Abstract
Background
Takotsubo syndrome (TTS) is an emerging disease characterized by an acute and reversible myocardial dysfunction which may have an influence on clinical status and prognosis. Despite extensive research, its pathophysiology has not been completely elucidated; among other hypothesis, a heart-brain interaction has been proposed.
Methods
The aim of this study was to assess the impact of psychiatric disorders and of some personality types on the pathogenesis of TTS. We conducted a retrospective observational case-control study. We enrolled a total of 50 patients, 25 with a previous diagnosis of TTS and 25 patients with a history of acute coronary syndrome (ACS), that underwent a comprehensive lifetime psychiatric assessment.
Results
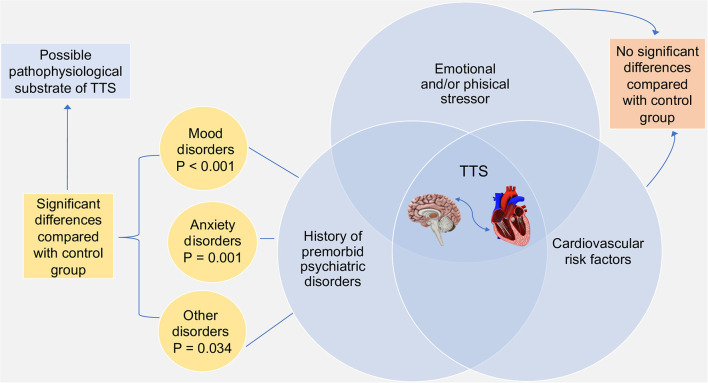
We found no significant difference between TTS and ACS patients in cardiovascular risk profile. The frequency of lifetime psychiatric disorders was significantly greater in TTS. In particular, in the univariate analysis, TTS group showed a higher prevalence of mood disorders (Major Depressive Disorder, Bipolar Disorder, Dysthymia; 16 vs. 2, P < 0.001) and anxiety disorder (Generalized Anxiety Disorder, Panic Disorder, Agoraphobia; 20 vs. 8, P = 0.001) compared with ACS group. There was also a significant tendency in TTS patients to psychotropic medication use, substance abuse, and psychologist or psychiatrist consulting. However, there was no difference between the groups in previous stressful events and Type D personality. Moreover, the multivariate analysis showed that mood disorders were independently associated with TTS (OR 16.9, 95% CI, 2.2–127).
Conclusion
Our study demonstrated that pre-existing anxiety disorders and mostly mood disorders were significantly higher in TTS patients than in ACS group, suggesting the role of psychiatric disorders as possible pathophysiological substrate of TTS.
Keywords: Takotsubo syndrome, acute coronary syndrome, psychopathology, mood disorders, anxiety disorders
Introduction
Takotsubo syndrome (TTS) is an emerging cardiovascular disease, characterized by an acute myocardial dysfunction, that predominantly affects postmenopausal women and that is often triggered by emotional or physical stressors (1). It is estimated that 1–3% of all patients and 5–6% of female patients undergoing coronary angiography for suspected acute coronary syndrome (ACS) have TTS (2). TTS usually presents with the occurrence of acute chest pain, dyspnea, palpitations, or syncope. However, it may be diagnosed incidentally by new ischemic electrocardiographic (ECG) changes, ventricular arrhythmias or elevation of cardiac biomarkers. The above findings and the echocardiographic evidence of regional contractile dysfunction make the differentiation between ACS and TTS challenging (2). However, despite the possible coexistence of TTS with ACS, coronary angiography usually does not show obstructive coronary artery disease (CAD) (3), and left ventriculography reveals peculiar and symmetric regional wall motion abnormalities, often in a circumferential apical distribution, hence the name “apical ballooning syndrome” (4).
