Abstract
The gut microbiome has increasingly been recognized as a critical and central factor in inflammatory bowel disease (IBD). Here, we review specific microorganisms that have been suggested to play a role in the pathogenesis of IBD and the current state of fecal microbial transplants as a therapeutic strategy in IBD. We discuss specific nutritional and dietary interventions in IBD and their effects on gut microbiota composition. Finally, we examine the role and mechanisms of the gut microbiome in mediating colitis-associated colon cancer.
Keywords: gut microbiome, inflammatory bowel disease, ulcerative colitis, Crohn’s disease, diet, colon cancer, immunity
1. Microbiome in the Pathogenesis of Inflammatory Bowel Disease (IBD)
The individual human lives in symbiosis with 100 trillion microbiota of the gastrointestinal tract, comprising more than 1000 different types, which are distributed among the genera; bacteria, bacteriophages (bacterial viruses), fungi, and protozoa [1]. The fungal and protozoan microbiome implications in IBD are, however, poorly described [2]. Sparse studies suggest that the protozoan microbiome in patients with active IBD display an increased prevalence of Blastocystis compared to those with quiescent disease or control subjects [3,4]. Additionally, studies report alterations in the diversity (measure of the number of species in a community, and a measure of the abundance of each species) and composition of the fungal microbiome among patients with IBD compared to healthy subjects [5,6,7,8,9,10], and, moreover, intra-individual changes in the fungal composition between inflamed and noninflamed mucosa have been observed in patients with Crohn’s disease (CD) [11]. Intestinal bacteria with associated bacteriophages and the intestinal epithelial cell layer are increasingly being studied, and exist in a dynamic tripartite—both mutualistic and parasitic—relationship, which recently started to be unraveled (Figure 1). Pattern recognition receptors (PRRs) specialized in recognizing bacteria and bacterial products are found in both immune and intestinal epithelial cells. In this way, intestinal epithelial cells balance the composition and luminal microbiota by regulating the secretion of mucus, antimicrobial peptides, and immune mediators, e.g., mucosal immunoglobulin A (IgA) [12]. Nevertheless, surprising evidence also points towards direct communication between bacteriophages and intestinal epithelial cells by bacteriophages adhering to mucosal surfaces, apical-to-basolateral transcytosis (i.e., endocytosis followed by exocytosis transporting bacteriophages across epithelial cells), and by the direct delivery of proteins and nucleic acids to eukaryotic cells [13]. In the following, we will focus on the bacteria and bacteriophages with respect to the pathogenesis of IBD.
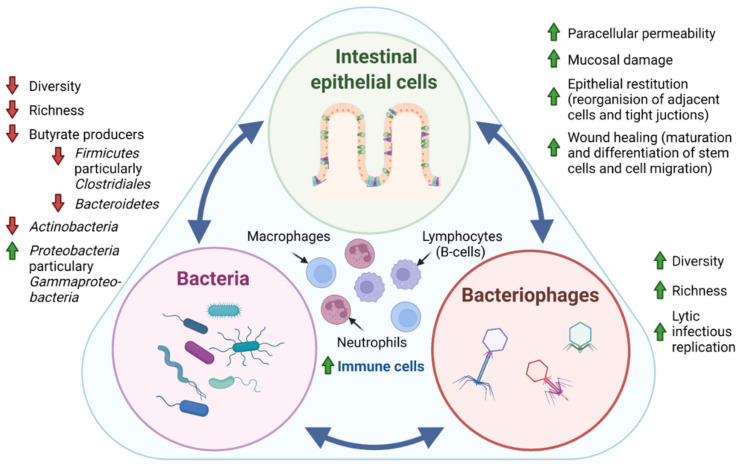
Figure 1.
Tripartite relationship between the intestinal epithelial cells, bacteria, and bacteriophages in IBD pathogenesis. In IBD pathogenesis, bacterial dysbiosis is characterized by decreased bacterial diversity (measure of the number of species in a community, and a measure of the abundance of each species) and richness (number of species in a community) evident by the depletion of the phyla Actinobacteria, Firmicutes, and Bacteroidetes and an enrichment of Proteobacteria. In contrast, studies generally suggest that intestinal bacteriophages, which are viruses that infect and replicate within bacteria, display increased diversity and richness. Interestingly, it has recently been suggested that the temperate phage population displays a shift from lysogenic to lytic replication in patients with IBD [44]. Where intestinal epithelial cells are known to directly regulate the secretion of mucus, antimicrobial peptides, and immune mediators through patterns recognition receptors (PRR), surprising evidence also points towards direct communication between bacteriophages and epithelial cells by adhering to mucosal surfaces, apical-to-basolateral transcytosis, and by the direct delivery of proteins and nucleic acids to eukaryotic cells. Thus, the intestinal epithelial cell layer, intestinal bacteria, and bacteriophages exist in a dynamic tripartite—both mutualistic and parasitic—relationship. Further, sparse studies propose that fungal and protozoan microbiomes are also affected in IBD pathogenesis, displaying both altered diversity and composition. The mechanistic interplay between intestinal epithelial cells, bacteria, bacteriophages, as well as fungi and protozoa, has yet to be unraveled, but would potentially provide insight for future clinical applications of microbiota in IBD. Green arrow: increased, red arrow: decreased.
1.1. Bacteria in IBD
The microbiome of patients with IBD is characterized by bacterial dysbiosis (i.e., an imbalance of pathogenic and commensal bacteria). Bacterial diversity has been shown to be reduced during active inflammation in IBD [14,15]. Furthermore, gut microbiome composition has been shown to vary based on their location along the gastrointestinal tract [16]. This observation is probably driven by mucosal changes in tissue oxygenation and disruption of the mucosal barrier function in IBD [15]. Bacterial dysbiosis, which refers to an imbalance of pathogenic and commensal bacteria, is in IBD characterized by a depletion of the phyla Actinobacteria, Firmicutes, and Bacteroidetes [17,18,19,20], and an enrichment of Proteobacteria [21]. Interestingly, Firmicutes and Bacteroidetes are primary producers of energy substrates for intestinal epithelial cells and anti-inflammatory agents, including butyrate and other short-chain fatty acids (SCFAs) [22,23]. Not surprisingly, fecal samples of patients with IBD display a decreased amount of SCFAs [24]. Moreover, long-term remission normalizes both the bacterial microbiota and SCFAs levels in a majority of IBD patients, although with pronounced interindividual variations [25,26,27]. Additionally, low levels of Firmicutes and Faecalibacterium species appear to be related to a high risk of relapse and post-operative recurrence of IBD patients [28,29,30,31]. Polymorphisms of the NOD2 gene are associated with an abundance of Faecalibacterium prausnitzii, the Roseburia genus and the Enterobacteriaceae family [32,33]. Additionally, the microbiome is affected by the diet of the host [34,35]. Interestingly, the intake of prebiotics such as nondigestible fibers is positively correlated with circulating serum levels of granulocyte-macrophage colony stimulating factor (GM-CSF) and negatively correlated with interleukin (IL)-6 and IL-8. These cytokines play central roles in the pathogenesis of IBD [36] and could be a result of altered bacteria or bacterial metabolites in the intestinal lumen. Thus, an intimate relationship between host bacterial microbiome and epithelial cells is evident in the pathogenesis of IBD. Hence, bacteria or bacterial products regulate components of the immune system, but an intestinal chronic low-grade inflammatory environment causing tissue oxygenation and disruption of the mucosal barrier may, on the other hand, significantly impact the microbiome by selecting against inflammatory sensitive species and inducing blooms in evolutionary adapted species.
1.2. Bacteriophages in IBD
The virome of the gut is dominated by viruses that infect bacteria, the so-called bacteriophages (phages), that can present themselves as RNA or both double- and single-stranded DNA [37]. Thus, patients with IBD display an elevated intestinal phage diversity and abundance [38,39]. Importantly, this expansion and diversification of the intestinal bacteriophages is not secondary to the observed concomitant and significantly reduced bacterial diversity [39].
Bacteriophages can indirectly stimulate the immune system by mediating bacterial lysis, which subsequently cause the release of phosphorus-containing bacterial components along with active enzymes [40], but they can also be directly sensed by intestinal epithelial cells and innate immune cells. In fact, bacteriophages have recently been found to be embedded within the intestinal mucus, and are transported across the intestinal epithelial barrier via transcytosis [13].
Moreover, a recent study has proposed a possible mechanism for bacteriophage-mediated mucosal immunity [41]. This murine study suggested that increased bacteriophage levels may exacerbate colitis via the nucleotide-sensing receptor, Toll-like receptor (TLR) 9, and IFN-γ on immune cells [41]. Together with a positive correlation between mucosal IFN-γ and bacteriophage levels in patients with ulcerative colitis (UC), IFN-γ was proposed to be important for bacteriophage-mediated mucosal immunity and IBD [41]. Taken together, the above-mentioned studies underscore the importance of understanding the direct effects on bacteriophages, not only on bacteria, but also on both immune and epithelial cells.
