Abstract
Background: Suicide is a significant public health problem and one of the leading causes of death worldwide. The effect of religion on suicidal behaviors (i.e., ideation, plan, attempt, and death) is an important issue worthy of consideration.
Methods: Major electronic databases, including MEDLINE, Web of Science, and Scopus, were searched for the articles published until 26 April 2021. Reference lists were also screened. Observational studies addressing the associations between religion and suicidal behaviors were also examined. Between-study heterogeneity was investigated using the χ2, τ2, and I2 statistics. The probability of publication bias was explored using the Begg and Egger tests, as well as trim-and-fill analysis. The effect size was expressed as odds ratio (OR) with 95% confidence intervals (CIs) using a random-effects model.
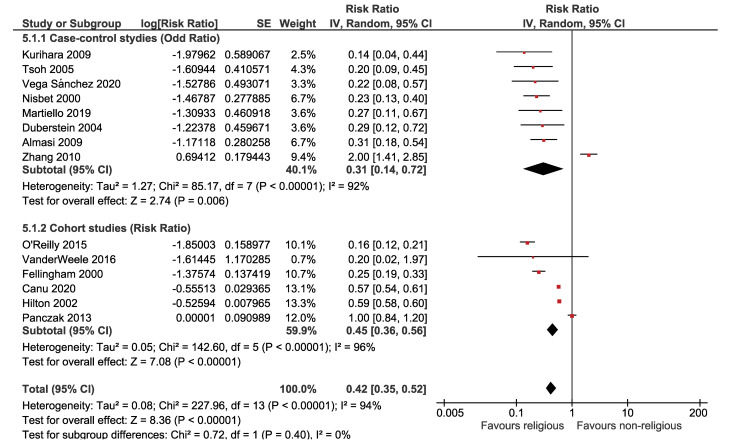
Results: Out of 11389 identified studies, 63 articles were eligible, involving 8,053,697 participants. There was an inverse association between religion and suicidal ideation OR = 0.83 (95% CI: 0.78, 0.88; P<0.001), suicidal plan OR = 0.93 (95% CI: 0.83, 1.04; P = 0.200), suicide attempt OR = 0.84 (95% CI: 0.79, 0.89; P<0.001), and completed suicide OR = 0.31 (95% CI: 0.14, 0.72; P = 0.006). There was a no evidence of publication bias.
Conclusions: The results of this meta-analysis support the notion that religion can play a protective role against suicidal behaviors. Nonetheless, the effect of religion on suicidal behaviors varies across countries with different religions and cultures. Although this association does not necessarily imply causation, an awareness of the relationship between religion and suicide risk can be of great help in suicide prevention policies and programs.
Keywords: Suicide plan, Suicidal ideation, Attempted suicide, Completed suicide, Meta-analysis, Religion, Spirituality
Background
Suicide is one of the top 20 leading causes of death and premature mortality in people of all ages across the globe,1,2 the third major cause of death among people aged 15-44 years, and the second leading cause of death in 10-24 year-olds.3 The individuals who die due to suicide outnumber those who die in war. In fact, for every death caused by conflict, five deaths are caused by suicide.4 Based on the World Health Organization (WHO), around one million people die from suicide every year, resulting in a global mortality rate of 16 per 100 000, or one death every 40 seconds.3 These figures understate the problem since they do not include attempted suicides, which are up to 20 times more common than suicide deaths;3 moreover, many people who have suicidal thoughts never seek services.5
Evidence suggests that there is no known single cause for suicide, rather it is a complicated event influenced by a variety of psychological, social, biological, cultural, and environmental factors.3,6,7 Epidemiological research has demonstrated that several behavioral factors, such as alcohol consumption,8 drug abuse,9 and smoking,10 have a role to play in suicide. Another factor that plays a pivotal role in one’s lifestyle, general health, and wellbeing is religion.11 Based on the Gallup surveys conducted in 114 countries in 2009, religion plays an essential role in the lives of numerous people around the world. About 84% of adults reported that religion was an essential part of their daily lives. In 10 nations and territories, at least 98% of people claimed that religion was significant in their daily lives.12 Another poll conducted by Gallup International in 2012 involving 50 000 people selected from 57 countries across the world in five continents revealed that 59%, 23%, and 13% of participants considered themselves to be religious, non-religious, and convinced atheists, respectively.13
The relationship between religion and suicidal behaviors was examined by a few review studies.14,15 So far, the only meta-analysis that assessed the relationship between religion and suicide is the study conducted by Wu et al in 2015.16 They only investigated the association between religion and suicide death. Nonetheless, the relationship between religion and other aspects of suicidal behaviors has not been fully assessed. Furthermore, several epidemiological studies addressing the relationship between religion and suicide have been performed and published on the relationship between religion and suicide since then. In light of the aforementioned issues, this meta-analysis aimed to update the results of the previous one with current evidence and assess the relationship between religion and all aspects of suicidal behaviors, such as suicidal ideations, suicide plans, suicide attempts, and suicide deaths.
Methods
The Vice-chancellor of Research and Technology, Hamadan University of Medical Sciences, approved and funded this systematic review. We prepared this report based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement.17
Eligibility criteria
The exposure of interest was religious beliefs and/or practices, for example, people who manifest devotion to a deity, believe in God or gods, and follow the practices of a religion. We considered people religious regardless of what religion (Islam, Christianity, Judaism, Buddha, Hindu, Shinto, etc.) they believed in and how frequently they attended religious services. The believers were compared with nonbelievers or atheism, and the outcome of interest was suicide. Suicidal behaviors were categorized as suicidal ideation (seriously thinking about committing suicide during the past 12 months or lifetime), suicidal plan (making a plan to commit suicide during the past 12 months or lifetime), suicide attempt (actually attempting suicide during the past 12 months or lifetime), and completed suicide (suicide death).18 We excluded those studies addressing religiously motivated terrorism and suicidal operations.
Observational studies (cohort, case-control, and cross-sectional studies) addressing the relationship between religion and suicidal behaviors were included regardless of language, publishing date, nationality, race, age, and gender. The studies that compared suicide rates between different religions or did not discriminate among different types of suicidal behaviors were excluded. The studies investigating the suicidal terrorist attacks were also ruled out.
Information sources and search
Major electronic databases, including MEDLINE, Web of Science, and Scopus were searched for articles until 26 April 2021 using the keywords: (suicide or suicidal or suicidality) and (religion or religious or religiosity or spirituality or spiritual). The reference lists of the included papers were screened to identify more eligible studies.
Study selection
The search results were combined using EndNote reference manager software, and duplicate papers of the same study were removed. The titles and abstracts of the papers were screened and ineligible studies were excluded by two authors (JP and FG) independently. Disagreements were resolved by discussion. The full text of the potentially eligible papers was retrieved and examined for further evaluation.
Data extraction
The necessary extracted data from relevant studies were imported into an electronic datasheet prepared by Stata software. The following information was extracted: first author’s name, year of publication, country, study population (general population, patients with mood disorders, students, workers, veterans, as well as lesbian, gay, bisexual, and transgender (LGBQ) people), age mean/range, gender, study design (cohort, case-control, cross-sectional), suicidal behaviors (ideation, plan, attempt, death), effect estimate (risk ratio, odds ratio), sample size, effect size and its related 95% confidence intervals (CIs).
