Abstract
Objectives
Up-to-date information on the current practices and attitudes of veterinarians in Australia to acute pain management in cats was sought in 2017–2018 in the first nationwide survey in over 20 years.
Methods
An online survey was created, consisting of 54 questions in four sections, with 18 feline-specific questions. Veterinarians throughout Australia were invited to participate in the survey through advertisements in the veterinary press, electronic and regular mail, and through in-clinic visits and promotional materials.
Results
A total of 614 veterinarians completed the survey, with 513 (83.6%) completing the feline-specific section. The demographics of the respondents of this survey were an accurate representation of the registered veterinarians in Australia at the time. Multiple different opioids and non-steroidal anti-inflammatory drugs (NSAIDs) were widely available in practices to manage pain, with analgesic efficacy reported as the primary factor influencing drug selection. Opioids were most commonly used in the preoperative period and NSAIDs were most commonly used postoperatively. Despite the wide availability in clinic (>99%), only 55% of respondents reported regularly using local anaesthetic techniques in cats. Pain assessment of hospitalised patients was primarily performed by veterinarians (91.1%); however, 84.7% of respondents did not routinely use a validated pain scale.
Conclusions and relevance
Veterinary practitioners in Australia are adequately equipped with analgesic medication to treat pain in their patients. In the management of acute pain in cats, they frequently use a multimodal approach and practice a variety of analgesic protocols. Based on the results of this survey, potential areas for improvement in feline pain management include an increase in duration of postoperative analgesia and more routine use of validated pain scales, performed by nurses and veterinarians alike, to assess individual analgesic needs.
Keywords: Analgesia, pain, survey, NSAID, opioid
Introduction
Effective pain management is essential for animal well-being and to achieve positive health outcomes. Inadequate pain management in the postoperative period has been demonstrated to delay feeding, prolong recovery and contribute to patient morbidity, while poorly managed chronic pain can negatively affect quality of life.1,2
Many factors can influence pain management practices, including staff knowledge of, familiarity with and attitudes to analgesic drugs and techniques, and the use of pain assessments.3,4 Surveys of veterinarians have previously assessed these factors and demonstrated both geographical differences and temporal variation.
There are limited published data regarding pain management in dogs and cats by veterinarians in Australia, and the data available demonstrate a significant temporal change in practices. For example, in a 1996 survey of veterinarians in Australia, only 6% of respondents reported providing analgesia for feline and canine ovariohysterectomy, while 96% of veterinarians from a single state in Australia (Queensland) reported providing pain relief for canine ovariohysterectomy in 2012.5,6 A 2014 comparative survey of Australian, New Zealand and UK veterinarians showed high use of analgesia in cats undergoing gonadectomy, with 92.2% (castration) and 95% (ovariohysterectomy) of respondents providing pre- and intraoperative analgesia overall. 7 Despite a significant improvement in pre- and intraoperative analgesia, the provision of take-home pain relief after discharge was found to be suboptimal at only 16.1% and 3.8% for cat ovariohysterectomies and castrations, respectively, highlighting opportunities for improved pain recognition and management in practice. 7
The objective of this study was to obtain data on the pain management practices of companion animal veterinarians in Australia to understand the current state of pain management in dogs and cats, and to potentially identify suboptimal pain management practices. Through this knowledge, strategies may be implemented to optimise pain management and patient wellbeing. The data presented herein are part of the feline component of this Australia-wide survey.
Materials and methods
An online questionnaire was developed comprising 54 questions in four sections: (1) demographics and practice details; (2) analgesic drugs and techniques; and acute and chronic pain management in (3) dogs and (4) cats. The first two sections were mandatory, while respondents could choose to complete one or both of the species-specific sections. Survey questions were, in part, based on previously published work, 8 to allow meaningful temporal and geographical comparisons to be made. A full copy of the questionnaire is available as supplementary material. Veterinarians were invited to participate through advertisements in the veterinary press, electronic and regular mail, and through in-clinic visits and promotional materials. The predetermined study period was from November 2017 to March 2018.
Demographic data collected in section 1 included the respondent’s sex; when and where they graduated; if they were a specialist or general practitioner; and the type of practice (eg, small animal vs mixed practice, and proportion of canine and feline cases). Postcode data were collected and used to inform relative socioeconomic and remoteness measures using the Socio-Economic Indexes for Areas (SIEFA; Australian Bureau of Statistics) database and Accessibility/Remoteness Index of Australia (ARIA+; Australian Bureau of Statistics).
The second section investigated what drugs were available for use in the respondents’ practice and provided information on pain assessment in the clinic.
The canine- and feline-specific sections questioned respondents on acute and chronic pain management. For acute pain management this included questions on the use of non-steroidal anti-inflammatory drugs (NSAIDs), opioids and local anaesthetics, including factors relevant in drug selection. Pain rankings and analgesia protocols for a variety of common surgical and medical conditions were investigated. For chronic pain management, respondents provided information on treatment recommendations for mild, moderate and severe osteoarthritis, and on factors relevant to selection of NSAIDs and nutraceuticals in these patients.
In this paper, specific data relevant to acute pain management in cats are presented, together with the generic questions regarding demographics and treatment availability.
Data analyses
Data were exported from SurveyMonkey to Microsoft Excel (version 16). Descriptive statistical analysis was performed using R Studio (version 1.1.442). Graphs were produced using GraphPad Prism version 9.0.0 for Windows (GraphPad Software). Descriptive statistics were calculated for each of the questions for all respondents and groups of respondents based on their responses to the demographic questions (ie, sex, socioeconomic status, practitioner type [general practitioner/specialist], time since graduation and practice type).
