Abstract
Diagnostic delays (time from the first symptoms to diagnosis) are common in inflammatory bowel disease (IBD) and may lead to worse disease progression and treatment outcomes. This study aimed to determine the duration of diagnostic delays (DD) and to explore associated factors in a cohort of children with IBD in New Zealand. In this study, patients with IBD diagnosed as children and their parents/caregivers completed questionnaires on the patients’ medical history, diagnostic experience, and demographic characteristics. The parent/caregiver questionnaire also included the Barriers to Care Questionnaire (BCQ). Patients’ healthcare data was reviewed to summarise the history of clinical visits and determine symptoms. Total DD, healthcare DD, patient DD and parent DD were derived from the primary dataset. Factors associated with the different types of DD were explored with a series of simple linear and logistical ordinal regressions. A total of 36 patients (Crohn’s disease 25, ulcerative colitis 10; male 17) were included. They were diagnosed at a median age of 12 years (interquartile range (IQR) 10–15 years). Total healthcare delay (from first healthcare visit to formal diagnosis) was median (IQR) 15.4 (6.5–34.2) months. The median (IQR) specialist-associated delay was 4.5 (0–34) days. Higher household income was associated with shorter healthcare delay (p < 0.018), while lower overall BCQ scores (indicating more barriers experienced) were associated with longer total healthcare DD. Higher scores in each subscale of BCQ (Skills; Pragmatics; Expectations; Marginalization; Knowledge and Beliefs) were also significantly associated with shorter total healthcare delay (p < 0.04). This study found substantial diagnostic delays in paediatric patients with IBD and identified significant associations between longer total healthcare diagnostic delays and overall household income and higher self-reported barriers to accessing healthcare.
Keywords: diagnostic delay, IBD, Crohn’s disease, ulcerative colitis, paediatric, children
1. Introduction
Inflammatory Bowel Diseases (IBD) are a group of chronic inflammatory conditions of the gastrointestinal tract. The two main types are Crohn’s disease (CD) and ulcerative colitis (UC) [1,2,3]. The aetiology of IBD is unclear, but they are typically characterized by the onset of a range of gastrointestinal symptoms such as abdominal pain, diarrhoea and haematochezia. Some individuals will present with more atypical symptoms, such as anaemia or extraintestinal manifestations [1,2,3,4,5]. The challenges of these diseases include variable disease course and severity of symptoms in addition to risk of surgery and side effects of medication, which can affect patients’ quality of life [5]. Due to atypical disease presentation such as extra intestinal symptoms, timely diagnosis is not always straightforward.
Individuals diagnosed with IBD may have variable duration of symptoms prior to the diagnosis, also known as diagnostic lag or diagnostic delay (DD). There are three types of DD—patient-associated delay, parent-associated delay and healthcare-associated delay. Potential reasons contributing to longer DD include poor health literacy and long waits due to limited resource availability [6]. Some studies have found that as many as ~20% of children are diagnosed 12 months or more after their symptoms first appear [4,7]. Similarly, other investigations found median delays between 2 months and 4.5 months, [7,8,9,10,11,12,13,14], while two additional reports [15,16] demonstrated delays as medians of over 8 months.
Prolonged DD poses ongoing disease burdens for the patient and potentially results in worse disease and treatment outcomes and lasting physical and psychological damage. Occult or uncontrolled inflammatory activity in children may lead to growth failure while also increasing the risk for the development of complicated disease that may prompt intestinal surgery [15,16]. In addition to physical consequences, prolonged unmanaged IBD symptoms may translate to lost school days, decreased self-esteem and increasing social isolation that may have long-lasting effects [17].
The increasing incidence of IBD worldwide pressures healthcare systems to meet the needs of the increasing number of patients with IBD [18]. Increasing rates of IBD have been noted in children in New Zealand [19,20]. Reducing the DD could be one way of decreasing this burden [3]. No studies have estimated DD in the New Zealand paediatric population, and, to our knowledge, no in-depth studies have been conducted to investigate the barriers to timely IBD diagnosis in children. The aims of this study were to (i) estimate the total DD in children in New Zealand; (ii) determine what proportion of the DD is attributed to patient-associated delay and healthcare-associated delay; and (iii) explore the underlying demographic and socioeconomic factors associated with DD.
2. Materials and Methods
2.1. Study Sample
Study participants were recruited from a regional Southern District Health Board (SDHB) IBD database “Episoft” (Sydney, Australia) and South Island paediatric IBD patient database [21]. Patients known to have been diagnosed with IBD before their 18th birthday were mailed invitations to participate in the study. The package included study information, consent forms and the study questionnaires in paper (TeleForm, version 16.2, 2017, OpenText, ON, Canada) and a link to an online version (REDCap, version 10.1.12, Vanderbilt University, Nashville, TN, USA) for the patients and their parents/caregivers [22,23]. Prepaid return envelopes were included. Patients who did not respond within a month from the initial contact were mailed a second invitation package and/or were contacted via phone or email.
2.2. Study Questionnaries
Study questionnaires were designed by an interdisciplinary research team and included questions on the timing and type of the first IBD symptoms, reasons for delays in notifying healthcare providers, the experience of the diagnostic process and any treatment methods sought.
The parent/caregiver questionnaire also included the Barriers to Care Questionnaire (BCQ) [24] that has been validated in children with chronic illness and special healthcare needs [25]. The BCQ questionnaire consists of five subscales, namely: skills, pragmatics, expectations, marginalisation and knowledge and beliefs (further detailed in the original publication). The BCQ total scale and each of the subscales is scored 0–100, with higher scores being indicative of lower experienced barriers to utilise healthcare [24].
The data from completed paper questionnaires were transferred to a Microsoft Excel spreadsheet using data collection program TeleForm (version 16.2, 2017, OpenText, Waterloo, ON, Canada), and all the entries were manually curated. Responses from paper questionnaires and REDCap were merged in the Excel sheet.
2.3. Healthcare Data
All available healthcare data from up to three years before the formal diagnosis date were reviewed for the consented patients (Figure 1). These data included records from the SDHB database (Health Connect South), general practitioners’ clinical databases and the Southern Community Laboratories’ (SCL) database.
One member of the research team (BSK) extracted information on all the potentially relevant clinical visits for each patient in the pre-diagnostic period. Clinical visits were considered potentially relevant if they reported symptoms indicative of IBD. Data extractions were conducted in consultation with two gastroenterologists (AD and MS) and further reviewed by KA for consistency.