Methodological quality
The Newcastle Ottawa Scale (NOS) was used for assessing the quality of the included studies.19 Based on this tool, each study is judged on three domains: (a) the selection of the study groups, (b) the comparability of the groups, (c) and the ascertainment of the exposure/outcome of interest. Each item of high quality is given a star. Up to nine stars were assigned to the highest-quality studies. Studies with six or fewer stars were deemed low-quality, while those with seven or more stars were regarded as high-quality.
Heterogeneity and reporting biases
Heterogeneity across studies was examined by χ2 test,20 and its quantity was measured by the I2 statistic.21 Meta-regression analysis was performed to explore the sources of heterogeneity. The following variables were considered potential sources of heterogeneity: six WHO regions (Region of the Americas, European Region, Eastern Mediterranean Region, South-East Asian Region, Western Pacific Region, African Region), type of population (general population, people with mental/mood disorders, veterans, students, workers, people with comorbidities, drug disorders, LGBQ people), gender (female, male), study design (cohort, case-control, cross-sectional), suicide time (last month, last year), type of belief (just religious beliefs, religious observance), adjustment (adjusted, unadjusted), and quality of the studies (high, low). The possibility of publication bias was explored using Egger’s test,22 Begg’s test,23 and the trim-and-fill method.24
Summary measures
The relationship between religion and suicidal behaviors was measured using risk ratio (RR) and odds ratio (OR) with their 95% CIs. Wherever reported, we used full adjusted forms of RR and OR controlled for at least one or more potential confounding factors. The data were analyzed at a significance level of 0.05 using the random-effects model.25 The Stata software (version 16) and RevMan (version 5.4.1) were used for data analysis.
Sensitivity analysis
When between-study heterogeneity was moderate to high (I2 ≥ 50%), the sensitivity analysis was performed using the MetaPlot Stata command based on the sequential algorithm.26-28
Results
Description of studies
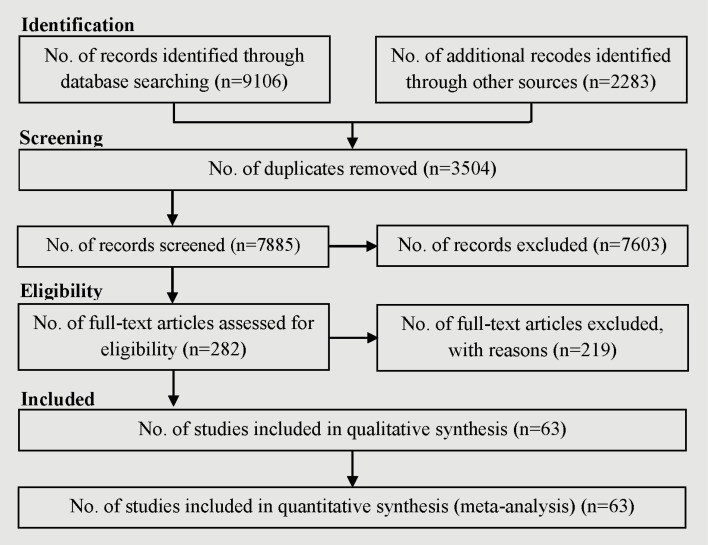
A total of 11 389 references, including 9106 articles, were identified through searching the electronic databases until 26 April 2021, and 2283 articles through screening the reference list of included studies. After the removal of 3504 duplicates, 7603 references were excluded after screening their titles and abstracts. Out of 282 references considered potentially eligible after screening, 219 were excluded since they lacked one or more Population, Intervention, Comparison, Outcomes and Study (PICOS) criteria. Some papers did not separate suicidal ideation from attempted suicide cases, some reported self-harm rather than suicide, some did not report the association numerically, and some others were review articles rather than original articles. Finally, 63 references29-91 remained for meta-analysis (Figure 1) involving 8 053 697 participants. Based on the NOS, the quality of 49 studies was high and the quality of 14 studies was low (Table 1).
Figure 1.
Flow of information through the different phases of the systematic review.
Table 1. Characteristics of the included studies .
| 1 st Author year | Country | Study population | Age | Sex | Study design | Religion | Sample | NOS-stars | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Abdu 2020 | Ethiopia | Students | 21.00 | Both | Cross-sectional | All religions | 523 | ********* | High |
| Akbari 2015 | Iran | General population | 25.86 | Both | Case-control | All religions | 600 | ********* | High |
| Almasi 2009 | Hungary | General population | 33-64 | Both | Case-control | All religions | 388 | ********* | High |
| Almeida 2012 | Australia | General population | 60-101 | Both | Cross-sectional | All religions | 21 290 | ******* | High |
| Blackmore 2008 | USA | General population | 32.00 | Both | Cross-sectional | All religions | 36 984 | ******* | High |
| Blosnich 2020 | USA | LGBQ people | 18.29 | Both | Cross-sectional | All religions | 40 150 | ********* | High |
| Brito 2021 | France | General population | 18-60 | Both | Cross-sectional | All religions | 38 694 | ********* | High |
| Burlaka 2020 | Ukrain | Students | 19.19 | Both | Cross-sectional | Christianity | 1005 | ********* | High |
| Burshtein 2016 | Israel | General population | 18-34 | Both | Cross-sectional | Judaism | 4914 | ********* | High |
| Canu 2020 | Switzerland | Workers | 18-65 | Male | Cohort | All religions | 1 534 564 | ********* | High |
| Caribé 2012 | Brazil | General population | 33.49 | Male | Case-control | All religions | 224 | ********* | High |
| Caribé 2015 | Brazil | Mental disorders | 42.95 | Both | Cross-sectional | All religions | 164 | ******** | High |
| Chatters 2011 | USA | General | 18 + | Both | Cross-sectional | All religions | 6082 | ******* | High |
| Currier 2017 | USA | Veteran | 28.60 | Both | Cross-sectional | All religions | 125 | ****** | Low |
| de Sá SousaI 2020 | Brazil | Student | 16.40 | Both | Cross-sectional | All religions | 674 | ********* | High |
| Dervic 2004 | USA | Mental disorders | 36.80 | Both | Cross-sectional | All religions | 371 | ***** | Low |
| Duberstein 2004 | USA | General population | 68.30 | Both | Case-control | All religions | 172 | ********* | High |
| Fellingham 2000 | USA | General population | 15-34 | Male | Cohort | Christianity | 1 100 620 | ******** | High |
| Garroutte 2003 | USA | General population | 33.70 | Both | Cross-sectional | Christianity | 1456 | ******** | High |
| Hilton 2002 | USA | General population | 15-34 | Male | Cohort | Christianity | 15 555 | ****** | Low |
| Hoffman 2014 | USA | Students | 16.04 | Both | Cross-sectional | All religions | 700 | ********* | High |
| Huang 2020 | China | Drug abusers | 39.22 | Both | Cross-sectional | Buddhist | 486 | ******* | High |
| Jacob 2019 | Spain | General | 46.30 | Both | Cross-sectional | All religions | 7403 | ********* | High |