The respondent postcodes were classified based on remoteness according to the Accessibility/Remoteness Index of Australia as major cities, inner regional, outer regional, remote or very remote. Where a single postcode included multiple remoteness classifications, the overall measure of remoteness was based on the least remote category. Relative socioeconomic advantage and disadvantage of respondent postcodes were determined from SIEFA database. The Index of Relative Socioeconomic Advantage or Disadvantage (IRSAD) ranks areas on a continuum from most disadvantaged to most advantaged using variables such as income, education, employment, occupation and housing. High, medium and low areas were defined as those classified in the top, middle and bottom thirds, respectively.
Results
Demographics
A total of 614 veterinarians completed the survey, with all of these completing the canine section and 513 (83.6%) completing the feline section. The demographics of the respondents are given in Table 1.
Table 1.
Demographics of the 614 veterinarian survey respondents
| Demographics | Number of respondents | Percentage of total (%) |
|---|---|---|
| Years since graduation | ||
| 0–2 | 50 | 8.14 |
| 3–5 | 81 | 13.19 |
| 6–10 | 107 | 17.43 |
| 11–20 | 154 | 25.08 |
| 21+ | 222 | 36.16 |
| Training | ||
| General practitioner | 606 | 98.7 |
| Specialist | 8 | 1.3 |
| Sex | ||
| Female | 414 | 67.43 |
| Male | 200 | 32.57 |
| Veterinary school | ||
| Charles Sturt University | 20 | 3.26 |
| James Cook University | 33 | 5.37 |
| Massey University | 15 | 2.44 |
| Murdoch University | 77 | 12.54 |
| University of Adelaide | 11 | 1.79 |
| University of Melbourne | 106 | 17.26 |
| University of Queensland | 153 | 24.92 |
| University of Sydney | 143 | 23.29 |
| Overseas | 56 | 9.12 |
| Practice details | ||
| Mixed animal | 163 | 26.55 |
| Small animal only | 451 | 73.45 |
| Time spent on | ||
| Mixed | 97 | 15.8 |
| Predominantly cats | 9 | 1.47 |
| Predominantly dogs | 508 | 82.74 |
| Region | ||
| Major city | 364 | 60.1 |
| Inner regional | 152 | 25.1 |
| Outer regional | 79 | 13 |
| Remote and very remote | 11 | 1.8 |
| IRSAD score* | ||
| High | 267 | 44.6 |
| Medium | 190 | 31.8 |
| Low | 141 | 23.6 |
Index of Relative Socioeconomic Advantage or Disadvantage (IRSAD) scores are a measure of socioeconomic advantage or disadvantage based on geographical location and categorised into high, medium and low areas (top, middle and bottom thirds, respectively)
Analgesic drugs and techniques
The availability of different pharmaceuticals within a practice to manage pain is shown in Table 2. Most practices had multiple different NSAIDs (mode = 3) and opioids (mode = 4) available. Five practices reported not having any opioids available, but all had at least one NSAID. All but one practice (99.8%) stocked cyclooxygenase 2 (COX-2)-preferential NSAIDs; the remaining practice stocked only COX-2 selective NSAIDs (coxibs). Nearly all (95.4%) stocked both full and partial mu opioid agonists. Most practices had local anaesthetic agents and a range of adjunct analgesics available. Note that pharmaceuticals selected in this section were those available in the clinic, and their availability in the clinic does not imply they were used in cats (eg, paracetamol [acetaminophen]).
Table 2.
Availability of non-steroidal anti-inflammatory drugs (NSAIDs), opioids, local anaesthetics and adjunct pain management medications in the veterinarians’ practice
| Number (%) | |
|---|---|
| NSAIDs | |
| Meloxicam | 610 (99.35) |
| Carprofen | 502 (81.76) |
| Firocoxib | 428 (69.71) |
| Robenacoxib | 207 (33.71) |
| Mavacoxib | 131 (21.34) |
| Tolfenamic acid | 14 (2.28) |
| Piroxicam | 9 (1.47) |
| Phenylbutazone | 2 (0.33) |
| Ketoprofen | 2 (0.33) |
| Flunixin | 5 (0.81) |
| Opioids | |
| Methadone | 584 (95.11) |
| Butorphanol | 579 (94.30) |
| Buprenorphine | 577 (93.97) |
| Fentanyl patch | 421 (68.57) |
| Morphine | 212 (34.53) |
| Fentanyl | 168 (27.36) |
| Codeine | 25 (4.07) |
| Buprenorphine patch | 4 (0.65) |
| Hydromorphone | 1 (0.16) |
| None | 6 (0.98) |
| Local anaesthetics | |
| Lignocaine (lidocaine) | 593 (97.21) |
| Bupivacaine | 308 (50.49) |
| Mepivacaine | 25 (4.10) |
| Other | 16 (2.62) |
| None | 5 (0.82) |
| Adjunct treatments | |
| Tramadol | 585 (95.28) |
| Medetomidine | 573 (93.32) |
| Maropitant | 577 (93.97) |
| Ketamine | 551 (89.74) |
| Gabapentin | 539 (87.79) |
| Paracetamol | 83 (13.52) |
A total of 610 respondents for the local anaesthetic question
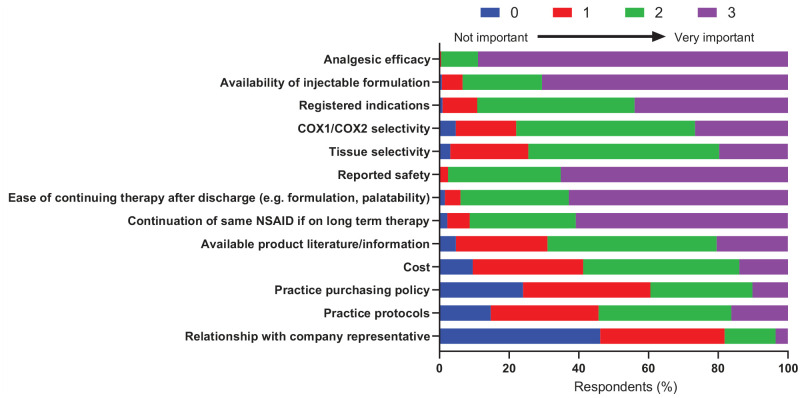
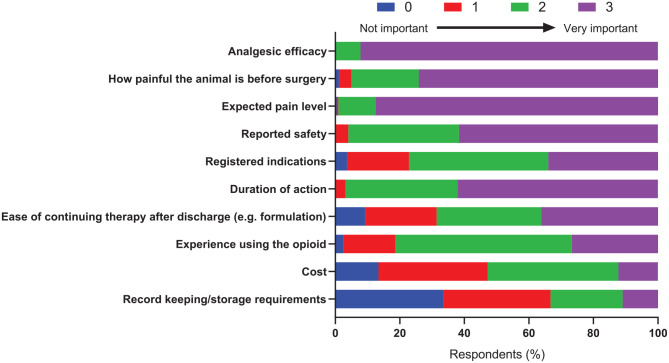
The importance of factors influencing the choice of NSAIDs and opioids in the peri-/postoperative period is shown in Figures 1 and 2. For both NSAIDs and opioids, efficacy was reported as the primary factor in drug selection.
