Abstract
Objective
To investigate the pattern of accuracy change in artificial intelligence-assisted landmark identification (LI) using a convolutional neural network (CNN) algorithm in serial lateral cephalograms (Lat-cephs) of Class III (C-III) patients who underwent two-jaw orthognathic surgery.
Methods
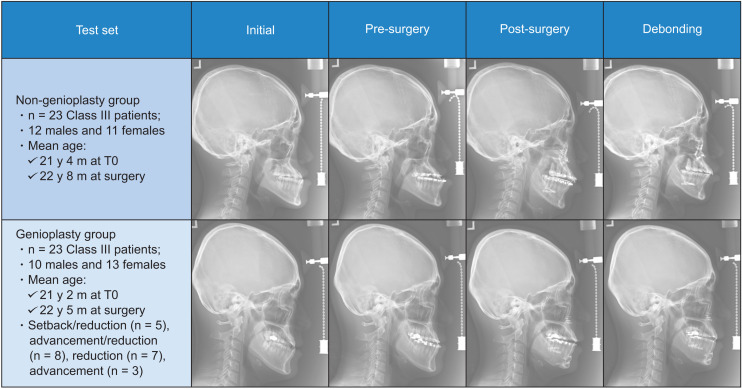
A total of 3,188 Lat-cephs of C-III patients were allocated into the training and validation sets (3,004 Lat-cephs of 751 patients) and test set (184 Lat-cephs of 46 patients; subdivided into the genioplasty and non-genioplasty groups, n = 23 per group) for LI. Each C-III patient in the test set had four Lat-cephs initial (T0), pre-surgery (T1, presence of orthodontic brackets [OBs]), post-surgery (T2, presence of OBs and surgical plates and screws [S-PS]), and debonding (T3, presence of S-PS and fixed retainers [FR]). After mean errors of 20 landmarks between human gold standard and the CNN model were calculated, statistical analysis was performed.
Results
The total mean error was 1.17 mm without significant difference among the four time-points (T0, 1.20 mm; T1, 1.14 mm; T2, 1.18 mm; T3, 1.15 mm). In comparison of two time-points ([T0, T1] vs. [T2, T3]), ANS, A point, and B point showed an increase in error (p < 0.01, 0.05, 0.01, respectively), while Mx6D and Md6D showeda decrease in error (all p < 0.01). No difference in errors existed at B point, Pogonion, Menton, Md1C, and Md1R between the genioplasty and non-genioplasty groups.
Conclusions
The CNN model can be used for LI in serial Lat-cephs despite the presence of OB, S-PS, FR, genioplasty, and bone remodeling.
Keywords: Convolutional neural network, Landmark identification, Two-jaw orthognathic surgery, Serial lateral encephalogram
INTRODUCTION
Owing to the high prevalence of Class III malocclusion and negative social recognition of the prognathic appearance,1,2 Korea has become one of the countries that performs two-jaw orthognathic surgery (TJ-OGS) extensively in patients with skeletal Class III malocclusion. To obtain a successful treatment outcome, the following four steps should be performed precisely: (1) diagnosis and gross treatment planning for pre-surgical orthodontic treatment and orthognathic surgery using initial cephalograms, (2) planning for the direction and amount of surgical movement using pre-surgical cephalograms, (3) assessment of surgical outcome and planning for post-surgical orthodontic treatment using post-surgical cephalograms, and (4) comprehensive assessment of orthodontic treatment and orthognathic surgery using debonding cephalograms.3,4 Furthermore, superimposition of serial cephalograms taken at different time-points is also important to assess the outcomes of pre- and post-surgical orthodontic treatment and orthognathic surgery. Accurate detection of cephalometric landmarks is mandatory to perform these procedures.
An artificial intelligence (AI) algorithm including convolutional neural network (CNN) can help clinicians detect cephalometric landmarks with an accuracy that is close to that of human experts.5-12 Previous AI studies have regarded the accuracy within a range of 2 mm as a clinically acceptable performance in landmark identification.8,12-15 However, it appears to be a lenient standard for appropriate clinical use. Therefore, use of stricter criteria (i.e., range within at least 1.5 mm) is necessary in determining the accuracy of landmark identification for clinical relevance.
In addition, most AI studies on the accuracy of automated landmark identification8,13-15 have trained and tested their models using initial lateral cephalograms only, which do not have orthodontic brackets (OB), surgical plates and screws (S-PS), fixed retainer (FR), and bone remodeling changes. To the best of our knowledge, no study has compared the accuracy of automated landmark identification in serial cephalograms at the four time-points covering from the initial, pre-surgery, post-surgery, to debonding stages in orthognathic surgery cases. Therefore, the purpose of the study was to investigate the pattern of accuracy change in AI-assisted landmark identification in serial lateral cephalograms of Class III patients who underwent pre- and post-surgical orthodontic treatment and TJ-OGS using a cascade CNN algorithm and strict criteria for determining the degree of accuracy.
MATERIALS AND METHODS
Data set
A total of 3,188 lateral cephalograms of 797 patients with Class III malocclusion were used for the training and validation sets and the test set for automated landmark identification using the CNN model. The inclusion criteria were as follows: (1) Class III patient who underwent pre- and post-surgical orthodontic treatment and TJ-OGS with/without genioplasty and (2) Class III patient whose serial lateral cephalograms were available. The exclusion criterion was Class III patient who had craniofacial deformities.
The training and validation sets for automated landmark identification by the CNN model included 3,004 lateral cephalograms of 751 Class III patients from 10 institutions (Table 1). Some of the patients who belonged to the training or validation set had more than four lateral cephalograms because additional progress lateral cephalograms were taken between time-points, while some of them had missing lateral cephalograms at specific timepoints.