One of the major obstacles to comprehensively defining the virome is “viral dark matter”, i.e., metagenomic sequences originating from viruses, which, do not align with any reference virus sequences [42]. This is caused by a lack of universal marker genes on phages (similar to the 16S ribosomal RNA gene in bacteria or the 18S and internal transcriptional spacer (ITS) ribosomal RNA genes in eukaryotes), a lack of taxonomic information due to poorly populated databases, and the fact that the virome exhibits an enormous diversity and interindividual variation [43]. Additionally, bacteriophages remain hard to culture and are challenging to analyze. Nevertheless, recent data using whole-virome analysis have shed some light on the viral dark matter in IBD [44]. Intestinal bacteriophages exist in two states: lytic or temperate. The lytic cycle results in destruction of the infected cells, and the temperate phages integrate their genomes into their host bacterial chromosome [45]. At some point, temperate bacteriophages can switch from the lysogenetic life cycle to the lytic life cycle. Interestingly, in this study, the temperate phage population displayed a shift from lysogenic to lytic replication in patients with IBD [44]. Unlike prior database-dependent methods, no changes were observed in viral richness (number of species in a community) in healthy subjects compared to patients with IBD [44], which challenges the current knowledge of a phage-related IBD pathogenesis. More research, with targeted analyses of the viral dark matter, is needed to unravel the nature of bacteriophage-mediated mucosal immunity in IBD.
1.3. Clinical Relevance of Gut Microbiota in IBD
Previously, it was believed that patients with CD would benefit from antibiotic therapies, resulting in a deleterious effect on the intestinal microbiota [46]. Nonetheless, exposure with antibiotics has been associated with increased microbial dysbiosis [47], and no scientific evidence exists for a beneficial effect of the antibiotic treatment of patients with CD without fistulas or ongoing infections. Instead, an increasing number of clinical trials have been initiated with the aim of investigating the therapeutic effect of fecal microbiota transplantation (FMT) in patients with IBD [48,49].
In the largest, double-blind, randomized, placebo-controlled clinical trial of donor FMT for UC to date, the primary outcome was defined as steroid-free clinical remission with endoscopic remission or response. The primary outcome was achieved in 11 (27%) of 41 patients allocated FMT versus three (8%) of 40 who were assigned placebo (p < 0.04) [50]. Another study of adults with mild to moderate UC compared anaerobically prepared pooled donor FMT versus autologous FMT. Here, 12 of the 38 participants (32%) receiving pooled donor FMT, as compared to 3 of the 35 (9%) receiving autologous FMT, experienced an 8-week steroid-free clinical remission (p < 0.03) [51]. These studies and other published data indicate that donor FMT induces remission in a statistically significant proportion of UC patients [50,51,52,53].
However, available studies in patients with CD are scarce and under-powered. One study with adult colonic or ileo-colonic CD (n = 17, 8 FMT and 9 sham) showed that the steroid-free clinical remission rate at 10 and 24 weeks was 4 of 9 (44%) and 3 of 9 (33%), respectively, in the sham transplantation group and 7 of 8 (88%) and 4 of 8 (50%) in the FMT group (p > 0.05 at both time points), and none of the patients reached the primary endpoint [54]. These results are currently being tested in a larger ongoing clinical trial (n = 24) (ClinicalTrials.gov identifier NCT02097797). Interestingly, several studies in both UC and CD have revealed a significant shift in fecal microbial composition towards a greater microbial diversity, like that of healthy subjects in patients who experienced clinical responses [53,55,56,57]. Although FMT studies to date report low FMT-associated adverse effects in UC [52,56], one study reported flares within a few days of undergoing FMT in CD [57]. Thus, further research is warranted to assess the long-term maintenance of remission and safety of both donor and therapeutically optimized donor-derived strains [58]. Other important issues to address include the applied delivery method (e.g., delivery via colonic transendoscopic tube or encapsulated delivery either orally or via topical application [59,60]); fecal sample preparation and storing (fresh or frozen), or if one should help facilitate the colonization of microbiota using bowel lavage or antibiotics, risking the elimination of preexisting beneficial bacteria prior to the therapeutic intervention. Additionally, in the future, microbiota may possibly be used as a noninvasive biomarker for preventative, diagnostic, prognostic, and monitoring purposes among patients with IBD [61,62].
2. Dietary Modulation of the Gut Microbiome in IBD
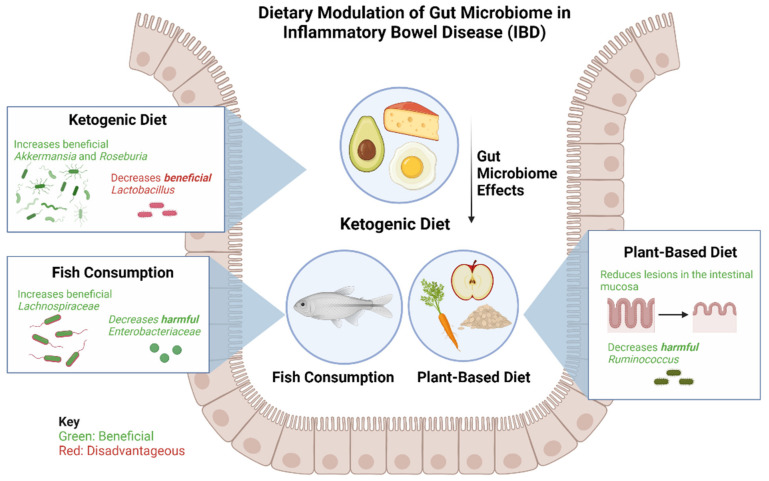
Interests in the diet’s ability to alter the gut microbiome as a therapeutic strategy among patients with IBD has grown tremendously in recent years (Figure 2) [63]. Several nutritional therapies have been explored among pediatric patients with IBD. For example, the Crohn’s Disease Exclusion Diet (CDED) is a high protein, low-fat diet that includes foods such as chicken, fish, eggs, rice, potatoes, and various fruits and vegetables. This intervention has been effective for mild to moderate CD in children, as well as for patients whose response to anti-TNF biologic treatments plateaued [63]. Levine et al. found that remission in the CDED groups was associated with changes in microbial diversity, a decrease in Proteobacteria and an increase in Firmicutes, particularly Clostridiales. Remission also led to a significant decrease in Proteobacteria, particularly Gammaproteobacteria [64].
Figure 2.
Effects of a ketogenic diet, plant-based diet, and fish consumption on gut microbiome in patients with IBD. The ketogenic diet has been shown to increase beneficial bacteria Akkermansia and Roseburia and consequently decrease beneficial Lactobacillus. The plant-based diet has been found to be beneficial in reducing lesions of the intestinal mucosa and reducing harmful Ruminococcus. Fish consumption leads to an increase in beneficial Lachnospiraceae and a decrease in harmful Enterobacteriaceae.
A Ketogenic Diet (KD) and Low-Carbohydrate Diet (LCD) show promising changes in the specific composition and function of gut microbiota and metabolites in mice [65]. The study by Kong et al. found that, after inducing colitis, KD significantly reduced inflammatory responses, protected intestinal barrier function, and reduced the expression of inflammatory cytokines, whereas the opposite effects were observed for the LCD [65]. These findings indicate a promising dietary strategy for treating IBD, and demonstrate, for the first time, that fecal microbiota transplantation from donors on a KD confers microbiota benefits and relieves colitis in dextran sulfate sodium (DSS)-induced recipients [64]. KD dramatically increased the abundance of Akkermansia and Roseburia; expanding the abundance of Akkermansia has been associated with improved glucose homeostasis, modulated immune responses, and protected barrier function [65]. It should, however, be noted that while KD alleviated the progression of intestinal inflammation, it also reduced the abundance of some healthy bacteria, such as Lactobacillus, compared with a normal diet [65].
Fiber in fruits and vegetables has been shown to provide several benefits to patients with IBD, such as prolonging remission and reducing lesions in the intestinal mucosa, while an imbalance in the consumption of fiber is a risk factor for IBD development [66]. Furthermore, a diet rich in oats prevents the worsening of gastrointestinal symptoms in UC, while a diet rich in high-fiber legumes mitigates intestinal inflammation in rodent models of IBD [66].
As previously mentioned, the production of SCFAs from fiber in gut microbiota has been established as a protective agent against IBD in recent years [66]. The most-studied SCFAs (butyrate, acetate, and propionate) exert anti-inflammatory effects in IBD by inhibiting NF-ĸB activation to suppress cytokines [66]. Butyrate, produced by the microbe Firmicutes, exists at highest concentrations in the colon and cecum, and propionate and acetate are byproducts from Bacteroidetes in the small and large intestines. SCFA production from fiber is crucial for reducing the inflammatory response in patients with IBD; therefore, a diet rich in fiber is essential to gut health [66].