| Joel Wong 2011 | USA | Students | 23.11 | Both | Cross-sectional | All religions | 1377 | ******* | High |
| Kim 2019 | Korea | General population | 35-49 | Female | Cross-sectional | All religions | 2649 | ****** | Low |
| Kovess-Masfety 2011 | Europe | General population | No data | Both | Cross-sectional | All religions | 21 425 | ********* | High |
| Kurihara 2009 | Indonesia | General population | 41.40 | Both | Case-control | Hindu | 180 | ******** | High |
| Lawrence 2016 | USA | Mental disorders | No data | Both | Cross-sectional | All religions | 321 | ******* | High |
| Lee 2017 | Korea | General | 60-90 | Both | Cross-sectional | All religions | 93 151 | ********* | High |
| Lester 2012 | USA | General population | 23.00 | Both | Cross-sectional | All religions | 149 | **** | Low |
| Lytle 2018 | USA | LGBQ people | 22.50 | Both | Cross-sectional | All religions | 20 702 | ********* | High |
| Martiello 2019 | Italy | General population | 25 + | Both | Case-control | All religions | 484 | ****** | Low |
| Mirzaie 2013 | Iran | Students | 21.16 | Both | Cross-sectional | All religions | 452 | ****** | Low |
| Nisbet 2000 | USA | General population | 50 + | Both | Case-control | All religions | 4863 | ****** | Low |
| Nkansah-Amankra 2012 | USA | General | 26-34 | Both | Cohort | All religions | 9412 | ********* | High |
| Nonnemaker 2003 | USA | Students | 6-18 | Both | Cross-sectional | All religions | 18 924 | ******* | High |
| O'Reilly 2015 | UK | General population | 16-74 | Both | Cohort | All religions | 1 106 104 | ********* | High |
| Panczak 2013 | Switzerland | General population | 35-94 | Both | Cohort | Christianity | 3 688 617 | ******* | High |
| Peltzer 2017 | Asia | Students | 18-30 | Both | Cohort | All religions | 4675 | ******* | High |
| Rasic 2009 | Canada | General population | 15 + | Both | Cohort | All religions | 36 984 | ******* | High |
| Rasic 2011 | USA | General population | 30 + | Both | Cohort | All religions | 1091 | ********* | High |
| Rew 2001 | USA | General population | 10-19 | Both | Cohort | All religions | 10 059 | ****** | Low |
| Robins 2009 | USA | Students | 18-21 | Both | Cross-sectional | All religions | 454 | ******** | High |
| Rushing 2013 | USA | Mental disorders | 59 + | Both | Cross-sectional | All religions | 248 | ******* | High |
| Sidhartha 2006 | India | General population | 12-19 | Both | Cross-sectional | Hindu | 1205 | ****** | Low |
| Sisask 2010 | Cross-National | General population | No data | Both | Case-control | All religions | 8303 | ********* | High |
| Snarr 2010 | USA | Veterans | No data | Both | Cross-sectional | All religions | 52 780 | ********* | High |
| Stolz 2016 | Multinational | General population | No data | Both | Cross-sectional | All religions | 6791 | ********* | High |
| Stroppa 2013 | Brazil | Mental disorders | 46.20 | Both | Cross-sectional | All religions | 168 | ***** | Low |
| Sun 2018 | China | General population | 15-54 | Both | Case-control | All religions | 1582 | ******* | High |
| Taylor 2011 | USA | General population | 18 + | Both | Cross-sectional | All religions | 6082 | ******* | High |
| Thanh 2006 | Vietnam | General population | 14 + | Both | Cross-sectional | All religions | 2280 | ********* | High |
| Toussaint 2015 | USA | General population | No data | Both | Cross-sectional | All religions | 4448 | ******* | High |
| Trevino 2014 | USA | Chronic diseases | 20 + | Both | Cross-sectional | All religions | 603 | ********* | High |
| Tsoh 2005 | China | General population | 65 + | Both | Case-control | All religions | 224 | ******* | High |
| Umamaheswari 2014 | India | Mental disorders | No data | Both | Case-control | Hindu | 130 | **** | Low |
| Ursano 2015 | USA | Veterans | 18 + | Both | Cross-sectional | All religions | 38 507 | ********* | High |
| VanderWeele 2016 | USA | General population | 30-55 | Both | Cohort | All religions | 89 708 | ********* | High |
| Vega Sánchez 2020 | Spain | General population | No data | Both | Case-control | All religions | 273 | ****** | Low |
| Wang 2015 | China | General population | 18 + | Both | Cross-sectional | All religions | 2769 | ******** | High |
| Yen 2005 | Taiwan | General population | 65-74 | Both | Cross-sectional | All religions | 897 | ******* | High |
| Zhang 2010 | China | General population | 15-34 | Both | Case-control | All religions | 808 | ****** | Low |
LGBQ acronym stands for lesbian, gay, bisexual, and queer/questioning.
The studies that addressed the association between religion and various types of suicidal behaviors were as follows: suicidal ideations (37 studies), suicide plan (3 studies), suicide attempt (32 studies), and suicide death (14 studies). The number of studies presented in the forest plots may be more than the total number of included studies since some studies reported the association between religion and different types of suicidal behaviors simultaneously. Due to substantial heterogeneity across the included studies, a meta-regression was performed considering several variables, including WHO regions, type of population, gender, study design, suicide time, type of belief, adjustment, and quality of the studies; nonetheless, neither was statistically significant.
Association between religion and suicide
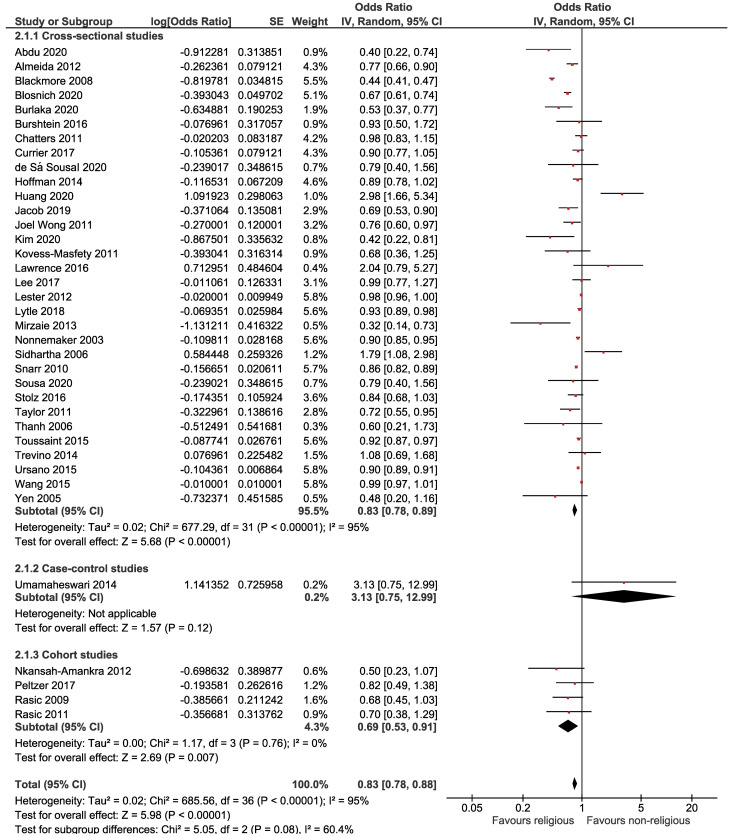
The association between religion and suicidal ideation is presented in Figure 2, pointing to a significant inverse association between religion and suicidal ideation. Based on this forest plot, the estimated OR of suicidal ideation for believers versus nonbelievers was 0.83 (95% CI: 0.78, 0.88). The overall effect measure demonstrated that religion significantly decreases the risk of suicidal ideation by 17% (P < 0.001). Between-study heterogeneity was high (I2 = 95%). The overall effect became slightly weaker (OR = 0.88; 95% CI, 0.84, 0.91; I2 = 47%) after performing a sensitivity analysis (Table 2). There was no evidence of publication bias based on the Begg test (P = 0.505) and Egger test (P = 0.130).
