Abstract
Studies in military personnel are scarce and have reported increased rates of medical consultations and insomnia. The COVID-19 pandemic has been associated with a number of factors that increase the prevalence of insomnia, which has established consequences in the military. However, reported data are from different settings. We aimed to identify the prevalence and factors associated with insomnia during the second COVID-19 epidemic wave in Lambayeque, Peru. A retrospective study in 566 participants was conducted face-to-face in November 2021. The dependent variable was insomnia, measured with the Insomnia Severity Index. The independent variables were socio-labor variables, physical activity, food insecurity, eating behavior disorder, fear of COVID-19, and resilience. The prevalence of insomnia was 23% (95% CI: 19.6–26.7%). In multivariate analysis, insomnia was associated with a personal history of mental health (PR: 1.71, 95% CI: 1.01–2.93), food insecurity (PR: 1.43, 95% CI: 1.05–1.95), fear of COVID-19 (PR: 2.57, 95% CI: 1.87–3.54), and high resilience (PR: 0.60, 95% CI: 0.42–0.86). Overall, the Peruvian military population presents a high prevalence of insomnia during the pandemic period. Special attention should be paid to factors that influence insomnia. Prevention and promotion programs should be established to reverse this negative trend in the military.
Keywords: COVID-19, mental health, insomnia, public health, sleep quality
1. Introduction
At the end of 2019, the first case of COVID-19 infection was reported in China, Wuhan, which was declared a pandemic by the World Health Organization (WHO) on 11 March 2020. In Peru, up to 13,236 cases per day were reported, ranking as the fifth country with the highest mortality worldwide and confirming that the second wave of infection was devastating [1]. This situation led to changes in sleep patterns and rhythms across the board due to unprecedentedly high levels of stress [2]. Ideal sleep requires four essential attributes: good sleep quality, defined as the self-satisfaction of the sleep experience [3], an adequate sleep duration of at least 7 h, a regular circadian rhythm, and the absence of sleep disturbances [4]. Insomnia, defined as “difficulty initiating or maintaining sleep, waking too early, and inability to return to sleep,” is associated with waking fatigue [5].
The pandemic has variously affected the mental health of the general population. The highest estimate of depression was found in Africa (45%), of anxiety in Asia (34%), and of insomnia in Latin America (35%) [6]. Factors associated with insomnia in this context include death in the family, higher scores of stress, anxiety, and depression [7], having a job [8], having friends with COVID-19, and feeling estranged from family [9]. However, unlike the general population, military personnel represent a group that performs high-risk operations, such as emergency and disaster response. This involves intense exposure to stressors that lead to sleep disturbances, in addition to experiencing irregular and prolonged work schedules [10]. The American Academy of Sleep Medicine and the Sleep Research Society have proposed that adults get at least seven hours of sleep per night on a regular basis to maintain good health [11]. However, it is quite common for military personnel to get less than six hours of sleep per night [12], which translates into the development of sleep disorders.
Although research in military personnel is scarce, a study in the United States reported that the rates of consultations for insomnia increased from 16 to 75 per 1000 service members between 2005 and 2014 [13]. Another study in this country reported that insomnia rates increased from 6 to 272 per 10,000 service members between 2005 and 2019 [14]. Insomnia has also been identified as one of the most common symptoms of military personnel returning from deployment, with rates as high as 63.6% [15]. With respect to the consequences in the military, these have been reported to range from impairment of cognitive functions [16], increased risk of automobile accidents [17], and the development of chronic pathologies such as type II diabetes and hypertension [18], to a link with suicidal ideation [19].
The COVID-19 pandemic has affected mental health globally [20]. Although this context has been associated with the development of mental disorders, little research has been conducted in the military population. According to a pre-pandemic meta-analysis, insomnia is more likely to develop with age, alcohol dependence, white race, female sex, deployment and combat experience, depression, post-traumatic stress disorder, traumatic brain injury, and anxiety [21]. However, current studies have not evaluated other variables such as tobacco use, personal mental health history, work time, food insecurity, eating disorder, physical activity, and fear of COVID-19 infection. These variables are important because they may have a major influence on insomnia during the pandemic. In addition, previous studies in this context have included mostly military veterans [22], who represent a totally different group from the active military. Moreover, no reports of insomnia have been observed in military personnel from Latin American countries, in which the development of insomnia may occur differently.
Therefore, our study aimed to identify the prevalence and factors associated with insomnia in military personnel during the second wave of the COVID-19 epidemic in northern Peru.
2. Materials and Methods
2.1. Study Design and Population
A secondary data analysis of a cross-sectional study was conducted in military personnel in the city of Lambayeque, located in northern Peru. The data were collected from 2 to 9 November 2021, during the second COVID-19 epidemic wave in the country. In the primary study, the sample size was estimated considering a population size of 820 military personnel, an expected prevalence of 12.8% [23], a 99% confidence level, and a precision of 2.5%, which resulted in a sample size of 485 individuals. To this was added a 10% rejection rate and 10% incomplete registrations, calculating a required sample size of 582 individuals. Non-probabilistic snowball sampling was performed. Inclusion criteria were that the personnel were actively working during the pandemic or had worked at least 1 month. In the primary study, a total of 710 military personnel accepted to participate. For the present study, 144 of them were excluded as they did not fully respond to the Insomnia Severity Index (ISI). Therefore, the sample selected for the analysis consisted of 566 individuals.
