Abstract
Simple Summary
Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest cancers worldwide, associated with a 98% loss of life expectancy and a 30% increase in disability-adjusted life years. Image-based artificial intelligence (AI) can help improve outcomes for PDAC given that current clinical guidelines are non-uniform and lack evidence-based consensus. However, research on image-based AI for PDAC is too scattered and lacking in sufficient quality to be incorporated into clinical workflows. In this review, an international, multi-disciplinary team of the world’s leading experts in pancreatic cancer breaks down the patient pathway and pinpoints the current clinical touchpoints in each stage. The available PDAC imaging AI literature addressing each pathway stage is then rigorously analyzed, and current performance and pitfalls are identified in a comprehensive overview. Finally, the future research agenda for clinically relevant, image-driven AI in PDAC is proposed.
Abstract
Pancreatic ductal adenocarcinoma (PDAC), estimated to become the second leading cause of cancer deaths in western societies by 2030, was flagged as a neglected cancer by the European Commission and the United States Congress. Due to lack of investment in research and development, combined with a complex and aggressive tumour biology, PDAC overall survival has not significantly improved the past decades. Cross-sectional imaging and histopathology play a crucial role throughout the patient pathway. However, current clinical guidelines for diagnostic workup, patient stratification, treatment response assessment, and follow-up are non-uniform and lack evidence-based consensus. Artificial Intelligence (AI) can leverage multimodal data to improve patient outcomes, but PDAC AI research is too scattered and lacking in quality to be incorporated into clinical workflows. This review describes the patient pathway and derives touchpoints for image-based AI research in collaboration with a multi-disciplinary, multi-institutional expert panel. The literature exploring AI to address these touchpoints is thoroughly retrieved and analysed to identify the existing trends and knowledge gaps. The results show absence of multi-institutional, well-curated datasets, an essential building block for robust AI applications. Furthermore, most research is unimodal, does not use state-of-the-art AI techniques, and lacks reliable ground truth. Based on this, the future research agenda for clinically relevant, image-driven AI in PDAC is proposed.
Keywords: pancreatic cancer, artificial intelligence, imaging, radiology, pathology
1. Introduction
Pancreatic cancer is one of the deadliest cancers worldwide, with a 5-year survival rate of less than 5% [1]. Pancreatic ductal adenocarcinoma (PDAC), the most common and aggressive type of pancreatic cancer, has become a medical emergency in the past decades. PDAC tumours present highly aggressive behavior, leading to 98% life expectancy loss and a 30% increase in disability-adjusted life years [2,3]. Recently, there have been some improvements in the survival rates of early-stage, resected patients following neo-adjuvant chemotherapy [4]. However, this translates into negligible increase in survival for the whole PDAC patient population as in the absence of effective prevention and screening protocols, most patients are diagnosed with advanced disease [4]. Still, research funding for PDAC remains significantly lower than for other cancer types, leading it to be flagged as a neglected cancer by both the European Commission and the United States Congress [2].
Cross-sectional imaging, namely computed tomography (CT), magnetic resonance (MR), 18fluoro-2-deoxy-d-glucose positron emission tomography/computed tomography (18FDG PET/CT), and endoscopic ultrasound (EUS), play a crucial role in PDAC management. Nevertheless, current international guidelines for image-based stratification, treatment response prediction, and evaluation are heterogeneous and ineffective [5]. Histopathology analysis is considered the gold standard for PDAC diagnosis and characterization. Still, it remains challenging even for experienced pathologists due to marked morphological tumour heterogeneity and the limited amount of tumour tissue in biopsy [6,7,8]. Moreover, histopathology evaluation of treatment response is imprecise, of limited clinical relevance, and affected by interobserver variation [9].
Artificial intelligence (AI) has gained considerable interest in oncology, as it has the potential to leverage high amounts of data to produce individualised recommendations based on each patient’s clinical picture [10]. As the volume of multi-modal data acquired in routine clinical practice increases, AI can support clinicians and ultimately guide decision making at each step of the patient pathway by focusing on well-validated applications at meaningful clinical touchpoints [10]. Commercial clinical AI is already a reality for diseases such breast, colon, and lung cancer, with multiple FDA-approved products on the market for applications such as disease screening, diagnosis, and tumour characterization [11]. Currently, there are two main approaches for image-based AI: radiomics and convolutional neural networks (CNNs). Radiomics predicts an outcome by feeding manually defined texture and shape features extracted from a region of interest to machine learning models. Deep learning-based CNNs, on the other hand, automatically compute the relevant features directly from the imaging during training, in a neural network comprising a sequence of convolutional and pooling operations. Since the introduction of AlexNet in 2012, CNNs have evolved enormously and are now dominating image analysis, but the transition from hand-crafted radiomic features to deep learning in the medical domain has been gradual [12,13].
The number of publications on AI for clinical decision-making in oncology has increased exponentially in the past few years [12]. However, AI research in PDAC is still at a preliminary stage compared to other cancer diseases, with limited private and public datasets and a lack of independent, external model validation. As a result, no AI applications have been implemented in clinical practice for PDAC.
The contributions of this review are threefold. First, an international, multi-disciplinary, multi-institutional expert panel breaks down the PDAC patient clinical pathway and identifies the most relevant clinical questions for image-based AI research. Second, we analyse the available literature addressing these clinical questions and identify current trends and knowledge gaps. Finally, we define the research agenda for clinical AI research in PDAC imaging, along with the necessary steps towards clinically relevant AI applications that can improve patient outcomes.
2. PDAC Patient Pathway
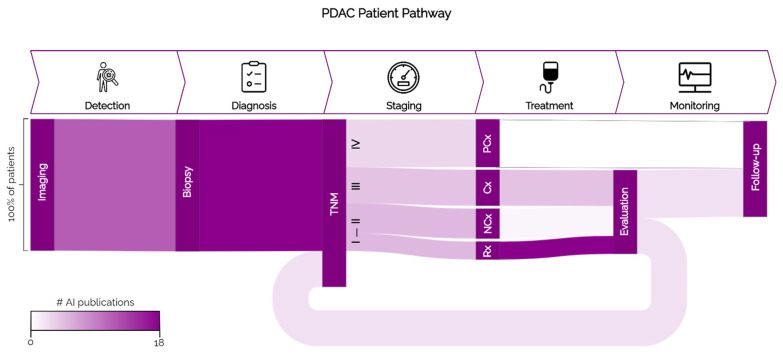
The typical cancer patient pathway is generally subdivided into five steps: detection, diagnosis, staging, treatment, and monitoring. In each step of the patient pathway there are critical patient and clinician decision-oriented touchpoints that could benefit from AI [10]. These touchpoints are specific for each cancer subtype and regard clinical decisions that are suboptimal with currently implemented workflows and guidelines [10]. The specific steps of the PDAC patient pathway are illustrated in Figure 1, and the clinical touchpoints for potential AI development in each step are explored in the following sections.
Figure 1.
PDAC patient pathway. The steps of the general cancer patient pathway are shown in the top part of the figure. Below, the vertical boxes show the actions/guidelines for PDAC used in each step. The width of the streams represents the proportion of patients that go through each branch of the pathway, and the colours of the streams represent the number of AI publications found on that topic. Rx: resection; nCTx: neoadjuvant chemo(radio)therapy; aCTx: adjuvant/induction therapy; Px: palliative care.
2.1. Detection
Timely detection is crucial to improve PDAC patients’ outcomes, as the 5-year survival increases from only 3% in metastatic patients to 42% when the tumour is still confined to the primary site [14]. According to the Japan Pancreatic Cancer Registry, patients in the earliest disease stage show a survival rate as high as 80.4% but account for only 0.8% of cases [15]. Due to the low incidence of PDAC, defining and screening groups at risk is a vital step to improve patient outcome. Research on risk factors, new screening protocols, and non-invasive tumour biomarkers is on the rise, but so far there are no validated biomarkers or tools for early detection. Therefore, screening is still not part of the PDAC patient pathway as it is cost-prohibitive with current technology. The most used modality for PDAC detection is multi-phase contrast-enhanced CT (CECT). However, early PDAC detection on CECT remains challenging, as lesions are small (size <2 cm), present poorly defined margins, and are more often iso-attenuating [5,16]. Radiologists’ sensitivity at detecting lesions with size smaller than 2 cm on CECT has been reported to be as low as 58% [5,16]. Contrast-enhanced MRI is highly effective at detecting tumours that are poorly visible on CECT, but is not yet routinely implemented in the clinic [17]. EUS is a widely accepted modality for the diagnosis of PDAC.
Early detection can be facilitated by the timely identification of secondary imaging signs predictive of PDAC, such as main pancreatic duct cut-off or dilation, parenchymal atrophy, and irregular pancreatic contour [5,18]. These signs are often visible on CECT scans 18 to 12 months prior to clinical diagnosis, but the reported radiologists’ sensitivity for their timely detection is only 44%, limiting the chances of early action [18].
2.2. Diagnosis
PDAC symptoms are mostly unspecific in early disease stages, and as lesional appearances are heterogeneous on CECT, patients are often initially misdiagnosed with other, more common abdominal diseases with similar symptomatology (e.g., gallbladder diseases, acute or chronic pancreatitis, duodenum cancer) [18,19]. Initially misdiagnosed patients are reported to present higher rates of abdominal pain, weight loss, and acute pancreatitis than correctly diagnosed patients, and are at a higher risk of advanced disease [19]. EUS is also a widely accepted imaging modality for the diagnosis of PDAC, especially for lesions less than 2–3 cm in size in which it reaches superior sensitivity compared to CT [20]. Furthermore, EUS has a high negative predictive value and can be used to reliably exclude pancreatic cancer [20]. Histopathology assessment is the current gold standard for PDAC diagnosis confirmation and is usually based on EUS fine-needle cytology or biopsy. Nevertheless, the morphological distinction of PDAC from other lesions on small biopsies or cytology samples can be challenging, especially given the minimal amount of lesional material that is often contained in these samples [21].
2.3. Staging
Following histopathology diagnosis, the most used method for PDAC staging is the TNM classification by the American Joint Committee on Cancer (AJCC). The local tumour extent (T stage), the dissemination to the regional lymph nodes (N stage), and the metastatic spread to distant sites (M stage) are used to stratify patients, determine their prognosis, and indicate treatment and monitoring strategy [19]. Nevertheless, the TNM classification’s predictiveness for overall survival (OS) is not reliable [21]. A 2018 multicentre study aiming to validate the AJCC TNM 8th edition in a cohort of 1525 patients receiving pancreatoduodenectomy reported a concordance index of 0.57 (95% CI, 0.55–0.60) for OS prediction [22].
2.4. Treatment
The most common treatment options for PDAC are resection and chemo(radio)therapy, in particular using FOLFIRINOX and gemcitabine–abraxane [2]. Surgical resection (Rx) is the only option for potential long-term survival, but as can be seen in Figure 1 is only suitable for a minority (10–15%) of patients (stages I, II). Most patients are diagnosed in later disease stages (III, IV) where Rx is no longer possible due to metastasis or extensive vessel involvement [23]. Imaging assessment of tumour-vascular contact primarily determines eligibility for Rx, but there are no widely accepted, evidence-based guidelines for the appropriate tumour resectability criteria [5,24]. As a result, the 5-year survival rate of resected PDAC patients is only 30–58%, with 69–75% of patients relapsing within two years [1,25].