Alternatively, fish consumption can lower the risk of IBD. Studies have found ω3FAs to support anti-inflammatory processes when interacting with microbes and alter microbiota diversity, increase beneficial bacteria, and reduce harmful bacteria. ω3FAs encourage growth of SCFA-producing microbes, including the Lachnospiraceae, and lessen the abundance of pathogenic microbes, such as Enterobacteriaceae, in infants [66]. However, the exact pathways and interactions between ω3FAs and the microbes themselves remain unclear.
As interest grows in the benefits of a plant-based diet in IBD, studies have demonstrated that processed and animal-derived foods, in contrast, are associated with higher abundances of CD and UC inflammatory species such as Ruminococcus, as well as with an elevated calprotectin, the gut-specific inflammatory marker [67]. Allin et al. found that processed meat, soft drinks, refined sweetened foods, and salty foods are associated with a higher risk of developing IBD [68]. The study associates the excessive ingestion of ultra-processed foods (UPF) with an increased risk of IBD. Thus, compared with one serving of UPF per day, 5 or more servings per day was associated with a hazard ratio of IBD of 1.82 (95% confidence interval, 1.22–2.72). Unprocessed foods, such as white meat, dairy, starch, fruit, vegetables, and legumes, were shown not to be associated with IBD, while fried foods were associated with a higher rate of both CD and UC. IBD development is not affected by individual food categories (meats, dairy, starch, and fruit and vegetables), suggesting that consuming overly processed foods may be a major factor in diet-related IBD development [69].
Why and how processed/animal-derived foods in the gut may cause inflammation is still unknown. However, it is suggested that the processed sugars, red meats, and saturated fats abundant in the Western diet drastically alter the tissue and barrier function of the intestines, which trigger an inflammatory response leading to an imbalance of the TH17/Treg axis [69]. It is currently unknown whether Western diets also lead to adverse IBD outcomes in patients with well-established CD or UC; thus, a gap exists, which future studies must investigate.
3. Gut Microbiome and Colitis-Associated Colon Cancer
Patients with IBD are at a higher risk of developing colon cancer [70,71,72]. The two main types of IBD both greatly increase the risk for colitis-associated cancer (CAC). Thus, UC increases a patient’s cumulative risk of developing CAC by up to 18–20%, while CD increases the cumulative risk by up to 8% after having the disease for 30 years [73]. Although the disease etiologies of both IBD and CAC are complex, growing evidence suggests that the microbiome may play a major role in CAC (Figure 3) [74,75,76].
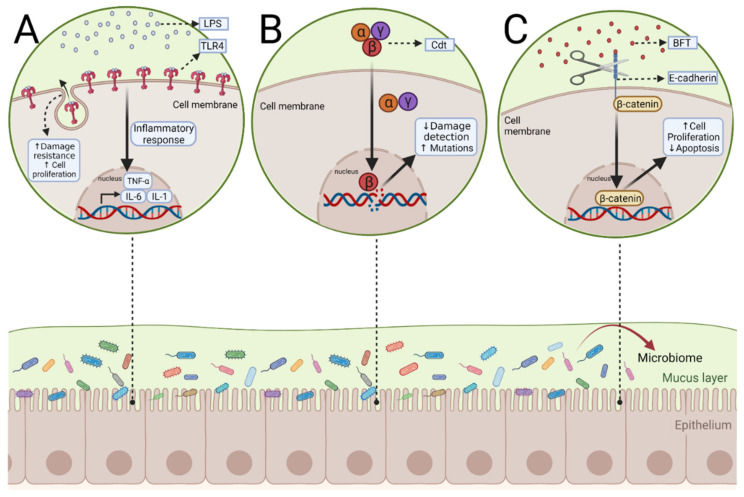
Figure 3.
Potential mechanisms of microbial activation of pathways leading to colitis-associated colon cancer. (A) Lipopolysaccharides (LPS) produced by gram-negative bacteria such as F. nucleatum and Salmonella bind to the receptor TLR4. This leads to the transcription of inflammatory cytokines such as tumor necrosis factor (TNF-α), interleukin-6 (IL-6), IL-1, and type I interferons. During IBD, TLR4 is upregulated and may cause CAC, due to its proliferation-promoting ability. (B) In this scenario, the heterotrimer produced by pathogenic gram-negative bacteria, Cytolethal distending toxin (Cdt), can directly induce CAC. CdtB is the only active subunit and can make DNA double-stranded breaks or single-stranded breaks. Chronic exposure to CdtB can reduce the damage response system and increase the chance of mutations. (C) When Bacteroides fragilis toxin (BFT) produced by Bacteroides fragilis binds to E-cadherin, it can cause cleavage of the protein receptor, Β-catenin, normally bound E-cadherin dissociates and becomes a transcription factor for cell proliferation. BFT also delays the apoptosis of intestinal epithelial cells.
The large surface of the digestive tract is constantly in contact with both commensal and pathogenic bacteria. The luminal surface is covered in mucus, which acts as the first line of defense against these pathogens [77]. In turn, pathogenic bacteria have evolved different mechanisms to cross the mucus, then bind to and proliferate on epithelial cells [78]. The host defense systems are subsequently activated through the innate immune system, such as antimicrobial peptides (AMPs), which are stimulated by microbiota metabolites [79]. Defensins are the most common AMP in the gut and are effective in controlling targeted bacteria by forming pores in their membrane [80]. Concurrently, epithelial cells and immune cells of the intestinal wall recognize these bacteria through pattern-recognition receptors (PRRs). One of the roles of these PRRs is to act as a bridge between the innate and adaptive immune system.
There are four major PRR classes: toll-like receptors (TLRs), nucleotide-binding oligomerization domain-like receptors (NLR), C-type lectin receptors (CLR), and RIG-1 like receptors (RLR) [77,80]. Many of these PRRs, such as TLRs, recognize pathogens from their pathogen-associated molecular patterns (PAMPS), as well as danger-associated molecular patterns (DAMPs) that come from stressed or damaged cells [81,82]. Signaling from TLR4 might act as a pivotal pathogen-activated tumor signal pathway in the development of CAC [83,84]. TLR4 binds to lipopolysaccharide (LPS) from gram-negative bacteria, such as Fusobacterium nucleatum and Salmonella [85,86]. These two pathogens were strongly associated with the development of CAC [87,88,89,90]. Once LPS is bound to TLR4, the receptor complex triggers intracellular signaling, resulting in the transcription of inflammatory cytokines [91]. These inflammatory cytokines include TNF-α, IL-6, IL-1, and type I interferons [92]. In intestinal epithelial cells, Toll-like receptor (TLR) 4 expression is relatively low; however, it is significantly upregulated during IBD development and CAC [93]. TLR4 knockout mice given DSS to induce IBD showed insufficient epithelial repair. TLR4 also plays a role in the proliferation of intestinal epithelial cells [94,95,96]. Therefore, the proliferation-promoting effect from TLR4 is required for resistance against inflammation-induced intestinal damage [97]. However, the upregulation and chronic activation of TLR4 could lead to the development of CAC because of this proliferation-promoting property. In addition, TLR4 may provide malignant cells with protection from apoptosis [97]. It has been found that mice with acute colitis and TLR4 knockout had increased intestinal epithelial cell apoptosis [98]. This effect is necessary during colonic inflammation to protect and repair injured epithelial cells, but can have negative outcomes due to the onset of tumorigenesis. TLR4 is an example of how the host immune response may lead to CAC; however, the next section will describe how the microbiome itself can directly induce CAC.
Another way that the gut microbiota is involved in the development of CAC is through the production of protein toxins with carcinogenic effects [99]. These carcinogenic effects occur when toxins either target DNA causing genomic instability (genotoxins) or alter the cellular signaling, stimulating proliferation and resistance to apoptosis (cytotoxins) [100]. Two major types of genotoxins that have the potential to cause DNA damage are cytolethal distending toxin (Cdt) and colibactin [101]. Cdts are released by at least 30 pathogenic gram-negative bacteria, including Salmonella [102]. As a heterotrimer, the only enzymatically active subunit is the CdtB subunit [103]. Once it has been transported to the nucleus at low doses, the CdtB subunit can cause DNA single-strand breaks (SSBs), whereas at high doses, it can cause double-stranded breaks (DSBs), activating the DNA damage response [104]. However, chronic exposure to sublethal doses of Cdt can impact the damage response, causing reduced damage detection and increased mutations [105]. Another genotoxin is colibactin, secreted by Escherichia coli (E. coli) strains with the phylogenetic group B2 [106]. Colibactin’s chemical structure and genotoxic mechanism have remained elusive, because it is produced in small quantities and is very unstable [107]. It is believed that, similar to Cdts, it causes double-strand breaks (DSBs), incomplete DNA repair, and chromosomal instability [108].
