.Friis K., Pedersen M.H., Larsen F.B., Lasgaard M. A National Population Study of the Co-Occurrence of Multiple Long-Term Conditions in People with Multimorbidity, Denmark, 2013. Prev. Chronic Dis. 2016;13:150404. doi: 10.5888/pcd13.150404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Oostrom S.H., Picavet H.S.J., van Gelder B.M., Lemmens L.C., Hoeymans N., van Dijk C.E., Verheij R.A., Schellevis F.G., Baan C.A. Multimorbidity and Comorbidity in the Dutch Population—Data from General Practices. BMC Public Health. 2012;12:715. doi: 10.1186/1471-2458-12-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Violán C., Roso-Llorach A., Foguet-Boreu Q., Guisado-Clavero M., Pons-Vigués M., Pujol-Ribera E., Valderas J.M. Multimorbidity Patterns with K-Means Nonhierarchical Cluster Analysis. BMC Fam. Pract. 2018;19:108. doi: 10.1186/s12875-018-0790-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnett K., Mercer S.W., Norbury M., Watt G., Wyke S., Guthrie B. Epidemiology of Multimorbidity and Implications for Health Care, Research, and Medical Education: A Cross-Sectional Study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 39.Guisado-Clavero M., Roso-Llorach A., López-Jimenez T., Pons-Vigués M., Foguet-Boreu Q., Muñoz M.A., Violán C. Multimorbidity Patterns in the Elderly: A Prospective Cohort Study with Cluster Analysis. BMC Geriatr. 2018;18:16. doi: 10.1186/s12877-018-0705-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keetile M., Navaneetham K., Letamo G. Prevalence and Correlates of Multimorbidity among Adults in Botswana: A Cross-Sectional Study. PLoS ONE. 2020;15:e0239334. doi: 10.1371/journal.pone.0239334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Prados-Torres A., Poblador-Plou B., Calderón-Larrañaga A., Gimeno-Feliu L.A., González-Rubio F., Poncel-Falcó A., Sicras-Mainar A., Alcalá-Nalvaiz J.T. Multimorbidity Patterns in Primary Care: Interactions among Chronic Diseases Using Factor Analysis. PLoS ONE. 2012;7:e32190. doi: 10.1371/journal.pone.0032190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schäfer I., von Leitner E.-C., Schön G., Koller D., Hansen H., Kolonko T., Kaduszkiewicz H., Wegscheider K., Glaeske G., van den Bussche H. Multimorbidity Patterns in the Elderly: A New Approach of Disease Clustering Identifies Complex Interrelations between Chronic Conditions. PLoS ONE. 2010;5:e15941. doi: 10.1371/journal.pone.0015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schäfer I., Hansen H., Schön G., Höfels S., Altiner A., Dahlhaus A., Gensichen J., Riedel-Heller S., Weyerer S., Blank W.A., et al. The Influence of Age, Gender and Socio-Economic Status on Multimorbidity Patterns in Primary Care. First Results from the Multicare Cohort Study. BMC Health Serv. Res. 2012;12:89. doi: 10.1186/1472-6963-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knudsen A.K., Allebeck P., Tollånes M.C., Skogen J.C., Iburg K.M., McGrath J.J., Juel K., Agardh E.E., Ärnlöv J., Bjørge T., et al. Life Expectancy and Disease Burden in the Nordic Countries: Results from the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet Public Health. 2019;4:e658–e669. doi: 10.1016/S2468-2667(19)30224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Almqvist C., Adami H.-O., Franks P.W., Groop L., Ingelsson E., Kere J., Lissner L., Litton J.-E., Maeurer M., Michaëlsson K., et al. LifeGene—A Large Prospective Population-Based Study of Global Relevance. Eur. J. Epidemiol. 2011;26:67–77. doi: 10.1007/s10654-010-9521-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LifeGene Description of the LifeGene Resource; LifeGene 2017. [(accessed on 18 May 2022)]. Available online: https://lifegene.se/wp-content/uploads/1LifeGeneresource20170203version24.pdf.
