Abstract
Simple Summary
Patients with low-glycolytic hepatocellular carcinoma (HCC) show better clinical outcomes than those with hypoxic and high-glycolytic HCC. Low-glycolytic HCCs seem to utilize carbon sources other than glucose for metabolic fuel and tumor growth. However, by increasing tumor size, its outgrowth perfusion generates hypoxic foci inside the tumor and becomes more aggressive and resistant to therapy. In this study, we found that SLC13A5/NaCT is an important solute carrier (SLC) in low-glycolytic HCCs. To adapt to hypoxic conditions, low-glycolytic cancer cells have to switch metabolism from oxidative phosphorylation to hypoxia-induced glycolysis by the upregulation of HIF1α. However, extracellular citrate treatment in HCCs with high SLC13A5/NaCT expression had reduced glucose uptake due to HIF1α degradation, inducing the failure of metabolic adaptation to hypoxia, resulting in anti-cancer effects in in vitro and in vivo animal models.
Abstract
HCC is well known for low glycolysis in the tumors, whereas hypoxia induces glycolytic phenotype and tumor progression. This study was conducted to evaluate the expression of SLCs in human HCCs and investigated whether extracellular nutrient administration related to SLCs in low-glycolytic HCC can prevent hypoxic tumor progression. SLCs expression was screened according to the level of glycolysis in HCCs. Then, whether extracellular nutrient treatment can affect hypoxic tumor progression, as well as the mechanisms, were evaluated in an in vitro cell line and an in vivo animal model. Low-glycolytic HCCs showed high SLC13A5/NaCT and SLC16A1/MCT1 but low SLC2A1/GLUT1 and HIF1α/HIF1α expression. Especially, high SLC13A5 expression was significantly associated with good overall survival in the Cancer Genome Atlas (TCGA) database. In HepG2 cells with the highest NaCT expression, extracellular citrate treatment upon hypoxia induced HIF1α degradation, which led to reduced glycolysis and cellular proliferation. Finally, in HepG2-animal models, the citrate-treated group showed smaller tumor with less hypoxic areas than the vehicle-treated group. In patients with HCC, SLC13A5/NaCT is an important SLC, which is associated with low glycolysis and good prognosis. Extracellular citrate treatment induced the failure of metabolic adaptation to hypoxia and tumor growth inhibition, which can be a potential therapeutic strategy in HCCs.
Keywords: SLC13A5/NaCT, citrate, cancer metabolism, hepatocellular carcinoma, hypoxia
1. Introduction
Hepatocellular carcinoma (HCC) is the sixth most common diagnosed cancer and the third leading cause of cancer-related mortality worldwide [1]. HCC undergoes a characteristic hemodynamic transition from a predominantly portal to a solely arterial blood supply during tumor progression. As a result, HCC growth outpaces perfusion despite increased arterial flow, which eventually leads to hypoxia and progression to an aggressive tumor [2]. Hypoxia in HCCs causes differences in metabolic phenotypes on 18F-fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT), a functional imaging modality for tumor glycolysis [3]. While hypoxic tumor regions of HCC are associated with increased glycolysis on 18F-FDG PET/CT (high-glycolytic HCC), tumors without hypoxia show low-level 18F-FDG uptake (low-glycolytic HCC) [2]. More importantly, an increased glycolytic phenotype on PET/CT is associated with large tumor size, high histological grade, and poor clinical outcomes [4,5,6]. Therefore, the inhibition of glycolytic metabolism can effectively prevent tumor progression in HCCs.
Cell requires sufficient nutrient supply, including carbon and nitrogen sources, to support growth and survival [7]. The solute carrier (SLC) group of membrane transport proteins participates as a metabolic gateway in cellular nutrient uptake [8]. Particularly, the use of glucose is important for the generation of adenosine triphosphate (ATP) and building blocks for cellular proliferation [9]. Thus, cancer cells induce changes in metabolic programs from oxidative phosphorylation to glycolysis through increased expression of the glucose transporter [10]. However, low-glycolytic tumors seem to utilize carbon sources other than glucose for bioenergetics and tumor proliferation [9,11]. Furthermore, acetate uptake through the increased expression of monocarboxylate transporter 1 (MCT1) is an important factor in generating Acetyl-CoA for energy production (via the tricarboxylic acid (TCA) cycle) and biomass in low-glycolytic HCCs [12,13,14]. Thus, 11C-acetate, a radioactive version of acetate, has been proposed as a complementary radiotracer for detecting low-glycolytic HCCs that cannot be identified by 18F-FDG [15]. However, apart from acetate, there is limited information on other carbon sources for tumor growth in low-glycolytic HCCs. Furthermore, low-glycolytic HCCs depend on oxidative phosphorylation using alternative carbon sources other than glucose. Citrate is a well-known tricarboxylic acid (TCA) cycle intermediate and an important carbon source for the biosynthesis of fatty acid and cholesterol synthesis [16,17]. The pool of cellular citrate was previously believed to be derived mainly from the reverse TCA cycle through glucose-derived pyruvate and reductive carboxylation of glutamine [18]. However, several lines of evidence suggest that the uptake and utilization of citrate from the extracellular space may play a role in cancer biology [19,20,21]. An elevated cytosolic citrate concentration inhibits the growth of several types of human cancer cells [22,23,24].
To investigate the utilization of carbon sources in low-glycolytic HCCs, we compared the expression of SLCs in human HCCs with low versus high glucose uptake. Then, in HCCs with low glycolysis, the most expressed SLC and its metabolic substrate was selected to investigate its effects on glucose metabolism and tumor growth in vitro and in vivo.
2. Materials and Methods
2.1. Human HCC Samples
The use of tissue samples for this study was approved by the Institutional Review Board at Yonsei University Health System Severance Hospital (Seoul, Korea, Yonsei IRB number 4-2015-0904). This study was conducted according to the current guidelines for ethical research. All patients provided oral and written consent after receiving detailed information on the study and agreed to data collection. Our study included patients with CC treated by curative surgical resection who had undergone 18F-FDG scans for preoperative staging at our institution. Gene expression profiles and protein expression for SLCs were compared between high and low 18F-FDG tumors. HCC with 18F-FDG uptake higher than that in the background liver was classified as a high-glycolytic tumor.