2.4. Data Extraction
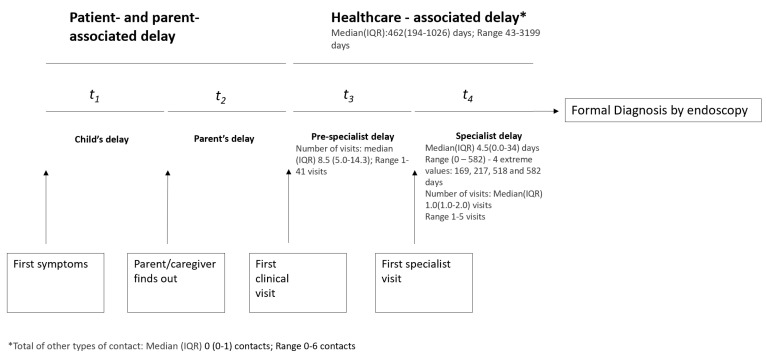
Time points of interest extracted from the healthcare data, patient and parent questionnaires are summarised in Table A1. The data of interest included the patients’ healthcare visits from the first symptoms to formal diagnoses (Figure 2). Formal diagnosis was defined as the endoscopy date. The following variables were derived:
Patient-associated delay: Time from the first symptoms to notifying parent/caregiver.
Parent-associated delay: Time from parents noticing the symptoms to seeking healthcare.
- Healthcare delay: From the first clinical visit to formal diagnosis.
-
a.Pre-specialist delay: First healthcare visit to specialist visit/formal diagnosis.
-
b.Specialist delay: Time from the first specialist visit to formal diagnosis.
-
a.
Total DD: From first symptoms (as reported by the patient/parent) to formal diagnosis of disease.
Number of clinical contacts: Number of in-person visits to health professional with complaints related to the IBD diagnosis were counted. Additional forms of contact, such as phone calls, emails and others were counted separately. The number of hospitalisations was also counted for each participant.
2.5. Statistical Analysis
Descriptive statistics were derived to summarise the demographic features, key disease symptoms, DD and associated barriers’ data. Measures of central tendency were set as mean and median, while variability was defined as standard deviation (SD) and 25th to 75th percentile (IQR), respectively. These measures were derived for the continuous data and proportions for the categorical data. Series of simple linear regressions were performed to model the effects of relevant variables on the total healthcare DD (continuous estimate from healthcare data) (Table A4). Logistic ordinal regression was used to model the patient- and parent-associated DD (categorical responses in the questionnaire). Explanatory variables for the models were derived from the available literature and based on the clinical experience of the research team. Multiple adjustment was not performed due to the exploratory nature of the study and the small sample size. All the analyses were performed using the statistical programming language R [26]. Statistical significance was defined as p < 0.05, but findings approaching significance were reported for the sake of completeness.
3. Results
3.1. Data Summary
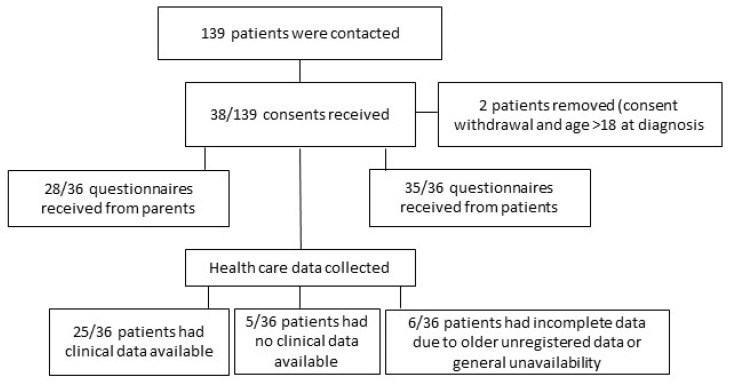
A total of 38 (27%) of the 139 invited patients consented to participation in the study (Figure 1). One of the 38 subjects did not complete the study questionnaire, and one was excluded as the patient was diagnosed after their 18th birthday, making a final study number of 36. A total of 9 questionnaires were completed on REDCap and 27 on paper; 28 parents/caregivers of the 36 participating patients with IBD completed the parent/caregiver questionnaire (5 via REDCap and 23 on paper).
Figure 1.
Study participation and the responses received.
3.2. Study Sample
The majority of patients (33/35) stated their ethnicity as New Zealand European, while a minority of Asian (1/35), Middle Eastern/Latin American/African (1/35) and Mixed Māori and European (2/33) were also represented. The included patients were diagnosed at a median (IQR) 12 (10–15) years of age with either CD (n = 25) or UC (n = 10) (Table 1). The median (IQR) time since diagnosis (at the point of study) was 9.5 (4–12) years.
Table 1.
Demographic characteristics of study participants (patients with inflammatory bowel disease and their parents/caregivers).
| Patient Characteristics | % (n) |
|---|---|
| Age at the time of the study, years | |
| Median (IQR) | 22 (15–28) |
| Range | 8–72 |
| Time since diagnosis *, years | |
| Median (IQR) | 9.5 (4–12) |
| Range | 0–59 |
| Age at diagnosis, years | |
| Median (IQR) | 12 (10–15) |
| Range | 0–17 years |
| Sex, male | 47 (17/36) |
| Ethnicity | |
| NZ European ** | 94 (33/35) |
| Asian | 3 (1/35) |
| MELAA (Middle Eastern/Latin American/African) | 3 (1/35) |
| Mixed Māori and European | 6 (2/33) |
| Diagnosis | |
| Crohn’s disease | 71 (25/35) |
| Ulcerative Colitis | 29 (10/35) |
| Parent/caregiver characteristics | % (n) |
| Ethnicity | |
| NZ European | 89 (25/28) |
| Other European | 7 (2/28) |
| MELAA (Middle Eastern/Latin American/African) | 4 (1/28) |
| Highest level of education in the household (at the time of diagnosis) | |
| High school or less | 18 (5/28) |
| Apprenticeship or advanced | 54 (15/28) |
| University degree | 29 (8/28) |
| Employment (at the time of diagnosis) | |
| Both employed | 3 (10/28) |
| One employed | 25 (7/28) |
| None employed | 0 (0/28) |
| At least one employed (only info from one parent) | 39 (11/28) |
| Income *** (at the time of diagnosis) | |
| Below average | 21 (6/28) |
| Middle | 54 (15/28) |
| Above average | 25 (7/28) |
Some missing data for one patient, hence the different denominators for Ethnicity and Diagnosis summary statistics. * In time since diagnosis, only 2 patients were diagnosed 40 and 59 years ago. ** Out of whom 1/33 were of mixed Asian ethnicity. *** Average income at the time of the study in New Zealand was NZD 100.103 according to: https://www.stats.govt.nz/information-releases/household-income-and-housing-cost-statistics-year-ended-june-2017 (accessed on 1 February 2020).
