Abstract
A 43‐year‐old Caucasian man was admitted to hospital due to shortness of breath, right lumbar pain and lower left limb swelling. Arterial blood gas sample showed mild hypoxemia and respiratory alkalosis. CT scan confirmed pulmonary embolism, splenic and bilateral renal ischemic lesions. Echocardiography showed right ventricular and coronary sinus (CS) dilatation. Using contrast echocardiography, a superior sinus venous atrial septal defect and persistent left superior vena cava (PLSVC) draining in CS were suspected. Cardiac CT confirmed the diagnosis and showed overriding right superior vena cava (RSVC) draining in both atria. The patient underwent successful surgical correction.
Keywords: ASD, PLSVC
1. CASE REPORT
1.1. Presentation
A 43‐year‐old caucasian man was admitted to the emergency department (ED) due to shortness of breath, right lumbar pain, and lower left limb swelling. Physical examination showed tachypnea (22/min), tachycardia (100 bpm), mild jugular venous distension and lower left limb edema. Blood pressure was 130/90 mmHg. D‐Dimer was 2.812 ng/ml (n.v. 0‐278); Hs‐troponin T was .02 ng/ml (n.v. 0 – .01). A complete blood count was normal. Arterial blood gas sample showed: pH 7.48, pCO2 28 mmHg, pO2 65 mmHg, sO2 94%, HCO3 − 20 mmol/L, FiO2 21%. Electrocardiogram showed sinus tachycardia at a rate of 100 bpm and no other abnormal findings. SARS‐CoV‐2 polymerase chain reaction test was negative. Bedside transthoracic echocardiography showed right ventricular dilatation with mildly reduced systolic function, mild tricuspid regurgitation and coronary sinus (CS) dilatation (maximum diameter 26 mm). A contrast‐enhanced CT scan of chest, abdomen and inferior limbs showed pulmonary embolus in the right pulmonary artery and in its inferior segmental and sub‐segmental branches, ground‐glass appearance of the right lower‐inferior pulmonary lobe, thrombus in the left femoral vein extended to the external and common iliac veins. Splenic and bilateral renal ischemic lesions were also detected. The patient started Fondaparinux 7.5 milligrams per day and, as a high risk pulmonary embolism, he was transferred to our Coronary Intensive Care Unit according to current guidelines. 1
1.2. Medical history
The patient reported mild systemic hypertension, dyslipidemia and hypothyroidism treated with levothyroxine. He was a non‐smoker and a social drinker. There was no history of diabetes, cardiovascular diseases, or significant family history.
1.3. Differential diagnosis
Considering both systemic and pulmonary embolism, two main differential diagnoses were evaluated:
-
‐
hypercoagulation state with venous and arterial thrombosis;
-
‐
right‐to‐left shunt with pulmonary and paradoxical systemic embolism.
CS dilatation suggested the following hypothesis: persistent left superior vena cava (PLSVC) with or without associated atrial septal defect (ASD), unroofed CS, coronary fistula, right ventricular overload.
1.4. Other investigations
Blood test was performed to evaluate coagulation pathway including protein C and protein S deficiencies, Factor V Leiden mutation, antithrombin III deficiency, prothrombin gene (20210G > A) mutation, methyl‐tetrahydrofolate reductase (MTHFR) gene mutations, anticardiolipin antibodies and lupus anticoagulant. All blood tests for hypercoagulation state were negative. Additional tests for seronegative anti‐phospholipid syndrome were also negative.
Transthoracic echocardiography confirmed right ventricular and CS dilatation without evidence of shunt in the region of the fossa ovalis as evaluated with color‐Doppler. Unroofed CS and sinus venosus defect could not be excluded. A dilated CS was compatible with both these two defects. Contrast enhanced echocardiography was performed to assess potential abnormal intra‐cardiac shunt. After administration of agitated normal saline in the left antecubital vein, complete opacification of the CS and, then, of the right heart chambers was demonstrated (Figure 1 Panel A and Movie S1). These findings were consistent with PLSVC. In the parasternal long axis view, but not in the apical projections, some microbubbles were observed in the left chambers. After administration of contrast by the right antecubital vein, simultaneous and complete opacification of right and left chambers was observed with contrast coming from the atrial roofs (Figure 1 Panel B and Movie S2). A communication between the atria was suspected but the ASD was not visualized, and a transesophageal echocardiogram (TE) was performed. TE showed atrial septal aneurysm without shunt evaluated at color Doppler in the region of the fossa ovalis. Inferior vena cava drained in the right atrium. Discontinuity of the superior atrial septum consistent with superior sinus venosus ASD was detected (Figure 1 Panel C, white arrow). After the administration of agitated normal saline by the right arm, contrast entered simultaneously in both right and left atrium from the right and left atrial roofs (Figure 1 Panel D). No sign of discontinuity of the roof between CS and the left atrium was detected. Left pulmonary veins drained in the LA while the drainage of the right pulmonary veins was not visualized. All these findings were consistent with superior sinus venosus ASD. Administration of agitated saline from the lower limb resulted in traces of contrast in the left chambers only.
