Abstract
Family caregiving is a public health issue because of caregivers’ significant contribution to the health and social care systems, as well as the substantial impact that giving and receiving care has on the health and quality of life of care receivers and caregivers. While there have been many studies that associate caregivers’ care work, financial difficulty, navigation, and other caregiving factors with family caregivers’ psychological distress, we were interested not only in the factors related to family caregiver anxiety but also in hypothesizing how those effects occur. In this study, we used Andrew Hayes’ PROCESS moderation analysis to explore the link between caregiver frailty, weekly care hours, and perceptions of financial difficulty, social support, and anxiety. In this analysis, we included 474 caregivers with relatively complete data on all of the variables. In regression analysis after controlling for gender and age, social loneliness (β = 0.245), frailty (β = 0.199), financial difficulty (β = 0.196), care time (β = 0.143), and navigation confidence (β = 0.131) were all significant. We then used PROCESS Model 6 to determine the significance of the direct, indirect, and total effects through the serial mediation model. The model pathway from frailty to care time to financial difficulty to social loneliness to anxiety was significant. The proportions of family caregivers who were moderately frail, anxious, and experiencing social loneliness after eighteen months of the COVID-19 pandemic found in this survey should be of concern to policymakers and healthcare providers.
Keywords: family caregivers, carers, anxiety, frailty, loneliness, social support, COVID-19, mediation analysis
1. Introduction
Public health’s goal is to protect and improve the health of individuals, communities, and populations of all sizes from neighborhoods to the world. Family caregiving is a public health issue because of caregivers’ significant contribution to the health and social care systems within countries [1,2,3], as well as the substantial impact that giving and receiving care has on the health and quality of life of care-receivers and caregivers [4,5].
Current Canadian health systems depend on family caregivers to provide 80–90% of the day-to-day assistance and care management required by care-receivers living in the community [6,7], and assist with 15 to 30% of the care for congregate-care residents [8,9,10]. Having a caregiver is associated with care-receiver’s decreased healthcare utilization and risk of institutionalization [11]. Many family caregivers are caring more intensively and for longer due to increased life expectancies, a higher proportion of older adults living with frailty and complex chronic conditions who need care, and structural changes such as smaller families, divorce, geographic mobility, and employed spouses/partners that have reduced family caregiver supply [12,13,14]. Caregivers are experiencing increasing frailty [15], deteriorating physical health [14], declining levels of cognitive functioning [16], and increasing distress and anxiety [17,18,19,20]. In 2010, 16% of Canadian caregivers of home care clients were distressed [7] and distress rose to 33% by 2016 [21,22]. Anxiety rates of over 50% were reported during the COVID-19 pandemic [19,23,24,25,26].
Exposure to chronic stress and anxiety has been proposed as accelerators for caregivers’ health decline [26,27] and frailty [28,29]. However, frailty and poor health can also increase caregiver stress [28,30]. For example, Smagula and colleagues [30] showed that 82% of caregivers providing intensive help with activities of daily living were suffering from anxiety; however, those who were frail, that is, exhibiting white matter brain pathology, reported strain at much lower levels of care work.
Review: Factors Associated with Caregiver Anxiety
Caregiving intensity, whether it is measured by hours of care or the type and the quantity of assistance provided, is associated with caregiver anxiety and distress [6,13]. InterRAI Home Care assessment research associates caregiver distress with caring for more than 21 hours weekly, caring for someone with dementia, depression, or dementia-related responsive behaviors, and co-residing with the care-receiver [31,32,33]. Distress on RAI-Home Care assessment includes expressing feelings of anger, depression, or the inability to continue with caring activities.
Family caregivers reported that their care work increased substantially in the COVID-19 pandemic [23,24,34]. Objective assessments confirmed that formal support for family caregivers in the first six months of the COVID-19 pandemic (March–September 2020) decreased [25]. In Canada, Sinn and colleagues [34] found there were significantly fewer home care admissions, significantly fewer standardized assessments, and significantly more clients who received no personal support services or rehabilitation services despite assessed needs. Clients who had been receiving services received significantly fewer hours of personal support and therapy visits per month.
Out-of-pocket caregiving costs [35] and difficulty navigating health and community systems [33,36,37,38] are also identified as factors that contribute to family caregiver workload and anxiety [33,36,37,38]. In 2012, one in five Canadian caregivers were experiencing financial hardship [36]. Caregivers experience financial hardships from out-of-pocket care expenses as well as lost income and reduced pensions due to reduced work hours or leaving the workforce to care. In 2017, Taylor and Quesnel-Vallée [38] estimated that family caregivers were spending 15 to 50% of the time on the structural burden of care—that is finding, negotiating for, and then managing health and social care services for the care receiver.
Social supports can moderate the effect that stressors like intensive care work and financial difficulty have on family caregivers [20,39,40]. According to stress-buffering theory, perceptions that social support is available, that is, family or friends who one feels close to or are available to help when one has a problem, can mitigate the effects of stressors on caregiver’s anxiety and distress [41,42]. During the pandemic, social support from family and friends decreased [23,24,43,44,45].
While there have been many studies that associate care work, financial difficulty, and inadequate social support with increases in family caregivers’ psychological distress, little research has been conducted on how these factors might connect to caregiver health and anxiety. In this study, we used Andrew Hayes’ PROCESS moderation analysis to explore the link between caregiver frailty, weekly care hours, perceptions of financial difficulty, and social support and anxiety.
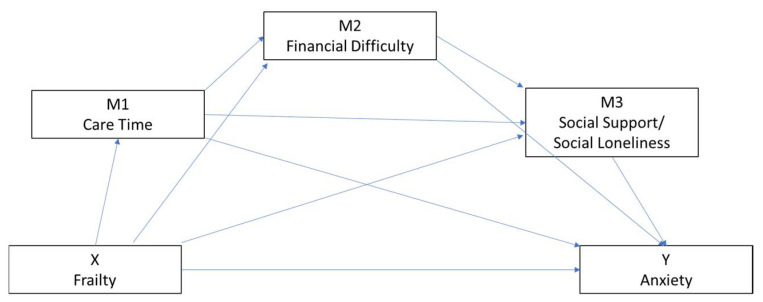
Theoretically, we hypothesized that: (1) caregivers’ health (frailty) is positively associated with anxiety; (2) the association between caregiver frailty and caregiver anxiety will be mediated by weekly care work, perceived financial difficulty and social support; and (3) there will be a causal serial mediation pathway from care time to perceived financial difficulty and social support. The proposed serial mediation model in this study is depicted in Figure 1.
Figure 1.
Hypothesized serial moderation model.
2. Materials and Methods
A cross-sectional survey of the effects of COVID-19 on Alberta family caregivers was conducted online on the secure REDCap survey platform from 21 June 2021 to 31 August 2021. Alberta is a land-locked western province in Canada. About 15% of the population lives in rural and remote areas and 85% lives in urban and suburban settings. The inclusion criteria were: (1) 14 years of age and older; (2) a family caregiver (carer, care partner) defined as any person who takes on a generally unpaid caring role providing emotional, physical, or practical support in response to another person’s disability, mental illness, drug or alcohol dependency, chronic condition, dementia, terminal or serious illness, frailty from ageing, or COVID-19 [46]; and (3) resides in Alberta.
The health research ethics board at the University of Alberta approved all study methods. To recruit participants, we approached health and community organizations who work with family caregivers by email to advise family caregivers about the survey in their newsletters and posters. We also used social media platforms such as Twitter, LinkedIn, and Facebook to inform family caregivers directly about the survey. All participants were asked to read information about the study and provided implied consent by clicking on the survey (Supplementary File S1). Of the 685 people who clicked on the survey, 556 current family caregivers responded to more than three quarters of the questions (81.17%).
2.1. Data Collection
The survey consisted of 30 closed questions (Likert scale, yes/no, list) and five open-ended questions. As per our ethics approval, participants were informed it was their choice to answer or skip questions they did not wish to answer. The survey sections used in this study consisted of four main sections: (1) care work; (2) health (frailty, anxiety, changes in physical and mental health); (3) stressors (financial, navigation, social loneliness); and (4) demographics (of both caregiver and care-receiver). The full survey can be found in the supplemental materials (Supplementary File S1 Survey).