As illustrated in Figure 1, most patients receive chemo(radio)therapy at some point during treatment [4]. Neo-adjuvant chemo(radio)therapy (nCTx) intends to optimise surgical outcome in patients with resectable disease, while adjuvant chemo(radio)therapy (aCTx) is used to downstage unresectable patients. After aCTx, patients may become resectable and undergo Rx or be referred to palliative care (Px), which is intended to suppress disease-related pain and lengthen the patient’s life. Although most patients experience chemotherapy-induced toxicity, often with limited efficacy due to biological resistance, a priori prediction of chemotherapy response is still not possible in current clinical work-up [26,27].
2.5. Treatment Monitoring
Following curative resection, histopathology analysis of the resected specimen is performed to confirm the diagnosis of PDAC and to map the extent of disease. This includes the assessment of lymph node metastases (LNM), tumour permeation along lymphatics/blood vessels, and the clearance to the resection margins (resection margin status) [28]. Nevertheless, the prognostic value of these parameters is still controversial, with several studies reporting no significant relationship to survival [28,29,30]. The main reasons for the low predictive power of histopathology findings are the lack of standardised evaluation, consensus definitions, and reporting approaches [31,32].
In patients undergoing chemo(radio)therapy, imaging is critical for determining therapeutic response and selection of the next treatment approach, as acquiring a biopsy could lead to an increase of inflammation [32]. The Response Evaluation Criteria in Solid Tumours (RECIST) 1.1 (2009) is the current standard to evaluate chemo(radio)therapy. This is a purely morphological criteria that quantitatively tracks tumour burden changes based on alterations to the lesions’ size. Although RECIST shows some success in monitoring response based on metastases assessment, it is ineffective when considering the primary tumour, as PDAC lesions present poorly defined borders and significant heterogeneity in regression/progression patterns [32]. Furthermore, chemo(radio)therapy often results in necrotic, fibrous, or inflammatory changes, which translate into an apparent enlargement of the lesion in CT/MRI scans that can be misinterpreted as tumour progression [32].
Current histopathological tumour regression grade (TRG) systems for PDAC are based on a semiquantitative evaluation of the destruction of cancer cells, the amount of residual viable cancer, or the extent of fibrosis induced by treatment. However, current TRG systems are based on imprecise, difficult-to-apply criteria, and a standardised and widely accepted grading system for the histological evaluation of TRG in pancreatic cancer has not yet been established [9,33,34]. These factors make RECIST and histopathology TRG insufficient for predicting local oncological response in PDAC patients [31,32].
3. Materials and Methods
Searches were conducted on PubMed, Web of Science, Cochrane, and Embase on 14 September 2021 and updated on 25 January 2022. Additional information about the search strategy can be found in Appendix A and Table A1. Articles were included for evaluation if patient information was available, cohort size was larger than 20 patients, AI was developed to predict a given outcome related to PDAC, and the proposed AI model used imaging (CT, MRI, EUS, PET-CT, whole-slide images (WSI)) as input. Articles were excluded if the research used non-human subjects, did not show any performance, did not report how results were validated.,or used the same cohort for training and reporting of the results.
4. Results
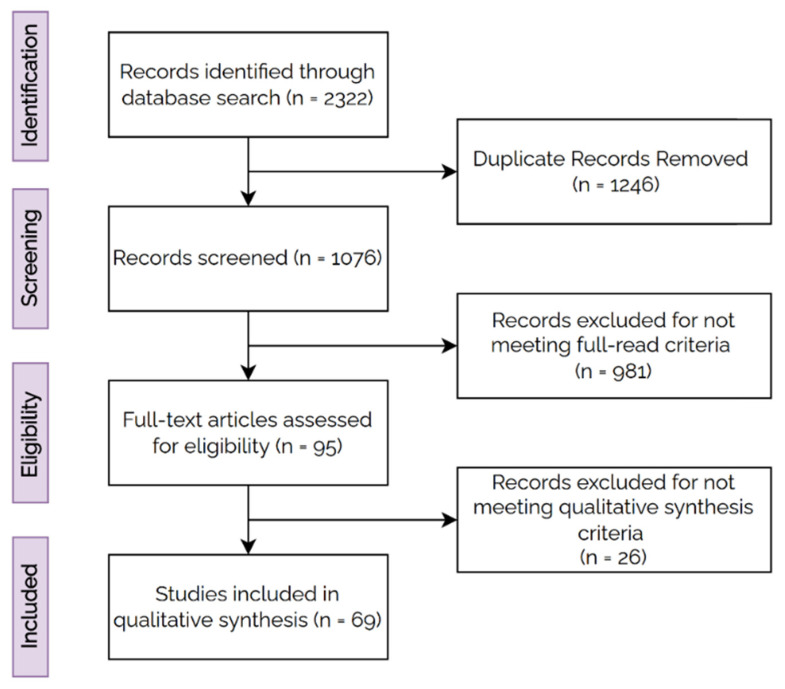
A total of 2322 records were retrieved from the electronic databases, and 1076 articles remained after duplicate removal. Titles and abstracts were reviewed on the basis of the inclusion criteria, and 95 articles were eligible for full-text screening. Finally, a total of 69 studies fulfilled the inclusion criteria and were considered for analysis. The flowchart for the inclusion of studies is shown in Figure 2.
Figure 2.
PRISMA Flowchart for inclusion criteria.
4.1. Detection
Eleven articles addressed AI for automated PDAC detection (Table 1). Only three articles stratified the results based on tumour size, reporting model performance for the subgroup of lesions with sizes smaller than 2 cm [35,36,37]. Two papers (Alves et al. (2022) and Wang et al. (2021)) reported the results for both lesion detection and localization, and only one paper proposed a fully automatic approach (Alves et al. (2022)) [35,38]. The study by Liu et al. (2020) was the only one comparing AI performance to radiologists based on the analysis of radiology reports, but no reader study was conducted [37]. As is shown in Table 1, only three studies externally tested the proposed models, and four articles used internal cross-validation without separate testing set [35,36,37,38,39,40,41].
Table 1.
Summary of papers on AI for PDAC detection. The performance for the validation and test sets is reported with respective 95% Confidence Interval or standard deviation when it was provided.
| Authors (Year) | Data | Approach | Model | Metric | Validation Performance | Test Performance | Dev. Cohort | Test Cohort |
|---|---|---|---|---|---|---|---|---|
| Alves et al. (2022) [35] | CT | DL | 3D nnU-Net |
AUC | 0.991 (0.970–1.0) |
** 0.889 (0.833–0.946) |
242 | ** 361 |
| Wang et al. (2021) [38] | CT | DL | 2D U-Net | SEN, SPE | 0.998, 0.965 | .. | 800 | .. |
| Liu et al. (2020) [37] | CT | DL | 2D VGG | AUC | 1.000 (0.999–1.000) |
* 0.997 (0.992–1.000) * 0.999 (0.998–1.000) ** 0.920 (0.891–0.948) |
412 | * 139 * 189 ** 363 |
| Ma et al. (2020) [39] | CT | DL | 2D 4-layer CNN | AUC | 0.9652 | .. | 412 | .. |
| Tonozuka et al. (2020) [42] | EUS | DL | 2D 7-layer CNN | AUC | 0.924 | * 0.940 | 93 | * 47 |
| Qiu et al. (2021) [43] | CT | Radiomics | SVM | AUC | 0.88 (0.84–0.92) |
* 0.79 (0.71–0.87) |
312 | * 93 |
| Chen et al. (2021) [36] | CT | Radiomics | XGBoost | AUC | .. | * 0.98 (0.96–0.99) ** 0.76 (0.71–0.82) |
944 | * 383 ** 212 |
| Chu et al. (2020) [40] | CT | Radiomics | RF | SEN, SPE, ACC | 0.950, 0.923, 0.936 | .. | 380 | .. |
| Chu et al. (2019) [44] | CT | Radiomics | RF | AUC | .. | * 0.999 | 255 | * 125 |
| Li et al. (2018) [41] | 18FDG PET-CT | Radiomics | SVM-RF | SEN, SPE, ACC | 0.952 ± 0.009, 0.975 ± 0.004, 0.965 ± 0.007 | .. | 80 | .. |
| Ozkan et al. (2015) [45] | EUS | Radiomics | ANN | SEN, SPE, ACC | .. | * 0.833 ± 0.112, 0.933 ± 0.075, 0.875 ± 0.047 | 172 | * 72 images |
** external test set, * internal test set. Abbreviations are: DL—deep learning, XGBoost—extreme gradient boost, SVM—support vector machine, VGG—visual geometry group, RF—random forest, ANN—artificial neural network, CNN—convolutional neural network, AUC—area under the receiver operating characteristic curve, SEN—sensitivity, SPE—specificity, ACC—accuracy, Dev. Cohort—development cohort (training + validation).
4.2. Diagnosis
Eighteen papers explored AI for differential PDAC diagnosis (Table 2). The majority of papers (14/18) focused on radiology imaging, mostly (13/14) regarding binary classification between PDAC and another type of lesion, with only one paper tackling multiclass classification [46]. Three publications focused on AI for the histopathological diagnosis of PDAC. Fu et al. (2021) and Naito et al. (2021) proposed DL approaches for PDAC diagnosis and segmentation in WSI, while Kriegsmann et al. (2021) were the first to utilise DL to automatically identify different anatomical tissue structures and diseases on WSI [8,47,48]. AI validation is limited. Only three studies externally tested the proposed models, while nine papers had internal cross-validation, without a separate testing set [8,46,49].
Table 2.
