Abstract
Objective
This study aimed to evaluate the effect of electroacupuncture preconditioning on regional cerebral oxygen saturation (rSO2) levels in elderly patients with diabetes.
Methods
Forty patients undergoing elective diabetic foot surgery were enrolled in this study. All patients were aged 65 years and above and weighed 45–75 kg. All were characterized as class II or III according to the American Society of Anesthesiologists’ physical status classification system. Patients were divided randomly into an electroacupuncture group (group E) and a control group (group C); both groups comprised 20 patients. In group E, the DU20 (Baihui), DU24 (Shenting), and EX-HN1 (Sishencong) acupoints were selected for electroacupuncture 30 min prior to administering anesthesia, while in group C, patients underwent routine anesthesia without electroacupuncture. The patients in both groups were anesthetized using a sciatic nerve block. The number of cases with increased or decreased regional oxygen saturation (rSO2) compared with the baseline as well as rSO2 variability in the two groups were recorded and compared.
Results
There was no significant difference in the preoperative rSO2 values between the two groups (54.4 ± 4.8 (L), 53.9 ± 5.2 (R) [group C] vs 54.1 ± 5.2 (L), 54.5 ± 4.6 (R)[group E]). Compared with group C, the rSO2 in group E increased (50.3 ± 3.9 [group C] vs 58.4 ± 3.2[group E]), and this difference was statistically significant (P < 0.001).
Conclusion
Electroacupuncture stimulation can increase rSO2 levels in patients with diabetes.
Clinical Registration Number
ChiCTR2100048783 (http://www.chictr.org.cn).
Keywords: electroacupuncture, preconditioning, regional cerebral oxygen saturation, diabetes
Introduction
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia that affects multiple organs and systems. Type 2 diabetes mellitus (T2DM) accounts for 90–95% of the population with diabetes,1 and according to the most recent data provided by the International Diabetes Federation (https://www.diabetesatlas.org), 537 million adults worldwide were expected to have diabetes in 2021; by 2045, this figure is anticipated to rise to 783 million. Approximately 40% of patients with diabetes will also develop cognitive impairment.2
Patients with diabetes have a 50% higher risk of developing dementia compared with patients without the disease.2,3 Research has highlighted diabetes as the fourth-highest risk factor for dementia in China, a country in which 6.3% of patients with dementia can be linked to diabetes.4 Furthermore, when subjected to the trauma of surgery, patients with diabetes are also more likely to suffer brain damage.
The condition known as diabetic foot is one of the most common complications of T2DM. The prevalence of this condition in patients with diabetes is 6.3% worldwide, while the incidence of diabetic foot ulcers in China is 4.1%.5 Diabetic foot, as a late complication of diabetes, is characterized by skin infections and ulcers and may even affect deep tissue. The condition is caused by microangiopathy and peripheral neuropathy and can affect the central nervous system as the disease progresses. Diabetic foot is the main cause of non-traumatic amputation worldwide.6 The 7-year average incidence of amputation in patients with moderate diabetic foot ulcers was 9.9%.7 Additionally, amputation was indicated as being associated with an increase in overall cognitive impairment and the impairment of episodic memory in elderly patients with diabetic foot.8
The monitoring of regional cerebral oxygen saturation (rSO2) is a new and non-invasive method of monitoring brain oxygen balance and can reflect changes in the brain’s oxygen supply and consumption. It can accurately and promptly reflect cerebral perfusion and cerebral oxygen supply/demand during surgery, thereby guiding the regulation of the supply of intraoperative cerebral oxygen and blood. This can effectively reduce intraoperative brain injury and the incidence of postoperative complications.9–12 Preliminary research conducted for the present study showed that the baseline values of left and right rSO2 decreased in patients with diabetes compared with patients without the disease.13 However, few studies have focused on the clinical features of the “fragile brain” in elderly patients with diabetes, and there is a gap in the knowledge regarding the monitoring of intraoperative cerebral perfusion and oxygen supply. In addition, there is a lack of effective prevention and treatment measures in place for managing the cognitive functioning of these patients.