Table 1.
Composition of the training, validation, and test dataset
| Institution | Training set | Validation set | Test set | Sum | |
|---|---|---|---|---|---|
| Seoul National University Dental Hospital | 1,292 | 100 | 52 | 1,444 | |
| Kyung Hee University Dental Hospital | 607 | 100 | 48 | 755 | |
| Kyungpook National University Dental Hospital | 133 | 30 | 20 | 183 | |
| Asan Medical Center | 144 | 32 | 24 | 200 | |
| Ewha University Medical Center | 116 | 20 | 12 | 148 | |
| Wonkwang University Dental Hospital | 95 | 26 | 8 | 129 | |
| Ajou University Dental Hospital | 84 | 20 | 12 | 116 | |
| Korea University Anam Hospital | 62 | 25 | 0 | 87 | |
| Chonnam National University Dental Hospital | 48 | 16 | 8 | 72 | |
| Chosun University Dental Hospital | 45 | 9 | 0 | 54 | |
| Total | Lateral cephalograms | 2,626 | 378 | 184 | 3,188 |
| Class III patients | 751* | 46 | 797 | ||
*Class III patients had various numbers of lateral cephalograms, which belonged to the training or validation set.
For the test set, Class III patients with cephalograms obtained at the following timepoints were selected: initial (T0), pre-surgery (T1, taken at least 1 month before TJ-OGS; presence of OBs), post-surgery (T2, taken at least 2 months after TJ-OGS; presence of OBs and S-PS), and debonding (T3, presence of S-PS, FR, and bone remodeling change). As a result, the test set consisted of 184 cephalograms of 46 Class III patients from eight institutions (Table 1). It was subdivided into the genioplasty and non-genioplasty groups (n = 23 patients per group). Their characteristics are enumerated in Figure 1.
Figure 1.
Composition of the test set.
T0, initial.
Ethical approval
This nationwide multicenter study was reviewed and approved by the Institutional Review Board (IRB) Committee of 10 institutions: Seoul National University Dental Hospital (ERI18002), Kyung Hee University Dental Hospital (KH-DT19006), Kyungpook National University Dental Hospital (KNUDH-2019-03-02-00), Asan Medical Center (2019-0408), Ewha University Medical Center (EUMC 2019-04-017-009), Wonkwang University Dental Hospital (WKDIRB201903-01), Ajou University Dental Hospital (AJIRB-MED-MDB-19-039), Korea University Anam Hospital (K2019-0543-010), Chonnam National University Dental Hospital (CNUDH-EXP-2021-001), and Chosun University Dental Hospital (CUDHIRB 1901 005 R01).
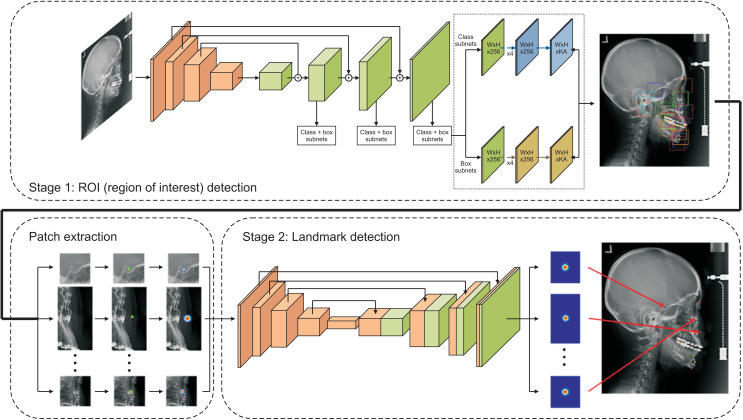
Cascade CNN
Data sets were obtained from 10 centers using anonymized Digital Imaging and Communications in Medicine (DICOM) file format. Since finding the exact location of landmarks in a large lateral cephalogram image is relatively difficult, a fully automated landmark prediction algorithm with the cascade network was developed.12 Two steps were followed: 1) detection of the region of interest (256 × 256 and 512 × 512 pixels depending on the landmark) using the RetinaNet16 and 2) prediction of the landmark using the U-Net17 (Figure 2).
Figure 2.
General schematic of the cascade convolution neural network algorithm for artificial intelligence-assisted landmark identification.
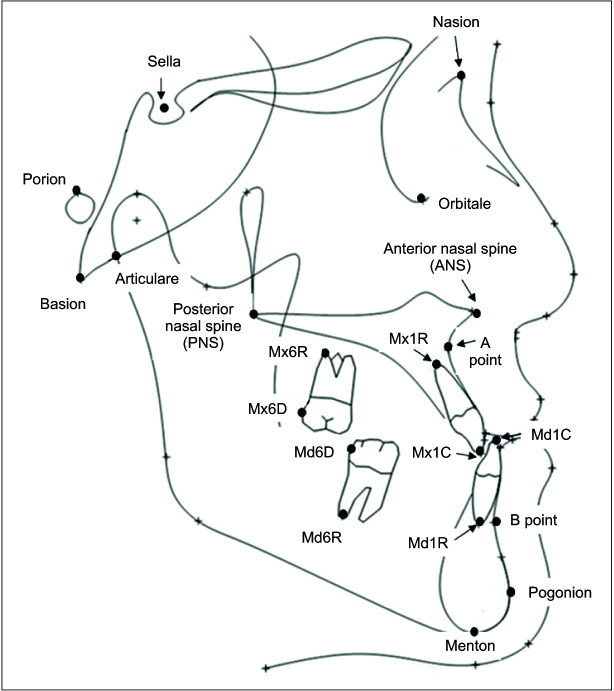
Cephalometric landmarks
Definitions of 12 skeletal and eight dental landmarks are presented in Figure 3 and Table 2. The landmarks were digitized by a single orthodontist who had 20 years of experience (human gold standard, HMH) and by the CNN model.