TTS has long been considered a benign disease, since the ventricular dysfunction recovers within days or weeks (2); however, several studies demonstrated that the mortality of hospitalized patients, during the acute phase, is 4–5%, mainly due to acute heart failure or malignant ventricular arrhythmias, and the rate of long-term complications is high (5, 6). Therefore, a full comprehension of the pathophysiological mechanisms underlying the syndrome and the subsequent use of tailored therapies is crucial to improve outcomes (1).
Nowadays, the pathophysiology of TTS has not been completely clarified and different mechanisms have been proposed (1). Several emotional stressors (e.g., divorce, death of a family member, and financial problems) or physical ones (e.g., physical activity, thyrotoxicosis, sepsis, pregnancy, ACS, and stroke) have been identified as possible triggers of the syndrome (5). These stimuli may promote a sympathetic stimulation, confirmed by increased levels of plasma catecholamines, which may ultimately induce direct toxicity on cardiomyocytes, epicardial, or microvascular coronary artery spasm and acute coronary microvascular dysfunction (7–12). However, only a minority of people who experienced acute stressors then developed TTS, supporting the existence of predisposing substrates on which precipitating factors impact (2).
Based on the role of stressful stimuli and on the evidence of structural anatomical brain differences between TTS patients and healthy controls, a heart-brain interaction has been proposed to play a pivotal role in the development of TTS (13). Furthermore, previous studies have suggested that premorbid psychiatric disease could be an important predisposing risk factor for TTS (14, 15).
The aim of the present study was to assess the influence of psychiatric disorders, as a psychopathological substrate, in patients with TTS compared with patients with ACS.
Materials and Methods
We designed a retrospective observational case-control study to assess the impact of psychiatric disorders and of some personality types in TTS patients. From December 2018 to December 2021, we enrolled a total of 50 patients, 25 with a previous diagnosis of TTS and 25 patients with a history of ACS. All patients underwent a comprehensive lifetime psychiatric assessment.
The inclusion criterion was a previous diagnosis of TTS (study group) or ACS (control group), while the exclusion criteria included neurodegenerative diseases and ongoing acute psychiatric disorders.
Since all TTS patients were female, we enrolled only women in the control group to exclude the possibility of a gender-related bias.
The diagnosis of TTS was defined according to the “InterTAK criteria” (2): echocardiographic or ventriculographic evidence of apical or midventricular, basal or focal wall motion abnormalities; emotional or physical triggers that precede the onset of symptoms; new ECG ST-T abnormalities; moderately high levels of troponins and brain natriuretic peptides. The control group included patients with previous diagnosis of ST segment Elevation Myocardial Infarction (STEMI), Non-ST segment Elevation Myocardial Infarction (NSTEMI) and Unstable Angina (UA), defined according to the most recent European Guidelines (16, 17).
Both groups of patients were interviewed far from the acute phase (at a minimum of 3-month after discharge) because we assumed that the timing of psychiatric interview may impact on reliability and reproducibility of the diagnosis. In particular, the distress related to hospitalization for acute cardiovascular disease may hinder or exalt the accurate diagnosis of psychiatric disorders.
We acquired in-hospital clinical-instrumental data, including demographics assessment, cardiovascular risk profile, pharmacological anamnesis, echocardiographic evaluation, and angiographic data. All patients were questioned about their medical history and lifestyle, including the use of psychotropic drugs or substance abuse.
Several instruments were used to assess the psychological and psychopathological profile of TTS and ACS patients, including: the Emotion Regulation Questionnaire (ERQ), performed to evaluate individual tendencies to reappraise and to suppress the expression of emotions (18); the Connor-Davidson Resilience Scale (CD-RISC), used to measure stress coping ability and stress reactions (19); the DS-14, a measure of negative affectivity and social inhibition, typical features of Type D personality (20); the PID-5, a useful screening tool for personality disorders (21); the Mini International Neuropsychiatric Interview (MINI), a short structured diagnostic interview administered to diagnose the most frequent mental disorders (22) in a revised Italian version according to the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria; the Social Readjustment Rating Scale (SRRS), a questionnaire to identify major stressful life events (23).