Electroacupuncture has been proven to have unique advantages in the treatment of diabetes and common complications of the disease, such as neuropathy, nephropathy, retinopathy, and other chronic complications.14,15 Animal experiments showed that electroacupuncture could improve the learning and memory abilities of diabetic rats with cognitive impairment16 and improve the learning and memory function of the hippocampus in diabetic mice.17 In a clinical trial, electroacupuncture improved cerebral oxygen saturation in elderly patients with fragile brain function during hip arthroplasty.18 However, at the time of conducting the present study, no related reports could be found on using electroacupuncture to improve rSO2 levels in patients with diabetes undergoing foot amputation.
The present study employed a combination of traditional Chinese medicine (TCM) and Western medicine approaches with the application of electroacupuncture in elderly patients undergoing foot amputation and investigated the effects of electroacupuncture on cerebral perfusion and oxygen supply. The rSO2 levels of patients were monitored in an attempt to establish an effective method for improving the quality of life of elderly individuals with diabetes undergoing amputation.
Information and Methods
General Information
Patients who underwent elective diabetic foot amputation in the Beijing Traditional Chinese Medicine Hospital between March and June 2021 were enrolled in this study. The patients were divided randomly into one of two groups, ie, an electroacupuncture group (group E) and a control group (group C); both groups included 20 patients. The ethics committee of the hospital approved the study (2021BL02-042), and the patients or their families provided informed consent for inclusion in the research.
Inclusion Criteria
The following inclusion criteria were observed: (1) patients aged 65 years or older, (2) patients who were characterized as having a class II or III physical status based on the American Society of Anesthesiologists’ classification system, and (3) patients with a history of diabetes longer than 10 years. All patients met the diagnostic criteria for the condition of diabetic foot and were scheduled to undergo this elective procedure. The diabetic foot diagnostic criteria were based on China’s guidelines for diabetic foot prevention (2019).17
Exclusion Criteria
The following exclusion criteria were observed: (1) patients with skin damage at the acupuncture site or a forehead skin infection, which made it impossible to place an rSO2 monitoring electrode, (2) patients with severe hearing and visual impairment or reading and comprehension difficulties, (3) patients with an existing history of cerebrovascular disease, and (4) patients with a pacemaker.
Elimination Criteria
The following elimination criteria were observed: (1) patients who failed to meet the inclusion criteria but were erroneously included, (2) patients who were included but did not receive electroacupuncture treatment and rSO2 monitoring, and (3) patients with markedly incomplete records.
Randomization and Blinding
Patients who met the inclusion criteria were included in the study and randomly assigned to one of the two groups. The resulting randomly assigned sequence outcomes were recorded and placed in a sealed and light-tight envelope in coded order. Each participant was assigned an envelope. When the study began, the investigator opened the envelopes in sequence and assigned the subject to the corresponding group. The outcome-evaluator blind method was applied in this study, and neither the outcome evaluator nor the statistical analyst was aware of the composition of the two groups.
Research Methods
None of the patients included in the study were given preoperative medication, and the same anesthesia protocol was used for all participants. After the patient entered the operating room, venous access was obtained, and the following parameters were monitored: electrocardiogram, heart rate, noninvasive blood pressure, and blood oxygen saturation. In addition, the intraoperative rSO2 values of the two groups were monitored using a near-infrared spectrometer (INVOSTM 5100C, Medtronic, USA). Electrodes were placed on both sides of the forehead to monitor the rSO2, while the patient lay in the supine position, breathing quietly. Baseline levels were recorded once the reading was stable; thereafter, the machine collected data every 30 sec. Following surgery, the lowest rSO2 value on both sides was used for analysis using the INVOS™ Analytics Tool (v.1.0) software. In group E, after the initial monitoring of each parameter, electroacupuncture was performed 30 min before the anesthetic was administered.
Based on the observed results of previously conducted clinical trials, patients received electroacupuncture at DU20 (Baihui: on the head, located at the midline of the head in line with the apex of the ears), DU24 (Shenting: on the head, 0.5 cun (1 cun = 0.33 m) directly above the midpoint of the anterior hairline), and EX-HN1 (Sishencong: four points at the vertex of the scalp, grouped around DU20, and located 1 cun anteriorly, posteriorly, and laterally to it). The electroacupuncture instrument was connected, and the selected acupoints were electrically stimulated by a dilatational wave-type using 2/10 Hz. The waveform of a complete dilatational wave lasted 14 sec and alternated for 5 and 9 sec between 2 and 10 Hz. The stimulation intensity was gradually adjusted to the maximum value that the patient could tolerate, and the stimulation lasted 30 min. The protocol for the patients in group C was the same as for those in group E, but in the former, no electroacupuncture treatment was given.