2.1.1. Weekly Care Work
Family caregivers who were caring before COVID-19 were asked whether care time increased, remained stable, or decreased. We assessed the number of hours devoted to weekly care time during COVID-19 with the following options ≤10 h, 11–20 h, 21–30 h, 31–40 h, 41–80 h, 81–120 h and 121–168 h.
2.1.2. Frailty
Frailty has been acknowledged as a new public health priority because of its association with multimorbity, hospitalizations, hospital readmission, institutionalization, increased healthcare costs and mortality [47,48,49]. Rockwood [49] defines frailty “as the term widely used to denote a multidimensional syndrome of loss of reserves (energy, physical ability, cognition, health) that gives rise to vulnerability.” The primary reason for congregate care admission is the caregiver’s health failing where they become too frail to care. We consider frailty screening to be one step in an approach towards promoting family caregivers’ health and wellbeing. In this study we used a self-report version of the Clinical Frailty Scale [CFS] [48,49], initially used in an assessment study of the effects of frailty assessment and social prescribing [50]. The CFS was originally validated for face-to-face screening by a health provider, but adaptations are permitted. We used Rasiah’s [50] nine questions to assess caregiver’s frailty (See CFS Scale in Supplementary File S2).
2.1.3. Anxiety
We assessed anxiety with Tluczek and colleagues’ [51] validated [51,52,53] six-item State Anxiety Scale short-form version of the State Trait Anxiety Inventory [STAI]. Both the long and short forms measure feelings of worry, tension, nervousness, and apprehension, with questions like “I feel comfortable” or “I feel good”. Questions 1, 3, and 6 are worded positively, then reversed scored so that higher scores indicate higher anxiety. The score is multiplied by 20/6 to obtain scores ranging from 20–80. The Cronbach’s alphas for the six-item short-form State Anxiety Scale ranged from 0.74 to 0.82 [51,52,53]. In this case, the standardized Cronbach’s alpha was 0.85.
2.1.4. Social Loneliness
In this study we used the three item social loneliness subscale from the DeJong Gierveld Loneliness Scale [54] to measure caregivers’ perceptions of the social support available from family and friends. The three positively worded questions “There are plenty of people I can lean on in case of trouble”, “There are plenty of people I can count on completely”, and “There are enough people I feel close to” are answered on a three-point scale of no, more or less, and yes. To avoid bias, “no” and “more or less” are scored as 1, and “yes” as a 0, yielding total scores of 3. Higher scores indicate more social loneliness or lower social support. In a large seven country sample, the social loneliness subscale had a 0.85 Cronbach’s alpha [54], and in this provincial sample, the standardized alpha coefficient was 0.89.
2.1.5. Other Stressors
We assumed that financial difficulty and difficulty navigating health and social care systems could be stressful. To assess caregivers’ perceptions of their financial difficulty, we asked them, “During the pandemic, have you experienced financial hardships because of caregiving responsibilities?” rated on a scale of none, a few, moderate, and a lot. The ability to access services and supports was assessed with the question, “How would you rate your ability to access services and navigate the healthcare system?” with answers “very capable”, “somewhat capable”, “neutral”, “a little capable”, and “not at all capable”.
2.2. Data Analysis
Data analysis proceeded in three stages. First, we used descriptive statistics to examine distributions for categorical variables and means and standard deviations for continuous variables. We explored associations with Pearson correlation analysis stepwise linear regression to examine the caregiver factors associated with caregivers’ anxiety even though Hayes advises that the moderator variables significant in the PROCESS moderation analysis may not be significant in regression models [55]. A three-step hierarchical linear regression was conducted with anxiety as the dependent variable. The hierarchical regression analysis results consist of model comparisons and a model interpretation based on an alpha of 0.05. Then, in order to address our moderation hypothesis, we used SPSS Version 26 (IBM, Armonk, NY, USA) and version 4 of Hayes [55] PROCESS moderation/ mediation data analysis program. The answers “Don’t know” and “Prefer not to answer” were treated as missing values and were managed by excluding them list-wise. The statistical significance was set at p < 0.05.
The SPSS PROCESS model runs each predictor factor individually. The moderation models were tested in two steps, first the parallel model and then the serial process version. Both the parallel (Model 4) and serial (Model 6) moderation analysis based on 5000 bootstrap samples using a 95% confidence interval were calculated.
3. Results
3.1. Participants
In this analysis, we included 474 caregivers with relatively completed data on all of the variables. The majority were women (83.3%), were 55 to 64 years of age (36.5%), cared for a parent (43.9%), and were well-educated, that is had college or technical training and higher (86.4%). Over two-thirds (66.7%) rated themselves as healthy (1–3 on the frailty scale). Almost half (48.7%) were experiencing financial difficulty, 44.3% were providing care for 21 or more hours per week, and 13.4% were not confident about their ability to navigate health and community systems (See Table 1).
Table 1.
Caregiver socio-demographic variables.
| Variables and Values | N (%) | M (SD) |
|---|---|---|
| Sex | ||
| Women | 396 (83.5%) | |
| Men | 71 (15.0%) | |
| Non-Binary, Trans, Other | 7 (1.5%) | |
| Age | ||
| 15–24 | 7 (1.5%) | |
| 25–34 | 22 (4.6%) | |
| 35–44 | 37 (7.8%) | |
| 45–54 | 82 (17.3%) | |
| 55–64 | 173 (36.5%) | |
| 65–74 | 119 (25.1%) | |
| 75–84 | 32 (6.8%) | |
| 85–94 | 2 (0.4%) | |
| Relationship to receiver | ||
| Parent/In-Law | 208 (43.9%) | |
| Spouse/Partner | 91 (19.2%) | |
| Sibling | 33 (7.0%) | |
| Child | 99 (20.9%) | |
| Other Relative | 11 (2.3%) | |
| Friend/Neighbour | 12 (2.5%) | |
| Other | 20 (4.2%) | |
| Education | ||
| Grade school | 2 (0.4%) | |
| High school | 63 (13.3%) | |
| College/ Technical training | 175 (36.9%) | |
| University degree | 121 (25.5%) | |
| Postgraduate degree, professional designation | 110 (23.2%) | |
| Weekly Care Hours | ||
| ≤10 | 185 (39.0%) | |
| 11–20 | 78 (16.4%) | |
| 21–30 | 34 (7.2%) | |
| 31–40 | 32 (6.8%) | |
| 41–80 | 43 (9.1%) | |
| 81–120 | 49 (10.5%) | |
| 121–168 | 52 (11.0%) | |
| Financial hardship | ||
| None | 243(51.3%) | |
| A Few | 130 (27.4%) | |
| Moderate | 50 (10.5%) | |
| A Lot | 51 (10.7%) | |
| Navigation confidence | ||
| Very confident | 162 (34.2%) | |
| Confident | 188 (39.7%) | |
| Neutral | 56 (11.8%) | |
| A little confident | 46 (9.7%) | |
| Not at all confident | 22 (4.6%) | |
| Frailty (1–9) | 2.61 (1.32) | |
| 1–3 Good health | 321 (67.7%) | |
| 4–6 Frail | 152 (32.1%) | |
| 7–9 Severe Frailty | 1 (0.2%) | |
| Physical health changes in last year | ||
| Improved | 19 (4%) | |
| Remained same | 183 (39%) | |
| Deteriorated | 272 (57%) | |
| Mental health changes in last year | ||
| Improved | 16 (3%) | |
| Remained same | 132 (28%) | |
| Deteriorated | 36 (69%) | |
| Anxiety (20–80) | 48.45 (13.51) | |
| ≤41 Low anxiety | 133 (28.1%) | |
| >42 Moderate-high | 341 (71.9%) | |
| Social Loneliness (0–3) | 2.13 (1.17) | |
3.2. Caregiver Factors Associated with Caregiver’s Anxiety
Table 2 summarizes the hierarchal linear regression models testing the independent associations between demographics, stressors, and perceived social support (social loneliness). Multicollinearity was not present (tolerance values were more than 0.1 and variance inflation factors were less than 10). See Supplementary File S3: Figure S1 Scatterplot with Loess curve to check homoscedasticity assumptions; Supplementary File S4: Figure S2 P-P Plot, checking for normality of estimation error assumption; and Supplementary File S5: Table S1 Correlations among key variables.
