Abstract
Introduction
There has been increasing interest in using deep parasternal intercostal plane (PIP) block as a supplement to multimodal analgesia regimens in cardiac surgery. The aim of this study was to observe cutaneous sensory block distribution and its duration for deep PIP blocks in patients undergoing open cardiac surgery.
Methods
This observational, prospective clinical study consisted of 113 participants. All patients received bilateral ultrasound-guided deep PIP block with 40 ml 0.33% ropivacaine. The primary study outcome was cutaneous sensory block distribution of deep PIP blocks in patients undergoing open cardiac surgery. Secondary outcome included block duration in all participants. The area of cutaneous sensory block was tested by using a cold stimulus (ice cube) 30 min after the end of deep PIP block administration. Cutaneous sensory testing was performed once every hour after extubation until the return of normal sensation.
Results
Thirty minutes after bilateral deep PIP block administration, the successful block rate of dermatomes T4 to T6 was almost 100%. However, T2 (percentage of left T2 block: 64.6%; percentage of right T2 block: 42.5%) and T3 (percentage of left T3 block: 88.5%; percentage of right T3 block: 87.6%) had a lower percentage of success. A few patients had blocked dermatomes at T1 or T7 (percentage of left T1 block: 7.08%; percentage of right T1 block: 2.65%; percentage of left T7 block: 6.19%; percentage of right T7 block: 10.6%). The mean effective duration of the deep PIP block was 17 h.
Conclusion
Bilateral deep PIP blocks can produce a widespread cutaneous sensory blockade with variable dermatomal distribution in the mid-sternum for a considerable effective duration.
Trial Registration
This study was registered in the Chinese Clinical Trial Registry (ChiCTR2100047755).
Keywords: Deep parasternal intercostal plane block, Open cardiac surgery, Ropivacaine, Cutaneous sensory blocked, Cold stimulus
Key Summary Points
| Why carry out this study? |
| What are cutaneous sensory block distribution and its duration for deep parasternal intercostal plane (PIP) blocks in patients undergoing open cardiac surgery? |
| Bilateral deep PIP blocks can produce a widespread cutaneous sensory blockade with variable dermatomal distribution in the mid-sternum for a considerable effective duration. |
| What was learned from the study? |
| The present study showed that ultrasound-guided bilateral deep PIP blocks in patients undergoing open cardiac surgery produce a widespread cutaneous sensory blockade with percentage of blocked dermatomes (T4–T6) of almost 100%, with T2 and T3 at about 50% and 80%, and a few patients had blocked dermatomes at T1 or T7. |
Introduction
Open cardiac surgical patients typically suffer from severe postoperative pain [1], and the mid-sternum is the main source of pain after surgery[2]. Recently, there has been increasing interest in using deep parasternal intercostal plane (PIP) block as a supplement to multimodal analgesia regimens for patients undergoing open cardiac surgery [3, 4]. The ultrasound-guided deep PIP block was first reported by Ueshima in 2015 [5]. Ibrahim et al, [6] reported that the use of deep PIP block decreased perioperative fentanyl consumption and reduced postoperative pain intensity in pediatric cardiac surgery patients. Otake et al. [7] found that the combination of PECS and deep PIP blocks provided effective perioperative pain relief for breast cancer surgery. Our previous studies [8, 9] also demonstrated that bilateral deep PIP blocks can provide good perioperative analgesia for patients undergoing open cardiac surgery and promote postoperative recovery. Almost all studies have considered that deep PIP blocks cover the anterior branches of intercostal nerves from T2 to T6 in the internal mammary area [6–9]. However, transversus thoracis muscle was announced as the most variable in the human body [10] because some studies found that transversus thoracis muscle showed variations in its attachments not only in different patients, but also on the opposite sides of the same patient [11]. We assumed that sensory block of deep PIP blocks was related to thoracic muscle location. Based on variability of transversus thoracis muscle and clinical experiences, we hypothesized that bilateral deep PIP blocks could provide a difference in height of the block between left and right sides.