While cytotoxins do not directly interact with DNA and, thus, do not explicitly cause mutations, they can induce CAC through cellular signaling, which affects cellular proliferation and cell cycle checkpoints. For example, Bacteroides fragilis toxin (BFT) is produced by enterotoxigenic Bacteroides fragilis causing diarrhea and epithelial damage [105]. BFT can lead to cleavage of the tumor suppressor, E-cadherin. The extracellular domain of E-cadherin is necessary for cell–cell contact and cell proliferation, while the intracellular domain is bound to β-catenin. Once dissociated, β-catenin becomes a transcription factor for cell proliferation. BFT also delays the apoptosis of intestinal epithelial cells.
In CRC (patients alive five years after diagnosis) patients, there is an accumulation of pathogenic bacteria with a decrease in butyrate-producing bacteria [105]. Butyrate is a short-chain fatty acid (SCFA) that plays an important role in gut homeostasis by reducing the pH and oxygen levels, creating a favorable environment for anaerobic bacteria, and reducing the Enterobacteriaceae pathogens. Therefore, its reduction, combined with an increase in CAC-inducing bacteria, contributes to the development of CAC. The gut microbiome of CRC patients, when compared to healthy patients, has been characterized by an increase in Fusobacterium (particularly Fusobacterium nucleatum), Enterococcus, Esherichia/Shigella, Bacteroides fragilis, Klebsiella, Peptostreptococcus, and Streptococcus with a concurrent decrease in Lachnospiraceae, a butyrate-producing family of bacteria.
As chronic colitis increases the chance of developing colon cancer, certain IBD therapies such as mesalamine (5-ASA) have been shown to have chemopreventive effects for CAC in observational studies [106,107]. It was discovered that 5-ASA has beneficial effects in UC patients by re-establishing a healthy gut microbiota. Dai et al. observed, through 16S rRNA sequencing, that there was a significant change in the gut microbiota of treatment-naïve UC patients [107]. There was an increase in the following genera: Escherichia-shigella, Megamonas, Clostridium_sensu_stricto_1, Enterococcus and Citrobacter. After 5-ASA treatment, 49 candidate genera were significantly reversed, including Enterococcus. Enterococcus is of particular interest because it was significantly correlated with UC pathogenesis [107]. In addition, Enterococcus faecalis has been shown to play a role in the development of adenocarcinoma in IBD. However, the mechanisms by which Enterococcus may cause CAC remain unclear [108].
Vitamin D deficiency is common among patients with IBD. It is appreciated that vitamin D may modulate intestinal immunity and suppress inflammation [109,110,111,112]. Studies in mice have shown that vitamin D can decrease CD4+ and CD8+ proliferation and subsequent inflammatory cytokines [113,114]. Furthermore, vitamin D may also alter inflammation by interacting with dendritic cells, macrophages, antigen-presenting cells, and NK cells [114]. Prior studies in mice have shown that vitamin D may reduce CAC. Murine models of colitis that were provided with supplemental vitamin D experienced a significant decrease in colon tumor formation, which was mediated through MAPK signaling [115]. In another study, conditional intestinal vitamin D receptor (VDR) knockout led to an increased number of colon tumors in a murine colitis, which shifted the gut bacteria profile to be more susceptible to carcinogenesis, as well as increasing secondary bile acids [116].
Finally, it is important to look at the role that vitamin D plays in altering the microbiome and how this may affect CAC. For example, in a study with pre-diabetic individuals who were vitamin-D-deficient, it was found that vitamin D supplementation was inversely correlated with Firmicutes (genus Ruminococcus) [117], one of the genera that was positively correlated with tumor counts in murine models of colitis [104]. Furthermore, vitamin D appears to stimulate the expression of PRRs, which could help protect the epithelial tissue layer in the colon from bacterial invasion [118]. In a prior study [119], Singh et al. found that, among vitamin-D-deficient patients, the gut microbiome between vitamin D supplementation responders versus non-responders showed significant differences in the major gut bacterial phyla. In a randomized, double-blinded study of vitamin D supplementation of healthy adults, increased concentrations of serum vitamin D were associated with an increased number of beneficial bacteria, and a decreased level of pathogenic bacteria [120]. Future studies, however, are needed to understand the chemoprotective effects of vitamin D on risk of colon cancer among patients with IBD and the mechanisms of how the gut microbiome may mediate this effect.
4. Conclusions
IBD is characterized by gut microbial dysbiosis with decreased beneficial/commensal bacteria (Firmicutes, Actinobacteria, and Bacteroides) and an enrichment of pathogenic/colitogenic Proteobacteria. There is increasing evidence that gut viruses, such as bacteriophages, may impact IBD, but studies have been limited by technological challenges with measuring and interpreting the gut virome. Fecal transplants have been explored in relatively small studies in patients with IBD, with mixed overall results (some benefits in UC, inconclusive results for CD). Dietary interventions, such as the CDED, ketogenic diet, low-carbohydrate diet, and plant-based diets, may have beneficial effects on patients with IBD by improving gut microbial diversity and increasing beneficial gut bacteria. Gut microbiota-derived antigens and toxins may mediate their carcinogenic effects by activating innate immune signaling pathways, stimulating cell proliferation/inhibiting apoptosis, and directly damaging DNA. The chemoprotective effects of mesalamine, as well as vitamin D and the VDR, on the development of colitis-associated colon cancer may be mediated through alterations in the gut microbiome. Future studies are needed to investigate whether manipulating the gut microbiome through these chemoprotective agents or other strategies may mitigate the risk of colitis-associated colon cancer among patients with IBD.
Author Contributions
J.G. conceptualized, compiled, and edited the review. T.L.B. and O.H.N. performed the literature review and drafted the section on “Microbiome in the pathogenesis of IBD.” M.T. and S.R.S. performed the literature review and drafted the section on “Dietary Modulation of the Gut Microbiome in IBD.” R.S.S., D.R.H. and S.R.R. performed the literature review and drafted the section on “Gut Microbiome and Colitis-Associated Colon Cancer.” All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
JG is in part supported by a Chan Zuckerberg Biohub Physician Scientist Scholar Award, NIH NIDDK LRP Award (L30 DK126220), and a Doris Duke Physician Scientist Fellowship Award (Grant #2021091).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Almeida A., Mitchell A.L., Boland M., Boland M., Forster S., Gloor G., Tarkowska A., Lawley T.D., Finn R.D. A new genomic blueprint of the human gut microbiota. Nature. 2019;568:499–504. doi: 10.1038/s41586-019-0965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guzzo G.L., Andrews J.M., Weyrich L.S. The Neglected Gut Microbiome: Fungi, Protozoa, and Bacteriophages in Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2022;28:1112–1122. doi: 10.1093/ibd/izab343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen A.M., Stensvold C.R., Mirsepasi H., Engberg J., Friis-Møller A., Porsbo L.J., Hammerum A.M., Nordgaard-Lassen I., Nielsen H.V., Krogfelt K.A. Active ulcerative colitis associated with low prevalence of Blastocystis and Dientamoeba fragilis infection. Scand. J. Gastroenterol. 2013;48:638–639. doi: 10.3109/00365521.2013.780094. [DOI] [PubMed] [Google Scholar]