We estimated a statistical power of 100% to evaluate the hypothesis of this study. We considered the expected prevalence of insomnia of 11.9% reported in Mexico [24] and the observed prevalence of insomnia of 23% according to the primary study, using a sample size of 582 participants.
2.2. Procedure
The present study was carried out in two phases: the first consisted of requesting permission from the Lambayeque military personnel infantry brigade and creating the questionnaire in the REDCap data entry system. The second phase consisted of face-to-face enrollment in compliance with biosecurity measures, which included data collection by field interviewers in two shifts lasting two hours. Finally, a member of the research team was instructed to carry out quality control of the data entered.
2.3. Questionnaire and Variables
The questionnaire consisted of 7 sections covering (1) sociodemographic data, (2) ISI, (3) resilience scale, (4) Household Food Security Access Scale (HFIAS), (5) Eating Disorder Scale (EAT-26), (6) Fear of COVID-19 Scale, and (7) Physical Activity Questionnaire (IPAQ-S).
General information was obtained on age (in years), sex (female, male), marital status (single, married, cohabitant, divorced), religion (none, Catholic, non-Catholic), self-report of frequent tobacco and alcohol consumption (no, yes), self-report of previous pathologies (arterial hypertension, type 2 diabetes), self-report of personal and family history of any mental health disorder (no, yes), seeking mental support (no, yes), having children (no, yes), trust in the government to manage the COVID-19 pandemic (no, yes), and time working in the military institution in the face of the COVID-19 pandemic (1 to 6 months, 7 to 12 months, 8 to 18 months, 19 months or more).
2.4. Dependent Variable
Insomnia scale (ISI). It is composed of 7 items that assess the nature, severity, and impact of insomnia. Higher scores reflect a higher degree of insomnia [25]. It has been validated in older adults, primary care patients, and the general Spanish-speaking population, demonstrating reliability with a Cronbach’s alpha of 0.82. [26]. The presence of insomnia was defined by a score of more than 8 points [27].
2.5. Independent Variables
Resilience scale (CD-RISC). The Connor-Davidson Short Resilience Scale, consisting of 10 items, was used. This instrument has been validated in the general Spanish-speaking population, showing a Cronbach’s alpha of 0.89 (general population) and a test–retest reliability of 0.87 (people with generalized anxiety disorder (GAD) and post-traumatic stress disorder) [28]. It was evaluated through a 5-point Likert scale with a score of 0 to 4. In general, it shows excellent psychometric properties and allows an efficient measurement of resilience [29]. A cut-off point of 30 was used to categorize high (>30) and low (<30) resilience [30].
Scale of access to food security in the household (HFIAS). This scale was developed by the United States Agency for International Development and includes 9 items, which correspond to questions about food in the last 4 weeks. The respondent is asked whether the household in which they live had experienced food insecurity in a given period, together with anxiety that they may have experienced, the quality and insufficient intake of food, and physical consequences. Responses are categorized into food insecurity (question 1), mild food insecurity (questions 2–4), moderate food insecurity (questions 5 and 6), and severe food insecurity (questions 6–9) [31]. The presence of food insecurity was categorized as mild, moderate, and severe. The instrument has been validated in Spanish-speaking older adults [31] and showed high internal consistency (α = 0.74) [32].
Eating disorder scale (EAT-26). This scale consists of 26 questions measured through a Likert scale with six response options (“never”, “rarely”, “sometimes”, “often”, “very often”, and “always”. The instrument has been validated in a Spanish-speaking female population, with a Cronbach’s alpha coefficient of 92.1% [33]. A score of 20 was considered the cut-off point for assuming the presence of an eating disorder [34].
Physical activity questionnaire (IPAQ-S). This scale considers the four components of physical activity (leisure, home maintenance, occupational, and transportation) [35]. It consists of 9 items and evaluates the physical activity reported in the last 7 days. It allows a weighted estimate of total physical activity to be obtained from the activities reported per week. The level of physical activity was categorized as low, moderate, and high. It has been validated in Spanish-speaking populations and applied in a Latin American population [36].
Fear of COVID-19 Scale. This scale consists of seven items and is reliable and valid for assessing fear of COVID-19 among the general population. It has shown a Cronbach’s alpha coefficient of 0.82 [37]. In the present study, a score greater than 16.5 was used as a cut-off point to assume the presence of fear of COVID-19 [38]. An investigation of the psychometric properties of the Spanish version of the COVID-19 Fear Scale in a sample of the Peruvian population demonstrated adequate measurement properties in terms of both reliability and validity [39].
2.6. Statistical Analysis
Survey data were organized in Microsoft Windows Excel® and analyzed in Stata 16.1 (StataCorp LLC, College Station, TX, USA).
Descriptive statistics were used to identify sample characteristics. Categorical variables are described as frequencies and percentages, and continuous variables are described as mean (standard deviation) or median (range) values, as appropriate.
Results with p-values less than 0.05 were considered statistically significant. To evaluate the factors associated with the dependent variable (insomnia), we constructed simple and multiple regression models, estimated prevalence ratios (PRs) and 95% confidence intervals (95%CI), and used generalized linear models (GLM) with the Poisson distribution family, robust variance, and log-link function.
2.7. Ethical Considerations
The protocol of the present study was evaluated and approved by the Institutional Research Ethics Committee (CIEI) of the Universidad San Martin de Porres. Informed consent was obtained from each individual. Participation in the study was voluntary, without any form of coercion. The data were anonymous, coded, and confidential.