- 47.Basso L., Boecking B., Brueggemann P., Pedersen N.L., Canlon B., Cederroth C.R., Mazurek B. Gender-Specific Risk Factors and Comorbidities of Bothersome Tinnitus. Front. Neurosci. 2020;14:706. doi: 10.3389/fnins.2020.00706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Basso L., Boecking B., Brueggemann P., Pedersen N.L., Canlon B., Cederroth C.R., Mazurek B. Subjective Hearing Ability, Physical and Mental Comorbidities in Individuals with Bothersome Tinnitus in a Swedish Population Sample. In: Schlee W., Langguth B., Kleinjung T., Vanneste S., De Ridder D., editors. Progress in Brain Research. Volume 260. Elsevier; Amsterdam, The Netherlands: 2021. pp. 51–78. [DOI] [PubMed] [Google Scholar]
- 49.De Ridder D., Schlee W., Vanneste S., Londero A., Weisz N., Kleinjung T., Shekhawat G.S., Elgoyhen A.B., Song J.-J., Andersson G., et al. Progress in Brain Research. Volume 260. Elsevier; Amsterdam, The Netherlands: 2021. Tinnitus and Tinnitus Disorder: Theoretical and Operational Definitions (an International Multidisciplinary Proposal) pp. 1–25. [DOI] [PubMed] [Google Scholar]
- 50.R Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2020. [Google Scholar]
- 51.Zhang R., Lu Y., Shi L., Zhang S., Chang F. Prevalence and Patterns of Multimorbidity among the Elderly in China: A Cross-Sectional Study Using National Survey Data. BMJ Open. 2019;9:e024268. doi: 10.1136/bmjopen-2018-024268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Spertus J.A., Dawson J., Masoudi F.A., Krumholz H.M., Reid K.J., Peterson E.D., Rumsfeld J.S. Cardiovascular Outcomes Research Consortium Prevalence and Predictors of Angina Pectoris One Month after Myocardial Infarction. Am. J. Cardiol. 2006;98:282–288. doi: 10.1016/j.amjcard.2006.01.099. [DOI] [PubMed] [Google Scholar]
- 53.Zhang J., Liu C., Pan C., Bai M., Zhang J., Peng Y., Zheng D., Zhang Z. Effect of Multiple Clinical Factors on Recurrent Angina after Percutaneous Coronary Intervention: A Retrospective Study from 398 ST-Segment Elevation Myocardial Infarction Patients. Medicine. 2016;95:e5015. doi: 10.1097/MD.0000000000005015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Parashar S., Rumsfeld J.S., Reid K.J., Buchanan D., Dawood N., Khizer S., Lichtman J., Vaccarino V. Impact of Depression on Sex Differences in Outcome After Myocardial Infarction. Circ. Cardiovasc. Qual. Outcomes. 2009;2:33–40. doi: 10.1161/CIRCOUTCOMES.108.818500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hirschtritt M.E., Lee P.C., Pauls D.L., Dion Y., Grados M.A., Illmann C., King R.A., Sandor P., McMahon W.M., Lyon G.J., et al. Lifetime Prevalence, Age of Risk, and Genetic Relationships of Comorbid Psychiatric Disorders in Tourette Syndrome. JAMA Psychiatry. 2015;72:325. doi: 10.1001/jamapsychiatry.2014.2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Martino D., Ganos C., Pringsheim T.M. International Review of Neurobiology. Volume 134. Elsevier; Amsterdam, The Netherlands: 2017. Tourette Syndrome and Chronic Tic Disorders: The Clinical Spectrum Beyond Tics; pp. 1461–1490. [DOI] [PubMed] [Google Scholar]
- 57.Sharma S.R., Gonda X., Tarazi F.I. Autism Spectrum Disorder: Classification, Diagnosis and Therapy. Pharmacol. Ther. 2018;190:91–104. doi: 10.1016/j.pharmthera.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 58.Christensen D.L., Baio J., Braun K.V.N., Bilder D., Charles J., Constantino J.N., Daniels J., Durkin M.S., Fitzgerald R.T., Kurzius-Spencer M., et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2012. MMWR Surveill. Summ. 2016;65:1–23. doi: 10.15585/mmwr.ss6503a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Greene A.L., Eaton N.R. Panic Disorder and Agoraphobia: A Direct Comparison of Their Multivariate Comorbidity Patterns. J. Affect. Disord. 2016;190:75–83. doi: 10.1016/j.jad.2015.09.060. [DOI] [PubMed] [Google Scholar]