FIGURE 1.
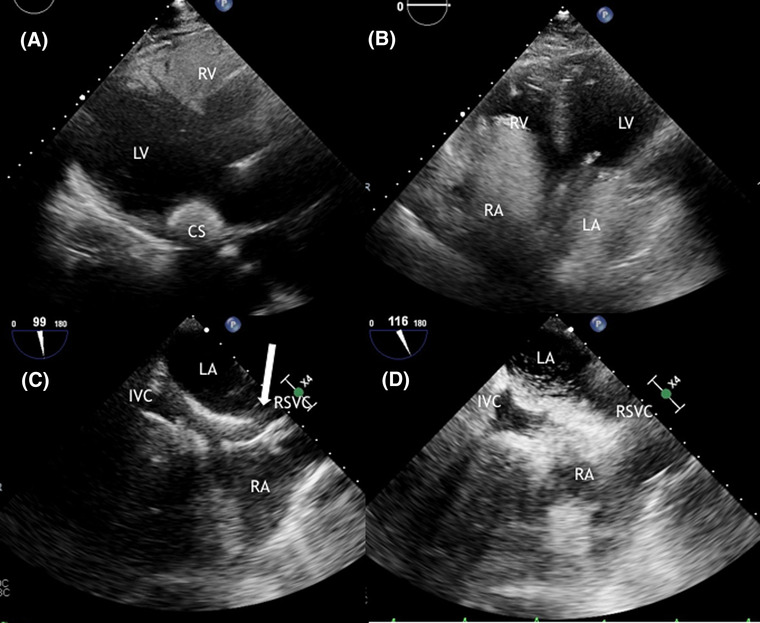
Panel A: Transthoracic echocardiography in parasternal long‐axis view after administration of agitated normal saline in the left antecubital vein showed complete opacification of the coronary sinus and then, of the right chambers. Panel B: Transthoracic echocardiography in four chambers view after administration of contrast by the right antecubital veins showed simultaneous and complete opacification of right and left chambers, with contrast coming from the atrial roofs. Panel C: Transesophageal echocardiography in bicaval view showed superior atrial septum discontinuity consistent with superior sinus venosus atrial septal defect (white arrow). Panel D: Transesophageal echocardiography in bicaval view after the administration of agitated normal saline by the right arm showed contrast entering simultaneously in both right and left atrium from the atrial roofs. CS, coronary sinus; LA, left atrium; LV, left ventricle; IVC, inferior vena cava; RA, right atrium; RSVC, right superior vena cava; RV, right ventricle
Right heart catheterization was performed showing normal pulmonary arterial pressures. Systolic, diastolic and mean pulmonary arterial pressures were 22, 7, and 12 mmHg, respectively. Wedge pressure and right atrial pressure were 8 and 2 mmHg, respectively. Total pulmonary arterial resistance was within the normal limits. An increase in oxygen saturation of 7% at the atrial level from the right superior vena cava (RSVC) was detected (oxygen saturation measurements: upper RSVC 68%, inferior vena cava 69%, right atrium 75%, right ventricle 76%, pulmonary artery 76%, aorta 92%). Systemic flow rate (Qs) was 8.3 L/min, pulmonary flow rate (Qp) was 10.5 L/min and Qp/Qs was 1.26.
A cardiac CT confirmed the presence of PLSVC and superior sinus venosus ASD with an overriding RSVC draining in both right and left atrium (Figure 2 Panel A). Moreover, an extra‐cardiac shunt was found with upper right pulmonary vein draining in the right RSVC (Figures 2 Panel B and 3).