Table 2.
Hierarchical Linear Regressions Results of Caregiver Factors with Caregivers’ Anxiety.
| Standardized β | 95% CI | p | |
|---|---|---|---|
| Demographic factors | R2 = 0.046 F = 11.33 (2,471), p < 0.001 | ||
| Age | −0.213 | −3.15, −1.28 | <0.001 |
| Gender | −0.060 | −4.80, 0.93 | 0.185 |
| Stressors | R2 = 0.308 F = 44.11 (4,467), p < 0.001 | ||
| Age | −0.116 | −20.3, −0.38 | 0.004 |
| Gender | −0.0922 | −5.44, −0.47 | 0.039 |
| Care work: hours weekly | 0.144 | 0.58,2.12 | <0.001 |
| Navigation confidence | 0.122 | 0.52, 2.43 | <0.003 |
| Financial Difficulty | 0.229 | 1.90, 4.24 | <0.001 |
| Frailty | 0.268 | 1.93, 3.67 | <0.001 |
| Perceived Social Support | R2 = 0.359 F = 37.12 (1,466), p < 0.001 | ||
| Age | −0 0.117 | −2.02, −0.42 | 0.003 |
| Gender | −0 0.098 | −5.53, −0.74 | 0.010 |
| Care work: hours weekly | 0.127 | 0.45,1.93 | 0.002 |
| Navigation confidence | 0.113 | 0.43, 2.28 | 0.004 |
| Financial Difficulty | 0.200 | 1.55, 3.81 | <0.001 |
| Frailty | 0.210 | 1.33, 3.05 | <0.001 |
| Social Loneliness | 0.241 | 1.87, 3.65 | <0.001 |
In step one, age and gender explained 4.6% of the variance in anxiety. Stressors, including weekly hours of care work, difficulty navigating, financial difficulty, and caregiver frailty explained an additional 25.3% of the variance in anxiety in step 2. In step 3, social loneliness explained an additional 5.3% of the variance in anxiety. In this final model, all the factors remained significantly and independently related to worse caregiver anxiety and explained 35.2% of the variance in anxiety.
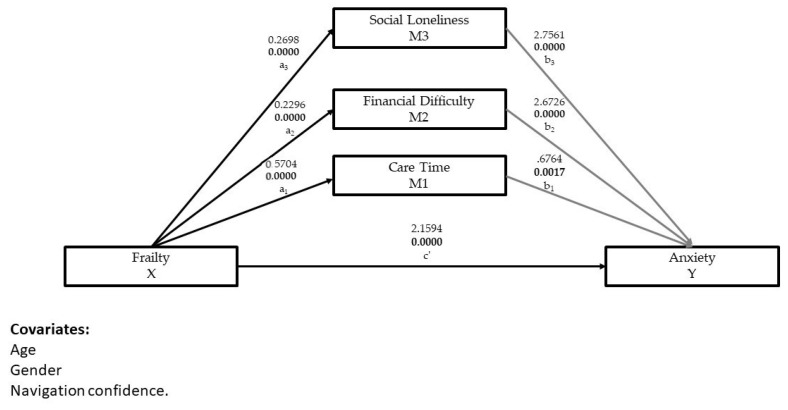
3.3. Testing the Parallel Mediation Model
Theoretically, we assumed that the direct effect of caregiver frailty on anxiety was mediated by weekly hours of care work, financial difficulty, and social loneliness. After controlling for age, gender, and navigation confidence, we used PROCESS Model 4 to determine the significance of the direct, indirect and total effects of a parallel mediation model. Results of the parallel mediation analysis indicate that frailty is indirectly related to anxiety through the relationships with care time, financial difficulty, and social loneliness. As can be seen in Figure 2 and Table 3, caregivers reporting more frailty reported higher levels of anxiety (β = 2.159, t = 4.909, 0.0005), more care time (β = 0.570, t = 6.302, 0.0005), financial difficulty (β = 0.229, t = 6.79, 0.0005), and social loneliness (β = 0.269, t = 6.525, 0.0005). The mediators care time (β = 0.676, t = 3.148, 0.0017), financial difficulty (β = 2.673, t = 4.635, 0.0005), and social loneliness (β = 2.756, t = 6.076, 0.0005) were also positively associated with anxiety. On the bias-correct bootstrap analysis, the total indirect effects of the mediators on care work, financial difficulty, and social loneliness (a1 + b1 + a2 + b2 + a3 + b3 = 1.743, 95% CI 1.226, 2.351) were significant, agreeing with our parallel mediation hypothesis. See Table 3.
Figure 2.
The parallel mediating effects of care time, financial difficulty, and social loneliness in a relationship between frailty and anxiety.
Table 3.
Testing weekly care work, financial difficulty, and social loneliness as mediators in the relationship between caregiver frailty and anxiety.
| Model Pathways | Coeff. β | Stan. Coeff. | SE | 95% CI | p | Model Summary | |
|---|---|---|---|---|---|---|---|
| Total effect of X Frailty on Y Anxiety | c | 3.903 | 0.439 | 3.04, 4.76 | 0.0005 | ||
| X Frailty to M1 Care work | a1 | 0.570 | 0.2879 | 0.091 | 0.393, 0.748 | 0.0005 | R2 = 0.088 F(4,469) = 11.368 p = 0.0005 |
| X Frailty to M2 Financial difficulty | a2 | 0.229 | 0.2952 | 0.034 | 0.163, 0.296 | 0.0005 | R2 = 0.174 F(4,469) = 24.651 p = 0.0005 |
| X Frailty to M3 Social Loneliness | a3 | 0.269 | 0.2960 | 0.041 | 0.189, 0.351 | 0.0005 | R2 = 0.101 F(4,469) = 13.172 p = 0.0005 |
| Direct Effect X Frailty to Y Anxiety | c’ | 2.159 | 0.2068 | 0.439 | 1.2949, 3.024 | 0.0005 | R2 = 0.228 F(4,469)=34.673 p = 0.0005 |
| M1 Care time to Y Anxiety | b1 | 0.676 | 0.1284 | 0.215 | 0.254, 1.099 | 0.0017 | |
| M2 Financial difficulty to Y Anxiety | b2 | 2.673 | 0.1992 | 0.5767 | 1.539, 3.806 | 0.0005 | |
| M3 Social loneliness to Y Anxiety | b3 | 2.756 | 0.2407 | 0.454 | 1.865, 3.647 | 0.0005 | |
| Indirect Effects of X on Y | |||||||
| Total Indirect effects of X (a1 + b1 + a2 + b2 + a3 + b3) | 1.743 | 0.289 | 1.226, 2.351 | Sig | |||
| Care time (a1 + b1) | 0.386 | 0.151 | 0.119, 0.716 | Sig | |||
| Financial difficulty (a2 + b2) | 0.614 | 0.178 | 0.297, 0.986 | Sig | |||
| Social loneliness (a3 + b3) | 0.744 | 0.177 | 0.429, 1.125 | Sig |
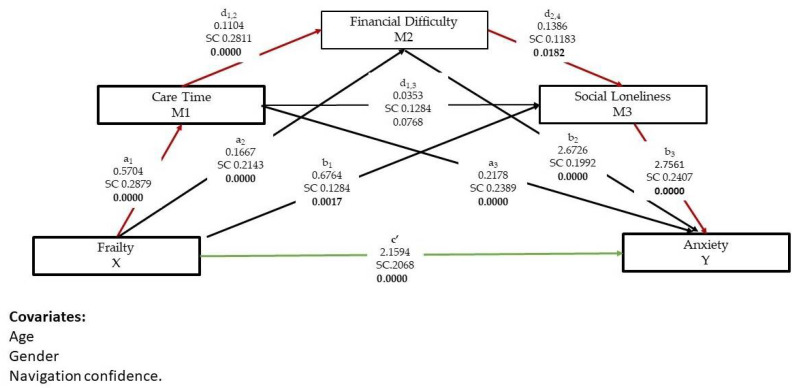
3.4. Testing the Serial Mediation Analysis
The serial mediation model assumes that there is a causal path from M1 care time to M2 financial difficulty to M3 social loneliness, and estimates this effect, whereas the parallel model assumes the effect is zero. After controlling for age, gender, and navigation confidence, we used PROCESS Model 6 to determine the significance of the direct, indirect and total effects of the serial mediation model. See Table 4. The total effect consists of a direct effect c’, from X frailty to Y anxiety and seven specific indirect effects (Figure 3). The direct effect c’ of frailty (X) on the anxiety (Y) is 2.16. The effect is significant (p = 0.0005). In other words, when controlling for other variables in the model, anxiety will increase by 2.16 points for a 1-point difference on the frailty scale.