Summary of papers on AI for PDAC differential diagnosis. The performance for the validation and test sets is reported with respective 95% Confidence Interval or standard deviation when it was provided.
| Authors (Year) | Tissues of Interest | Data | Approach | Model | Metric | Validation Results | Test Results |
Dev. Cohort |
Test Cohort |
|---|---|---|---|---|---|---|---|---|---|
| Si et al. (2021) [46] | PDAC, IPMN, SCN, other | CT | DL | ResNet + U-Net |
ACC | .. | ** 0.827 | 319 | ** 347 |
| Naito et al. (2021) [47] | PDAC | WSI | DL | EfficientNet-B1 | AUC | .. | * 0.984 (0.960–0.998) |
413 | * 120 |
| Fu et al. (2021) [8] | PDAC | WSI | DL | Inception + U-Net | ACC | .. | * 1.0 ** 0.904 |
90 | * 47 ** 52 |
| Kriegsmann et al. (2021) [48] | PDAC | WSI | DL | EfficientNet | BACC | .. | * 0.921 | 201 | .. |
| Ziegelmayer et al. (2020) [50] | PDAC, AIP | CT | DL | RF | AUC | 0.90 ± 0.02 | .. | 86 | .. |
| Liu et al. (2019) [51] | PDAC | CT | DL | Faster R-CNN |
AUC | .. | * 0.9632 | 238 | * 100 |
| Saftoiu et al. (2015) [52] | PDAC, MFP | EUS | ML | 2-layer ANN | SEN, SPE | .. | * 0.946 (0.882–0.978), 0.944 (0.839–0.986) |
142 | * 25 |
| Ebrahimian et al. (2021) [53] | Benign vs Malignant | CT | Radiomics | RF | AUC | .. | * 0.76 | 59 | * 44 |
| Deng et al. (2021) [49] | PDAC, MFP | MR | Radiomics | SVM | AUC | 0.997 (0.990–1.0) |
** 0.962 (0.907–1.0) |
64 | ** 55 |
| Ma et al. (2021) [54] | PDAC, CP | CT + clinical | Radiomics | LASSO | AUC | 0.980 (0.961–1.000) |
.. | 175 | .. |
| Liu et al. (2021) [55] | PDAC, AIP | 18FDG PET-CT | Radiomics | SVM | AUC | 0.966 ± 0.008 | .. | 112 | .. |
| Ren et al. (2020) [56] | PDAC, PAC | CT | Radiomics | RF | AUC | 0.82 | .. | 112 | .. |
| Ren et al. (2020) [57] | PDAC, MFP | CT | Radiomics | RF | AUC | 0.98 (0.97–1.0) |
.. | 109 | .. |
| Park et al. (2020) [58] | PDAC, AIP | CT | Radiomics | RF | AUC | .. | * 0.975 (0.936–1.0) |
120 | * 62 |
| He et al. (2019) [59] | PDAC, PNEN | CT | Radiomics | LASSO | AUC | 0.960 (0.942–0.979) |
* 0.884 (0.831–0.927) |
100 | * 47 |
| Ren et al. (2019) [60] | PDAC, MFP | CT | Radiomics | LR | AUC | .. | * 0.9 | 109 | * 40 |
| Zhang et al. (2019) [61] | PDAC, AIP | 18FDG PET-CT | Radiomics | SVM- RF | AUC | 0.93 | .. | 111 | .. |
| Saftoiu et al. (2012) [62] | PDAC, CP | EUS | Radiomics | 2-layer ANN | AUC | 0.94 (0.91–0.97) |
.. | 258 | .. |
** external test set, * internal test set. Abbreviations are: MFP—mass-forming pancreatitis, CP—chronic pancreatitis, AIP—autoimmune pancreatitis, IPMN—intraductal papillary mucinous neoplasm, SCN—serous cystic neoplasm, PNEN—pancreatic neuroendocrine neoplasms, PAC—pancreatic adenosquamous carcinoma, DL—deep learning, ML—machine learning, SVM—supported vector machine, RF—random forest, LASSO—least absolute shrinkage and selection operator, LR—logistic regression, ANN—artificial neural network, AUC—area under the receiver operating characteristic curve, SEN—sensitivity, SPE—specificity, BACC—balanced accuracy, Dev. Cohort—development cohort (training + validation).
4.3. Staging
Thirteen AI papers covered staging (Table 3). Only one publication considered histopathological data. Two articles (An et al., (2021) and Chaddad et al., (2020)) used DL, with the remaining majority using radiomics [63,64]. Most papers considered surrogate end points (histological grade of differentiation, presence of LNM, etc.) as ground truth for model development, with only one considering OS. The study from Chaddad et al., (2021) divided patients into short- and long-term survivors with a set threshold [64]. Only two papers used an external dataset to validate their performance [65,66].
Table 3.
Summary of papers on AI for stratification of PDAC patients. The performance for the validation and test sets is reported with respective 95% Confidence Interval or standard deviation when it was provided.
| Authors (Year) | Ground Truth | Data | Approach | Model | Metric | Validation Performance | Test Performance | Dev. Cohort |
Test Cohort |
|---|---|---|---|---|---|---|---|---|---|
| An et al. (2021) [63] | LNM | CT + clinical | DL | Resnet-18 | AUC | 0.90 (0.88–0.92) |
* 0.92 (0.91–0.92) |
113 | * 35 |
| Chaddad et al. (2020) [64] | Short term vs. long-term survival | CT | DL + ML | CNN + RF | AUC | 0.72 | .. | 159 | .. |
| Song et al. (2013) [67] |
Grading 1 vs. 2 |
WSI | ML | SVM | AUC | 0.79 | .. | 240 | .. |
| Bianet al. (2022) [68] | LNM | MR | Radiomics | LR | AUC | 0.75 (0.68–0.82) |
* 0.81 (0.69–0.94) |
180 | * 45 |
| Shi et al. (2022) [65] | LNM | MR + clinical | Radiomics | LR | AUC | 0.909 (0.854–0.964) |
* 0.835 (0.751–0.919) ** 0.805 (0.720–0.890) |
199 | ** 52 |
| Bian et al. (2021) [69] |
TIL | MR | Radiomics | XGBoost | AUC | 0.86 (0.79–0.93) |
* 0.79 (0.64–0.93) |
116 | * 40 |
| Cen et al. (2021) [70] | Stage I–II vs. Stage III–IV |
CT | Radiomics | LR | AUC | 0.940 (0.871–0.979) |
* 0.912 (0.781–0.978) |
94 | * 41 |
| Zhang et al. (2021) [71] | Liver metastasis vs. other metastasis | CT | Radiomics | RF | AUC | 0.81 | .. | 77 | .. |
| Xing et al. (2021) [72] | Grading 1 vs. 2/3 |
18FDG PET-CT | Radiomics | XGBoost | AUC | .. | * 0.921 (0.846–0.996) |
99 | * 50 |
| Kaissis et al. (2020) [73] | QMS | CT | Radiomics | RF | AUC | 0.93 ± 0.01 | .. | 181 | .. |
| Chen et al. (2020) [74] | PV-SMV invasion | CT | Radiomics | ElasticNet | AUC | 0.871 (0.795–0.946) |
* 0.848 (0.724–0.971) |
88 | 58 |
| Liu et al. (2020) [75] |
LNM | CT | Radiomics | LR | AUC | 0.841 (0.768–0.925) |
.. | 85 | .. |
| Li et al. (2020) [76] |
LNM | CT + clinical | Radiomics | LR | AUC | .. | * 0.912 (0.778–1) |
118 | *41 |
| Chang et al. (2020) [66] | Grading 1/2 vs. 3 |
CT | Radiomics | LASSO | AUC | 0.961 (0.935–0.987) |
* 0.91 (0.864–0.956) ** 0.77 (0.661–0.878) |
151 | * 150 ** 100 |
| Longlong et al. (2020) [77] |
Grading 1 vs. 2 vs. 3 |
CT | Radiomics | RF | AUC | 0.77 (0.64–0.87) |
* 0.70 (0.47–0.86) |
58 | * 25 |
| Qiu et al. (2019) [78] |
Grading 1/2 vs. 3 |
CT | Radiomics | SVM | SEN, SPE, ACC |
78 95 86 |
.. | 56 | .. |
** external test set, * internal test set. Abbreviations are: LNM—lymph node metastasis, TIL—tumour infiltrating lymphocytes, Grading—grade comparison (low vs. high), QMS—quasi mesenchymal subtype, PV-SMV—portal vein superior mesenteric vein, DL—deep learning, ML—machine learning, SVM—supported vector machine, RF—random forest, LR—logistic regression, CNN—convolutional neural network, XGBoost—extreme gradient boost, AUC—area under the receiver operating characteristic curve, SEN—sensitivity, SPE—specificity, ACC—accuracy, Dev. Cohort—development cohort (training + validation).
4.4. Treatment
Twenty-two studies use pre-treatment imaging to predict treatment response, with the majority of studies (17/22) focusing on patients diagnosed with resectable disease (Table 4). Eleven studies expressed treatment response by predicting OS, of which two (Healy et al., and Zhang et al.) validated the performance in an external cohort [79,80]. Six articles used deep learning (three with the same cohort), with the remaining 16 using radiomics.
Table 4.
Summary of papers on AI for PDAC treatment response prediction. The performance for the validation and test sets is reported with respective 95% Confidence Interval or standard deviation when it was provided.
| Authors (Year) | Treatment | Predict | Data | Approach | Model | Metric | Validation Results | Test Results |
Dev. Cohort |
Test Cohort |
|---|---|---|---|---|---|---|---|---|---|---|
| Yao et al. (2021) [81] | Resection | OS | CT | DL | Conv- LSTM |
CI | 0.667 | .. | 296 | .. |
| Zhang et al. (2020) [80] | Resection | OS | CT | DL | CNN | CI | .. | ** 0.651 | 68 | ** 30 |
| Watson et al. (2020) [82] | Chemotherapy | PR vs. NR | CT + clinical |
DL | LeNet | AUC | .. | * 0.785 | .. | * 65 |
| Zhang et al. (2021) [83] | Resection | 2-year survival | CT | DL + ML | RF | AUC | .. | * 0.84 (0.70–0.98) |
68 | * 30 |
| Li et al. (2021) [84] | Resection | 1-year and 2-year recurrence risk | CT + clinical | DL + ML | ANN | AUC | 0.916 (0.860–0.955) 0.872 (0.809–0.921) |
** 0.764 (0.644–0.859) ** 0.773 (0.654–0.866) |
153 | ** 47 |
| Zhang et al. (2020) [83] | Resection | Death risk | CT | DL + ML | RF | AUC | 0.72 (0.58–0.86) |
** 0.81 (0.64–0.98) |
68 | ** 30 |
| Healy et al. (2021) [79] | Resection | OS | CT | Radiomics | CPH | CI | 0.626 (0.625–0.627) |
** 0.545 (0.543–0.546) |
352 | ** 215 |
| Shi et al. (2021) [85] | Resection | OS | CT | Radiomics | CPH | CI | 0.74 (0.70–0.78) |
* 0.73 (0.66–0.79) |
210 | * 89 |
| Wei et al. (2021) [86] | Resection | 1-year RFS | 18FDG PET-CT | Radiomics | CPH | CI | 0.890 (0.835–0.945) |
* 0.865 (0.778–0.952) |
109 | * 47 |
| Xie et al. (2020) [87] | Resection | OS | CT | Radiomics | CPH | CI | .. | * 0.726 (0.646–0.806) |
147 | * 73 |
| Park et al. (2020) [88] | Resection | OS | CT | Radiomics | RF | CI | 0.74 | .. | 153 | .. |
| Parr et al. (2020) [89] | Radiotherapy | OS | CT | Radiomics | CPH | CI | 0.68 | .. | 74 | .. |
| Kaissis et al. (2020) [90] | Resection | OS | CT + clinical + genomics |
Radiomics | LPCA | CI | 0.65 (0.60–0.69) |
.. | 103 | |
| Hui et al. (2020) [91] | Resection margin | R0 vs. R1 | CT | Radiomics | SVM | AUC | 0.8641 | .. | 86 | .. |
| Bian et al. (2020) [92] | Resection margin | R0 vs. R1 | CT | Radiomics | LR | AUC | 0.750 (0.672–0.824) |
.. | 181 | .. |
| Tang et al. (2019) [93] | Resection | NER (>12 months) vs. ER (<12 months) |
MR | Radiomics | LR | AUC | 0.802 (0.721–0.868) |
* 0.807 (0.677–0.902) ** 0.781 (0.699–0.850) |
177 | * 74 ** 126 |
| Zhou et al. (2019) [94] | Irradiation stent | RSFS | CT | Radiomics | CPH | CI | 0.791 (0.614–0.967) |
* 0.779 (0.504–1.000) |
74 | * 32 |
| Cozzi et al. (2019) [95] | Radiotherapy | OS | CT | Radiomics | CPH | CI | .. | * 0.75 ± 0.03 | 60 | * 40 |
| Kaissis et al. (2019) [96] | Chemotherapy | OS | MR | Radiomics | GBDT | CI | 0.71 (0.60–0.80) |
.. | 55 | .. |
| Kaissis et al. (2019) [97] | Resection | Above vs. below average OS | MR | Radiomics | RF | AUC | 0.93 ± 0.07 | * 0.9 | 102 | * 30 |
| Chakraborty et al. (2017) [98] | Resection | Survival < 2 years vs. survival > 2 years | CT | Radiomics | Bayes | AUC | 0.9 | .. | 35 | .. |
| Cui et al. (2016) [99] | Radiotherapy | OS | 18FDG PET-CT | Radiomics | CPH | CI | 0.623 | * 0.661 (0.418–0.841) |
90 | * 49 |
** external test set, * internal test set. Abbreviations are: PR—pathological response, NR—no response, NER—non-early recurrence, ER—early recurrence, RFS—recurrence-free survival, RSFS—restenosis-free survival, DL—deep learning, ML—machine learning, SVM—supported vector machine, RF—random forest, CPH—Cox proportional hazard, GBDT—gradient-boosted decision tree, LPCA—linear principle component analysis, LR—logistic regression, ANN—artificial neural network, AUC—area under the receiver operating characteristic curve, CI—concordance index, Dev. Cohort—development cohort (training + validation).