Figure 2.
Forest plot of the association between religion and suicidal ideation.
Table 2. Results of sensitivity analysis .
| Variables | Before the sensitivity analysis | After the sensitivity analysis | ||||||
| Studies | χ 2 | I 2 | OR (95% CI) | Studies | χ 2 | I 2 | OR (95% CI) | |
| Suicidal ideation | 37 | 0.001 | 95% | 0.83 (0.78, 0.88) | 30 | 0.002 | 47% | 0.88 (0.84, 0.91) |
| Suicidal plan | 3 | 0.002 | 84% | 0.93 (0.83, 1.04) | 2 | 0.531 | 0% | 0.89 (0.83, 0.94) |
| Suicide attempt | 31 | 0.001 | 86% | 0.84 (0.79, 0.89) | 24 | 0.009 | 45% | 0.91 (0.88, 0.95) |
| Completed suicide | 8 | 0.001 | 92% | 0.31 (0.14, 0.72) | 7 | 0.900 | 0% | 0.25 (0.19, 0.33) |
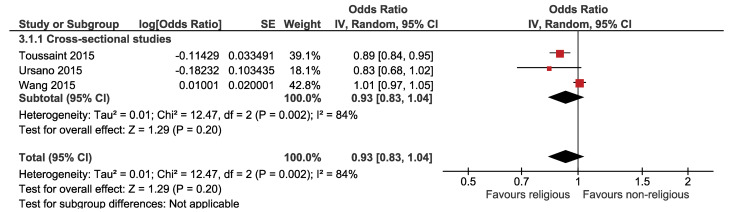
The association between religion and suicide plan is displayed in Figure 3, which illustrates that the association between religion and the suicidal plan was not statistically significant. Based on this forest plot, the estimated OR of the suicidal plan for believers versus nonbelievers was 0.93 (95% CI: 0.83, 1.04). The overall effect measure indicated that religion decreases the risk of the suicide plan by 7% (P = 0.200). Between-study heterogeneity was high (I2 = 84%). The overall effect became stronger and significant (OR, 0.89; 95% CI, 0.83, 0.94; I2 = 0%) after performing a sensitivity analysis (Table 2). There was no evidence of publication bias based on the Begg test (P = 0.602) and Egger test (P = 0.445).
Figure 3.
Forest plot of the association between religion and suicide plan.
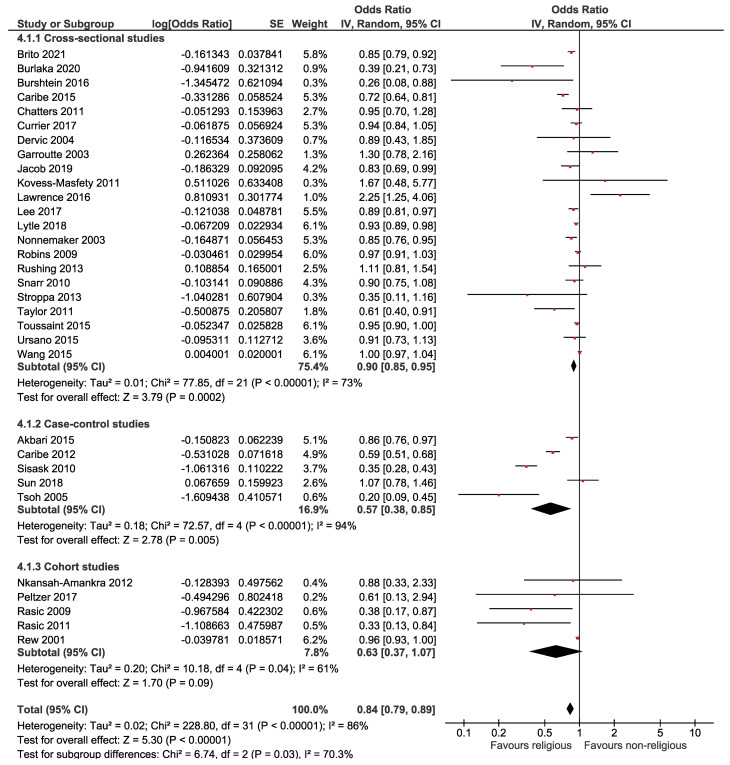
The relationship between religion and suicide attempts is displayed in Figure 4, revealing a significant inverse association between religion and suicide attempts. Based on this forest plot, the estimated OR of suicide attempts for believers versus nonbelievers was 0.84 (95% CI: 0.79, 0.89). The overall effect measure shows that religion decreases the risk of the suicidal plan by 16% (P < 0.001). Between-study heterogeneity was high (I2 = 86%). The overall effect became weaker (OR = 0.91; 95% CI, 0.88, 0.95; I2 = 45%) after performing a sensitivity analysis (Table 2). The Begg test revealed no evidence of publication bias (P = 0.347); however, the Egger test did show evidence of publication bias (P = 0.007). However, the trim-and-fill analysis estimated no missing studies.
Figure 4.
Forest plot of the association between religion and suicide attempt.
The association between religion and suicide death is presented in Figure 5, which shows a significant inverse association between religion and suicide death. According to the forest plot, the estimated OR of suicide attempts for believers versus nonbelievers was 0.31 (95% CI: 0.14, 0.72). The overall effect measure demonstrates that religion decreases the risk of suicide death by 69% (P < 0.001). Between-study heterogeneity was high (I2 = 92%). The overall effect became stronger (OR, 0.25; 95% CI, 0.19, 0.33; I2 = 0%) after performing a sensitivity analysis (Table 2). There was no evidence of publication bias based on the Begg test (P = 0.928) and Egger test (P = 0.177).
Figure 5.
Forest plot of the association between religion and suicide death.
Discussion
The results of this meta-analysis pointed to the overall mild-to-moderate protective relationship of religiosity with suicidal ideation, suicide plans, and suicide attempt, as well as a strong protective relationship between religiosity and suicide death. Nevertheless, the observed association between religion and suicidal behaviors does not necessarily imply a direct cause-and-effect relationship. Suicide is a highly complex issue that is associated with a range of risk and protective factors at both individual and contextual levels.3,6,7 Religion is a multi-factorial phenomenon; therefore, we cannot regard risk and protective factors as individual items, rather they should be deemed as a cluster. Diseases are promoted by risk factors while being prevented by protective factors. In this regard, diseases will not develop if risk and protective factors are in balance or if protective factors dominate risk factors.92 Therefore, the role of religion in the prevention of suicide should be considered, along with other influential factors.