Observation Indices
The rSO2 values were observed and recorded. Currently, as there is no recognized standard for a “normal” rSO2 range, in this study, the normal value of rSO2 was taken as approximately 70% ± 6%, which reflected the rSO2 of healthy participants. The rSO2 in the patients with diabetes tended to be 57.3% ± 8.9%, which is lower than this study’s normal level.10
Generally, cerebral ischemia or hypoxia is considered to occur when the absolute value of the rSO2 is below 50%. The rSO2 baseline (rSO2baseline), the maximum rSO2 (rSO2max), and the minimum rSO2 (rSO2min) values were recorded, and the following indices were calculated: (1) the average rSO2 values; (2) the number of patients whose mean rSO2 value increased or decreased compared with the baseline value, ie, the number of patients with a 20% < rSO2 rise ≤ 30%, 10% < rSO2 rise ≤ 20%, 0% < rSO2 rise ≤ 10%, −10% ≤ rSO2 rise < 0%, −10% ≤ rSO2 rise < −20%, and −20% ≤ rSO2 rise < −30%, and (3) the intraoperative increase in rSO2 variability (rSO2max − rSO2baseline), and the intraoperative decrease in rSO2 variability (rSO2baseline − rSO2min).
The Anesthesia Protocol
All patients were anesthetized using an ultrasound-guided sciatic nerve block and a popliteal approach combined with electrical nerve stimulation.
Medication: 10 mL of 1% ropivacaine + 10 mL of 2% lidocaine + 5 mL of 0.9% normal saline were given, with a volume range of 20–25 mL according to body weight.
Statistical Analysis
The data were statistically analyzed using SPSS Statistics 25.0 software. Normally distributed measurement data were expressed as mean ± standard deviation (X ± SD), and comparisons between groups were made using a t-test. Non-normally distributed measurement data were expressed as median (quartile) and compared using the Mann–Whitney U-test. Count data were expressed as numbers or percentages and were compared using the Wilcoxon rank–sum test. A value of P < 0.05 was considered to indicate statistical significance.
Results
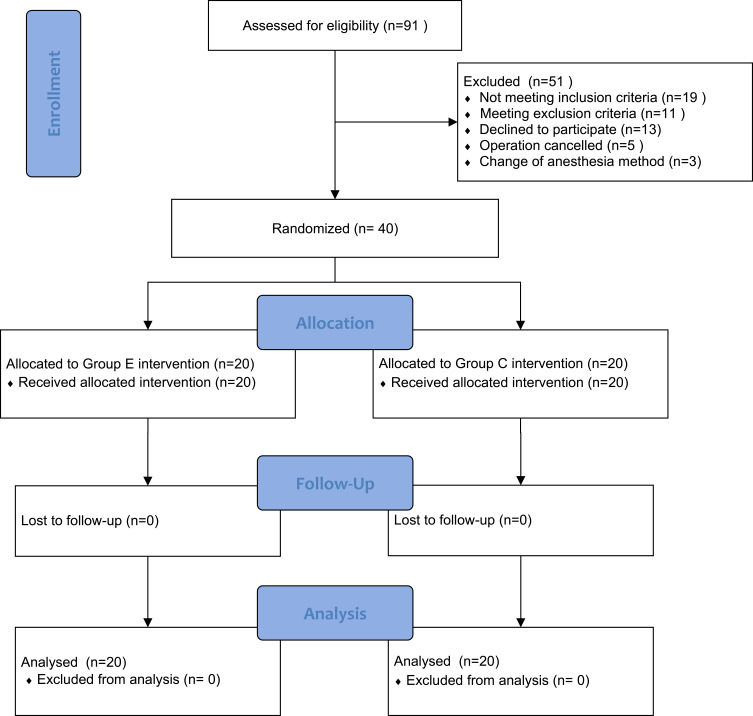
A total of 84 patients were eligible for screening from March to June 2021; among them, 40 patients were randomly assigned and included in the statistical analysis (Figure 1).
Figure 1.
Flowchart showing trial group assignments, loss to follow-up, and analysis.