To our knowledge, there have been no detailed studies focusing on cutaneous sensory block distribution and its duration for bilateral deep PIP blocks. Therefore, the purpose of this study was to observe cutaneous sensory block distribution and its duration for deep PIP blocks in patients undergoing open cardiac surgery.
Methods
This single-center, observational, prospective clinical study was approved by the ethics committee of First Affiliated Hospital of Nanchang University (approval number 2021027), and written informed consent was obtained from all subjects participating in the trial. The trial was registered before patient enrollment at Chinese Clinical Trial Registry (ChiCTR2100047755). Our study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Inclusion and Exclusion Criteria
This study was performed with adult patients between 18–70 years old who had an American Society of Anesthesiologists physical status II–III and were undergoing elective heart valve replacement surgery with median sternotomy approach. The exclusion criteria were patients who refused to participate in this trial or having allergy to ropivacaine, secondary surgery, hepatic or renal failure, chronic pain, urgent surgery, communication disability or drug addiction.
Ultrasound‐Guided Deep PIP Block
All enrolled patients had established intravenous access after entering the designated block ward, and they were sedated with intravenous (IV) midazolam 1 mg and sufentanil 5 µg. Electrocardiography, non-invasive arterial pressure and pulse oximetry were continuously monitored in all patients in our study during the deep PIP block period. All participants were kept in the supine position to perform bilateral deep PIP blocks under aseptic conditions. During the deep PIP block, a 20-gauge, 70-mm needle (Tuoren, Henan, China) was used with a high-frequency linear ultrasound probe (Huasheng, Shenzhen, China). The operator used ultrasonography to determine the anterior T4–T5 interspace, and the ultrasound probe parallel to the rib was placed lateral to the sternal border. Then, we found three muscles next to the sternum (pectoralis major internal muscle, intercostal muscle and transversus thoracis muscle). The deep PIP was located between intercostal muscle and transversus thoracis muscle, and the operator also found the internal thoracic artery and vein which passed through the deep PIP to verify this plane. All subjects underwent in-plane technique, and saline (2 ml) was injected to the deep PIP to confirm the location of the needle tip in the target plane. Then, the deep PIP blocks were followed by administered of 0.33% ropivacaine 40 ml in total (20 ml injected into each side) into the fascial plane. A successful injection of deep PIP block requires that the space between the intercostal muscle and transversus thoracis muscle expands when injected and shrinks rapidly when this is stopped (Fig. 1). All deep PIP blocks were completed by the same skilled anesthesiologist within 20 min.
Fig. 1.
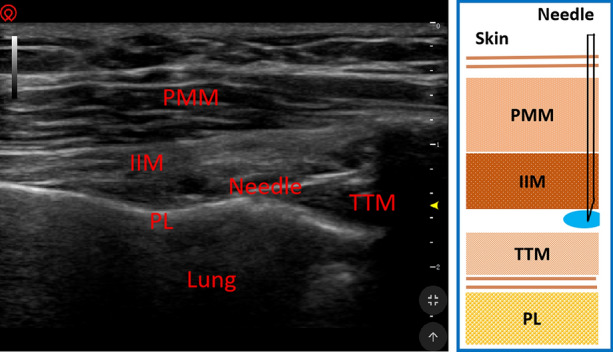
Example picture and ultrasound image of deep parasternal intercostal plane block. PMM pectoralis major muscle; IIM internal intercostal muscle; TTM transversus thoracis muscle; PL pleura
Anesthesia
All patients received general anesthesia with midazolam, sufentanil, etomidate and rocuronium for tracheal intubation. Anesthesia maintenance was achieved with rocuronium, sufentanil and propofol, and the BIS was maintained between 45 and 55 in all patients. Patient-controlled analgesia with intravenous sufentanil was used to perform postoperative analgesia, and flurbiprofen axetil was injected according to the demands of the patients.