FIGURE 2.
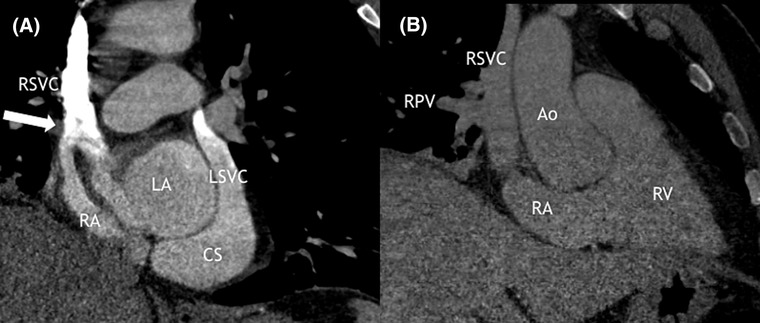
Panel A: Cardiac computed tomography showed persistent left superior vena cava draining in coronary sinus; sinus venosus ASD (white arrow) with an overriding superior vena cava draining in both right and left atrium. Panel B: Cardiac computed tomography showed partial anomalous pulmonary venous drainage in right superior vena cava. Ao, aorta; CS, coronary sinus; LA, left atrium; LSVC, left superior vena cava; RA, right atrium; RPV, right pulmonary vein; RSVC, right superior vena cava; RV, right ventricle
FIGURE 3.
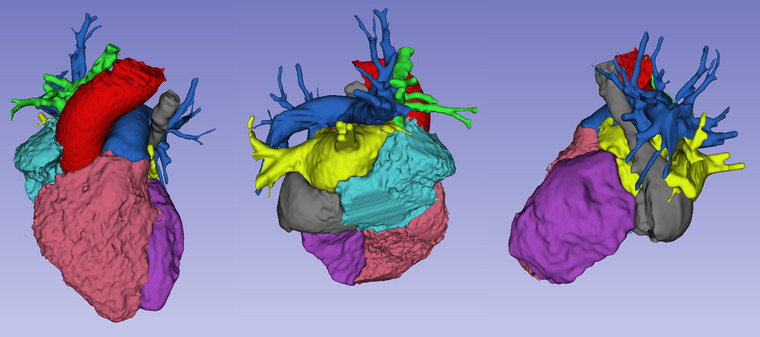
Three‐dimensional reconstruction of the cardiac computer tomography showing persistent left superior vena cava draining in coronary sinus and partial anomalous pulmonary venous drainage in right superior vena cava. Segments are displayed as follow. Red: aorta; purple: left ventricle; yellow: left atrium and pulmonary veins draining in left atrium; blue: pulmonary artery; pink: right ventricle; light blue: right atrium; gray: persistent left superior vena cava draining in coronary sinus; green: right superior vena cava and partial pulmonary venous drainage
1.5. Management
The patient was treated with fondaparinux, then switched to apixaban 5 mg bis in die, and diuretics to reduce the lower limb swelling. Considering the paradoxical embolic event and the systemic desaturation, surgical correction of the congenital defect was proposed but the patient initially refused surgery. He was discharged after inferior vena cava venous filter placement, to reduce the possible systemic paradoxical embolization. At 1‐year follow‐up the patient was asymptomatic, with no need for oxygen supplementation and only modest bilateral limb swelling. After the last outpatient visit, he decided to undergo surgery. The intervention consisted in a RSVC section with right pulmonary veins repositioning in left atrium via atrial septal defect. For this purpose, two bovine pericardium patches were used. At the end of the intervention, left and right subclavian veins (the latter through the innominate vein) drained into the left persistent superior vena cava and, through the CS, into the right atrium.
Post‐operative echocardiogram with administration of agitated normal saline from both arms was performed. Administration of normal saline by the right arm did not show simultaneous opacification of right and left chambers anymore. On the contrary, consecutive opacification of the CS and then of the right sections was detected when saline solution was injected from both arms (Figure 4 Panel A and B).
FIGURE 4.