Figure 1.
The importance of factors influencing peri- and postoperative non-steroidal anti-inflammatory drug (NSAID) choice for cats, rated on a four-point scale (0–3), with 0 being not important and 3 being very important. COX = cyclooxygenase
Figure 2.
The importance of factors influencing peri- and postoperative opioid choice for cats, rated on a four-point scale (0–3), with 0 being not important and 3 being very important
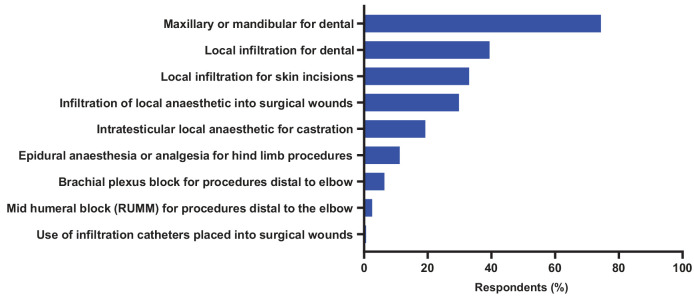
Although local anaesthetics were widely available (>99% of respondents), only 55% of veterinarians reported using them routinely in cats. Routine use of local anaesthetics in cats was more common in small animal-only practices (58%) vs mixed practices (48%). Of those using local anaesthetics regularly, maxillary or mandibular blocks used in dental procedures were the most commonly performed technique (Figure 3).
Figure 3.
Local anaesthetic techniques performed by veterinarians who routinely use local anaesthetics in cats. RUMM = radial, ulnar, musculocutaneous and median nerves
Pain assessment
Veterinarians (91.1%) rather than veterinary nurses (8.9%) were reported as the person that routinely assess the pain needs of patients in hospital, and in most cases respondents (84.7%) did not routinely use a validated pain scale. Of those that did use pain scales, the most frequently used was the Glasgow Composite Measure Pain Scale (43.6%), followed by the Colorado State University Pain Scale (21.3%); however, the species in which they were used was not specified.9–11
Acute pain management
The timing of first administration of NSAIDs and opioids in the perioperative period (from premedication/induction of anaesthesia until 24 h after surgery) to a healthy cat undergoing surgery is shown in Figure 4. More recently graduated veterinarians (<10 years since graduating) were less likely to administer NSAIDs intraoperatively than veterinarians who had graduated 10 or more years prior (11.5% vs 19.6%, respectively). Opioids were most commonly used in the preoperative period, and NSAIDs were most commonly used postoperatively.
Figure 4.
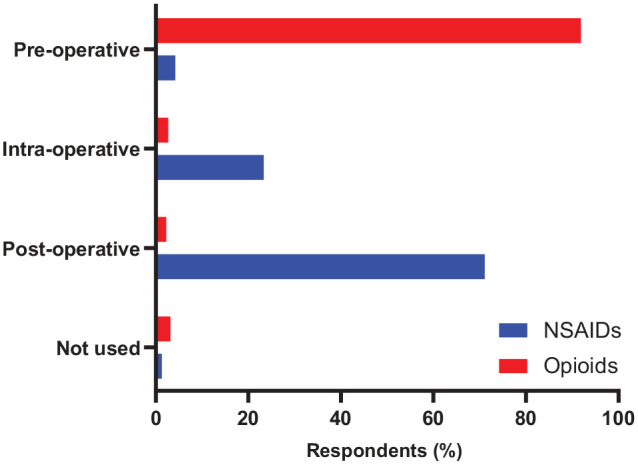
Timing of when a non-steroidal anti-inflammatory drug (NSAID) or opioid is first administered in a healthy cat in the perioperative period. ‘Preoperative’ was defined as the time from premedication to the induction of anaesthesia; ‘intraoperative’ was the time from induction of anaesthesia to extubation/recovery (cat in sternal recumbency); and ‘postoperative’ as the time from anaesthetic recovery (cat in sternal recumbency) onward
When using NSAIDs perioperatively, intravenous fluids (71.2%) and preoperative blood tests (complete blood count and/or biochemistry; 61.8%) were frequently performed, while 18.5% of respondents stated that they did not perform any specific testing or monitoring (Figure 5). There was no difference in the use of any of the tests or monitoring procedures for cats regardless of the recency of graduation (<10 years vs ⩾10 years).