A vast majority of literature observes a protective effect of religion on suicidal behaviors rather than supports. Several mechanisms have been proposed to explain the protective role of religiosity against suicide. Most religions have strict prohibitions against suicide; therefore, those who are more committed to such religions are less likely to commit suicide. Furthermore, it has been proposed that all major religions discourage all forms of violence, including suicide, and advocate peace and unity which may be deemed life-affirming values, thereby preventing suicide.15,93 In addition to sanctioning suicide, participation in organized religions allows members of the congregation and clergies to form an extended support network, which has been demonstrated to be a protective factor against suicidal behaviors.94 Religious belief has also been linked to lower levels of violence and hostility which have constantly been shown to be associated with suicidal behaviors.95 Furthermore, many religions forbid illegal activities, including substance misuse, alcohol consumption, and smoking which have been associated with suicide.8-10 Therefore, the restriction of high-risk behaviors may have an indirect protective impact against suicide.
There was considerable heterogeneity across the included studies (small P value of χ2 and large I2 statistic). The results of the statistical tests used to examine heterogeneity should be interpreted cautiously. The χ2test has low statistical power when the sample size is small or the number of studies is limited. The test, on the other hand, has high power in detecting a modest level of heterogeneity when the sample size or number of the included studies is large.20 Consequently, a portion of the observed heterogeneity can be attributed to the large sample size (involving 8 053 697 participants) and the great number of studies included in the meta-analysis. Nevertheless, inconsistencies across studies can account for a portion of the observed heterogeneity. The observed heterogeneity can be justified on the ground that the results of individual studies come from varied settings with different religions, as well as varying degrees of religious fidelity and adherence to religious teachings. This diversity may be a source of the observed heterogeneity.
Wu et al16 conducted a meta-analysis in 2015 to examine the association between religion and completed suicide. They found nine studies that altogether included 2339 suicide cases and 5252 participants. They reported an overall protective effect of religiosity from completed suicide (OR = 0.38; 95% CI: 0.21, 0.71) and concluded that religion may play a protective role against suicide in a majority of settings. The results of the referred research were consistent with the findings of the present study. The overall measure produced from OR, estimating the probability of completed suicide, was larger than that obtained from RR, as depicted in Figure 4. The rationale for this is straightforward since OR tends to overstate the degree of the relationship.96
This meta-analysis is associated with a few limitations and considerations that should be taken into account when interpreting the results. Firstly, the studies included in this meta-analysis, except in a few cases, did not set out to assess the effect of different types of religions, denominations, intensity, and spirituality on suicidal behaviors. Therefore, religion was treated as a binary entity and neither captured this dimensionality nor measured the effect of different aspects of religion on suicidal behaviors. Secondly, the number of studies addressing the association between religion and “suicide plans” was relatively small. This issue reduced the strength of association and the generalizability of the results considering the relationship between religion and suicide plans. Thirdly, we imported the adjusted forms of RR and OR into the meta-analysis wherever feasible. Nevertheless, the confounding effect could not be entirely ruled out since some studies provided crude forms of RR or OR estimates. This problem might lead to an overestimation of the overall effect size of religion. Fourthly, there were eight studies (mainly old studies) that appeared to be eligible for this meta-analysis; nonetheless, their full texts were not available and their corresponding authors did not respond. This issue might raise the possibility of selection bias. Finally, we did not evaluate the religiously motivated suicidal operations and terrorism which is a matter of a completely different nature and has not been the subject of this research. Despite the aforementioned limitations, we developed a wide search strategy to include as many studies as possible, including 56 studies involving 8 053 697 participants. The current meta-analysis was able to examine the association between religiosity and the overall suicide burden.
Conclusion
This meta-analysis addressed the association between religiosity and suicide. The results of this study support the notion that religion can play a protective role against suicidal behaviors. Based on current evidence, religious affiliation and participation significantly decreased the risk of suicidal ideation, suicide plans, suicide attempt, and completed suicide. Although this association does not necessarily imply causation, an awareness of the relationship between religion and suicide risk can be of great help in suicide prevention policies and procedures.
Acknowledgments
We would like to appreciate the Vice-Chancellor for Research and Technology of the Hamadan University of Medical Sciences for approval of this study.
Authors’ contribution
Jalal Poorolajal contributed to the study conception and design, analysis and interpretation of data, and drafting of the manuscript. Mahmoud Goudarzi contributed to the study design and critical revision. Fatemeh Gohariensaf contributed to the acquisition of data and critical revision. Nahid Darvishi contributed to the study design, acquisition of data, and critical revision. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Availability of data and material
Not available.
Conflicts of interest
The authors declare that they have no conflict of interest.
Consent for publication
All authors agree with the publication of this manuscript in the current format.
Ethics approval
There was no human subject in this study.
Funding
The Vice-Chancellor of Research and Technology, Hamadan University of Medical Sciences funded this study (140006164895). However, the funder had no role in the study design, data collection, and analysis, decision to publish, or manuscript preparation.
Highlights
This meta-analysis revealed the extent to which religion can affect suicidal behaviors (i.e., ideation, plan, attempt, and death).
This meta-analysis pointed to the inverse association of religion with suicidal ideation, suicidal plan, suicide attempt, and suicide death.
Religion reduced the risk of suicidal ideation, suicidal plan, suicide attempt, and suicide death by 17%, 7%, 16%, and 69%, respectively.
The results of this meta-analysis can be of great help in designing suicide prevention policies and programs.
Please cite this article as follows: Poorolajal J, Goudarzi M, Gohari-Ensaf F, Darvishi N. Relationship of religion with suicidal ideation, suicide plan, suicide attempt, and suicide death: a meta-analysis. J Res Health Sci. 2022; 22(1):e00537. doi:10.34172/jrhs.2022.72
References
- 1. World Health Organization. Suicide prevention. WHO; 2013. Available from: http://www.who.int/mental_health/prevention/en/. Accessed August 19, 2013.
- 2.Poorolajal J, Esmailnasab N, Ahmadzadeh J, Azizi Motlagh T. The burden of premature mortality in Hamadan province in 2006 and 2010 using standard expected years of potential life lost: a population-based study. Epidemiol Health. 2012;34:e2012005. doi: 10.4178/epih/e2012005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. Suicide prevention (SUPRE). Geneva: WHO; 2013. Available from: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/. Accessed August 19, 2013.
- 4. World Health Organization. 10 facts on injuries and violence Beginning. Geneva: WHO; 2013. Available from: http://www.who.int/features/factfiles/injuries/facts/en/index1.html. Accessed August 20,2013.
- 5. Centers for Disease Control and Prevention. Understanding suicide: fact sheet. Atlanta: CDC; 2013. Available from: http://www.cdc.gov/violenceprevention/pub/suicide_factsheet.html. Accessed August 20,2013.