Comparison of General Factors
The age, gender, weight, body mass index, diabetes duration, hypertension, chronic lung disease, preoperative hemoglobin level, preoperative white blood cell count, body temperature, smoking history, Wagner classification of diabetic foot, left and right rSO2, and anesthetic time were compared between the two groups. The differences between the groups were not statistically significant (P > 0.05); hence, the two groups were comparable (Table 1).
Table 1.
General Patient Information (n = 20)
| Item | Electroacupuncture Group | Control Group |
|---|---|---|
| Age (year) | 68.7 ± 2.9 | 70.7 ± 5.2 |
| Gender (Male/Female) | 14/6 | 13/7 |
Weight (Kg,  ) ) |
63.8 ± 13.1 | 64.5 ± 9.4 |
| BMI | 24.1 ± 4.3 | 23.6 ± 3.5 |
| Diabetes duration (year) | 17.2 ± 2.6 | 18.2 ± 3.2 |
| Hypertension (n, %) | 12 (60) | 12 (60) |
| History of chronic lung disease | 3 (15) | 2 (10) |
| Preoperative hemoglobin level (g/L) | 10.6 ±1.2 | 10.8 ± 1.4 |
| Preoperative white blood cell count (×109/L) | 7.84 ±2.21 | 7.39 ± 2.66 |
| Body temperature (°C) | 36.39 ± 0.37 | 36.42 ± 0.39 |
| Smoking history (n, %) | 10 (50) | 12 (60) |
| Wagner classification of diabetic foot (n/%) | ||
| 1 | 0 (0) | 1 (5) |
| 2 | 3 (15) | 3 (15) |
| 3 | 7 (35) | 8 (40) |
| 4 | 9 (45) | 7 (35) |
| 5 | 1 (5) | 1 (5) |
| Left rSO2 (%) | 54.1 ± 5.2 | 54.4 ± 4.8 |
| Right rSO2 (%) | 54.5 ± 4.6 | 53.9 ± 5.2 |
| Anesthetic time (min) | 59.2 ± 15.2 | 64.8 ± 14.7 |
Comparison of the Baseline, Maximum, and Minimum Regional Cerebral Oxygen Saturation
The rSO2baseline, rSO2max, and rSO2min values were higher in group E compared with group C, and the observed differences were statistically significant (P < 0.001, Table 2).
Table 2.
Comparison of rSO2baseline, rSO2max and rSO2min Between the Two Groups (n=20)
| Item | Electroacupuncture Group | Control Group | P |
|---|---|---|---|
| rSO2 maximum (%) | 66.5 ± 4.12 | 58.4 ± 3.8 | 0.000* |
| rSO2 minimum (%) | 71.1 ± 5.9 | 63.4 ± 4.3 | 0.000* |
| rSO2 average (%) | 58.4 ± 3.2 | 50.3 ± 3.9 | 0.000* |
Note: Compared with group C, *P<0.01.
Comparison of Intraoperative Changes in the Regional Cerebral Oxygen Saturation Values
No patient in either group demonstrated a decrease in rSO2 of more than 20%. In group E, the rSO2 increased in all patients, while in group C, the rSO2 increased in 13 cases and decreased in 7 cases. The increase in the rSO2 area under the curve was significantly higher in group E than in group C (P < 0.001, Table 3).
Table 3.
Comparison of the Number of Cases of Intraoperative Changes in Cerebral Oxygen Saturation Between the Two Groups (n=20)
| Item | Electroacupuncture Group | Control Group | Z or t | P |
|---|---|---|---|---|
| 30%≤rSO2 increased>20%(n,%) | 4 (20%) | 0 | −4.235 | 0.000* |
| 20%≤rSO2 increased>10%(n,%) | 14 (70%) | 5 (25%) | −3.881 | 0.000* |
| 10%≤rSO2 increased>0 (n,%) | 2 (10%) | 8 (40%) | 22.67 | 0.000* |
| Total rSO2 increase (n, %) | 20 (100%) | 13 (65%) | ||
| 0<rSO2 decreased ≤10% (n,%) | 0 | 5 (25%) | 4.651 | 0.000* |
| 10<rSO2 decreased ≤20% (n, %) | 0 | 2 (10%) | 2.31 | 0.001* |
| 20<rSO2 decreased ≤30% (n, %) | 0 | 0 | 0 | 1 |
| Total rSO2 decrease (n, %) | 0 (0) | 7 (35%) |
Note: Compared with group C, *P<0.01.