3.3. Healthcare-Associated Diagnostic Delays
Data from 28 of the 36 patients were available for healthcare delay analysis. For these patients, the total healthcare delay was a median (IQR) 15.4 (6.5–34.2) months with a full range of 1.4–107 months. Within the healthcare delay, the median (IQR) specialist-associated delay was 4.5 (0–34) days. The specialist delay estimates included four extreme values of 169, 217, 518 and 582 days. Over these periods, the study participants had a median (IQR) of 9 (5–14) healthcare visits prior to seeing a specialist (range 1–41 visits) and a median (IQR) of 1 (1–2) specialist visits before their diagnosis with IBD (range 1–5 visits) (Figure 2).
Figure 2.
Diagnostic delay timeline and the variables of interest.
3.4. Patient-Associated Delays
Although the largest proportion of patients (n = 8/33) waited one to four weeks to inform someone about their symptoms, some (n = 3/33) took more than a year. Most of the patients (n = 28/33) reported their initial symptoms to their parent or caregiver, subsequent to which the majority (n = 28/33) saw a general practitioner (GP) or family doctor as their first healthcare visit (Table 2).
Table 2.
Patient questionnaire: IBD symptoms and reporting prior to diagnosis (n = 35).
| Question | % (n) |
|---|---|
| What were your initial symptoms? (multiple choices possible) | |
| Abdominal pain | 74 (26/35) |
| Diarrhoea | 69 (24/35) |
| Tiredness | 63 (22/35) |
| Blood in stool | 60 (21/35) |
| Weight loss | 54 (19/35) |
| Nausea | 26 (9/35) |
| Vomiting | 23 (8/35) |
| Pus in stool | 11 (4/35) |
| Constipation | 9 (3/35) |
| Fever | 6 (2/35) |
| How long after you first noticed symptoms did you tell someone? | |
| Less than a week | 18 (6/33) |
| 1 week to less than 1 month | 24 (8/33) |
| 1 month to less than 2 months | 15 (5/33) |
| 2 months to less than 1 years | 15 (5/33) |
| More than 1 year | 9 (3/33) |
| Do not know/ remember | 18 (6/33) |
| Who did you tell first about the symptoms? | |
| Parent/caregiver | 85 (28/33) |
| GP/family doctor | 6 (2/33) |
| Other—parents/caregivers noticed/the patient was an infant | 9 (3/33) |
| Which healthcare professional did you see first? | |
| GP/family doctor | 85 (28/33) |
| Multiple | 3 (1/33) |
| Emergency Department | 3 (1/33) |
| Do not know/remember | 9 (3/33) |
| Overall experience of the diagnostic process: | |
| Very good | 12 (4/33) |
| Good | 9 (3/33) |
| Neither good nor bad | 30 (10/33) |
| Bad | 24 (8/33) |
| Very bad | 9 (3/33) |
| Do not know/ remember | 15 (5/33) |
Full questionnaire responses were not available for 2 patients.
3.5. Parent-Associated Delays
A total of eighteen of the 28 parents surveyed reported having no prior knowledge about IBD and its symptoms (Table A3). Consistent with the patient questionnaire, most parents (n = 18/28) reported that they first became aware of their child’s symptoms when their child told them, and 21/28 contacted their GP as the first healthcare contact. The total score in the BCQ was a median (IQR) of 61 (48–74). The specific questionnaire scores are summarised in Table A5.
3.6. Healthcare Diagnostic Delays: Simple Linear Regression Analysis
Patients’ sex (p = 0.75) or type of IBD diagnosis (p = 0.66) did not predict the length of healthcare DD. Furthermore, the educational level of the parents/caregivers (p > 0.24) or their knowledge of IBD (p = 0.19) also did not predict the duration of the healthcare DD. However, above average household income predicted shorter healthcare DD when compared to lower than average household income. Those with above average income had a mean (SD) 79 (82) % shorter healthcare DD than those with below average income (p = 0.018).
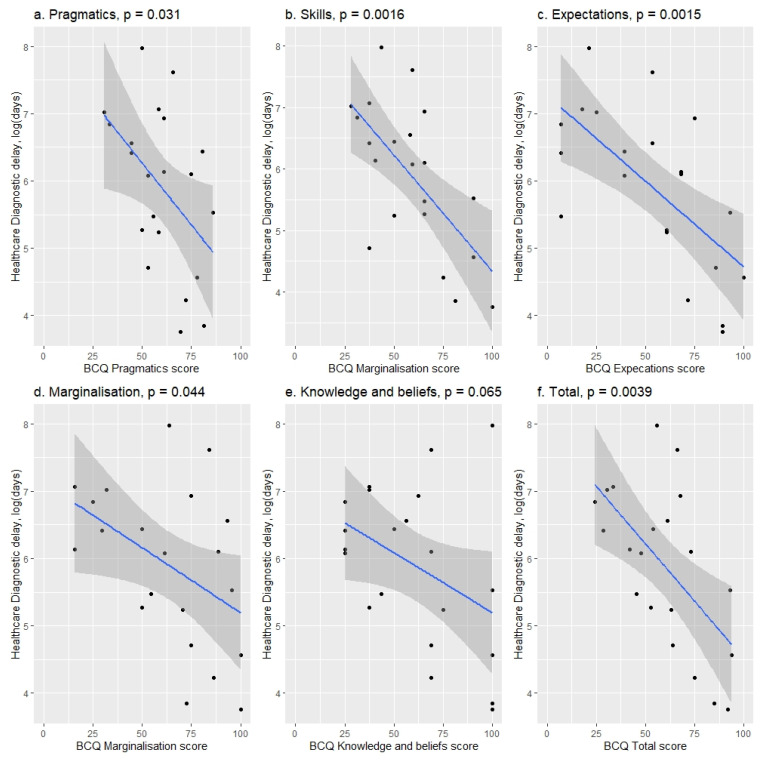
BCQ results were found to be predictive of the healthcare delay (Figure 3 and Table A4). Lower scores (indicating more barriers experienced) in skills (p = 0.0016), pragmatics (p = 0.031), expectations (p = 0.0015), marginalization (p = 0.044) and knowledge and beliefs (p = 0.0035) and the total BCQ score (p = 0.0024) were associated with longer healthcare delays. A 10-point increase in any of the subscales (scale 1–100) resulted in a mean (SD) 16 (9) % to 37 (10) % decrease in healthcare DD (depending on the subscale) (Table A4).