2.2. Cell Culture
HepG2 cells were cultured in RPMI-1640 (Hyclone, Logan, UT, USA), whereas SK-Hep1 and Huh7 were cultured in Dulbecco’s Modified Eagle Medium (Hyclone, Logan, UT, USA). All media were supplemented with 10% fetal bovine serum (Thermo Fisher, Waltham, MA, USA) and 1% penicillin/streptomycin (Thermo Fisher, Waltham, MA, USA). All cell lines were purchased from the Korean Cell Line Bank (http://cellbank.snu.ac.kr, accessed on 14 July 2020). In addition, a predesigned siRNA targeting hypoxia-inducible factor 1α (HIF1α) and mouse double minute 2 homolog (MDM2) was purchased from Bioneer (Daejeon, Korea). The cells were transfected using Lipofectamine RNAi MAX (Invitrogen, cat #13778-075, Waltham, MA, USA) following the manufacturer’s instructions. To induced hypoxic conditions, we used a hypoxia incubator (1% O2) or 100 μM CoCl2, depending on the experiment, since Western blotting (WB) showed that both conditions resulted in a similar expression of HIF1α (Figure S1).
2.3. In Vitro 14C-Deoxyglucose (DG) and 14C-Citrate Uptake Assay
HepG2 cells were incubated with sodium citrate (1 or 5 mM) and CoCl2 (100 μM, Sigma-Aldrich, St. Louis, MO, USA). After incubating for 24 h, cells were treated for 1 h with 0.5 μCi 14C-DG (Perkin Elmer, Waltham, MA, USA) in DMEM medium (Gibco, cat # 11966-025, Waltham, MA, USA) with 5 mM glucose, or 0.1 μCi 14C-citrate (PerkinElmer) in a reaction buffer containing 25 mM HEPES (pH 7.5), 140 mM sodium chloride, 5.4 mM potassium chloride, 0.8 mM magnesium sulfate, 1.8 mM calcium chloride, 25 mM Tris-HCl, and 5 mM D-glucose for 2 h. After washing with PBS, the cells were lysed using 0.1 N NaOH lysis buffer (Sigma-Aldrich) for 2 h. The cell lysates were collected in 6 mL pony vials (Perkin Elmer) containing 5 mL Ultima Gold liquid scintillation cocktail (Perkin Elmer) and measured using a liquid scintillation counter (Perkin Elmer). The measured count per minute was normalized to the protein concentration determined using a bicinchoninic acid protein assay kit (Thermo Fisher, Waltham, MA, USA).
2.4. Cell Viability and ATP Measurement
HepG2 cells were treated with sodium citrate (1 or 5 mM) under hypoxia. After 24 h, the cell viability of HepG2 cells was estimated using a cell counting kit (CCK-8). The absorbance was measured at a wavelength of 450 nm. ATP levels were determined using an ATP assay kit (Abcam, Cambridge, UK) according to the manufacturer’s instructions. Cell viability (absorbance: 562 nm) and ATP (absorbance: 570 nm) were measured using a microplate reader (Molecular Devices, Sunnyvale, CA, USA). All experiments were performed at least three times with three wells in each condition.
2.5. Western Blotting
Total protein was extracted using sodium dodecyl sulfate (SDS) lysis buffer (1% SDS, 60 mM Tris-HCl) with protease inhibitor (Roche) and phosphatase inhibitor (PhosSTOP, Roche, Basel, Switzerland). ImageQuant LAS 4000 mini (GE, Chicago, IL, USA) was used for the digital visualization of the chemiluminescent Western blots. These experiments were replicated at least three times with similar results. ImageJ (National Institutes of Health, Bethesda, Maryland, USA) software (ver 1.4.3) was used for band quantification. The primary antibodies in the present study for WB are listed in Table S1.
2.6. Flow Cytometry
HepG2 cells (1 × 106 cells/mL) were prepared following the manufacturer’s instructions to measure the apoptotic rate using the FITC Annexin V apoptosis detection kit I (BD science) and mitochondrial reactive oxygen species (ROS) using the MitoSOX (Invitrogen, Waltham, MA, USA). Apoptotic rate and ROS were quantitatively analyzed using the BD FACS LSR II SORP system (BD science, Franklyn-lake, NJ, USA). Details of the gating strategy for analysis are shown in Figure S2.
2.7. In Vivo Experiment Using HepG2-Xenograft Animal Model
All animal experiments were approved by The Institutional Animal Care and Use Committee of the Yonsei University Health System (approval number: 2020-0242). Four-to-five-week-old female BALB/c nude mice were purchased from Orient Bio (Gyeonggi-do, Korea). HepG2 cells (1 × 107 cells 100 μL PBS) mixed with 100 μL matrigel were subcutaneously injected into the right leg of each mouse. Tumor size was calculated as 1/2 × A × B2 (where A is the long axis, and B is the short axis). When the tumor size reached 300 mm3, the mice were allowed to drink water supplemented with the vehicle (PBS) or citrate (4 g/kg daily) for 28 days.
2.8. RNA Expression
The Cancer Genome Atlas (TCGA) data were obtained from the OncoLnc TCGA data portal (www.oncolnc.org, accessed on 14 July 2020). A set of 360 HCC samples with high and low gene expression groups (30–70 percentile) was used for analysis. GraphPad Prism 9 (San Diego, CA, USA) was used for mapping. Total RNAs were extracted from human HCC tissues and cell lines using a RNeasy Mini Kit (QIAGEN, Munich, Germany) for RNA expression profiling. RNA sequencing and data analysis were assessed by EBIOGEN Inc. (Seoul, Korea).
2.9. Statistical Analysis
Statistical analyses were performed using GraphPad Prism software (GraphPad Software, Inc. (California, CA, USA)). Results were expressed as means ± SEM (range). The p-values between groups were calculated using one-way analysis of variance (ANOVA) with Tukey’s multiple comparison test in multiple groups and unpaired t-tests in two groups. A log-rank test was conducted to compare overall survival (OS). Pearson’s correlation coefficient was used to calculate the correlation between the two factors. A p-value of less than 0.05 was considered significant.