3. Results
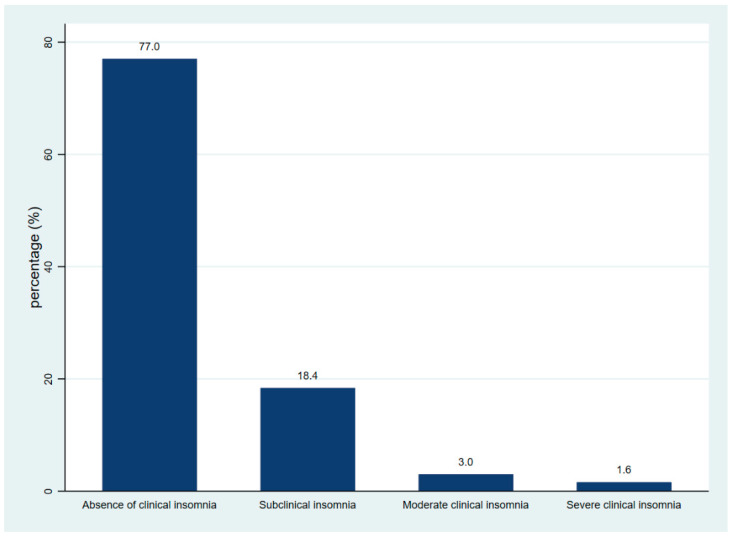
The median age was 22 years, with an age range of 19 to 31 years. The male sex predominated (95.8%, n = 503). A total of 26.5% (n = 139) reported having children. In relation to substance use, alcoholism and smoking were present in 17.1% (n = 90) and 6.7% (n = 35) of respondents, respectively. In relation to comorbidities, overweight was present in 33.3% (n = 172), 9.5% (n = 50) had hypertension, and 1.9% (n = 10) had diabetes. Physical activity was high in 80.0% (n = 424), and working time was greater than 19 months in 36.3% (n = 186). Resilience was low in 56.4% (n = 296). Fear of COVID-19 was present in 19.2% (n = 101) of participants (Table 1). The prevalence of insomnia was 23% (95% CI: 19.56–26.66%). A detailed comparison of the severity of insomnia symptoms is shown in Figure 1.
Table 1.
Characteristics of study participants (n = 566).
| Characteristics | n (%) |
|---|---|
| Age | 22 (19–31) * |
| Sex | |
| Female | 22 (4.2) |
| Male | 503 (95.8) |
| Marital status | |
| Single | 390 (74.3) |
| Married | 117 (22.3) |
| Cohabitant | 12 (2.3) |
| Divorced | 6 (1.1) |
| Religion | |
| None | 80 (15.2) |
| Catholic | 359 (68.4) |
| Non-Catholic | 86 (16.4) |
| Parenting | 139 (26.5) |
| Alcoholism | 90 (17.1) |
| Smoking | 35 (6.7) |
| Comorbidities | |
| Hypertension | 50 (9.5) |
| Diabetes | 10 (1.9) |
| Body mass index | |
| Underweight/Normal | 312 (60.4) |
| Overweight | 172 (33.3) |
| Obesity | 33 (6.4) |
| Personal mental health history | |
| No | 518 (98.7) |
| Yes | 7 (1.3) |
| Family history of mental health | |
| No | 502 (95.6) |
| Yes | 23 (4.4) |
| Seeking mental health help | |
| No | 482 (91.8) |
| Yes | 43 (8.2) |
| Confidence in government to handle the pandemic | |
| Yes | 288 (54.9) |
| No | 237 (45.1) |
| Working time | |
| 1 to 6 months | 134 (26.2) |
| 7 to 12 months | 82 (16.0) |
| 13 to 18 months | 110 (21.5) |
| 19 months or more | 186 (36.3) |
| Food insecurity | |
| No | 265 (50.5) |
| Yes | 260 (49.5) |
| Physical activity | |
| Low | 64 (12.2) |
| Moderate | 37 (7.1) |
| High | 424 (80.8) |
| Eating behavior disorder | |
| No | 471 (89.7) |
| Yes | 54 (10.3) |
| Resilience | |
| Low | 296 (56.4) |
| High | 229 (43.6) |
| Fear scale | |
| No | 424 (80.8) |
| Si | 101 (19.2) |
| Insomnia | |
| Absence of clinical insomnia | 436 (77.0) |
| Subclinical insomnia | 104 (18.4) |
| Moderate clinical insomnia | 17 (3.0) |
| Severe clinical insomnia | 9 (1.6) |
* Median (25–75th percentile).
Figure 1.
Frequency of insomnia symptoms according to severity based on Insomnia Severity Index-7.