Figure 3.
BCQ subscales relation to total healthcare delay. Higher scores on each individual subscale in the BCQ questionnaire correspond to lower healthcare delay. Median (IQR) for each subscale: pragmatics, 61 (51–72); skills, 59 (44–70); expectations, 61 (38–73); marginalisation, 66 (48–85); knowledge and beliefs, 63 (41–72).
The dataset contained two extreme healthcare delay values of over five years. The analyses were performed with the complete dataset and with exclusion of the two extreme cases. The findings were consistent between the two datasets (Table A4).
3.7. Patient and Parent-Associated Delay: Logistic Ordinal Regression Outcomes
Female patients had a significantly higher risk of increased patient-associated DD (p = 0.032) (Table A2). Households with higher education had lower probability of longer patient-associated delay (p = 0.030) but not parent-associated delays (p = 0.12). Higher household income appeared to be associated with decreased risk of longer patient-associated DD (p = 0.06). Analysis did not identify any other predictors of patient- or parent-associated delays. A full summary of analysis outcomes is reported in (Table A2).
4. Discussion
This study involved an in-depth investigation of the nature and duration of diagnostic delays in individuals diagnosed with IBD in childhood in New Zealand and found substantial healthcare-, patient- and parent-associated delays. Factors that significantly influenced the healthcare-associated diagnostic delays in this cohort included household income, self-reported healthcare-utilisation knowledge, skills and pragmatics as captured by the BCQ questionnaire.
The length of total DD outlined in the current study exceeds delays from some previously published work, where median total DD was reported to be between 3 months and 4.5 months [7,8,9,10,11,12,13,14,27]. These articles all focused on paediatric patients in Western Europe except two that where from Canada [7] and Israel [11]. However, two other paediatric studies from Saudi Arabia and New Zealand reported substantially longer total DD with medians of two years and 8.4 months [28,29]. In contrast, specialist delays in the current study were considerably shorter than those described in a Spanish paediatric study by Jiménez et al. [10]. The pre-specialist delay of 15.3 months exceeds the findings in another paediatric report from Saudi Arabia of 8 months for CD and 5 months for UC [30]. The majority (75%) of the healthcare visits prior to seeing a diagnosing specialist were visits to a general practitioner (GP).
The total median (IQR) score in the Barriers to Care Questionnaire (BCQ) was 61 (48–74). It was found that a 10-point increase in any of the questionnaire subscales (which translates to fewer reported barriers) was associated with lower healthcare DD (16 (9)% to 37 (10)% depending on the specific subscale). While there are multiple factors implicated, this finding highlights an important set of systemic and patient-level barriers that result in worse clinical outcomes. Self-reported barriers such as pragmatics, feelings of marginalisation and health system knowledge and beliefs were all significantly associated with diagnostic delay outcomes. A recent study by Stamm et al. (2020) [31] found a low gastroenterologist count per population and gaps in gastroenterology specialist coverage across New Zealand. While Stamm et al. (2020) [31] did not focus on paediatric gastroenterology services, it captured an important systemic challenge associated with wide geographical dispersion of the population of New Zealand that could be expected to contribute to diagnostic delays. Similarly, Basu et al. (2019) [32] found referral delay in cancer patients associated with economic and geographical barriers to healthcare. It is important to highlight that a relatively small increase in BCQ score resulted in a substantial decrease in diagnostic delays, which may suggest some important targets for future interventions to decrease diagnostic delays in this patient population.
There are many reasons for DD, but accessible information, a user-friendly and intuitive healthcare system with ensured continuity of clinical care and easier access to healthcare could help decrease healthcare diagnostic delays [32,33]. Further studies are required to identify the most effective interventions to decrease these barriers.
The current study found that children from households with higher than average incomes had a shorter healthcare DD compared to those with lower than average incomes. This could be due to the patients from lower than average households facing more logistical obstacles, such as difficult access to healthcare or not having the same financial freedom to take time off for doctors’ visits. However, a recent Austrian study found no influence of household income on total DD [3]. It is important to highlight that direct comparisons between countries are complicated by differences in healthcare systems, economic and geographic factors, among others.
In the current study, 42% of the subjects waited less than one month before seeking help, while the same was true for 61% of the parents/caregivers seeking healthcare support for their children. These results are shorter than the patient-associated delay presented in Nahon et al. (2014) [30], who found a median (IQR) delay of 6 (1–24) months for CD and 2.4 (0.3–7) months for UC. In contrast to this, the patient-associated delay found in the current study is slightly longer than those reported by Treviño et al. (2020) [10], which found an overall median (IQR) of 13.8 (6.9–32.4) days.
A likely contributor to the length of DD could be the type and severity of the symptoms, with more atypical symptoms prolonging the time it takes to suspect a potential IBD diagnosis. For instance, patients with haematochezia had a shorter time to diagnosis than those without haematochezia in one report [34]. The current study also gathered detailed information on the type and character of symptoms at disease onset, both from medical records and from patients and their parents/caregivers. The most common symptoms reported by patients were abdominal pain, diarrhoea, tirednes, and blood in the stool. Patients who presented with atypical symptoms, such as muscle pain, joint pain or skin rash, had longer delays that included 8 to 33 healthcare visits. However, a detailed analysis on the type of symptoms and patient-/parent-associated DD was not conducted due to the small sample size.
The majority of the parents/caregivers became aware of their child’s symptoms when the child informed them. With younger children, parents/caregivers rely more on non-verbal communication explaining a possible association between younger age and longer healthcare DD. In contrast, older children are more independent and self-aware, which can delay the parents/caregivers’ awareness due to the nature of the symptoms. This trend of longer patient delay was also significant in female patients. Some patients specifically reported this in their responses to the questionnaires. An association between younger age and longer DD has been noted in some previous reports [35,36]. However, one report found no relationship between age at diagnosis and DD [37], while several reports have indicated longer DD in older patients [38,39,40].
The limitations to the study were first, potential recall bias in questionnaire responses since the included patients were diagnosed a median of 9.5 years prior to the study. However, the healthcare DD data were derived from clinical records, and should not be impacted by the time since diagnosis. Second, there is potential selection bias, as patients who had strong positive or negative experiences during their pre-diagnostic period could be more inclined to participate. Third, while the BCQ was validated in children with asthma [24,25], it has not been validated in patients with IBD. The strengths of the study include a detailed investigation incorporating clinical records and responses from, patients and parents/caregivers.