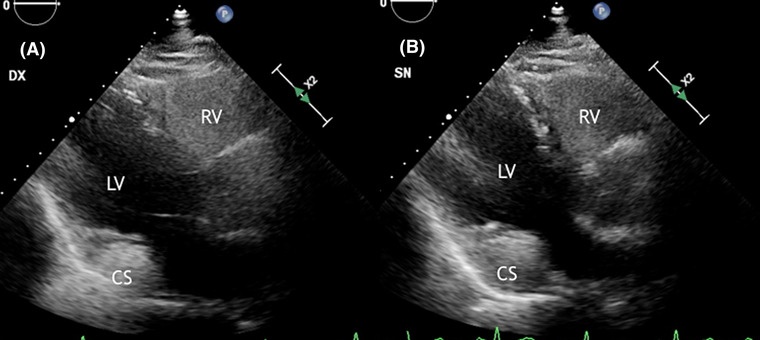
Panel A: Postoperative transthoracic echocardiography in parasternal long‐axis view after administration of agitated normal saline in the left antecubital vein showed complete opacification of the coronary sinus and then, of the right chambers. Panel B: Postoperative transthoracic echocardiography in parasternal long‐axis view after administration of agitated normal saline in the right antecubital vein: showed complete opacification of the coronary sinus and then, of the right chambers and no opacification of the left chambers
2. DISCUSSION
This case highlights the variety of clinical and anatomical presentations of ASDs. ASDs comprise ostium secundum ASDs, ostium primum ASDs, sinus venosus ASDs and CS defects with the former being the most frequent type. 2 Sinus venosus ASDs are rare cardiac abnormalities occurring at the posterior level of the atrial septum, close to the junction of the superior (more frequently) or inferior vena cava with the right atrium. 2 They usually cause left‐to‐right shunt and are often associated with partial anomalous pulmonary venous drainage from the right lung and with anomalous superior vena cava connection to both the atria. 3 , 4 A recent study investigated the variety of anatomical presentation of superior sinus venosus defects in 96 patients showing that anomalous connection of the right upper pulmonary vein was present in all cases and superior vena cava frequently over‐rode the atrial septum. 5
Instead of atrial septation abnormalities, sinus venosus ASDs should be considered as “cavo‐pulmonary venous defects” due to an abnormal embryogenesis of the pulmonary and systemic venous systems. 4 , 6 , 7 These entities comprise some anatomical variation of the same defect (the lack of separation of superior vena cava and right pulmonary veins walls). The clinical presentation depends on the cavo‐pulmonary communication and the veno‐atrial connection: mostly right atrial, biatrial, and mostly left atrial. 6 Various degree of overriding superior or inferior vena cava has been considered as the key feature of sinus venous defects. 8
In the reported case, the presence of RSVC overriding the atrial septum causes a certain grade of desaturation because of venous blood draining in both right and left shunt. The complex association of interatrial communication, overriding RSVC and anomalous vein drainage partially balance systemic and pulmonary flow rate determining only a mild increase of Qp/Qs. The presented case is also characterized by the presence of a PLSVC, draining into the CS. Association of sinus venosus defects with PLSVC has been previously described. 6 , 9 The presence of PLSVC draining directly into the right atrium reduces the amount of venous blood entering in the left atrium through the defect and consequently it could contribute to postpone the clinical manifestations.
In such a situation, the cardiac abnormality may be silent except for modest systemic desaturation or paradoxical embolic events. 9 Generally, ASDs discovered during adulthood, causes shortness of breath, reduced exercise capacity and atrial arrhythmias as first manifestations, due to right chambers enlargement and, in some cases, to the occurrence of pulmonary hypertension. 2 Concomitant pulmonary and systemic embolic events as the first manifestations of this complex cardiac abnormality have been never described.
The presence of both pulmonary and systemic embolic events should raise the suspicion of a hypercoagulation state or the presence of abnormal intra‐cardiac shunt. On the other hand, the detection of dilated CS should promote further cardiac investigation. In fact, dilated CS may occur in the contest of PLSVC (which may be associated with ASD), unroofed CS, coronary artery to CS fistula, impaired RV function and RV overload. 10 In our case, right chamber dilatation with impaired function discovered by echocardiogram could be initially interpreted only as a consequence of the pulmonary embolism. However, the absence of any evidence of significant pulmonary hypertension makes this conclusion less likely. Dilated CS and the presence of concomitant pulmonary and systemic embolisms suggested a more complex clinical situation and the presence of a possible intra‐cardiac defect. Contrast echocardiography using agitated normal saline is a useful tool for bedside evaluation of intra‐cardiac shunt, especially in intensive care setting, 11 even if the most widespread use is the diagnosis of patent foramen ovale. Correct evaluation of the cardiac chamber enhancement sequences may be a powerful tool even in more complex cardiac abnormalities, as in the presented case.