4.5. Treatment Monitoring
We found two publications regarding treatment evaluation and no publications for follow-up. The study by Janssen et al. (2021) takes a step in the direction of more objective and reproducible TRG systems for patients undergoing nCTx by automatically segmenting relevant structures on WSI of resection specimens [100]. The authors used a cohort of 64 specimens and achieved F1-scores of 0.86 ± 0.09, 0.74 ± 0.12, and 0.86 ± 0.07 for the segmentation of tumour, normal ducts, and remaining non-tumour epithelium, respectively. Nasief et al. (2019) proposed an AI model based on delta radiomics from daily longitudinal scans to predict response to neoadjuvant chemoradiation therapy [101]. This study included 90 patients, divided into good and poor responders based on a modified Ryan Scheme for histopathology-based TRG, and the model achieved an AUC of 0.98 in the independent test set (40 patients) [101].
5. Discussion
Clinically relevant AI is developed to assist, replace, or go beyond clinicians’ knowledge on solving problems that affect patient outcomes. AI can significantly impact healthcare by leveraging big data, especially in neglected diseases such as PDAC, but it is essential that research is performed at high-quality standards and focuses on clinical validity, utility, and usability [10].
There are critical steps in the PDAC patient pathway where clinical guidelines are still lacking. In this review, such moments and subsequent opportunities for AI research are identified in consensus by a consortium of radiologists, pathologists, and AI experts from multiple international institutions. We propose that for radiology and pathology AI to advance PDAC care, future research should focus on early diagnosis, data-driven tumour characterisation, survival-based patient staging, treatment response prediction, and monitoring.
Early detection, arguably the most pressing issue in PDAC management, is closely linked to identifying small lesions and secondary anatomical signs [102]. However, our results show this is still not considered in AI-based detection research, as there are no studies on pre-diagnostic detection of secondary signs, and most studies do not disaggregate performance based on tumour size/stage. Additionally, there is a lack of research on lesion localization and a general absence of well-curated datasets, with positive and negative cases being retrieved from completely different populations, which does not reflect the clinical landscape and can introduce bias. For AI to improve PDAC detection, it is crucial to acquire and make publicly available well-curated, multimodal datasets that contain a significant proportion of small (<2 cm or even <1 cm) tumours, which should be treated as a subgroup of interest when reporting model performance.
Current research separates detection, which is defined as distinction between PDAC patients and healthy controls, from differential diagnosis, defined as distinction between PDAC and other types of pancreatic lesions. Only one study developed AI for simultaneous detection and characterisation of pancreatic lesions on CECT [46]. The remaining publications focused on binary distinction between PDAC and one other malignancy, limiting the proposed models’ clinical use. Furthermore, it is important to consider that PDAC diagnosis currently relies on high-quality, adequate imaging with multi-phasic scanning protocols, which may not be widely available due to resource limitations. In the future, research should strive towards a single-use case for radiology-based AI in PDAC diagnosis that includes both the detection of a lesion and its correct classification among a variety of pancreatic diseases in accessible, standard-of-care imaging. The current priority is the curation of large datasets with representative percentages of each lesion type and the integration of different imaging modalities that offer complementary information regarding lesion characterisation.
Research in AI for histopathological PDAC diagnosis is scarce. Only three publications were found to address this topic. While histopathology is considered the gold standard for confirming PDAC diagnosis, it is a time-consuming process that suffers from non-uniform implementation in clinical practice and interobserver variability. Developing powerful AI models for histopathological PDAC diagnosis is fundamental to advance AI research at all steps of the patient pathway. Such models would optimise clinical workflows and empower the generation of reliable ground truth, which could be employed to develop AI with other (non-invasive) modalities, in a timely and cost-effective manner.
AI for PDAC staging lacks a solid reference standard. TNM staging and histopathological grade do not correlate sufficiently with OS and suffer from inter-reader variability. Yet, most AI publications (12/13) focused on grade differentiation and LNM prediction. Only one study considered OS as the outcome, dividing patients into short- and long-term survival based on a threshold derived from the development cohort [64]. In the absence of an international consensus that relates surrogate endpoints to survival, AI research using clinically obtained low- and high-grade differentiation and predicting LNM is not clinically relevant. Future AI research should focus on discovering new data-driven staging biomarkers that relate histopathology and imaging to OS.
AI research for treatment response prediction disproportionally focuses on post-surgery patient outcome, with most included papers considering only resectable patients. Given that 80–85% of patients are diagnosed with unresectable disease, AI research on prediction of response to resection will have a minor impact on improving overall PDAC patients’ outcomes [103]. Instead, research efforts should focus on later disease stages, predicting response to (neo-)adjuvant/palliative chemo(radio)therapy. While most papers addressing treatment response considered survival as the outcome measure, there were also publications that aimed at predicting resection margin status and histopathology-based treatment effect. AI should not focus on these endpoints as they do not accurately reflect whether a patient responds to treatment. There were no publications considering multiple treatment options, with all studies focusing on the prediction of response to a single treatment regime. Future AI research should consider multiple treatment options for a given patient, providing the most favourable suggestion based on survival as the outcome measure.
AI research for treatment monitoring is lagging behind, as to date only two publications considered post-treatment imaging to evaluate response. The results from a segmentation network approach (Janssen et al. (2021)) are promising, but they were not validated externally, and further research is necessary to integrate this AI tool into a reliable TRS system for neoadjuvant chemotherapy [100]. Nasief et al. (2019) used longitudinal scans to monitor chemoradiotherapy response, but the authors considered the histopathology-based treatment response as ground truth [101]. Clinically relevant AI applications should directly predict OS and recurrence from large, well-curated radiology and pathology datasets. Additionally, AI algorithms for treatment monitoring should strive to assist clinicians by indicating the best action at a given time-point, such as timely termination of treatment to prevent unnecessary comorbidities, selecting re-staging time points, adjusting the treatment regime, or choosing the optimal schedule for long-term patient follow-up.
Overall, four main research agenda topics emerge from this comprehensive literature review for clinical image-based AI in PDAC (Table 5). First, there is an urgent need for more and good quality data. Large, well-curated, multi-institutional private and public PDAC datasets are essential for AI development and testing. This allows deep neural networks to extract powerful predictive and diagnostic biomarkers that generalise well in multiple cohorts. Second, easily accessible radiomics AI still dominates the field, with comparatively little work on much more powerful deep learning CNNs. As data availability and quality increases, research should focus on developing models that are entirely and exclusively data-driven. Third, the entire research field needs to globally shift to using better-quality ground truths that represent actual clinical endpoints (such as OS and disease-free survival) as the gold standard for model development. Clinical guideline parameters such as TNM staging, histopathology-based tumour response scores, margin status, and RECIST are hardly predictive of patient outcomes and should not be considered a valid outcome for AI model development. AI in PDAC should improve current clinical workflow rather than replicate/automate existing ineffective practices. Finally, the realm of multimodal AI for PDAC remains unexplored. In a complex and heterogeneous disease such as PDAC, combining information from imaging, histopathology, genetics, and clinical records is crucial to discovering meaningful patterns in the data and building robust prediction models. AI-based imaging biomarkers that stratify PDAC phenotypes predictive of outcome can support individualised care, for instance through the development of pharmacogenomic treatment regimes.
Table 5.
Overview of the main topics for future clinical AI research in PDAC imaging.
| Research Agenda for Clinical AI in PDAC Imaging |
|---|
|
6. Conclusions
In conclusion, the future of AI in PDAC lies in addressing the relevant clinical questions, establishing multi-institutional collaborations for the curation of large-scale datasets, and integrating multiple data modalities. By putting forward these issues in the context of current image-based AI literature for PDAC, we hope to help advance meaningful research that will ultimately translate into the improvement of PDAC outcomes, by helping to select the best treatments, for the right patients, at the right time.
Acknowledgments
The PANCAIM consortium partners that contributed to this work are Geert Litjens, David Chang, Caroline Verbeke, Núria Malats, and Matthias Löhr. G.L. contributed to supervision and writing—review and editing. D.C., C.V., N.M., and M.L. contributed to the writing—review and editing.
Appendix A
This scoping review adhered to the PRISMA guidelines. Searches were conducted on PubMed, Web of Science, Cochrane, and Embase on 14 September 2021, and updated on 25 January 2022. The used search string was the following.
Table A1.