Comparison of the Variability in the Increase/Decrease in Regional Cerebral Oxygen Saturation in the Two Groups
The increase of rSO2 in group C was lower than that in group E, and the decrease was higher than that in group E; these differences were statistically significant (P < 0.001, Table 4).
Table 4.
Comparison of the Increase or Decrease in Variability of Cerebral Oxygen Saturation Between the Two Groups (n=20)
| Item | Electroacupuncture Group | Control Group | t | P |
|---|---|---|---|---|
| Increased variability of rSO2 | 16.80 ±6.15 | 9.28 ± 5.50 | 4.078 | 0.000* |
| Reduced variability of rSO2 | −4.05 ± 4.71 | 3.88 ± 4.89 | −5.233 | 0.000* |
Note: Compared with group C, *P < 0.01.
Discussion
Diabetes mellitus is known as an independent risk factor for perioperative neurocognitive impairment.19 Patients with diabetes who require foot surgery are often in the later stages of diabetes, and as a result of the microvascular brain disease caused by the disease, their risk of dementia is significantly higher than in the general population. Long-term hyperglycemia and advanced glycation end products can damage cerebral vascular endothelial cells, causing thickening of the capillary basement membrane and cerebral atherosclerosis. This will lead to a decrease in the number of capillaries, an increase in the number of arteriovenous short circuits, and a decrease in cerebral blood flow or insufficient perfusion, which, in turn, can lead to ischemia and hypoxic injury of the brain tissue.20 Diabetes mellitus increases platelet aggregation and plasma viscosity and reduces cerebral blood flow and cerebral oxygen supply. It can also lead to cerebral microvascular disease, increasing the permeability of the blood–brain barrier and reducing its integrity, making it easier for macromolecular proteins to enter the brain parenchyma and resulting in neuronal damage and apoptosis.
Furthermore, hyperglycemia and its related blood glucose metabolic disorders can lead to an increase in neuronal oxidative stress injury, necrosis, and neuroinflammation, causing a decline in the cognitive function of patients as well as the occurrence of diabetic encephalopathy. An existing study found that diabetes mellitus increased the risk of perioperative neurological dysfunction in elderly people by 26%.21 One possible reason for this was that the trauma of surgery aggravated the central inflammatory reaction of diabetes itself. Often, patients with diabetes and foot complications require surgery and are prone to cognitive decline due to the progression of diabetes. If this is combined with the trauma of surgery, patients will be more likely to experience difficulties related to memory, visual memory, concentration, language comprehension, and social skills and suffer an overall decline in cognitive function.
Monitoring peripheral pulse oxygen concentration alone cannot effectively reflect the oxygen supply to the brain. Measuring rSO2 levels is a non-invasive and uninterrupted method for observing the balance of cerebral oxygen supply and demand as well as cerebral blood perfusion. Additionally, rSO2 has a proven ability for the early identification and prediction of the occurrence of perioperative neurological dysfunction in almost all types of surgeries.22,23 Studies have shown that elderly patients were more prone to a decrease in rSO2 during surgery, and a decrease in intraoperative rSO2 was significantly correlated with the occurrence of postoperative delirium.22 Furthermore, rSO2 values below 50% or a decrease of more than 20% from baseline values indicated cerebral ischemia and the potential presence of blood, as confirmed by the testing of auditory-evoked potentials.24 Therefore, the intraoperative monitoring of rSO2 can be used as an auxiliary means for predicting the occurrence of postoperative delirium.22 For groups with a high risk of cognitive impairment, understanding the oxygen supply and demand of the brain through rSO2 monitoring can inform the timely adjustment of an anesthetic plan and reduce potential risk factors linked to cognitive impairment to some degree, and it may be conducive to the rapid rehabilitation of patients.
An existing study conducted by the current authors found that the baseline values of left and right rSO2 were lower in patients with diabetes compared with patients without the disease, suggesting that the brain tissue of patients with diabetes was in a state of hypoxia relative to that of patients without diabetes.10 The same study also indicated that the baseline value of rSO2 was significantly lower in patients with a history of diabetes mellitus longer than 10 years compared with patients with a history of 10 years or less. This suggested that the longer the duration of diabetes, the higher the risk of cerebral ischemia and hypoxia. The results of a linear regression analysis showed that the baseline level of rSO2 decreased with age.10 Therefore, the present study focused on the effect of electroacupuncture on rSO2 in elderly patients with diabetes with a duration of more than 10 years.