3. Results
3.1. Correlation of SLC-Related Genes and Proteins in HCC Patients with High- and Low-Glycolysis
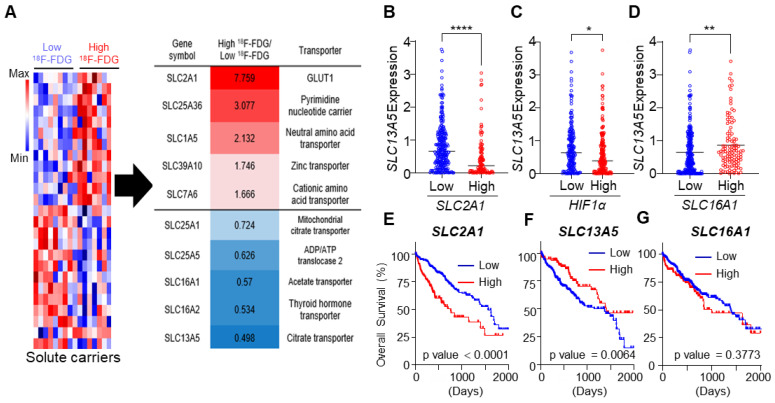
We analyzed the expression of SLC genes between high- and low-glycolytic tumors. SLCs are major nutrient transporters exhibiting various expression levels in cancers with different metabolic phenotypes. Our gene expression profiles of patients with HCC revealed that 25 of the SLC-related genes were significantly dysregulated between high- and low-glycolytic tumors. Upregulation of SLC2A1 (glucose transporter, fold change: 7.759), SLC1A5 (neutral amino acid transporter, fold change: 2.132), and SLC7A6 (cationic amino acid transporter, fold change: 1.666) and downregulation of SLC16A1 (monocarboxylate transporter, MCT1, fold change: 0.57) and SLC13A5 (citrate transporter, fold change: 0.498) in high-glycolytic HCCs (n = 8) compared to low-glycolytic HCCs (n = 8, Figure 1A) were observed. To confirm the results of the gene expression profiles, we performed TCGA analysis including HCCs from 360 patients. A significant negative correlation between SLC2A1 and SLC13A5 (p < 0.0001), as well as between HIF1α and SLC13A5 (p = 0.0158), and a positive correlation between SLC16A1 and SLC13A5 (p = 0.008) were revealed (Figure 1B–D and Figure S3). Furthermore, survival analysis using the database showed that SLC2A1 (p < 0.0001) and SLC13A5 (p = 0.0064), but not SLC16A1 (p = 0.3773) expression was associated with OS (Figure 1E–G). SLC13A5 and SLC16A1 were highly expressed in low-glycolytic HCCs without HIF1α expression. Given the prognostic value for predicting OS, SLC13A5 was more important than SLC16A1.
Figure 1.
Reciprocal expression of solute carrier (SLC)-related gene in patients with hepatocellular carcinoma (HCC) with high-and low-glycolysis. (A) Heat-map of SLC-related genes of frozen tissues from patients with HCC with high 18F-fluorodeoxyglucose (FDG) (n = 8) or low 18F-FDG (n = 8). (B–D) The expression of SLC13A5 with low and high SLC2A1 (B), HIF1α (C), and SLC16A1 (D) expression groups (70-30 percentile) in the Cancer Genome Atlas (TCGA) dataset of HCC patients. (E–G) The median OS based on the TCGA dataset of HCC patients in low and high expression groups (70-30 percentile) in indicated genes. Data were represented as mean ± SEM and were compared using unpaired two-tailed t-tests and log-rank tests. * p < 0.05, ** p < 0.01, **** p < 0.0001.
3.2. Citrate Treatment Affects HIF1α in HCC Cells with High NaCT Expression
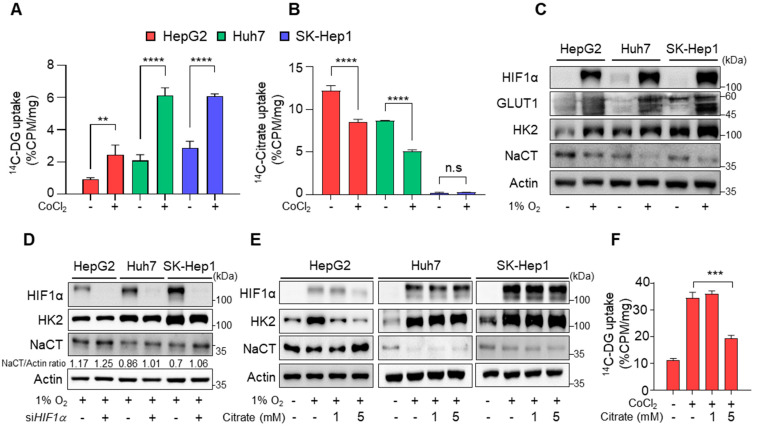
The results from human data showed a significant negative correlation between NaCT and HIF1α expression, which raised the question of whether citrate affects HIF1α expression and glycolysis in HCCs. To further investigate the role of citrate, 14C-DG and 14C-citrate uptake were screened in human HCC cell lines. There was an inverse correlation between 14C-DG and 14C-citrate uptake among the HCC cell lines, in which HepG2 cells had the lowest 14C-DG but the highest 14C-citrate uptake (Figure 2A,B). When the hypoxic condition was induced, increased 14C-DG uptake and decreased 14C-citrate uptake were noted in HepG2 and Huh7 cells, respectively (Figure 2A,B). Consistent with the uptake assay, HepG2 showed the highest NaCT expression but the lowest hexokinase 2 (HK2) expression. However, the expression of SLCs was reversed in hypoxia (Figure 2C). When cells were transfected with siHIF1α, reduced NaCT expression upon hypoxia was restored (Figure 2D). The results confirmed an inverse correlation between HIF1α and NaCT expression. Membranous GLUT1 is responsible for the constitutive uptake of glucose into cells [25]. HepG2 cells showed high cytoplasmic expression of GLUT1, which could not be differentiated from membranous GLUT1 on WB analysis. Therefore, HK2 was used for WB studies as a surrogate for glycolysis (Figure S4).
