INTRODUCTION
Regional anaesthesia techniques are indicated in patients with upper limb procedures having pulmonary injuries to avoid airway interventions and protect the lungs. However, 20 ml of local anaesthetic (LA) injected with ultrasound (US) guidance for interscalene block can lead to hemidiaphragmatic paresis in 17 to 46% of patients.[1,2] We describe our experience in three patients where an US-guided catheter was positioned in the interscalene area, and incremental doses of LA were injected with concomitant monitoring of diaphragmatic movements and oxygen saturation. Institutional ethics committee approval was obtained and the study was performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all patients.
CASE REPORT
From January 2018 until January 2021, three patients who sustained fracture of the proximal humerus and multiple ribs with a pulmonary injury were admitted in the intensive care unit (ICU). On arrival, the rib fracture score,[2] oxygen requirements, and numerical rating score (NRS) on parenteral analgesics were noted. Despite intravenous fentanyl infusion (0.5 mg/kg), NRS persisted more than 4 and all patients received a single-shot US-guided serratus anterior plane block (SAPB).[3] Computed tomography (CT) of chest was performed in all patients considering a persistent low oxygen saturation [Table 1] [Figure 1a and b]. In order to facilitate early fixation and subsequent mobilisation, patients were posted for surgery. A continuous incremental interscalene block (CIIB) was proposed with incremental LA injection and assessment of the oxygen saturation and diaphragmatic excursions on the ipsilateral side.
Table 1.
Demographics, injuries, analgesic patterns, investigations and anticoagulants
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Age (years) | 28 | 45 | 32 |
| Gender | Male | Male | Male |
| Bone fractures | Left proximal humerus and left 1-7 MRFS, blunt injury | Right proximal humerus and right 2-8 MRFS | Left proximal humerus and left 3-7 MRFS, |
| Head Injury | |||
| Thoracic Injury | GCS13/15 | GCS14/15 | GCS15/15 |
| Abdominal Injury | No visceral injury | No visceral injury | No visceral injury |
| No visceral injury | No visceral injury | No visceral injury | |
| RFS | 9 | 7 | 7 |
| SpO2 on admission without oxygen support | 88% | 92% | 93% |
| Analgesics | PCM/D/FI | PCM/FI | PCM/FI |
| Post-analgesic NRS at 12 h | 6 | 7 | 6 |
| Bed side SAPB | Left SAPB at 4th rib with bolus 30ml 0.2% ropivacaine and infusion 0.1% ropivacaine 8ml/h | Right SAPB at 5th rib with bolus 30ml 0.2% ropivacaine | Left SAPB at 4th rib with bolus 30ml 0.2% ropivacaine and infusion 0.1% ropivacaine 8ml/h |
| Infusion 0.1% ropivacaine 8ml/h | |||
| Bed side USG | Pleural effusion, pericardial effusion | Pleural effusion | Pleural effusion |
| Diaphragm function | Normal | Normal | Normal |
| HRCT contrast | Negative for PE; | Negative for PE; | Negative for PE; |
| Pleural and pericardial effusion; Left lower lobe collapse and consolidation of apices | Pleural effusion; right lower lobe collapse | Pleural effusion; Left lower lobe collapse and consolidation of apices | |
| Preoperative LMWH | Yes-stopped 12 h prior to block | Yes-stopped 12 h prior to block | Yes-stopped 12 h prior to block |
| CIIB volume | 3+3ml | 3+3+3ml | 3+3ml |
| Oxygen saturation | *Lowest SpO2=90% at 30th minute | *Lowest SpO2=88% at 30th minute | *Lowest SpO2=97% at 30thminute |
| Anaesthesia | Adequate sensory analgesia | Adequate sensory analgesia | Adequate sensory analgesia |
GCS - Glasgow coma scale; RFS - rib fracture score; MRFS - multiple rib fractures; NRS -numerical rating scale, PCM -paracetamol; D - diclofenac; FI - fentanyl infusion; Abd - abdominal; SAPB - serratus anterior plane block; USG - ultrasonography; HRCT - high-resolution computed tomography; PE - pulmonary embolism; LMWH - low molecular weight heparin; SpO2 - peripheral oxygen saturation; CIIB - continuous incremental interscalene block; *on oxygen support
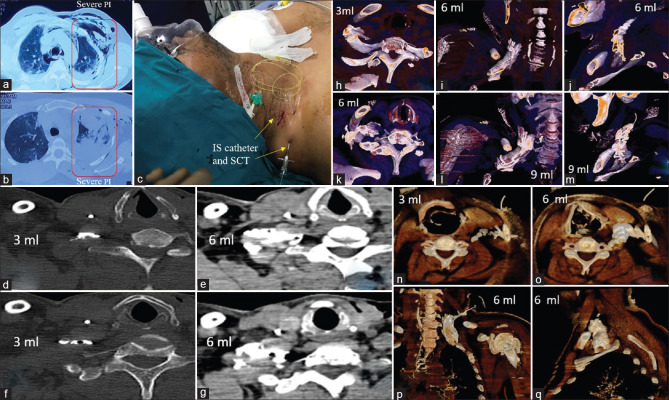
Figure 1.