- 60.Parreira P., Maher C.G., Steffens D., Hancock M.J., Ferreira M.L. Risk Factors for Low Back Pain and Sciatica: An Umbrella Review. Spine J. 2018;18:1715–1721. doi: 10.1016/j.spinee.2018.05.018. [DOI] [PubMed] [Google Scholar]
- 61.Younes M., Béjia I., Aguir Z., Letaief M., Hassen-Zrour S., Touzi M., Bergaoui N. Prevalence and Risk Factors of Disk-Related Sciatica in an Urban Population in Tunisia. Joint Bone Spine. 2006;73:538–542. doi: 10.1016/j.jbspin.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 62.Bandelow B. Generalized Anxiety Disorder and Pain. In: Finn D.P., Leonard B.E., editors. Modern Trends in Pharmacopsychiatry. Volume 30. S. Karger AG; Basel, Switzerland: 2015. pp. 153–165. [DOI] [PubMed] [Google Scholar]
- 63.Carta M.G., Moro M.F., Pinna F.L., Testa G., Cacace E., Ruggiero V., Piras M., Romano F., Minerba L., Machado S., et al. The Impact of Fibromyalgia Syndrome and the Role of Comorbidity with Mood and Post-Traumatic Stress Disorder in Worsening the Quality of Life. Int. J. Soc. Psychiatry. 2018;64:647–655. doi: 10.1177/0020764018795211. [DOI] [PubMed] [Google Scholar]
- 64.Lichtenstein A., Tiosano S., Amital H. The Complexities of Fibromyalgia and Its Comorbidities. Curr. Opin. Rheumatol. 2018;30:94–100. doi: 10.1097/BOR.0000000000000464. [DOI] [PubMed] [Google Scholar]
- 65.Løge-Hagen J.S., Sæle A., Juhl C., Bech P., Stenager E., Mellentin A. Prevalence of Depressive Disorder among Patients with Fibromyalgia: Systematic Review and Meta-Analysis. J. Affect. Disord. 2019;245:1098–1105. doi: 10.1016/j.jad.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 66.Borchers A.T., Gershwin M.E. Fibromyalgia: A Critical and Comprehensive Review. Clin. Rev. Allergy Immunol. 2015;49:100–151. doi: 10.1007/s12016-015-8509-4. [DOI] [PubMed] [Google Scholar]
- 67.Angst F., Angst J., Ajdacic-Gross V., Aeschlimann A., Rössler W. Epidemiology of Back Pain in Young and Middle-Aged Adults: A Longitudinal Population Cohort Survey From Age 27–50 Years. Psychosomatics. 2017;58:604–613. doi: 10.1016/j.psym.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 68.Cho C.-H., Jung S.-W., Park J.-Y., Song K.-S., Yu K.-I. Is Shoulder Pain for Three Months or Longer Correlated with Depression, Anxiety, and Sleep Disturbance? J. Shoulder Elb. Surg. 2013;22:222–228. doi: 10.1016/j.jse.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 69.Heikkinen J., Honkanen R., Williams L., Leung J., Rauma P., Quirk S., Koivumaa-Honkanen H. Depressive Disorders, Anxiety Disorders and Subjective Mental Health in Common Musculoskeletal Diseases: A Review. Maturitas. 2019;127:18–25. doi: 10.1016/j.maturitas.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 70.Mäntyselkä P., Lupsakko T., Kautiainen H., Vanhala M. Neck-Shoulder Pain and Depressive Symptoms: A Cohort Study with a 7-Year Follow-Up. Eur. J. Pain. 2010;14:189–193. doi: 10.1016/j.ejpain.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 71.Viana M.C., Lim C.C.W., Garcia Pereira F., Aguilar-Gaxiola S., Alonso J., Bruffaerts R., de Jonge P., Caldas-de-Almeida J.M., O’Neill S., Stein D.J., et al. Previous Mental Disorders and Subsequent Onset of Chronic Back or Neck Pain: Findings from 19 Countries. J. Pain. 2018;19:99–110. doi: 10.1016/j.jpain.2017.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Goesling J., Clauw D.J., Hassett A.L. Pain and Depression: An Integrative Review of Neurobiological and Psychological Factors. Curr. Psychiatry Rep. 2013;15:421. doi: 10.1007/s11920-013-0421-0. [DOI] [PubMed] [Google Scholar]