Figure 5.
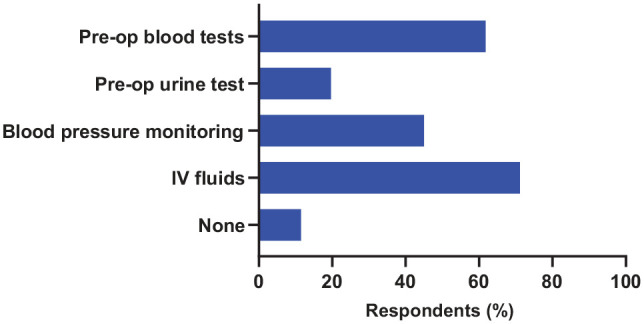
Testing and monitoring performed by veterinarians when using non-steroidal anti-inflammatory drugs (NSAIDs) preoperatively (pre-op) and/or intraoperatively in cats. IV = intravenous
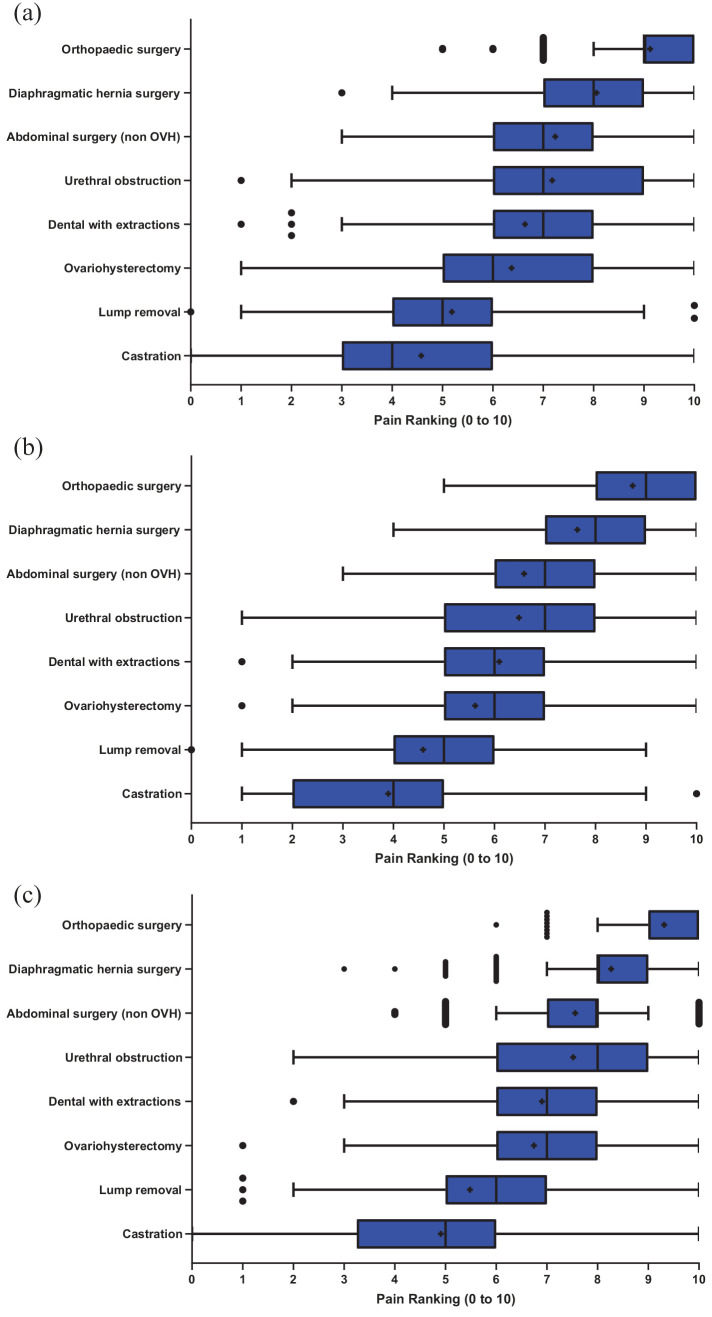
Pain ranking
Respondents were asked to provide estimated pain scores using a numerical rating scale of 0–10 (no pain to worst imaginable pain) for cats undergoing a variety of common surgical procedures or with defined medical conditions. Summary data are shown in Figure 6a. Male respondents reported lower pain scores than female respondents across all scenarios. Sex differences are shown in Figure 6b,c. Time since graduation (<10 years vs ⩾10 years) did not significantly affect the reported median pain rankings.
Figure 6.