Search strategy. MeSH terms and keywords for the included databases.
| Database | Search Strategy |
|---|---|
| PubMed | (“Pancreatic Neoplasms”(Mesh:NoExp) OR “Carcinoma, Pancreatic Ductal”(Mesh) OR “Pancreatic Intraductal Neoplasms”(Mesh) OR (Pancrea*(tiab) AND (Neoplasm*[tiab] OR cancer*[tiab] OR Carcinoma*[tiab] OR Adenocarcinoma*[tiab])) OR PDAC(tiab)) AND (“Artificial Intelligence”(Mesh) OR AI(tiab) OR Artificial Intelligence(tiab) OR CNN(tiab) OR Convnet(tiab) OR Deep Learning(tiab) OR Machine learning (tiab) OR Neural network*(tiab) OR pathomic*(tiab) OR radiomic*(tiab) OR supervised Learning(tiab) OR Transfer Learning(tiab) OR Unet(tiab) OR unsupervised Learning(tiab)) |
| Embase | (“Pancreatic Neoplasms” or “Carcinoma, Pancreatic Ductal” or “Pancreatic Intraductal Neoplasms” or (Pancrea* and (Neoplasm* or cancer* or Carcinoma* or Adenocarcinoma*)) or PDAC).mp. and (“Artificial IntelligenceOR AI” or CNN or Convnet or “Deep Learning” or “Machine learning” or “Neural network*” or pathomic* or radiomic* or “supervised Learning” or “Transfer Learning” or Unet or “unsupervised Learning”). |
| Web of Science | (TS = ((“Pancreatic Neoplasms” OR “Carcinoma, Pancreatic Ductal” OR “Pancreatic Intraductal Neoplasms” OR (Pancrea* AND (Neoplasm* OR cancer* OR Carcinoma* OR Adenocarcinoma*)) OR PDAC))) AND TS = ((“Artificial Intelligence”OR AI OR CNN OR Convnet OR “Deep Learning” OR “Machine learning” OR “Neural network*” OR pathomic* OR radiomic* OR “supervised Learning” OR “Transfer Learning” OR Unet OR “unsupervised Learning”)) |
| Cochrane | (“Pancreatic Neoplasms”(Mesh:NoExp) OR “Carcinoma, Pancreatic Ductal”(Mesh) OR (Pancrea*[tiab] AND (Neoplasm*[tiab] OR cancer*[tiab] OR Carcinoma*[tiab] OR Adenocarcinoma*[tiab])) OR PDA*(tiab)) AND (“Artificial Intelligence”(Mesh) OR AI(tiab) OR Artificial Intelligence(tiab) OR CNN(tiab) OR Convnet(tiab) OR Deep Learning(tiab) OR Machine learning (tiab) OR Neural network*(tiab) OR pathomic*(tiab) OR radiomic*(tiab) OR supervised Learning(tiab) OR Transfer Learning(tiab) OR Unet(tiab) OR unsupervised Learning(tiab)) |
Two independent reviewers (M.S. and N.A.) screened the titles and subsequently reviewed all full-text articles based on preselected variables to compare results. A third independent expert reviewer (P.V.) reviewed the full-text articles for digital pathology imaging. Conflicting evaluations were resolved by discussions between the three reviewers.
Inclusion criteria and corresponding number of records excluded at each step (n) were the following:
Full-read criteria:
-
(1)
Study was published in a peer-reviewed journal and was not an abstract, review paper, conference paper, commentary, editorial, or not available. (n = 293)
-
(2)
Study considered patients clinically diagnosed with pancreatic cancer (pancreatic ductal adenocarcinoma or non-specified type of pancreatic cancer). (n = 343)
-
(3)Study used AI to predict an outcome related to one of the following tasks (n = 289):
-
○Detection: determine the presence or absence of PDAC in an input image with or without localization of the tumours.
-
○Diagnosis: differentiate between PDAC and other benign and/or malignant pancreatic lesions.
-
○Staging: stratify PDAC patients into different subgroups based on clinical/histopathological outcomes or survival.
-
○Treatment indication: predict treatment response based on pre-treatment data.
-
○Treatment response prediction: monitor treatment response based on follow-up data.
-
○
-
(4)
Study used medical images as input. Included modalities were computed tomography (CT), magnetic resonance (MR), ultrasound (EUS), 18fluoro-2-deoxy-d-glucose positron emission tomography/computed tomography (18FDG PET/CT), and whole-slide images (WSI). (n = 56)
Qualitative synthesis criteria:
-
(5)
Study included a population larger than 20 patients. (n = 3)
-
(6)
Clinical information regarding patients in the used cohorts was available. Minimum required fields were: number of patients, age distribution, and sex distribution. (n = 14)
-
(7)
Study reports results in at least one patient cohort not used to train the model. (n = 3)
-
(8)
Study reports how the results were obtained. (n = 6)
A data selection template was designed to evaluate research characteristics and performance. All variables are evaluated independently by the three reviewers (M.S., N.A., and P.V.).
The template included the following fields:
Modality (CT, MR, EUS, 8FDG PET/CT, WSI)
Task (detection, diagnosis, staging, treatment, monitoring)
Tissue of interest (PDAC, pancreatic cancer)
Tumour location (head, neck, body, tail)
Disease stage (I, II, III, IV)
Therapy
Type of AI (Radiomics, Deep Learning, other)
Model
Ground truth
Performance metric
Type of internal validation (single split, cross-validation)
Performance on training set
Performance on internal validation set
Performance on internal test set
Performance on external test set
Cohort size for development set (train/validation)
Patient distribution for development set with regard to considered ground truth
Cohort size for internal test set
Patient distribution for internal test set with regard to considered ground truth
Cohort size for external test set
Patient distribution for external test set with regard to considered ground truth
Author Contributions
M.S. and N.A. contributed equally to conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, validation, visualization, writing—original draft, and writing—review and editing. P.V. contributed to conceptualisation, data curation, formal analysis, investigation, writing—original draft. H.H. and J.H. contributed equally to funding acquisition, project administration, supervision, writing—original draft, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
For all authors there is no conflict of interest.
Funding Statement
This project received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No. 101016851, project PANCAIM.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bengtsson A., Andersson R., Ansari D. The Actual 5-Year Survivors of Pancreatic Ductal Adenocarcinoma Based on Real-World Data. Sci. Rep. 2020;10:16425. doi: 10.1038/s41598-020-73525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michl P., Löhr M., Neoptolemos J.P., Capurso G., Rebours V., Malats N., Ollivier M., Ricciardiello L. UEG Position Paper on Pancreatic Cancer. Bringing Pancreatic Cancer to the 21st Century: Prevent, Detect, and Treat the Disease Earlier and Better. United Eur. Gastroenterol. J. 2021;9:860. doi: 10.1002/ueg2.12123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Löhr J.M. Pancreatic Cancer Should Be Treated as a Medical Emergency. BMJ. 2014;349:g5261. doi: 10.1136/bmj.g5261. [DOI] [PubMed] [Google Scholar]
- 4.Latenstein A.E.J., van der Geest L.G.M., Bonsing B.A., Groot Koerkamp B., Haj Mohammad N., de Hingh I.H.J.T., de Meijer V.E., Molenaar I.Q., van Santvoort H.C., van Tienhoven G., et al. Nationwide Trends in Incidence, Treatment and Survival of Pancreatic Ductal Adenocarcinoma. Eur. J. Cancer. 2020;125:83–93. doi: 10.1016/j.ejca.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Elbanna K.Y., Jang H.J., Kim T.K. Imaging Diagnosis and Staging of Pancreatic Ductal Adenocarcinoma: A Comprehensive Review. Insights Imaging. 2020;11:58. doi: 10.1186/s13244-020-00861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baxi V., Edwards R., Montalto M., Saha S. Digital Pathology and Artificial Intelligence in Translational Medicine and Clinical Practice. Mod. Pathol. 2021;35:23–32. doi: 10.1038/s41379-021-00919-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sántha P., Lenggenhager D., Finstadsveen A., Dorg L., Tøndel K., Amrutkar M., Gladhaug I.P., Verbeke C. Morphological Heterogeneity in Pancreatic Cancer Reflects Structural and Functional Divergence. Cancers. 2021;13:895. doi: 10.3390/cancers13040895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fu H., Mi W., Pan B., Guo Y., Li J., Xu R., Zheng J., Zou C., Zhang T., Liang Z., et al. Automatic Pancreatic Ductal Adenocarcinoma Detection in Whole Slide Images Using Deep Convolutional Neural Networks. Front. Oncol. 2021;11:665929. doi: 10.3389/fonc.2021.665929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janssen B.V., Tutucu F., van Roessel S., Adsay V., Basturk O., Campbell F., Doglioni C., Esposito I., Feakins R., Fukushima N., et al. Amsterdam International Consensus Meeting: Tumor Response Scoring in the Pathology Assessment of Resected Pancreatic Cancer after Neoadjuvant Therapy. Mod. Pathol. 2021;34:4–12. doi: 10.1038/s41379-020-00683-9. [DOI] [PubMed] [Google Scholar]
- 10.Kann B.H., Hosny A., Aerts H.J.W.L. Artificial Intelligence for Clinical Oncology. Cancer Cell. 2021;39:916–927. doi: 10.1016/j.ccell.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Leeuwen K.G., Schalekamp S., Rutten M.J.C.M., van Ginneken B., de Rooij M. Artificial Intelligence in Radiology: 100 Commercially Available Products and Their Scientific Evidence. Eur. Radiol. 2021;31:3797–3804. doi: 10.1007/s00330-021-07892-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krizhevsky A., Sutskever I., Hinton G.E. ImageNet Classification with Deep Convolutional Neural Networks. Commun ACM. 2017;60:84–90. doi: 10.1145/3065386. [DOI] [Google Scholar]
- 13.Litjens G., Kooi T., Bejnordi B.E., Setio A.A.A., Ciompi F., Ghafoorian M., van der Laak J.A.W.M., van Ginneken B., Sánchez C.I. A Survey on Deep Learning in Medical Image Analysis. Med. Image Anal. 2017;42:60–88. doi: 10.1016/j.media.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Survival Rates for Pancreatic Cancer. [(accessed on 6 April 2022)]. Available online: https://www.cancer.org/cancer/pancreatic-cancer/detection-diagnosis-staging/survival-rates.html.