Outcomes and Assessments
The primary study outcome was cutaneous sensory block distribution of deep PIP blocks in patients undergoing open cardiac surgery. Secondary outcome included the block duration in all participants.
The area of cutaneous sensory blocked was tested by another investigator using a cold stimulus (ice cube) at half an hour after the end of deep PIP block administration. All patients in our study were tested with an ice cube before block placement so that they knew what “normal” felt like. Cutaneous sensory testing by the application of the cold stimulus was performed once every hour after extubation until the return of normal sensation. The effective duration of the blockade was recorded and defined as the time from the local anesthetic injection (for the deep PIP block) to sensation returned to normal. We used the dichotomous method (successful block or failed block) to assess the area of cutaneous sensory blocked changes. Successful block was defined as the sensation to cold being lost, and failed block was defined as the sensation to cold being a continuous normal sensation. The cold stimulus was moved laterally at about 1 cm/s from the median line of the thorax at 0.5-cm intervals and stopped at the mid-clavicular line. During the cold stimulus, areas of sensory change were marked on the skin of the chest.
Statistical Analysis
Statistical analysis was performed using SAS software (version 9.1.3, Cary, NC, USA). Shapiro-Wilk test was used to check whether the data conformed to the normal distribution. Numerical data with a normal distribution were reported as mean (SD) and those that were not normally distributed as medians and quartiles.
The authors calculated the patient sample size of our trial based on a pilot study (n = 10 patients), which compared the percentage of left and right T2 block (60% vs 40%). An estimated sample size of 100 patients was needed with a type I error of α = 0.05, type II error of β = 0.1 and power of 90%. We finally included 20% more patients for analysis to compensate for possible dropout in our trial (n = 120 in our trial).
Results
A total of 120 patients initially consented for the present study and received ultrasound-guided bilateral deep PIP block according to the study protocol. Of the enrolled patients, seven were excluded for the following reasons: threer decided to leave the study, two had redo surgery, and two had postoperative delirium. Ultimately, data for 113 participants were analyzed in our study. Demographic and surgical data of all participants are shown in Table 1.
Table 1.
Main characteristics of the patients
| Characteristics | Value, mean (SD) or median (interquartile range) |
|---|---|
| Age, years | 47 (18) |
| Height, cm | 168 (12) |
| Weight, kg | 67 (14) |
| Duration of surgery, min | 190 (31) |
| Cardiopulmonary bypass time (min) | 67 (24) |
| Intraoperative bleeding volume (ml) | 734 (259) |
| Intraoperative urine output (ml) | 900 (278) |
| Sex (male/female) | 45/55 |
| Duration between block and extubation | 8.5 (1.5) |
| Postoperative sufentanil consumption (μg/kg) | 112 (32) |
| Postoperative flurbiprofen axetil consumption (mg) | 250 (150–350) |
Thirty minutes after bilateral deep PIP block administration, the cutaneous sensory block area was tested using a cold stimulus, as shown in Table 2. The successful block rate of dermatomes T4 to T6 at 30 min was almost 100% (Table 2). However, T2 (percentage of left T2 block: 64.6% [0.550–0.732]; percentage of right T2 block: 42.5% [0.334–0.521]) and T3 (percentage of left T3 block: 88.5% [0.808–0.935]; percentage of right T3 block: 87.6% [0.798–0.928]) had a lower percentage of success (Table 2). A few patients had blocked dermatomes at T1 or T7 (percentage of left T1 block: 7.08% [0.033–0.139]; percentage of right T1 block: 2.65% [0.007–0.081]; percentage of left T7 block: 6.19% [0.027–0.128]; percentage of right T7 block: 10.6% [0.059–0.182]). The mean effective duration of the deep PIP block was 17 h (11.017–23.001).
Table 2.