Figure 3.
The skeletal and dental landmarks.
See Table 2 for definitions of the other landmarks.
Table 2.
The definition of cephalometric landmarks
| Compartment | Landmark | Description | ||
|---|---|---|---|---|
| Skeletal landmark | Cranial base | Nasion (N) | The most anterior point on the frontonasal suture in the midsagittal plane | |
| Sella (S) | Center of the Sella Turcica | |||
| Porion (Por) | The most superior point of the external auditory meatus | |||
| Orbitale (Or) | The most inferior point of the orbital cavity contour | |||
| Basion (Ba) | The most posterior and inferior point of the occipital bone | |||
| Maxilla | Anterior | ANS | The tip of anterior nasal spine | |
| A point | The deepest point between ANS and the upper incisal alveolus | |||
| Posterior | PNS | The most posterior point of the hard palate | ||
| Mandible | Anterior | B point | The deepest point between Pogonion and the lower incisal alveolus | |
| Pogonion (Pog) | The most anterior point on the symphysis | |||
| Posterior | Articulare (Ar) | Intersection between the inferior cranial base surface and the posterior surface of condyle | ||
| Bottom | Menton (Me) | The most inferior point on the symphysis | ||
| Dental landmark | Maxillary dentition | Anterior | Mx1C | Crown tip of the maxillary central incisor |
| Mx1R | Root apex of the maxillary central incisor | |||
| Posterior | Mx6D | Distal contact point of the maxillary first molar | ||
| Mx6R | Distobuccal root apex of the maxillary first molar | |||
| Mandibular dentition | Anterior | Md1C | Crown tip of the mandibular central incisor | |
| Md1R | Root apex of the mandibular central incisor | |||
| Posterior | Md6D | Distal contact point of the mandibular first molar | ||
| Md6R | Distal root apex of the mandibular first molar | |||
Measurement variables (Table 3)
Table 3.
The absolute values of error, distribution of error, accuracy percentage, and degree of accuracy for each landmark
| Compartment | Land-mark | Absolute value of error (Err) | Distribution | Accuracy | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD (mm) | Excellent (Err <1.0 mm) |
Good (1.0 ≤ Err < 1.5 mm) |
Fair (1.5 ≤ Err < 2.0 mm) |
Acceptable (2.0 ≤ Err < 2.5 mm) |
Unacceptable (2.5 mm ≤ Err) |
Accuracy percentage | Degree of accuracy | ||||||
| Skeletal landmark | Cranial base | Nasion | 0.59 ± 0.48 | 157 (85.3) | 18 (9.8) | 4 (2.2) | 3 (1.6) | 2 (1.1) | 175 (95.1) | Very high | |||
| Sella | 0.46 ± 0.23 | 180 (97.8) | 4 (2.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 184 (100) | Very high | |||||
| Porion | 1.07 ± 0.69 | 103 (56.0) | 37 (20.1) | 24 (13.0) | 14 (7.6) | 6 (3.3) | 140 (76.1) | High | |||||
| Orbitale | 1.21 ± 1.01 | 92 (50.0) | 44 (23.9) | 21 (11.4) | 12 (6.5) | 15 (8.2) | 136 (73.9) | High | |||||
| Basion | 1.64 ± 1.61 | 82 (44.6) | 34 (18.5) | 21 (11.4) | 13 (7.1) | 34 (18.5) | 116 (63.1) | Medium | |||||
| Maxilla | Anterior | ANS | 1.39 ± 1.01 | 72 (39.1) | 48 (26.1) | 23 (12.5) | 14 (7.6) | 27 (14.7) | 120 (65.2) | Medium | |||
| A point | 1.41 ± 0.99 | 86 (46.7) | 30 (16.3) | 22 (12.0) | 18 (9.8) | 28 (15.2) | 116 (63.0) | Medium | |||||
| Posterior | PNS | 1.19 ± 0.89 | 97 (52.7) | 37 (20.1) | 24 (13.0) | 13 (7.1) | 13 (7.1) | 134 (72.7) | High | ||||
| Mandible | Anterior | B point | 1.15 ± 0.96 | 106 (57.6) | 36 (19.6) | 21 (11.4) | 8 (4.3) | 13 (7.1) | 142 (77.2) | High | |||
| Pogonion | 0.79 ± 0.68 | 140 (76.1) | 28 (15.2) | 7(3.8) | 1 (0.5) | 8 (4.3) | 168 (91.3) | Very high | |||||
| Bottom | Menton | 0.77 ± 0.44 | 143 (77.7) | 29 (15.8) | 8 (4.3) | 3 (1.6) | 1 (0.5) | 172 (93.5) | Very high | ||||
| Posterior | Articulare | 0.77 ± 0.45 | 138 (75.0) | 34 (18.5) | 10 (5.4) | 1 (0.5) | 1 (0.5) | 172 (93.5) | Very high | ||||
| Dental landmark | Maxillary dentition | Anterior | Mx1C | 0.44 ± 0.37 | 178 (96.7) | 2 (1.1) | 2 (1.1) | 1 (0.5) | 1 (0.5) | 180 (97.8) | Very high | ||
| Mx1R | 1.55 ± 1.09 | 63 (34.2) | 43 (23.4) | 36 (19.6) | 12 (6.5) | 30 (16.3) | 106 (57.6) | Medium | |||||
| Posterior | Mx6D | 1.43 ± 1.08 | 76 (41.3) | 42 (22.8) | 23 (12.5) | 17 (9.2) | 26 (14.1) | 118 (64.1) | Medium | ||||
| Mx6R | 1.68 ± 1.08 | 51 (27.7) | 44 (23.9) | 35 (19.0) | 19 (10.3) | 35 (19.0) | 95 (51.6) | Medium | |||||
| Mandibular dentition | Anterior | Md1C | 0.49 ± 0.64 | 172 (93.5) | 7 (3.8) | 0 (0.0) | 2 (1.1) | 3 (1.6) | 179 (97.3) | Very high | |||