(a and b) Right multiple rib fractures, subcutaneous emphysema, haemothorax (c) Right continuous interscalene block with subcutaneous tunnelling (d) Computed tomography axial 3 ml contrast in interscalene groove (e) Computed tomography axial 6ml contrast spilling over the scalene muscles (f and g) Computed tomography axial 3 ml sandwiched in interscalene groove (h) Axial volume rendering technique [inferior view] depicts linear contrast delineating the interscalene groove (hollow area).3 ml injection highlighting the middle scalene muscle and overlying the first rib (i) Coronal volume rendering technique image depicting the flow of 6 ml from medial to lateral and below the clavicle (j) Sagittal volume rendering technique image depicting the flow of 6 ml from medial to lateral and below the clavicle and in approximation to first rib (k) With 6ml injection, the inferior view portrays the three roots which appear distinctively, as the contrast spreads more laterally and posteriorly over the middle and posterior scalene muscles (l) Sagittal volume rendering technique image depicting the flow of 6ml from cephalad to caudal and between the clavicle and the first rib (m) Sagittal volume rendering technique image depicting the expansion as 9ml occupies the brachial plexus sheath (n) Axial volume rendering technique image; 3ml contrast is restricted to the interscalene groove (o) Axial volume rendering technique image illustrates spread over the anterior scalene muscle and beneath the sternocleidomastoid (p) Coronal volume rendering technique depicts the contrast spread in the interscalene groove and spilling over the scalene muscles (q) Sagittal volume rendering technique portrays the contrast as a thick band beneath the clavicle and close to the first rib. (IS – interscalene; SCT – subcutaneous tunnelling; 3 ml, 6 ml, 9 ml – volume of contrast injected; PI – pulmonary injury)
Patients were wheeled into the recovery room of the operation theatre with 6 L/min of oxygen through face mask. With the patient lying in a 45-degree semi-recumbent supine position, a linear array high-frequency US transducer (5-12 MHz, Sonosite M-Turbo, United States of America) was placed in the mid-axillary line and diaphragm excursion was assessed prior to block, 5, 15 and 30 min after each injection of LA, in the immediate postoperative period, and at 2, 12 and 24 h postoperatively in the ICU. The domes of the hemidiaphragm (right and left separately) were identified and its excursion was measured in the M-mode during rest and maximal forced inspiration.
Baseline oxygen saturation, blood pressures and heart rate were monitored in each patient. The anterolateral neck on the side of surgery was prepared and draped for CIIB. A linear array (3-12MHz) probe was deployed in a transverse oblique axis, at the level of C7vertebra (absence of anterior tubercle). After identification of C7 nerve root, the C5 and C6 roots were identified with a slight cephalad shift, sandwiched between the anterior and middle scalene muscles. The dorsal scapular and long thoracic nerves were identified in the middle scalene muscle and the phrenic nerve was recognised on the anterior scalene muscle. An out of plane approach was implemented, and 2 ml of 1% lidocainewas infiltrated until the middle scalene muscle. An 18 gauge insulated needle (Contiplex B-Braun, United States of America) was inserted [Figure 1c] as the tip penetrated the medial border of the middle scalene muscle and was positioned between the perimysium of the middle scalene muscle and sheath of the brachial plexus. After removal of the stylet, a 20 gauge catheter (Contiplex B-Braun, United States of America–single-end hole tip) was inserted through the cannula, in real-time sonographic guidance, and the tip was visualised protruding from the bevel of needle. The distance of the catheter from the tip of the cannula was 1-2 cm. Injection of 2 ml of 0.9% saline confirmed position of the catheter with distention of the space between the perimysium and the sheath (extra-neural). Consequently, the following protocol was followed:
A fresh LA preparation containing 5 ml of 2% lidocaine and 5 ml of 0.5% bupivacaine (total 10ml) was prepared. After each injection of boluses of 3ml around 10 min apart, through the catheter, respiratory monitoring (respiratory rate, diaphragmatic excursion in real time, oxygen saturation), blockade of dermatomes (C5,6) and pain on slight motor movement of the shoulder joint was evaluated. Patient preparedness for the surgery was announced when sensory blunting to needle prick (26 gauge), no pain on slight shoulder movement, minimal diaphragmatic paresis (up to 50% of the original excursion) and oxygen saturation not less than 90% with supplemental oxygen of 4-6 l/minute were confirmed [Table 1]. Volumes of LA injected were 6 to 9 ml. In addition, all patients received superficial cervical plexus block with 2 ml of 0.25% bupivacaine.