- 4.Tito R.Y., Chaffron S., Caenepeel C., Lima-Mendez G., Wang J., Vieira-Silva S., Falony G., Hildebrand F., Darzi Y., Rymenans L., et al. Population-level analysis of Blastocystis subtype prevalence and variation in the human gut microbiota. Gut. 2019;68:1180–1189. doi: 10.1136/gutjnl-2018-316106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chehoud C., Albenberg L.G., Judge C., Hoffmann C., Grunberg S., Bittinger K., Baldassano R.N., Lewis J.D., Bushman F.D., Wu G.D. Fungal Signature in the Gut Microbiota of Pediatric Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2015;21:1948–1956. doi: 10.1097/MIB.0000000000000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sokol H., Leducq V., Aschard H., Pham H.P., Jegou S., Landman C., Cohen D., Liguori G., Bourrier A., Nion-Larmurier I., et al. Fungal microbiota dysbiosis in IBD. Gut. 2017;66:1039–1048. doi: 10.1136/gutjnl-2015-310746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoarau G., Mukherjee P.K., Gower-Rousseau C., Hager C., Chandra J., Retuerto M.A., Neut C., Vermeire S., Clemente J., Colombel J.F., et al. Bacteriome and Mycobiome Interactions Underscore Microbial Dysbiosis in Familial Crohn’s Disease. MBio. 2016;7:e01250-16. doi: 10.1128/mBio.01250-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qiu X., Ma J., Jiao C., Mao X., Zhao X., Lu M., Wang K., Zhang H. Alterations in the mucosa-associated fungal microbiota in patients with ulcerative colitis. Oncotarget. 2017;8:107577–107588. doi: 10.18632/oncotarget.22534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liguori G., Lamas B., Richard M.L., Brandi G., Da Costa G., Hoffmann T.W., Di Simone M.P., Calabrese C., Poggioli G., Langella P., et al. Fungal Dysbiosis in Mucosa-associated Microbiota of Crohn’s Disease Patients. J. Crohns Colitis. 2016;10:296–305. doi: 10.1093/ecco-jcc/jjv209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lavelle A., Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2020;17:223–237. doi: 10.1038/s41575-019-0258-z. [DOI] [PubMed] [Google Scholar]
- 11.Jain U., Ver Heul A.M., Xiong S., Gregory M.H., Demers E.G., Kern J.T., Lai C.-W., Muegge B.D., Barisas D.A.G., Leal-Ekman J.S., et al. Debaryomyces is enriched in Crohn’s disease intestinal tissue and impairs healing in mice. Science. 2021;371:1154–1159. doi: 10.1126/science.abd0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abraham C., Abreu M.T., Turner J.R. Pattern Recognition Receptor Signaling and Cytokine Networks in Microbial Defenses and Regulation of Intestinal Barriers: Implications for Inflammatory Bowel Disease. Gastroenterology. 2022;162:1602–1616.e6. doi: 10.1053/j.gastro.2021.12.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen S., Baker K., Padman B.S., Patwa R., Dunstan R.A., Weston T.A., Schlosser K., Bailey B., Lithgow T., Lazarou M., et al. Bacteriophage Transcytosis Provides a Mechanism to Cross Epithelial Cell Layers. MBio. 2017;8:e01874-17. doi: 10.1128/mBio.01874-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manichanh C., Rigottier-Gois L., Bonnaud E., Gloux K., Pelletier E., Frangeul L., Nalin R., Jarrin C., Chardon P., Marteau P., et al. Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach. Gut. 2006;55:205–211. doi: 10.1136/gut.2005.073817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gevers D., Kugathasan S., Denson L.A., Vázquez-Baeza Y., Van Treuren W., Ren B., Schwager E., Knights D., Song S.J., Yassour M., et al. The treatment-naive microbiome in new-onset Crohn’s disease. Cell Host Microbe. 2014;15:382–392. doi: 10.1016/j.chom.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sepehri S., Kotlowski R., Bernstein C.N., Krause D.O. Microbial diversity of inflamed and noninflamed gut biopsy tissues in inflammatory bowel disease. Inflamm. Bowel Dis. 2007;13:675–683. doi: 10.1002/ibd.20101. [DOI] [PubMed] [Google Scholar]
- 17.Lloyd-Price J., Arze C., Ananthakrishnan A.N., Schirmer M., Avila-Pacheco J., Poon T.W., Andrews E., Ajami N.J., Bonham K.S., Brislawn C.J., et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature. 2019;569:655–662. doi: 10.1038/s41586-019-1237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michail S., Durbin M., Turner D., Griffiths A.M., Mack D.R., Hyams J., Leleiko N., Kenche H., Stolfi A., Wine E. Alterations in the gut microbiome of children with severe ulcerative colitis. Inflamm. Bowel Dis. 2012;18:1799–1808. doi: 10.1002/ibd.22860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alam M.T., Amos G.C.A., Murphy A.R.J., Murch S., Wellington E.M.H., ArJasaradnam R.P. Microbial imbalance in inflammatory bowel disease patients at different taxonomic levels. Gut Pathog. 2020;12:1. doi: 10.1186/s13099-019-0341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou Y., Zhi F. Lower Level of Bacteroides in the Gut Microbiota Is Associated with Inflammatory Bowel Disease: A Meta-Analysis. Biomed Res. Int. 2016;2016:5828959. doi: 10.1155/2016/5828959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vester-Andersen M.K., Mirsepasi-Lauridsen H.C., Prosberg M.V., Mortensen C.O., Träger C., Skovsen K., Thorkilgaard T., Nøjgaard C., Vind I., Krogfelt K.A., et al. Increased abundance of proteobacteria in aggressive Crohn’s disease seven years after diagnosis. Sci. Rep. 2019;9:13473. doi: 10.1038/s41598-019-49833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stoeva M.K., Garcia-So J., Justice N., Myers J., Tyagi S., Nemchek M., McMurdie P.J., Kolterman O., Eid J. Butyrate-producing human gut symbiont, Clostridium butyricum, and its role in health and disease. Gut Microbes. 2021;13:1907272. doi: 10.1080/19490976.2021.1907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chia L.W., Mank M., Blijenberg B., Aalvink S., Bongers R.S., Stahl B., Knol J., Belzer C. Bacteroides thetaiotaomicron Fosters the Growth of Butyrate-Producing Anaerostipes caccae in the Presence of Lactose and Total Human Milk Carbohydrates. Microorganisms. 2020;8:1513. doi: 10.3390/microorganisms8101513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huda-Faujan N., Abdulamir A.S., Fatimah A.B., Anas O.M., Shuhaimi M., Yazid A., Loong Y. The impact of the level of the intestinal short chain Fatty acids in inflammatory bowel disease patients versus healthy subjects. Open Biochem. J. 2010;4:53–58. doi: 10.2174/1874091X01004010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stange E.F., Schroeder B.O. Microbiota and mucosal defense in IBD: An update. Expert Rev. Gastroenterol. Hepatol. 2019;13:963–976. doi: 10.1080/17474124.2019.1671822. [DOI] [PubMed] [Google Scholar]
- 26.Kumari R., Ahuja V., Paul J. Fluctuations in butyrate-producing bacteria in ulcerative colitis patients of North India. World J. Gastroenterol. 2013;19:3404–3414. doi: 10.3748/wjg.v19.i22.3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wills E.S., Jonkers D.M., Savelkoul P.H., Masclee A.A., Pierik M.J., Penders J. Fecal microbial composition of ulcerative colitis and Crohn’s disease patients in remission and subsequent exacerbation. PLoS ONE. 2014;9:e90981. doi: 10.1371/journal.pone.0090981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rajca S., Grondin V., Louis E., Vernier-Massouille G., Grimaud J.C., Bouhnik Y., Laharie D., Dupas J.-L., Pillent H., Picon L., et al. Alterations in the intestinal microbiome (dysbiosis) as a predictor of relapse after infliximab withdrawal in Crohn’s disease. Inflamm. Bowel Dis. 2014;20:978–986. doi: 10.1097/MIB.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 29.Braun T., Di Segni A., BenShoshan M., Neuman S., Levhar N., Bubis M., Picard O., Sosnovski K., Efroni G., Farage Barhom S., et al. Individualized Dynamics in the Gut Microbiota Precede Crohn’s Disease Flares. Am. J. Gastroenterol. 2019;114:1142–1151. doi: 10.14309/ajg.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 30.Wright E.K., Kamm M.A., Wagner J., Teo S.-M., De Cruz P., Hamilton A.L., Ritchie K.J., Inouye M., Kirkwood C.D. Microbial Factors Associated with Postoperative Crohn’s Disease Recurrence. J. Crohns Colitis. 2017;11:191–203. doi: 10.1093/ecco-jcc/jjw136. [DOI] [PubMed] [Google Scholar]
- 31.Varela E., Manichanh C., Gallart M., Torrejón A., Borruel N., Casellas F., Guarner F., Antolin M. Colonisation by Faecalibacterium prausnitzii and maintenance of clinical remission in patients with ulcerative colitis. Aliment. Pharmacol. Ther. 2013;38:151–161. doi: 10.1111/apt.12365. [DOI] [PubMed] [Google Scholar]