In conclusion, the current study identified long total and healthcare DD in children diagnosed with IBD in NZ and highlighted potential factors that impede timely diagnosis, including prolonged periods of DD before seeing a specialist. Future research is required on how to effectively address the barriers to timely diagnostic delay. Possible interventions could include enhancing modes of communication between GPs and specialists as well as fast track systems to enable prompt assessment of patients with suspected IBD [41].
Acknowledgments
Great appreciation is given to the General Practitioners in New Zealand who spent time retrieving and contributing data.
Appendix A
Table A1.
Definitions and data sources.
| Event of Interest (Dates) | Definition and Specification |
|---|---|
| First symptoms 1 | First IBD symptoms, as reported by the patient or their parent/caregiver. |
| First contact with parents/caregivers/other 1 | Defined as the first person the child presented the symptoms to, such as parent, caregiver, other family member. In case the patient went directly to a doctor this would be their first contact. |
| First healthcare contact 2 | First visit to a healthcare professional due to potential IBD symptoms. All obtained healthcare data were reviewed for the first presentation with the following symptoms as defined in [1,2] and Community Health pathways *:
|
| First relevant specialist visit 2 | First specialist that would make final diagnosis/start of treatment; in this study gastroenterologist. |
| Formal diagnosis 2 | IBD diagnosis confirmed by endoscopy |
| Patient-associated delay | Time from the first symptoms to notifying parent/caregiver |
| Parent-associated delay | Time from parents noticing the symptoms to seeking healthcare |
| Healthcare delay | From the first clinical visit to formal diagnosis |
| Total DD ** | From first symptoms (as reported by the patient/parent) to formal diagnosis of disease |
| Number of clinical contacts | Number of in-person visits to healthcare professional with complains related to the IBD diagnosis were counted. Additional forms of contact, such as phone calls, emails and other were counted separately. The number of hospitalisations was also counted for each participant. |
| Other types of contact | Contacts with healthcare professional not made in-person e.g., e-mail, phone call, text message. |
Data source: 1—Patient and parent questionnaires; 2—Healthcare notes. * Community Health pathways is an international collective of health and social care organisations that deliver reliable source of information to clinicians [42]. ** Diagnostic Delay.
Table A2.
Predictors for patient-associated and parent-associated delays. Logistic ordinal regression outcomes.
| Predictors | Outcome Variables | |||||
|---|---|---|---|---|---|---|
| Patient Delayb, n = 29 | Parent Delayb, n = 27 | |||||
| Coefficient Estimate (SD) |
p-Value | AIC Value | Coefficient Estimate (SD) |
p-Value | AIC Value | |
| Age at first symptomsa | OR: 0.96 (1.10) | 0.72 | 91.8 | OR: 0.97 (1.07) |
0.63 | 80.8 |
| Patient Sex b, baseline—Male | OR: 5.1 (2.1) | 0.032 * | 87.0 | OR: 0.74 (2.08) | 0.68 | 80.9 |
| Patient diagnosisb, base—Crohn’s | OR: 1.16 (2.1) | 0.84 | 91.9 | OR: 1.57 (2.63) | 0.64 | 80.8 |
| Highest level of education in the household at diagnosisb, baseline—no qualification | OR: 0.30 (1.74) | 0.030 * | 62.1 | OR: 0.48 (1.61) | 0.12 | 78.6 |
| Complete log | ||||||
| Apprenticeship or advanced training (level 4–6) | ||||||
| University degree | ||||||
| Household income at diagnosisb, baseline—below average | OR: 0.38 (1.7) | 0.060 | 63.7 | OR: 0.59 (1.78) | 0.34 | 80.1 |
| Complete log | ||||||
| Average | ||||||
| Above average | ||||||
| Parents/caregivers had prior knowledge of IBD before diagnosisb, baseline—no | - | - | - | OR: 2.70 (2.13) | 0.19 | 79.2 |
| Barriers to care Questionnaire | ||||||
| Skillsa | - | - | - | OR: 1.0 (1.0) | 0.40 | 78.4 |
| Pragmaticsa | - | - | - | OR: 1.0 (1.0) | 0.73 | 79.0 |
| Expectationsa | - | - | - | OR: 1.0 (1.0) | 0.81 | 79.1 |
| Marginalizationa | - | - | - | OR: 1.0 (1.0) | 0.65 | 78.9 |
| Knowledge and Beliefsa | - | - | - | OR: 1.0 (1.0) | 0.67 | 78.9 |
| Totala | - | - | - | OR: 1.0 (1.0) | 0.60 | 78.9 |
| Reservations to share symptoms by the patientb, no | OR: 0.99 (1.01) | 0.40 | 91.2 | - | - | - |
*—statistically significant results. a—continuous variable b—categorical variable. Abbreviations: OR—odds ratio; SD—standard deviation; AIC—Akaike Information Criterion.
Table A3.
Parent/caregiver questionnaire: Symptoms and disease course.
| Question | % (n) |
|---|---|
| How old was your child when their symptoms first occurred? | |
| 0–4 years | 30 (8/27) |
| 5–9 years | 4 (1/27) |
| 10–14 years | 52 (14/27) |
| 15–18 years | 15 (4/27) |
| How did you become aware of their symptoms? (multiple choices possible) | |
| My child told me | 64 (18/28) |
| School teachers or school nurses told me | 14 (4/28) |
| I noticed them myself | 54 (15/28) |
| Who did you contact first about the symptoms? | |
| GP | 75 (21/28) |
| Paediatrician | 4 (1/28) |
| Other: | 21 (6/28) |
| Plunket nurse | 7 (2/28) |
| Surgeon | 4 (1/28) |
| GP and Gastroenterologist | 4 (1/28) |
| GP and Paediatrician | 4 (1/28) |
| GP and Emergency department | 4 (1/28) |
| How long did you initially wait before seeking help from a healthcare professional? | |
| Less than a week | 36 (10/28) |
| 1 week—less than a month | 25 (7/28) |
| 1 month—less than 2 months | 7 (2/28) |
| 2 months—less than 6 months | 14 (4/28) |
| 6 months | 4 (1/28) |
| More than 1 year | 4 (1/28) |
| I do not know/remember | 11 (3/28) |
| Did you have any prior knowledge about IBD and its symptoms BEFORE your child experienced them? | |
| Yes | 14 (4/28) |
| No | 64 (18/28) |
| Some | 21 (6/28) |
No data available for 6 patients, hence the different denominators. GP; General Practitioner, n; number.