- 73.Thiagarajah A.S., Guymer E.K., Leech M., Littlejohn G.O. The Relationship between Fibromyalgia, Stress and Depression. Int. J. Clin. Rheumatol. 2014;9:371–384. doi: 10.2217/ijr.14.30. [DOI] [Google Scholar]
- 74.Hooten W.M. Chronic Pain and Mental Health Disorders. Mayo Clin. Proc. 2016;91:955–970. doi: 10.1016/j.mayocp.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 75.IsHak W.W., Wen R.Y., Naghdechi L., Vanle B., Dang J., Knosp M., Dascal J., Marcia L., Gohar Y., Eskander L., et al. Pain and Depression: A Systematic Review. Harv. Rev. Psychiatry. 2018;26:352–363. doi: 10.1097/HRP.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 76.Han C., Pae C.-U. Pain and Depression: A Neurobiological Perspective of Their Relationship. Psychiatry Investig. 2015;12:1. doi: 10.4306/pi.2015.12.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Goldenberg D.L. Pain/Depression Dyad: A Key to a Better Understanding and Treatment of Functional Somatic Syndromes. Am. J. Med. 2010;123:675–682. doi: 10.1016/j.amjmed.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 78.Sheng J., Liu S., Wang Y., Cui R., Zhang X. The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plast. 2017;2017:9724371. doi: 10.1155/2017/9724371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walker A.K., Kavelaars A., Heijnen C.J., Dantzer R. Neuroinflammation and Comorbidity of Pain and Depression. Pharmacol Rev. 2014;66:80–101. doi: 10.1124/pr.113.008144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tegethoff M., Stalujanis E., Belardi A., Meinlschmidt G. Chronology of Onset of Mental Disorders and Physical Diseases in Mental-Physical Comorbidity—A National Representative Survey of Adolescents. PLoS ONE. 2016;11:e0165196. doi: 10.1371/journal.pone.0165196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Person H., Keefer L. Psychological Comorbidity in Gastrointestinal Diseases: Update on the Brain-Gut-Microbiome Axis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107:110209. doi: 10.1016/j.pnpbp.2020.110209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Koloski N.A., Jones M., Talley N.J. Evidence That Independent Gut-to-Brain and Brain-to-Gut Pathways Operate in the Irritable Bowel Syndrome and Functional Dyspepsia: A 1-Year Population-Based Prospective Study. Aliment. Pharmacol. Ther. 2016;44:592–600. doi: 10.1111/apt.13738. [DOI] [PubMed] [Google Scholar]
- 83.Hsu C.-C., Hsu Y.-C., Chang K.-H., Lee C.-Y., Chong L.-W., Lin C.-L., Shang C.-S., Sung F.-C., Kao C.-H. Depression and the Risk of Peptic Ulcer Disease: A Nationwide Population-Based Study. Medicine. 2015;94:e2333. doi: 10.1097/MD.0000000000002333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Taha F., Lipsitz J.D., Galea S., Demmer R.T., Talley N.J., Goodwin R.D. Anxiety Disorders and Risk of Self-Reported Ulcer: A 10-Year Longitudinal Study among US Adults. Gen. Hosp. Psychiatry. 2014;36:674–679. doi: 10.1016/j.genhosppsych.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 85.Drossman D.A. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features, and Rome IV. Gastroenterology. 2016;150:1262–1279.e2. doi: 10.1053/j.gastro.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 86.Enck P., Aziz Q., Barbara G., Farmer A.D., Fukudo S., Mayer E.A., Niesler B., Quigley E.M.M., Rajilić-Stojanović M., Schemann M., et al. Irritable Bowel Syndrome. Nat. Rev. Dis. Primers. 2016;2:16014. doi: 10.1038/nrdp.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Barandouzi Z.A., Starkweather A.R., Henderson W.A., Gyamfi A., Cong X.S. Altered Composition of Gut Microbiota in Depression: A Systematic Review. Front. Psychiatry. 2020;11:541. doi: 10.3389/fpsyt.2020.00541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Samuels D.V., Rosenthal R., Lin R., Chaudhari S., Natsuaki M.N. Acne Vulgaris and Risk of Depression and Anxiety: A Meta-Analytic Review. J. Am. Acad. Dermatol. 2020;83:532–541. doi: 10.1016/j.jaad.2020.02.040. [DOI] [PubMed] [Google Scholar]