| Md1R | 1.57 ± 1.04 | 64 (34.8) | 43 (23.4) | 29 (15.8) | 18 (9.8) | 30 (16.3) | 107 (58.2) | Medium | |||||
| Posterior | Md6D | 1.67 ± 1.24 | 54 (29.3) | 41 (22.3) | 33 (17.9) | 30 (16.3) | 26 (14.1) | 95 (51.6) | Medium | ||||
| Md6R | 2.03 ± 1.35 | 46 (25.0) | 30 (16.3) | 25 (13.6) | 28 (15.2) | 55 (29.9) | 76 (41.3) | Low | |||||
| Total | 1.17 ± 1.04 | 2,100 (57.1) | 631 (17.1) | 368 (10.0) | 227 (6.2) | 354 (9.6) | 2,731 (74.2) | High | |||||
Values are presented as number (%).
Err, absolute value of error; SD, standard deviation; Accuracy percentage (AP); error range within 1.5 mm was considered accurate.
The degree of accuracy was defined as very high (90% ≤ AP), high (70% ≤ AP < 90%), medium (50% ≤ AP < 70%), and low (AP < 50%).
See Table 2 for definitions of each landmark.
The mean values of absolute errors for each landmark were calculated using the absolute distance between the human gold standard and AI-assisted detection. The degree of error was allocated into excellent (< 1.0 mm), good (1.0–1.5 mm), fair (1.5–2.0 mm), acceptable (2.0–2.5 mm), and unacceptable (> 2.5 mm) groups. Then, the accuracy percentage (AP) was calculated using a formula (percentage of the excellent and good groups among the total degree of error groups), which means that the error range within 1.5 mm was considered accurate. The degree of accuracy was defined as “very high” (AP > 90%), “high” (AP, 70–90%), “medium” (AP, 50–70%), and “low” (AP < 50%).
Intra-examiner reliability
Twenty randomly selected lateral cephalogram images were re-digitized with an interval of 2 weeks by the same operator (HMH). Since no significant difference was found in the values of the x- and y-coordinates between the first and second measurements in the Wilcoxon signed rank test (p > 0.05), the first set of measurements was used for further analysis.
Statistics
Repeated measures analysis of variance (ANOVA), and post-hoc test for within-subject by Tukey's adjustment for multiple comparisons were performed to find out the difference between T0, T1, T2, and T3 stages. Repeated measures multivariate analysis of variance (MANOVA) was performed to compare between ‘before-surgery group', including T0 and T1, and ‘after-surgery group', including T2 and T3. Statistical analysis was done using SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA) and SAS 9.4 (SAS Institute Inc., Cary, NC, USA.) and p-values of < 0.05 were considered statistically significant.
RESULTS
Evaluation of total landmarks (Table 3)
The total landmarks showed a good mean error value (1.17 mm), and the total AP had a high degree of accuracy (74.2%).
Evaluation of skeletal landmarks (Table 3)
Nasion and Sella showed an excellent mean error value and a very high degree of accuracy (0.59 mm and 95.1%; 0.46 mm and 100%, respectively), while Porion and Orbitale showed a good mean error value and a high degree of accuracy (1.07 mm and 76.1%; 1.21 mm and 73.9%, respectively). On the other hand, Basion showed a fair mean error value (1.64 mm) and a medium degree of accuracy (63.1%).
ANS and A point showed a good mean error value and a medium degree of accuracy (1.39 mm and 65.2%; 1.41 mm and 63.0%, respectively). PNS had a good mean error value (1.19 mm) and a high degree of accuracy (72.7%).
Pogonion, Menton, and Articulare showed an excellent mean error value and a very high degree of accuracy (0.79 mm and 91.3%; 0.77 mm and 93.5%; and 0.77 mm and 93.5%, respectively). B point showed a good mean error value (1.15 mm) and a high degree of accuracy (77.2 %).
Evaluation of dental landmarks (Table 3)
Mx1C showed an excellent mean error value (0.44 mm) and a very high degree of accuracy (97.8%), while Mx6D had a good mean error value (1.43 mm) and a medium degree of accuracy (64.1%). On the other hand, Mx1R and Mx6R had a fair mean error value and a medium degree of accuracy (1.55 mm and 57.6%; 1.68 mm and 51.6%, respectively).
Md1C demonstrated an excellent mean error value (0.49 mm) and a very high degree of accuracy (97.3%), while Md1R had a fair mean error value (1.57 mm) and a medium degree of accuracy (58.2%). Md6D had a fair mean error value (1.67 mm) and medium accuracy (51.6%), and Md6R exhibited an acceptable mean error value (2.03 mm) and a low degree of accuracy (41.3%).