Figure 2.
Reduction of glycolysis after citrate treatment. (A,B) In vitro 14C-DG uptake (A) and 14C-citrate (B) in HCC cells after incubation with or without 100 μM CoCl2. (C) The expression of HIF1α, GLUT1, HK2, NaCT, and β-actin in HCC cells after 24 h incubation under 21% or 1% O2. (D) HIF1α, HK2, NaCT, and β-actin expression levels in HCC cells after transfection with siRNA oligos against HIF1α (siHIF1α) or scrambled siRNA oligos for 24 h under 1% O2 conditions. (E) HIF1α, HK2, NaCT, and β-actin expression levels in HCC cells after treatment with the indicated condition for 24 h. (F) In vitro 14C-DG uptake in HepG2 cells after the indicated treatment. Data were represented as mean ± SEM and were compared using unpaired two-tailed t-tests and one-way ANOVA tests. ** p < 0.01, *** p < 0.001, **** p < 0.0001; n.s, not significant. Full Western Blot images can be found in Figure S9.
Next, to see the effects of extracellular citrate on HIF1α expression and tumor glycolysis, HCC cell lines were treated with citrate for 24 h under hypoxic conditions. Citrate treatment significantly reduced HIF1α and HK2 expression and increased NaCT expression in HepG2 cells. However, citrate treatment did not affect HIF1α and NaCT expression in Huh7 and SK-Hep1 cells with high glucose uptake and low NaCT expression (Figure 2E and Figure S5). Accordingly, hypoxia-induced increased 14C-DG uptake was significantly reduced (Figure 2F). These findings indicate that citrate treatment decreased hypoxia-induced glycolysis via reduced HIF1α expression in HCC cells with a high transport capacity for citrate.
3.3. Effects of Citrate Treatment on Glycolytic Pathway and HIF1α Regulation
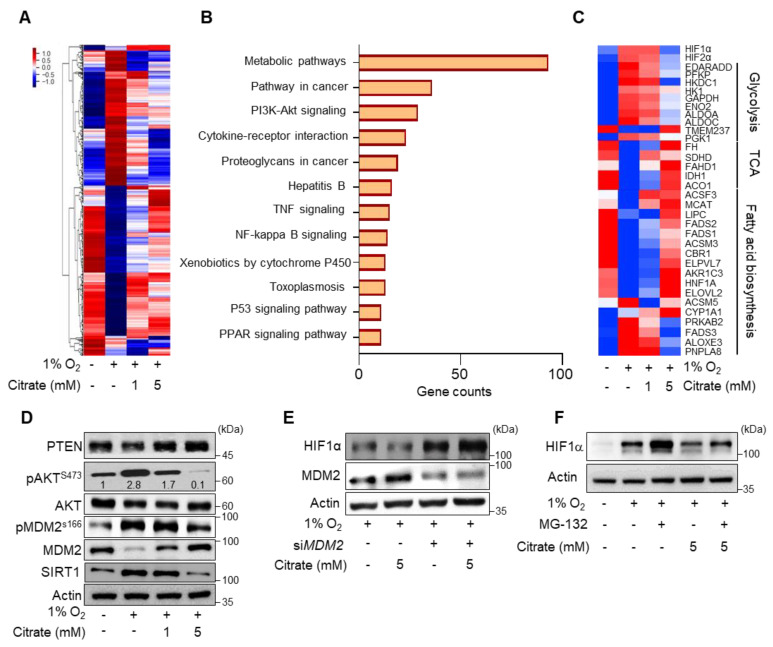
To understand the effect of citrate treatment on cellular metabolism, we analyzed global gene expression profiles in HepG2 cells. The hierarchical clustering heat-map analysis was performed with dysregulated genes after treatment with 1 and 5 mM citrate under hypoxia compared to normoxia. Gene expression was dysregulated in a dose-dependent manner (Figure 3A). In fact, gene expression patterns of 5 mM citrate treatment under hypoxia resembled those of normoxia. In addition, we evaluated the biological functions of the 4334 dysregulated genes following 5 mM citrate treatment using Kyoto Encyclopedia of Genes and Genomes pathway analyses (Figure 3B). The dysregulated genes were mainly associated with the following categories: metabolic pathway, pathway in cancer, and phosphoinositide 3-kinase (PI3K)/protein kinase B (AKT) signaling pathway. Among the metabolic pathway, oxidative phosphorylation (p = 0.0), pantothenate and CoA biosynthesis (p = 0.008), glycerolipid (p = 0.01), and ether lipid (p = 0.04) metabolism pathways were upregulated, whereas hypoxia (p = 0.008), KRAS signaling (p = 0.04), and notch signaling (p = 0.012) pathways were downregulated after citrate treatment (Figure S6). Therefore, in cancer metabolism, mitochondria-related pathways are significantly regulated at the gene expression level by citrate treatment. In the metabolic pathway category, glycolytic metabolism-related genes (HK1, PFKP, ALDOA, GAPDH, and PGK1) were dose-dependently downregulated. In contrast, the genes related to the TCA cycle (FH, SDHD, IDH1, and ACO1) and fatty acid synthesis (FADS1, FADS2, ELOVL2, and MCAT) were upregulated (Figure 3C).
Figure 3.
Effect of citrate treatment on HIF1α expression. (A) Heat-map representing color-coded expression levels of differentially expressed genes (p > 0.05, normalized data(log2) > 4, up- or downregulated > 1.5-fold) in HepG2 cells after treatment with or without citrate treatment under 1% O2 for 24 h. (B) Top 12 significantly enriched pathways of differentially expressed genes associated with citrate treatment under hypoxic conditions as analyzed by the Kyoto Encyclopedia of Genes and Genomes pathway analysis. (C) Heat-map of dysregulated genes related to glycolysis, TCA cycle, and fatty acid biosynthesis after treatment with the same as (A). (D) PTEN, phosphor (p) AKT (S473), AKT, MDM2, pMDM2 (S166), SIRT1, and β-actin expression levels in HepG2 cells after incubation with citrate (0, 1, or 5 mM) under 21% or 1% O2 for 24 h. (E) HIF1α, MDM2, and β-actin expression levels in HCC cells after transfection with siRNA oligos against MDM2 (siMDM2) or scrambled siRNA oligos for 24 h incubation upon indicated condition. (F) HIF1α and β-actin expression levels in HepG2 cells after treatment with citrate and MG-132 under 21% or 1% O2 for 8 h. Full Western Blot images can be found in Figure S10.