Table 4.
Serial mediators in the relationship between caregiver frailty and anxiety.
| Model Pathways | Coeff. β | Stan. Coeff | SE | 95% CI | p | Model Summary | |
|---|---|---|---|---|---|---|---|
| Total effect of X on Y | c | 3.903 | 0.439 | 3.040, 4.765 | 0.0005 | ||
| X Frailty to Y Anxiety | c’ | 2.159 | 0.2068 | 0.439 | 1.295,3.024 | 0.0005 | |
| X Frailty to M1 Care work | a1 | 0.570 | 0.2879 | 0.091 | 0.393, 0.748 | 0.0005 | R2 = 0.077 F(4,470) = 9.838 p = 0.0005 |
| X Frailty to M2 Financial difficulty | a2 | 0.183 | 0.2143 | 0.034 | 0.117, 0.249 | 0.0005 | R2 = 0.246 F(5,468) = 30.498 p = 0.0005 |
| M1 Care time to M2 Financial difficulty | d1,2 | 0.110 | 0.2811 | 0.017 | 0.078, 0.143 | 0.0005 | |
| X Frailty to M3 Social loneliness | a3 | 0.218 | 0.2389 | 0.044 | 0.132, 0.304 | 0.0005 | R2 = 0.123 F(6,467) = 10.874 p = 0.0005 |
| M1 Care time to M3 Social loneliness | d1,3 | 0.035 | 0.0768 | 0.022 | −0.008, 078 | 0.1068 | |
| M2 Financial difficulty to M3 Social Support | d2,4 | 0.139 | 0.1183 | 0.059 | 0.024, 0.254 | 0.0182 | |
| Direct Effect X Frailty to Y Anxiety | c’ | 2.159 | 0.2068 | 0.439 | 1.295, 3.024 | 0.0005 | R2 = 0.359 F(7,466) = 37.227 p = 0.0005 |
| M1 Care time to Y Anxiety | b1 | 0.6764 | 0.1284 | 0.215 | 0.254, 1.099 | 0.0017 | |
| M2 Financial difficulty to Y Anxiety | b2 | 2.673 | 0.1192 | 0.577 | 1.539, 3.806 | 0.0005 | |
| M3 Social loneliness to Y Anxiety | b3 | 2.756 | 0.2407 | 0.454 | 1.865, 3.67 | 0.0005 | |
| Indirect effects of X on Y | |||||||
| Total Indirect effects of X (a1 + b1 + a2 + b2 + a3 + b3) | 1.743 | 0.1670 | 0.297 | 1.209, 2.369 | Sig. | ||
| X Frailty to M1 Care time to Y Anxiety | 0.386 | 0.0370 | 0.151 | 0.119, 0.707 | Sig. | ||
| X Frailty to M2 Financial Difficulty to Y Anxiety | 0.446 | 0.0427 | 0.142 | 0.203, 0.759 | Sig. | ||
| X Frailty to M3 Social loneliness to Y Anxiety | 0.600 | 0.0575 | 0.170 | 0.306, 0.976 | Sig. | ||
| X Frailty to M3 Social loneliness to Y Anxiety | 0.168 | 0.0161 | 0.061 | 0.069, 0.307 | Sig. | ||
| X Frailty to M1 Care time to M3 Social loneliness to Y Anxiety | 0.056 | 0.0053 | 0.036 | −0.011, 0.131 | Not (includes 0) | ||
| X Frailty to M2 Financial Difficulty to M3 Social loneliness to Y Anxiety | 0.064 | 0.0061 | 0.302 | 0.014, 0.129 | Sig. | ||
| X Frailty to M1 Care time to M2 Financial to M3 Social loneliness to Y Anxiety | 0.024 | 0.0023 | 0.114 | 0.005, 049 | Sig. | ||
Figure 3.
The serial mediating effects of care time, financial difficulty and social loneliness in a relationship between frailty and anxiety.
Calculating the indirect effects requires computing the model pathway from frailty to care time (M1) to financial difficulty (M2) to social loneliness (M3) to anxiety. The 95% bias corrected confidence interval based on 5000 bootstrap samples indicated the indirect effects (a1 + b1 + a2 + b2 + a3 + b3 = 1.743, SE 0.297) to be entirely above zero (1.209, 2.369). Following Hayes [55], it was significant as the bootstrapping 95% confidence interval does not contain 0. This result lends support to the serial mediating role of care time, financial difficulty, and social loneliness in increasing family caregiver anxiety. Notably the serial mediation model pathway frailty to care time (M1) to social loneliness (M3) to anxiety that did not include financial difficulty (M2) was not significant (β = 0.056, SE 0.036, CI-0.011, 0.131). Moreover, caregivers with greater frailty reported greater anxiety even after taking into account frailty’s indirect effects through care time, financial distress, and social loneliness (c’= 2.159, p = 0.0005).
4. Discussion
In this analysis, we were interested not only in the factors related to family caregiver anxiety, but also in hypothesizing how those effects occur. In regression analysis after controlling for gender and age, social loneliness (β = 0.245), frailty (β = 0.199), financial difficulty (β = 0.196), weekly care time (β = 0.143), and navigation confidence (β = 0.131) were all significant. We then used mediation analysis to evaluate the hypothesis that caregiver’s health measured as frailty transmitted its effect on anxiety during the COVID-19 pandemic.
Analysis confirmed our hypothesis that increasing weekly care time would likely increase financial difficulty which in turn would lead to social loneliness, and together positively mediated the effect of caregiver frailty on caregiver anxiety. In the serial mediation analysis, two caregivers that differ by one scale point in frailty are estimated to differ by 3.90 units in anxiety, with the frailer caregivers reporting higher anxiety. They differ by 1.74 units in anxiety as a result of the positive effect of frailty through weekly care work, which in turn is associated with more financial difficulty, social loneliness and anxiety. Independent of the mechanism of the indirect effects of weekly care work, financial difficulty, and social loneliness, the two caregivers are estimated to differ by 2.12 units in anxiety, with the more stressed frail caregiver reporting higher anxiety.
Smagula’s 2017 research [30] makes the link between increased anxiety from caregiving and the caregiver’s poor health measured in terms of white matter damage, yet caregiver frailty is often not considered in the caregiving research. In this study, about a third of caregivers rated themselves as moderately frail, that is, more tired, having more trouble obtaining supports, and/or needing practical or physical assistance with finances, transportation, or heavy housework (See scale in supplementary materials) [50]. Frailty is a public health measure that indicates increased risk of poor health [56,57,58]. Rockwood’s [56] notion in frailty is that as problems with health accumulate, they start to erode higher order functions like being able to “think and do as they please; look after themselves, interact with other people, and move about without falling” (p. 254).