Comparison of the mean errors among the four timepoints (T0, T1, T2, and T3) (Table 4)
Table 4.
Comparison of mean errors among the four time-points (T0, T1, T2 and T3) and between two time-points ([T0, T1] vs. [T2, T3])
| Compartment | Landmark | Initial stage (T0) |
Pre-surgery stage (T1) | Post-surgery stage (T2) | Debonding stage (T3) | Multiple comparison | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Among T0, T1, T2 and T3 stages† | (T0, T1) vs. (T2, T3)‡ | |||||||||||||||
| Mean ± SD (mm) | Mean ± SD (mm) | Mean ± SD (mm) | Mean ± SD (mm) | p-value | Tukey HSD test |
p-value | Contrast matrix with the MANOVA | |||||||||
| Skeletal landmark | Cranial base | Nasion | 0.58 ± 0.42 | 0.59 ± 0.48 | 0.55 ± 0.39 | 0.64 ± 0.60 | 0.698 | 0.852 | ||||||||
| Sella | 0.48 ± 0.23 | 0.43 ± 0.19 | 0.41 ± 0.20 | 0.50 ± 0.27 | 0.155 | 0.986 | ||||||||||
| Porion | 1.04 ± 0.55 | 1.07 ± 0.76 | 1.17 ± 0.85 | 1.01 ± 0.57 | 0.493 | 0.566 | ||||||||||
| Orbitale | 1.19 ± 0.88 | 1.15 ± 0.88 | 1.39 ± 1.40 | 1.10 ± 0.76 | 0.454 | 0.618 | ||||||||||
| Basion | 1.41 ± 1.32 | 1.59 ± 1.60 | 1.95 ± 1.94 | 1.61 ± 1.52 | 0.148 | 0.092 | ||||||||||
| Maxilla | Anterior | ANS | 1.07 ± 0.78 | 1.22 ± 0.97 | 1.78 ± 1.22 | 1.49 ± 0.87 | 0.003** | T0a, T1a, T2b, and T3ab |
0.003** | (T0, T1) < (T2, T3) |
||||||
| A point | 1.27 ± 0.89 | 1.28 ± 0.78 | 1.50 ± 1.07 | 1.59 ± 1.16 | 0.151 | 0.040* | (T0, T1) < (T2, T3) |
|||||||||
| Posterior | PNS | 1.16 ± 0.79 | 1.14 ± 0.87 | 1.29 ± 1.09 | 1.17 ± 0.82 | 0.823 | 0.587 | |||||||||
| Mandible | Anterior | B point | 1.00 ± 0.97 | 1.01 ± 0.61 | 1.29 ± 1.24 | 1.31 ± 0.91 | 0.142 | 0.008** | (T0, T1) < (T2, T3) |
|||||||
| Pogonion | 0.66 ± 0.48 | 0.80 ± 0.72 | 0.82 ± 0.69 | 0.86 ± 0.77 | 0.277 | 0.260 | ||||||||||
| Bottom | Menton | 0.83 ± 0.52 | 0.70 ± 0.39 | 0.74 ± 0.38 | 0.82 ± 0.45 | 0.298 | 0.786 | |||||||||
| Posterior | Articulare | 0.76 ± 0.39 | 0.75 ± 0.42 | 0.73 ± 0.40 | 0.84 ± 0.58 | 0.540 | 0.616 | |||||||||
| Dental landmark | Maxillary dentition | Anterior | Mx1C | 0.48 ± 0.37 | 0.49 ± 0.55 | 0.41 ± 0.26 | 0.38 ± 0.18 | 0.355 | 0.096 | |||||||
| Mx1R | 1.83 ± 1.24 | 1.37 ± 1.14 | 1.56 ± 1.02 | 1.54 ± 1.17 | 0.166 | 0.714 | ||||||||||
| Posterior | Mx6D | 1.66 ± 1.18 | 1.63 ± 1.31 | 1.20 ± 0.80 | 1.23 ± 0.88 | 0.032* | T0b, T1ab, T2a, and T3ab |
0.008** | (T2, T3) < (T0, T1) |
|||||||
| Mx6R | 1.89 ± 1.15 | 1.65 ± 1.08 | 1.57 ± 1.03 | 1.60 ± 1.05 | 0.349 | 0.194 | ||||||||||
| Mandibular dentition | Anterior | Md1C | 0.48 ± 0.45 | 0.62 ± 1.10 | 0.47 ± 0.39 | 0.37 ± 0.31 | 0.215 | 0.096 | ||||||||
| Md1R | 1.77 ± 1.22 | 1.52 ± 1.00 | 1.37 ± 0.96 | 1.63 ± 0.95 | 0.303 | 0.400 | ||||||||||
| Posterior | Md6D | 2.15 ± 1.79 | 1.71 ± 0.91 | 1.51 ± 1.14 | 1.33 ± 0.75 | 0.008** | T0b, T1ab, T2a, and T3a |
0.003** | (T2, T3) < (T0, T1) |
|||||||
| Md6R | 2.21 ± 1.64 | 2.08 ± 1.36 | 1.94 ± 1.25 | 1.89 ± 1.12 | 0.579 | 0.242 | ||||||||||
| Total | 1.20 ± 1.10 | 1.14 ± 1.02 | 1.18 ± 1.09 | 1.15 ± 0.95 | 0.376 | 0.895 | ||||||||||
No significant difference was found in the overall mean errors (p > 0.05). Only three landmarks, namely ANS, Mx6D, and Md6D showed a significant difference in the mean errors among the four timepoints (ANS, increase in the mean error from T0 and T1 to T2, p < 0.01; Mx6D, decrease in the mean error from T0 to T2, p < 0.05; Md6D, decrease in the mean error from T0 to T2 and T3, p < 0.01).