Statistical analysis was performed using statistical software package Statistic for Data Analysis (SPSS) version 27. In the univariate analysis, Chi-square or Fisher's exact tests were used to compare categorical variables between TTS patients and ACS patients. Continuous variables were listed as mean ± standard deviation (SD) and were compared between groups using t-tests. A two-side P-value < 0.05 was required for statistical significance. Moreover, multivariable regression analysis was performed and Adjusted Odd Ratios (OR) with 95% confidence intervals (95% CI) were calculated.
Results
Clinical characteristics of the two groups are presented in Table 1: TTS and ACS patients are all female, and the mean age is respectively 67 ± 11.4 years old and 71.2 ± 10.3 years old in the two groups. We found no significant difference in TTS and ACS patients in cardiovascular risk profile (dyslipidemia, diabetes, hypertension, smoke, body mass index, cardiovascular family history, chronic kidney disease and hyperuricemia). Furthermore, no significant differences were found in previous episodes of TTS or ACS. The frequency of psychiatric disorders was significantly greater in patients with TTS compared with ACS patients. In particular the TTS group showed a higher prevalence of mood disorders (MD), i.e., Major Depressive Disorder, Bipolar Disorder, and Dysthymia (16 vs. 2, P < 0.001), anxiety disorders (AD), i.e., Generalized Anxiety Disorder, Panic Disorder and Agoraphobia (20 vs. 8, P = 0.001), and other disorders, i.e., Post-Traumatic Stress Disorder, Eating disorders and Alcohol Use Disorder (8 vs. 2, P = 0.034) compared with the control group (Table 2). Moreover, among patients with TTS, more than half of them received multiple diagnosis of psychiatric disorders in their lifetime.
Table 1.
Clinical features of TTS and ACS patients.
| TTS (n = 25) | ACS (n = 25) | P-value | |
|---|---|---|---|
| Age (mean ± SD) | 67 ± 11.4 | 71.2 ± 10.3 | 0.169 |
| Female sex | 25 (100%) | 25 (100%) | 1 |
| Diabetes | 2 (8%) | 3 (12%) | 0.751 |
| Hypertension | 10 (40%) | 15 (60%) | 0.316 |
| Dyslipidemia | 11 (44%) | 15 (60%) | 0.604 |
| Smoker | 12 (48%) | 8 (32%) | 0.087 |
| BMI | 23.1 ± 3.5 | 24.2 ± 3.9 | 0.19 |
| CV family history | 8 (32%) | 10 (40%) | 0.895 |
| CKD | 2 (8%) | 2 (8%) | 0.855 |
| Hyperuricemia | 1 (4%) | 3 (12%) | 0.363 |
| Polivascular disease | 1 (4%) | 2 (8%) | 0.658 |
| Previous ACS | 1 (4%) | 2 (8%) | 0.658 |
| Previous TTS | 1 (4%) | 0 | 0.270 |
Values are n (%) or mean ± SD.
TTS, Takotsubo Syndrome; ACS, Acute Coronary Syndrome.
Table 2.
Psychiatric features of TTS and ACS patients.
| TTS (n = 25) | ACS (n = 25) | P-value | |
|---|---|---|---|
| Mood disorders | 16 (64%) | 2 (8%) | <0.001 |
| Anxiety disorders | 20 (80%) | 8 (32%) | 0.001 |
| Other disorders | 8 (32%) | 2 (8 %) | 0.034 |
| Previous stressful events | 25 (100%) | 22 (88%) | 0.07 |
| D personality | 4 (16%) | 2 (8%) | 0.38 |
| Psychiatrist/psychologist | 16 (64%) | 3 (12%) | 0.01 |
| Psychotropic drugs | 18 (72%) | 7 (28%) | 0.02 |
| Substance abuse | 5 (20%) | 0 | 0.018 |
| Cognitive restructuring | 28.5 ± 8.7 | 28.4 ± 9.86 | 0.9 |
| Response suppression | 13.3 ± 5.8 | 14.7 ± 6.4 | 0.4 |
| Negative affectivity | 12.2 ± 5.9 | 14.8 ± 5.4 | 0.1 |
| Social inhibition | 7 ± 4.3 | 5.8 ± 3.1 | 0.28 |
| CD-RISK | 64.7 ± 13.8 | 65.36 ± 15.2 | 0.88 |
| Language/learning problems | 1 (4%) | 2 (8%) | 0.5 |
Values are n (%) or mean ± SD.