Tukey plots of pain scores given by survey respondents for common surgical and medical conditions in cats on a scale of 0–10, where 0 is no pain and 10 is the worst pain imaginable. (a) Combined male and female respondent scores; (b) male respondent scores; (c) female respondent scores. + represents mean pain score OVH = ovariohysterectomy
Pain management protocols
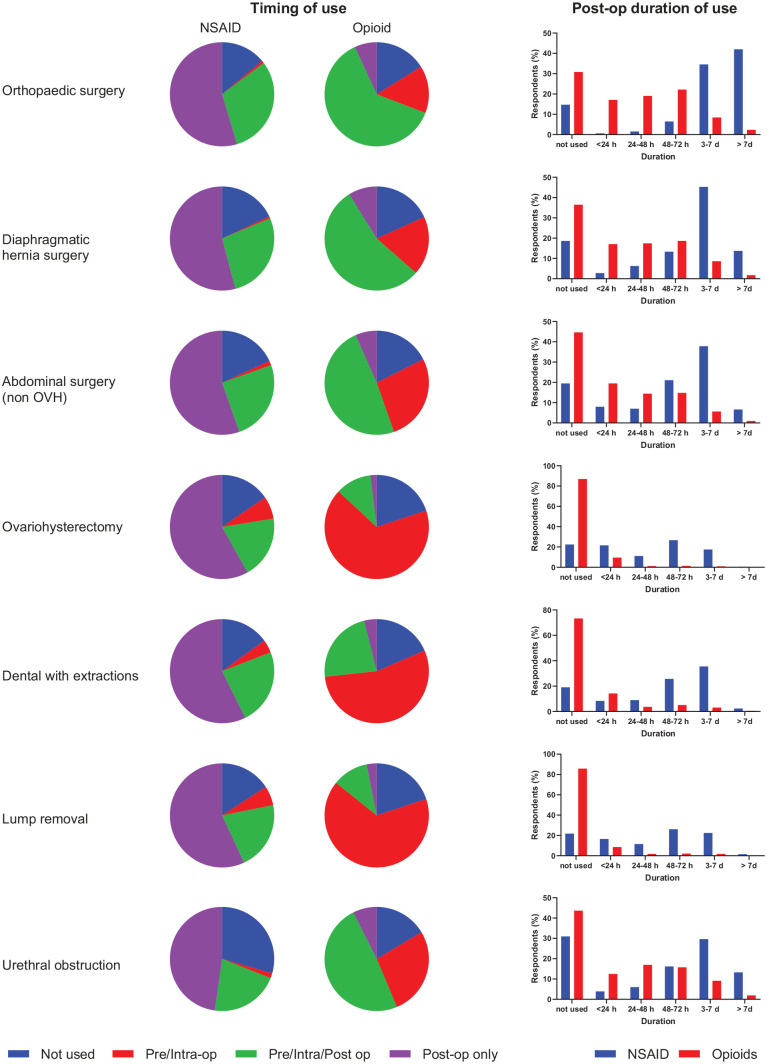
NSAIDs and opioids were the most frequently used drugs in managing the clinical conditions and procedures described, with multimodal analgesia commonly used. A summary of the timing and duration of NSAID and opioid administration for each condition or procedure is shown in Figure 7. Tabulated full data on analgesia protocols, including the use of local anaesthetics and adjunct therapies, is provided in full in the supplementary material.
Figure 7.
Summary of non-steroidal anti-inflammatory drug (NSAID) and opioid use (timing and postoperative duration) for various surgeries and medical conditions in cats. OVH = ovariohysterectomy.
Discussion
Pain management is a critical aspect of veterinary practice. The results of the current survey found that practitioners in Australia are adequately equipped to treat pain in their patients, frequently use a multimodal approach and practice a variety of analgesic protocols to manage acute pain in cats. Potential areas for protocol optimisation based on these data include increased duration of postoperative analgesia and more routine use of validated pain scales to assess individual analgesic needs.
Geographical and temporal differences in feline analgesia are reported in the literature; however, the lack of longitudinal studies in the same population make it difficult to determine the relative contribution of each factor. For example, while the perceived relative pain levels have not changed over time, the absolute scores assigned to procedures have increased, with the average reported pain score for a cat undergoing ovariohysterectomy surgery increasing from 3–4.05 in the mid-to-late 1990s to 6.4 in the current survey.12,13 Analgesic use has also increased over time. In 1999, only 26% of British veterinarians were administering analgesics for cats undergoing ovariohysterectomy and only 13.7% of cats undergoing neutering were intentionally administered perioperative analgesia by South African veterinarians.14,15 This compares to 84.6% and 80.1% of veterinarians in Australia administering NSAIDs and opioids, respectively, in the current study. These results are similar to those of veterinarians in Ontario, Canada, in 2012 and Brazil in 2007–2008, where 84% provided perioperative analgesia and 78% provided analgesia before and during anaesthesia for cat ovariohysterectomy, respectively.16,17 Such changes may reflect increasing awareness of pain in cats and the importance of its management, although geographical differences cannot be excluded. However, some longitudinal data in Australia are available, which suggest that pain management in cats has remained stable over the past decade, with 29.3% providing pre- and intraoperative NSAIDs for cat ovariohysterectomies in 2010–2011, 7 and 26.5% (pre-/intra- and pre-/intra-/postoperative, with postoperative only excluded) in the current study. This is still well below that of veterinarians in the UK, where 71.4% were giving NSAIDs (44.3% alone, 27.1% in combination with opioids) pre-/intraoperatively for cat ovariohysterectomies and castrations in 2010–2011, 7 and 98% reported to be administering NSAIDs pre-/intraoperatively to dogs and cats for routine surgeries in 2013. 8
Global bodies recommend NSAIDs as the mainstay for management of mild-to-moderate perioperative pain, as well as chronic pain management; however, the published literature has identified geographical differences in the pattern of use.2,18 For routine surgeries such as neutering cats, veterinarians in Australia and New Zealand have been reported to be more likely to administer NSAIDs postoperatively, while UK veterinarians administer NSAIDs pre-/intraoperatively and postoperatively.7,8 Australian and New Zealand veterinarians have been reported to be either more likely to prescribe an opioid in the pre-/intraoperative period than UK veterinarians or have similar administration rates as their northern hemisphere colleagues.7,8 This pattern, where the majority of Australian veterinarians administer NSAIDs in the postoperative period only and opioids pre-/intraoperatively, was reflected in the current study. Farnworth et al suggest differences in considerations regarding the risks associated with NSAIDs to be a possible reason for the regional differences seen. 7 The reduced use of NSAIDs in cats in Australia may reflect concern about potential side effects, as well as a lack of medication licensed for perioperative injection followed by oral administration (in Australia, meloxicam is registered for a single injection only, unlike in Europe where veterinarians can follow this with an oral solution).