3. CONCLUSION
Sinus venous defects can present themselves with different anatomical configuration in the context of a cavo‐pulmonary malformation. As a consequence, clinical presentation can vary, and diagnosis may be challenging. Different grades of overriding superior vena cava can be associated with systemic desaturation and the bridge between the pulmonary and systemic circulation allows paradoxical embolization. The presence of concomitant pulmonary embolism may further complicate the clinical presentation due to its hemodynamic effect on the right ventricle. The use of contrast echocardiography with agitated normal saline could be a useful and bed‐side tool in diagnosis of septation defect also in the context of complex congenital abnormalities.
CONFLICTS OF INTEREST
Nothing to Disclose.
Supporting information
Supporting Information
Supporting Information
ACKNOWLEDGMENTS
Open Access Funding provided by Universita degli Studi di Roma La Sapienza within the CRUI‐CARE Agreement.
Filomena D, Monosilio S, Sannino M, et al. Complex connections: a young man presenting with shortness of breath, hypoxemia, right lumbar pain and left limb swelling. Echocardiography. 2022;39:631–636. 10.1111/echo.15330
[Correction added on 16 May 2022, after first online publication: CRUI funding statement has been added.]
REFERENCES
- 1. Konstantinides SV, Meyer G, Bueno H, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543‐603. [DOI] [PubMed] [Google Scholar]
- 2. Brida M, Chessa M, Celermajer D, et al. Atrial septal defect in adulthood: a new paradigm for congenital heart disease. Eur Heart J. 2021:1‐14. [DOI] [PubMed] [Google Scholar]
- 3. Jost CHA, Connolly HM, Danielson GK, et al. Sinus venosus atrial septal defect: long‐term postoperative outcome for 115 patients. Circulation. 2005;112(13):1953‐1958. [DOI] [PubMed] [Google Scholar]
- 4. Kanakis M, Martens T, Laskari C, et al. Right superior vena cava draining into the left atrium in a patient with sinus venosus defect. J Card Surg. 2020;35(11):3224‐3226. [DOI] [PubMed] [Google Scholar]
- 5. Relan J, Gupta SK, Rajagopal R, et al. Clarifying the anatomy of the superior sinus venosus defect. Heart. 2021. heartjnl‐2021‐319334. [DOI] [PubMed] [Google Scholar]
- 6. Van Praagh S, Geva T, Lock JE, Del Nido PJ, Vance MS, Van Praagh R. Biatrial or left atrial drainage of the right superior vena cava: anatomic, morphogenetic, and surgical considerations—report of three new cases and literature review. Pediatr Cardiol. 2003;24(4):350‐363. [DOI] [PubMed] [Google Scholar]
- 7. Butts RJ, Crean AM, Hlavacek AM, et al. Veno‐venous bridges: the forerunners of the sinus venosus defect. Cardiol Young. 2011;21(6):623‐630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang H, Guan H, Wang DW. Partial anomalous pulmonary venous connection to superior vena cava that overrides across the intact atrial septum and has bi‐atrial connection in a 75‐year‐old female presenting with pulmonary hypertension. BMC Cardiovasc Disord. 2014;14(1):1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oliver JM, Gallego P, Gonzalez A, Dominguez FJ, Aroca A, Mesa JM. Sinus venosus syndrome: atrial septal defect or anomalous venous connection? A multiplane transoesophageal approach. Heart. 2002;88(6):634‐638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kolski BC, Khadivi B, Anawati M, Daniels LB, Demaria AN, Blanchard DG. The dilated coronary sinus: utility of coronary sinus cross‐sectional area and eccentricity index in differentiating right atrial pressure overload from persistent left superior vena cava. Echocardiography. 2011;28(8):829‐832. [DOI] [PubMed] [Google Scholar]
- 11. Montrief T, Alerhand S, Denault A, Scott J. Point‐of‐care echocardiography for the evaluation of right‐to‐left cardiopulmonary shunts: a narrative review. Can J Anesth. 2020;67(12):1824‐1838. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information