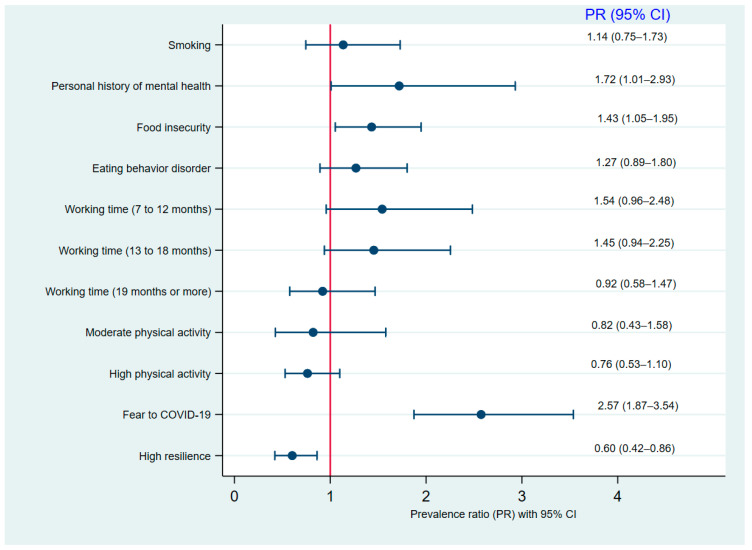
In the simple regression analysis (Table 2), a statistically significant association was identified between insomnia and the presence of smoking (PR: 1.86, 95% CI: 1.09–3.19), personal history of mental health (PR: 3.19, 95% CI: 1.95–5.23), work time from 7 to 12 months (PR: 1.63, 95% CI: 1.03–2.55) and 8 to 18 months (PR: 1.74, 95% CI: 1.15–2.64), food insecurity (PR: 1.44, 95% CI: 1.06–1.96), a high level of physical activity (PR: 0.63, 95% CI: 0.43–0.92), eating behavior disorder (PR: 2.18, 95% CI: 1.55–3.07), fear of COVID-19 (PR: 3.36, 95% CI: 2.50–4.50), and high resilience (PR: 0.48, 95% CI: 0.34–0.69). Likewise, in the multiple regression analysis (Figure 2), the prevalence of insomnia was higher in people who have had a personal history of mental health (PR: 1.71, 95% CI: 1.01–2.93), food insecurity (PR: 1.43, 95% CI: 1.05–1.95), and fear of COVID-19 (PR: 2.57, CI: 1.87–3.54). In contrast, the prevalence of insomnia was reduced by 40% in military personnel with a high level of resilience (PR: 0.60, 95% CI: 0.42–0.86).
Table 2.
Factors associated with insomnia in simple regression analysis.
| Characteristics | Insomnia | ||
|---|---|---|---|
| Simple Regression | |||
| PR | 95% CI | p * | |
| Age (years) | 0.99 | 0.97–1.00 | 0.146 |
| Sex | |||
| Female | Ref. | ||
| Male | 0.95 | 0.49–1.84 | 0.877 |
| Single | |||
| No | Ref. | ||
| Yes | 1.43 | 0.97–2.09 | 0.068 |
| Religion | |||
| None | Ref. | ||
| Catholic | 1.16 | 0.72–1.86 | 0.547 |
| Non-Catholic | 1.42 | 0.82–2.47 | 0.21 |
| Parenting | 0.72 | 0.49–1.04 | 0.08 |
| Alcoholism | 1.31 | 0.92–1.87 | 0.138 |
| Smoking | 1.86 | 1.09–3.19 | 0.023 |
| Comorbidities | |||
| Hypertension | 1.26 | 0.79–2.00 | 0.319 |
| Diabetes | 1.6 | 0.72–3.56 | 0.247 |
| Body mass index | |||
| Underweight/Normal | Ref. | ||
| Overweight | 0.77 | 0.54–1.09 | 0.14 |
| Obesity | 1.07 | 0.61–1.89 | 0.81 |
| Personal history of mental health | |||
| No | Ref. | ||
| Yes | 3.19 | 1.95–5.23 | <0.001 |
| Family history of mental health | |||
| No | Ref. | ||
| Yes | 1.23 | 0.64–2.35 | 0.529 |
| Confidence in government to handle the pandemic | |||
| Yes | Ref. | ||
| No | 1.17 | 0.86–1.58 | 0.312 |
| Working time | |||
| 1 to 6 months | Ref. | ||
| 7 to 12 months | 1.63 | 1.03–2.55 | 0.035 |
| 13 to 18 months | 1.74 | 1.15–2.64 | 0.009 |
| 19 months or more | 0.78 | 0.49–1.25 | 0.304 |
| Food insecurity | |||
| No | Ref. | ||
| Yes | 1.44 | 1.06–1.96 | 0.019 |
| Physical activity | |||
| Low | Ref. | ||
| Moderate | 0.6 | 0.29–1.21 | 0.151 |
| High | 0.63 | 0.43–0.92 | 0.017 |
| Eating behavior disorder | |||
| No | Ref. | ||
| Yes | 2.18 | 1.55–3.07 | <0.001 |
| Fear of COVID-19 | |||
| No | Ref. | ||
| Yes | 3.36 | 2.50–4.50 | <0.001 |
| Resilience | |||
| Low | Ref. | ||
| High | 0.48 | 0.34–0.69 | <0.001 |
* p-values obtained with generalized linear models, Poisson family, log-link function, and robust variance. Significant p-values are highlighted in bold.
Figure 2.
Forest plot of the factors associated with insomnia in multiple regression analysis.
4. Discussion
4.1. Prevalence of Insomnia
The prevalence of insomnia in the military was 23% during the second wave of the COVID-19 epidemic in Peru. This result is higher than that found in the general Mexican population (11.9%) [24]. However, a higher prevalence of insomnia was found in the general Argentine population (65.6%) [40]. These differences could be due to the times at which the surveys were measured, the characteristics of the population, and the difference in the instruments used. This may also be different due to particular factors in the military, such as post-traumatic stress disorder, increased risk of physical injury, and experience of traumatic events [21]. In addition, our result is higher than those reported in U.S. military members, who showed a prevalence of 11.5%, 16.3%, and 19.9% in pre-deployment military, veterans, and active military from three major services, respectively [41,42,43]. These differences could be explained by the fact that previous studies were conducted in the United States, in which there has been better control of the pandemic than in Peru. However, no similar studies have been found in Latin America, so it is suggested to increase the regional evidence to determine measures to prevent insomnia in military personnel.