Comparison of the mean errors between the two timepoints ([T0, T1] vs. [T2, T3]) (Table 4)
ANS, A point, and B point showed an increase in the mean error after TJ-OGS (ANS, p < 0.01; A point, p < 0.05; B point, p < 0.01), while Mx6D and Md6D showed a decrease in the mean error after TJ-OGS (all p < 0.01).
Comparison of the mean errors between the genioplasty and non-genioplasty groups (Table 5)
Table 5.
Comparison of mean errors in each time-point (from T0 to T3) between the genioplasty and non-genioplasty groups
| Genioplasty group | Non-genioplasty group | p-value† | ||
|---|---|---|---|---|
| B point | Initial stage (T0) | 0.87 ± 0.46 | 1.13 ± 1.30 | 0.386 |
| Pre-surgery stage (T1) | 0.99 ± 0.60 | 1.03 ± 0.63 | 0.855 | |
| Post-surgery stage (T2) | 1.21 ± 0.70 | 1.37 ± 1.63 | 0.670 | |
| Debonding stage (T3) | 1.25 ± 0.82 | 1.37 ± 1.01 | 0.682 | |
| p-value‡ | 0.184 | 0.543 | ||
| Pog | Initial stage (T0) | 0.61 ± 0.38 | 0.71 ± 0.57 | 0.468 |
| Pre-surgery stage (T1) | 0.66 ± 0.39 | 0.95 ± 0.93 | 0.171 | |
| Post-surgery stage (T2) | 0.81 ± 0.82 | 0.84 ± 0.56 | 0.898 | |
| Debonding stage (T3) | 0.95 ± 0.87 | 0.77 ± 0.66 | 0.436 | |
| p-value‡ | 0.109 | 0.463 | ||
| Menton | Initial stage (T0) | 0.71 ± 0.35 | 0.95 ± 0.63 | 0.117 |
| Pre-surgery stage (T1) | 0.71 ± 0.47 | 0.68 ± 0.28 | 0.813 | |
| Post-surgery stage (T2) | 0.68 ± 0.38 | 0.79 ± 0.38 | 0.334 | |
| Debonding stage (T3) | 0.82 ± 0.48 | 0.81 ± 0.43 | 0.926 | |
| p-value‡ | 0.578 | 0.186 | ||
| Md1C | Initial stage (T0) | 0.58 ± 0.53 | 0.39 ± 0.33 | 0.149 |
| Pre-surgery stage (T1) | 0.38 ± 0.18 | 0.87 ± 1.52 | 0.138 | |
| Post-surgery stage (T2) | 0.39 ± 0.25 | 0.56 ± 0.48 | 0.155 | |
| Debonding stage (T3) | 0.30 ± 0.14 | 0.44 ± 0.41 | 0.137 | |
| p-value‡ | 0.062 | 0.156 | ||
| Md1R | Initial stage (T0) | 1.64 ± 1.13 | 1.90 ± 1.32 | 0.484 |
| Pre-surgery stage (T1) | 1.22 ± 0.68 | 1.83 ± 1.18 | 0.040* | |
| Post-surgery stage (T2) | 1.61 ± 1.03 | 1.12 ± 0.84 | 0.082 | |
| Debonding stage (T3) | 1.53 ± 0.88 | 1.73 ± 1.03 | 0.484 | |
| p-value‡ | 0.380 | 0.091 | ||
Values are presented as mean ± standard deviation.
*p < 0.05.
†Comparison between genioplasty and nongenioplasty groups by independent t-test.
‡Comparison mean error among T0, T1, T2, and T3 stages by repeated measures analysis of variance (ANOVA).
See Table 2 for definitions of each landmark.
No significant difference in the mean errors in the landmarks located adjacent to the genioplasty area (B point, Pogonion, Menton, Md1C, and Md1R) existed in each timepoint between the two groups, except Md1R at T1 (p < 0.05).
DISCUSSION
Since TJ-OGS induces the position change and bone remodeling in the skeletal structures and produces the metallic images of the OB, SP-S, and FR, the accuracy and reliability of cephalometric landmark identification in serial lateral cephalograms are important for assessment of treatment outcomes.18
As total landmarks exhibited a good mean error value and a high degree of accuracy (1.17 mm and 74.2%, respectively, Table 3) without significant difference among the four time-points (T0, 1.20 mm; T1, 1.14 mm; T2, 1.18 mm; T3, 1.15 mm; p > 0.05, Table 4), accuracy of the AI-assisted digitization was not significantly affected by the presence of OB, SP-S, FR, and bone remodeling change during orthodontic treatment and TJ-OGS.
Regardless of the degree of accuracy of each landmark (Table 3), none of the five cranial base landmarks exhibited a significant difference in the mean errors among the four time-points (T0, T1, T2, and T3) and between the two time-points ([T0, T1] vs. [T2, T3]) (Table 4). Accuracy of the cranial base landmarks can be regarded as baseline for comparison of serial lateral cephalograms because the positions of these cranial base landmarks are not affected by TJ-OGS.