We hypothesized that caregiver frailty, characterized by a decline in functioning across multiple physiological symptoms [49], would make it more exhausting to provide care as well as to coordinate and manage care. Numerous studies associate caregiver health with caregiver burden and distress [13,59,60,61]. Many authors propose that caregiving can adversely affect caregivers’ psychological and physical health [62,63,64,65], and that poor health will also increase distress [66,67,68,69,70,71]. Notably, in our serial mediation model, caregivers with greater frailty reported greater anxiety even after taking into account frailty’s indirect effect through care time, financial distress, and social loneliness.
Frail caregivers would benefit from a comprehensive frailty assessment and person-centered preventative approaches to improve their wellbeing [29,50]. In this survey we used the self-assessment version of the Clinical Frailty Scale [50] piloted to understand if assessing people’s risks and needs, and then facilitating referrals to healthcare and community resources could remediate frailty. Although identification and treatment of frailty is not currently standard practice in primary care [62], there is mounting evidence that assessing frailty in primary care and then person-centered intervention is feasible [72,73,74,75,76,77]. Frail caregivers would benefit from a comprehensive frailty assessment and person-centered preventative approaches to improve their wellbeing [29,50].
It is not surprising that weekly hours of care time mediated anxiety in this analysis. Caregiver distress begins to rise significantly for those providing over 21 hours of care per week [31,32]. Weekly care time and care intensity increased substantially at the outset of the COVID-19 pandemic as home care supports and respite were reduced, and day programs closed in order to redirect healthcare resources into acute care and reduce risk of COVID transmission [34,35,78]. Caregivers reported that without stimulation and social interaction, the care-receiver’s health deteriorated, which increased their care time and intensity. COVID-19 sanitation protocols also increased care time. In this survey, over half of the caregivers reported that their physical health (58%) and mental health (69%) deteriorated. Family caregivers would benefit from being asked about their situations by healthcare providers and access to more homecare supports.
Just under half (47.7%) of these caregivers reported that they were experiencing financial hardships due to their caregiving. Keating and colleagues’ taxonomy of care costs revealed three cost domains: employment consequences, care work, and care-related out of pocket costs [39]. In 2014, compared to before they started caring, Carers UK reported that caregivers experienced higher utility bills (77%), transportation costs (67%) and also spent more on cleaning products, food and clothing [79]. Qualitatively, in this survey, many caregivers reported they had to reduce their work hours or quit work to provide care.
We also asked caregivers what care expenses were higher since the COVID-19 pandemic was declared. They reported that during the COVID-19 pandemic they experienced higher food costs (44%); personal protective equipment and supplies (40%); care supplies such as incontinence products, meal replacements, bandages (29%); over the counter medical expenses (26%); mobility equipment like walkers and wheelchairs (17%); and household expenses (utility bills, rent, taxes, insurance) (24%). Extra expenses and financial distress can result in caregivers having to reduce their own expenses [39]. In addition to reducing their opportunities to save or invest, they may have to reduce spending on discretionary activities that bring them joy [39]. Poverty is the single largest determinant of health [80], and ill health is an obstacle to sustaining care [13,15,16]. We need to raise awareness of the effects of caregiving on incomes, employment, and pension credits.
Loneliness and social isolation also increased as the result of public health physical and social distancing protocols [23,24,81]. Our findings indicate that the association between frailty and loneliness was also moderated by social loneliness. In this survey the proportions of caregivers reporting that their social networks were lacking was high: 74% did not have enough people to rely on when they have problems, 73% did not have enough people they could trust completely, and 66% did not have enough people they felt close to. Social support from family and friends that typically is associated with reduced anxiety [40,41] was not available in the COVID-19 pandemic. Loneliness carries the same risk to health as smoking 15 cigarettes a day and being an alcoholic [82], thus ensuring that family caregivers have time to maintain their social networks should be a public health priority.
Strengths and Limitations
This study has several limitations. First, we cannot equivocally claim that weekly care time, financial difficulty, and social loneliness cause anxiety. This is a cross-sectional study. We are basing our analysis on theoretical arguments which Andrew Hayes [55] suggests does not explicitly establish cause, stating that “one can conduct a mediation analysis even if one cannot unequivocally establish causality” (pg. 81). Second, these measures were all self-reported. The frailty measure, in particular, may be prone to a social desirability bias. In this survey the ratings went from 1, the least frailty, to 9, the most frailty. Rasaih and colleagues found that older people rated frailty higher when ratings went from most to least frailty [50]. Third, while anxiety and social loneliness were rated on well validated scales and were thus less subject to desirability bias, they are still self-report tools. They cannot be considered as reliable as objective diagnostic tools.
Despite these limitations, there are strengths. This study mirrors many other studies that demonstrated worldwide increases in caregiver anxiety, care work, financial difficulty, loneliness, and care work [23,24,25,26,43,78,81,83,84]. We used regression analysis and validated scales to examine the factors related to anxiety and then used mediation analysis to test hypotheses about the processes by which giving care can cause anxiety. Typically, anxiety rises as care responsibilities, exhaustion, and worry increase [67], and in this study, moderation analysis confirmed that increased weekly care hours, financial distress, and social loneliness were significant factors. While anxiety is a known risk factor for poor health [67], mediation analysis demonstrated that frailty also increases anxiety directly and indirectly. This implies that healthcare providers should routinely assess family caregivers’ frailty and distress.
5. Conclusions
Our findings provide some insight into the relationship between caregivers’ health, measured as frailty, and their anxiety. Frailty levels were directly related to levels of caregivers’ anxiety and also indirectly moderated through weekly hours of care work, financial distress, and social loneliness. The proportions of family caregivers who were moderately frail, anxious, and experiencing social loneliness after eighteen months of the COVID-19 pandemic found in this survey should be of concern to policy makers and healthcare providers.
Acknowledgments
We thank the interview and survey participants for their time.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19148636/s1, Supplementary File S1: Survey Questions; Supplementary File S2: Self-Report version of the Clinical Frailty Scale; Supplementary File S3: Figure S1 Scatterplot with Loess curve to check homoscedasticity assumptions; Supplementary File S4: Figure S2 P-P Plot, checking for normality of estimation error assumption; Supplementary File S5: Supplementary Table Correlations among key variables; Supplementary File S6: CHERRIES Checklist for Reporting Results of Internet E-Surveys.
Author Contributions
Conceptualization, S.A. and J.P.; methodology, S.A., T.L., J.P., L.C., B.D. and P.G.J.T.; software, S.A., J.P., B.D. and P.G.J.T.; validation, S.A., J.P., T.L., L.C., B.D. and P.G.J.T.; formal analysis, S.A., J.P., B.D. and P.G.J.T.; investigation, S.A., J.P., T.L., L.C., B.D. and P.G.J.T.; resources, S.A., J.P., B.D. and P.G.J.T.; data curation, S.A., J.P. and T.L.; writing—original draft preparation, S.A.; writing—review and editing, S.A., J.P., T.L., L.C., B.D. and P.G.J.T.; visualization, S.A., J.P., B.D. and P.G.J.T.; supervision, J.P.; project administration, S.A.; funding acquisition, J.P., B.D. and P.G.J.T. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Health Ethics Research Board of the University of Alberta (PRO-00097996 9 June 2020 to 28 April 2023).
Informed Consent Statement
Participants provided implied consent by continuing to the survey after reading the information about the study.
Data Availability Statement
Data belong to the survey Impact of COVID-19 on Family Caregivers in Alberta and the data are owned by Jasneet Parmar the principal investigator. People interested in obtaining the data set can contact Sharon Anderson, research coordinator of the study. Email sdanders@ualberta.ca.