TTS, Takotsubo Syndrome; ACS, Acute Coronary Syndrome; CD-RISK, Connor Davidson Resilience Scale.
In confirmation of the above findings, there was a relevant tendency for TTS patients to psychologist or psychiatrist consulting (16 vs. 3, P = 0.01) but also to make use of psychotropic medication (18 vs. 7, P = 0.02) and substances of abuse (5 vs. 0, P = 0.018) (Table 2). Conversely, there was no difference between the groups in previous stressful events (25 vs. 22, P = 0.07) and Type D personality (negative affectivity and social inhibition; 4 vs. 2, P = 0.38; Table 2). In order to increase the strength of these associations and to evaluate the influence of confounding factors on final results, we created a multivariate logistic regression model adjusted for the six variables whose differences were statistically significant on univariate analysis between the two groups (mood disorders, anxiety disorders, other psychiatric disorders, psychiatrist/psychologist, psychotropic drugs, and substance abuse). Mood disorders were independently associated with TTS, OR 16.9 (95% CI 2.2–127).
Discussion
Since its first description in 1990, TTS has gained worldwide recognition (5). Even if several mechanisms have been proposed, such as catecholamine-induced myocardial toxicity (8), epicardial or microvascular coronary artery spasm (9, 10) and acute coronary microvascular dysfunction, the etiopathogenesis of TTS is still matter of debate (1). We hypothesized that the susceptibility to TTS could be related to a history of pre-morbid psychiatric disorders. To test this assumption, we performed a retrospective case-control study in which 25 patients with previous diagnosis of TTS and as many with previous diagnosis of ACS underwent a comprehensive lifetime psychiatric assessment, using a systematic interview.
In our study, among TTS patients, the diagnosis of either MD (16 vs. 2, P < 0.001) or AD (20 vs. 8, P = 0.001) were significantly higher than in ACS group. In particular, MD was independently associated with TTS, OR 16.9 (95% CI 2.2–127). MD and AD were found, respectively, in 64% and 80% of TTS patients, much more than the estimated lifetime prevalence in the general population (24). Moreover, more than half of TTS patients (14; 56%) received multiple diagnosis of psychiatric disorders.
Other studies have yielded similar results: in particular, a case-control study showed an association between TTS with depressive disorders, but not with anxiety syndromes (25) and other authors demonstrated a higher frequency of depressive and anxiety disorders in TTS patients compared to ACS patients (14, 15); contrarily two case-control studies showed that higher levels of anxiety, but not depression, were associated with the occurrence of TTS (26, 27).
Moreover, in our study the prevalence of “other disorders” (Post-Traumatic Stress Disorder, Eating disorders and Alcohol Use Disorder) was significantly higher (8 vs. 2, P = 0.034) in patients with TTS compared to control group.
Nowadays, it is well-known that TTS is predominantly preceded by emotional or physical stressors (5). All TTS patients have experienced at least one stressful event; however, it was not significantly higher compared to ACS group (25 vs. 22, P = 0.07). Probably, this result might support the existence of predisposing substrates that underlie the development of TTS. Moreover, despite proposed as a key role for increasing biological reactivity to acute emotional stress, the prevalence of Type D personality (characterized by negative affectivity and social inhibition) (28) did not significantly differ between TTS and ACS patients (4 vs. 2, P = 0.38).