- 15.Egawa S., Toma H., Ohigashi H., Okusaka T., Nakao A., Hatori T., Maguchi H., Yanagisawa A., Tanaka M. Japan Pancreatic Cancer Registry; 30th Year Anniversary: Japan Pancreas Society. Pancreas. 2012;41:985–992. doi: 10.1097/MPA.0b013e318258055c. [DOI] [PubMed] [Google Scholar]
- 16.Ho Yoon S., Min Lee J., Yoon Cho Kyung Bun Lee J., Eun Kim J., Kyoung Moon S., Jin Kim S., Hyun Baek J., Ho Kim S., Hyung Kim S., Young Lee J., et al. Small (≤20 mm) Pancreatic Adenocarcinomas: Analysis of Enhancement Patterns and Secondary Signs with Multiphasic Multidetector CT. Radiology. 2011;259:2. doi: 10.1148/radiol.11101133/-/DC1. [DOI] [PubMed] [Google Scholar]
- 17.Kim J.H., Park S.H., Yu E.S., Kim M.H., Kim J., Byun J.H., Lee S.S., Hwang H.J., Hwang J.Y., Lee S.S., et al. Visually Isoattenuating Pancreatic Adenocarcinoma at Dynamic-Enhanced CT: Frequency, Clinical and Pathologic Characteristics, and Diagnosis at Imaging Examinations. Radiology. 2010;257:87–96. doi: 10.1148/radiol.10100015. [DOI] [PubMed] [Google Scholar]
- 18.Singh D.P., Sheedy S., Goenka A.H., Wells M., Lee N.J., Barlow J., Sharma A., Kandlakunta H., Chandra S., Garg S.K., et al. Computerized Tomography Scan in Pre-Diagnostic Pancreatic Ductal Adenocarcinoma: Stages of Progression and Potential Benefits of Early Intervention: A Retrospective Study. Pancreatology. 2020;20:1495–1501. doi: 10.1016/j.pan.2020.07.410. [DOI] [PubMed] [Google Scholar]
- 19.Edge S.B., Compton C.C. The American Joint Committee on Cancer: The 7th Edition of the AJCC Cancer Staging Manual and the Future of TNM. Ann. Surg. Oncol. 2010;17:1471–1474. doi: 10.1245/s10434-010-0985-4. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalo-Marin J., Vila J.J., Perez-Miranda M. Role of Endoscopic Ultrasound in the Diagnosis of Pancreatic Cancer. World J. Gastrointest. Oncol. 2014;6:360–368. doi: 10.4251/wjgo.v6.i9.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song W., Miao D.L., Chen L. Nomogram for Predicting Survival in Patients with Pancreatic Cancer. OncoTargets Ther. 2018;11:539–545. doi: 10.2147/OTT.S154599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Roessel S., Kasumova G.G., Verheij J., Najarian R.M., Maggino L., de Pastena M., Malleo G., Marchegiani G., Salvia R., Ng S.C., et al. International Validation of the Eighth Edition of the American Joint Committee on Cancer (AJCC) TNM Staging System in Patients with Resected Pancreatic Cancer. JAMA Surg. 2018;153:e183617. doi: 10.1001/jamasurg.2018.3617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wittel U.A., Lubgan D., Ghadimi M., Belyaev O., Uhl W., Bechstein W.O., Grützmann R., Hohenberger W.M., Schmid A., Jacobasch L., et al. Consensus in Determining the Resectability of Locally Progressed Pancreatic Ductal Adenocarcinoma—Results of the Conko-007 Multicenter Trial. BMC Cancer. 2019;19:979. doi: 10.1186/s12885-019-6148-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong S.B., Lee S.S., Kim J.H., Kim H.J., Byun J.H., Hong S.M., Song K.B., Kim S.C. Pancreatic Cancer CT: Prediction of Resectability According to NCCN Criteria. Radiology. 2018;289:710–718. doi: 10.1148/radiol.2018180628. [DOI] [PubMed] [Google Scholar]
- 25.Lambert A., Schwarz L., Borbath I., Henry A., van Laethem J.L., Malka D., Ducreux M., Conroy T. An Update on Treatment Options for Pancreatic Adenocarcinoma. Ther. Adv. Med. Oncol. 2019;11:1758835919875568. doi: 10.1177/1758835919875568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pearce A., Haas M., Viney R., Pearson S.A., Haywood P., Brown C., Ward R. Incidence and Severity of Self-Reported Chemotherapy Side Effects in Routine Care: A Prospective Cohort Study. PLoS ONE. 2017;12:e0184360. doi: 10.1371/journal.pone.0184360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harder F.N., Jungmann F., Kaissis G.A., Lohöfer F.K., Ziegelmayer S., Havel D., Quante M., Reichert M., Schmid R.M., Demir I.E., et al. [18F]FDG PET/MRI Enables Early Chemotherapy Response Prediction in Pancreatic Ductal Adenocarcinoma. EJNMMI Res. 2021;11:70. doi: 10.1186/s13550-021-00808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Demir I.E., Jäger C., Schlitter M.M., Konukiewitz B., Stecher L., Schorn S., Tieftrunk E., Scheufele F., Calavrezos L., Schirren R., et al. R0 Versus R1 Resection Matters after Pancreaticoduodenectomy, and Less after Distal or Total Pancreatectomy for Pancreatic Cancer. Ann. Surg. 2017;268:1058–1068. doi: 10.1097/SLA.0000000000002345. [DOI] [PubMed] [Google Scholar]
- 29.Karjol U., Chandranath A., Jonnada P., Cherukuru S., Annavarjula V., Morla S.A. Lymph Node Ratio as a Prognostic Marker in Pancreatic Cancer Survival: A Systematic Review and Meta-Analysis. Cureus. 2020;12:e9597. doi: 10.7759/cureus.9597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tummers W.S., Groen J.V., Sibinga Mulder B.G., Farina-Sarasqueta A., Morreau J., Putter H., van de Velde C.J., Vahrmeijer A.L., Bonsing B.A., Mieog J.S., et al. Impact of Resection Margin Status on Recurrence and Survival in Pancreatic Cancer Surgery. Br. J. Surg. 2019;106:1055. doi: 10.1002/bjs.11115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perri G., Prakash L.R., Katz M.H.G. Response to Preoperative Therapy in Localized Pancreatic Cancer. Front. Oncol. 2020;10:516. doi: 10.3389/fonc.2020.00516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baliyan V., Kordbacheh H., Parakh A., Kambadakone A. Response Assessment in Pancreatic Ductal Adenocarcinoma: Role of Imaging. Abdom. Radiol. 2018;43:435–444. doi: 10.1007/s00261-017-1434-7. [DOI] [PubMed] [Google Scholar]
- 33.van Roessel S., Janssen B.V., Soer E.C., Fariña Sarasqueta A., Verbeke C.S., Luchini C., Brosens L.A.A., Verheij J., Besselink M.G. Scoring of Tumour Response after Neoadjuvant Therapy in Resected Pancreatic Cancer: Systematic Review. Br. J. Surg. 2021;108:119–127. doi: 10.1093/bjs/znaa031. [DOI] [PubMed] [Google Scholar]
- 34.Verbeke C., Häberle L., Lenggenhager D., Esposito I. Pathology Assessment of Pancreatic Cancer Following Neoadjuvant Treatment: Time to Move On. Pancreatology. 2018;18:467–476. doi: 10.1016/j.pan.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 35.Alves N., Schuurmans M., Litjens G., Bosma J.S., Hermans J., Huisman H. Fully Automatic Deep Learning Framework for Pancreatic Ductal Adenocarcinoma Detection on Computed Tomography. Cancers. 2022;14:376. doi: 10.3390/cancers14020376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen X., Chen Z., Li J., Zhang Y.D., Lin X., Qian X. Model-Driven Deep Learning Method for Pancreatic Cancer Segmentation Based on Spiral-Transformation. IEEE Trans. Med. Imaging. 2021;41:75–87. doi: 10.1109/TMI.2021.3104460. [DOI] [PubMed] [Google Scholar]
- 37.Liu K.L., Wu T., Chen P.T., Tsai Y.M., Roth H., Wu M.S., Liao W.C., Wang W. Deep Learning to Distinguish Pancreatic Cancer Tissue from Non-Cancerous Pancreatic Tissue: A Retrospective Study with Cross-Racial External Validation. Lancet Digit. Health. 2020;2:e303–e313. doi: 10.1016/S2589-7500(20)30078-9. [DOI] [PubMed] [Google Scholar]
- 38.Wang Y., Tang P., Zhou Y., Shen W., Fishman E.K., Yuille A.L. Learning Inductive Attention Guidance for Partially Supervised Pancreatic Ductal Adenocarcinoma Prediction. IEEE Trans. Med. Imaging. 2021;40:2723–2735. doi: 10.1109/TMI.2021.3060066. [DOI] [PubMed] [Google Scholar]
- 39.Ma H., Liu Z.X., Zhang J.J., Wu F.T., Xu C.F., Shen Z., Yu C.H., Li Y.M. Construction of a Convolutional Neural Network Classifier Developed by Computed Tomography Images for Pancreatic Cancer Diagnosis. World J. Gastroenterol. 2020;26:5156–5168. doi: 10.3748/wjg.v26.i34.5156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chu L.C., Solmaz B., Park S., Kawamoto S., Yuille A.L., Hruban R.H., Fishman E.K. Diagnostic Performance of Commercially Available vs. in-House Radiomics Software in Classification of CT Images from Patients with Pancreatic Ductal Adenocarcinoma vs. Healthy Controls. Abdom. Radiol. 2020;45:2469–2475. doi: 10.1007/s00261-020-02556-w. [DOI] [PubMed] [Google Scholar]
- 41.Li S., Jiang H., Wang Z., Zhang G., Yao Y. An Effective Computer Aided Diagnosis Model for Pancreas Cancer on PET/CT Images. Comput. Methods Programs Biomed. 2018;165:205–214. doi: 10.1016/j.cmpb.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 42.Tonozuka R., Itoi T., Nagata N., Kojima H., Sofuni A., Tsuchiya T., Ishii K., Tanaka R., Nagakawa Y., Mukai S. Deep Learning Analysis for the Detection of Pancreatic Cancer on Endosonographic Images: A Pilot Study. J. Hepatobiliary Pancreat. Sci. 2021;28:95–104. doi: 10.1002/jhbp.825. [DOI] [PubMed] [Google Scholar]
- 43.Qiu J.J., Yin J., Qian W., Liu J.H., Huang Z.X., Yu H.P., Ji L., Zeng X.X. A Novel Multiresolution-Statistical Texture Analysis Architecture: Radiomics-Aided Diagnosis of PDAC Based on Plain CT Images. IEEE Trans. Med. Imaging. 2021;40:12–25. doi: 10.1109/TMI.2020.3021254. [DOI] [PubMed] [Google Scholar]
- 44.Chu L.C., Park S., Kawamoto S., Fouladi D.F., Shayesteh S., Zinreich E.S., Graves J.S., Horton K.M., Hruban R.H., Yuille A.L., et al. Utility of CT Radiomics Features in Differentiation of Pancreatic Ductal Adenocarcinoma From Normal Pancreatic Tissue. AJR Am. J. Roentgenol. 2019;213:349–357. doi: 10.2214/AJR.18.20901. [DOI] [PubMed] [Google Scholar]