- 6.Amiri B, Pourreza A, Rahimi Foroushani A, Hosseini SM, Poorolajal J. Suicide and associated risk factors in Hamadan province, west of Iran, in 2008 and 2009. J Res Health Sci. 2012;12(2):88–92. [PubMed] [Google Scholar]
- 7.Poorolajal J, Rostami M, Mahjub H, Esmailnasab N. Completed suicide and associated risk factors: a six-year population based survey. Arch Iran Med. 2015;18(1):39–43. [PubMed] [Google Scholar]
- 8.Darvishi N, Farhadi M, Haghtalab T, Poorolajal J. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS One. 2015;10(5):e0126870. doi: 10.1371/journal.pone.0126870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poorolajal J, Haghtalab T, Farhadi M, Darvishi N. Substance use disorder and risk of suicidal ideation, suicide attempt and suicide death: a meta-analysis. J Public Health (Oxf) 2016;38(3):e282–e91. doi: 10.1093/pubmed/fdv148. [DOI] [PubMed] [Google Scholar]
- 10.Poorolajal J, Darvishi N. Smoking and suicide: a meta-analysis. PLoS One. 2016;11(7):e0156348. doi: 10.1371/journal.pone.0156348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morton KR, Lee JW, Martin LR. Pathways from religion to health: mediation by psychosocial and lifestyle mechanisms. Psycholog Relig Spiritual. 2017;9(1):106–17. doi: 10.1037/rel0000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Crabtree S. Religiosity Highest in World’s Poorest Nations. Gallup; 2010. Available from: https://news.gallup.com/poll/142727/religiosity-highest-world-poorest-nations.aspx. Updated August 31, 2010. Accessed July 15, 2021.
- 13. Gilani IS, Shahid R, Zuettel I. Global Index of Religiosity and Atheism. Zurich: WIN-Gallup International; 2012.
- 14.Lawrence RE, Oquendo MA, Stanley B. Religion and suicide risk: a systematic review. Arch Suicide Res. 2016;20(1):1–21. doi: 10.1080/13811118.2015.1004494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gearing RE, Alonzo D. Religion and suicide: new findings. J Relig Health. 2018;57(6):2478–99. doi: 10.1007/s10943-018-0629-8. [DOI] [PubMed] [Google Scholar]
- 16.Wu A, Wang JY, Jia CX. Religion and completed suicide: a meta-analysis. PLoS One. 2015;10(6):e0131715. doi: 10.1371/journal.pone.0131715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. Definitions: self-directed Violence. CDC; 2014. Available from: http://www.cdc.gov/violenceprevention/suicide/definitions.html. Updated December 13, 2013. Accessed September 8, 2014.
- 19. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ontario: Ottawa Hospital Research Institute; 2009. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed March 25, 2014.
- 20. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0. The Cochrane Collaboration; 2008. Available from: www.cochrane-handbook.org. Updated February 2008.
- 21.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 24.Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95(449):89–98. doi: 10.1080/01621459.2000.10473905. [DOI] [Google Scholar]
- 25.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 26.Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37(5):1148–57. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Poorolajal J, Mahmoodi M, Majdzadeh R, Fotouhi A. Metaplot: a novel Stata graph for assessing heterogeneity at a glance. Iran J Public Health. 2010;39(2):102–4. [PMC free article] [PubMed] [Google Scholar]
- 28.Poorolajal J, Noornejad S. Metaplot: a new Stata module for assessing heterogeneity in a meta-analysis. PLoS One. 2021;16(6):e0253341. doi: 10.1371/journal.pone.0253341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdu Z, Hajure M, Desalegn D. Suicidal behavior and associated factors among students in Mettu University, South West Ethiopia, 2019: an institutional based cross-sectional study. Psychol Res Behav Manag. 2020;13:233–43. doi: 10.2147/prbm.s240827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akbari M, Haghdoost AA, Nakhaee N, Bahramnejad A, Baneshi MR, Zolala F. Risk and protective factor for suicide attempt in Iran: a matched case-control study. Arch Iran Med. 2015;18(11):747–52. [PubMed] [Google Scholar]
- 31.Almasi K, Belso N, Kapur N, Webb R, Cooper J, Hadley S. et al. Risk factors for suicide in Hungary: a case-control study. BMC Psychiatry. 2009;9:45. doi: 10.1186/1471-244x-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Almeida OP, Draper B, Snowdon J, Lautenschlager NT, Pirkis J, Byrne G. et al. Factors associated with suicidal thoughts in a large community study of older adults. Br J Psychiatry. 2012;201(6):466–72. doi: 10.1192/bjp.bp.112.110130. [DOI] [PubMed] [Google Scholar]
- 33.Blackmore ER, Munce S, Weller I, Zagorski B, Stansfeld SA, Stewart DE. et al. Psychosocial and clinical correlates of suicidal acts: results from a national population survey. Br J Psychiatry. 2008;192(4):279–84. doi: 10.1192/bjp.bp.107.037382. [DOI] [PubMed] [Google Scholar]
- 34.Blosnich JR, De Luca S, Lytle MC, Brownson C. Questions of faith: religious affiliations and suicidal ideation among sexual minority young adults. Suicide Life Threat Behav. 2020;50(6):1158–66. doi: 10.1111/sltb.12679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brito MA, Amad A, Rolland B, Geoffroy PA, Peyre H, Roelandt JL. et al. Religiosity and prevalence of suicide, psychiatric disorders and psychotic symptoms in the French general population. Eur Arch Psychiatry Clin Neurosci. 2021;271(8):1547–57. doi: 10.1007/s00406-021-01233-3. [DOI] [PubMed] [Google Scholar]
- 36.Burlaka V, Hong JS, Serdiuk O, Krupelnytska L, Paschenko S, Darvishov N. et al. Suicidal behaviors among Ukrainian college students: the role of substance use, religion, and depression. Int J Ment Health Addict. 2021;19(6):2392–406. doi: 10.1007/s11469-020-00333-w. [DOI] [Google Scholar]
- 37.Burshtein S, Dohrenwend BP, Levav I, Werbeloff N, Davidson M, Weiser M. Religiosity as a protective factor against suicidal behaviour. Acta Psychiatr Scand. 2016;133(6):481–8. doi: 10.1111/acps.12555. [DOI] [PubMed] [Google Scholar]
- 38.Guseva Canu I, Bovio N, Wild P, Bopp M. Identification of socio-demographic, occupational, and societal factors for guiding suicide prevention: a cohort study of Swiss male workers (2000-2014) Suicide Life Threat Behav. 2021;51(3):540–53. doi: 10.1111/sltb.12746. [DOI] [PubMed] [Google Scholar]
- 39.Caribé AC, Nunez R, Montal D, Ribeiro L, Sarmento S, Quarantini LC. et al. Religiosity as a protective factor in suicidal behavior: a case-control study. J Nerv Ment Dis. 2012;200(10):863–7. doi: 10.1097/NMD.0b013e31826b6d05. [DOI] [PubMed] [Google Scholar]
- 40.Caribé AC, Studart P, Bezerra-Filho S, Brietzke E, Nunes Noto M, Vianna-Sulzbach M. et al. Is religiosity a protective factor against suicidal behavior in bipolar I outpatients? J Affect Disord. 2015;186:156–61. doi: 10.1016/j.jad.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 41.Chatters LM, Taylor RJ, Lincoln KD, Nguyen A, Joe S. Church-based social support and suicidality among African Americans and Black Caribbeans. Arch Suicide Res. 2011;15(4):337–53. doi: 10.1080/13811118.2011.615703. [DOI] [PubMed] [Google Scholar]