Table A4.
Predictors for total healthcare delay. Simple linear regression.
| Explanatory Variables | Outcome Variable—Total Healthcare Delay a, n = 26 | ||
|---|---|---|---|
| % Change (SD) | p-Value | Adj. R-Sq. Value | |
| Patient’s Age at first symptoms a | |||
| Complete log | −7 (4) % | 0.11 | 0.069 |
| Filtered log | −7 (4) % | 0.091 | 0.091 |
| Sex of the patient b, baseline male | |||
| Complete log | 17 (64) % | 0.75 | −0.039 |
| Filtered log | −17 (60) % | 0.70 | −0.040 |
| IBD diagnosis b, baseline Crohn’s disease | |||
| Complete log | 27 (70) % | 0.66 | −0.036 |
| Filtered log | −6 (71) % | 0.90 | −0.047 |
| Highest level of education in the household at diagnosis b, baseline—no qualification | |||
| Complete log | 0.0093 | ||
| Approximately average | 166 (123) % | 0.24 | |
| Above average | 16 (88) % | 1.0 | |
| Filtered log | 0.064 | ||
| Approximately average | 166 (109.4) % | 0.20 | |
| Above average | −17 (79.8) % | 0.76 | |
| Household income at diagnosis b, baseline—below average | |||
| Complete log | 0.31 | ||
| Average | −21 (65.6) % | 0.64 | |
| Above Average | −85 (82.5) % | 0.0059 ** | |
| Filtered log | 0.31 | ||
| Average | 6 (66.6) % | 0.91 | |
| Above Average | −79 (82.0) % | 0.018 * | |
| Parents/caregivers had prior knowledge of IBD before diagnosis b, baseline—no | |||
| Complete log | −52 (71.5) % | 0.19 | 0.037 |
| Filtered log | −43 (68.8) % | 0.27 | −0.015 |
| Barriers to Care Questionnaire | |||
|
Skills a
Complete log Filtered log |
|||
| −4 (1.0) % | 0.0016 ** | 0.39 | |
| −3 (0.99) % | 0.0023 ** | 0.38 | |
| Pragmatics a | |||
| Complete log | −4 (1.6) % | 0.031 * | 0.18 |
| Filtered log | −3 (1.5) % | 0.044 * | 0.16 |
| Expectations a | |||
| Complete log | −3 (0.69) % | 0.0015 ** | 0.39 |
| Filtered log | −2 (0.69) % | 0.0037 ** | 0.35 |
| Marginalisation a | |||
| Complete log | −2 (0.90) % | 0.044 * | 0.15 |
| Filtered log | −2 (0.91) % | 0.031 ** | 0.19 |
| Knowledge and Beliefs a | |||
| Complete log | −4 (2.1) % | 0.065 | 0.12 |
| Filtered log | −3 (0.78) % | 0.0035 *** | 0.35 |
| Total a | |||
| Complete log | −3 (1.0) % | 0.0039 *** | 0.33 |
| Filtered log | −3 (0.95) % | 0.0024 *** | 0.38 |
*, **, ***—statistically significant results. a—continuous variable; b—categorical variable. Complete log—refers to analysis with the complete data set and the outcome variable (diagnostic delay) log transformed in the simple linear regression model. Filtered log—refers to analysis with 2 extreme diagnostic delay values removed and the outcome variable (diagnostic delay) log transformed in the simple linear regression model.
Table A5.
Barriers to Care Questionnaire scores relation to healthcare diagnostic delays.
| Range and Median (IQR) for Individual BCQ Subscales, n = 27 | |
|---|---|
| Total Score | |
| Median (IQR) | 61 (48–74) |
| Range | 24–94 |
| Skills Score | |
| Median (IQR) | 59 (44–70) |
| Range | 28–100 |
| Pragmatics Score | |
| Median (IQR) | 61 (51–72) |
| Range | 31–86 |
| Expectations Score | |
| Median (IQR) | 61 (38–73) |
| Range | 7–100 |
| Marginalisation Score | |
| Median (IQR) | 66 (48–85) |
| Range | 16–100 |
| Knowledge & Beliefs Score | |
| Median (IQR) | 63 (41–72) |
| Range | 25–100 |
Abbreviations: IQR—interquartile range: 25th to 75th percentile; BCQ—Barriers to Care Questionnaire.
Author Contributions
Conceptualization, A.S.D., M.S. and K.A.; data curation, B.S.K. and K.A.; formal analysis, K.A.; funding acquisition, A.S.D.; investigation, B.S.K.; methodology, A.S.D. and K.A.; project administration, K.A.; resources, A.S.D., M.S. and K.A.; supervision, A.S.D., M.S. and K.A.; visualization, K.A.; writing—original draft, B.S.K. and K.A.; writing—review & editing, B.S.K., A.S.D., K.K., M.S. and K.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Human Ethics Committee of University of Otago (protocol code REF: H19/101, date: 22/07/2019).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
De-identified raw data will be made available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding. ASD’s research activities supported by Cure Kids. The APC was funded by Editorial Board allocation to ASD.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gomollón F., Dignass A., Annese V., Tilg H., Van Assche G., Lindsay J.O., Peyrin-Biroulet L., Cullen G.J., Daperno M., Kucharzik T., et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 1: Diagnosis and Medical Management. J. Crohn’s Colitis. 2017;11:3–25. doi: 10.1093/ecco-jcc/jjw168. [DOI] [PubMed] [Google Scholar]
- 2.Magro F., Gionchetti P., Eliakim R., Ardizzone S., Armuzzi A., Barreiro-de Acosta M., Burisch J., Gecse K.B., Hart A.L., Hindryckx P., et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J. Crohn’s Colitis. 2017;11:649–670. doi: 10.1093/ecco-jcc/jjx008. [DOI] [PubMed] [Google Scholar]
- 3.Austrian IBD Study Group (ATISG) Novacek G., Gröchenig H.P., Haas T., Wenzl H., Steiner P., Koch R., Feichtenschlager T., Eckhardt G., Mayer A., et al. Diagnostic delay in patients with inflammatory bowel disease in Austria. Wien. Klin. Wochenschr. 2019;131:104–112. doi: 10.1007/s00508-019-1451-3. [DOI] [PubMed] [Google Scholar]
- 4.Yu Y.R., Rodriguez J.R. Clinical presentation of Crohn’s, ulcerative colitis, and indeterminate colitis: Symptoms, extraintestinal manifestations, and disease phenotypes. Semin. Pediatric Surg. 2017;26:349–355. doi: 10.1053/j.sempedsurg.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Mikocka-Walus A., Knowles S.R., Keefer L., Graff L. Controversies Revisited: A Systematic Review of the Comorbidity of Depression and Anxiety with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2016;22:752–762. doi: 10.1097/MIB.0000000000000620. [DOI] [PubMed] [Google Scholar]