Conflicts of Interest
The authors declare that they have no conflicts of interest. The funder had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Funding Statement
This research was funded by the Northern Alberta Academic Family Medicine Fund R15P02.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fast J. Value of Family Caregiving in Canada. University of Alberta; Edmonton, AB, Canada: 2022. [(accessed on 28 February 2022)]. Available online: https://rapp.ualberta.ca/wp-content/uploads/sites/49/2022/02/Family-caregiving-worth-97-billion_2022-02-20.pdf. [Google Scholar]
- 2.Buckner L., Yeandle S. Valuing Carers 2015: The Rising Value of Carers’ Support. Carers UK; London, UK: 2015. [(accessed on 21 January 2016)]. Available online: https://www.carersuk.org/for-professionals/policy/policy-library?task=download&file=policy_file&id=5479. [Google Scholar]
- 3.American Association of Retired Persons . Caregiving in the U.S. American Association of Retired Persons & National Alliance for Caregiving; Washington, DC, USA: 2021. [(accessed on 28 February 2022)]. Available online: https://www.caregiving.org/wp-content/uploads/2021/01/full-report-caregiving-in-the-united-states-01-21.pdf. [Google Scholar]
- 4.Centers for Disease Control and Prevention . Caregiving for Family and Friends—A Public Health Issue. Centers for Disease Control and Prevention; Washington, DC, USA: 2019. [(accessed on 28 February 2022)]. Available online: https://www.cdc.gov/aging/agingdata/docs/caregiver-brief-508.pdf. [Google Scholar]
- 5.Talley R.C., Crews J.E. Framing the public health of caregiving. Am. J. Public Health. 2007;97:224–228. doi: 10.2105/AJPH.2004.059337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Committee on Family Caregiving for Older Adults. Board on Health Care Services. Health and Medicine Division . In: Families Caring for an Aging America. Schulz R., Eden S., editors. Health and Medicine Division; National Academies of Sciences, Engineering and Medicine; Washington, DC, USA: 2016. [PubMed] [Google Scholar]
- 7.Canadian Institutes of Health Information . Supporting Informal Caregivers: The Heart of Home Care. Canadian Institutes of Health Information; Ottawa, ON, Canada: 2010. [(accessed on 28 February 2022)]. Available online: https://secure.cihi.ca/free_products/Caregiver_Distress_AIB_2010_EN.pdf. [Google Scholar]
- 8.Barken R., Lowndes R. Supporting family involvement in long-term residential care: Promising practices for relational care. Qual. Health Res. 2018;28:60–72. doi: 10.1177/1049732317730568. [DOI] [PubMed] [Google Scholar]
- 9.Gaugler J.E. Family involvement in residential long-term care: A synthesis and critical review. Aging Ment. Health. 2005;9:105–118. doi: 10.1080/13607860412331310245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puurveen G., Baumbusch J., Gandhi P. From Family involvement to family inclusion in nursing home settings: A critical interpretive synthesis. J. Fam. Nurs. 2018;24:60–85. doi: 10.1177/1074840718754314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedman E.M., Rodakowski J., Schulz R., Beach S.R., Martsolf G.R., James A.E. Do family caregivers offset healthcare costs for older adults? A mapping review on the costs of care for older adults with versus without caregivers. Gerontologist. 2019;59:e535–e551. doi: 10.1093/geront/gny182. [DOI] [PubMed] [Google Scholar]
- 12.Kumagai N. Distinct Impacts of high-intensity caregiving on caregivers’ mental health and continuation of caregiving. Health Econ. Rev. 2017;7:1. doi: 10.1186/s13561-017-0151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulz R., Beach S.R., Friedman E.M., Martsolf G.R., Rodakowski J., Everette James A. Changing structures and processes to support family caregivers of seriously ill patients. J. Palliat. Med. 2018;21:S36–S42. doi: 10.1089/jpm.2017.0437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bom J., Bakx P., Schut F., Van Doorslaer E. The impact of informal caregiving for older adults on the health of various types of caregivers: A systematic review. Gerontologist. 2019;59:e629–e642. doi: 10.1093/geront/gny137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barbosa F., Voss G., Delerue Matos A. Do European co-residential caregivers aged 50+ have an increased risk of frailty? Health Soc. Care Community. 2020;2:2418–2430. doi: 10.1111/hsc.13064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barbosa F., Voss G., Delerue Matos A. Health impact of providing informal care in Portugal. BMC Geriatr. 2020;20:440. doi: 10.1186/s12877-020-01841-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith L., Shin J.I., Oh H., López Sánchez G.F., Underwood B., Jacob L., Veronese N., Soysal P., Butler L., Barnett Y., et al. Anxiety symptoms among informal caregivers in 47 low- and middle-income countries: A cross-sectional analysis of community-based surveys. J. Affect. Disord. 2022;298:532–539. doi: 10.1016/j.jad.2021.11.029. [DOI] [PubMed] [Google Scholar]
- 18.Zhu X.R., Zhu Z.R., Wang L.X., Zhao T., Han T. Prevalence and risk factors for depression and anxiety in adult patients with epilepsy: Caregivers’ anxiety and place of residence do matter. Epilepsy Behav. 2022;129:108628. doi: 10.1016/j.yebeh.2022.108628. [DOI] [PubMed] [Google Scholar]
- 19.Sharma R., Jafra B.S., Tiewsoh K., Kumar K., Kaur N., Sharawat I.K., Dawman L. Distress, anxiety, and its correlates among caregivers of children with kidney diseases during covid-19 pandemic lockdown. Arch. Pediatrie. 2022;29:243–248. doi: 10.1016/j.arcped.2022.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tay D.L., Iacob E., Reblin M., Cloyes K.G., Jones K.G., Hebdon M.C.T., Mooney K., Beck A.C., Ellington L. What contextual factors account for anxiety and depressed mood in hospice family caregivers? Psycho-Oncology. 2022;31:316–325. doi: 10.1002/pon.5816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackenzie I. Caregivers in Distress: A Growing Problem. Office of the Seniors Advocate; Victoria, BC, Canada: 2017. [(accessed on 20 September 2017)]. Available online: https://www.seniorsadvocatebc.ca/app/uploads/sites/4/2017/08/Caregivers-in-Distress-A-Growing-Problem-Final.pdf. [Google Scholar]
- 22.Health Quality Ontario . The Reality of Caring: Distress among Caregivers of Home Care Patients. Queen’s Printer for Ontario; Toronto, ON, Canada: 2016. [(accessed on 20 September 2017)]. Available online: https://www.hqontario.ca/Portals/0/documents/system-performance/reality-caring-report-en.pdf. [Google Scholar]
- 23.Anderson S., Parmar J., Dobbs B., Tian P.G.J. A tale of two solitudes: Loneliness and anxiety of family caregivers caring in community homes and congregate care. Int. J. Environ. Res. 2021;18:10010. doi: 10.3390/ijerph181910010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beach S.R., Schulz R., Donovan R., Rosland A.M. Family caregiving during the covid-19 pandemic. Gerontologist. 2021;61:650–660. doi: 10.1093/geront/gnab049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bergmann M., Wagner M. The Impact of covid-19 on informal caregiving and care receiving across Europe during the first phase of the pandemic. Front. Public Health. 2021;9:673874. doi: 10.3389/fpubh.2021.673874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park S.S. Caregivers’ mental health and somatic symptoms during covid-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76:E235–E240. doi: 10.1093/geronb/gbaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bennett J.M., Fagundes C.P., Kiecolt-Glaser C.P. The chronic stress of caregiving accelerates the natural aging of the immune system. In: Bosch J., Phillips A., Lord J., editors. Immunosenescence. Springer; New York, NY, USA: 2013. pp. 35–46. [DOI] [Google Scholar]
- 28.Canevelli M., Bersani F.S., Sciancalepore F., Salzillo M., Cesari M., Tarsitani L., Pasquini M., Ferracuti S., Biondi M., Bruno G. Frailty in caregivers and its relationship with psychological stress and resilience: A cross-sectional study based on the deficit accumulation model. J. Frailty Aging. 2022;11:59–66. doi: 10.14283/jfa.2021.29. [DOI] [PubMed] [Google Scholar]