4.2. Factors Associated with Insomnia
In this study, having a history of mental health problems increased the prevalence of insomnia by 72%. This result coincides with a study that reported that having a history of head injury and mental health outcomes increases the probability of developing insomnia [43]. Likewise, a systematic review showed that the combined outcome of four comorbidities increases the risk in active duty personnel by up to 53% [21]. This finding could be explained by the fact that sleep disorders such as insomnia may be due to a psychiatric disorder and may also predispose a serving military member to develop post-traumatic stress disorder and other psychiatric conditions [44].
Having food insecurity increased the prevalence of insomnia by 43%. However, we did not find a similar study that associated these variables. Nevertheless, it differs from what was found in a study conducted in young people, in which 11% had food insecurity, and they were more likely to have problems falling asleep and staying asleep [45]. A similar situation was observed in a study that identified mental health outcomes and food insecurity in women, finding that food insecurity increased the risk of negative mental health symptoms [46]. The association that we found could be due to the fact that military personnel who have felt the effects of the economic impact of COVID-19 on their family basket probably experience excessive worry and high levels of stress, resulting in a lack of sleep [47].
Experiencing a high resilience pattern reduced the prevalence of insomnia by 40%. This situation supports the knowledge that attenuated stressor reactivity resulting from poor sleep quality reflects reduced resilience [48]. Our result is similar to a study that identified higher levels of insomnia in the group with low levels of resilience [43]. It should be noted that this study was conducted on a sample of military veterans. Likewise, the development of resilience as a measure of protection against mental health problems has been reported during the pandemic [22,49].
Fear of COVID-19 increased the prevalence of insomnia by 157%. This result is similar to that reported in Pakistani workers during the pandemic, in which fear of COVID-19 may be negatively associated with sleep quality [47]. This is similar to another study conducted in Bangladesh, in which fear of COVID-19 was found to be a significant predictor of sleep quality [50]. Our result coincides with a study conducted in university students that identified that the fear of contagion significantly influenced the development of insomnia in up to 32.9% [51]. It should be noted that these studies were not conducted in the military.
Military personnel in Peru have supported the containment of the epidemic waves of COVID-19 under the declaration of a national state of emergency. The measures applied consisted of supporting citizen security, which ensured compliance with the quarantine. Their participation contributed to reducing the number of COVID-19 infections and deaths [52]. However, greater exposure to pandemic-related events may have increased fear of contagion compared to the general population, contributing to increased rates of insomnia. We recommend that special attention be paid to potential predictors of insomnia in military personnel, the most important being the presence of an eating disorder and food insecurity. Appropriate agencies, through their welfare offices or mental health areas, should establish an ongoing assessment of the development of insomnia. In addition, adequate sleep quality programs should be implemented to reverse its consequences.
Our study has important strengths. We were able to obtain a large sample of the study population. Furthermore, the data were measured in person, which reduces measurement bias in the variables analyzed. Additionally, we used validated instruments to determine the severity of insomnia and other covariates influencing the dependent variable. However, the cross-sectional design of the primary study does not allow us to identify causal relationships between the study variables. In addition, it is not possible to generalize the results of this research to the entire population of interest, given that it captured data from military personnel from a single region of northern Peru. Finally, since the study is the result of a secondary data analysis, it was not possible to measure other important variables that may influence insomnia and sleep quality in the evaluated military personnel (e.g., post-traumatic stress disorder, combat and deployment experience, and number of traumatic events).
5. Conclusions
The prevalence of insomnia in Peruvian military personnel was higher than that in other military groups during the COVID-19 pandemic. However, more information is needed in this context to understand whether the pandemic significantly increased insomnia rates in the military. Special attention should be paid to the associated factors in order to focus interventions on vulnerable members. In addition, programs to promote good-quality sleep should be implemented. Our results contribute to the knowledge of insomnia in military personnel and to the potential implementation of policies to prevent its negative effects.
Acknowledgments
M.J.V.-G. was supported by the Fogarty International Center of the National Institutes of Mental Health (NIMH) under Award Number D43TW009343 and the University of California Global Health Institute.