- 6.Rogala L., Miller N., Graff L.A., Rawsthorne P., Clara I., Walker J.R., Lix L., Ediger J.P., McPhail C., Bernstein C.N. Population-based controlled study of social support, self-perceived stress, activity and work issues, and access to health care in inflammatory bowel disease. Inflamm. Bowel Dis. 2008;14:526–535. doi: 10.1002/ibd.20353. [DOI] [PubMed] [Google Scholar]
- 7.Ricciuto A., Fish J.R., Tomalty D.E., Carman N., Crowley E., Popalis C., Muise A., Walters T.D., Griffiths A.M., Church P.C. Diagnostic delay in Canadian children with inflammatory bowel disease is more common in Crohn’s disease and associated with decreased height. Arch. Dis. Child. 2018;103:319–326. doi: 10.1136/archdischild-2017-313060. [DOI] [PubMed] [Google Scholar]
- 8.De Greef E., Mahachie John J.M., Hoffman I., Smets F., Van Biervliet S., Scaillon M., Hauser B., Paquot I., Alliet P., Arts W., et al. Profile of pediatric Crohn’s disease in Belgium. J. Crohn’s Colitis. 2013;7:e588–e598. doi: 10.1016/j.crohns.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 9.Gower-Rousseau C., Dauchet L., Vernier-Massouille G., Tilloy E., Brazier F., Merle V., Dupas J.-L., Savoye G., Baldé M., Marti R., et al. The Natural History of Pediatric Ulcerative Colitis: A Population-Based Cohort Study. Am. J. Gastroenterol. 2009;104:2080–2088. doi: 10.1038/ajg.2009.177. [DOI] [PubMed] [Google Scholar]
- 10.Jiménez Treviño S., Pujol Muncunill G., Martín-Masot R., Rodríguez Martínez A., Segarra Cantón O., Peña Quintana L., Armas Ramos H., Eizaguirre Arocena F.J., Barrio Torres J., García Burriel J.I., et al. Spanish Pediatric Inflammatory Bowel Disease Diagnostic Delay Registry: SPIDER Study from Sociedad Española de Gastroenterología, Hepatología y Nutrición Pediátrica. Front. Pediatr. 2020;8:584278. doi: 10.3389/fped.2020.584278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rinawi F., Assa A., Eliakim R., Mozer-Glassberg Y., Nachmias-Friedler V., Niv Y., Rosenbach Y., Silbermintz A., Zevit N., Shamir R. Risk of Colectomy in Patients with Pediatric-onset Ulcerative Colitis. J. Pediatric Gastroenterol. Nutr. 2017;65:410–415. doi: 10.1097/MPG.0000000000001545. [DOI] [PubMed] [Google Scholar]
- 12.Savoye G., Salleron J., Gower-Rousseau C., Dupas J.-L., Vernier-Massouille G., Fumery M., Merle V., Lerebours E., Cortot A., Turck D., et al. Clinical predictors at diagnosis of disabling pediatric Crohn’s disease. Inflamm. Bowel Dis. 2012;18:2072–2078. doi: 10.1002/ibd.22898. [DOI] [PubMed] [Google Scholar]
- 13.Schoepfer A., Santos J., Fournier N., Schibli S., Spalinger J., Vavricka S., Safroneeva E., Aslan N., Rogler G., Braegger C., et al. Systematic Analysis of the Impact of Diagnostic Delay on Bowel Damage in Paediatric Versus Adult Onset Crohn’s Disease. J. Crohn’s Colitis. 2019;13:1334–1342. doi: 10.1093/ecco-jcc/jjz065. [DOI] [PubMed] [Google Scholar]
- 14.Timmer A., Behrens R., Buderus S., Findeisen A., Hauer A., Keller K.-M., Kliemann G., Lang T., Lohr W., Rzehak P., et al. Childhood Onset Inflammatory Bowel Disease: Predictors of Delayed Diagnosis from the CEDATA German-Language Pediatric Inflammatory Bowel Disease Registry. J. Pediatrics. 2011;158:467–473.e2. doi: 10.1016/j.jpeds.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 15.Lee D., Koo J.S., Choe J.W., Suh S.J., Kim S.Y., Hyun J.J., Jung S.W., Jung Y.K., Yim H.J., Lee S.W. Diagnostic delay in inflammatory bowel disease increases the risk of intestinal surgery. World J. Gastroenterol. 2017;23:6474–6481. doi: 10.3748/wjg.v23.i35.6474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abraham B.P., Mehta S., El-Serag H.B. Natural history of pediatric-onset inflammatory bowel disease: A systematic review. J. Clin. Gastroenterol. 2012;46:581–589. doi: 10.1097/MCG.0b013e318247c32f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubinsky M. Special issues in pediatric inflammatory bowel disease. World J. Gastroenterol. 2008;14:413–420. doi: 10.3748/wjg.14.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coppell K.J., Galts C.P.-C., Huizing F.Y., Norton J.K., Gray A.R., Schultz K., Hobbs C.E., Aluzaite K., Schultz M. Annual Incidence and Phenotypic Presentation of IBD in Southern New Zealand: An 18-Year Epidemiological Analysis. Inflamm. Intest. Dis. 2018;3:32–39. doi: 10.1159/000492615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lopez R.N., Evans H.M., Appleton L., Bishop J., Chin S., Mouat S., Gearry R.B., Day A.S. Prospective Incidence of Paediatric Inflammatory Bowel Disease in New Zealand in 2015: Results from the Paediatric Inflammatory Bowel Disease in New Zealand (PINZ) Study. J. Pediatr. Gastroenterol. Nutr. 2018;66:e122–e126. doi: 10.1097/MPG.0000000000001806. [DOI] [PubMed] [Google Scholar]
- 20.Lopez R.N., Appleton L., Gearry R.B., Day A.S. Rising Incidence of Paediatric Inflammatory Bowel Disease in Canterbury, New Zealand, 1996–2015. J. Pediatr. Gastroenterol. Nutr. 2018;66:e45–e50. doi: 10.1097/MPG.0000000000001688. [DOI] [PubMed] [Google Scholar]
- 21.O’Neill J. IBD Database. EpiSoft. [(accessed on 25 May 2021)]. Available online: https://episofthealth.com/solutions-other-specialties/other-specialties-ibd-emr-01-scheduling/