While the preoperative use of NSAIDs, prior to tissue injury, may – theoretically – be of benefit in reducing subsequent nociception and the intensity of postoperative pain, apart from a single study with carprofen, there is a paucity of veterinary literature critically assessing this approach, with data extrapolated from human medicine. 19 The more encompassing preventive analgesia approach considers the potential benefits of treatment given in the perioperative period in preventing operative pain and central sensitisation, irrespective of its timing in relation to tissue injury.20,21 Additional studies are needed in both human and veterinary medicine to elucidate the relative benefits of pre-emptive (preoperative) vs preventive analgesia; however, it may be that differences in the timing of administration of NSAIDs in the perioperative period may be of little clinical relevance.
The veterinarian’s knowledge and comfort in using certain analgesics and/or techniques, in addition to capability in assessing and diagnosing pain, impact on the effectiveness of pain management protocols. 3 Use of validated pain scales performed at appropriate time intervals assist in assessing sufficiency of analgesia; however, a proactive approach in which pain is pre-empted and analgesia provided based on its expected severity and duration, can improve patient wellbeing. Guidelines such as those produced by the World Small Animal Veterinary Association (WSAVA) provide standard recommendations for some procedures and set a useful minimum benchmark recommendation. 2 When comparing the WSAVA recommendations for postoperative pain relief for ovariohysterectomy (up to 72 h) to the present study, more than half the respondents (55.8%) may be providing insufficient postoperative pain relief. This may be an optimistic view, however, as this calculation includes respondents reported as treating with NSAIDs for 48–72 h postoperatively (ie, some of these will be <72 h). Additionally, previous work has noted that veterinarians in the UK administer a single dose of an injectable NSAID (carprofen) to a cat assuming that it provides up to 72 h of analgesia based on an interpretation of pharmacokinetic data; however, there are no published efficacy data to support this duration. 8 Thus, if a similar view is held in Australia, respondents may have overestimated the duration of analgesia they are providing, and, despite their best intentions, are not treating in accordance with WSAVA recommendations.Differences in study design limit direct comparisons with other papers; however, prior research does provide some important insights into the practices of veterinarians with regard to the duration of postoperative analgesia being prescribed. The results of the current survey are consistent with the conclusion by Farnworth et al, 7 in that many cats were only receiving analgesia at the clinic and not beyond the first 24 h after surgery (likely provided by a NSAID and/or opioid given perioperatively). Similarly, a recent (2020) New Zealand study showed that the most common treatment regimen for feline ovariohysterectomy (52%) was the administration of a single injection of meloxicam, postoperatively. 22
The role of sex on the perception and management of pain has been previously reported, with a number of studies demonstrating that female veterinarians rank pain higher than male veterinarians.4,23,24 Sex-related differences in the individual perception and experience of pain between males and females are reported, with biological, social and psychological mechanisms proposed to account for these differences. 25 Using a variety of experimental models, females are reported to experience greater pain sensitivity than males, and, clinically, females are at increased risk for chronic pain syndromes. 25 Projection of personal pain experiences when considering the pain of their patients may result in greater empathy, which could account for reported sex differences in pain assessment. The empathy of the observer has been shown to influence pain perception, with higher empathy associated with increased estimates of pain. 26 Female veterinarians have been reported to be more empathetic than males, which may account for the differences in pain perception reported in the current study. 27 However, sex differences in pain assessment and management are not uniform across the published literature, likely reflecting the complex and multifaceted nature of pain assessment and its management.7,28
Evidence for the effect of time since graduation on pain management is mixed. Older publications have reported that more recent graduates were more likely to prescribe analgesia, whereas more recent publications report that the effect of recency or year of graduation varies from having some effect, a non-significant effect or no association with analgesic use.7,8,12,13,17 This latter observation was similar to that of the current study where the recency of graduation (<10 years vs ⩾10 years) did not influence the duration of postoperative analgesia provided after a cat ovariohysterectomy. It has been previously described that recent graduates (<10 years since graduating) assign higher pain scores for surgical procedures than more experienced colleagues; however, this finding was not repeated in the current study or in a 2015 study of veterinarians in the UK.8,16 The lack of significant effect of time since graduation on pain management practices in the current study compared with earlier work may potentially reflect a general improvement in knowledge, education and training in this area over time, or geographical differences.
Previous work has shown that analgesic use is associated with how painful a procedure is perceived to be. 29 In the current study, for procedures considered more painful, the nature and timing of analgesia differed to routine surgeries. A greater proportion of veterinarians prescribed opioids and NSAIDs throughout the surgery (pre-, intra- and postoperatively) in the conditions and surgeries ranked as more painful vs the routine procedures, where there was a more distinct use of opioids pre- and intraoperatively, and NSAIDs postoperatively. There was also a longer duration of postoperative analgesia provided for more painful surgeries or procedures, with NSAIDs predominantly prescribed during this period. Cat ovariohysterectomy (6.4) and castrations (4.6) were given mean pain rankings lower than the same procedures in dogs (6.7 and 5.5, respectively), a finding also documented by others. 8 This difference in ranking may be explained by a perception of reduced pain in cats due to less tissue disruption in these procedures, a perceived difference in pain thresholds between species or, differences – real or perceived – in owner acceptance of veterinary recommendations for postoperative pain relief. Regardless of the underlying reason, this difference may help to explain the reduced duration of postoperative analgesia provided to cats vs dogs following routine procedures.