Author Contributions
Conceptualization, M.J.V.-G. and C.K.P.-R.; methodology, M.J.V.-G.; formal analysis, M.J.V.-G. and J.P.Z.-V.; investigation, J.P.Z.-V., C.K.P.-R. and P.G.-E.; data curation, M.J.V.-G. and J.P.Z.-V.; writing—original draft preparation, J.P.Z.-V., C.K.P.-R. and P.G.-E.; writing—review and editing, J.P.Z.-V., P.G.-E. and M.J.V.-G.; supervision, M.J.V.-G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study analyzed a secondary database that collected data without identifiers and did not violate the integrity of the participants. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Research Ethics Committee of the Universidad San Martin de Porres-USMP (CIEI-USMP N°0269).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The dataset generated and analyzed during the current study is not publicly available because the ethics committee has not provided permission/authorization to publicly share the data but are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gutiérrez-Tudela J.W. La pandemia de la COVID-19 en el Perú: Análisis epidemiológico de la segunda ola. Rev. De La Soc. Peru. De Med. Interna. 2021;34:129. doi: 10.36393/spmi.v34i4.627. [DOI] [Google Scholar]
- 2.Hossain M.M., Sultana A., Purohit N. Mental Health Outcomes of Quarantine and Isolation for Infection Prevention: A Systematic Umbrella Review of the Global Evidence. Epidemiol. Health. 2020;42:e2020038. doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson K.L., Davis J.E., Corbett C.F. Sleep Quality: An Evolutionary Concept Analysis. Nurs. Forum. 2022;57:144–151. doi: 10.1111/nuf.12659. [DOI] [PubMed] [Google Scholar]
- 4.Chaput J.-P., Dutil C., Sampasa-Kanyinga H. Sleeping Hours: What Is the Ideal Number and How Does Age Impact This? Nat. Sci. Sleep. 2018;10:421–430. doi: 10.2147/NSS.S163071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buysse D.J. Insomnia. JAMA. 2013;309:706–716. doi: 10.1001/jama.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang S.X., Chen J. Scientific Evidence on Mental Health in Key Regions under the COVID-19 Pandemic—Meta-Analytical Evidence from Africa, Asia, China, Eastern Europe, Latin America, South Asia, Southeast Asia, and Spain. Eur. J. Psychotraumatol. 2021;12:2001192. doi: 10.1080/20008198.2021.2001192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Karaki G., Hallit S., Malaeb D., Kheir N., Sacre H., Salameh P., Hallit R. Prevalence and Factors Associated with Insomnia Among a Representative Sample of the Lebanese Population: Results of a Cross-Sectional Study. J. Epidemiol. Glob. Health. 2020;10:124–130. doi: 10.2991/jegh.k.200117.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aernout E., Benradia I., Hazo J.-B., Sy A., Askevis-Leherpeux F., Sebbane D., Roelandt J.-L. International Study of the Prevalence and Factors Associated with Insomnia in the General Population. Sleep Med. 2021;82:186–192. doi: 10.1016/j.sleep.2021.03.028. [DOI] [PubMed] [Google Scholar]
- 9.Guo J., Yang L., Xu Y., Zhang C., Luo X., Liu S., Yao L., Bai H., Zong X., Zhang J., et al. Prevalence and Risk Factors Associated with Insomnia Symptoms Among the Chinese General Public After the Coronavirus Disease 2019 Epidemic Was Initially Controlled. Nat. Sci. Sleep. 2021;13:703–712. doi: 10.2147/NSS.S307996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Capaldi V.F., Kim J.R., Grillakis A.A., Taylor M.R., York C.M. Insomnia in the Military: Application and Effectiveness of Cognitive and Pharmacologic Therapies. Curr. Psychiatry Rep. 2015;17:85. doi: 10.1007/s11920-015-0622-9. [DOI] [PubMed] [Google Scholar]
- 11.Watson N.F., Badr M.S., Belenky G., Bliwise D.L., Buxton O.M., Buysse D., Dinges D.F., Gangwisch J., Grandner M.A., Kushida C., et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843–844. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller N.L., Shattuck L.G. Sleep Patterns of Young Men and Women Enrolled at the United States Military Academy: Results from Year 1 of a 4-Year Longitudinal Study. Sleep. 2005;28:837–841. doi: 10.1093/sleep/28.7.837. [DOI] [PubMed] [Google Scholar]
- 13.Caldwell J.A., Knapik J.J., Lieberman H.R. Trends and Factors Associated with Insomnia and Sleep Apnea in All United States Military Service Members from 2005 to 2014. J. Sleep Res. 2017;26:665–670. doi: 10.1111/jsr.12543. [DOI] [PubMed] [Google Scholar]
- 14.Moore B.A., Tison L.M., Palacios J.G., Peterson A.L., Mysliwiec V. Incidence of Insomnia and Obstructive Sleep Apnea in Active Duty United States Military Service Members. Sleep. 2021;44:zsab024. doi: 10.1093/sleep/zsab024. [DOI] [PubMed] [Google Scholar]
- 15.Mysliwiec V., Gill J., Lee H., Baxter T., Pierce R., Barr T.L., Krakow B., Roth B.J. Sleep Disorders in US Military Personnel: A High Rate of Comorbid Insomnia and Obstructive Sleep Apnea. Chest. 2013;144:549–557. doi: 10.1378/chest.13-0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Zambotti M., Goldstone A., Colrain I.M., Baker F.C. Insomnia Disorder in Adolescence: Diagnosis, Impact, and Treatment. Sleep Med. Rev. 2018;39:12–24. doi: 10.1016/j.smrv.2017.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erickson E.A., Stahlman S., McNellis M.G. Insomnia and Motor Vehicle Accident-Related Injuries, Active Component, U.S. Armed Forces, 2007–2016. MSMR. 2017;24:2–11. [PubMed] [Google Scholar]