- 45.Ozkan M., Cakiroglu M., Kocaman O., Kurt M., Yilmaz B., Can G., Korkmaz U., Dandil E., Eksi Z. Age-Based Computer-Aided Diagnosis Approach for Pancreatic Cancer on Endoscopic Ultrasound Images. Endosc. Ultrasound. 2016;5:101–107. doi: 10.4103/2303-9027.180473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Si K., Xue Y., Yu X., Zhu X., Li Q., Gong W., Liang T., Duan S. Fully End-to-End Deep-Learning-Based Diagnosis of Pancreatic Tumors. Theranostics. 2021;11:1982–1990. doi: 10.7150/thno.52508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Naito Y., Tsuneki M., Fukushima N., Koga Y., Higashi M., Notohara K., Aishima S., Ohike N., Tajiri T., Yamaguchi H., et al. A Deep Learning Model to Detect Pancreatic Ductal Adenocarcinoma on Endoscopic Ultrasound-Guided Fine-Needle Biopsy. Sci. Rep. 2021;11:8454. doi: 10.1038/s41598-021-87748-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kriegsmann M., Kriegsmann K., Steinbuss G., Zgorzelski C., Kraft A., Gaida M.M. Deep Learning in Pancreatic Tissue: Identification of Anatomical Structures, Pancreatic Intraepithelial Neoplasia, and Ductal Adenocarcinoma. Int. J. Mol. Sci. 2021;22:5385. doi: 10.3390/ijms22105385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deng Y., Ming B., Zhou T., Wu J.L., Chen Y., Liu P., Zhang J., Zhang S.Y., Chen T.W., Zhang X.M. Radiomics Model Based on MR Images to Discriminate Pancreatic Ductal Adenocarcinoma and Mass-Forming Chronic Pancreatitis Lesions. Front. Oncol. 2021;11:811. doi: 10.3389/fonc.2021.620981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ziegelmayer S., Kaissis G., Harder F., Jungmann F., Müller T., Makowski M., Braren R. Deep Convolutional Neural Network-Assisted Feature Extraction for Diagnostic Discrimination and Feature Visualization in Pancreatic Ductal Adenocarcinoma (PDAC) versus Autoimmune Pancreatitis (AIP) J. Clin. Med. 2020;9:4013. doi: 10.3390/jcm9124013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu S.L., Li S., Guo Y.T., Zhou Y.P., Zhang Z.D., Li S., Lu Y. Establishment and Application of an Artificial Intelligence Diagnosis System for Pancreatic Cancer with a Faster Region-Based Convolutional Neural Network. Chin. Med. J. 2019;132:2795–2803. doi: 10.1097/CM9.0000000000000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Səftoiu A., Vilmann P., Dietrich C.F., Iglesias-Garcia J., Hocke M., Seicean A., Ignee A., Hassan H., Streba C.T., Ioncicə A.M., et al. Quantitative Contrast-Enhanced Harmonic EUS in Differential Diagnosis of Focal Pancreatic Masses (with Videos) Gastrointest. Endosc. 2015;82:59–69. doi: 10.1016/j.gie.2014.11.040. [DOI] [PubMed] [Google Scholar]
- 53.Ebrahimian S., Singh R., Netaji A., Madhusudhan K.S., Homayounieh F., Primak A., Lades F., Saini S., Kalra M.K., Sharma S. Characterization of Benign and Malignant Pancreatic Lesions with DECT Quantitative Metrics and Radiomics. Acad. Radiol. 2021;29:705–713. doi: 10.1016/j.acra.2021.07.008. [DOI] [PubMed] [Google Scholar]
- 54.Ma X., Wang Y.-R., Zhuo L.-Y., Yin X.-P., Ren J.-L., Li C.-Y., Xing L.-H., Zheng T.-T. Retrospective Analysis of the Value of Enhanced CT Radiomics Analysis in the Differential Diagnosis between Pancreatic Cancer and Chronic Pancreatitis. Int. J. Gen. Med. 2022;15:233–241. doi: 10.2147/IJGM.S337455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu Z., Li M., Zuo C., Yang Z., Yang X., Ren S., Peng Y., Sun G., Shen J., Cheng C., et al. Radiomics Model of Dual-Time 2-[18F]FDG PET/CT Imaging to Distinguish between Pancreatic Ductal Adenocarcinoma and Autoimmune Pancreatitis. Eur. Radiol. 2021;31:6983–6991. doi: 10.1007/s00330-021-07778-0. [DOI] [PubMed] [Google Scholar]
- 56.Ren S., Zhao R., Cui W., Qiu W., Guo K., Cao Y., Duan S., Wang Z., Chen R. Computed Tomography-Based Radiomics Signature for the Preoperative Differentiation of Pancreatic Adenosquamous Carcinoma From Pancreatic Ductal Adenocarcinoma. Front. Oncol. 2020;10:1618. doi: 10.3389/fonc.2020.01618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ren S., Zhao R., Zhang J., Guo K., Gu X., Duan S., Wang Z., Chen R. Diagnostic Accuracy of Unenhanced CT Texture Analysis to Differentiate Mass-Forming Pancreatitis from Pancreatic Ductal Adenocarcinoma. Abdom. Radiol. 2020;45:1524–1533. doi: 10.1007/s00261-020-02506-6. [DOI] [PubMed] [Google Scholar]
- 58.Park S., Chu L.C., Hruban R.H., Vogelstein B., Kinzler K.W., Yuille A.L., Fouladi D.F., Shayesteh S., Ghandili S., Wolfgang C.L., et al. Differentiating Autoimmune Pancreatitis from Pancreatic Ductal Adenocarcinoma with CT Radiomics Features. Diagn. Interv. Imaging. 2020;101:555–564. doi: 10.1016/j.diii.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 59.He M., Liu Z., Lin Y., Wan J., Li J., Xu K., Wang Y., Jin Z., Tian J., Xue H. Differentiation of Atypical Non-Functional Pancreatic Neuroendocrine Tumor and Pancreatic Ductal Adenocarcinoma Using CT Based Radiomics. Eur. J. Radiol. 2019;117:102–111. doi: 10.1016/j.ejrad.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 60.Ren S., Zhang J., Chen J., Cui W., Zhao R., Qiu W., Duan S., Chen R., Chen X., Wang Z. Evaluation of Texture Analysis for the Differential Diagnosis of Mass-Forming Pancreatitis From Pancreatic Ductal Adenocarcinoma on Contrast-Enhanced CT Images. Front. Oncol. 2019;9:1171. doi: 10.3389/fonc.2019.01171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang Y., Cheng C., Liu Z., Wang L., Pan G., Sun G., Chang Y., Zuo C., Yang X. Radiomics Analysis for the Differentiation of Autoimmune Pancreatitis and Pancreatic Ductal Adenocarcinoma in 18 F-FDG PET/CT. Med. Phys. 2019;46:4520–4530. doi: 10.1002/mp.13733. [DOI] [PubMed] [Google Scholar]
- 62.Sǎftoiu A., Vilmann P., Gorunescu F., Janssen J., Hocke M., Larsen M., Iglesias-Garcia J., Arcidiacono P., Will U., Giovannini M., et al. Efficacy of an Artificial Neural Network-Based Approach to Endoscopic Ultrasound Elastography in Diagnosis of Focal Pancreatic Masses. Clin. Gastroenterol. Hepatol. 2012;10:84–90. doi: 10.1016/j.cgh.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 63.An C., Li D., Li S., Li W., Tong T., Liu L., Jiang D., Jiang L., Ruan G., Hai N., et al. Deep Learning Radiomics of Dual-Energy Computed Tomography for Predicting Lymph Node Metastases of Pancreatic Ductal Adenocarcinoma. Eur. J. Nucl. Med. Mol. Imaging. 2021;49:1187–1199. doi: 10.1007/s00259-021-05573-z. [DOI] [PubMed] [Google Scholar]
- 64.Chaddad A., Sargos P., Desrosiers C. Modeling Texture in Deep 3D CNN for Survival Analysis. IEEE J. Biomed. Health Inform. 2021;25:2454–2462. doi: 10.1109/JBHI.2020.3025901. [DOI] [PubMed] [Google Scholar]
- 65.Shi Z., Ma C., Huang X., Cao D. Magnetic Resonance Imaging Radiomics-Based Nomogram From Primary Tumor for Pretreatment Prediction of Peripancreatic Lymph Node Metastasis in Pancreatic Ductal Adenocarcinoma: A Multicenter Study. J. Magn. Reson. Imaging. 2022;55:823–839. doi: 10.1002/jmri.28048. [DOI] [PubMed] [Google Scholar]
- 66.Chang N., Cui L., Luo Y., Chang Z., Yu B., Liu Z. Development and Multicenter Validation of a CT-Based Radiomics Signature for Discriminating Histological Grades of Pancreatic Ductal Adenocarcinoma. Quant. Imaging Med. Surg. 2020;10:692–702. doi: 10.21037/qims.2020.02.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Song J.W., Lee J.H. New Morphological Features for Grading Pancreatic Ductal Adenocarcinomas. BioMed Res. Int. 2013;2013:175271. doi: 10.1155/2013/175271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bian Y., Guo S., Jiang H., Gao S., Shao C., Cao K., Fang X., Li J., Wang L., Ma C., et al. Radiomics Nomogram for the Preoperative Prediction of Lymph Node Metastasis in Pancreatic Ductal Adenocarcinoma. Cancer Imaging. 2022;22:4. doi: 10.1186/s40644-021-00443-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bian Y., Liu Y.F., Jiang H., Meng Y., Liu F., Cao K., Zhang H., Fang X., Li J., Yu J., et al. Machine Learning for MRI Radiomics: A Study Predicting Tumor-Infiltrating Lymphocytes in Patients with Pancreatic Ductal Adenocarcinoma. Abdom. Radiol. 2021;46:4800–4816. doi: 10.1007/s00261-021-03159-9. [DOI] [PubMed] [Google Scholar]
- 70.Cen C., Liu L., Li X., Wu A., Liu H., Wang X., Wu H., Wang C., Han P., Wang S. Pancreatic Ductal Adenocarcinoma at CT: A Combined Nomogram Model to Preoperatively Predict Cancer Stage and Survival Outcome. Front. Oncol. 2021;11:1980. doi: 10.3389/fonc.2021.594510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang T., Dong X., Zhou Y., Liu M., Hang J., Wu L. Development and Validation of a Radiomics Nomogram to Discriminate Advanced Pancreatic Cancer with Liver Metastases or Other Metastatic Patterns. Cancer Biomark. 2021;32:541–550. doi: 10.3233/CBM-210190. [DOI] [PubMed] [Google Scholar]
- 72.Xing H., Hao Z., Zhu W., Sun D., Ding J., Zhang H., Liu Y., Huo L. Preoperative Prediction of Pathological Grade in Pancreatic Ductal Adenocarcinoma Based on 18F-FDG PET/CT Radiomics. EJNMMI Res. 2021;11:19. doi: 10.1186/s13550-021-00760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaissis G.A., Ziegelmayer S., Lohöfer F.K., Harder F.N., Jungmann F., Sasse D., Muckenhuber A., Yen H.Y., Steiger K., Siveke J., et al. Image-Based Molecular Phenotyping of Pancreatic Ductal Adenocarcinoma. J. Clin. Med. 2020;9:724. doi: 10.3390/jcm9030724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen F., Zhou Y., Qi X., Zhang R., Gao X., Xia W., Zhang L. Radiomics-Assisted Presurgical Prediction for Surgical Portal Vein-Superior Mesenteric Vein Invasion in Pancreatic Ductal Adenocarcinoma. Front. Oncol. 2020;10:2521. doi: 10.3389/fonc.2020.523543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Liu P., Gu Q., Hu X., Tan X., Liu J., Xie A., Huang F. Applying a Radiomics-Based Strategy to Preoperatively Predict Lymph Node Metastasis in the Resectable Pancreatic Ductal Adenocarcinoma. J. X Ray Sci. Technol. 2020;28:1113–1121. doi: 10.3233/XST-200730. [DOI] [PubMed] [Google Scholar]