- 42.Currier JM, Smith PN, Kuhlman S. Assessing the unique role of religious coping in suicidal behavior among US Iraq and Afghanistan veterans. Psycholog Relig Spiritual. 2017;9(1):118–23. doi: 10.1037/rel0000055. [DOI] [Google Scholar]
- 43.de la Vega Sánchez D, Guija JA, Pérez-Moreno P, Kelly SA, Santos M, Oquendo MA. et al. Association of religious activity with male suicide deaths. Suicide Life Threat Behav. 2020;50(2):449–60. doi: 10.1111/sltb.12600. [DOI] [PubMed] [Google Scholar]
- 44.de Sá Sousa CM, Mascarenhas MDM, Gomes KRO, Rodrigues MTP, Miranda CES, de Macêdo Gonçalves Frota K. Suicidal ideation and associated factors among high school adolescents. Rev Saude Publica. 2020;54:33. doi: 10.11606/s1518-8787.2020054001637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dervic K, Oquendo MA, Grunebaum MF, Ellis S, Burke AK, Mann JJ. Religious affiliation and suicide attempt. Am J Psychiatry. 2004;161(12):2303–8. doi: 10.1176/appi.ajp.161.12.2303. [DOI] [PubMed] [Google Scholar]
- 46.Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34(7):1331–7. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- 47.Fellingham GW, McBride K, Tolley HD, Lyon JL. Statistics on suicide and LDS Church involvement in males age 15-34. Brigham Young Univ Stud. 2000;39(2):173–80. [PubMed] [Google Scholar]
- 48.Garroutte EM, Goldberg J, Beals J, Herrell R, Manson SM. Spirituality and attempted suicide among American Indians. Soc Sci Med. 2003;56(7):1571–9. doi: 10.1016/s0277-9536(02)00157-0. [DOI] [PubMed] [Google Scholar]
- 49.Hilton SC, Fellingham GW, Lyon JL. Suicide rates and religious commitment in young adult males in Utah. Am J Epidemiol. 2002;155(5):413–9. doi: 10.1093/aje/155.5.413. [DOI] [PubMed] [Google Scholar]
- 50.Hoffman S, Marsiglia FF. The impact of religiosity on suicidal ideation among youth in central Mexico. J Relig Health. 2014;53(1):255–66. doi: 10.1007/s10943-012-9654-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Huang JX, Xu YM, Zhong BL. Relationship between Buddhist belief and suicide risk in Chinese persons undergoing methadone maintenance therapy for heroin dependence. Front Psychiatry. 2020;11:414. doi: 10.3389/fpsyt.2020.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jacob L, Haro JM, Koyanagi A. The association of religiosity with suicidal ideation and suicide attempts in the United Kingdom. Acta Psychiatr Scand. 2019;139(2):164–73. doi: 10.1111/acps.12972. [DOI] [PubMed] [Google Scholar]
- 53.Wong YJ, Brownson C, Schwing AE. Risk and protective factors associated with Asian American students’ suicidal ideation: a multicampus, national study. J Coll Stud Dev. 2011;52(4):396–408. doi: 10.1353/csd.2011.0057. [DOI] [Google Scholar]
- 54.Kim GU, Son HK, Kim MY. Factors affecting suicidal ideation among premenopausal and postmenopausal women. J Psychiatr Ment Health Nurs. 2021;28(3):356–69. doi: 10.1111/jpm.12679. [DOI] [PubMed] [Google Scholar]
- 55.Kovess-Masfety V, Boyd A, Haro JM, Bruffaerts R, Villagut G, Lépine JP. et al. High and low suicidality in Europe: a fine-grained comparison of France and Spain within the ESEMeD surveys. J Affect Disord. 2011;133(1-2):247–56. doi: 10.1016/j.jad.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kurihara T, Kato M, Reverger R, Tirta IG. Risk factors for suicide in Bali: a psychological autopsy study. BMC Public Health. 2009;9:327. doi: 10.1186/1471-2458-9-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lawrence RE, Brent D, Mann JJ, Burke AK, Grunebaum MF, Galfalvy HC. et al. Religion as a risk factor for suicide attempt and suicide ideation among depressed patients. J Nerv Ment Dis. 2016;204(11):845–50. doi: 10.1097/nmd.0000000000000484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee H, Seol KH, Kim JW. Age and sex-related differences in risk factors for elderly suicide: differentiating between suicide ideation and attempts. Int J Geriatr Psychiatry. 2018;33(2):e300–e6. doi: 10.1002/gps.4794. [DOI] [PubMed] [Google Scholar]
- 59.Lester D. Spirituality and religiosity as predictors of depression and suicidal ideation: an exploratory study. Psychol Rep. 2012;110(1):247–50. doi: 10.2466/02.12.pr0.110.1.247-250. [DOI] [PubMed] [Google Scholar]
- 60.Lytle MC, Blosnich JR, De Luca SM, Brownson C. Association of religiosity with sexual minority suicide ideation and attempt. Am J Prev Med. 2018;54(5):644–51. doi: 10.1016/j.amepre.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Martiello MA, Boncompagni G, Lacangellera D, Corlito G. Risk factors for suicide in rural Italy: a case-control study. Soc Psychiatry Psychiatr Epidemiol. 2019;54(5):607–16. doi: 10.1007/s00127-018-1632-9. [DOI] [PubMed] [Google Scholar]
- 62.Mirzaie SN, Shams Alizadeh N. Prevalence rate of suicidal thoughts and its related factors in the medical students in Kurdistan University of Medical Sciences. Sci J Kurd Univ Med Sci. 2013;18(1):18–26. Persian. [Google Scholar]
- 63.Nisbet PA, Duberstein PR, Conwell Y, Seidlitz L. The effect of participation in religious activities on suicide versus natural death in adults 50 and older. J Nerv Ment Dis. 2000;188(8):543–6. doi: 10.1097/00005053-200008000-00011. [DOI] [PubMed] [Google Scholar]
- 64.Nkansah-Amankra S, Diedhiou A, Agbanu SK, Agbanu HL, Opoku-Adomako NS, Twumasi-Ankrah P. A longitudinal evaluation of religiosity and psychosocial determinants of suicidal behaviors among a population-based sample in the United States. J Affect Disord. 2012;139(1):40–51. doi: 10.1016/j.jad.2011.12.027. [DOI] [PubMed] [Google Scholar]
- 65.Nonnemaker JM, McNeely CA, Blum RW. Public and private domains of religiosity and adolescent health risk behaviors: evidence from the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003;57(11):2049–54. doi: 10.1016/s0277-9536(03)00096-0. [DOI] [PubMed] [Google Scholar]
- 66.O’Reilly D, Rosato M. Religion and the risk of suicide: longitudinal study of over 1 million people. Br J Psychiatry. 2015;206(6):466–70. doi: 10.1192/bjp.bp.113.128694. [DOI] [PubMed] [Google Scholar]
- 67.Panczak R, Spoerri A, Zwahlen M, Bopp M, Gutzwiller F, Egger M. Religion and suicide in patients with mental illness or cancer. Suicide Life Threat Behav. 2013;43(2):213–22. doi: 10.1111/sltb.12009. [DOI] [PubMed] [Google Scholar]