- 18.Lewis P.E., Emasealu O.V., Rohrbeck P., Hu Z. Risk of Type II Diabetes and Hypertension Associated with Chronic Insomnia among Active Component, U.S. Armed Forces, 1998–2013. MSMR. 2014;21:6–13. [PubMed] [Google Scholar]
- 19.Tucker R.P., Cramer R.J., Langhinrichsen-Rohling J., Rodriguez-Cue R., Rasmussen S., Oakey-Frost N., Franks C.M., Cunningham C.C.A. Insomnia and Suicide Risk: A Multi-Study Replication and Extension among Military and High-Risk College Student Samples. Sleep Med. 2021;85:94–104. doi: 10.1016/j.sleep.2021.06.032. [DOI] [PubMed] [Google Scholar]
- 20.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., et al. Mental Health Care for Medical Staff in China during the COVID-19 Outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang Y., Xu J., Zheng S., Xu S., Wang Y., Du J., Xiao L., Zhang R., Wang H., Tang Y., et al. The risk factors for insomnia and sleep-disordered breathing in military communities: A meta-analysis. PLoS ONE. 2021;16:e0250779. doi: 10.1371/journal.pone.0250779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hill M.L., Nichter B., Na P.J., Norman S.B., Morland L.A., Krystal J.H., Pietrzak R.H. Mental Health Impact of the COVID-19 Pandemic in U.S. Military Veterans: A Population-Based, Prospective Cohort Study. Psychol. Med. 2021;52:1–12. doi: 10.1017/S0033291721002361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pietrzak R.H., Tsai J., Southwick S.M. Association of Symptoms of Posttraumatic Stress Disorder with Posttraumatic Psychological Growth Among US Veterans During the COVID-19 Pandemic. JAMA Netw. Open. 2021;4:e214972. doi: 10.1001/jamanetworkopen.2021.4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodríguez-Hernández C., Medrano-Espinosa O., Hernández-Sánchez A., Rodríguez-Hernández C., Medrano-Espinosa O., Hernández-Sánchez A. Salud mental de los mexicanos durante la pandemia de COVID-19. Gac. Médica De México. 2021;157:228–233. doi: 10.24875/GMM.20000612. [DOI] [PubMed] [Google Scholar]
- 25.Sierra J.C., Guillén-Serrano V., Santos-Iglesias P. Insomnia Severity Index: Some indicators about its reliability and validity on an older adults sample. Rev. Neurol. 2008;47:566–570. [PubMed] [Google Scholar]
- 26.Fernandez-Mendoza J., Rodriguez-Muñoz A., Vela-Bueno A., Olavarrieta-Bernardino S., Calhoun S.L., Bixler E.O., Vgontzas A.N. The Spanish Version of the Insomnia Severity Index: A Confirmatory Factor Analysis. Sleep Med. 2012;13:207–210. doi: 10.1016/j.sleep.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 27.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an Outcome Measure for Insomnia Research. Sleep Med. 2001;2:297–307. doi: 10.1016/S1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 28.García-León M.-Á., González-Gómez A., Robles-Ortega H., Padilla J.-L., Peralta-Ramírez M.-I., García-León M.-Á., González-Gómez A., Robles-Ortega H., Padilla J.-L., Peralta-Ramírez M.-I. Propiedades Psicométricas de La Escala de Resiliencia de Connor y Davidson (CD-RISC) En Población Española. An. De Psicol. 2019;35:33–40. doi: 10.6018/analesps.35.1.314111. [DOI] [Google Scholar]
- 29.Karaırmak O. Establishing the Psychometric Qualities of the Connor-Davidson Resilience Scale (CD-RISC) Using Exploratory and Confirmatory Factor Analysis in a Trauma Survivor Sample. Psychiatry Res. 2010;179:350–356. doi: 10.1016/j.psychres.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 30.Leiva León N.F. La Resilencia Como Factor Asociado al SINDROME de Burnout, Depresión y Ansiedad en el Personal de Salud que Labora en las Unidades de Cuidados Intensivos Durante la Pandemia COVID-19 en el Perú. 2021. [(accessed on 23 February 2022)]. Available online: https://repositorio.upch.edu.pe/handle/20.500.12866/8964.
- 31.Vargas Puello V., Alvarado Orellana S., Atalah Samur E. Inseguridad Alimentaria En Adultos Mayores En 15 Comunas Del Gran Santiago: Un Tema Pendiente. Nutr. Hosp. 2013;28:1430–1437. doi: 10.3305/nh.2013.28.5.6663. [DOI] [PubMed] [Google Scholar]
- 32.Hamedi-Shahraki S., Mir F., Amirkhizi F. Food Insecurity and Cardiovascular Risk Factors among Iranian Women. Ecol. Food Nutr. 2021;60:163–181. doi: 10.1080/03670244.2020.1812596. [DOI] [PubMed] [Google Scholar]
- 33.Constaín G.A., Ricardo Ramírez C., Rodríguez-Gázquez M. de los Á.; Álvarez Gómez, M.; Marín Múnera, C.; Agudelo Acosta, C. Validez y utilidad diagnóstica de la escala EAT-26 para la evaluación del riesgo de trastornos de la conducta alimentaria en población femenina de Medellín, Colombia. Aten Primaria. 2014;46:283–289. doi: 10.1016/j.aprim.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Constaín G.A., Rodríguez-Gázquez M. de los Á.; Ramírez Jiménez, G.A.; Gómez Vásquez, G.M.; Mejía Cardona, L.; Cardona Vélez, J. Validez y utilidad diagnóstica de la escala Eating Attitudes Test-26 para la evaluación del riesgo de trastornos de la conducta alimentaria en población masculina de Medellín, Colombia. Atención Primaria. 2017;49:206–213. doi: 10.1016/j.aprim.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mantilla Toloza S.C., Gómez-Conesa A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iberoam Fisioter Kinesiol. 2007;10:48–52. doi: 10.1016/S1138-6045(07)73665-1. [DOI] [Google Scholar]