- 89.Sood S., Jafferany M., Vinaya kumar S. Depression, Psychiatric Comorbidities, and Psychosocial Implications Associated with Acne Vulgaris. J. Cosmet. Dermatol. 2020;19:3177–3182. doi: 10.1111/jocd.13753. [DOI] [PubMed] [Google Scholar]
- 90.Kauppi S., Jokelainen J., Timonen M., Tasanen K., Huilaja L. Adult Patients with Atopic Eczema Have a High Burden of Psychiatric Disease: A Finnish Nationwide Registry Study. Acta Derm. Venereol. 2019;99:647–651. doi: 10.2340/00015555-3165. [DOI] [PubMed] [Google Scholar]
- 91.Schmitt J., Romanos M., Pfennig A., Leopold K., Meurer M. Psychiatric Comorbidity in Adult Eczema. Br. J. Dermatol. 2009;161:878–883. doi: 10.1111/j.1365-2133.2009.09309.x. [DOI] [PubMed] [Google Scholar]
- 92.Picardi A., Pasquini P. Toward a Biopsychosocial Approach to Skin Diseases. Adv. Psychosom. Med. 2007;28:109–126. doi: 10.1159/000106800. [DOI] [PubMed] [Google Scholar]
- 93.Barankin B., DeKoven J. Psychosocial Effect of Common Skin Diseases. Can. Fam. Physician. 2002;48:712–716. [PMC free article] [PubMed] [Google Scholar]
- 94.Yang L., Li C., Li X., Zhai M., An Q., Zhang Y., Zhao J., Weng X. Prevalence of Developmental Dyslexia in Primary School Children: A Systematic Review and Meta-Analysis. Brain Sci. 2022;12:240. doi: 10.3390/brainsci12020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Krafnick A.J., Evans T.M. Neurobiological Sex Differences in Developmental Dyslexia. Front. Psychol. 2019;9:2669. doi: 10.3389/fpsyg.2018.02669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mugnaini D., Lassi S., La Malfa G., Albertini G. Internalizing Correlates of Dyslexia. World J. Pediatr. 2009;5:255–264. doi: 10.1007/s12519-009-0049-7. [DOI] [PubMed] [Google Scholar]
- 97.Schulte-Körne G. The Prevention, Diagnosis, and Treatment of Dyslexia. Dtsch. Ärzteblatt Int. 2010;107:718–727. doi: 10.3238/arztebl.2010.0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nelson J.M., Gregg N. Depression and Anxiety Among Transitioning Adolescents and College Students With ADHD, Dyslexia, or Comorbid ADHD/Dyslexia. J. Atten. Disord. 2012;16:244–254. doi: 10.1177/1087054710385783. [DOI] [PubMed] [Google Scholar]
- 99.Wang L. Anxiety and Depression among Chinese Children with and without Reading Disabilities. Dyslexia. 2021;27:355–372. doi: 10.1002/dys.1691. [DOI] [PubMed] [Google Scholar]
- 100.Fond G., Loundou A., Hamdani N., Boukouaci W., Dargel A., Oliveira J., Roger M., Tamouza R., Leboyer M., Boyer L. Anxiety and Depression Comorbidities in Irritable Bowel Syndrome (IBS): A Systematic Review and Meta-Analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2014;264:651–660. doi: 10.1007/s00406-014-0502-z. [DOI] [PubMed] [Google Scholar]
- 101.Stasi C., Rosselli M., Bellini M., Laffi G., Milani S. Altered Neuro-Endocrine–Immune Pathways in the Irritable Bowel Syndrome: The Top-down and the Bottom-up Model. J. Gastroenterol. 2012;47:1177–1185. doi: 10.1007/s00535-012-0627-7. [DOI] [PubMed] [Google Scholar]