- 68.Peltzer K, Yi S, Pengpid S. Suicidal behaviors and associated factors among university students in six countries in the Association of Southeast Asian Nations (ASEAN) Asian J Psychiatr. 2017;26:32–8. doi: 10.1016/j.ajp.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 69.Rasic D, Robinson JA, Bolton J, Bienvenu OJ, Sareen J. Longitudinal relationships of religious worship attendance and spirituality with major depression, anxiety disorders, and suicidal ideation and attempts: findings from the Baltimore epidemiologic catchment area study. J Psychiatr Res. 2011;45(6):848–54. doi: 10.1016/j.jpsychires.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 70.Rasic DT, Belik SL, Elias B, Katz LY, Enns M, Sareen J. Spirituality, religion and suicidal behavior in a nationally representative sample. J Affect Disord. 2009;114(1-3):32–40. doi: 10.1016/j.jad.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 71.Rew L, Thomas N, Horner SD, Resnick MD, Beuhring T. Correlates of recent suicide attempts in a triethnic group of adolescents. J Nurs Scholarsh. 2001;33(4):361–7. doi: 10.1111/j.1547-5069.2001.00361.x. [DOI] [PubMed] [Google Scholar]
- 72.Robins A, Fiske A. Explaining the relation between religiousness and reduced suicidal behavior: social support rather than specific beliefs. Suicide Life Threat Behav. 2009;39(4):386–95. doi: 10.1521/suli.2009.39.4.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rushing NC, Corsentino E, Hames JL, Sachs-Ericsson N, Steffens DC. The relationship of religious involvement indicators and social support to current and past suicidality among depressed older adults. Aging Ment Health. 2013;17(3):366–74. doi: 10.1080/13607863.2012.738414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sidhartha T, Jena S. Suicidal behaviors in adolescents. Indian J Pediatr. 2006;73(9):783–8. doi: 10.1007/bf02790385. [DOI] [PubMed] [Google Scholar]
- 75.Sisask M, Varnik A, Kolves K, Bertolote JM, Bolhari J, Botega NJ. et al. Is religiosity a protective factor against attempted suicide: a cross-cultural case-control study. Arch Suicide Res. 2010;14(1):44–55. doi: 10.1080/13811110903479052. [DOI] [PubMed] [Google Scholar]
- 76.Snarr JD, Heyman RE, Slep AM. Recent suicidal ideation and suicide attempts in a large-scale survey of the US Air Force: prevalences and demographic risk factors. Suicide Life Threat Behav. 2010;40(6):544–52. doi: 10.1521/suli.2010.40.6.544. [DOI] [PubMed] [Google Scholar]
- 77.Poorolajal J, Panahi S, Ghaleiha A, Daryaei S, Darvishi N. Suicide and associated risk factors among college students. International Journal of Epidemiologic Research. 2017;4:245–50. [Google Scholar]
- 78.Stolz E, Fux B, Mayerl H, Rásky É, Freidl W. Passive suicide ideation among older adults in Europe: a multilevel regression analysis of individual and societal determinants in 12 countries (SHARE) J Gerontol B Psychol Sci Soc Sci. 2016;71(5):947–58. doi: 10.1093/geronb/gbw041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stroppa A, Moreira-Almeida A. Religiosity, mood symptoms, and quality of life in bipolar disorder. Bipolar Disord. 2013;15(4):385–93. doi: 10.1111/bdi.12069. [DOI] [PubMed] [Google Scholar]
- 80.Sun L, Zhang J. Suicide acceptability and suicide attempt: a case-control study with medically serious suicide attempters aged 15 to 54 years in rural China. J Nerv Ment Dis. 2018;206(9):694–8. doi: 10.1097/nmd.0000000000000863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Taylor RJ, Chatters LM, Joe S. Religious involvement and suicidal behavior among African Americans and Black Caribbeans. J Nerv Ment Dis. 2011;199(7):478–86. doi: 10.1097/NMD.0b013e31822142c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tran Thi Thanh H, Tran TN, Jiang GX, Leenaars A, Wasserman D. Life time suicidal thoughts in an urban community in Hanoi, Vietnam. BMC Public Health. 2006;6:76. doi: 10.1186/1471-2458-6-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Toussaint L, Wilson CM, Wilson LC, Williams DR. Religiousness and suicide in a nationally representative sample of Trinidad and Tobago adolescents and young adults. Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1441–50. doi: 10.1007/s00127-015-1045-y. [DOI] [PubMed] [Google Scholar]
- 84.Trevino KM, Balboni M, Zollfrank A, Balboni T, Prigerson HG. Negative religious coping as a correlate of suicidal ideation in patients with advanced cancer. Psychooncology. 2014;23(8):936–45. doi: 10.1002/pon.3505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tsoh J, Chiu HF, Duberstein PR, Chan SS, Chi I, Yip PS. et al. Attempted suicide in elderly Chinese persons: a multi-group, controlled study. Am J Geriatr Psychiatry. 2005;13(7):562–71. doi: 10.1176/appi.ajgp.13.7.562. [DOI] [PubMed] [Google Scholar]
- 86.Umamaheswari V, Avasthi A, Grover S. Risk factors for suicidal ideations in patients with bipolar disorder. Bipolar Disord. 2014;16(6):642–51. doi: 10.1111/bdi.12179. [DOI] [PubMed] [Google Scholar]
- 87.Ursano RJ, Heeringa SG, Stein MB, Jain S, Raman R, Sun X. et al. Prevalence and correlates of suicidal behavior among new soldiers in the US Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Depress Anxiety. 2015;32(1):3–12. doi: 10.1002/da.22317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.VanderWeele TJ, Li S, Tsai AC, Kawachi I. Association between religious service attendance and lower suicide rates among US women. JAMA Psychiatry. 2016;73(8):845–51. doi: 10.1001/jamapsychiatry.2016.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang Z, Koenig Harold G, Ma W, Liu L. Religious involvement, suicidal ideation and behavior in mainland China. Int J Psychiatry Med. 2015;48(4):299–316. doi: 10.2190/PM.48.4.e. [DOI] [PubMed] [Google Scholar]
- 90.Yen YC, Yang MJ, Yang MS, Lung FW, Shih CH, Hahn CY. et al. Suicidal ideation and associated factors among community-dwelling elders in Taiwan. Psychiatry Clin Neurosci. 2005;59(4):365–71. doi: 10.1111/j.1440-1819.2005.01387.x. [DOI] [PubMed] [Google Scholar]
- 91.Zhang J, Wieczorek W, Conwell Y, Tu XM, Wu BY, Xiao S. et al. Characteristics of young rural Chinese suicides: a psychological autopsy study. Psychol Med. 2010;40(4):581–9. doi: 10.1017/s0033291709990808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Poorolajal J. Equivalence model: a new graphical model for causal inference. Epidemiol Health. 2020;42:e2020024. doi: 10.4178/epih.e2020024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Agoramoorthy G, Hsu MJ. The suicide paradigm: insights from ancient Hindu scriptures. J Relig Health. 2017;56(3):807–16. doi: 10.1007/s10943-015-0178-3. [DOI] [PubMed] [Google Scholar]
- 94.Caribé AC, Studart P, Bezerra S, Brietzke E, Noto MN, Vianna-Sulzbach M. et al. Is religiosity a protective factor against suicidal behavior in bipolar I outpatients? J Affect Disord. 2015;186:156–61. doi: 10.1016/j.jad.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 95.Koenig HG. Research on religion, spirituality, and mental health: a review. Can J Psychiatry. 2009;54(5):283–91. doi: 10.1177/070674370905400502. [DOI] [PubMed] [Google Scholar]
- 96. Szklo M, Nieto FJ. Epidemiology: Beyond the Basics. Sudbury: Jones & Bartlett Publishers; 2007.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not available.