Three error patterns were found in the maxillary skeletal landmarks. First, the mean errors of ANS were different among the four time-points (T0, 1.07 mm; T1, 1.22 mm; T2, 1.78 mm; T3, 1.49 mm; p < 0.01, Table 4) and presented an increased error value after TJ-OGS than before it ([T0, T1] vs. [T2, T3]; p < 0.01, Table 4). This suggested that the metal image of the SP-S adjacent to ANS as well as surgical shape modification of ANS19,20 (Figure 1) could affect the accuracy of AI-assisted landmark detection. Second, although the error of A point was not significantly different among the four time-points (T0, 1.27 mm; T1, 1.28 mm; T2, 1.50 mm; T3, 1.59 mm; Table 4), it presented an increase in the mean error value after TJ-OGS than before it ([T0, T1] vs. [T2, T3]; p < 0.05, Table 4). This occurred because A point might be less affected by the metal image of the SP-S installed at the maxilla and have a lower chance for surgical shape modification, compared to ANS (Figure 1). Furthermore, A point might be less affected by the metal image of SP-S installed lateral to the pyriform aperture in the maxilla and have a lower chance for surgical shape modification relative to ANS. Third, in case of posterior impaction and/or anteroposterior movement of the maxilla, the position of PNS had to be changed. However, for PNS, no significant difference was found either among the four time-points (T0, 1.16 mm; T1, 1.14 mm; T2, 1.29 mm; T3, 1.17 mm; p > 0.05, Table 4) or between the two time-points ([T0, T1] vs. [T2, T3]; p > 0.05, Table 4). No significant difference in accuracy between time points means that the amount error of landmark at four or two timepoints was neither significantly increased nor decreased. This might be due to (1) an absence of the metal image of the SP-S within the region of interest of PNS and (2) an easily defined the end point of the hard palate.
There are three explanations for the errors in the mandibular skeletal landmarks. First, since there were no metal images within the region of interest of Articulare and Menton, their mean errors were not significantly different among the four time-points and between the two time-points (all p > 0.05, Table 4). Second, the mean error of Pogonion was not significantly different among the four time-points and between the two time-points (p > 0.05, Table 4), which suggests that the metal image of the SP-S adjacent to Pognion (Figure 1) might not affect the accuracy of AI-assisted landmark detection. Third, although the mean errors of B point did not significantly differ among the four time-points (T0, 1.00 mm; T1, 1.01 mm; T2, 1.29 mm; T3, 1.31 mm; p > 0.05, Table 4), comparison of the two time-points revealed an increase in error after TJ-OGS ([T0, T1] vs. [T2, T3]; p < 0.01, Table 4). These findings suggest that the metal image of the SP-S adjacent to the B point (Figure 1) might affect the accuracy of AI-assisted landmark detection.
There are two sources of errors in the dental landmarks. First, regardless of the degree of accuracy in the dental landmarks (Table 3), Mx1C, Md1C, Mx1R, Md1R, Mx6R, and Md6R did not exhibit significant difference in the mean errors among the four time-points and between the two time-points (all p > 0.05, Table 4). Second, the mean errors of Mx6D and Md6D were significantly different among the four time-points (Mx6D: T0, 1.66 mm; T1, 1.63 mm; T2, 1.20 mm; T3, 1.23 mm; Md6D, T0, 2.15 mm; T1, 1.71 mm; T2, 1.51 mm; T3, 1.33 mm; all p < 0.01, Table 4) and presented decreased mean error values after TJ-OGS ([T0, T1] vs. [T2, T3]; all p < 0.01, Table 4). The possible reasons for these might be the following: (1) Horizontal and vertical overlapping of the right and left maxillary and mandibular first molars made it difficult to accurately locate the Mx6D and Mn6D at T0 lateral cephalogram; and (2) Orthodontic treatment and TJ-OGS improved the alignment of the maxillary and mandibular dentition and corrected the cant, shift and yaw of the maxilla and mandible, reducing the double images of the maxillary and mandibular first molars.
No significant difference was found in the mean errors in the landmarks adjacent to the genioplasty area including B point, Pogonion, Menton, Md1C, and Md1R (all p > 0.05, Table 5). The possible reasons for this are as follows: (1) Menton and Md1C were located relatively far from the SP-S installed at the symphysis and their shapes were not affected by orthognathic surgery; (2) Since Pogonion and B point are the most forward and deepest points on the anterior surface of the symphysis, respectively, they can be easily identified despite the presence of the metal image of the SP-S; and (3) Although Md1R had a fair mean error value and a medium degree of accuracy (1.57 mm and 58.2%, respectively), these patterns were not aggravated at T2 and T3 despite the presence of the metal image of the SP-S.
CONCLUSIONS
The cascade CNN algorithm proposed in this study showed a possibility of landmark identification from bony anatomies in serial lateral cephalograms despite the presence of OB, S-PS, FR, genioplasty, and bone remodeling.
However, since Mx1R, Mx6R, Md1R, Md6D, and Md 6R showed more than 1.5 mm of error and less than 60% of AP, it is necessary to increase the accuracy and reliability of landmark identification of the dental landmarks, especially the distal root apex of the mandibular first molar.
When the AI-assisted landmark identification is used, clinicians should consider these characteristics.
SUPPLEMENTAL VIDEO
A video presentation of this article is available at https://youtu.be/gGGYjWS7_KQ or www.e-kjo.org.