Few respondents in the current study reported using validated pain scales, consistent with data reported elsewhere.8,30 Effective pain management can be optimised by detecting changes in behaviour with the use of validated and reliable pain-assessment tools, 18 especially those that define an intervention level, 31 and the use of these tools is strongly recommended by veterinary specialists. 18 The use of pain scales aid in the detection of subtle pain behaviour in patients and may influence the provision of analgesics, as seen in a UK survey, where more veterinarians using pain-assessment tools prescribed perioperative opioids and postoperative NSAIDs to cats. 8 However, this may not be a causal relationship, as veterinarians with a particular interest in pain management may be both more likely to use pain scales and more proactive in their provision of perioperative analgesia due to their special interest and level of education. The use of a pain scale does, however, promote the recognition of pain behaviours, which – when coupled with a predetermined intervention level – may result in alterations to analgesic plans, including the use of additional analgesics. It is recognised that having all staff trained in pain recognition and the use of formalised pain charting is important for managing pain in veterinary patients.2,18 This appears to be occurring in the UK, where 85% of respondents claimed that both veterinarians and nurses were responsible for perioperative pain assessment, 8 unlike the present survey where, overwhelmingly, the veterinarian was responsible (91%).
A potential limitation of the current study is the non-random, self-section method of enrolment used. It is accepted that such an approach may lead to bias. With the current survey, it is possible that this approach selected for veterinarians, for example, with a particular interest or expertise in pain management, or those who were more comfortable in doing an online survey. In the case of the former, such a bias may lead to the results of this study presenting a ‘best-case scenario’. Despite the non-random self-selection nature of enrolment, the demographics of respondents are broadly representative of the Australian veterinary workforce in terms of sex, type of practice and number of years since graduation. Similarly, the universities within Australia from which respondents graduated could also be considered representative, with more respondents trained at the larger and longer-standing universities of Sydney, Melbourne and Queensland. There were 12,769 registered veterinarians in Australia in 2018, of which 73% were reported to be in clinical practice, meaning 6.6% of practicing veterinarians in Australia participated in this survey. 32 It is therefore likely that these results provide an accurate picture of the current state of acute pain management in cats in Australia.
Conclusions
Appropriate pain management is essential in modern clinical practice to maximise patient health and welfare and enhance the veterinarian–owner–pet relationship. 18 This study highlights opportunities to further optimise pain management protocols for veterinary staff in Australia to manage acute and perioperative pain in cats through the use of validated pain scales, a more holistic clinic-based approach to pain assessment, including both veterinarians and nurses, and an increased duration of postoperative analgesia.
Supplemental Material
Pain survey
Tabulated full data on analgesia protocols
Acknowledgments
The authors would like to thank the International Society for Feline Medicine, the Centre for Veterinary Education (CVE) and Boehringer Ingelheim Animal Health Australia Territory Managers for their support in promoting the survey to veterinarians in Australia. We thank Associate Professor Navneet Dhand for his advice and assistance in reviewing the data. The greatest debt of thanks goes to the more than 600 veterinarians who took the time to share their thoughts on pain management by completing the survey.
Footnotes
Supplementary material: The following files are available online:
Pain survey.
Tabulated full data on analgesia protocols.
All the authors are current or former employees of Boehringer Ingelheim Animal Health Australia.
Funding: Funding for this study was provided by Boehringer Ingelheim Animal Health Australia.
Ethical approval: This work did not involve the use of animals and therefore ethical approval was not specifically required for publication in JFMS.
Informed consent: This work did not involve the use of animals and therefore informed consent was not required. No animals or humans are identifiable within this publication, and therefore additional informed consent for publication was not required.
ORCID iD: Louise Rae  https://orcid.org/0000-0003-3370-4891
https://orcid.org/0000-0003-3370-4891
Phillip McDonagh  https://orcid.org/0000-0001-7722-5281
https://orcid.org/0000-0001-7722-5281
This paper was handled and processed by the European Editorial Office (ISFM) for publication in JFMS
Accepted: 6 August 2021
References
- 1. Holte K, Kehlet H. Effect of postoperative epidural analgesia on surgical outcome. Minerva Anestesiol 2002; 68: 157–164. [PubMed] [Google Scholar]
- 2. Mathews K, Kronen PW, Lascelles D, et al. Guidelines for recognition, assessment and treatment of pain. J Small Anim Pract 2014; 55: E10–E68. [DOI] [PubMed] [Google Scholar]
- 3. Berry S. Analgesia in the perioperative period. Vet Clin Small Anim 2015; 45: 1013–1027. [DOI] [PubMed] [Google Scholar]
- 4. Beswick A, Dewey C, Johnson R, et al. An interesting survey of Ontario veterinarians’ knowledge and attitudes on pain in dogs and cats in 2012. Can Vet J 2016; 57: 1274–1280. [PMC free article] [PubMed] [Google Scholar]