- 29.Giovannelli J., Pinon A., Lenain M., Cleys A.L., Lefebvre B., Capon N., Spychala S., Boulanger E., Cassagnaud P., Barthoulot M. The relationship between social deprivation and a frailty index of cumulative deficits in French middle-aged caregivers. BMC Geriatr. 2022;22:15. doi: 10.1186/s12877-021-02736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smagula S.F. Beach, S.; Rosso, S.; Newman, A.B., Schulz, R. Brain structural markers and caregiving characteristics as interacting correlates of caregiving strain. Am. J. Geriatr. Psychiatry. 2017;25:582–591. doi: 10.1016/j.jagp.2017.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pauley T., Chang B.W., Wojtak A., Seddon A., Hirdes J. Predictors of caregiver distress in the community setting using the home care version of the resident assessment instrument. Prof. Case Manag. 2018;23:60–69. doi: 10.1097/NCM.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 32.Sinn C.-L.J., Souza R., Betini D., Wright J., Eckler L., Chang B.W., Hogeveen S., Turcotte L., Hirdes J.P. Adverse events in home care: Identifying and responding with interrai scales and clinical assessment protocols. Can. J. Aging. 2018;37:60–69. doi: 10.1017/S0714980817000538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Canadian Institutes of Health Information . 1 in 3 Unpaid Caregivers in Canada Are Distressed. Canadian Institutes of Health Information; Ottawa, ON, Canada: 2020. [(accessed on 6 August 2021)]. Available online: https://www.cihi.ca/en/1-in-3-unpaid-caregivers-in-canada-are-distressed. [Google Scholar]
- 34.Sinn C.L.J., Sultan H., Turcotte L.A., McArthur C., Hirdes J.P. Patterns of home care assessment and service provision before and during the COVID-19 pandemic in Ontario, Canada. PLoS ONE. 2022;17:e0266160. doi: 10.1371/journal.pone.0266160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Duncan K.A., Shooshtari S., Roger K., Fast J., Han J. The cost of caring: Out-of-pocket expenditures and financial hardship among Canadian carers. Int. J. Care Caring. 2020;4:141–166. doi: 10.1332/239788220X15845551975572. [DOI] [Google Scholar]
- 36.Teng C., Sellars M., Pond D., Latt M.D., Waite L.M., Sinka V., Logeman C., Tong A. Making decisions about long-term institutional care placement among people with dementia and their caregivers: Systematic review of qualitative studies. Gerontologist. 2020;60:e329–e346. doi: 10.1016/j.jalz.2019.06.3548. [DOI] [PubMed] [Google Scholar]
- 37.Fast J. Caregiving for Older Adults with Disabilities: Present Costs, Future Challenges. Institute for Research on Public Policy; Montreal, QB, USA: 2015. [(accessed on 30 January 2016)]. Available online: https://irpp.org/wp-content/uploads/2015/12/study-no58.pdf. [Google Scholar]
- 38.Taylor M.G., Quesnel-Vallée A. The structural burden of caregiving: Shared challenges in the United States and Canada. Gerontologist. 2017;57:19–25. doi: 10.1093/geront/gnw102. [DOI] [PubMed] [Google Scholar]
- 39.Keating N.C., Fast J.E., Lero D.S., Lucas S.J., Eales J. A taxonomy of the economic costs of family care to adults. J. Econ. Ageing. 2014;3:11–20. doi: 10.1016/j.jeoa.2014.03.002. [DOI] [Google Scholar]
- 40.Stewart M., Barnfather A., Neufeld A., Warren S., Letourneau N., Liu L. Accessible support for family caregivers of seniors with chronic conditions: From isolation to inclusion. Can. J. Aging. 2006;25:179–192. doi: 10.1353/cja.2006.0041. [DOI] [PubMed] [Google Scholar]
- 41.Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psych. Bull. 1985;98:310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- 42.Gottlieb A., Golander H., Bar-Tal Y., Gottlieb D. The influence of social support and perceived control on handicap and quality of life after stroke. Aging Clin. Exp. Res. 2001;13:11–15. doi: 10.1007/BF03351488. [DOI] [PubMed] [Google Scholar]
- 43.Budnick A., Hering C., Eggert S., Teubner C., Suhr R., Kuhlmey A., Gellert P. Informal caregivers during the COVID-19 pandemic perceive additional burden: Findings from an ad-hoc survey in Germany. BMC Health Serv. Res. 2021;21:353. doi: 10.1186/s12913-021-06359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dhiman S., Sahu P.K., Reed W.R., Ganesh G.S., Goyal R.K., Jain S. Impact of covid-19 outbreak on mental health and perceived strain among caregivers tending children with special needs. Res. Dev. Disabil. 2020;107:103790. doi: 10.1016/j.ridd.2020.103790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Greenberg N.E., Wallick A., Brown L.M. Impact of covid-19 pandemic restrictions on community-dwelling caregivers and persons with dementia. Psychol. Trauma Theory Res. Pract. Policy. 2020;12:S220–S221. doi: 10.1037/tra0000793. [DOI] [PubMed] [Google Scholar]
- 46.L’Heureux T., Parmar J., Dobbs B., Charles L., Tian P.G.J., Sacrey L.-A., Anderson S. Rural family caregiving: A closer look at the impacts of health, care work, financial distress, and social loneliness on anxiety. Healthcare. 2022;10:1155. doi: 10.3390/healthcare10071155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Muscedere J., Andrew M.K., Bagshaw S.M., Estabrooks C., Hogan D., Holroyd-Leduc J., Howlett S., Lahey W., Maxwell C., McNally M., et al. Screening for frailty in Canada’s health care system: A time for action. Can. J. Aging. 2016;35:281–297. doi: 10.1017/S0714980816000301. [DOI] [PubMed] [Google Scholar]
- 48.Rockwood K. Rationing care in covid-19: If we must do it, can we do better? Age Ageing. 2021;50:3–6. doi: 10.1093/ageing/afaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rockwood K., Song X., MacKnight C., Bergman H., Hogan D.B., McDowell I., Mitnitski A. A global clinical measure of fitness and frailty in elderly people. Can. Med. Assoc. J. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rasiah J., O’Rourke T., Dompé B., Rolfson D., Mansell B., Pereira R., Chan T., McDonald K., Summach A. Customizing a program for older adults living with frailty in primary care. J. Prim. Care Community Health. 2021;12:21501327211034807. doi: 10.1177/21501327211034807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tluczek A., Henriques J.B., Brown R.L. Support for the reliability and validity of a six-item state anxiety scale derived from the State-Trait Anxiety Inventory. J. Nurs. Meas. 2009;17:19–28. doi: 10.1891/1061-3749.17.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br. J. Clin. Psych. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 53.Chlan L., Savik K., Weinert C. Development of a shortened State anxiety scale from the Spielberger State-Trait Anxiety Inventory (STAI) for patients receiving mechanical ventilatory support. J. Nurs. Meas. 2003;11:283–293. doi: 10.1891/jnum.11.3.283.61269. [DOI] [PubMed] [Google Scholar]
- 54.De Jong Gierveld J., Van Tilburg T. A 6-item scale for overall, emotional, and social loneliness—Confirmatory tests on survey data. Res. Aging. 2006;28:582–598. doi: 10.1177/0164027506289723. [DOI] [Google Scholar]
- 55.Hayes A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis. A Regression—Based Approach. 2nd ed. The Gilford Press; New York, NY, USA: 2018. [Google Scholar]