TTS patients showed a high prevalence of cardiovascular risk factors, similar to ACS group. Probably, the progression of cardiovascular risk factors might have promoted the development of endothelial dysfunction (29), a common pathophysiological feature of TTS (30). In this regard Naegele et al. demonstrated that endothelial dysfunction is common in patients with TTS, which also suggests the propensity for coronary artery spasm (31).
Finally, in confirmation of the importance of psychiatric disorders, TTS patients made use of psychotropic medication (18 vs. 7, P = 0.02) and substances of abuse (5 vs. 0, P = 0.018), and consulted psychologist or psychiatrist (16 vs. 3, P = 0.01) more frequently than ACS patients.
Our findings might support the role of psychiatric disorders as possible correlate of neurologically mediated susceptibility to TTS, reinforcing the concept of the heart-brain interaction (32).
In this regard, some studies documented alterations of brain regions involved in autonomic functions and in regulation of the limbic system (13, 33). In particular, Templin et al. suggested that patients with TTS have structural brain alterations and hypoconnectivity of the amygdala, a component of the limbic system that notably plays a pivotal role in the response to acute stressors (13). Moreover, evidences showed that amygdalar activity independently predicts cardiovascular events (34). Interestingly, Radfar et al., through 18F-FDG-PET/CT imaging, demonstrated that baseline amygdalar activity is higher in individuals who subsequently develop TTS, supporting the existence of a predisposing neurobiological substrate of TTS (35).
Our study demonstrated that pre-existing anxiety disorders and mostly mood disorders were significantly higher in TTS patients than in ACS group, suggesting the role of psychiatric disorders as possible pathophysiological substrate of TTS, using, for the first time, a lifetime systematic psychiatric assessment performed far from the acute phase (Figure 1).
Figure 1.
Pathophysiological substrates of TTS and major results of the study.
This study has potential limitations. Firstly, there is a small-size population, which may make the result inaccurate because the data is not enough: only 50 participants. Secondly, the retrospective nature of the study gives an inferior level of evidence and the lack of follow-up data does not allow to determine whether psychiatric morbidity also have a prognostic role. Further studies are needed to confirm our findings in larger cohorts and to determine the role of MD and AD in the pathophysiology of TTS.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee Fondazione Policlinico Universitario Agostino Gemelli Rome. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LG, FC, DD'A, and GPo conducted the study. GPr, GC, AI, and MS supported the realization of the study. GPr and GC had a leading role in writing the manuscript. LG, FC, DD'A, and GPo had a leading role in manuscript revision. All authors have read and agreed to the content of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of Takotsubo syndrome. Circulation. (2017) 135:2426–41. 10.1161/CIRCULATIONAHA.116.027121 [DOI] [PubMed] [Google Scholar]
- 2.Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, et al. International expert consensus document on Takotsubo syndrome (part i): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J. (2018) 39:2032–46. 10.1093/eurheartj/ehy076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haghi D, Papavassiliu T, Hamm K, Kaden JJ, Borggrefe M, Suselbeck T. Coronary artery disease in takotsubo cardiomyopathy. Circ J. (2007) 71:1092–4. 10.1253/circj.71.1092 [DOI] [PubMed] [Google Scholar]