Finally, we investigated the underlying mechanisms on how citrate treatment affects HIF1α expression. Our analysis showed significant changes of expression in HIF1α stability-related gene (PTEN, AKT, MDM2, and SIRT1) upon citrate treatment. The upregulation of phosphatase and tensin homolog and MDM2, and downregulation of phosphorylated(p) AKT, pMDM2, and Sirtuin1 (SIRT1) were also identified in protein levels (Figure 3D). MDM2 is known to increase proteasomal degradation of HIF1α through PTEN/PI3K/AKT signaling [26]. Additionally, we found that MDM2-silenced HepG2 cells failed to degrade HIF1α (Figure 3E). Furthermore, HIF1α expression was partially reversed by MG-132, a proteasome inhibitor, suggesting the involvement of the ubiquitin–proteasome pathway (Figure 3F). Taken together, the results suggest that citrate treatment affected HIF1α expression at the protein stability level in the proteasomal pathway.
3.4. Anti-Tumor Effects of Citrate in Human HCC Cell Lines and Mouse Xenograft Models
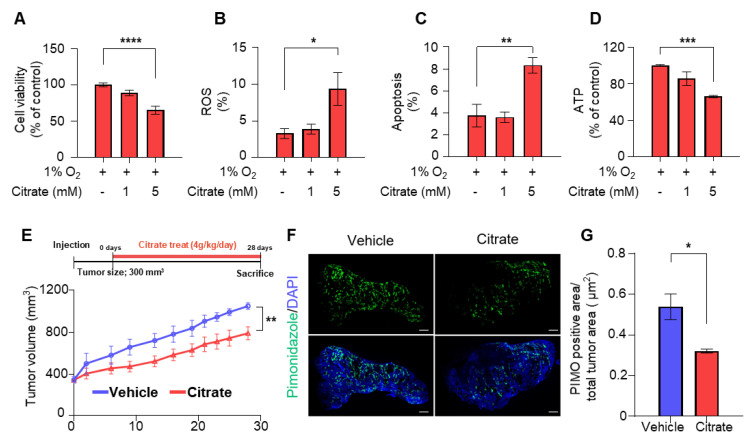
We evaluated cell viability in hypoxia based on the impact of HIF1α degradation by citrate treatment. Cell viability was significantly reduced after 5 mM citrate treatment in HepG2 cells, but not in Huh7 and SK-Hep1 cells, with lower citrate transport capacity (Figure 4A and Figure S7A–C). In addition, intracellular ROS levels and apoptosis were increased (Figure 4B,C and Figure S2), but intracellular ATP levels were significantly reduced (Figure 4D).
Figure 4.
Anti-tumor effect of citrate in vitro and in vivo studies. (A) Cell viability in HepG2 cells following indicated treatment under 1% O2 for 24 h. (B) ROS production was measured by flow cytometry using MitoSOX staining in HepG2 cells following treatment with the same as (A). (C) Rates of apoptosis (%) counted by flow cytometry following staining with Annexin V-fluorescein isothiocyanate and PI in HepG2 cells after treatment with the same as (A). (D) ATP levels in HepG2 cells after treatment with the same as (A). (E) The average tumor volumes of mice receiving drinking water supplemented with vehicle (n = 5) or citrate (4 g/kg/day, n = 6) for 28 days. (F) Representative images of immunofluorescence staining with pimonidazole. (G) Quantification of the percentage of pimonidazole-positive area from vehicle (n = 4) or citrate-treated (n = 4) mice. Data represented as mean ± SEM and were compared using unpaired two-tailed t-tests and one-way ANOVA tests. * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001.
Next, we evaluated the anti-cancer effects of citrate in vivo. Mouse xenograft using HepG2 cells were allowed to drink water supplemented with the vehicle or citrate at 4 g/kg/day for 28 days (Figure 4E). Citrate treatment significantly reduced tumor volumes, and the growth rate was lower than that observed with vehicle treatment (−4.8%, Figure 4E). In addition, mouse xenografts in the citrate-treated group showed significantly smaller hypoxic regions than the tumors in the vehicle-treated group, consistent with the HIF1α degradation upon citrate treatment in the in vitro cell line experiments (Figure 4F,G and Figure S8). In addition, as in the in vitro experiment, p-AKT was downregulated, whereas PTEN and MDM2 was upregulated after citrate treatment (Figure S8). Moreover, the reduction of HIF1α-related protein (GLUT1), proliferation index (Ki67) and angiogenesis (CD31), and the increased level of cleaved caspase-3 (CC3) were observed in citrate-treated animal model (Figure S8). To summarize, citrate treatment showed anti-tumor effects in the in vitro cell lines and in vivo mouse xenografts.
4. Discussion
Increased glycolysis measured using 18F-FDG PET/CT is associated with hypoxia, which leads to resistance to chemotherapy and radiotherapy, as well as poor clinical outcomes in patients with HCC [27,28]. Thus, inhibiting HIF1α expression can ameliorate dysregulated glucose metabolism, which can effectively prevent tumor progression in HCCs. In this study, gene expression profiles in human HCCs showed an opposing pattern of SLC expression in tumor regions with or without increased 18F-FDG uptake. Tumor regions without increased 18F-FDG uptake showed increased SLC13A5 and SLC16A1 expression, whereas tumors with increased 18F-FDG uptake showed high SLC2A1 and HIF1α. Although MCT1 expression is already well-known, our study discovered high SLC13A5 expression in HCCs of low glycolysis.