Postoperatively, patients were counselled and an informed consent was obtained and in the 2nd postoperative hour patients were wheeled to the computed tomography (CT) suite in the same institute with monitoring. Omnipaque (300 mg/ml iodine) 1 ml diluted in 10 ml 0.9% normal saline was injected through the catheter in the same sequence as performed for the surgical procedure. CT analysis revealed contrast spread in the interscalene groove with a volume of 3 ml and to the scalene muscles with volumes of 6 and 9 ml. However, there was no neuraxial spread [Figures 1d-q].
Postoperatively, 0.2% ropivacaine 5ml was injected intermittently whenever patient reported pain (NRS >4) even after 1 g of intravenous paracetamol. Catheters were removed at the end of the 48th hour. Neurological examination of the operated side did not reveal nerve injuries in all three patients.
DISCUSSION
US-guided interscalene blocks have resulted in hemi-diaphragmatic paresis even with lower volumes of LA. A 5ml single bolus[4] and 7 ml through the catheter[5] have resulted in hemi- diaphragmatic paresis in 45and 100% patients, respectively. A meta-analysis evaluating the advantages of single bolus interscalene block suggests that the duration of analgesia provided by interscalene block is limited to 6 and 8 h with motion and at rest, respectively, with rebound pain from 16th to 24th hour requiring parenteral analgesics.[6] High volume [25-50 ml] hybrid block and a selective trunk block have also been reported for patients with proximal humeral fractures without pulmonary injuries.[7] To our knowledge, a CIIB with incremental LA injections with respiratory monitoring is not reported yet.
CONCLUSION
CIIB with incremental LA injections with respiratory monitoring can provide adequate anaesthesia with minimal respiratory compromise in patients with pulmonary injury undergoing proximal humerus surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ayyanagouda B, Hosalli V, Kaur P, Ambi U, Hulkund SY. Hemi-diaphragmatic paresis following extrafascial versus conventional intrafascial approach for interscalene brachial plexus block: A double-blind randomised, controlled trial. Indian J Anaesth. 2019;63:375–81. doi: 10.4103/ija.IJA_69_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saini S, Rao SM, Agrawal N, Gupta A. Comparison of analgesic efficacy of shoulder block versus interscalene block for postoperative analgesia in arthroscopic shoulder surgeries:A randomised trial. Indian J Anaesth. 2021;65:451–7. doi: 10.4103/ija.IJA_110_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.May L, Hillermann C, Patil S. Rib fracture management. BJA Educ. 2016;16:26–32. [Google Scholar]
- 4.Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 ml) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008;101:549–56. doi: 10.1093/bja/aen229. [DOI] [PubMed] [Google Scholar]
- 5.Vandepitte C, Gautier P, Xu D, Salviz EA, Hadzic A. Effective volume of ropivacaine 0.75% through a catheter required for interscalene brachial plexus blockade. Anesthesiology. 2013;118:863–7. doi: 10.1097/ALN.0b013e3182850dc7. [DOI] [PubMed] [Google Scholar]
- 6.Vorobeichik L, Brull R, Bowry R, Laffey JG, Abdallah FW. Should continuous rather than single-injection interscalene block be routinely offered for major shoulder surgery?A meta-analysis of the analgesic and side-effects profiles. Br J Anaesth. 2018;120:679–92. doi: 10.1016/j.bja.2017.11.104. [DOI] [PubMed] [Google Scholar]
- 7.Sivakumar RK, Areeruk P, Karmakar MK. Selective trunk block (SeTB):A simple alternative to hybrid brachial plexus block techniques for proximal humeral fracture surgery during the COVID-19 pandemic. Reg Anesth Pain Med. 2021;46:376–8. doi: 10.1136/rapm-2020-101733. [DOI] [PubMed] [Google Scholar]