- 32.Aschard H., Laville V., Tchetgen E.T., Knights D., Imhann F., Seksik P., Zaitlen N., Silverberg M.S., Cosnes J., Weersma R.K., et al. Genetic effects on the commensal microbiota in inflammatory bowel disease patients. PLoS Genet. 2019;15:e1008018. doi: 10.1371/journal.pgen.1008018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knights D., Silverberg M.S., Weersma R.K., Gevers D., Dijkstra G., Huang H., Tyler A.D., Van Sommeren S., Imhann F., Stempak J.M., et al. Complex host genetics influence the microbiome in inflammatory bowel disease. Genome Med. 2014;6:107. doi: 10.1186/s13073-014-0107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoffmann C., Dollive S., Grunberg S., Chen J., Li H., Wu G.D., Lewis J.D., Bushman F.D. Archaea and fungi of the human gut microbiome: Correlations with diet and bacterial residents. PLoS ONE. 2013;8:e66019. doi: 10.1371/journal.pone.0066019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.David L.A., Maurice C.F., Carmody R.N., Gootenberg D.B., Button J.E., Wolfe B.E., Ling A.V., Devlin A.S., Varma Y., Fischbach M.A., et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olendzki B., Bucci V., Cawley C., Maserati R., McManus M., Olednzki E., Madziar C., Chiang D., Ward D.V., Pellish R., et al. Dietary manipulation of the gut microbiome in inflammatory bowel disease patients: Pilot study. Gut Microbes. 2022;14:2046244. doi: 10.1080/19490976.2022.2046244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duan Y., Young R., Schnabl B. Bacteriophages and their potential for treatment of gastrointestinal diseases. Nat. Rev. Gastroenterol. Hepatol. 2022;19:135–144. doi: 10.1038/s41575-021-00536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang W., Jovel J., Halloran B., Wine E., Patterson J., Ford G., O’keefe S., Meng B., Song D., Zhang Y., et al. Metagenomic analysis of microbiome in colon tissue from subjects with inflammatory bowel diseases reveals interplay of viruses and bacteria. Inflamm. Bowel Dis. 2015;21:1419–1427. doi: 10.1097/MIB.0000000000000344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Norman J.M., Handley S.A., Baldridge M.T., Droit L., Liu C.Y., Keller B.C., Kambal A., Monaco C.L., Zhao G., Fleshner P., et al. Disease-specific alterations in the enteric virome in inflammatory bowel disease. Cell. 2015;160:447–460. doi: 10.1016/j.cell.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Heyer C.M., Weiss E., Schmucker S., Rodehutscord M., Hoelzle L.E., Mosenthin R., Stefalnski V. The impact of phosphorus on the immune system and the intestinal microbiota with special focus on the pig. Nutr. Res. Rev. 2015;28:67–82. doi: 10.1017/S0954422415000049. [DOI] [PubMed] [Google Scholar]
- 41.Gogokhia L., Buhrke K., Bell R., Hoffman B., Brown D.G., Hanke-Gogokhia C., Ajami N.J., Wong M.C., Ghazaryan A., Valentine J.F., et al. Expansion of Bacteriophages Is Linked to Aggravated Intestinal Inflammation and Colitis. Cell Host Microbe. 2019;25:285–299.e288. doi: 10.1016/j.chom.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tisza M.J., Pastrana D.V., Welch N.L., Stewart B., Peretti A., Starrett G.J., Pang Y.-Y.S., Krishnamurthy S.R., Pesavento P.A., McDermott D.H., et al. Discovery of several thousand highly diverse circular DNA viruses. eLife. 2020;9:e51971. doi: 10.7554/eLife.51971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reyes A., Haynes M., Hanson N., Angly F.E., Heath A.C., Rohwer F., Gordon J.I. Viruses in the faecal microbiota of monozygotic twins and their mothers. Nature. 2010;466:334–338. doi: 10.1038/nature09199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clooney A.G., Sutton T.D.S., Shkoporov A.N., Holohan R.K., Daly K.M., O’Regan O., Ryan F.J., Draper L.A., Plevy S.E., Ross R.P., et al. Whole-Virome Analysis Sheds Light on Viral Dark Matter in Inflammatory Bowel Disease. Cell Host Microbe. 2019;26:764–778.e765. doi: 10.1016/j.chom.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 45.Chen Y., Yang L., Yang D., Song J., Wang C., Sun E., Gu C., Chen H., Tong Y., Tao P., et al. Specific Integration of Temperate Phage Decreases the Pathogenicity of Host Bacteria. Front. Cell. Infect. Microbiol. 2020;10:14. doi: 10.3389/fcimb.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Colombel J.F., Cortot A., van Kruiningen H.J. Antibiotics in Crohn’s disease. Gut. 2001;48:647. doi: 10.1136/gut.48.5.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lewis J.D., Chen E.Z., Baldassano R.N., Otley A.R., Griffiths A.M., Lee D., Bittinger K., Bailey A., Friedman E.S., Hoffmann C., et al. Inflammation, Antibiotics, and Diet as Environmental Stressors of the Gut Microbiome in Pediatric Crohn’s Disease. Cell Host Microbe. 2015;18:489–500. doi: 10.1016/j.chom.2015.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Allegretti J.R., Mullish B.H., Kelly C., Fischer M. The evolution of the use of faecal microbiota transplantation and emerging therapeutic indications. Lancet. 2019;394:420–431. doi: 10.1016/S0140-6736(19)31266-8. [DOI] [PubMed] [Google Scholar]
- 49.Luo H., Cao G., Luo C., Tan D., Vong C.T., Xu Y., Wang S., Lu H., Wang Y., Jing W. Emerging pharmacotherapy for inflammatory bowel diseases. Pharmacol. Res. 2022;178:106146. doi: 10.1016/j.phrs.2022.106146. [DOI] [PubMed] [Google Scholar]
- 50.Paramsothy S., Kamm M.A., Kaakoush N.O., Walsh A.J., van den Bogaerde J., Samuel D., Leong R.W.L., Connor S., Ng W., Paramsothy R., et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: A randomised placebo-controlled trial. Lancet. 2017;389:1218–1228. doi: 10.1016/S0140-6736(17)30182-4. [DOI] [PubMed] [Google Scholar]
- 51.Costello S.P., Hughes P.A., Waters O., Bryant R.V., Vincent A.D., Blatchford P., Katsikeros R., Makanyanga J., Campaniello M.A., Mavrangelos C., et al. Effect of Fecal Microbiota Transplantation on 8-Week Remission in Patients with Ulcerative Colitis: A Randomized Clinical Trial. JAMA. 2019;321:156–164. doi: 10.1001/jama.2018.20046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moayyedi P., Surette M.G., Kim P.T., Libertucci J., Wolfe M., Onischi C., Armstrong D., Marshall J.K., Kassam Z., Reinisch W., et al. Fecal Microbiota Transplantation Induces Remission in Patients with Active Ulcerative Colitis in a Randomized Controlled Trial. Gastroenterology. 2015;149:102–109.e106. doi: 10.1053/j.gastro.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 53.Brezina J., Bajer L., Wohl P., Ďuricová D., Hrabák P., Novotný A., Koželuhová J., Lukáš M., Mrázek J., Fliegerová K., et al. Fecal Microbial Transplantation versus Mesalamine Enema for Treatment of Active Left-Sided Ulcerative Colitis-Results of a Randomized Controlled Trial. J. Clin. Med. 2021;10:2753. doi: 10.3390/jcm10132753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sokol H., Landman C., Seksik P., Berard L., Montil M., Nion-Larmurier I., Bourrier A., Le Gall G., Lalande V., De Rougemont A., et al. Fecal microbiota transplantation to maintain remission in Crohn’s disease: A pilot randomized controlled study. Microbiome. 2020;8:12. doi: 10.1186/s40168-020-0792-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vaughn B.P., Vatanen T., Allegretti J.R., Bai A., Xavier R.J., Korzenik J., Gevers D., Ting A., Robson S.C., Moss A.C. Increased Intestinal Microbial Diversity Following Fecal Microbiota Transplant for Active Crohn’s Disease. Inflamm. Bowel Dis. 2016;22:2182–2190. doi: 10.1097/MIB.0000000000000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rossen N.G., Fuentes S., van der Spek M.J., Tijssen J.G., Hartman J.H.A., Duflou A., Löwenberg M., Van Den Brink G.R., Mathus-Vliegen E.M.H., de Vos W.M., et al. Findings from a Randomized Controlled Trial of Fecal Transplantation for Patients With Ulcerative Colitis. Gastroenterology. 2015;149:110–118.e114. doi: 10.1053/j.gastro.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 57.Gutin L., Piceno Y., Fadrosh D., Lynch K., Zydek M., Kassam Z., LaMere B., Terdiman J., Ma A., Somsouk M., et al. Fecal microbiota transplant for Crohn disease: A study evaluating safety, efficacy, and microbiome profile. United Eur. Gastroenterol. J. 2019;7:807–814. doi: 10.1177/2050640619845986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lima S.F., Gogokhia L., Viladomiu M., Chou L., Putzel G., Jin W.-B., Pires S., Guo C.-J., Gerardin Y., Crawford C.V., et al. Transferable Immunoglobulin A-Coated Odoribacter splanchnicus in Responders to Fecal Microbiota Transplantation for Ulcerative Colitis Limits Colonic Inflammation. Gastroenterology. 2022;162:166–178. doi: 10.1053/j.gastro.2021.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Peng Z., Xiang J., He Z., Zhang T., Xu L., Cui B., Li P., Huang G., Ji G., Nie Y., et al. Colonic transendoscopic enteral tubing: A novel way of transplanting fecal microbiota. Endosc. Int. Open. 2016;4:E610–E613. doi: 10.1055/s-0042-105205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Crothers J.W., Chu N.D., Nguyen L.T.T., Phillips M., Collins C., Fortner K., Del Rio-Guerra E., Lavoie B., Callas P., Velez M., et al. Daily, oral FMT for long-term maintenance therapy in ulcerative colitis: Results of a single-center, prospective, randomized pilot study. BMC Gastroenterol. 2021;21:281. doi: 10.1186/s12876-021-01856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sarrabayrouse G., Elias A., Yanez F., Mayorga L., Varela E., Bartoli C., Casellas F., Borruel N., de Guise C.H., Machiels K., et al. Fungal and Bacterial Loads: Noninvasive Inflammatory Bowel Disease Biomarkers for the Clinical Setting. MSystems. 2021;6:e01277-20. doi: 10.1128/mSystems.01277-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Metwaly A., Reitmeier S., Haller D. Microbiome risk profiles as biomarkers for inflammatory and metabolic disorders. Nat. Rev. Gastroenterol. Hepatol. 2022;19:383–397. doi: 10.1038/s41575-022-00581-2. [DOI] [PubMed] [Google Scholar]