- 4.Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa M, et al. Angina Pectoris-Myocardial Infarction Investigations in Japan Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. (2001) 38:11–8. 10.1016/S0735-1097(01)01316-X [DOI] [PubMed] [Google Scholar]
- 5.Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, et al. Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. N Engl J Med. (2015) 373:929–38. 10.1056/NEJMoa1406761 [DOI] [PubMed] [Google Scholar]
- 6.Stiermaier T, Moeller C, Oehler K, Desch S, Graf T, Eitel C, et al. Long-term excess mortality in takotsubo cardiomyopathy: predictors, causes and clinical consequences. Eur J Heart Fail. (2016) 18:650–6. 10.1002/ejhf.494 [DOI] [PubMed] [Google Scholar]
- 7.Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. (2005) 352:539–48. 10.1056/NEJMoa043046 [DOI] [PubMed] [Google Scholar]
- 8.Lyon AR, Rees PS, Prasad S, Poole-Wilson PA, Harding SE. Stress (Takotsubo) cardiomyopathy–a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med. (2008) 5:22–9. 10.1038/ncpcardio1066 [DOI] [PubMed] [Google Scholar]
- 9.Sato HTH, Uchida T, Dote K, Ishihara M. Tako-tsubo like left ventricular dysfunction due to multivessel coronary spasm. In: Kodama K, Haze K, Hori M, editors, Clinical Aspect of Myocardial Injury: From Ischaemia to Heart Failure. (In Japanese). Tokyo: Kagakuhyoronsha Publishing; (1990). p. 56–64. [Google Scholar]
- 10.Angelini P. Transient left ventricular apical ballooning: a unifying pathophysiologic theory at the edge of Prinzmetal angina. Catheter Cardiovasc Interv. (2008) 71:342–52. 10.1002/ccd.21338 [DOI] [PubMed] [Google Scholar]
- 11.Galiuto L, De Caterina AR, Porfidia A, Paraggio L, Barchetta S, Locorotondo G, et al. Reversible coronary microvascular dysfunction: a common pathogenetic mechanism in Apical Ballooning or Tako-Tsubo Syndrome. Eur Heart J. (2010) 31:1319–27. 10.1093/eurheartj/ehq039 [DOI] [PubMed] [Google Scholar]
- 12.Galiuto L, Crea F. Primary and secondary takotsubo syndrome: pathophysiological determinant and prognosis. Eur Heart J Acute Cardiovasc Care. (2020) 9:690–3. 10.1177/2048872620963493 [DOI] [PubMed] [Google Scholar]
- 13.Templin C, Hänggi J, Klein C, Topka MS, Hiestand T, Levinson RA, et al. Altered limbic and autonomic processing supports brain-heart axis in Takotsubo syndrome. Eur Heart J. (2019) 40:1183–7. 10.1093/eurheartj/ehz068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Summers MR, Lennon RJ, Prasad A. Pre-morbid psychiatric and cardiovascular diseases in apical ballooning syndrome (tako-tsubo/stress-induced cardiomyopathy): potential pre-disposing factors? J Am Coll Cardiol. (2010) 55:700–1. 10.1016/j.jacc.2009.10.031 [DOI] [PubMed] [Google Scholar]
- 15.Delmas C, Lairez O, Mulin E, Delmas T, Boudou N, Dumonteil N, et al. Anxiodepressive disorders and chronic psychological stress are associated with Tako-Tsubo cardiomyopathy- New Physiopathological Hypothesis. Circ J. (2013) 77:175–80. 10.1253/circj.CJ-12-0759 [DOI] [PubMed] [Google Scholar]
- 16.Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2018) 39:119–77. 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 17.Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. (2021) 42:1289–367. 10.1093/eurheartj/ehab088 [DOI] [PubMed] [Google Scholar]
- 18.Seixas R, Pignault A, Houssemand C. Emotion regulation questionnaire-adapted and individual differences in emotion regulation. Eur J Psychol. (2021) 17:70–84. 10.5964/ejop.2755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depr Anxiety. (2003) 18:76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 20.Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. (2005) 67:89–97. 10.1097/01.psy.0000149256.81953.49 [DOI] [PubMed] [Google Scholar]