Sensory block distribution at 30 min after the deep PIP blocks
| Blocking plane | Left deep PIP block Effective percentage of block |
95% confidence intervals | Right deep PIP block Effective percentage of block |
95% confidence intervals |
|---|---|---|---|---|
| T1 | 8 (7.08%) | 0.033–0.139 | 3 (2.65%) | 0.007–0.081 |
| T2 | 73 (64.6%) | 0.550–0.732 | 48 (42.5%) | 0.334–0.521 |
| T3 | 100 (88.5%) | 0.808–0.935 | 99 (87.6%) | 0.798–0.928 |
| T4 | 112 (99.1%) | 0.945–1.000 | 113 (100%) | 0.959–1.000 |
| T5 | 113 (100%) | 0.959–1.000 | 113 (100%) | 0.959–1.000 |
| T6 | 113 (100%) | 0.959–1.000 | 112 (99.1%) | 0.945–1.000 |
| T7 | 7 (6.19%) | 0.027–0.128 | 12 (10.6%) | 0.059–0.182 |
PIP parasternal intercostal plane
Discussion
The present study demonstrated that ultrasound‐guided bilateral deep PIP blocks with 0.33% ropivacaine 40 ml produced a widespread cutaneous sensory block in the internal mammary area. The percentage of blocked dermatomes (T4–T6) was almost 100%, with T2 and T3 at about 50% and 80%, and a few patients had blocked dermatomes at T1 or T7 in open cardiac patients undergoing ultrasound‐guided bilateral deep PIP blocks. We found that the effective duration of the bilateral deep PIP blocks was 17 h.
Transversus thoracis muscle plane block or parasternal block is no longer among the standardized nomenclature in the regional anesthesia ASRA-ESRA Delphi consensus of accepted chest wall blocks [12]. Depending on the new standardize nomenclature, deep PIP block is the most suitable block name in our study [12]. Harmonization and standardization of nomenclature will potentially improve teaching and research on deep PIP blocks, ultimately resulting in dissemination that will benefit patient care [12]. No patients had complications related to the deep PIP block, such as ropivacaine allergy, pneumothorax, hematoma, infection and injury of the internal mammary artery and vein. This is consistent with Ueshima's findings [13].
All patients in our study were valve replacement patients undergoing open heart surgery. Patients undergoing internal mammary artery harvesting for coronary artery bypass grafting (CABG) experienced more intense pain [14]. The internal mammary artery runs between intercostal muscle and transversus thoracic muscle, and the deep PIP block risks internal mammary artery injury or hematoma. In addition, patients undergoing coronary artery bypass grafting could have tissue disruption in the PIP due to internal mammary artery harvest, increasing the recognition difficulty of transverse thoracic muscle [15]. Therefore, the PIP block may have decreased efficacy because of tissue disruption and scar tissue formation in the PIP. Therefore, our study did not include patients undergoing open heart surgery with CABG.
Several clinical trials found that the deep PIP block provided effective analgesia and reduced perioperative opioid consumption for cardiac surgery [16, 17], open pectus carinatum surgery [18], breast surgery [19], subcutaneous implantable cardioverter-defibrillator placement [20] and pericardial drainage [21]. Almost all these articles found that ultrasound-guided deep PIP blocks covered the anterior branches of intercostal nerves from T2 to T6, releasing the pain in the internal mammary area. Furthermore, a cadaveric study by Ueshima et al. [22] demonstrated that an ultrasound-guided deep PIP block could involve many anterior branches of intercostal nerves (T2–T6). However, our study found that the percentage of blocked dermatomes (T4–T6) was almost 100%, with T2 and T3 at about 50% and 80%, and a few patients undergoing ultrasound‐guided bilateral deep PIP blocks had blocked dermatomes at T1 or T7. The clinical implications of our study were that the cutaneous sensory block distribution of deep PIP blocks was variable, and it was necessary to perform several blocks to cover the area from T1 to T7 in clinical work. To the best of our knowledge, this is the first trial to identify cutaneous sensory block distribution of bilateral deep PIP blocks in patients undergoing open cardiac surgery.