- 63.Hart L., Verburgt C.M., Wine E., Zachos M., Poppen A., Chavannes M., Van Limbergen J., Pai N. Nutritional Therapies and Their Influence on the Intestinal Microbiome in Pediatric Inflammatory Bowel Disease. Nutrients. 2022;14:4. doi: 10.3390/nu14010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Levine A., Wine E., Assa A., Sigall Boneh R., Shaoul R., Kori M., Cohen S., Peleg S., Shamaly H., On A., et al. Crohn’s Disease Exclusion Diet Plus Partial Enteral Nutrition Induces Sustained Remission in a Randomized Controlled Trial. Gastroenterology. 2019;157:440–450.e8. doi: 10.1053/j.gastro.2019.04.021. [DOI] [PubMed] [Google Scholar]
- 65.Kong C., Yan X., Liu Y., Huang L., Zhu Y., He J., Gao R., Kalady M.F., Goel A., Qin H., et al. Ketogenic diet alleviates colitis by reduction of colonic group 3 innate lymphoid cells through altering gut microbiome. Signal Transduct. Target. Ther. 2021;6:154. doi: 10.1038/s41392-021-00549-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.O’Mahony C., Amamou A., Ghosh S. Diet–Microbiota Interplay: An Emerging Player in Macrophage Plasticity and Intestinal Health. Int. J. Mol. Sci. 2022;23:3901. doi: 10.3390/ijms23073901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bolte L.A., Vich Vila A., Imhann F., Collij V., Gacesa R., Peters V., Wijmenga C., Kurilshikov A., Campmans-Kuijpers M.J.E., Fu J., et al. Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut. 2021;70:1287–1298. doi: 10.1136/gutjnl-2020-322670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Allin K.H., Ungaro R.C., Agrawal M. Ultraprocessed Foods and the Risk of Inflammatory Bowel Disease: Is it Time to Modify Diet? Gastroenterology. 2022;162:652–654. doi: 10.1053/j.gastro.2021.09.053. [DOI] [PubMed] [Google Scholar]
- 69.Tracy M., Khalili H. You Are What You Eat? Growing Evidence That Diet Influences the Risk of Inflammatory Bowel Disease. J. Crohns Colitis. 2022;20:jjac025. doi: 10.1093/ecco-jcc/jjac025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ekbom A., Helmick C., Zack M., Adami H.-O. Ulcerative Colitis and Colorectal Cancer. N. Engl. J. Med. 1990;323:1228–1233. doi: 10.1056/NEJM199011013231802. [DOI] [PubMed] [Google Scholar]
- 71.Ekbom A., Adami H.-O., Helmick C., Zack M. Increased risk of large-bowel cancer in Crohn’s disease with colonic involvement. Lancet. 1990;336:357–359. doi: 10.1016/0140-6736(90)91889-I. [DOI] [PubMed] [Google Scholar]
- 72.Jess T., Rungoe C., Peyrin–Biroulet L. Risk of Colorectal Cancer in Patients with Ulcerative Colitis: A Meta-analysis of Population-Based Cohort Studies. Clin. Gastroenterol. Hepatol. 2012;10:639–645. doi: 10.1016/j.cgh.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 73.Grivennikov S.I. Inflammation and colorectal cancer: Colitis-associated neoplasia. Semin. Immunopathol. 2013;35:229–244. doi: 10.1007/s00281-012-0352-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dalton-Griffin L., Kellam P. Infectious causes of cancer and their detection. J. Biol. 2009;8:67. doi: 10.1186/jbiol168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wu S., Rhee K.-J., Albesiano E., Rabizadeh S., Wu X., Yen H.-R., Huso D.L., Brancati F.L., Wick E., McAllister F., et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat. Med. 2009;15:1016–1022. doi: 10.1038/nm.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Castellarin M., Warren R.L., Freeman J.D., Dreolini L., Krzywinski M., Strauss J., Barnes R., Watson P., Allen-Vercoe E., Moore R.A., et al. Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res. 2012;22:299–306. doi: 10.1101/gr.126516.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ribet D., Cossart P. How bacterial pathogens colonize their hosts and invade deeper tissues. Microbes Infect. 2015;17:173–183. doi: 10.1016/j.micinf.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 78.Kang M., Martin A. Microbiome and colorectal cancer: Unraveling host-microbiota interactions in colitis-associated colorectal cancer development. Semin. Immunol. 2017;32:3–13. doi: 10.1016/j.smim.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 79.Gubatan J., Holman D.R., Puntasecca C.J., Polevoi D., Rubin S.J., Rogalla S. Antimicrobial peptides and the gut microbiome in inflammatory bowel disease. World J. Gastroenterol. 2021;27:7402–7422. doi: 10.3748/wjg.v27.i43.7402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Babamale A.O., Chen S.-T. Nod-like Receptors: Critical Intracellular Sensors for Host Protection and Cell Death in Microbial and Parasitic Infections. Int. J. Mol. Sci. 2021;22:11398. doi: 10.3390/ijms222111398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kashani B., Zandi Z., Pourbagheri-Sigaroodi A., Bashash D., Ghaffari S.H. The role of toll-like receptor 4 (TLR4) in cancer progression: A possible therapeutic target? J. Cell. Physiol. 2021;236:4121–4137. doi: 10.1002/jcp.30166. [DOI] [PubMed] [Google Scholar]
- 82.Mokhtari Y., Pourbagheri-Sigaroodi A., Zafari P., Bagheri N., Ghaffari S.H., Bashash D. Toll-like receptors (TLRs): An old family of immune receptors with a new face in cancer pathogenesis. J. Cell. Mol. Med. 2021;25:639–651. doi: 10.1111/jcmm.16214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guo J., Liao M., Wang J. TLR4 signaling in the development of colitis-associated cancer and its possible interplay with microRNA-155. Cell Commun. Signal. 2021;19:90. doi: 10.1186/s12964-021-00771-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garcia M.M., Goicoechea C., Molina-Álvarez M., Pascual D. Toll-like receptor 4: A promising crossroads in the diagnosis and treatment of several pathologies. Eur. J. Pharmacol. 2020;874:172975. doi: 10.1016/j.ejphar.2020.172975. [DOI] [PubMed] [Google Scholar]
- 85.Liu L., Li Y.H., Niu Y.B., Sun Y., Guo Z.J., Li Q., Li C., Feng J., Cao S.S., Mei Q.B. An apple oligogalactan prevents against inflammation and carcinogenesis by targeting LPS/TLR4/NF-κB pathway in a mouse model of colitis-associated colon cancer. Carcinogenesis. 2010;31:1822–1832. doi: 10.1093/carcin/bgq070. [DOI] [PubMed] [Google Scholar]
- 86.Zha L., Garrett S., Sun J. Salmonella Infection in Chronic Inflammation and Gastrointestinal Cancer. Diseases. 2019;7:28. doi: 10.3390/diseases7010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fantini M.C., Guadagni I. From inflammation to colitis-associated colorectal cancer in inflammatory bowel disease: Pathogenesis and impact of current therapies. Dig. Liver Dis. 2021;53:558–565. doi: 10.1016/j.dld.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 88.Yu T., Guo F., Yu Y., Sun T., Ma D., Han J., Qian Y., Kryczek I., Sun D., Nagarsheth N., et al. Fusobacterium nucleatum Promotes Chemoresistance to Colorectal Cancer by Modulating Autophagy. Cell. 2017;170:548–563.e16. doi: 10.1016/j.cell.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mishra V., Pathak C. Human Toll-Like Receptor 4 (hTLR4): Structural and functional dynamics in cancer. Int. J. Biol. Macromol. 2019;122:425–451. doi: 10.1016/j.ijbiomac.2018.10.142. [DOI] [PubMed] [Google Scholar]