Metabolic phenotypes in tumors are related to the differing utilization of nutrients and aberrant expression of the nutrient transporters [8,29,30]. Although it might be important for developing therapeutic strategies, little is known about the metabolic characteristics and clinical significance of cancers using different nutrients. In human HCCs, it is already apparent that increased acetate metabolism through MCT1 expression plays an important role as an alternative carbon source of glucose for supporting tumor growth [14,31]. Compared to glycolytic tumors, HCCs with acetate utilization were less malignant and associated with better patient prognosis [32,33]. Previously, there was no information on whether acetate is the only carbon source in low-glycolytic HCCs. In this study, we found citrate to be another carbon source. SLC13A5/NaCT, a plasma membrane citrate transporter, has recently been identified as a metabolic target in human liver cancer cell lines [34]. However, the character of HCCs with increased SLC13A5/NaCT expression was unknown. Our result showed that increased citrate uptake was associated with decreased glucose uptake in in vitro cancer cell lines, mouse xenograft models, and human HCCs. More importantly, we found a significant negative correlation between NaCT and HIF1α expression in human HCC, suggesting that citrate can be potential therapeutic strategy preventing metabolic adaptation to hypoxic tumor. However, the mechanism of HIF1α-mediated regulation of SLC13A5/NaCT expression has not been addressed in this study.
In normoxia, citrate reduces glucose flux into cancer cells [21]. Here, we investigated the impact of extracellular citrate treatment on cancer metabolism under hypoxia. In HCC cells with NaCT expression, citrate treatment induced increased NaCT expression and intracellular citrate uptake, which downregulated the genes related to glycolysis despite hypoxia.
Next, we investigated how citrate induced the reduction of HIF1α under hypoxia. HIF1α levels can be controlled at the protein level by the ubiquitin–proteasome pathway and translational modifications, and at the mRNA level [35]. In this study, we found significantly increased MDM2 in the PTEN–PI3K–AKT–MDM2 pathway upon citrate treatment. MDM2, a ubiquitin ligase, binds to HIF1α for degradation by the ubiquitin–proteasome pathway under hypoxia [35]. In addition, phospho-MDM2 (pMDM2) translocation to the nucleus is mediated by the upregulation of phospho-AKT (pAKT) [26,36]. We assume that citrate treatment reduces pAKT activity (Figure 3D), resulting in the inhibition of pMDM2 translocation from the cytoplasm to the nucleus. An increased amount of unphosphorylated MDM2 in the cytoplasm may be involved in the proteasomal degradation of HIF1α. Gene silencing of MDM2 and treatment with proteasome inhibitor failed to degrade HIF1α upon citrate treatment, confirming the role of citrate in HIF1α degradation through 26S proteasomes. In addition, MDM2 increases the ubiquitination and proteasomal degradation of SIRT1. Given the role of SIRT1 in stabilizing HIF1α by direct binding and deacetylation in hypoxia [37,38], the decreased level of SIRT1 might contribute to the increased HIF1α degradation by MDM2. Taken together, we found a new regulatory mechanism in which citrate treatment reduced HIF1α expression through the regulation of protein degradation via increased MDM2 and decreased SIRT1 expression.
A few case reports have shown anti-tumor effect of oral citrate administration in patients [39,40]. Thereafter, studies have investigated the anti-cancer properties of citrate treatment and the potential mechanisms related to it [22,23,24]. In lung and breast cancer animal models, citrate treatments inhibited tumor growth by suppressing the insulin-like growth factor type 1 receptor (IGF-1R)/AKT/PTEN/eukaryotic translation initiation factor 2A (eIF2A) pathway [22]. Wang et al. reported similar results by inhibiting phosphofructokinase 1 (PFK1), a glycolytic enzyme in a gastric cancer model [23]. In this study, we also found that citrate treatment reduced tumor cell growth in an in vitro cell line and resulted in smaller and fewer hypoxic tumors with a decreased proliferative index in in vivo animal models. In contrast to previous studies, we observed that increased intracellular citrate uptake caused HIF1α degradation through the PTEN–PI3K–AKT–MDM2 pathway, responsible for reduced glucose flux. Accordingly, reduced intracellular ATP and increased ROS levels and apoptosis contributed to reduced cellular proliferation. Future studies are required to determine the potential of citrate treatment to overcome chemotherapy resistance.
5. Conclusions
There is a contrasting pattern of GLUT1 and NaCT expression in HCCs, meaning that cancer cells with low glucose uptake have high citrate uptake and vice versa. In turn, citrate treatment suppresses HIF1α stability and glycolysis, which can be a therapeutic strategy to prevent further hypoxic tumor progression and overcome chemotherapy resistance in low-glycolytic HCCs with citrate dependence.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers14143355/s1, Figure S1: Expression of HIF1α in CoCl2 and 1% O2. Figure S2: Flow cytometry gating strategy for HepG2 cells. Figure S3: Correlation analysis of SLC13A5 expression in TCGA dataset of HCC patients. Figure S4: Localization of GLUT1 in HCC cells. Figure S5: Quantification of the HIF1α expression level in HCC cells. Figure S6: Gene set enrichment analysis (GSEA) enrichment plots. Figure S7: The effect of citrate treatment in HCC cells under hypoxia. Figure S8: Immunostaining of HCC from HepG2 xenograft model with vehicle and citrate-treated group, Figure S9: Uncropped Western Blot images from Figure 2, Figure S10: Uncropped Western Blot images from Figure 3, Table S1: Antibody of target protein.