- 5. Watson A, Nicholson A, Church DB, et al. Use of anti-inflammatory and analgesic drugs in dogs and cats. Aust Vet J 1996; 74: 203–210. [DOI] [PubMed] [Google Scholar]
- 6. Weber GH, Morton JM, Keates H. Postoperative pain and perioperative analgesic administration in dogs: practices, attitudes and beliefs of Queensland veterinarians. Aust Vet J 2012; 90: 186–193. [DOI] [PubMed] [Google Scholar]
- 7. Farnworth M, Adams N, Keown A, et al. Veterinary provision of analgesia for domestic cats (Felis catus) undergoing gonadectomy: a comparison of samples from New Zealand, Australia and the United Kingdom. N Z Vet J 2014; 62: 117–122. [DOI] [PubMed] [Google Scholar]
- 8. Hunt JR, Knowles TG, Lascelles BD, et al. Prescription of perioperative analgesics by UK small animal veterinary surgeons in 2013. Vet Rec 2015; 176: 493. [DOI] [PubMed] [Google Scholar]
- 9. Reid J, Scott EM, Calvo G, et al. Definitive Glasgow acute pain scale for cats: validation and intervention level. Vet Rec 2017; 180: 449. DOI: 10.1136/vr.104208. [DOI] [PubMed] [Google Scholar]
- 10. Reid J, Nolan A, Hughes J, et al. Development of the short-form Glasgow Composite Measure Pain Scale (CMPS-SF) and derivation of an analgesic intervention score. Anim Welf 2007; 16: 97–104. [Google Scholar]
- 11. Shipley H, Guedes A, Graham L, et al. Preliminary appraisal of the reliability and validity of the Colorado State University Feline Acute Pain Scale. J Feline Med Surg 2019; 21: 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dohoo SE, Dohoo IR. Factors influencing the postoperative use of analgesics in dogs and cats by Canadian veterinarians. Can Vet J 1996; 37: 552–556. [PMC free article] [PubMed] [Google Scholar]
- 13. Lascelles BDX, Capner CA, Waterman-Pearson AE. Current British veterinary attitudes to perioperative analgesia for cats and small mammals. Vet Rec 1999; 145: 601–604. [DOI] [PubMed] [Google Scholar]
- 14. Joubert KE. The use of analgesic drugs by South African veterinarians: continuing education. J S Afr Vet Assoc 2001; 72: 57–60. [DOI] [PubMed] [Google Scholar]
- 15. Lascelles BDX, Capner CA, Waterman-Pearson AE. Current British veterinary attitudes to perioperative analgesia for cats and small mammals. Vet Rec 1999; 145: 601. DOI: 10.1136/vr.145.4.95. [DOI] [PubMed] [Google Scholar]
- 16. Lorena SE, Luna SP, Lascelles BDX, et al. Current attitudes regarding the use of perioperative analgesics in dogs and cats by Brazilian veterinarians. Vet Anaesth Analg 2014; 41: 82–89. [DOI] [PubMed] [Google Scholar]
- 17. Reimann J, Dewey C, Bateman SW, et al. Perioperative analgesic use by Ontario veterinarians, 2012. Can Vet J 2017; 58: 149–156. [PMC free article] [PubMed] [Google Scholar]
- 18. Epstein ME, Rodanm I, Griffenhagen G, et al. 2015 AAHA/AAFP pain management guidelines for dogs and cats. J Feline Med Surg 2015; 17: 251–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lascelles B, Cripps P, Jones A, et al. Efficacy and kinetics of carprofen, administered preoperatively or postoperatively, for the prevention of pain in dogs undergoing ovariohysterectomy. Vet Surg 1998; 27: 568–582. [DOI] [PubMed] [Google Scholar]
- 20. Katz J, Clarke H, Seltzer Z. Preventive analgesia. Anesth Analg 2011; 113: 1242–1253. [DOI] [PubMed] [Google Scholar]
- 21. Clark L. Pre-emptive or preventive analgesia – lessons from the human literature? Vet Anaesth Analg 2014; 41: 109–112. [DOI] [PubMed] [Google Scholar]
- 22. Gates MC, Littlewood KE, Kongara K, et al. Cross-sectional survey of anaesthesia and analgesia protocols used to perform routine canine and feline ovariohysterectomies. Vet Anaesth Analg 2020; 47: 38–46. [DOI] [PubMed] [Google Scholar]
- 23. Raekallio M, Heinonen KM, Kuussaari J, et al. Pain alleviation in animals: attitudes and practices of Finnish veterinarians. Vet J 2003; 165: 131–135. [DOI] [PubMed] [Google Scholar]
- 24. Huxley JN, Whay HR. Current attitudes of cattle practitioners to pain and the use of analgesics in cattle. Vet Rec 2006; 159: 662. DOI: 10.1136/vr.159.20.662. [DOI] [PubMed] [Google Scholar]
- 25. Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 2013; 111: 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Green AD, Tripp DA, Sullivan MJL, et al. The relationship between empathy and estimates of observed pain. Pain Med 2009; 10: 381–392. [DOI] [PubMed] [Google Scholar]
- 27. Colombo ES, Crippa F, Calderari T, et al. Empathy toward animals and people: The role of gender and length of service in a sample of Italian veterinarians. J Vet Behav Clin Appl Res 2017; 17: 32–37. [Google Scholar]
- 28. Gruen ME, White P, Hare B. Do dog breeds differ in pain sensitivity? Veterinarians and the public believe they do. PLoS One 2020; 15: e0230315. DOI: 10.1371/journal.pone.0230315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hewson CJ, Dohoo IR, Lemke KA. Factors affecting the use of postincisional analgesics in dogs and cats by Canadian veterinarians in 2001. Can Vet J 2006; 47: 453–459. [PMC free article] [PubMed] [Google Scholar]
- 30. Catanzaro A, Salvo AD, Steagall PV, et al. Preliminary study on attitudes, opinions and knowledge of Italian veterinarians with regard to abdominal visceral pain in dogs. Vet Anaesth Analg 2016; 43: 361–370. [DOI] [PubMed] [Google Scholar]
- 31. Reid J, Nolan AM, Scott EM. Measuring pain in dogs and cats using structured behavioural observation. Vet J 2018; 236: 72–79. [DOI] [PubMed] [Google Scholar]
- 32. Australian Veterinary Association. Australian veterinary workforce survey 2018. www.ava.com.au/policy-advocacy/advocacy/workforce/workforce-data/ (2019, accessed August 19, 2021). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pain survey
Tabulated full data on analgesia protocols