Currently, only a few studies have been completed on rSO2-monitoring-oriented intervention strategies in patients with diabetes at home and abroad. Presently, the evaluation of the postoperative cognitive function of patients in clinical research is primarily carried out using a psycho-neurological evaluation scale. This requires considerable cooperation on the part of participants, is typically time consuming and energy intensive for clinicians, includes a degree of subjectivity, can result in significant clinical differences, and cannot rule out the influence of the learning effect. In the current study, rSO2 monitoring was used as an objective basis for the evaluation of the effect of electroacupuncture on the postoperative cognitive function of patients with diabetes.
A large number of TCM works and studies,25,26 such as the Code of Practice for Chinese Medicine, state that DU20 and DU24 are the two most frequently used acupoints for the treatment of cognitive-related symptoms. These are two important acupoints of the Du meridian and fulfill the functions of dredging that meridian, regulating and refreshing the mind, inducing resuscitation, and calming the spirit. Accordingly, they are important acupoints for the treatment of mental diseases. The Du meridian is closely related to the function of the central nervous system; it can circulate Qi and blood, remove phlegm and blood stasis, and regulate and stimulate the Yang Qi of the human body. The EX-HN1 acupoint is at the very top of the head, ie, the Yang Qi position. Acupuncture of the EX-HN1 acupoint can regulate the meridian Qi of the entire body and has the effects of calming the mind, benefiting intelligence, strengthening the brain, and regulating the mind. An existing study revealed that electroacupuncture stimulation of the DU20 and DU24 points could regulate the Du meridian, stimulate blood circulation, tonify kidney yin, and nourish bone marrow, thereby improving the cognitive impairment of diabetes mellitus.27 Therefore, the above acupoints were selected for electrical stimulation in this study.
To date, there have been multiple studies on the relationship between acupuncture and cognitive function.27–29 Research has shown that perioperative acupoint stimulation could protect brain function by increasing the level of superoxide dismutase, inhibiting the oxidative stress response, and reducing the release of proteins that could cause brain injuries, thereby reducing the occurrence of postoperative cognitive impairment in elderly patients.28,29 In a prospective randomized controlled trial of elderly patients undergoing spinal surgery, Zhang et al30 found that preoperative electroacupuncture pretreatment of the DU20, ST36 (Dazhui), and ST36 (Zusanli) acupoints could reduce serum interleukin (IL) levels of IL6 and IL-10, inhibit the inflammatory response, and reduce the incidence of postoperative cognitive dysfunction. Soligo et al17 identified that electroacupuncture could improve the memory-related function of the hippocampus in diabetic rats, restore the damaged long-term potentiation of the dentate gyrus, and increase the expression of vesicular glutamate transporter 1, thereby normalizing the activity-dependent release of proNGF in the hippocampus of diabetic rats. This suggested that electroacupuncture could promote hippocampal nervous activity as well as neuronal metabolism and function, thereby improving diabetic cognitive impairment. The current study demonstrated that electroacupuncture could increase the absolute value of rSO2 in patients undergoing diabetic foot surgery, indicating an increase in regional cerebral blood flow and oxygen supply.
The current study had some limitations that may have affected its results. These were as follows: (1) a small sample size, (2) only patients with diabetes aged 65 or older were included, (3) participants’ cognitive function was not evaluated, and (4) only the effect of acupuncture on rSO2 was observed. Accordingly, the authors aim to further explore the correlation between changes in rSO2 and postoperative cognitive dysfunction in patients with diabetes in the future.
Conclusion
This study demonstrated that electroacupuncture stimulation of the DU20, DU24, and EX-HN1 acupoints could enhance the rSO2 of elderly patients with diabetes. Based on the potential value of rSO2 in predicting postoperative cognitive function, it is speculated that electroacupuncture preconditioning had a potentially neuroprotective effect on elderly patients with diabetes.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding Statement
The current research was funded by Beijing Municipal Science and Technology Commission (Code: Z171100001017061), Chinese medicine special of the capital (Code: 17ZY04), Beijing Municipal Administration of Hospitals Incubating Program (Code: PZ2017028), and CFH (Code: 2022-2-2232).