ACKNOWLEDGEMENTS
This research was supported by grants from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute and funded by the Ministry of Health &Welfare (HI18C1638) and the Technology Innovation Program (20006105) funded by the Ministry of Trade, Industry & Energy, Republic of Korea.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Im DH, Kim TW, Nahm DS, Chang YI. Current trends in orthodontic patients in Seoul National University Dental Hospital. Korean J Orthod. 2003;33:63–72. [Google Scholar]
- 2.Piao Y, Kim SJ, Yu HS, Cha JY, Baik HS. Five-year investigation of a large orthodontic patient population at a dental hospital in South Korea. Korean J Orthod. 2016;46:137–45. doi: 10.4041/kjod.2016.46.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nielsen IL. Maxillary superimposition: a comparison of three methods for cephalometric evaluation of growth and treatment change. Am J Orthod Dentofacial Orthop. 1989;95:422–31. doi: 10.1016/0889-5406(89)90304-1. [DOI] [PubMed] [Google Scholar]
- 4.Johnston C, Burden D, Kennedy D, Harradine N, Stevenson M. Class III surgical-orthodontic treatment: a cephalometric study. Am J Orthod Dentofacial Orthop. 2006;130:300–9. doi: 10.1016/j.ajodo.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 5.Hutton TJ, Cunningham S, Hammond P. An evaluation of active shape models for the automatic identification of cephalometric landmarks. Eur J Orthod. 2000;22:499–508. doi: 10.1093/ejo/22.5.499. [DOI] [PubMed] [Google Scholar]
- 6.Leonardi R, Giordano D, Maiorana F, Spampinato C. Automatic cephalometric analysis. Angle Orthod. 2008;78:145–51. doi: 10.2319/120506-491.1. [DOI] [PubMed] [Google Scholar]
- 7.Leonardi R, Giordano D, Maiorana F. An evaluation of cellular neural networks for the automatic identification of cephalometric landmarks on digital images. J Biomed Biotechnol. 2009;2009:717102. doi: 10.1155/2009/717102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arık SÖ, Ibragimov B, Xing L. Fully automated quantitative cephalometry using convolutional neural networks. J Med Imaging (Bellingham) 2017;4:014501. doi: 10.1117/1.JMI.4.1.014501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JH, Yu HJ, Kim MJ, Kim JW, Choi J. Automated cephalometric landmark detection with confidence regions using Bayesian convolutional neural networks. BMC Oral Health. 2020;20:270. doi: 10.1186/s12903-020-01256-7.afefdf9724c3499f8ceb3b2da99bc7dc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vandaele R, Aceto J, Muller M, Péronnet F, Debat V, Wang CW, et al. Landmark detection in 2D bioimages for geometric morphometrics: a multi-resolution tree-based approach. Sci Rep. 2018;8:538. doi: 10.1038/s41598-017-18993-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khanagar SB, Al-Ehaideb A, Vishwanathaiah S, Maganur PC, Patil S, Naik S, et al. Scope and performance of artificial intelligence technology in orthodontic diagnosis, treatment planning, and clinical decision-making - a systematic review. J Dent Sci. 2021;16:482–92. doi: 10.1016/j.jds.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim J, Kim I, Kim YJ, Kim M, Cho JH, Hong M, et al. Accuracy of automated identification of lateral cephalometric landmarks using cascade convolutional neural networks on lateral cephalograms from nationwide multi-centres. Orthod Craniofac Res. 2021;24 Suppl 2:59–67. doi: 10.1111/ocr.12493. [DOI] [PubMed] [Google Scholar]
- 13.Wang CW, Huang CT, Hsieh MC, Li CH, Chang SW, Li WC, et al. Evaluation and comparison of anatomical landmark detection methods for cephalometric X-ray images: a grand challenge. IEEE Trans Med Imaging. 2015;34:1890–900. doi: 10.1109/TMI.2015.2412951. [DOI] [PubMed] [Google Scholar]
- 14.Wang CW, Huang CT, Lee JH, Li CH, Chang SW, Siao MJ, et al. A benchmark for comparison of dental radiography analysis algorithms. Med Image Anal. 2016;31:63–76. doi: 10.1016/j.media.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Hwang HW, Park JH, Moon JH, Yu Y, Kim H, Her SB, et al. Automated identification of cephalometric landmarks: part 2-Might it be better than human? Angle Orthod. 2020;90:69–76. doi: 10.2319/022019-129.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin TY, Goyal P, Girshick R, He K, Dollar P. Focal loss for dense object detection. IEEE Trans Pattern Anal Mach Intell. 2020;42:318–27. doi: 10.1109/TPAMI.2018.2858826. [DOI] [PubMed] [Google Scholar]
- 17.Ronneberger O, Fischer P, Brox T. U-Net: convolutional networks for biomedical image segmentation. arXiv. 04597 [Preprint] 2015. [cited 2020 Dec 15]. Available from: https://doi.org/10.48550/arXiv.1505.04597 .
- 18.Roden-Johnson D, English J, Gallerano R. Comparison of hand-traced and computerized cephalograms: landmark identification, measurement, and superimposition accuracy. Am J Orthod Dentofacial Orthop. 2008;133:556–64. doi: 10.1016/j.ajodo.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 19.Ohba S, Nakao N, Nakatani Y, Yoshimura H, Minamizato T, Kawasaki T, et al. Effects of vertical movement of the anterior nasal spine on the maxillary stability after Le Fort I osteotomy for pitch correction. J Craniofac Surg. 2015;26:e481–5. doi: 10.1097/SCS.0000000000001968. [DOI] [PubMed] [Google Scholar]
- 20.Venkategowda PR, Prakash AT, Roy ET, Shetty KS, Thakkar S, Maurya R. Stability of vertical, horizontal and angular parameters following superior repositioning of maxilla by Le Fort I osteotomy: a cephalometric study. J Clin Diagn Res. 2017;11:ZC10–4. doi: 10.7860/JCDR/2017/22455.9133.48282d71af1641a99b0939efaf551007 [DOI] [PMC free article] [PubMed] [Google Scholar]