- 36.Limb E.S., Ahmad S., Cook D.G., Kerry S.M., Ekelund U., Whincup P.H., Victor C.R., Iliffe S., Ussher M., Fox-Rushby J., et al. Measuring Change in Trials of Physical Activity Interventions: A Comparison of Self-Report Questionnaire and Accelerometry within the PACE-UP Trial. Int. J. Behav. Nutr. Phys. Act. 2019;16:10. doi: 10.1186/s12966-018-0762-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020;20:1537–1545. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nikopoulou V.A., Holeva V., Parlapani E., Karamouzi P., Voitsidis P., Porfyri G.N., Blekas A., Papigkioti K., Patsiala S., Diakogiannis I. Mental Health Screening for COVID-19: A Proposed Cutoff Score for the Greek Version of the Fear of COVID-19 Scale (FCV-19S) Int. J. Ment. Health Addict. 2022;20:907–920. doi: 10.1007/s11469-020-00414-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huarcaya-Victoria J., Villarreal-Zegarra D., Podestà A., Luna-Cuadros M.A. Psychometric Properties of a Spanish Version of the Fear of COVID-19 Scale in General Population of Lima, Peru. Int. J. Ment. Health Addict. 2022;20:249–262. doi: 10.1007/s11469-020-00354-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Valiensi S.M., Folgueira A.L., Garay A. Early Impact on Sleep and Mental Health during the Mandatory Social Isolation of COVID-19 Outbreak: An Obser Vational Cross-Sectional Study Carried out in Argentina. Sleep Sci. 2022;15:41–48. doi: 10.5935/1984-0063.20200121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCarthy E., DeViva J.C., Na P.J., Pietrzak R.H. New-Onset and Exacerbated Insomnia Symptoms during the COVID-19 Pandemic in US Military Veterans: A Nationally Representative, Prospective Cohort Study. J. Sleep Res. 2022;31:e13450. doi: 10.1111/jsr.13450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Markwald R.R., Carey F.R., Kolaja C.A., Jacobson I.G., Cooper A.D., Chinoy E.D. Prevalence and Predictors of Insomnia and Sleep Medication Use in a Large Tri-Service US Military Sample. Sleep Health. 2021;7:675–682. doi: 10.1016/j.sleh.2021.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Taylor D.J., Pruiksma K.E., Hale W.J., Kelly K., Maurer D., Peterson A.L., Mintz J., Litz B.T., Williamson D.E. Prevalence, Correlates, and Predictors of Insomnia in the US Army Prior to Deployment. Sleep. 2016;39:1795–1806. doi: 10.5665/sleep.6156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Good C.H., Brager A.J., Capaldi V.F., Mysliwiec V. Sleep in the United States Military. Neuropsychopharmacology. 2020;45:176–191. doi: 10.1038/s41386-019-0431-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nagata J.M., Palar K., Gooding H.C., Garber A.K., Whittle H.J., Bibbins-Domingo K., Weiser S.D. Food Insecurity Is Associated with Poorer Mental Health and Sleep Outcomes in Young Adults. J. Adolesc. Health. 2019;65:805–811. doi: 10.1016/j.jadohealth.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maynard M., Andrade L., Packull-McCormick S., Perlman C.M., Leos-Toro C., Kirkpatrick S.I. Food Insecurity and Mental Health among Females in High-Income Countries. Int. J. Environ. Res. Public Health. 2018;15:E1424. doi: 10.3390/ijerph15071424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clercq D.D., Haq I.U., Azeem M.U., Khalid S. The Link between Fear about COVID-19 and Insomnia: Mediated by Economic Concerns and Psychological Distress, Moderated by Mindfulness. J. Manag. Organ. 2021;28:1–19. doi: 10.1017/jmo.2021.3. [DOI] [Google Scholar]
- 48.Hansen D.A., Satterfield B.C., Layton M.E., Van Dongen H.P.A. Sleep Deprivation and Sleep-Onset Insomnia Are Associated with Blunted Physiological Reactivity to Stressors. Mil. Med. 2021;186:246–252. doi: 10.1093/milmed/usaa464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Di Trani M., Mariani R., Ferri R., De Berardinis D., Frigo M.G. From Resilience to Burnout in Healthcare Workers During the COVID-19 Emergency: The Role of the Ability to Tolerate Uncertainty. Front. Psychol. 2021;12:646435. doi: 10.3389/fpsyg.2021.646435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Siddique R.F., Ahmed O., Hossain K.N. Relationship between the Fear of COVID-19 Disease and Sleep Quality: The Mediating Role of Stress. Heliyon. 2021;7:e07033. doi: 10.1016/j.heliyon.2021.e07033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vilca L.W., Chávez B.V., Fernández Y.S., Caycho-Rodríguez T., White M. Impact of the Fear of Catching COVID-19 on Mental Health in Undergraduate Students: A Predictive Model for Anxiety, Depression, and Insomnia. Curr. Psychol. 2022:1–8. doi: 10.1007/s12144-021-02542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Presidencia de la Republica Jefe de Estado: Labor Sacrificada y Heroica de Las Fuerzas Armadas Es Fundamental Para Reducir Las Cifras de Contagios y Fallecimientos Por COVID-19. [(accessed on 14 June 2022)]. Available online: https://www.gob.pe/institucion/presidencia/noticias/304332-jefe-de-estado-labor-sacrificada-y-heroica-de-las-fuerzas-armadas-es-fundamental-para-reducir-las-cifras-de-contagios-y-fallecimientos-por-covid-19.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and analyzed during the current study is not publicly available because the ethics committee has not provided permission/authorization to publicly share the data but are available from the corresponding author on reasonable request.