An autopsy study of 120 subjects [23] provided detailed basic information on the variety of transversus thoracic muscles. The study found that the number of slips forming the transversus thoracis in their sample varied: slips to the fourth, fifth and sixth ribs on both sides occurred in most cases; slip to the first, second, third and seventh ribs on both sides presented variability [19]. The rate of muscle attachment to T1 was 7.5% on the left side and 0.8% on the right side; T2 was 60.8% on the left side and 38. 3% on the right side; T3 was 85.8% on the left side and 85% on the right side; T4 was 99.2% on the left side and 99.2% on the right; T5 was 100% on the left side and 100% on the right; T6 was 99.2% on the left side and 98.3% on the right; T7 was 5.8% on the left side and 9.2% on the right [23]. The variety of the transversus thoracic muscle is very consistent with unstable cutaneous sensory block distribution of bilateral deep PIP blocks in our trail. Therefore, we thought that the great variation of transverse thoracic muscle would lead to uncertain cutaneous sensory block distribution of deep PIP blocks. Ueshima et al. [24] found that ropivacaine in the deep PIP spread faster and more widely between the fourth and fifth ribs than between the third and fourth ribs, which might be because the transversus thoracis slips to the fourth and fifth rib on both sides always existed.
Recently, some studies [25–27] compared deep PIP block with superficial parasternal intercostal plane (PIP) block in patients undergoing open cardiac surgery and found that superficial PIP block may have more advantages. First, superficial PIP block was performed by targeting a more superficial fascial plane at the level of the external intercostal membrane, resulting in a lower risk of pneumothorax. Second, the internal mammary artery and vein pass through the deep PIP, and the needle point is on this plane when blocking, so deep PIP block risks vascular laceration. Third, the pectoralis major muscle and external intercostal muscle were less variable than the transversus thoracic muscle, so cutaneous sensory block distribution of superficial PIP block may be more stable than deep PIP block. However, superficial PIP block requires each point of injection at the third and fifth intercostal spaces [28], and deep PIP block only requires each point of the T4–T5 interspace.
There are several limitations to our current study. First, we measured the effect of deep PIP blocks using a cold stimulus rather than postoperative analgesia for pain. Therefore, we did not observe the analgesic effect of deep PIP block in patients undergoing cardiac surgery. Second, we did not compare cutaneous sensory block distribution of deep PIP block with superficial PIP block to solve the current controversial issues. Third, we did not carry out an autopsy study of the transversus thoracic muscle in our country.
Conclusions
The present study showed that ultrasound‐guided bilateral deep PIP blocks in patients undergoing open cardiac surgery produce a widespread cutaneous sensory blockade with the percentage of blocked dermatomes (T4–T6) being almost 100%, with T2 and T3 at about 50% and 80%. A few patients had blocked dermatomes at T1 or T7.
Acknowledgements
We thank the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors. The project was funded by Department of Science and Technology of Jiangxi Province (20203BBGL73195) and (20212BAG70034).
Authorship
Yang Zhang, Jia Min and Shibiao Chen meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
YZ and SBC were responsible for, conceived and designed this study and collected the data. YZ and JM were responsible for study execution and manuscript writing. JM and SBC were responsible for data analysis. All authors have read and approved the final version of the manuscript.
Disclosures
Yang Zhang, Jia Min and Shibiao Chen have nothing to disclose.