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Beijing Hospital of Traditional Chinese Medicine (2021BL02-042). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Sun H, Saeedi P, Karuranga S, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi: 10.1016/j.diabres.2021.109119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Sloten TT, Sedaghat S, Carnethon MR, Launer LJ, Stehouwer CDA. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression. Lancet Diabetes Endocrinol. 2020;8(4):325–336. doi: 10.1016/S2213-8587(19)30405-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu SB, Dai Y, Zhao JN. Research progress of diabetic encephalopathy. Chin J Pharmacol Toxicol. 2019;33(06):444–445. [Google Scholar]
- 4.Liu Y, Zhang S, Tomata Y, Nurrika D, Sugawara Y, Tsuji I. The impact of risk factors for dementia in China. Age Ageing. 2020;49(5):850–855. doi: 10.1093/ageing/afaa048 [DOI] [PubMed] [Google Scholar]
- 5.Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017;49(2):106–116. doi: 10.1080/07853890.2016.1231932 [DOI] [PubMed] [Google Scholar]
- 6.Hingorani A, LaMuraglia GM, Henke P, et al. The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016;63(2Suppl):3S–21S. doi: 10.1016/j.jvs.2015.10.003 [DOI] [PubMed] [Google Scholar]
- 7.Lu Q, Wang J, Wei X, et al. Cost of diabetic foot ulcer management in China: a 7-year single-center retrospective review. Diabetes Metab Syndr Obes. 2020;13:4249–4260. doi: 10.2147/DMSO.S275814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Natovich R, Kushnir T, Harman-Boehm I, et al. Cognitive dysfunction: part and parcel of the diabetic foot. Diabetes Care. 2016;39(7):1202–1207. doi: 10.2337/dc15-2838 [DOI] [PubMed] [Google Scholar]
- 9.Jo YY, Shim JK, Soh S, Suh S, Kwak YL. Association between cerebral oxygen saturation with outcome in cardiac surgery: brain as an index organ. J Clin Med. 2020;9(3):840. doi: 10.3390/jcm9030840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qin XW, Chen XL, Yao L. The value of intraoperative monitoring of cerebral oxygen saturation on postoperative cognitive function in elderly patients undergoing cardiac surgery. Zhonghua Yi Xue Za Zhi. 2021;101(5):345–349. doi: 10.3760/cma.j.cn112137-20200527-01681 [DOI] [PubMed] [Google Scholar]
- 11.Kovarova L, Valerianova A, Kmentova T, Lachmanova J, Hladinova Z, Malik J. Low cerebral oxygenation is associated with cognitive impairment in chronic hemodialysis patients. Nephron. 2018;139(2):113–119. doi: 10.1159/000487092 [DOI] [PubMed] [Google Scholar]
- 12.Heringlake M, Garbers C, Käbler JH, et al. Preoperative cerebral oxygen saturation and clinical outcomes in cardiac surgery. Anesthesiology. 2011;114(1):58–69. doi: 10.1097/ALN.0b013e3181fef34e [DOI] [PubMed] [Google Scholar]
- 13.Chen ZY, Luo JS, Ding LL, et al. Study on baseline level of regional cerebral oxygen saturation and its influence factors. China Med Equip. 2021;18(07):39–43. [Google Scholar]
- 14.Mohamed A, Ismail A. Immediate fasting blood glucose response to electroacupunc- ture of ST36 versus CV12 in patients with type 2 diabetes mellitus: randomized controlled trial. Med Prim Care Rev. 2021;23(4):437–441. doi: 10.5114/fmpcr.2022.110370 [DOI] [Google Scholar]
- 15.Shin KM, Lee S, Lee EY, et al. Electroacupuncture for painful diabetic peripheral neuropathy: a multicenter, randomized, assessor-blinded, controlled trial. Diabetes Care. 2018;41(10):e141–e142. doi: 10.2337/dc18-1254 [DOI] [PubMed] [Google Scholar]
- 16.Yuan AH, Cao JP, Yang J, et al. [Electroacupuncture improves learning-memory ability in diabetic rats with cognitive impairment via inhabitating proinflammatory cytokine production through p38 MAPK and STAT3 pathway]. Zhen Ci Yan Jiu. 2020;45(8):603–610. doi: 10.13702/j.1000-0607.190870 [DOI] [PubMed] [Google Scholar]