Author Contributions
Conceptualization, M.Y. and M.L.; validation, S.Y.K., J.K., W.J.K., H.Y.K. and S.P.; formal analysis, S.Y.K.; investigation, S.Y.K., J.K., H.Y.K. and W.J.K.; resources, D.K., H.W.L., D.H.H. and K.S.K.; writing-original draft preparation, S.Y.K.; writing review and editing, Y.P., M.L. and M.Y.; visualization, S.Y.K.; supervision, S.P., M.L. and M.Y.; project administration, M.Y.; funding acquisition, M.L. and M.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Institutional Review Board of the Yonsei University Health System Severance Hospital (Seoul, Korea, Yonsei IRB number: 4-2015-0904, approval date: 16 November 2015). All experiments were performed in accordance with relevant guidelines and regulations. All animal experiments were approved by The Institutional Animal Care and Use Committee of the Yonsei University Health System (approval number: 2020-0242, approval date: 25 January 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data generated or analyzed during this study are included in this article and its supplementary data files. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the National Research Foundation of Korea (Seoul, Korea; grant numbers NRF-2020R1A2B5B01098109, NRF-2022RA2C1007956 and RS-2022-00144475) and by an Incheon National University Research Grant in 2019.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca-Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Hwang S.H., Lee M., Lee N., Park S., Kim C.K., Park M.A., Yun M. Increased 18F-FDG uptake on PET/CT is associated with poor arterial and portal perfusion on multiphase CT. Clin. Nucl. Med. 2016;41:296–301. doi: 10.1097/RLU.0000000000001105. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y., Stewart E., Desjardins L., Hadway J., Morrison L., Crukley C., Lee T.Y. Assessment of intratumor hypoxia by integrated 18F-FDG-PET / perfusion CT in a liver tumor model. PLoS ONE. 2017;12:e0173016. doi: 10.1371/journal.pone.0173016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang L.Y., Li Y., Dai Y.B., Wang D.H., Wang X.C., Cao Y., Liu W.W., Tao Z.H. Glycolysis-related gene expression profiling serves as a novel prognosis risk predictor for human hepatocellular carcinoma. Sci. Rep. 2021;11:1875. doi: 10.1038/s41598-021-98381-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee N.C.W., Carella M.A., Papa S., Bubici C. High expression of glycolytic genes in cirrhosis correlates with the risk of developing liver cancer. Front. Cell Dev. Biol. 2018;6:138. doi: 10.3389/fcell.2018.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen H., Wu Q., Peng L., Cao T., Deng M.L., Liu Y.W., Huang J., Hu Y., Fu N., Zhou K.B., et al. Mechanism, Clinical significance, and treatment strategy of Warburg effect in hepatocellular carcinoma. J. Nanomater. 2021;2021:5164100. doi: 10.1155/2021/5164100. [DOI] [Google Scholar]
- 7.Zhu J., Thompson C.B. Metabolic regulation of cell growth and proliferation. Nat. Rev. Mol. Cell Biol. 2019;20:436–450. doi: 10.1038/s41580-019-0123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y., Zhang Y., Sun K., Meng Z., Chen L. The SLC transporter in nutrient and metabolic sensing, regulation, and drug development. J. Mol. Cell Biol. 2019;11:1–13. doi: 10.1093/jmcb/mjy052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin C.Q., Qie S., Sang N.L. Carbon source metabolism and its regulation in cancer cells. Crit. Rev. Eukar. Gene. 2012;22:17–35. doi: 10.1615/CritRevEukarGeneExpr.v22.i1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liberti M.V., Locasale J.W. The Warburg effect: How does it benefit cancer cells? Trends Biochem. Sci. 2016;41:287. doi: 10.1016/j.tibs.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keenan M.M., Chi J.T. Alternative Fuels for cancer cells. Cancer J. 2015;21:49–55. doi: 10.1097/PPO.0000000000000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeon J.Y., Lee M., Whang S.H., Kim J.W., Cho A., Yun M. Regulation of acetate utilization by monocarboxylate transporter 1 (MCT1) in hepatocellular carcinoma (HCC) Oncol. Res. 2018;26:71–81. doi: 10.3727/096504017X14902648894463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yun M., Bang S.H., Kim J.W., Park J.Y., Kim K.S., Lee J.D. The importance of acetyl coenzyme A synthetase for C-11-acetate uptake and cell survival in hepatocellular carcinoma. J. Nucl. Med. 2009;50:1222–1228. doi: 10.2967/jnumed.109.062703. [DOI] [PubMed] [Google Scholar]
- 14.Schug Z.T., Vande Voorde J., Gottlieb E. The metabolic fate of acetate in cancer. Nat. Rev. Cancer. 2016;16:708–717. doi: 10.1038/nrc.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ho C.L., Yu S.C., Yeung D.W. 11C-acetate PET imaging in hepatocellular carcinoma and other liver masses. J. Nucl. Med. 2003;44:213–221. [PubMed] [Google Scholar]
- 16.Feron O. The many metabolic sources of Acetyl-CoA to support histone acetylation and influence cancer progression. Ann. Transl. Med. 2019;7((Suppl. S8)):S277. doi: 10.21037/atm.2019.11.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez-Reyes I., Chandel N.S. Mitochondrial TCA cycle metabolites control physiology and disease. Nat. Commun. 2020;11:102. doi: 10.1038/s41467-019-13668-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fendt S.M., Bell E.L., Keibler M.A., Olenchock B.A., Mayers J.R., Wasylenko T.M., Vokes N.I., Guarente L., Vander Heiden M.G., Stephanopoulos G. Reductive glutamine metabolism is a function of the alpha-ketoglutarate to citrate ratio in cells. Nat. Commun. 2013;4:2236. doi: 10.1038/ncomms3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mycielska M.E., Dettmer K., Rummele P., Schmidt K., Prehn C., Milenkovic V.M., Jagla W., Madej G.M., Lantow M., Schladt M., et al. Extracellular Citrate Affects Critical Elements o Cancer Cell Metabolism and Supports Cancer Development In Vivo. Cancer Res. 2018;78:2513–2523. doi: 10.1158/0008-5472.CAN-17-2959. [DOI] [PubMed] [Google Scholar]