- 21.Zhang P, Ouyang Z, Fang S, He J, Fan L, Luo X, et al. Personality inventory for DSM-5 brief form (PID-5-BF) in Chinese students and patients: evaluating the five-factor model and a culturally informed six-factor model. BMC Psychiatry. (2021) 21:107. 10.1186/s12888-021-03080-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. (1998) 59(Suppl.20):22–33. [PubMed] [Google Scholar]
- 23.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. (1967) 11:213–8. 10.1016/0022-3999(67)90010-4 [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: results from the WHO World Mental Health Survey Initiative. Depr Anxiety. (2010) 27:351–64. 10.1002/da.20634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sancassiani F, Carta MG, Montisci R, Preti A, Machado S, Moro MF, et al. Takotsubo syndrome is associated with mood disorders and antidepressants use, not with anxiety and impairment of quality of life due to the psychiatric disorder. Clin Pract Epidemiol Ment Health. (2018) 14:26–32. 10.2174/1745017901814010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goh AC, Wong S, Zaroff JG, Shafaee N, Lundstrom RJ. Comparing anxiety and depression in patients with Takotsubo stress cardiomyopathy to those with acute coronary syndrome. J Cardiopulm Rehabil Prev. (2016) 36:106–11. 10.1097/HCR.0000000000000152 [DOI] [PubMed] [Google Scholar]
- 27.Salmoirago-Blotcher E, Rosman L, Wittstein IS, Dunsiger S, Swales HH, Aurigemma GP, et al. Psychiatric history, post-discharge distress, and personality characteristics among incident female cases of takotsubo cardiomyopathy: a case-control study. Heart Lung. (2016) 45:503–9. 10.1016/j.hrtlng.2016.07.008 [DOI] [PubMed] [Google Scholar]
- 28.Compare A, Bigi R, Orrego PS, Proietti R, Grossi E, Steptoe A. Type D personality is associated with the development of stress cardiomyopathy following emotional triggers. Ann Behav Med. (2013) 45:299–307. 10.1007/s12160-013-9474-x [DOI] [PubMed] [Google Scholar]
- 29.Incalza MA, D'Oria R, Natalicchio A, Perrini S, Laviola L, Giorgino F. Oxidative stress and reactive oxygen species in endothelial dysfunction associated with cardiovascular and metabolic diseases. Vascul Pharmacol. (2018) 100:1–19. 10.1016/j.vph.2017.05.005 [DOI] [PubMed] [Google Scholar]
- 30.Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, et al. International expert consensus document on Takotsubo syndrome (part ii): diagnostic workup, outcome, and management. Eur Heart J. (2018) 39:2047–62. 10.1093/eurheartj/ehy077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Naegele M, Flammer AJ, Enseleit F, Roas S, Frank M, Hirt A, et al. Endothelial function and sympathetic nervous system activity in patients with Takotsubo syndrome. Int J Cardiol. (2016) 224:226–30. 10.1016/j.ijcard.2016.09.008 [DOI] [PubMed] [Google Scholar]
- 32.Goldfinger JZ, Nair A, Sealove BA. Brain-heart interaction in takotsubo cardiomyopathy. Heart Fail Clin. (2013) 9:217–23. 10.1016/j.hfc.2012.12.013 [DOI] [PubMed] [Google Scholar]
- 33.Hiestand T, Hänggi J, Klein C, Topka MS, Jaguszewski M, Ghadri JR, et al. Takotsubo syndrome associated with structural brain alterations of the limbic system. J Am Coll Cardiol. (2018) 71:809–11. 10.1016/j.jacc.2017.12.022 [DOI] [PubMed] [Google Scholar]
- 34.Tawakol A, Ishai A, Takx RA, Figueroa AL, Ali A, Kaiser Y, et al. Relation between resting amygdalar activity and cardiovascular events: a longitudinal and cohort study. Lancet. (2017) 389:834–45. 10.1016/S0140-6736(16)31714-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Radfar A, Abohashem S, Osborne MT, Wang Y, Dar T, Hassan MZO, et al. Stress-associated neurobiological activity associates with the risk for and timing of subsequent Takotsubo syndrome. Eur Heart J. (2021) 42:1898–908. 10.1093/eurheartj/ehab029 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.