Compliance with Ethics Guidelines
This single-center, observational, prospective clinical study was approved by the ethics committee of First Affiliated Hospital of Nanchang University (approval number 2021027), and written informed consent was obtained from all subjects participating in the trial. The trial was registered before patient enrollment at Chinese Clinical Trial Registry (ChiCTR2100047755). Our study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Lahtinen P, Kokki H, Hynynen M. Pain after cardiac surgery: a prospective cohort study of 1-year incidence and intensity. Anesthesiology. 2006;105:794–800. doi: 10.1097/00000542-200610000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Mueller XM, Tinguely F, Tevaearai HT, et al. Pain location, distribution, and intensity after cardiac surgery. Chest. 2000;118:391–396. doi: 10.1378/chest.118.2.391. [DOI] [PubMed] [Google Scholar]
- 3.Gde Putra Semara Jaya AA, Aida Rosita T, Aldy H, Arif M. Single-centre, double-blind, randomised, parallel-group, superiority study to evaluate the effectiveness of general anaesthesia and ultrasound-guided transversus thoracis muscle plane block combination in adult cardiac surgery for reducing the surgical stress response: clinical trial protocol. BMJ Open. 2021;11(11):e051008. [DOI] [PMC free article] [PubMed]
- 4.Satoru F, Matthew R, Philip MJ, et al. Transversus thoracis muscle plane block in cardiac surgery: a pilot feasibility study. Reg Anesth Pain Med. 2019;44:556–560. doi: 10.1136/rapm-2018-100178. [DOI] [PubMed] [Google Scholar]
- 5.Ueshima H, Kitamura A. Clinical experiences of ultrasound-guided transversus thoracic muscle plane block: a clinical experience. J Clin Anesth. 2015;27:428–429. doi: 10.1016/j.jclinane.2015.03.040. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim I, Abdelbaser N, Mageed A. Analgesic efficacy of ultrasound guided bilateral transversus thoracis muscle plane block in pediatric cardiac surgery: a randomized, double-blind, controlled study. J Clin Anesth. 2020;67:110002. doi: 10.1016/j.jclinane.2020.110002. [DOI] [PubMed] [Google Scholar]
- 7.Ueshima H, Otake H. Addition of transversus thoracic muscle plane block to pectoral nerves block provides more effective perioperative pain relief than pectoral nerves block alone for breast cancer surgery. Br J Anaesth. 2017;118(3):439–443. doi: 10.1093/bja/aew449. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Chen S, Gong H, Zhan B. Efficacy of bilateral transversus thoracis muscle plane block in pediatric patients undergoing open cardiac surgery. J Cardiothorac Vasc Anesth. 2020;34(9):2430–2434. doi: 10.1053/j.jvca.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Li X, Chen S. Bilateral transversus thoracis muscle plane block provides effective analgesia and enhances recovery after open cardiac surgery. J Card Surg. 2021;36(8):2818–2823. doi: 10.1111/jocs.15666. [DOI] [PubMed] [Google Scholar]
- 10.Hyrtl J. Lehrbuch der Anatomie des Menschen. 18. Wien: Wilhelm Braumüller; 1885. p. 474. [Google Scholar]
- 11.Salmons S. Muscle. 38 edition. In: Williams PL, Bannister LH, Berry M, Collins P, Dyson M, Dussek JE, Ferguson MWJ, editors. Gray’s anatomy. Churchill Livingstonem: Edinburgh; 1995. p. 815. [Google Scholar]
- 12.Kariem E-B, Morné W, Angela DS,et al. Standardizing nomenclature in regional anesthesia: an ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg Anesth Pain Med. 2021;46(7):571–580 [DOI] [PubMed]
- 13.Ueshima H, Otake H. Ultrasound-guided transversus thoracic muscle plane block: complication in 299 consecutive cases. J Clin Anesth. 2017;41:60. doi: 10.1016/j.jclinane.2017.03.056. [DOI] [PubMed] [Google Scholar]