- 90.Kamba A., Lee I.-A., Mizoguchi E. Potential association between TLR4 and chitinase 3-like 1 (CHI3L1/YKL-40) signaling on colonic epithelial cells in inflammatory bowel disease and colitis-associated cancer. Curr. Mol. Med. 2013;13:1110–1121. doi: 10.2174/1566524011313070006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ye K., Wu Y., Sun Y., Lin J., Xu J. TLR4 siRNA inhibits proliferation and invasion in colorectal cancer cells by downregulating ACAT1 expression. Life Sci. 2016;155:133–139. doi: 10.1016/j.lfs.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 92.Kuo W.-T., Lee T.-C., Yu L.C.-H. Eritoran Suppresses Colon Cancer by Altering a Functional Balance in Toll-like Receptors That Bind Lipopolysaccharide. Cancer Res. 2016;76:4684–4695. doi: 10.1158/0008-5472.CAN-16-0172. [DOI] [PubMed] [Google Scholar]
- 93.Wu Y., Wu J., Chen T., Li Q., Peng W., Li H., Tang X., Fu X. Fusobacterium nucleatum Potentiates Intestinal Tumorigenesis in Mice via a Toll-Like Receptor 4/p21-Activated Kinase 1 Cascade. Dig. Dis. Sci. 2018;63:1210–1218. doi: 10.1007/s10620-018-4999-2. [DOI] [PubMed] [Google Scholar]
- 94.Shi Y.-J., Gong H.-F., Zhao Q.-Q., Liu X.-S., Liu C., Wang H. Critical role of toll-like receptor 4 (TLR4) in dextran sulfate sodium (DSS)-Induced intestinal injury and repair. Toxicol. Lett. 2019;315:23–30. doi: 10.1016/j.toxlet.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 95.Fukata M., Chen A., Klepper A., Krishnareddy S., Vamadevan A.S., Thomas L.S., Xu R., Inoue H., Arditi M., Dannenberg A.L., et al. Cox-2 is regulated by toll-like receptor-4 (TLR4) signaling and is important for proliferation and apoptosis in response to intestinal mucosal injury. Gastroenterology. 2006;131:862–877. doi: 10.1053/j.gastro.2006.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fiorentini C., Carlini F., Germinario EA P., Maroccia Z., Travaglione S., Fabbri A. Gut Microbiota and Colon Cancer: A Role for Bacterial Protein Toxins? Int. J. Mol. Sci. 2020;21:6201. doi: 10.3390/ijms21176201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Candela M., Turroni S., Biagi E., Carbonero F., Rampelli S., Fiorentini C., Brigidi P. Inflammation and colorectal cancer, when microbiota-host mutualism breaks. World J. Gastroenterol. 2014;20:908–922. doi: 10.3748/wjg.v20.i4.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Grasso F., Frisan T. Bacterial Genotoxins: Merging the DNA Damage Response into Infection Biology. Biomolecules. 2015;5:1762–1782. doi: 10.3390/biom5031762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gargi A., Reno M., Blanke S. Bacterial toxin modulation of the eukaryotic cell cycle: Are all cytolethal distending toxins created equally? Front. Cell. Infect. Microbiol. 2012;2:124. doi: 10.3389/fcimb.2012.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Scott D.A., Kaper J.B. Cloning and sequencing of the genes encoding Escherichia coli cytolethal distending toxin. Infect. Immun. 1994;62:244–251. doi: 10.1128/iai.62.1.244-251.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fedor Y., Vignard J., Nicolau-Travers M.-L., Boutet-Robinet E., Watrin C., Salles B., Mirey G. From single-strand breaks to double-strand breaks during S-phase: A new mode of action of the Escherichia coli Cytolethal Distending Toxin. Cell. Microbiol. 2013;15:1–15. doi: 10.1111/cmi.12028. [DOI] [PubMed] [Google Scholar]
- 102.van Elsland D., Neefjes J. Bacterial infections and cancer. EMBO Rep. 2018;19:e46632. doi: 10.15252/embr.201846632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nougayrède J.-P., Homburg S., Taieb F., Boury M., Brzuszkiewicz E., Gottschalk G., Buchrieser C., Hacker J., Dobrindt U., Oswald E. Escherichia coli Induces DNA Double-Strand Breaks in Eukaryotic Cells. Science. 2006;313:848–851. doi: 10.1126/science.1127059. [DOI] [PubMed] [Google Scholar]
- 104.Healy A.R., Herzon S.B. Molecular Basis of Gut Microbiome-Associated Colorectal Cancer: A Synthetic Perspective. J. Am. Chem. Soc. 2017;139:14817–14824. doi: 10.1021/jacs.7b07807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wilson M.R., Jiang Y., Villalta P.W., Stornetta A., Boudreau P.D., Carrá A., Brennan C.A., Chun E., Ngo L., Samson L.D., et al. The human gut bacterial genotoxin colibactin alkylates DNA. Science. 2019;363:eaar7785. doi: 10.1126/science.aar7785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Stolfi C., Pallone F., Monteleone G. Colorectal Cancer Chemoprevention by Mesalazine and Its Derivatives. J. Biomed. Biotechnol. 2012;2012:980458. doi: 10.1155/2012/980458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dai L., Tang Y., Zhou W., Dang Y., Sun Q., Tang Z., Zhu M., Ji G. Gut Microbiota and Related Metabolites Were Disturbed in Ulcerative Colitis and Partly Restored After Mesalamine Treatment. Front. Pharmacol. 2021;11:620724. doi: 10.3389/fphar.2020.620724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Balish E., Warner T. Enterococcus faecalis Induces Inflammatory Bowel Disease in Interleukin-10 Knockout Mice. Am. J. Pathol. 2002;160:2253–2257. doi: 10.1016/S0002-9440(10)61172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Meeker S., Seamons A., Maggio-Price L., Paik J. Protective links between vitamin D, inflammatory bowel disease and colon cancer. World J. Gastroenterol. 2016;22:933–948. doi: 10.3748/wjg.v22.i3.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gubatan J., Moss A.C. Vitamin D in inflammatory bowel disease: More than just a supplement. Curr. Opin. Gastroenterol. 2018;34:217–225. doi: 10.1097/MOG.0000000000000449. [DOI] [PubMed] [Google Scholar]
- 111.Gubatan J., Mitsuhashi S., Longhi M.S., Zenlea T., Rosenberg L., Robson S., Moss A. Higher Serum Vitamin D Levels are Associated with Protective Serum Cytokine Profiles in Patients with Ulcerative Colitis. Cytokine. 2018;103:38–45. doi: 10.1016/j.cyto.2017.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gubatan J., Rubin S.J.S., Bai L., Haileselassie Y., Levitte S., Balabanis T., Patel A., Sharma A., Sinha S.R., Habtezion A. Vitamin D Is Associated with α4β7+ Immunophenotypes and Predicts Vedolizumab Therapy Failure in Patients with Inflammatory Bowel Disease. J. Crohns Colitis. 2021;15:1980–1990. doi: 10.1093/ecco-jcc/jjab114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Cantorna M.T., Waddell A. The vitamin D receptor turns off chronically activated T cells. Ann. N. Y. Acad. Sci. 2014;1317:70–75. doi: 10.1111/nyas.12408. [DOI] [PubMed] [Google Scholar]
- 114.Kongsbak M., Levring T., Geisler C., von Essen M. The Vitamin D Receptor and T Cell Function. Front. Immunol. 2013;4:148. doi: 10.3389/fimmu.2013.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Meeker S., Seamons A., Paik J., Treuting P.M., Brabb T., Grady W.M., Maggio-Price L. Increased dietary vitamin D suppresses MAPK signaling, colitis, and colon cancer. Cancer Res. 2014;74:4398–4408. doi: 10.1158/0008-5472.CAN-13-2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhang Y.G., Lu R., Wu S., Chatterjee I., Zhou D., Xia Y., Sun J. Vitamin D receptor protects against dysbiosis and tumorigenesis via the JAK/STAT pathway in intestine. Cell. Mol. Gastroenterol. Hepatol. 2020;10:729–746. doi: 10.1016/j.jcmgh.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ciubotaru I., Green S.J., Kukreja S., Barengolts E. Significant differences in fecal microbiota are associated with various stages of glucose tolerance in African American male veterans. Transl. Res. J. Lab. Clin. Med. 2015;166:401–411. doi: 10.1016/j.trsl.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liang X., Li H., Tian G., Li S. Dynamic microbe and molecule networks in a mouse model of colitis-associated colorectal cancer. Sci. Rep. 2014;4:4985. doi: 10.1038/srep04985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Singh P., Rawat A., Alwakeel M., Sharif E., Al Khodor S. The potential role of vitamin D supplementation as a gut microbiota modifier in healthy individuals. Sci. Rep. 2020;10:21641. doi: 10.1038/s41598-020-77806-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Charoenngam N., Shirvani A., Kalajian T.A., Song A., Holick M.F. The effect of various doses of oral vitamin D3 supplementation on gut microbiota in healthy adults: A randomized, double-blinded, dose-response study. Anticancer Res. 2020;40:551–556. doi: 10.21873/anticanres.13984. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.