- 17.Soligo M, Piccinin S, Protto V, et al. Recovery of hippocampal functions and modulation of muscarinic response by electroacupuncture in young diabetic rats. Sci Rep. 2017;7(1):9077. doi: 10.1038/s41598-017-08556-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li XF, Zheng M, Zhan WF, et al. Effect of electroacupuncture on intraoperative cerebral oxygen saturation and postoperative delirium in elderly patients with fragile brain function undergoing Hip replacement. Pract Geriatr. 2021;35(07):676–679. [Google Scholar]
- 19.Hermanides J, Qeva E, Preckel B, Bilotta F. Perioperative hyperglycemia and neurocognitive outcome after surgery: a systematic review. Minerva Anestesiol. 2018;84(10):1178–1188. doi: 10.23736/S0375-9393.18.12400-X [DOI] [PubMed] [Google Scholar]
- 20.Shi Y, Vanhoutte PM. Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes. 2017;9(5):434–449. doi: 10.1111/1753-0407.12521 [DOI] [PubMed] [Google Scholar]
- 21.Srikanth V, Sinclair AJ, Hill-Briggs F, Moran C, Biessels GJ. Type 2 diabetes and cognitive dysfunction-towards effective management of both comorbidities. Lancet Diabetes Endocrinol. 2020;8(6):535–545. doi: 10.1016/S2213-8587(20)30118-2 [DOI] [PubMed] [Google Scholar]
- 22.Kim J, Shim JK, Song JW, Kim EK, Kwak YL. Postoperative cognitive dysfunction and the change of regional cerebral oxygen saturation in elderly patients undergoing spinal surgery. Anesth Analg. 2016;123(2):436–444. doi: 10.1213/ANE.0000000000001352 [DOI] [PubMed] [Google Scholar]
- 23.Ding L, Chen DX, Li Q. Effects of electroencephalography and regional cerebral oxygen saturation monitoring on perioperative neurocognitive disorders: a systematic review and meta-analysis. BMC Anesthesiol. 2020;20(1):254. doi: 10.1186/s12871-020-01163-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blas M, Sulek C, Martin T, Lobato E. Use of near-infrared spectroscopy to monitor cerebral oxygenation during coronary artery bypass surgery in a patient with bilateral internal carotid artery occlusion. J Cardiothorac Vasc Anesth. 1999;13(6):732–735. doi: 10.1016/s1053-0770(99)90131-3 [DOI] [PubMed] [Google Scholar]
- 25.Gao L, Jia CH, Wang W. Recent advances in the study of ancient books on traditional Chinese medicine. World J Trad Chin Med. 2020;6(1):61. doi: 10.4103/wjtcm.wjtcm_3_20 [DOI] [Google Scholar]
- 26.Zheng HD, Wang ZQ, Li SS, et al. Effect of acupoints on acupuncture-moxibustion and its therapeutic mechanism. World J Trad Chin Med. 2020;2020:17–26. [Google Scholar]
- 27.Yang HP. Clinical Observation of Electroacupuncture at Baihui (GV20) and Sishencong (EX-HN1) for cognitive impairment associated with whole brain radiotherapy. Shanghai J Acupuncture Moxibust. 2020;39(03):305–309. [Google Scholar]
- 28.Ding LL, Kou SS, Wang Q, et al. Effect of transcutaneous electrical acupoint stimulation combined with Dexmedetomidine on postoperative delirium in elderly patients. China Med Herald. 2020;17(4):123–126. [Google Scholar]
- 29.Lu B, Ding LL, Wang Q, et al. Effect of transcutaneous electrical acupoint stimulation on cerebral oxygen metabolism, postoperative cognitive function and analgesic effect in elderly patients undergoing hip replacement. Progress Mod Biomed. 2019;19(16):3094–3097, 3114. [Google Scholar]
- 30.Zhang Q, Li YN, Guo YY, et al. Effects of preconditioning of electro-acupuncture on postoperative cognitive dysfunction in elderly: a prospective, randomized, controlled trial. Medicine. 2017;96(26):e7375. doi: 10.1097/MD.0000000000007375 [DOI] [PMC free article] [PubMed] [Google Scholar]