- 14.Mazzeffi M, Khelemsky Y. Poststernotomy pain: a clinical review. J Cardiothorac Vasc Anesth. 2011;25:1163–1178. doi: 10.1053/j.jvca.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Fujii S, Vissa D, Ganapathy S, Johnson M, Zhou J. Transversus thoracic muscle plane block on a cadaver with history of coronary artery bypass grafting. Region Anesth Pain Med. 2017;42(4):535–537. doi: 10.1097/AAP.0000000000000607. [DOI] [PubMed] [Google Scholar]
- 16.Bartlett E, Urman RD, Urits I, et al. Is bilateral transversus thoracis muscle plane block effective in minimizing pain in pediatric cardiac surgery? J Clin Anesth. 2020;1:110083. doi: 10.1016/j.jclinane.2020.110083. [DOI] [PubMed] [Google Scholar]
- 17.Zauk J, Wyatt K. Transversus thoracis muscle plane blocks for a patient with Maroteaux–Lamy syndrome undergoing mitral valve replacement. J Clin Anesth. 2021;72:110269. doi: 10.1016/j.jclinane.2021.110269. [DOI] [PubMed] [Google Scholar]
- 18.Ahiskalioglu A, Kucun T, Yayik AM, Ulas AB, Ates İ. Ultrasound-guided transversus thoracis muscle plane block provides effective postoperative analgesia for pediatric open pectus carinatum surgery: first report. Pain Med. 2021;22(5):1233–1235. doi: 10.1093/pm/pnaa250. [DOI] [PubMed] [Google Scholar]
- 19.Ueshima H, Otake H. A combination of an erector spinae plane block and a transversus thoracic muscle plane block for partial mastectomy. J Clin Anesth. 2019;54:1. doi: 10.1016/j.jclinane.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y, Min J, Chen S. Analgesic efficacy of regional anesthesia of the hemithorax in patients undergoing subcutaneous implantable cardioverter-defibrillator placement. J Cardiothorac Vasc Anesth. 2021;35(11):3288–3293. doi: 10.1053/j.jvca.2021.02.052. [DOI] [PubMed] [Google Scholar]
- 21.Ueshima H, Otake H. The lateral transversus thoracic muscle plane block is effective for the pericardial drainage. J Clin Anesth. 2017;42:12. doi: 10.1016/j.jclinane.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 22.Ueshima H, Takeda Y, Ishikawa S, Otake H. Ultrasound-guided transversus thoracic muscle plane block: a cadaveric study of the spread of injectate. J Clin Anesth. 2015;27(8):696. doi: 10.1016/j.jclinane.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 23.Lazar J, Stanislav H, Wladimir O. Variety of transversus thoracis muscle in relation to the internal thoracic artery: an autopsy study of 120 subjects. J Cardiothorac Surg. 2011;6:11. doi: 10.1186/1749-8090-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ueshima H, Otake H. Where is an appropriate injection point for an ultrasound-guided transversus thoracic muscle plane block? J Clin Anesth. 2016;33:190–191. doi: 10.1016/j.jclinane.2016.03.057. [DOI] [PubMed] [Google Scholar]
- 25.Scimia P, Fusco P, Tedesco M, Sepolvere G. Bilateral ultrasound-guided parasternal block for postoperative analgesia in cardiac surgery: could it be the safest strategy? Reg Anesth Pain Med. 2020;45(4):316–317. doi: 10.1136/rapm-2019-100872. [DOI] [PubMed] [Google Scholar]
- 26.Diego GS, Mario FP. Safer alternatives to transversus thoracis muscle plane block. Reg Anesth Pain Med. 2019 doi: 10.1136/rapm-2019-100666. [DOI] [PubMed] [Google Scholar]
- 27.Satoru F. Transversus thoracis muscle plane block and alternative techniques. Reg Anesth Pain Med. 2019 doi: 10.1155/2019/1716365. [DOI] [PubMed] [Google Scholar]
- 28.Costa F, Caruso S, Pascarella G, Nenna A, Grande S, Sarubbi D, Chello M, Agrò FE. Sternotomy debridement in critical patient with difficult predicted airway: can regional anesthesia be the labyrinth exit? Minerva Anestesiol. 2020;86(4):462–463. doi: 10.23736/S0375-9393.19.14133-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