- 102.Theoharides T.C., Tsilioni I., Arbetman L., Panagiotidou S., Stewart J.M., Gleason R.M., Russell I.J. Fibromyalgia Syndrome in Need of Effective Treatments. J. Pharmacol. Exp. Ther. 2015;355:255–263. doi: 10.1124/jpet.115.227298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Davis M.T., Holmes S.E., Pietrzak R.H., Esterlis I. Neurobiology of Chronic Stress-Related Psychiatric Disorders: Evidence from Molecular Imaging Studies. Chronic Stress. 2017;1:1–21. doi: 10.1177/2470547017710916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Smoller J.W. The Genetics of Stress-Related Disorders: PTSD, Depression, and Anxiety Disorders. Neuropsychopharmacology. 2016;41:297–319. doi: 10.1038/npp.2015.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Caspi A., Moffitt T.E. All for One and One for All: Mental Disorders in One Dimension. AJP. 2018;175:831–844. doi: 10.1176/appi.ajp.2018.17121383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kessler R.C., McLaughlin K.A., Green J.G., Gruber M.J., Sampson N.A., Zaslavsky A.M., Aguilar-Gaxiola S., Alhamzawi A.O., Alonso J., Angermeyer M., et al. Childhood Adversities and Adult Psychopathology in the WHO World Mental Health Surveys. Br. J. Psychiatry. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bellis M.A., Hughes K., Leckenby N., Hardcastle K.A., Perkins C., Lowey H. Measuring Mortality and the Burden of Adult Disease Associated with Adverse Childhood Experiences in England: A National Survey. J. Public Health. 2015;37:445–454. doi: 10.1093/pubmed/fdu065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C., Jones L., Dunne M.P. The Effect of Multiple Adverse Childhood Experiences on Health: A Systematic Review and Meta-Analysis. Lancet Public Health. 2017;2:e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 109.Mariotti A. The Effects of Chronic Stress on Health: New Insights into the Molecular Mechanisms of Brain–Body Communication. Future Sci. OA. 2015;1:FSO23. doi: 10.4155/fso.15.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ginzburg K., Solomon Z. Trajectories of Stress Reactions and Somatization Symptoms among War Veterans: A 20-Year Longitudinal Study. Psychol. Med. 2011;41:353–362. doi: 10.1017/S0033291710000528. [DOI] [PubMed] [Google Scholar]
- 111.Fischer S., Gaab J., Ehlert U., Nater U.M. Prevalence, Overlap, and Predictors of Functional Somatic Syndromes in a Student Sample. Int. J. Behav. Med. 2013;20:184–193. doi: 10.1007/s12529-012-9266-x. [DOI] [PubMed] [Google Scholar]
- 112.Gupta A., Silman A.J., Ray D., Morriss R., Dickens C., MacFarlane G.J., Chiu Y.H., Nicholl B., McBeth J. The Role of Psychosocial Factors in Predicting the Onset of Chronic Widespread Pain: Results from a Prospective Population-Based Study. Rheumatology. 2006;46:666–671. doi: 10.1093/rheumatology/kel363. [DOI] [PubMed] [Google Scholar]
- 113.Henningsen P., Zimmermann T., Sattel H. Medically Unexplained Physical Symptoms, Anxiety, and Depression: A Meta-Analytic Review. Psychosom. Med. 2003;65:528–533. doi: 10.1097/01.PSY.0000075977.90337.E7. [DOI] [PubMed] [Google Scholar]
- 114.Harris A.M., Orav E.J., Bates D.W., Barsky A.J. Somatization Increases Disability Independent of Comorbidity. J. Gen. Intern. Med. 2009;24:155–161. doi: 10.1007/s11606-008-0845-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pathirana T.I., Jackson C.A. Socioeconomic Status and Multimorbidity: A Systematic Review and Meta-Analysis. Aust. New Zealand J. Public Health. 2018;42:186–194. doi: 10.1111/1753-6405.12762. [DOI] [PubMed] [Google Scholar]