- 76.Li K., Yao Q., Xiao J., Li M., Yang J., Hou W., Du M., Chen K., Qu Y., Li L., et al. Contrast-Enhanced CT Radiomics for Predicting Lymph Node Metastasis in Pancreatic Ductal Adenocarcinoma: A Pilot Study. Cancer Imaging. 2020;20:12. doi: 10.1186/s40644-020-0288-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Longlong Z., Xinxiang L., Yaqiong G., Wei W. Predictive Value of the Texture Analysis of Enhanced Computed Tomographic Images for Preoperative Pancreatic Carcinoma Differentiation. Front. Bioeng. Biotechnol. 2020;8:719. doi: 10.3389/fbioe.2020.00719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Qiu W., Duan N., Chen X., Ren S., Zhang Y., Wang Z., Chen R. Pancreatic Ductal Adenocarcinoma: Machine Learning-Based Quantitative Computed Tomography Texture Analysis For Prediction Of Histopathological Grade. Cancer Manag. Res. 2019;11:9253–9264. doi: 10.2147/CMAR.S218414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Healy G.M., Salinas-Miranda E., Jain R., Dong X., Deniffel D., Borgida A., Hosni A., Ryan D.T., Njeze N., McGuire A., et al. Pre-Operative Radiomics Model for Prognostication in Resectable Pancreatic Adenocarcinoma with External Validation. Eur. Radiol. 2021;32:2492–2505. doi: 10.1007/s00330-021-08314-w. [DOI] [PubMed] [Google Scholar]
- 80.Zhang Y., Lobo-Mueller E.M., Karanicolas P., Gallinger S., Haider M.A., Khalvati F. CNN-Based Survival Model for Pancreatic Ductal Adenocarcinoma in Medical Imaging. BMC Med. Imaging. 2020;20:11. doi: 10.1186/s12880-020-0418-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yao J., Shi Y., Cao K., Lu L., Lu J., Song Q., Jin G., Xiao J., Hou Y., Zhang L. DeepPrognosis: Preoperative Prediction of Pancreatic Cancer Survival and Surgical Margin via Comprehensive Understanding of Dynamic Contrast-Enhanced CT Imaging and Tumor-Vascular Contact Parsing. Med. Image Anal. 2021;73:102150. doi: 10.1016/j.media.2021.102150. [DOI] [PubMed] [Google Scholar]
- 82.Watson M.D., Baimas-George M.R., Murphy K.J., Pickens R.C., Iannitti D.A., Martinie J.B., Baker E.H., Vrochides D., Ocuin L.M. Pure and Hybrid Deep Learning Models Can Predict Pathologic Tumor Response to Neoadjuvant Therapy in Pancreatic Adenocarcinoma: A Pilot Study. Am. Surg. 2021;87:1901–1909. doi: 10.1177/0003134820982557. [DOI] [PubMed] [Google Scholar]
- 83.Zhang Y., Lobo-Mueller E.M., Karanicolas P., Gallinger S., Haider M.A., Khalvati F. Improving Prognostic Performance in Resectable Pancreatic Ductal Adenocarcinoma Using Radiomics and Deep Learning Features Fusion in CT Images. Sci. Rep. 2021;11:1378. doi: 10.1038/s41598-021-80998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Li X., Wan Y., Lou J., Xu L., Shi A., Yang L., Fan Y., Yang J., Huang J., Wu Y., et al. Preoperative Recurrence Prediction in Pancreatic Ductal Adenocarcinoma after Radical Resection Using Radiomics of Diagnostic Computed Tomography. EClinicalMedicine. 2022;43:101215. doi: 10.1016/j.eclinm.2021.101215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shi H., Wei Y., Cheng S., Lu Z., Zhang K., Jiang K., Xu Q. Survival Prediction after Upfront Surgery in Patients with Pancreatic Ductal Adenocarcinoma: Radiomic, Clinic-Pathologic and Body Composition Analysis. Pancreatology. 2021;21:731–737. doi: 10.1016/j.pan.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 86.Wei M., Gu B., Song S., Zhang B., Wang W., Xu J., Yu X., Shi S. A Novel Validated Recurrence Stratification System Based on 18 F-FDG PET/CT Radiomics to Guide Surveillance After Resection of Pancreatic Cancer. Front. Oncol. 2021;11:650266. doi: 10.3389/fonc.2021.650266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xie T., Wang X., Li M., Tong T., Yu X., Zhou Z. Pancreatic Ductal Adenocarcinoma: A Radiomics Nomogram Outperforms Clinical Model and TNM Staging for Survival Estimation after Curative Resection. Eur. Radiol. 2020;30:2513–2524. doi: 10.1007/s00330-019-06600-2. [DOI] [PubMed] [Google Scholar]
- 88.Park S., Sham J.G., Kawamoto S., Blair A.B., Rozich N., Fouladi D.F., Shayesteh S., Hruban R.H., He J., Wolfgang C.L., et al. CT Radiomics-Based Preoperative Survival Prediction in Patients With Pancreatic Ductal Adenocarcinoma. AJR Am. J. Roentgenol. 2021;217:1104–1112. doi: 10.2214/AJR.20.23490. [DOI] [PubMed] [Google Scholar]
- 89.Parr E., Du Q., Zhang C., Lin C., Kamal A., McAlister J., Liang X., Bavitz K., Rux G., Hollingsworth M., et al. Radiomics-Based Outcome Prediction for Pancreatic Cancer Following Stereotactic Body Radiotherapy. Cancers. 2020;12:1051. doi: 10.3390/cancers12041051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kaissis G.A., Jungmann F., Ziegelmayer S., Lohöfer F.K., Harder F.N., Schlitter A.M., Muckenhuber A., Steiger K., Schirren R., Friess H., et al. Multiparametric Modelling of Survival in Pancreatic Ductal Adenocarcinoma Using Clinical, Histomorphological, Genetic and Image-Derived Parameters. J. Clin. Med. 2020;9:1250. doi: 10.3390/jcm9051250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hui B., Qiu J.J., Liu J.H., Ke N.W. Identification of Pancreaticoduodenectomy Resection for Pancreatic Head Adenocarcinoma: A Preliminary Study of Radiomics. Comput. Math. Methods Med. 2020;2020:2761627. doi: 10.1155/2020/2761627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bian Y., Jiang H., Ma C., Cao K., Fang X., Li J., Wang L., Zheng J., Lu J. Performance of CT-Based Radiomics in Diagnosis of Superior Mesenteric Vein Resection Margin in Patients with Pancreatic Head Cancer. Abdom. Radiol. 2020;45:759–773. doi: 10.1007/s00261-019-02401-9. [DOI] [PubMed] [Google Scholar]
- 93.Tang T., Liang T.-B., Zhang Q., Guo C., Zhang X., Lao M., Shen Y., Xiao W., Ying S., Sun K., et al. Development of a Novel Multiparametric MRI Radiomic Nomogram for Preoperative Evaluation of Early Recurrence in Resectable Pancreatic Cancer. J. Magn. Reson. Imaging. 2020;52:231–245. doi: 10.1002/jmri.27024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhou H.F., Han Y.Q., Lu J., Wei J.W., Guo J.H., Zhu H.D., Huang M., Ji J.S., Lv W.F., Chen L., et al. Radiomics Facilitates Candidate Selection for Irradiation Stents Among Patients With Unresectable Pancreatic Cancer. Front. Oncol. 2019;9:973. doi: 10.3389/fonc.2019.00973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cozzi L., Comito T., Fogliata A., Franzese C., Franceschini D., Bonifacio C., Tozzi A., Brina L.D., Clerici E., Tomatis S., et al. Computed Tomography Based Radiomic Signature as Predictive of Survival and Local Control after Stereotactic Body Radiation Therapy in Pancreatic Carcinoma. PLoS ONE. 2019;14:e0210758. doi: 10.1371/journal.pone.0210758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kaissis G., Ziegelmayer S., Lohöfer F., Steiger K., Algül H., Muckenhuber A., Yen H.Y., Rummeny E., Friess H., Schmid R., et al. A Machine Learning Algorithm Predicts Molecular Subtypes in Pancreatic Ductal Adenocarcinoma with Differential Response to Gemcitabine-Based versus FOLFIRINOX Chemotherapy. PLoS ONE. 2019;14:e0218642. doi: 10.1371/journal.pone.0218642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kaissis G., Ziegelmayer S., Lohöfer F., Algül H., Eiber M., Weichert W., Schmid R., Friess H., Rummeny E., Ankerst D., et al. A Machine Learning Model for the Prediction of Survival and Tumor Subtype in Pancreatic Ductal Adenocarcinoma from Preoperative Diffusion-Weighted Imaging. Eur. Radiol. Exp. 2019;3:41. doi: 10.1186/s41747-019-0119-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chakraborty J., Langdon-Embry L., Cunanan K.M., Escalon J.G., Allen P.J., Lowery M.A., O’Reilly E.M., Gönen M., Do R.G., Simpson A.L. Preliminary Study of Tumor Heterogeneity in Imaging Predicts Two Year Survival in Pancreatic Cancer Patients. PLoS ONE. 2017;12:e0188022. doi: 10.1371/journal.pone.0188022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cui Y., Song J., Pollom E., Alagappan M., Shirato H., Chang D.T., Koong A.C., Li R. Quantitative Analysis of (18)F-Fluorodeoxyglucose Positron Emission Tomography Identifies Novel Prognostic Imaging Biomarkers in Locally Advanced Pancreatic Cancer Patients Treated With Stereotactic Body Radiation Therapy. Int. J. Radiat. Oncol. Biol Phys. 2016;96:102–109. doi: 10.1016/j.ijrobp.2016.04.034. [DOI] [PubMed] [Google Scholar]
- 100.Janssen B.V., Theijse R., van Roessel S., de Ruiter R., Berkel A., Huiskens J., Busch O.R., Wilmink J.W., Kazemier G., Valkema P., et al. Artificial Intelligence-Based Segmentation of Residual Tumor in Histopathology of Pancreatic Cancer after Neoadjuvant Treatment. Cancers. 2021;13:5089. doi: 10.3390/cancers13205089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nasief H., Zheng C., Schott D., Hall W., Tsai S., Erickson B., Allen Li X. A Machine Learning Based Delta-Radiomics Process for Early Prediction of Treatment Response of Pancreatic Cancer. Npj Precis. Oncol. 2019;3:25. doi: 10.1038/s41698-019-0096-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kenner B., Chari S.T., Kelsen D., Klimstra D.S., Pandol S.J., Rosenthal M., Rustgi A.K., Taylor J.A., Yala A., Abul-Husn N., et al. Artificial Intelligence and Early Detection of Pancreatic Cancer: 2020 Summative Review. Pancreas. 2021;50:251–279. doi: 10.1097/MPA.0000000000001762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ryan D.P., Hong T.S., Bardeesy N. Pancreatic Adenocarcinoma. N. Engl. J. Med. 2014;371:1039–1049. doi: 10.1056/NEJMra1404198. [DOI] [PubMed] [Google Scholar]