- 20.Iacobazzi V., Infantino V. Citrate—New functions for an old metabolite. Biol. Chem. 2014;395:387–399. doi: 10.1515/hsz-2013-0271. [DOI] [PubMed] [Google Scholar]
- 21.Haferkamp S., Drexler K., Federlin M., Schlitt H.J., Berneburg M., Adamski J., Gaumann A., Geissler E.K., Ganapathy V., Parkinson E.L., et al. Extracellular citrate fuels cancer cell metabolism and growth. Front. Cell Dev. Biol. 2020;8:602476. doi: 10.3389/fcell.2020.602476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ren J.G., Seth P., Ye H.H., Guo K., Hanai J., Husain Z., Sukhatme V.P. Citrate suppresses tumor growth in multiple models through inhibition of glycolysis, the tricarboxylic acid cycle and the IGF-1R pathway. Sci. Rep. 2017;7:4537. doi: 10.1038/s41598-017-04626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang T.A., Zhang X.D., Guo X.Y., Xian S.L., Lu Y.F. 3-bromopyruvate and sodium citrate target glycolysis suppress surviving, and induce mitochondrial-mediated apoptosis in gastric cancer cells and inhibit gastric orthotopic transplantation tumor growth. Oncol. Rep. 2016;35:1287–1296. doi: 10.3892/or.2015.4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu Y., Zhang X., Ahang H., Lan J., Huang G., Varin E., Lincet H., Poulain L., Icard P. Citrate induces apoptotic cell death: A promising way to treat gastric carcinoma? Anticancer Res. 2011;31:797–805. [PubMed] [Google Scholar]
- 25.Yan Q.Y., Lu Y.T., Zhou L.L., Chen J.L., Xu H.J., Cai M.J., Shi Y., Jiang J.G., Xiong W.Y., Gao J., et al. Mechanistic insights into GLUT1 activation and clustering revealed by supper-resolution imaging. Proc. Natl. Acad. Sci. USA. 2018;115:7033–7038. doi: 10.1073/pnas.1803859115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joshi S., Singh A.R., Durden D.L. MDM2 regulates hypoxic hypoxia-inducible factor 1alpha stability in an E3 ligase, proteasome, and PETN-phosphatidylinositol 3-kinase-AKT dependent manner. J. Biol. Chem. 2014;289:22785–22797. doi: 10.1074/jbc.M114.587493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Y., Zschaeck S., Liq Q., Chen S., Chen L., Wu H. Metabolic parameters of sequential 18F-FDG PET/CT predict overall survival of esophageal cancer patients treated with (chemo-) radiation. Radiat. Oncol. 2019;14:35. doi: 10.1186/s13014-019-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li X.F., Du Y., Ma Y.Y., Postel G.C., Civelek A.C. F-18-Fluorodeoxyglucose uptake and tumor hypoxia: Revisit F-18-fluorodexyglucose in oncology application. Transl. Oncol. 2014;7:240–247. doi: 10.1016/j.tranon.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ganapathy V., Thangaraju M., Prasad P.D. Nutrient transporters in cancer: Relevance to Warburg hypothesis and beyond. Pharmacol. Ther. 2009;121:29–40. doi: 10.1016/j.pharmthera.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 30.Cassim S., Raymond V.A., Dehbidi-Assadzadeh L., Lapierre P., Bilodeau M. Metabolic reprogramming enables hepatocarcinoma cells to efficiently adapt and survive to a nutrient-restricted microenvironment. Cell Cycle. 2018;17:903–916. doi: 10.1080/15384101.2018.1460023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Comerford S.A., Huang Z., Du X., Wang Y., Cai L., Witkiewicz A.K., Walters H., Tantawy M.N., Fu A., Manning H.C., et al. Acetate dependence of tumors. Cell. 2014;159:1591–1602. doi: 10.1016/j.cell.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee M., Jeon J.Y., Neugent M.L., Kim J.W., Yun M. 18F-fluorodeoxyglucose uptake on positron emission tomography/computed tomography is associated with metastasis and epithelial-mesenchymal transition in hepatocellular carcinoma. Clin. Exp. Metastasis. 2017;34:251–260. doi: 10.1007/s10585-017-9847-9. [DOI] [PubMed] [Google Scholar]
- 33.Park J.W., Kim J.H., Kim S.K., Kang K.W., Park K.W., Choi J.I., Lee W.J., Kim C.M., Nam B.H. A prospective evaluation of 18F-FDG and 11C-acetate PET/CT for detection of primary and metastatic hepatocellular carcinoma. J. Nucl. Med. 2008;49:1912–1921. doi: 10.2967/jnumed.108.055087. [DOI] [PubMed] [Google Scholar]
- 34.Kopel J., Higuchi K., Ristic B., Sato T., Ramachandran S., Ganapathy V. The hepatic plasma membrane citrate transporter NaCT (SLC13A5) as a molecular target for metformin. Sci. Rep. 2020;10:8536. doi: 10.1038/s41598-020-65621-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iommarini L., Porcelli A.M., Gasparre G., Kurelac I. Non-canonical mechanisms regulating hypoxia-inducible factor 1 alpha in cancer. Front. Oncol. 2017;7:286. doi: 10.3389/fonc.2017.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Urso L., Calabrese F., Faveretto A., Conte P., Pasello G. Critical review about MDM2 in cancer: Possible role in malignant mesothelioma and implications for treatment. Crit. Rev. Oncol. Hematol. 2016;97:220–230. doi: 10.1016/j.critrevonc.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 37.Lim J.H., Lee Y.M., Chun Y.S., Chen J., Kim J.E., Park J.W. Sirtuin 1 modulates cellular responses to hypoxia by deacetylating hypoxia-inducible factor 1 alpha. Mol. Cell. 2010;38:864–878. doi: 10.1016/j.molcel.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 38.Joo H.Y., Yun M., Jeong J., Park E.R., Shin H.J., Woo S.R., Jung J.K., Kim Y.M., Park J.J., Kim J., et al. SIRT1 deacetylates and stabilizes hypoxia-inducible factor-1 alpha (HIF-1 alpha) via direct interactions during hypoxia. Biochem. Bioph. Res. Commun. 2015;462:294–300. doi: 10.1016/j.bbrc.2015.04.119. [DOI] [PubMed] [Google Scholar]
- 39.Halabe Bucay A. Hypothesis proved citric acid (citrate) does improve cancer: A case of a patient suffering from medullary thyroid cancer. Med. Hypotheses. 2009;73:271. doi: 10.1016/j.mehy.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 40.Bucay A.H. Clinical report: A patient with primary peritoneal mesothelioma that has improved after taking citric acid orally. Clin. Res. Hepatol. Gas. 2011;35:241. doi: 10.1016/j.clinre.2010.12.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this article and its supplementary data files. Further inquiries can be directed to the corresponding author.