- 116.Senn T.E., Walsh J.L., Carey M.P. The Mediating Roles of Perceived Stress and Health Behaviors in the Relation Between Objective, Subjective, and Neighborhood Socioeconomic Status and Perceived Health. Ann. Behav. Med. 2014;48:215–224. doi: 10.1007/s12160-014-9591-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Fortin M., Haggerty J., Sanche S., Almirall J. Self-Reported versus Health Administrative Data: Implications for Assessing Chronic Illness Burden in Populations. A Cross-Sectional Study. CMAJ Open. 2017;5:E729–E733. doi: 10.9778/cmajo.20170029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Muggah E., Graves E., Bennett C., Manuel D.G. Ascertainment of Chronic Diseases Using Population Health Data: A Comparison of Health Administrative Data and Patient Self-Report. BMC Public Health. 2013;13:16. doi: 10.1186/1471-2458-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Violán C., Foguet-Boreu Q., Hermosilla-Pérez E., Valderas J.M., Bolíbar B., Fàbregas-Escurriola M., Brugulat-Guiteras P., Muñoz-Pérez M.Á. Comparison of the Information Provided by Electronic Health Records Data and a Population Health Survey to Estimate Prevalence of Selected Health Conditions and Multimorbidity. BMC Public Health. 2013;13:251. doi: 10.1186/1471-2458-13-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Blane D.N., Lewandowska M. Living with Cancer and Multimorbidity: The Role of Primary Care. Curr. Opin. Supportive Palliat. Care. 2019;13:213–219. doi: 10.1097/SPC.0000000000000454. [DOI] [PubMed] [Google Scholar]
- 121.Fowler H., Belot A., Ellis L., Maringe C., Luque-Fernandez M.A., Njagi E.N., Navani N., Sarfati D., Rachet B. Comorbidity Prevalence among Cancer Patients: A Population-Based Cohort Study of Four Cancers. BMC Cancer. 2020;20:2. doi: 10.1186/s12885-019-6472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Caceres B.A., Travers J., Sharma Y. Differences in Multimorbidity among Cisgender Sexual Minority and Heterosexual Adults: Investigating Differences across Age-Groups. J. Aging Health. 2021;33:362–376. doi: 10.1177/0898264320983663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Saunders C.L., MacCarthy S., Meads C., Massou E., Mant J., Saunders A.M., Elliott M.N. Long-Term Conditions among Sexual Minority Adults in England: Evidence from a Cross-Sectional Analysis of Responses to the English GP Patient Survey. BJGP Open. 2021;5:1–10. doi: 10.3399/BJGPO.2021.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Valderas J.M., Starfield B., Sibbald B., Salisbury C., Roland M. Defining Comorbidity: Implications for Understanding Health and Health Services. Ann. Fam. Med. 2009;7:357–363. doi: 10.1370/afm.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Luijks H.D., Loeffen M.J., Lagro-Janssen A.L., van Weel C., Lucassen P.L., Schermer T.R. GPs’ Considerations in Multimorbidity Management: A Qualitative Study. Br. J. Gen. Pract. 2012;62:e503–e510. doi: 10.3399/bjgp12X652373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.van Weel C., Schellevis F.G. Comorbidity and Guidelines: Conflicting Interests. Lancet. 2006;367:550–551. doi: 10.1016/S0140-6736(06)68198-1. [DOI] [PubMed] [Google Scholar]
- 127.van der Heide I., Snoeijs S., Quattrini S., Struckmann V., Hujala A., Schellevis F., Rijken M. Patient-Centeredness of Integrated Care Programs for People with Multimorbidity. Results from the European ICARE4EU Project. Health Policy. 2018;122:36–43. doi: 10.1016/j.healthpol.2017.10.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available from Nancy Pedersen (nancy.pedersen@ki.se), Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden, but restrictions apply to the availability of these data: restrictions are based on the Swedish Act (2013:794) requiring that a valid ethical approval is obtained in Sweden.