- 56.Rockwood K., Theou O. Using the clinical frailty scale in allocating scarce health care resources. Can. Geriatr. J. 2020;23:210–215. doi: 10.5770/cgj.23.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Theou O., Park G.H., Garm A., Song X., Clarke B., Rockwood K. Reversing frailty levels in primary care using the CARES model. Can. Geriatr. J. 2017;20:105–111. doi: 10.5770/cgj.20.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Theou O., Pérez-Zepeda M.U., Van Der Valk A.M., Searle S.D., Howlett S.E., Rockwood K. A classification tree to assist with routine scoring of the Clinical Frailty Scale. Age Ageing. 2021;50:1406–1411. doi: 10.1093/ageing/afab006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Afram B., Stephan A., Verbeek H., Bleijlevens M.H.C., Suhonen R., Sutcliffe C., Raamat K., Cabrera E., Soto M.E., Hallberg I.R., et al. Reasons for Institutionalization of People with Dementia: Informal Caregiver Reports From 8 European Countries. J. Am. Med. Dir. Assoc. 2014;15:108–116. doi: 10.1016/j.jamda.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 60.Alvira M.C., Risco E., Cabrera E., Farré M., Rahm Hallberg I., Bleijlevens M.H.C., Meyer G., Koskenniemi J., Soto M.E., Zabalegui A., et al. The association between positive-negative reactions of informal caregivers of people with dementia and health outcomes in eight European countries: A cross-sectional study. J. Advan. Nurs. 2015;71:1417–1434. doi: 10.1111/jan.12528. [DOI] [PubMed] [Google Scholar]
- 61.Bevans M., Sternberg E.M. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012;307:398–403. doi: 10.1001/jama.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Adelman R.D., Tmanova L.L., Delgado D., Dion S., Lachs M.S. Caregiver Burden A Clinical Review. JAMA. 2014;311:1052–1059. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- 63.Allen A.P., Curran E.A., Duggan A., Cryan J.F., Chorcorain A.N., Dinan T.G., Molloy D.W., Kearney P.M., Clarke G. A systematic review of the psychobiological burden of informal caregiving for patients with dementia: Focus on cognitive and biological markers of chronic. Neurosci. Biobehav. Rev. 2017;73:123–164. doi: 10.1016/j.neubiorev.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 64.Bauer J.M., Sousa-Poza A. Impacts of informal caregiving on caregiver employment, health, and family. J. Pop. Ageing. 2015;8:113–145. doi: 10.1007/s12062-015-9116-0. [DOI] [Google Scholar]
- 65.Bosco N. Caring for carers. Implications and repercussions of reduced attention to family caregivers on individual health and collective wellbeing. Sociol. Lav. 2018:120–135. doi: 10.3280/SL2018-150007. [DOI] [Google Scholar]
- 66.Ahmed R., Bruce S., Jurcik T. Towards a socioecological framework to support mental health caregivers: Implications for social work practice and education. Soc. Work Ment. Health. 2018;16:105–122. doi: 10.1080/15332985.2017.1336744. [DOI] [Google Scholar]
- 67.Del-Pino-Casado R., Priego-Cubero E., López-Martínez C., Orgeta V. Subjective caregiver burden and anxiety in informal caregivers: A systematic review and meta-analysis. PLoS ONE. 2021;16:e0247143. doi: 10.1371/journal.pone.0247143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jansen L., Dauphin S., van den Akker M., De Burghgraeve T., Schoenmakers B., Buntinx F. Prevalence and predictors of psychosocial problems in informal caregivers of older cancer survivors—A systematic review: Still major gaps in current research. Eur. J. Cancer Care. 2018;27:e12899. doi: 10.1111/ecc.12899. [DOI] [PubMed] [Google Scholar]
- 69.Kimura N.R.S., Neto J.P.S., Santos R.L., Baptista M.A.T., Portugal G., Johannessen A., Barca M.L., Engedal K., Laks J., Rodrigues V.M., et al. Resilience in carers of people with young-onset Alzheimer disease. Int. J. Geriatr. Psychiatry. 2019;32:59–67. doi: 10.1177/0891988718824039. [DOI] [PubMed] [Google Scholar]
- 70.Moss K.O., Kurzawa C., Daly B., Prince-Paul M. Identifying and addressing family caregiver anxiety. J. Hosp. Palliat. Nurs. 2019;21:14–20. doi: 10.1097/NJH.0000000000000489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rozwadowski M., Dittakavi M., Mazzoli A., Hassett A.L., Braun T., Barton D.L., Carlozzi N., Sen S., Tewari M., Hanauer D.A., et al. Promoting health and well-being through mobile health technology (roadmap 2.0) in family caregivers and patients undergoing hematopoietic stem cell transplantation: Protocol for the development of a mobile randomized controlled trial. JMIR Res. Protoc. 2020;9:e19288. doi: 10.2196/19288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cezar N.O.D.C., Aprahamian I., Ansai J.H., de Oliveira M.P.B., da Silva D.C.P., Gomes W.D.L., Barreiros B.A., Langelli T.D.C.O., de Andrade L.P. Feasibility of reducing frailty components in older adults with Alzheimer’s dementia: A randomized controlled home-based exercise trial (AD-HOMEX) Exp. Gerontol. 2021;150:111390. doi: 10.1016/j.exger.2021.111390. [DOI] [PubMed] [Google Scholar]
- 73.Nwagwu V.C., Cigolle C., Suh T. Reducing Frailty to Promote Healthy Aging. Clin. Geriatr. Med. 2020;36:613–630. doi: 10.1016/j.cger.2020.06.005. [DOI] [PubMed] [Google Scholar]
- 74.Ghosh T.S., Rampelli S., Jeffery I.B., Santoro A., Neto M., Capri M., Giampieri E., Jennings A., Candela M., Turroni S., et al. Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: The NU-AGE 1-year dietary intervention across five European countries. Gut. 2020;69:1218–1228. doi: 10.1136/gutjnl-2019-319654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Akpan A., Roberts C., Bandeen-Roche K., Batty B., Bausewein C., Bell D., Bramley D., Bynum J., Cameron I.D., Chen L.K., et al. Standard set of health outcome measures for older persons. BMC Geriatr. 2018;18:36. doi: 10.1186/s12877-017-0701-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee D.R., Santo E.C., Lo J.C., Ritterman Weintraub M.L., Patton M., Gordon N.P. Understanding functional and social risk characteristics of frail older adults: A cross-sectional survey study. BMC Fam. Pract. 2018;19:170. doi: 10.1186/s12875-018-0851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee S.C., Tsai J.M., Tsai L.Y., Liang L.J., Wu C.P. Promoting physical activity and reducing frailty of middle-aged and older adults in community: The effects of a health promotion program combining smartphone learning and exercise. Int. J. Gerontol. 2019;13:320–324. doi: 10.6890/IJGE.201912_13(4).0011. [DOI] [Google Scholar]
- 78.Giebel C., Lion K., Mackowiak M., Chattat R., Kumar P.N.S., Cations M., Gabbay M., Moyle W., Ottoboni G., Rymaszewska J., et al. A qualitative 5-country comparison of the perceived impacts of COVID-19 on people living with dementia and unpaid carers. BMC Geriatr. 2022;22:116. doi: 10.1186/s12877-022-02821-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carers UK . Caring and Family Finances Inquiry. UK Report. Carers UK; London, UK: 2014. [(accessed on 24 April 2020)]. Available online: https://www.carersuk.org/for-professionals/policy/policy-library?task=download&file=policy_file&id=219. [Google Scholar]
- 80.Taylor L.A., Tan A.X., Coyle C.E., Ndumele C., Rogan E., Canavan M., Curry L.A., Bradley E.H. Leveraging the social determinants of health: What works? PLoS ONE. 2016;11:e0160217. doi: 10.1371/journal.pone.0160217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Messina A., Lattanzi M., Albanese E., Fiordelli M. Caregivers of people with dementia and mental health during covid-19: Findings from a cross-sectional study. BMC Geriatr. 2022;22:56. doi: 10.1186/s12877-022-02752-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 83.Irani E., Niyomyart A., Hickman R.L. Family Caregivers’ Experiences and Changes in Caregiving Tasks During the COVID-19 Pandemic. Clin. Nurs. Res. 2021;30:1088–1097. doi: 10.1177/10547738211014211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rosalynn Carter Institute for Caregiving . Caregivers in Crisis: A report on the Impacts of the Covid-19 Pandemic on the Mental Health and Well-Being of Caregivers. Rosalind Carter Institute for Caregiving; Americus, GA, USA: 2020. [(accessed on 30 December 2020)]. Available online: https://www.rosalynncarter.org/caregivers-in-crisis-rosalynn-carter-institute-report-sounds-the-alarm-on-caregiving-in-the-time-of-covid/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data belong to the survey Impact of COVID-19 on Family Caregivers in Alberta and the data are owned by Jasneet Parmar the principal investigator. People interested in obtaining the data set can contact Sharon Anderson, research coordinator of the study. Email sdanders@ualberta.ca.