- 22.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O’Neal L., McLeod L., Delacqua G., Delacqua F., Kirby J., et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seid M., Sobo E.J., Gelhard L.R., Varni J.W. Parents’ reports of barriers to care for children with special health care needs: Development and validation of the barriers to care questionnaire. Ambul. Pediatr. 2004;4:323–331. doi: 10.1367/A03-198R.1. [DOI] [PubMed] [Google Scholar]
- 25.Seid M., Opipari-Arrigan L., Gelhard L.R., Varni J.W., Driscoll K. Barriers to care questionnaire: Reliability, validity, and responsiveness to change among parents of children with asthma. Acad. Pediatr. 2009;9:106–113. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 26.R Core Team . R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2020. [Google Scholar]
- 27.Arcos-Machancoses J.V., Donat-Aliaga E., Polo-Miquel B., Masip-Simó E., Ribes-Koninckx C., Pereda-Pérez A. Description and study of risk factors for the diagnostic delay of paediatric inflammatory bowel disease. Anales de Pediatría. 2015;82:247–254. doi: 10.1016/j.anpedi.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 28.Saadah O.I., El Mouzan M., Al Mofarreh M., Al Edreesi M., Hasosah M., Al-Hussaini A., AlSaleem K. Characteristics of Pediatric Crohn’s Disease in Saudi Children: A Multicenter National Study. Gastroenterol. Res. Pract. 2016;2016:7403129. doi: 10.1155/2016/7403129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yap J., Wesley A., Mouat S., Chin S. Paediatric inflammatory bowel disease in New Zealand. N. Z. Med. J. 2008;121:17. [PubMed] [Google Scholar]
- 30.El Mouzan M., Al Saleem B., Hasosah M., Al-Hussaini A., Al Anazi A., Saadah O., Al Sarkhy A., Al Mofarreh M., Assiri A. Diagnostic delay of pediatric inflammatory bowel disease in Saudi Arabia. Saudi J. Gastroenterol. 2019;25:257. doi: 10.4103/sjg.SJG_457_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stamm R., Aluzaite K., Arnold M., Caspritz T., White C., Schultz M. Challenges for the future: The gastroenterology specialist workforce in New Zealand. N. Z. Med. J. 2020;133:9. [PubMed] [Google Scholar]
- 32.Basu A., Ghosh D., Mandal B., Mukherjee P., Maji A. Barriers and explanatory mechanisms in diagnostic delay in four cancers—A health-care disparity? South Asian J Cancer. 2019;8:221–225. doi: 10.4103/sajc.sajc_311_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walton L., McNeill R., Stevens W., Murray M., Lewis C., Aitken D., Garrett J. Patient perceptions of barriers to the early diagnosis of lung cancer and advice for health service improvement. Fam Pract. 2013;30:436–444. doi: 10.1093/fampra/cmt001. [DOI] [PubMed] [Google Scholar]
- 34.Nguyen V.Q., Jiang D., Hoffman S.N., Guntaka S., Mays J.L., Wang A., Gomes J., Sorrentino D. Impact of Diagnostic Delay and Associated Factors on Clinical Outcomes in a U.S. Inflammatory Bowel Disease Cohort: Inflamm. Bowel Dis. 2017;23:1825–1831. doi: 10.1097/MIB.0000000000001257. [DOI] [PubMed] [Google Scholar]
- 35.Zaharie R., Tantau A., Zaharie F., Tantau M., Gheorghe L., Gheorghe C., Gologan S., Cijevschi C., Trifan A., Dobru D., et al. Diagnostic Delay in Romanian Patients with Inflammatory Bowel Disease: Risk Factors and Impact on the Disease Course and Need for Surgery. J. Crohn’s Colitis. 2016;10:306–314. doi: 10.1093/ecco-jcc/jjv215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vavricka S.R., Spigaglia S.M., Rogler G., Pittet V., Michetti P., Felley C., Mottet C., Braegger C.P., Rogler D., Straumann A., et al. Systematic evaluation of risk factors for diagnostic delay in inflammatory bowel disease: Inflamm. Bowel Dis. 2012;18:496–505. doi: 10.1002/ibd.21719. [DOI] [PubMed] [Google Scholar]
- 37.Nahon S., Lahmek P., Lesgourgues B., Poupardin C., Chaussade S., Peyrin-Biroulet L., Abitbol V. Diagnostic delay in a French cohort of Crohn’s disease patients. J. Crohn’s Colitis. 2014;8:964–969. doi: 10.1016/j.crohns.2014.01.023. [DOI] [PubMed] [Google Scholar]
- 38.Maconi G., Orlandini L., Asthana A.K., Sciurti R., Furfaro F., Bezzio C., de Franchis R. The impact of symptoms, irritable bowel syndrome pattern and diagnostic investigations on the diagnostic delay of Crohn’s disease: A prospective study. Dig. Liver Dis. 2015;47:646–651. doi: 10.1016/j.dld.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 39.Li Y., Ren J., Wang G., Gu G., Wu X., Ren H., Hong Z., Hu D., Wu Q., Li G., et al. Diagnostic delay in Crohn’s disease is associated with increased rate of abdominal surgery: A retrospective study in Chinese patients. Dig. Liver Dis. 2015;47:544–548. doi: 10.1016/j.dld.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 40.Cantoro L., Di Sabatino A., Papi C., Margagnoni G., Ardizzone S., Giuffrida P., Giannarelli D., Massari A., Monterubbianesi R., Lenti M.V., et al. The Time Course of Diagnostic Delay in Inflammatory Bowel Disease Over the Last Sixty Years: An Italian Multicentre Study. J. Crohn’s Colitis. 2017;11:975–980. doi: 10.1093/ecco-jcc/jjx041. [DOI] [PubMed] [Google Scholar]
- 41.Car L.T., Papachristou N., Bull A., Majeed A., Gallagher J., El-Khatib M., Aylin P., Rudan I., Atun R., Car J., et al. Clinician-identified problems and solutions for delayed diagnosis in primary care: A PRIORITIZE study. BMC Fam Pract. 2016;17:131. doi: 10.1186/s12875-016-0530-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.HealthPathways. [(accessed on 25 May 2021)]. Available online: https://healthpathwaysglobal.org/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified raw data will be made available upon request.